Abstract
Trabecular meshwork (TM) and ciliary muscle (CM) contraction and relaxation function together to provide control of outflow. The active role the TM plays in the regulation of intraocular pressure (IOP) is mediated by cytoskeletal and contractility mechanisms as well as signal/transduction factors that mediate its response to stressors. This complex system is altered with age and the glaucomas, and it can be difficult to differentiate between the various etiological effects/agents. Factors such as a compromised antioxidant defense system and altered extracellular matrix metabolism are known to contribute to impaired outflow and may be common to primary open-angle glaucoma (POAG), exfoliation syndrome (XFS) and exfoliation glaucoma (XFG). Genes differentially expressed in diseased ocular tissue or in cultured HTM cell models, and thus implicated in the disease process, include SOD2, ALDH1A1, MGST1, LOX and LOXL1, elements of the transforming growth factor-beta (TGFβ) / bone morphogenetic protein (BMP) / SMAD signaling pathways, connective tissue growth factor (CTGF), matrix metalloproteinase-2 (MMP-2), a tissue inhibitor of metalloproteinases also known as TIMP-2 and endothelin-1 (ET-1). In exfoliation syndrome and XFG fibrillar, proteinaceous extracellular material is produced in excess and accumulates in both outflow pathways but does not always lead to elevated IOP. Locally produced material may accumulate in the intertrabecular spaces, juxtacanalicular (JCT) meshwork and the inner wall of Schlemm’s canal as a result of a combination of both excessive synthesis and insufficient degradation. An increase in JCT plaque and decreased cellularity in the TM are thought to contribute to decreased outflow facility in glaucoma patients, but XFG patient specimens show reduced extracellular plaque material in the JCT, and the structural integrity of trabecular endothelial cells is mostly retained and cellularity remains unchanged. The distinctions between causes/effects of structural changes leading to reduced outflow/elevated IOP are important for developing effective, individualized treatment strategies.
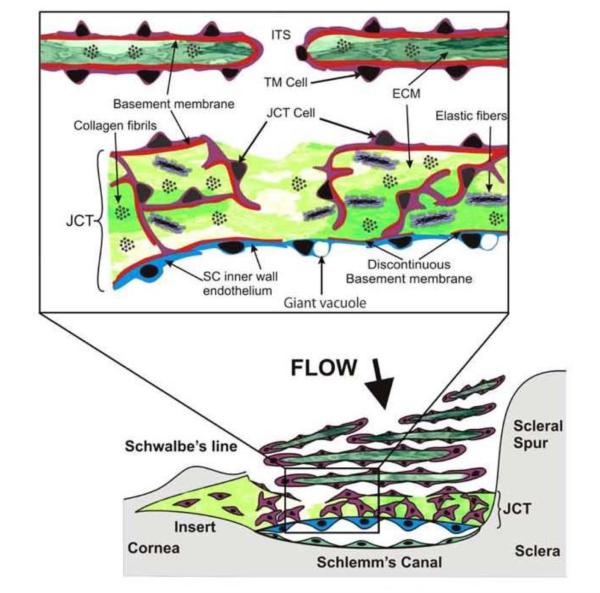
The trabecular outflow pathway is the main drainage system of aqueous humor in the eye. The core structures in the pathway are the trabecular meshwork (TM), the endothelial lining of Schlemm’s canal (SC), SC collector channels and aqueous veins. The TM has three distinct structural areas: the inner uveal meshwork, the corneoscleral meshwork and the juxtacanalicular (JCT) or cribriform region. The JCT is immediately adjacent to the inner wall of SC. (Fig 1) TM structure and experimental flow studies indicate that flow resistance is highest in the region of the JCT and the inner wall of SC, although the exact location/proportions of resistance are unclear.(1-5) The JCT contains an elastic-like network that connects to the inner wall endothelium of SC. The outer tendons of the ciliary muscle (CM), the corneoscleral TM, also insert into the network.(6,7) Contraction of the CM spreads the lamellated portion of the meshwork, expanding the area of filtration so that resistance is reduced.(7,8,9) The JCT region also contains electron microscopically optically empty spaces next to the inner wall endothelium, where giant vacuoles or pores are formed that open into SC. (10) It is thought that these spaces are aqueous humor pathways.
Figure 1.
Diagram of the outflow pathway and juxtacanalicular (JCT) or cribriform region. The lower portion of the figure shows a stylized view of the TM and the upper inset shows an expanded view of the JCT region. TM = trabecular meshwork, ECM = extracellular matrix, SC = Schlemm’s canal, ITS = intertrabecular space
Reprinted with permission from Acott TS, Kelley MJ Extracellular matrix in the trabecular meshwork. Exp Eye Res (2008) 86: 543-561.
Nerve endings have been identified in the scleral spur region that may be part of a mechanoreceptive system for responding to stress or strain in the connective tissue elements of the scleral spur, perhaps induced by ciliary muscle contraction or changes in intraocular pressure (IOP). (11) Morphologically distinct types, or proprioreceptors, are found in the CM. Receptors at the posterior muscle tips might measure stretch of the tendons, whereas the large mechanoreceptor-like endings located between the muscle tips and in the scleral spur region may respond to shear stress. With multiple types of intrinsic nerve cells, the contraction/relaxation of the CM might be able to respond locally to changes in the immediate environment. (12) Similarly cholinergic and nitrergic nerve terminals in contact with the elastic-like network of the TM and scleral spur could induce contraction and relaxation of TM and SS cells and also indicate some self regulatory ability.(13)
This configuration of structural elements illustrates how TM and CM contraction and relaxation function together to provide control of outflow and regulation of intraocular pressure (IOP). (14) Recent investigations into the role of endothelial nitric oxide (NO) synthase suggest that TM mechanosensitivity may be a part of the CM/TM homeostatic mechanism mediated in part by NO. (15) The active role that the TM plays in the regulation of IOP is also mediated by cytoskeleton and contractility mechanisms - the efferent arm of the reflexive and regulatory mechanism; their arrangement governs the final outflow facility. The endothelial NO synthase /NO system may be a signal/transduction arm that mediates response to the stressors, responses that are modulated afferently by the various sensors in the CM tendons, the CM apex and the TM itself. (16)
The synthesis and degradation of the TM extracellular matrix (ECM) also plays a role in outflow resistance and the glaucomatous disease process. (17 – 21) The ECM is comprised of a complex arrangement of fibronectin, collagen, laminin, proteoglycans, glycosaminoglycans, and matricellular proteins, which are mediated/modulated by elements of the transforming growth factor-b / bone morphogenetic protein / SMAD signaling pathways, connective tissue growth factor, matrix metalloproteinase-2, a tissue inhibitor of metalloproteinases also known as TIMP-2 and endothelin-1 (ET-1). (21 – 30) In addition, glucocorticoids and prostaglandin derivatives appear to modulate ECM turnover in the JCT.(31 – 35)
This complex system is altered with age and the glaucomas, and it can be difficult to differentiate between the various etiological effects/agents. With age, the number of TM cells decreases, pigmentation in TM cells increases, as does the incidence of cells detaching from trabeculae and adhesions between adjacent trabeculae.(36 - 38) An increase in accumulation of extracellular material in both the TM and CM is seen with increasing age, including in sheath-derived (SD) plaques and fibrillar material in the JCT, increasing outflow resistance in the TM outflow pathways (6, 39). These changes may be the result of imbalances in responses to age-related stresses such as oxidative damage to long-lived molecules, protein cross-linking and loss of elasticity that could in turn trigger an increase in production of factors such as transforming growth factor-b, interleukin-1 and CD44S, leading to increases in fibronectin and a decrease in the breakdown in ECM. (18, 20, 25, 35, 40, 41) Changes in the extracellular environment may result in decreases in outflow facility and uveoscleral outflow, which can contribute to an increase in IOP. (40, 42, 43)
Specimens of glaucomatous TM show fusion and thickening of trabecular lamellae, increased amounts SD plaque material in the JCT and an abundance of longspacing (lattice) collagen. (39, 40, 43, 44, 45) Quantitation of the area filled by the SD plaques reveals a significant increase of SD plaque material in glaucomatous eyes compared with normal eyes of a similar age range. The increase in SD plaque material is also inversely correlated with axon counts in the optic nerve, a measure of glaucomatous damage.(39, 44) Eyes with less damage (more axons) have smaller amounts of TM SD plaques than eyes with more damage (fewer axons). The decreased thickness of the JCT, thickened beams and shortening of the connecting fibrils found in the JCT elastic fiber network of glaucomatous eyes could reduce the ability of the tissue between the JCT and the inner wall of SC to expand. This reduces the amount of space for fluid flow and may diminish the influence of CM and TM contraction on outflow resistance. The resulting underperfusion of the TM could lead to an even greater increase in ECM buildup and tissue rigidity further increasing outflow resistance.(40, 46) Thus a self-perpetuating cycle could develop, which might be a factor in the pathogenesis of glaucoma.
The TM of glaucomatous eyes shows changes in glycosaminoglycan (GAG) composition with a decrease in hyaluronic acid (HA) and an increase in chondroitin sulfate (CS) both of which contribute to flow resistance and influence flow rate in vitro.(9, 45, 47 - 49) Factors such as a compromised antioxidant defense system and altered ECM metabolism are known to contribute to impaired outflow and may be common to primary open-angle glaucoma (POAG), exfoliation syndrome (XFS) and exfoliation glaucoma (XFG). (51-53)
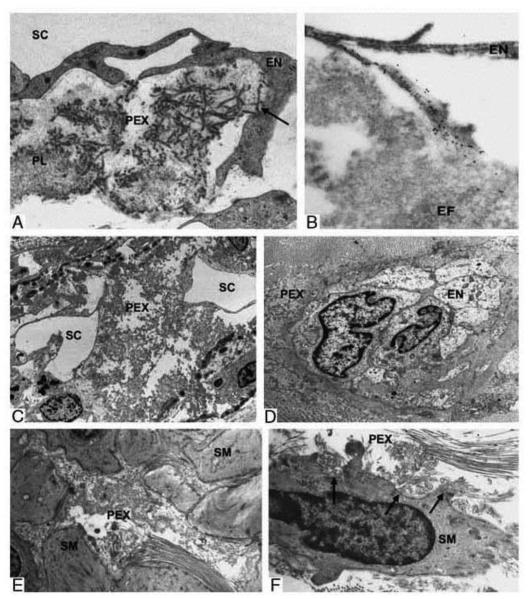
XFS is considered an age-related, systemic disorder that includes ocular indications.(54-55) In both XFS and XFG fibrillar, proteinaceous extracellular material (PEX) is produced in excess and accumulates in both outflow pathways.(51, 54, 56) PEX is found in isolated aggregates beneath the inner-wall endothelium of SC, as well as the uveal and JCT regions of the meshwork, which may limit aqueous access to the inner wall and SC.(56 - 58) (Fig 2) The dimensions of SC in POAG eyes are significantly smaller than those in normal eyes. (59) An inverse correlation between the amount of PEX material in the JCT and the length of the filtration region of SC indicates that eyes with larger amounts of PEX material also tend to have a smaller SC.(57) As noted above, increased SD plaques are correlated with fewer axons in the optic nerve in POAG.(44) In donor eyes with XFS the amount of PEX-material in the subendothelial region of SC was also inversely correlated with the number of axons in the optic nerve and was positively correlated with an increase in IOP, suggesting that the material contributes to an increase in outflow resistance.(56, 57) Both uveoscleral and trabecular outflow are reduced in XFG but only uveoscleral outflow is reduced in XFS, indicating that XFS might involve changes in the CM and its surrounding ECM.(60)
Figure 2.
Electron micrographs showing involvement of the outflow pathways in pseudoexfoliation (PEX) syndrome. A. Apparent production of PEX fibrils (arrow) by the inner wall endothelium (EN) of Schlemm canal (SC). B. Normal fibrillin-1 immunopositive (immunogold labelling) elastic microfibrils (EF) connecting Schlemm canal endothelium (EN) and juxtacanalicular plaques. C. Focal collapse and splitting of Schlemm canal (SC) by massive accumulation of PEX material. D. Collapse of aqueous vein showing accumulation of PEX material in its periphery (EN, vascular endothelium). E. Accumulation of PEX aggregates between smooth muscle (SM) cells of the anterior portion of the ciliary muscle. F. Apparent production of PEX fibrils by a smooth muscle cell of the ciliary muscle. Reprinted with permission from Schlötzer-Schrehardt U. Molecular pathology of pseudoexfoliation syndrome/glaucoma--new insights from LOXL1 gene associations. Exp Eye Res. 2009 Apr;88(4):776-85.
The presence of patches of PEX material in the uveal meshwork region suggests that PEX material washes into the meshwork from the aqueous. (57) PEX deposits may also be locally produced and accumulate in the intertrabecular spaces, JCT and the inner wall of SC.(56) The buildup of PEX is likely due to a combination of both excessive synthesis and insufficient degradation.(61) An increase in JCT plaques and decreased cellularity in the TM are thought to contribute to decreased outflow facility in glaucoma patients, but in TM specimens from XFG patients there is a reduction of extracellular plaque material in the JCT, the structural integrity of trabecular endothelial cells is mostly retained and TM cellularity remains unchanged. (8, 51, 56, 57, 58, 61, 62)
Understanding similarities and differences between aging, glaucoma and XFS/XFG will be critical for developing effective diagnostic and treatment strategies.
Acknowledgments
Conflicts of Interest and Source of Funding:
Supported by grants from the National Institutes of Health/National Eye Institute University of Wisconsin-Madison Core Grant for Vision Research (P30 EY016665); Research to Prevent Blindness, Inc., New York, NY, unrestricted departmental award; Ocular Physiology Research and Education Foundation
Footnotes
Author Disclosure Statement:
C.A. Rasmussen: No competing financial interests exist.
P.L. Kaufman: AGTC (C, R), Lens AR, Inc (F), WARF (F, P), Z Lens, LLC (F), Alcon (C, R), Allergan (C, R), Altheos, Inc (C, R), Bausch & Lomb (C, R), Amakem Therapeutics (C, R), Johnson & Johnson (C, R), Merck (C, R), Pfizer (C, R, F), Santen (F, C, R), Refocus (C, R). Honoraria (R), consultant (C), grants (F), patents (P)
References
- 1).Overby DR, Stamer WD, Johnson M. The changing paradigm of outflow resistance generation: toward synergistic models of the JCT and inner wall endothelium. Exp Eye Res. 2009;88:656–670. doi: 10.1016/j.exer.2008.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2).Rohen JW, Futa R, Lütjen-Drecoll E. The fine structure of the cribriform meshwork in normal and glaucomatous eyes as seen in tangential sections. Invest Ophthalmol Vis Sci. 1981;21:574–585. [PubMed] [Google Scholar]
- 3).Ethier CR, Kamm RD, Palaszewski BA, Johnson MC, Richardson TM. Calculations of flow resistance in the juxtacanalicular meshwork. Invest Ophthalmol Vis Sci. 1986;27:1741–1750. [PubMed] [Google Scholar]
- 4).Bill A, Svedbergh B. Scanning electron microscopic studies of the trabecular meshwork and the canal of Schlemm: An attempt to localize the main resistance to outflow of aqueous humor in man. Acta Ophthalmol. 1972;50:295. doi: 10.1111/j.1755-3768.1972.tb05954.x. [DOI] [PubMed] [Google Scholar]
- 5).Tripathi RC. Mechanism of the aqueous outflow across the trabecular wall of Schlemm's canal. Exp Eye Res. 1971;11:116–121. doi: 10.1016/s0014-4835(71)80073-8. [DOI] [PubMed] [Google Scholar]
- 6).Lütjen-Drecoll E, Rohen JW. Functional morphology of the trabecular meshwork. In: Bilyk J, Tasman W, Jaeger EA, editors. Duane's Foundations of Clinical Ophthalmology on CD-ROM. Vol. 1. Lippincott Williams & Wilkins, Vol; Philadelphia: 2006. pp. 1–28. Section 1, Ocular Anatomy, Embryology, and Teratology. [Google Scholar]
- 7).Lütjen-Drecoll E, Futa R, Rohen JW. Ultrahistochemical studies on tangential sections of the trabecular meshwork in normal and glaucomatous eyes. Invest Ophthalmol Vis Sci. 1981;21:563–573. [PubMed] [Google Scholar]
- 8).Lütjen-Drecoll E. Functional morphology of the trabecular meshwork in primate eyes. Prog Retin Eye Res. 1999 Jan;18:91–119. doi: 10.1016/s1350-9462(98)00011-1. [DOI] [PubMed] [Google Scholar]
- 9).Tamm ER. The trabecular meshwork outflow pathways: structural and functional aspects. Exp Eye Res. 2009;88:648–655. doi: 10.1016/j.exer.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 10).Lütjen-Drecoll E. Structural factors influencing outflow facility and its changeability under drugs: A study in Macaca arctoides. Invest Ophthalmol Vis Sci. 1973;12:280–294. [PubMed] [Google Scholar]
- 11).Tamm ER, Flügel C, Stefani FH, Lütjen-Drecoll E. Nerve endings with structural characteristics of mechanoreceptors in the human scleral spur. Invest Ophthalmol Vis Sci. 1994;35:1157–1166. [PubMed] [Google Scholar]
- 12).Flügel-Koch C, Neuhuber WL, Kaufman PL, Lütjen-Drecoll E. Morphologic indication for proprioception in the human ciliary muscle. Invest Ophthalmol Vis Sci. 2009;50(12):5529–5536. doi: 10.1167/iovs.09-3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Selbach JM, Gottanka J, Wittmann M, Lütjen-Drecoll E. Efferent and afferent innervation of primate trabecular meshwork and scleral spur. Invest Ophthalmol Vis Sci. 2000;41:2184–2191. [PubMed] [Google Scholar]
- 14).Kaufman PL. Enhancing trabecular outflow by disrupting the actin cytoskeleton, increasing uveoscleral outflow with prostaglandins, and understanding the pathophysiology of presbyopia interrogating Mother Nature: asking why, asking how, recognizing the signs, following the trail. Exp Eye Res. 2008;86:3–17. doi: 10.1016/j.exer.2007.10.007. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Stamer WD, Lei Y, Boussommier-Calleja A, Overby DR, Ethier CR. eNOS, a pressure-dependent regulator of intraocular pressure. Invest Ophthalmol Vis Sci. 2011;52:9438–9444. doi: 10.1167/iovs.11-7839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Kaufman PL, Rasmussen CA. Advances in glaucoma treatment and management: outflow drugs. Invest Ophthalmol Vis Sci. 2012;53:2495–2500. doi: 10.1167/iovs.12-9483m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Acott TS, Kelley MJ. Extracellular matrix in the trabecular meshwork. Exp Eye Res. 2008;86:543–561. doi: 10.1016/j.exer.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Fuchshofer R, Tamm ER. The role of TGF-β in the pathogenesis of primary open-angle glaucoma. Cell Tissue Res. 2012;347:279–290. doi: 10.1007/s00441-011-1274-7. [DOI] [PubMed] [Google Scholar]
- 19).Comes N, Buie LK, Borrás T. Evidence for a role of angiopoietin-like 7 (ANGPTL7) in extracellular matrix formation of the human trabecular meshwork: implications for glaucoma. Genes Cells. 2011;16:243–259. doi: 10.1111/j.1365-2443.2010.01483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Wordinger RJ, Fleenor DL, Hellberg PE, et al. Effects of TGF-beta2, BMP-4, and gremlin in the trabecular meshwork: implications for glaucoma. Invest Ophthalmol Vis Sci. 2007;48:1191–1200. doi: 10.1167/iovs.06-0296. [DOI] [PubMed] [Google Scholar]
- 21).McDowell CM, Tebow HE, Wordinger RJ, Clark AF. Smad3 is necessary for transforming growth factor-beta2 induced ocular hypertension in mice. Exp Eye Res. 2013;116:419–423. doi: 10.1016/j.exer.2013.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Choritz L, Machert M, Thieme H. Correlation of endothelin-1 concentration in aqueous humor with intraocular pressure in primary open angle and pseudoexfoliation glaucoma. Invest Ophthalmol Vis Sci. 2012;53:7336–7342. doi: 10.1167/iovs.12-10216. [DOI] [PubMed] [Google Scholar]
- 23).Junglas B, Yu AH, Welge-Lüssen U, Tamm ER, Fuchshofer R. Connective tissue growth factor induces extracellular matrix deposition in human trabecular meshwork cells. Exp Eye Res. 2009;88:1065–1075. doi: 10.1016/j.exer.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 24).Wang WH, McNatt LG, Pang IH, et al. Increased expression of the WNT antagonist sFRP-1 in glaucoma elevates intraocular pressure. J Clin Invest. 2008;118:1056–1064. doi: 10.1172/JCI33871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Faralli JA, Newman JR, Sheibani N, Dedhar S, Peters DM. Integrin-linked kinase regulates integrin signaling in human trabecular meshwork cells. Invest Ophthalmol Vis Sci. 2011;52:1684–1692. doi: 10.1167/iovs.10-6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27).Binninger EA, Schachtschabel DO, Rohen JW. Exogenous glycosaminoglycans stimulate hyaluronic acid synthesis by cultured human trabecular meshwork cells. Exp Eye Res. 1987;45:169–177. doi: 10.1016/s0014-4835(87)80087-8. [DOI] [PubMed] [Google Scholar]
- 28).Fuchshofer R, Stephan DA, Russell P, Tamm ER. Gene expression profiling of TGFbeta2- and/or BMP7-treated trabecular meshwork cells: Identification of Smad7 as a critical inhibitor of TGF-beta2 signaling. Exp Eye Res. 2009;88:1020–1032. doi: 10.1016/j.exer.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29).Medina-Ortiz WE, Belmares R, Neubauer S, Wordinger RJ, Clark AF. Cellular Fibronectin Expression in Human Trabecular Meshwork and Induction by Transforming Growth Factor-β2. Invest Ophthalmol Vis Sci. 2013;17;54:6779–6788. doi: 10.1167/iovs.13-12298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Browne JG, Ho SL, Kane R, Oliver N, Clark AF, O'Brien CJ, Crean JK. Connective tissue growth factor is increased in pseudoexfoliation glaucoma. Invest Ophthalmol Vis Sci. 2011;52:3660–3666. doi: 10.1167/iovs.10-5209. [DOI] [PubMed] [Google Scholar]
- 31).Clark AF, Wordinger RJ. The role of steroids in outflow resistance. Exp Eye Res. 2009;88:752–759. doi: 10.1016/j.exer.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 32).Johnson DH, Bradley JM, Acott TS. The effect of dexamethasone on glycosaminoglycans of human trabecular meshwork in perfusion organ culture. Invest Ophthalmol Vis Sci. 1990;31:2568–2571. [PubMed] [Google Scholar]
- 33).Cracknell KP, Grierson I. Prostaglandin analogues in the anterior eye: their pressure lowering action and side effects. Exp Eye Res. 2009;88:786–791. doi: 10.1016/j.exer.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 34).Ooi YH, Oh DJ, Rhee DJ. Effect of bimatoprost, latanoprost, and unoprostone on matrix metalloproteinases and their inhibitors in human ciliary body smooth muscle cells. Invest Ophthalmol Vis Sci. 2009;50:5259–5265. doi: 10.1167/iovs.08-3356. [DOI] [PubMed] [Google Scholar]
- 35).Yu AL, Fuchshofer R, Kampik A, Welge-Lüssen U. Effects of oxidative stress in trabecular meshwork cells are reduced by prostaglandin analogues. Invest Ophthalmol Vis Sci. 2008;49:4872–4880. doi: 10.1167/iovs.07-0984. [DOI] [PubMed] [Google Scholar]
- 36).Alvarado J, Murphy C, Polansky J, Juster R. Age-related changes in trabecular meshwork cellularity. Invest Ophthalmol Vis Sci. 1981;21:714–727. [PubMed] [Google Scholar]
- 37).Grierson I, Howes RC. Age-related depletion of the cell population in the human trabecular meshwork. Eye. 1987;1:204–210. doi: 10.1038/eye.1987.38. [DOI] [PubMed] [Google Scholar]
- 38).Grierson I, Wang Q, McMenamin PG, Lee WR. The effects of age and antiglaucoma drugs on the meshwork cell population. Res Clin Forums. 1982;4:69–78. [Google Scholar]
- 39).Lütjen-Drecoll E, Shimizu T. Rohrbach M, Rohen JW: Quantitative analysis of “plaque material” in the inner and outer wall of Schlemm's canal in normal and glaucomatous eyes. Exp Eye Res. 1986;42:443–455. doi: 10.1016/0014-4835(86)90004-7. [DOI] [PubMed] [Google Scholar]
- 40).Gabelt BT, Kaufman PL. Changes in aqueous humor dynamics with age and glaucoma. Prog Retin Eye Res. 2005 Sep;24:612–637. doi: 10.1016/j.preteyeres.2004.10.003. Review. [DOI] [PubMed] [Google Scholar]
- 41).Kelley MJ, Rose AY, Song K, Chen Y, Bradley JM, Rookhuizen D, Acott TS. Synergism of TNF and IL-1 in the induction of matrix metalloproteinase-3 in trabecular meshwork. Invest Ophthalmol Vis Sci. 2007;48:2634–2643. doi: 10.1167/iovs.06-1445. [DOI] [PubMed] [Google Scholar]
- 42).Tian B, Geiger B, Epstein DL, Kaufman PL. Cytoskeletal involvement in the regulation of aqueous humor outflow. Invest Ophthalmol Vis Sci. 2000;41:619–623. Review. [PubMed] [Google Scholar]
- 43).Gabelt BT, Gottanka J, Lütjen-Drecoll E, Kaufman PL. Aqueous humor dynamics and trabecular meshwork and anterior ciliary muscle morphologic changes with age in rhesus monkeys. Invest Ophthalmol Vis Sci. 2003;44:2118–2125. doi: 10.1167/iovs.02-0569. [DOI] [PubMed] [Google Scholar]
- 44).Gottanka J, Johnson DH, Martus P, Lütjen-Drecoll E. Severity of optic nerve damage in eyes with POAG is correlated with changes in the trabecular meshwork. J Glaucoma. 1997;6:123–132. [PubMed] [Google Scholar]
- 45).Tektas OY, Lütjen-Drecoll E. Structural changes of the trabecular meshwork in different kinds of glaucoma. Exp Eye Res. 2009;88:769–775. doi: 10.1016/j.exer.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 46).Rohen JW, Futa R, Lütjen-Drecoll E. The fine structure of the cribriform meshwork in normal and glaucomatous eyes as seen in tangential sections. Invest Ophthalmol Vis Sci. 1981;21:574–785. [PubMed] [Google Scholar]
- 47).Knepper PA, Goossens W, Palmberg PF. Glycosaminoglycan stratification of the juxtacanalicular tissue in normal and primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 1996;37:2414–2425. [PubMed] [Google Scholar]
- 48).Gong H, Underhill CB, Freddo TF. Hyaluronan in the bovine ocular anterior segment, with emphasis on the outflow pathways. Invest Ophthalmol Vis Sci. 1994;35:4328–4332. [PubMed] [Google Scholar]
- 49).Lütjen-Drecoll E, Schenholm M, Tamm E, Tengblad M. Visualization of hyaluronic acid in the anterior segment of rabbit and monkey eyes. Exp Eye Res. 1990;51:55–63. doi: 10.1016/0014-4835(90)90170-y. [DOI] [PubMed] [Google Scholar]
- 50).Knepper PA, Fadel JR, Miller AM, Goossens W, Choi J, Nolan MJ, Whitmer S. Reconstitution of trabecular meshwork GAGs: influence of hyaluronic acid and chondroitin sulfate on flow rates. J Glaucoma. 2005;14:230–238. doi: 10.1097/01.ijg.0000159130.00710.78. [DOI] [PubMed] [Google Scholar]
- 51).Schlötzer-Schrehardt U. Naumann GO Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol. 2006;141:921–937. doi: 10.1016/j.ajo.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 52).Streeten BW, Gibson S, Dark AJ. Pseudoexfoliative material contains an elastic microfibrillar-associated glycoprotein. Trans Am Ophthalmol Soc. 1986;84:304–320. [PMC free article] [PubMed] [Google Scholar]
- 53).Zenkel M, Lewczuk P, Jünemann A, Kruse FE, Naumann GO, Schlötzer-Schrehardt U. Proinflammatory cytokines are involved in the initiation of the abnormal matrix process in pseudoexfoliation syndrome/glaucoma. Am J Pathol. 2010;176:2868–2879. doi: 10.2353/ajpath.2010.090914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54).Schlötzer-Schrehardt U. Pseudoexfoliation syndrome: the puzzle continues. J Ophthalmic Vis Res. 2012;7:187–189. [PMC free article] [PubMed] [Google Scholar]
- 55).Elhawy E, Kamthan G, Dong CQ, Danias J. Pseudoexfoliation syndrome, a systemic disorder with ocular manifestations. Hum Genomics. 2012;10:6–22. doi: 10.1186/1479-7364-6-22. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56).Schlötzer-Schrehardt U, Naumann GO. Trabecular meshwork in pseudoexfoliation syndrome with and without glaucoma. A morphometric, ultrastructural study. Invest Ophthalmol Vis Sci. 1995;36:1750–1764. [PubMed] [Google Scholar]
- 57).Gottanka J, Flügel-Koch C, Martus P, Johnson DH, Lütjen-Drecoll E. Correlation of pseudoexfoliative material and optic nerve damage in pseudoexfoliation syndrome. Invest Ophthalmol Vis Sci. 1997;38:2435–2446. [PubMed] [Google Scholar]
- 58).Schlötzer-Schrehardt U, von der Mark K, Sakai LY, Naumann GO. Increased extracellular deposition of fibrillin-containing fibrils in pseudoexfoliation syndrome. Invest Ophthalmol Vis Sci. 1997;38:970–984. [PubMed] [Google Scholar]
- 59).Allingham RR, de Kater AW, Ethier CR. Schlemm's canal and primary open angle glaucoma: correlation between Schlemm's canal dimensions and outflow facility. Exp Eye Res. 1996;62:101–109. doi: 10.1006/exer.1996.0012. [DOI] [PubMed] [Google Scholar]
- 60).Johnson TV, Fan S, Camras CB, Toris CB. Aqueous humor dynamics in exfoliation syndrome. Arch Ophthalmol. 2008;126:914–920. doi: 10.1001/archopht.126.7.914. [DOI] [PubMed] [Google Scholar]
- 61).Schlötzer-Schrehardt U. Molecular pathology of pseudoexfoliation syndrome/glaucoma insights from LOXL1 gene associations. Exp Eye Res. 2009;88:776–785. doi: 10.1016/j.exer.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 62).Schlötzer-Schrehardt U, Lommatzsch J, Köchle M, Konstas AGP, Naumann GOH. Matrix metalloproteinases and their inhibitors in aqueous humor of patients with pseudoexfoliation syndrome, pseudoexfoliation glaucoma, and primary open-angle glaucoma. Invest. Ophthalmol.Vis. Sci. 2003;44:1117–1125. doi: 10.1167/iovs.02-0365. [DOI] [PubMed] [Google Scholar]