Abstract
Objective
The objective of this study was to provide preliminary findings from an ongoing randomized clinical trial using a canine-assisted intervention (CAI) for 24 children with ADHD.
Method
Project Positive Assertive Cooperative Kids (P.A.C.K.) was designed to study a 12-week cognitive-behavioral intervention delivered with or without CAI. Children were randomly assigned to group therapy with or without CAI. Parents of children in both groups simultaneously participated in weekly parent group therapy sessions.
Results
Across both treatment groups, parents reported improvements in children’s social skills, prosocial behaviors, and problematic behaviors. In both groups, the severity of ADHD symptoms declined during the course of treatment; however, children who received the CAI model exhibited greater reductions in the severity of ADHD symptoms than did children who received cognitive-behavioral therapy without CAI.
Conclusion
Results suggest that CAI offers a novel therapeutic strategy that may enhance cognitive-behavioral interventions for children with ADHD.
Keywords: canine-assisted therapy, ADHD, human–animal interactions, pet therapy
Treatment with stimulant medications has been clearly shown to reduce symptoms of ADHD with multiple empirical studies reporting impressive effect sizes (e.g., Farone & Buitelaar, 2010; MTA Cooperative Group, 1999). However, despite decades of research and clearly established immediate effects of medication treatment, long-term benefits remain unclear and treatment adherence is often poor. Reviews of the literature suggest that the average duration of medication treatment ranges between 1 and 3 years, with reports of undesirable side effects and a lack of response for a substantial number of children (Barbaresi et al., 2006; Van der Oord, Prins, Oosterlaan, & Emmelkamp, 2008). Moreover, medication treatment has not yet established positive long-term effects on academic outcomes (Langberg & Becker, 2012), cognition (Swanson, Baler, & Volkow, 2011), social relationships (Mrug et al., 2012), or functional impairment and adaptive behaviors (Epstein et al., 2011). Also, adolescents with ADHD continue to be at greater risk for early illicit substance use and substance abuse than their typically developing peers despite reported benefit from stimulant treatments as young children (Molina et al., 2013). In a recent large community-based sample of children treated with stimulant medications, symptoms were reduced but functional impairment remained (Epstein, 2011). As a result, there is a growing interest among families, clinicians, and educators in novel, nonpharmacological interventions that are aimed at improving social and occupational functioning.
Children with ADHD are often impaired in self-regulation and frequently do not attend to social cues. Specifically, they often experience peer rejection related to poor frustration tolerance, impatience with peers, anger management, and difficulties accepting consequences (Hoza et al., 2005). Evidence-based psychosocial interventions for ADHD include intense school-based behavior modification training, behavioral parent education, and social skills training (de Boo & Prins, 2007; Pelham, Wheeler, & Chronis, 1998; Webster-Stratton, Reid, & Hammond, 2001). Traditional social skills therapies for children with ADHD aim to acquire skills, enhance skill performance, remove interfering problem behaviors, and facilitate generalization of treatment gains (Elliott & Gresham, 1993). While effect sizes vary across the literature, therapies including cognitive-behavioral strategies and specifically social skills training have largely been found to be successful nonpharmacological interventions. For a more thorough review of these strategies, Storebo and colleagues (2011) published an extensive meta-analysis of this treatment modality.
Rationale for Enhancing Therapy With Canine-Assisted Intervention (CAI)
Recent advances in neuroimaging techniques reveal clear deficits of the nucleus accumbens in children with ADHD that give rise to deficits in arousal and self-regulation (Phelps & LeDoux, 2005). There is evidence that a lack of sufficient levels of catecholamines can result in poor regulation of executive function, attention, and emotional regulation (White, Helfinstein, Reeb-Sutherland, Degnan, & Fox, 2009). The relationship between emotion, motivation, and attention/learning processes is empirically supported (Phelps, Ling, & Carrasco, 2006; Kilpatrick & Cahill, 2003)—attention and emotion are intrinsically entwined. While ADHD is commonly recognized as a disorder with primary deficits in attention and behavior regulation, evidence has supported the theory that ADHD also involves motivation deficits due to under arousal of the catecholamine system (Luman, Oosterlaan, & Sergeant, 2005; Sonuga-Barke, 2002). Relative deficits in motivation suggests that it is more difficult for individuals with ADHD to engage attention in social settings, exercise self-regulation, and sustain sufficient motivation to participate in benign tasks (Sonuga-Barke, 2002). This “Motivational Hypothesis” suggests that one must boost emotion to improve attention and help children engage in learning novel concepts. A relative lack of “healthy” anxiety may result in a lack of social engagement or sensitivity to one’s environment, and lead to novelty seeking or reckless behavior.
Theoretically, human–animal interactions (HAIs; particularly human–canine interactions) as a novel stimuli, may “prime” children for therapy by heightening arousal, emotion, attention, and engagement in the therapeutic environment. There is a growing body of evidence indicating that the opportunity to interact with therapy animals can help motivate individuals to comply with the therapeutic process, productively engage with their therapist, and retain their motivation to participate in therapy overtime (Fine, 2010; Mallon, Ross, Ross, & Klee, 2010). Given the important role of emotion in learning, integrating animals into traditional psychosocial treatments for ADHD could provoke an emotional response beneficial to learning; this, in turn, could increase the effects of treatment, particularly on the increase of adaptive behaviors. For example, behavioral treatment goals for children with ADHD often include promoting empathy and perspective taking, as these social skills are typically underdeveloped in children with ADHD. Regular interactions with therapeutically trained dogs might impact these processes by stimulating an emotional response and activating attentional networks during more traditional cognitive-behavioral and behavior modification interventions, increasing the learning that takes place during therapy. Therefore, introducing animals into therapy could act as a catalyst for social learning.
There is prior scientific evidence for the value of HAI that supports the integration of animals into therapeutic models. For example, HAIs have been associated with psychological health and stress reduction (Odendaal, 2000; Gullone, 2003). Furthermore, the relationship between humans and pets is thought to improve social behavior and emotional attachment (Nagasawa, Kikusui, Onaka, & Ohta, 2009). Although the assistance of therapy dogs in psychosocial treatment settings for young children has long been considered beneficial, little empirical research has been conducted in these arenas (Fawcett & Gullone, 2001). Preliminary evidence indicates that CAIs are beneficial with children with neurodevelopmental disorders, including autism spectrum disorders and Down’s Syndrome (Limond, Bradshaw, & Cormack, 1997; Martin & Farnum, 2002). There are also reports that animal-assisted interventions have been successfully implemented with children with emotional and learning challenges in residential treatment (Mallon, 1994). However, to our knowledge, there currently are no published randomized studies examining HAIs or CAIs for children with ADHD.
The Present Study
Emerging interest in the role of HAI in child health and development calls for careful empirical evaluation of delivery, dose, and effects of HAI treatments. Project Positive Assertive Cooperative Kids (P.A.C.K.), an ongoing large-scale clinical trial, was developed to systematically examine the role of HAI in a novel, CAI combined with cognitive-behavioral treatment for children with ADHD and their parents. Preliminary results of that larger study are reported in this study in efforts to swiftly inform this understudied field. Two treatment groups (CAI and non-CAI) were compared in this randomized study. It was hypothesized both groups would show improvements in prosocial skills and reduced problematic behaviors, and that treatment effects would be greater for children in the canine-assisted group (CAI).
Research Questions and Hypotheses
Research Question 1: Do both treatment groups exhibit improvements in outcomes following intervention?
Hypothesis 1a: Children in both treatment groups will exhibit a reduction in problem behavior as measured by parent rating when compared with a wait-list (WL) control group.
Hypothesis 1b: Children in both treatment groups will demonstrate improvements on measures of social skills and prosocial behavior when compared with a WL control group, as reported by parents.
Research Question 2: Are there differences in outcomes between treatment groups (CAI and non-CAI)?
Hypothesis 2a: Children receiving CAI will exhibit greater reductions in ADHD symptoms than children receiving standard cognitive-behavioral therapy.
Hypothesis 2b: Children receiving CAI will exhibit greater reductions in problem behavior than children receiving standard cognitive-behavioral therapy.
Hypothesis 2c: Children receiving CAI will exhibit greater improvements on measures of social skills and prosocial behavior than children receiving standard cognitive-behavioral therapy.
Research Question 3: Are improvements associated with treatment efficacy maintained over time?
Hypothesis 3: Children in both treatment groups will maintain treatment gains at follow-up 6 weeks after the end of the intervention.
Method
Participants
Screening and eligibility criteria
As part of screening for study eligibility, parents completed a family medical and psychosocial history questionnaire. Researchers administered the Kaufman-Schedule for Affective Disorders and Schizophrenia for School-Age Children: Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997) and the Wechsler Abbreviated Scale of Intelligence, Fourth Edition (WASI-IV; Wechsler, 1999). Diagnostic eligibility was confirmed with the K-SADS-PL, which is a semistructured clinician-administered interview that includes coding criteria keyed to the guidelines of the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association [APA], 2000) for psychiatric disorders. To be eligible for the study, children had to meet diagnostic criteria for ADHD–Combined Type, be between the ages of 7 and 9 years, obtain an estimated full scale IQ score of 80 or above, and complete all screening measures. Exclusionary criteria included current use of medication for ADHD; a diagnosis of a pervasive developmental disorder, depression, anxiety, or epilepsy; and a history of cruelty to animals.
Randomization design
All participants are randomly assigned to one of two treatment groups:(a) a cognitive-behavioral group therapy incorporating a CAI with therapy dogs or (b) a cognitive-behavioral group therapy without therapy dogs (non-CAI). In efforts to establish treatment efficacy for both the CAI and the non-CAI treatment groups, a WL condition was implemented to control for the possible influence of time and child development on symptom severity in both groups. Specifically, half of all recruited participants, regardless of treatment group, were consented and assessed and then experienced a waiting period of 12 weeks prior to a subsequent assessment and the start of treatment. The remainder of participants recruited began immediate treatment (IT) subsequent to consent and assessment.
All parents rated the severity of their child’s ADHD symptoms prior to and throughout the course of intervention, and both parents and children participated in assessments immediately following the 12-week intervention period, and then again at 6 weeks post intervention.
Study sample
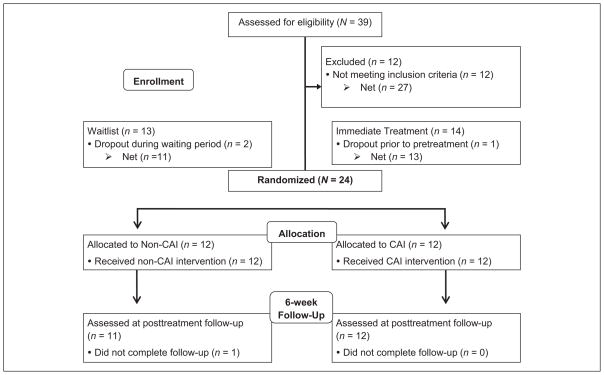
Participants in the present study represent the first two cohorts of Project P.A.C.K. (N = 24; see Table 1 for sample characteristics) for a preliminary evaluation of the effects of the 12-week P.A.C.K. treatment. Prior to enrollment and data collection, one parent (in two-parent families) was identified as the primary parent respondent (defined as parents who were primarily responsible for overseeing the child’s daily activities and whose schedule allowed him or her to attend all parent intervention sessions). The same primary parent (21 mothers and 3 fathers) completed all parent-rated measures obtained at screening and across all assessments, including during the course of intervention. After recruitment, two families in the WL condition dropped during the waiting period (after their assessment and prior to the start of treatment), one family in the IT condition dropped immediately prior to the start of treatment, and 1 parent did not complete ratings on the outcome measures at follow-up 6 weeks after treatment in the non-CAI group (see Figure 1 for a flow diagram of recruitment and group assignment design). Demographic characteristics and results listed in Table 1 are based on data collected from participants who completed the 12-week intervention.
Table 1.
Participant Characteristics by WL and IT Conditions and Intervention Groups.
| WL (n = 11)
|
IT (n = 13)
|
χ2 / t | Non-CAI (n = 12)
|
CAI (n = 12)
|
χ2 / t | |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | |||
| Child agea | 8.07 (.26) | 7.75 (.64) | 0.48 | 7.81(.63) | 7.99 (.87) | −0.58 |
| Child gender (% male) | 82% | 85% | 0.03 | 83% | 83% | 0.0 |
| Child ethnicity (% Hispanic/Latino) | 55% | 15% | 4.11* | 33% | 33% | 0.0 |
| Child race (%) | ||||||
| Caucasian | 45% | 62% | 0.62 | 67% | 42% | 1.51 |
| Hispanic/Latino | 27% | 8% | 67% | 25% | ||
| Asian | 18% | 8% | 17% | 8% | ||
| African American | 9% | 0% | — | 8% | ||
| Multiracial | 0% | 23% | 8% | 17% | ||
| Child % ODD comorbidity | 64% | 54% | 0.24 | 58% | 58% | 0.0 |
| Child full scale IQ | 109 (5.25) | 115 (2.77) | −1.14 | 115 (3.40) | 110 (4.60) | 0.93 |
| Child % history stimulant use | 0% | 23% | 2.90 | 17% | 8% | 0.38 |
| Maternal age | 34.27 (5.18) | 42.38 (5.45) | −3.71* | 38.17 (5.42) | 39.17 (7.91) | 0.64 |
| Maternal education (% attended college) | 73% | 100% | 4.05* | 92% | 83% | 0.54 |
| Paternal age | 38.20 (5.51) | 46.08 (9.30) | −2.37* | 43.50 (7.60) | 41.73(10.05) | 0.48 |
| Paternal education (% attended college) | 100% | 46% | 0.86 | 50% | 45% | 0.05 |
| Parent % married | 64% | 85% | 1.40 | 75% | 75% | 0.0 |
| SSIS-RS Social Skills | 70.82 (7.43) | 79.46 (9.47) | −2.45* | 76.00 (10.90) | 75.00 (8.31) | 0.25 |
| SSIS-RS Problem Behaviors | 134.09 (10.62) | 123.62 (7.32) | 2.85* | 127.67 (9.21) | 129.17 (11.59) | −0.35 |
| SCI Prosocial Orientation | 2.85 (0.54) | 3.19 (0.59) | −1.48 | 3.14 (0.72) | 2.92 (0.40) | 0.94 |
| ADHD-RS Total Score | — | — | — | 32.92 (2.66) | 28.17 (1.99) | 1.43 |
Note. WL = wait-list condition; IT = immediate treatment condition; non-CAI = non-canine assisted intervention; CAI = canine-assisted intervention; ODD = oppositional defiant disorder; SSIS-RS = Social Skills Improvement System–Rating Scales; SCI = Social Competence Inventory, ADHD-RS = ADHD–Rating Scale. Descriptive statistics are based on available data for all treatment completers. Two WL participants dropped during the waiting period prior to random assignment to the CAI or non-CAI treatment groups, resulting in the recruitment of two additional IT participants prior to randomization to prevent unbalanced intervention group size.
Age at baseline for WL and IT groups; age at pretreatment for treatment groups.
p < .05.
Figure 1.
CONSORT diagram to illustrate study recruitment, screening, random assignment, and treatment completion and follow-up.
Intervention
For a period of 12 weeks, each child participant attended an intervention group session twice a week; one weekday evening for 2 hr and on Saturday for 2½ hr, resulting in a total of 4½ hr per week of treatment for the child. Parents received 2 hr of group-based behavioral parent training (BPT) once a week that occurred during their child’s weekly evening sessions. Interventions for both groups incorporated curriculum based on components from the University of California (UC) Irvine Child Development School Social Skills model, the American Humane Kids Interacting With Dogs Safely™ (Deming, Jones, Caldwell, & Phillips, 2009) program from the American Humane Association, and the Intermountain Therapy Animals’ Reading Education Assistance Dogs program (ITA R.E.A.D.® Handbook, 2003–2004) curricula.
The CAI group included the participation of three certified therapy dogs, facilitated by their handlers (partners), during each intervention session. The non-CAI group received the same standard treatment curriculum but utilized toy dogs (realistic puppets) in lieu of live dogs.
Social skills curriculum
The social skills curriculum used in children’s therapeutic group sessions was originally developed for the UC Irvine Child Development School, a laboratory school environment for children with ADHD, and combines cognitive-behavioral and behavioral theories with behavior modification techniques and social problem-solving strategies to promote adaptive skill acquisition. The social skills training curriculum targets the specific skills of accepting consequences, ignoring provocation, appropriate assertiveness, social problem solving, cooperation, and good sportsmanship. This model, derived from research on programs designed to teach social skills and friendship-making skills (Asher & Oden, 1976, Michelson, Sugai, Wood, & Kazdin, 1983; Oden & Asher, 1977) has been adapted for children with ADHD and utilizes a combination of didactic instruction, modeling, and role-play, while implementing a token economy, group and individual contingencies, and differential positive reinforcement of adaptive behaviors that are incompatible with problem behaviors.
BPT
The parent training component of intervention consisted of 12, weekly, 2-hr sessions of BPT conducted with six families per treatment group. Sessions were based on a traditional BPT curriculum using behavior modification techniques in which parents were taught to target and modify their child’s specific problematic behaviors using positive reinforcement (e.g., labeled praise, tangible rewards, and privileges), nonphysical discipline (e.g., planned ignoring, time-outs), and standard parenting strategies (e.g., giving effective directions, when–then statements, transitional warnings, token economies, problem solving). In addition to techniques used to facilitate anger management and targeted social skills (e.g., emotion regulation strategies, labeling emotions, communication), common parenting challenges most frequently associated with ADHD (e.g., problems with self-regulation, organization, motivation, and persistence) were reviewed with parents along with prescribed weekly goals. Parent–child shared homework activities (e.g., reading a short story together) were assigned to encourage discussions focusing on targeted social skills and/or humane education topics. Parent sessions also provided an opportunity for families to receive therapeutic and educational support in dealing with their child’s ADHD symptoms.
Measures
ADHD–Rating Scale–Fourth Edition, Home and School Version (ADHD-RS-IV)
The ADHD-RS (DuPaul, Power, Anasto-poulos, & Reid, 1998) is an established measure of efficacy in clinical trials of ADHD treatments for children that consists of 18 items derived from the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; APA, 1994) criteria for ADHD. Parents rate the frequency of each symptom using a 4-point scale (never or rarely = 0, sometimes = 1, often = 2, very often = 3). The ADHD-RS yields three subscales: Inattention, Hyperactive/Impulsive, and Total symptoms. In this sample, the internal consistency (Cronbach’s α) was .88 for Total symptoms. The ADHD-RS was completed by parents at four time points during the course of intervention (Weeks 2, 4, 8, and 10).
Social Skills Improvement System–Rating Scales, Parent Form (SSIS-RS)
The parent-rated SSIS-RS (Gresham & Elliott, 2008) is a psychometrically sound 79-item measure that assesses two domains of children’s functioning: social skills and competing problem behaviors. Subscales within the Social Skills domain include Communication, Cooperation, Assertion, Responsibility, Empathy, Engagement, and Self-Control. Subscales comprising the Problem Behaviors domain include Internalizing, Externalizing, Bullying, Hyperactivity/Inattention, and Autism Spectrum. In this sample, Cronbach’s alphas were .86 for the Social Skills Scale and .78 for the Problem Behaviors Scale. Primary parent respondents of all participants completed the SSIS prior to treatment, immediately following treatment, and at a 6-week follow-up. The SSIS was also completed prior to the waiting period by parents in the WL control group.
Social Competence Inventory (SCI)
The SCI (Rydell, Hagekull, & Bohlin, 1997) is a validated, 25-item measure of behavioral aspects of social competence developed with parents and teachers of children ages 7 to 10 years. The SCI contains two scales derived from factor analysis: the Prosocial Orientation (PO) scale (i.e., the ability to engage in positive peer interactions) comprising items that assess positive actions such as helpfulness, generosity, empathy, social understanding, cooperation, and conflict resolution, and the Social Initiative (SI) scale (i.e., the ability to initiate and take part in social interactions opposed to withdrawal), comprising items that predict initiative behavior. Both scales have discriminated popular from rejected children in observed peer behavior at school; the SI scale differentiated popular from average children, and PO differentiated rejected from average children. Baseline scores on the SI scale (Cronbach’s α = .70) were significantly correlated with the SSIS-RS Social Skills Scale (r = .45, p = .03), which was not the case for the PO scale (Cronbach’s α = .84; r = .21, p = .33). The PO scale is believed to be differentially related to externalizing problems, whereas the SI scale may reflect internalizing problems. Because the PO scale appeared to assess a different level of social competence, the current study focused only on PO as a primary outcome. Primary parent respondents of all participants completed the SCI at prior to treatment, immediately following treatment, and at a 6-week follow-up, and parents in the WL control group also completed the SCI at the pre-WL assessment.
Primary Analyses
Chi-square tests and independent-samples t tests were used to determine the equivalency of the demographic characteristics and means of treatment outcomes (Social Skills, PO, and Problem Behaviors scores) for the groups and conditions. Intervention outcomes were evaluated by two distinct sets of analyses. ANCOVAs were used to examine treatment effects relative to the WL control condition by comparing post-WL scores on outcome measures to the posttreatment scores from the treatment condition while adjusting for the effects of baseline scores. Repeated-measures ANOVAs were used to evaluate treatment maintenance effects by testing changes in scores between posttreatment and 6-week follow-up.
To examine within-individual change (i.e., how outcomes for each child change over time) and between-individual differences in change (i.e., how individual change differs across children), a series of mixed multilevel models (MLM) with random coefficients were used to examine potential effects associated with the type of treatment (non-CAI vs. CAI) on primary intervention outcomes (ADHD symptoms, Social Skills, PO, and Problem Behaviors) and rate of change in outcomes across the pretreatment, posttreatment, and follow-up time points as well as across intervention weeks in a repeated-measures design. Multilevel modeling allows for the examination of between-person (Level 2 submodel) differences (e.g., treatment group) in within-person (Level 1 submodel) trajectories (e.g., change in ADHD symptoms over time) and do not require balanced data (i.e., the same number of time points for each individual) or equally spaced waves of data collection (for a review, see Singer & Willett, 2003), both of which are present in the current sample. For each of the four outcome measures, the results of a two-part analysis are reported. The linear rate of change in each outcome was first examined in an unconditional growth model (preliminary analyses indicated that there was no significant effect for quadratic time for ADHD-RS scores, and all other outcomes were limited to tests of linear time due to only three time points). In the second set of analyses, final models tested the effects of treatment group on initial (baseline) status and rate of change for each outcome over time. To reduce the risk of collinearity and to facilitate the interpretations of results, all continuous predictor variables were centered on their mean values. Child age at baseline, gender, and comorbid oppositional defiant disorder (ODD) were screened as potential covariates for inclusion in final models. None of these variables were significant predictors of pretreatment Social Skills, PO, or Problem Behaviors scores or predictors of changes in outcomes over time, and subsequently were not included in final models. Pseudo-R2 statistics were calculated to obtain global effect sizes (i.e., the proportion of total outcome variation “explained” by the combination of predictors in final models) and local effect sizes (i.e., the proportional reduction in Level 2 residual variances associated with each predictor variable) for each outcome at specified time points.
Results
Randomization and Equivalence of Groups
Differences between WL versus IT groups were assessed prior to treatment with chi-square tests and t tests to determine the equivalency of groups after randomization. There were few statistically significant group differences on the demographic or outcome variables presented in Table 1. Parents in the WL group were significantly younger than parents in the IT group (p < .01, p < .05, respectively) and waitlisted mothers had less education compared with mothers in the IT group (p < .05). Also compared with the IT group, the WL group included significantly more Hispanic/Latino children (p < .05) and had higher scores on the Social Skills scale and lower scores on the Problem Behaviors scale prior to treatment (p < .05, p < .05, respectively). Results from paired-samples t tests within the WL group showed that there were no significant differences between Social Skills scores prior to the waiting period (M = 73.00, SD = 8.29) and immediately before treatment (M = 70.82, SD = 7.43, t = .91, p = .39) or between Problem Behaviors scores at these same assessment points (M = 8.69, SD = 2.62 and M = 134.09, SD = 10.62, respectively; t = −1.26, p = .24), indicating that scores on these outcome measures remained relatively stable during the 12-week waiting period.
Randomization procedures resulted in comparable treatment groups immediately before treatment, with no significant differences in any of the demographic variables or outcome variables between the non-CAI and CAI treatment groups (see Table 1). All 24 families completed their randomly assigned 12-week intervention. Parent and child attendance were high for both treatment groups (parent M = 11.58, SD = .72 out of 12 sessions; child M = 22.04, SD = 1.33 out of 23 sessions).
Research Question 1: Do both treatment groups exhibit improvements in outcomes following intervention compared with a WL control group?
Hypothesis 1a: Children in both treatment groups will exhibit a reduction in parent-reported problem behaviors in comparison with the WL control group.
To evaluate the effect of treatment on children’s problematic behaviors, the change in scores from baseline to the post-WL period for the WL condition were compared with the change in pretreatment to posttreatment scores for the IT condition with ANCOVAs. Treatment condition (WL vs. IT) was the principle predictor of post-WL/treatment parent ratings of Problem Behaviors (e.g., hyperactive/impulsive, externalizing, bullying behaviors). Means, standard deviations, F values, p values, and effect size estimates are presented in Table 2. Results showed that problematic behaviors were significantly reduced posttreatment for the IT group relative to the post-WL problem behaviors in the WL group after controlling for baseline Problem Behaviors and Social Skills scores, F(1, 20) = 19.88, p < .001.
Table 2.
Descriptive statistics for Outcome Measures for Wait-List and Immediate Treatment Groups.
| Measure | Pre-wait-list
|
Pretreatment
|
Post-wait-list
|
Posttreatment
|
F | p | Effect size |
|---|---|---|---|---|---|---|---|
| WL
|
IT
|
WL
|
IT
|
||||
| M (SD) | M (SD) | M (SD) | M (SD) | ||||
| Problem Behaviors | 129.82 (8.69) | 123.62 (7.32) | 134.09 (10.62) | 112.23 (9.87) | 19.88 | <.0001 | 2.00 |
| Social Skills | 73.00 (8.29) | 79.46 (9.47) | 70.82 (7.43) | 92.77 (12.76) | 20.98 | <.0001 | 2.02 |
| Prosocial Orientation | 2.99 (.35) | 3.19 (.59) | 2.85 (.54) | 3.71 (.51) | 18.44 | <.0001 | 1.87 |
Note. WL = wait-list; IT = immediate treatment. Raw descriptive statistics means and standard deviations reported in the table are unadjusted for the effects of covariates and are based on data for treatment completers; n = 11 for WL and n = 13 for IT. Standardized mean effect sizes reflect adjusted Cohen’s d = (adjusted mean WL group – adjusted mean IT group)/square root of the mean square error.
Hypothesis 1b: Children in both treatment groups will demonstrate improvements on measures of social skills and prosocial behavior compared with a WL control group.
To evaluate the effect of treatment on children’s social skills, the change in scores from baseline to the post-WL period for the WL condition were compared with the change in pretreatment to posttreatment scores for the IT condition with ANCOVAs. Condition (WL vs. IT) was the principle predictor of parent ratings of Social Skills and PO behaviors after treatment. Adjusting for baseline Social Skills scores and comorbid ODD, posttreatment Social Skills scores were higher in the IT condition than were the post-WL scores in the WL condition, F(1, 20) = 20.98, p < .001 (see descriptive statistics in Table 2). Higher posttreatment PO behaviors for the IT condition were also reported compared with the post-WL scores of the WL condition, F(1, 19) = 18.44, p < .001, after adjusting for baseline SCI scores and comorbid ODD.
Research Question 2: Are there differences in outcomes between treatment groups (CAI and non-CAI)?
Hypothesis 2a: Children receiving CAI will exhibit greater reductions in ADHD symptoms than children receiving standard cognitive-behavioral therapy.
MLM analyses using random coefficients models were used to examine within-person change over time and between-person differences in ADHD symptoms. The unconditional growth model, which included only linear time as a predictor, showed that the average ADHD-RS score at Week 2 was 30.93 (SE = 1.78, p < .0001) with an average decline of 2.74 (SE = 0.71) points over subsequent weeks, indicating that parents reported significant reductions in children’s ADHD symptoms during the course of treatment for the overall sample, F(1, 23) = 15.21, p < .001.
To test whether parent ratings of child ADHD symptoms differed between non-CAI and CAI interventions over time, treatment group (non-CAI vs. CAI) was entered as the sole between-persons predictor of ADHD-RS scores, along with its interaction term with linear time. Social Skills, PO, and Problem Behaviors scores (and their interactions with treatment group and time) were screened as potential covariates for inclusion in the model. No significant interactions or main effects were found, and therefore these variables were not included in the final model. Time was centered at the first time point of data collection (Week 2) to represent baseline (initial status) mean scores. Table 3 presents descriptive statistics for ADHD-RS scores and estimates and standard errors for the fixed-effects of treatment group at each week of intervention. The severity of children’s ADHD symptoms did not differ between the non-CAI and CAI groups, F(1, 48) = 2.05, p = .16, as reported by parents in the second week of intervention, and no significant interaction was found between treatment group and time (β = −.64, SE = 1.40), F(1, 48) = 0.21, p = .65. In other words, at Week 2, initial ADHD-RS scores between the two intervention groups were roughly equivalent, and the rate of decline in scores across time was similar for both groups. Time and treatment group accounted for 53% of the total variation in ADHD-RS scores at Week 2, with treatment group explaining 10% of the variance in scores at baseline and 1.4% of the variance in the rate of change over time.
Table 3.
Means (Standard Deviations) and Multilevel Model Results for Treatment Group Differences in Intervention Outcomes.
| Outcome | Pretreatment
|
Posttreatment
|
Follow-up
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-CAIa | CAIb | β (SE) | Non-CAIa | CAIb | β (SE) | Non-CAIc | CAIb | β (SE) | |
| Problem Behaviors | 127.67 (9.21) | 129.17 (11.59) | 2.16 (3.17) | 115.33 (9.67) | 112.67 (14.72) | −.94 (2.44) | 118.27 (110.83) | 110.83 (11.42) | −4.06 (3.55) |
| Social Skills | 76.00 (10.90) | 75.00 (8.31) | 1.83 (2.81) | 86.42 (11.94) | 92.50 (13.88) | 0.64 (2.27) | 89.64 (11.05) | 92.33 (10.08) | −0.56 (3.36) |
| Prosocial Orientation | 3.14 (0.72) | 2.92 (0.40) | −.18 (0.19) | 3.47 (0.72) | 3.51 (0.62) | −0.16 (0.15) | 3.50 (0.70) | 3.43 (0.46) | −0.15 (0.15) |
| Week 2 | Week 4 | Week 8 | Week 10 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADHD-RS | 32.92 (9.20) | 28.17 (6.89) | −4.89 (3.41) | 31.08 (9.74) | 25.75 (6.96) | −5.37 (2.70) | 29.67 (6.64) | 22.67 (7.57) | −6.34 (2.35) | 25.33 (8.68) | 19.00 (7.34) | −6.82 (2.77) |
Note. Means and standard deviations reported in the table reflect descriptive statistics for raw scores unadjusted for covariates. Non-CAI = non-canine assisted intervention. CAI = canine-assisted intervention. ADHD-RS = ADHD–Rating Scale. Treatment group differences for each outcome were analyzed separately in random coefficients models.
n = 12;
n = 12;
n = 11.
To test for group differences in ADHD symptom severity at subsequent weeks during treatment, time was recentered at each time point (i.e., the intercept was shifted to a specified time point of data collection to represent the initial baseline mean score at that particular occasion when time = 0). Predicted mean ADHD-RS scores at each week for the CAI and non-CAI groups are shown in Figure 2. At Week 4 of treatment, significant group differences in ADHD symptoms appeared, F(1, 22) = 3.95, p < .05 (see Table 3). Parent ratings of children’s ADHD symptoms were lower in the CAI intervention compared with the non-CAI intervention and remained significantly lower at Week 8. F(1, 48) = 7.24, p < .01, and Week 10, F(1, 48) = 6.07, p < .05. The interaction between time and treatment group (and their lower order terms) accounted for 30% of the total variance in ADHD-RS scores at Week 4. The local pseudo-R2 effect size indicated that the Level 2 between-person intercept variance decreased by 17% after adding group to the model at Week 4, by 28% at Week 8, and by 27% at Week 10.
Figure 2.
Predicted mean ADHD-RS scores for non-CAI (n = 12) and CAI (n = 12) treatment groups across four time points.
Note. CAI = canine-assisted intervention.
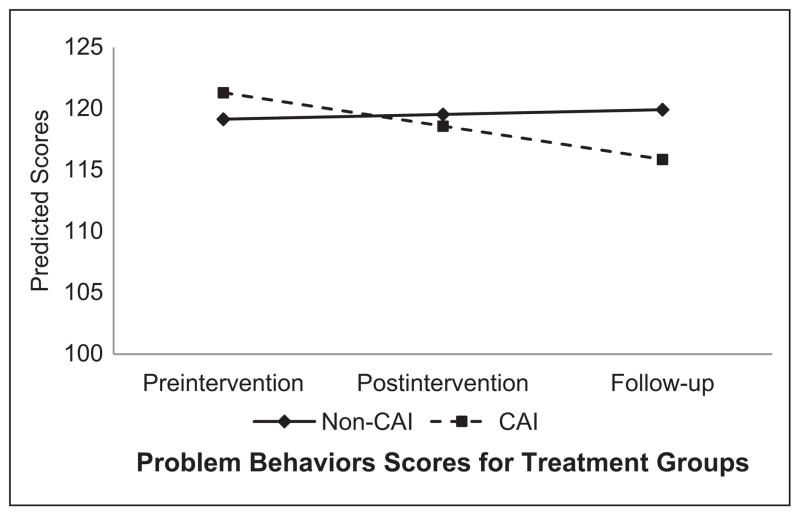
Hypothesis 2b: Children receiving canine-assisted therapy will exhibit greater reductions in problem behaviors than children receiving standard cognitive-behavioral therapy.
Multilevel random coefficients models were used to examine within-person change over time and between- person differences on the SSIS Problem Behaviors scores. The unconditional growth model showed that the average initial score for Problem Behaviors at pretreatment across both treatment groups was 125.96 (SE = 2.24, p < .0001) and declined by an average 7.04 (SE = 0.71) points across subsequent time points, indicating that parents reported significant reductions in children’s behavioral problems (e.g., externalizing behaviors, bullying, hyperactivity/impulsivity) over time for the overall sample, F(1, 23)= 49.56, p < .0001.
To test whether there were differences in Problem Behaviors scores over time as a function of type of intervention, treatment group (non-CAI vs. CAI) was entered as the between-persons predictor along with the fixed and random effect of time (and its interaction with group) and Social Skills scores as a covariate. Time was recentered at each time point in separate models to test for mean score differences at pretreatment, posttreatment, and follow-up (see Table 3). As illustrated in Figure 3, results indicated that there were no significant group differences in mean scores for Problem Behaviors scores between the CAI and the non-CAI interventions prior to the start of treatment, F(1, 22) = 0.46, p = .50; at posttreatment, F(1, 22) = 0.15, p = .70; or at 6-week follow-up, F(1, 22) = 1.30, p = .27. Treatment group was also not significantly associated with the rate of decline in Problem Behaviors scores across time, F(1, 22) = 1.79, p = .19.
Figure 3.
Predicted mean Problem Behaviors scores for non-CAI (n = 12) and CAI (n = 12) treatment groups plotted at each assessment time point.
Note. n = 11 for non-CAI at follow-up due to missing data. CAI = canine-assisted intervention.
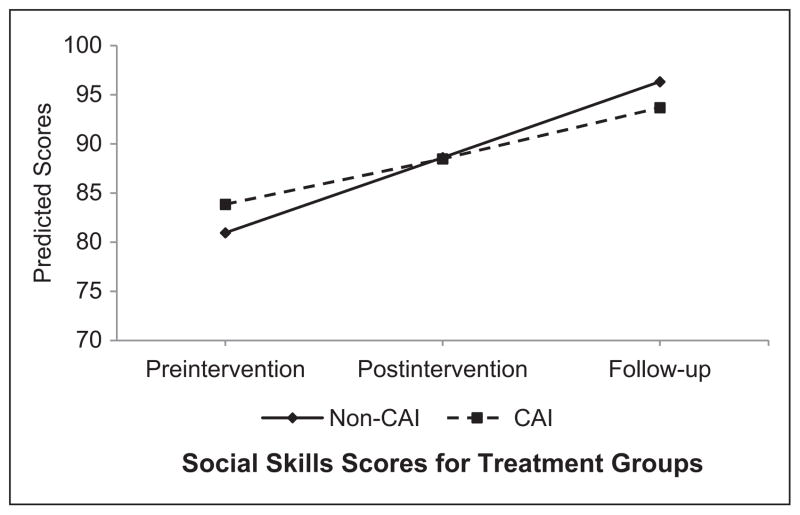
Hypothesis 2c: Children receiving canine-assisted therapy will exhibit greater improvements on measures of social skills and prosocial behavior than children receiving standard cognitive-behavioral therapy.
Random coefficients models were used to examine within-person change over time and between-person differences on the SSIS Social Skills and SCI Prosocial Behaviors scores across time. The unconditional growth model for Social Skills showed that the baseline mean score at pretreatment across both treatment groups was 85.35 (SE = 1.80, p < .0001) and increased an average of 7.80 (SE = 1.07) points across subsequent time points, indicating that parents reported significant improvements in children’s levels of social skills over time for the overall sample, F(1, 23) = 52.71, p < .0001. Results from the unconditional growth model for PO behaviors determined that the average pretreatment initial score for the overall sample was 3.11 (SE = 0.12, p < .0001) and increased an average of 0.21 points over time (SE = 0.04, p < .0001).
To test for mean group differences in Social Skills scores between the two types of interventions, treatment group (non-CAI vs. CAI) was entered as the between-persons predictor along with the fixed and random effect of time, the interaction between group and time, and Problem Behaviors as a covariate. Time was recentered at each time point in separate models to test for differences at pretreatment, posttreatment, and follow-up (see Table 3 for mean Social Skills scores at each time point). As illustrated in Figure 4, there were no significant differences in mean Social Skills scores between the non-CAI and CAI interventions at pretreatment, F(1, 22) = 0.43, p = .52; posttreatment, F(1, 22) = 0.08, p = .79; or follow-up, F(1, 22) = 0.03, p = .87. No significant interaction between treatment group and time was found (β = −1.19, SE = 2.11), F(1, 22) = 0.32, p =.58, indicating that the rate of improvement in scores across time was similar between treatment groups. Taken together, predictors in the full model (time, treatment group, the interaction between time and group, and Problem Behaviors scores) explained 19% of the total variation in Social Skills scores at posttreatment and 55% of the total variation at follow-up. Similarly, mean PO scores did not differ between non-CAI and CAI groups at pre-treatment, F(1, 22) = 0.88, p = .36; posttreatment, F(1, 22) = 1.19, p = .29; or follow-up, F(1, 22) = 1.00, p = .33, adjusting for the effects of SSIS Social Skills scores (see Table 3). Type of treatment group did not predict the rate of change in PO scores over time (β = .02, SE = 0.08), F(1, 22) = 0.04, p = .83. The combination of time, treatment group, the Time × Group interaction, and Social Skills scores accounted for 64% of the total variation in posttreatment PO scores and 42% of the total variation at follow-up.
Figure 4.
Predicted mean Social Skills scores for non-CAI (n = 12) and CAI (n = 12) treatment groups plotted at each assessment time point.
Note. n = 11 for non-CAI at follow-up due to missing data. CAI = canine-assisted intervention.
Research Question 3: Are improvements associated with treatment maintained over time?
Hypothesis 3: Children in both treatment groups will maintain treatment gains after 6 weeks.
To evaluate the maintenance of improvements over time across both the CAI and non-CAI treatment groups, repeated-measures ANOVAs were used to compare outcome scores at posttreatment with outcome scores at 6-week follow-up. Results indicated that there was a significant effect of time across pretreatment, posttreatment, and follow-up scores on Problem Behaviors, F(2, 42) = 22.76, p < .001, η2 = .52; Social Skills, F(2, 42) = 26.15, p < .001, η2 = .54; and PO, F(2, 42) = 15.83, p < .001, η2 = .43. No significant interactions between time and treatment group were found among any of the outcomes (all Fs < 1.80, all ps > .18), suggesting that differences in the outcomes across time points did not vary as a function of type of treatment (non-CAI vs. CAI). Post hoc pairwise comparisons with Bonferroni adjustments (α = .05 / 3 = .017) determined that there were no significant differences between posttreatment and follow-up Problem Behaviors scores, t(22) = −.22, p = .83, Cohen’s d = .06; no differences between posttreatment and follow-up Social Skills scores, t(22) = −.73, p = .48, Cohen’s d = .15; and no posttreatment to follow-up differences for PO scores, t(22) = −.20, p = .84, Cohen’s d = .02, suggesting that treatment gains were maintained for both treatment groups 6 weeks after intervention.
Discussion
Findings from this preliminary study provide initial support for the efficacy of a cognitive-behavioral group treatment enhanced with humane education for children with ADHD and social impairments. Across both treatment groups (CAI and non-CAI), parents reported improvements on measures of children’s social skills, prosocial behaviors, and competing problematic behaviors. For all child participants, the severity of their behavioral symptoms of ADHD showed a linear decline across time during the course of treatment; however, children who received the CAI model exhibited greater reductions in the severity of their ADHD symptoms than did children who received the enhanced cognitive-behavioral therapy intervention without CAI. Notable improvements in favor of the CAI intervention group emerged as early as the 4th week of treatment and were maintained at subsequent weeks of treatment. Thus, canine-assisted cognitive-behavioral therapy compared favorably with an enhanced cognitive-behavioral therapy without CAI specific to ADHD symptomology, whereas this pattern of findings was not apparent in outcomes of social skills and competing problematic internalizing and externalizing behaviors. Overall, these results suggest that a CAI offers a novel therapeutic strategy that may enhance traditional evidence-based interventions for children with impairment from the core symptoms of ADHD.
Limitations in this preliminary study include a small sample size, use of a single (parent) informant, and restricted measurements. It is also noted that parental ratings, by condition, were not blind and this may introduce an element of bias which should be considered when interpreting results. Future directions should include blind ratings and are discussed below. While results indicated that CAI was associated with greater improvements in ADHD symptoms, it was beyond the scope of the present study to identify the specific mechanisms behind these changes over time. Currently, a fully powered clinical trial examining outcomes for subsequent cohorts is underway.
Both therapy models were associated with parent ratings of improved social functioning in this sample of children with ADHD, yet children receiving the CAI treatment showed significantly greater improvements in inhibitory control and attention, both important aspects of executive functioning. During P.A.C.K. sessions, children spent time reading to dogs in a structured manner and practiced teaching dogs specific skills using commands and praise. In the non-CAI model, children read to dog puppets and taught specific skills (e.g., drawing, origami) to their peers using step-by-step instructions and praise. Thus, the primary difference between treatment models is likely the heightened demands that a live animal places on a child’s attention. If a child’s attention wanders when interacting with a dog puppet, the puppet does not engage in behaviors that draw the child back into engagement. In contrast, a live dog might prompt a child to maintain attention or refocus on the dog and task at hand. These interactions with a live animal, therefore, could become an opportunity to train attention, where the animal serves as a prompt to refocus attention on the therapeutic activity. Prior research examining mindful presence and “mindfulness” training has indicated that training one’s attention to focus on the present moment trains attention and improves performance on tasks requiring executive function (Zylowska et al., 2007). Similarly, studies of attention training (Tamm et al., 2010) indicate that inhibitory response and attention can be improved with training. It is plausible that dynamic, goal-directed interactions with dogs may enable children to focus on the present moment, thereby shaping concentration and on-task behaviors and reducing problems with sustained attention. Future research should examine this hypothesis by studying attention processes during therapy and attention outcomes based on executive function task performance. Moreover, it is possible that the inclusion of dogs in therapy also heightened emotion and engagement, thereby increasing the opportunity for learning during therapy sessions. Possible mechanisms contributing to these favorable findings warrant further discussion.
Implications for Future Research
Anecdotal reports have long claimed that the mere presence of dogs during therapy with children has a calming effect, thereby reducing stress and better priming children for therapy. Finding ways to more objectively measure this kind of “priming” and physiological stress reduction is key to enhancing our understanding of the physiological mechanisms contributing to the human–animal bond and its impact on intervention. In future research, it will be important to develop structured methods to assess child engagement during therapy. In addition, in efforts to counterbalance the impact of parental bias on ratings of behavior across treatment conditions, observations of children’s behavior should be rated by blind raters. Finally, examination of physiological responses related to stress, including heart rate, activity level, and salivary cortisol, will be important to address biological mechanisms of change.
As the field of HAI for children for children with ADHD develops, there are many more questions that need to be addressed in scientific research. What types of dogs work best? What skills or training do the dogs as well as therapists need? What parent and child characteristics moderate responses to CAI? Could HAI also reduce the risk of injury (e.g., dog bites) among impulsive children with greater risk for injury? Preliminary evidence suggests that further study in this field is warranted and timely.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and Mars-WALTHAM® Grant R01H066593. This research also was supported by funding from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through Grant UL1 TR000153, as well as funding from the NIH Loan Repayment Program (L60MD002127) awarded to Dr. Lakes.
Biographies
Sabrina E. B. Schuck, PhD, is an assistant clinical professor in the Department of Pediatrics at the University of California, Irvine. She is the principal investigator of Project Positive Assertive Cooperative Kids (P.A.C.K.). She collaborated on developing the theoretical rational for the study intervention and the protocol for practical application of those interventions. She collaborated on the hypotheses and analyses for the present study, and contributed to the development of the manuscript.
Natasha A. Emmerson, PhD, is a postdoctoral fellow in the Department of Pediatrics at the University of California, Irvine. She, an investigator of Project P.A.C.K., contributed to developing the overall intervention and protocol, collaborated on the hypotheses, and conducted all analyses for the present study to contribute to the development of the manuscript. Her research interests focus on novel cognitive-behavioral and alternative interventions using exercise and human–animal interventions for youth with neurodevelopmental disorders and their families.
Aubrey H. Fine, PhD, is a professor of education at California Polytechnic State University, San Bernardino, and is a consultant to the Project P.A.C.K. He collaborated on developing the theoretical rational for the study intervention and the protocol for practical application of those interventions. He was specifically involved in helping develop the human–animal interaction (HAI) intervention and contributed to the development of the manuscript.
Kimberley D. Lakes, PhD, is an assistant professor in the Department of Pediatrics at the University of California, Irvine. She is an investigator for the Project P.A.C.K. study, collaborated on the hypotheses and analyses for the present study, and contributed to the development of the manuscript.
Footnotes
Authors’ Note
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH).
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Asher SR, Oden SL. Children's failure to communicate: An assessment of comparision and egocentrism explanations. Developmental Psychology. 1976;12:132–139. doi: 10.1037/0012-1649.12.2.132. [DOI] [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Leibson CL, Jacobsen SJ. Long-term stimulant medication treatment of attention-deficit/hyperactivity disorder: Results from a population-based study. Journal of Developmental and Behavioral Pediatrics. 2006;27:1–10. doi: 10.1097/00004703-200602000-00001. [DOI] [PubMed] [Google Scholar]
- de Boo GM, Prins PJM. Social incompetence in children with ADHD: Possible moderators and mediators in social-skills training. Clinical Psychology Review. 2007;27:78–97. doi: 10.1016/j.cpr.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Deming J, Jones K, Caldwell S, Phillips A. KIDS: Kids Interacting With Dogs Safely™. Englewood, CO: American Humane Association; 2009. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD Rating Scale-IV. New York, NY: Guilford Press; 1998. [Google Scholar]
- Elliott SN, Gresham FM. Social skills intervention for children. Behavior Modification. 1993;17:287–313. doi: 10.1177/01454455930173004. [DOI] [PubMed] [Google Scholar]
- Epstein JN, Langberg JM, Lichtenstein PK, Altaye M, Brinkman WB, House K, Stark LJ. Attention-deficit/hyperactivity disorder outcomes for children treated in community-based pediatric settings. Archives of Pediatrics & Adolescent Medicine. 2010;164(2):160. doi: 10.1001/archpedi-atrics.2009.263. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Buitelaar J. Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. European Child & Adolescent Psychiatry. 2010;19:353–364. doi: 10.1007/s00787-009-0054-3. [DOI] [PubMed] [Google Scholar]
- Fawcett N, Gullone E. Cute and cuddly and a whole lot more? A call for empirical investigation into the therapeutic benefits of human–animal interaction for children. Behaviour Change. 2001;18:124–133. doi: 10.1375/bech.18.2.124. [DOI] [Google Scholar]
- Fine AH. Animals and therapists: Incorporating animals into psychotherapy: Guidelines and suggestions for therapists. In: Fine A, editor. Handbook on animal-assisted therapy: Theoretical foundations and guidelines for practice. 3. San Diego, CA: Academic Press; 2010. pp. 169–192. [Google Scholar]
- Gresham F, Elliott S. Social Skills Improvement System (SSIS) Minneapolis, MN: Pearson Assessment; 2008. [Google Scholar]
- Gullone E. The proposed benefits of incorporating non-human animals into preventative efforts for conduct disorder. Antrhrozoos. 2003;16:160–174. doi: 10.2752/089279303786992215. [DOI] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, Arnold LE. What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder? Journal of Consulting and Clinical Psychology. 2005;73:411–423. doi: 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- Intermountain Therapy Animals Handbook. Reading Education Assistance Dogs. Salt Lake City, UT: Intermountain Therapy Animals; 2003–2004. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kilpatrick L, Cahill L. Amygdala modulation of parahippocampal and frontal regions during emotionally influenced memory storage. Neuroimage. 2003;20:2091–2099. doi: 10.1016/j.neuroimage.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Langberg JM, Becker SP. Does long-term medication use improve the academic outcomes of youth with attention-deficit/hyperactivity disorder? Clinical Child and Family Psychology Review. 2012;15:215–233. doi: 10.1007/s10567-012-0117-8. [DOI] [PubMed] [Google Scholar]
- Limond JA, Bradshaw JWS, Cormack KFM. Behavior of children with learning disabilities interacting with a therapy dog. Antrhrozoös. 1997;10:84–89. doi: 10.2752/089279397787001139. [DOI] [Google Scholar]
- Luman M, Oosterlaan J, Sergeant JA. The impact of reinforcement contingencies on AD/HD: A review and theoretical appraisal. Clinical Psychology Review. 2005;25:183–213. doi: 10.1016/j.cpr.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Mallon GP. Some of our best therapists are dogs. Child & Youth Care Forum. 1994;23:89–101. doi: 10.1007/BF02209256. [DOI] [Google Scholar]
- Mallon GP, Ross SB, Ross L, Klee S. Designing and implementing animal-assisted therapy programs in health and mental health organizations: Rules and principles to guide program development. In: Fine A, editor. Handbook on animal-assisted therapy: Theoretical foundations and guidelines for practice. 3. San Diego, CA: Academic Press; 2010. pp. 135–147. [Google Scholar]
- Martin F, Farnum J. Animal-assisted therapy for children with pervasive developmental disorders. Western Journal of Nursing Research. 2002;24:657–670. doi: 10.1177/019394502320555403. [DOI] [PubMed] [Google Scholar]
- Michelson L, Sugai DP, Wood RP, Kazdin AE. Social skills assessment and training with children: An empirically based handbook. New York, NY: Plenum Press; 1983. [Google Scholar]
- Molina BSG, Hinshaw SP, Arnold LE, Swanson JM, Pelham WE, Hechtman LL, Marcus S. Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:250–263. doi: 10.1016/j.jaac.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrug S, Molina BSG, Hoza B, Gerdes AC, Hinshaw SP, Hechtman L, Arnold LE. Peer rejection and friendships in children with attention-deficit/hyperactiv-ity disorder: Contributions to long-term outcomes. Journal of Abnormal Child Psychology. 2012;40:1013–1026. doi: 10.1007/s10802-012-9610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MTA Cooperative Group. Moderators and mediators of treatment response for children with attention-deficit/hyperac-tivity disorder. Archives of General Psychiatry. 1999;56:1088–1096. doi: 10.1001/archpsyc.56.12.1088. [DOI] [PubMed] [Google Scholar]
- Nagasawa M, Kikusui T, Onaka T, Ohta M. Dog’s gaze at its owner increases owner’s urinary oxytocin during social interaction. Hormones and Behavior. 2009;55:434–441. doi: 10.1016/j.yhbeh.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Oden S, Asher SR. Coaching children in social skills for friendship making. Child Development. 1977;48:495–506. doi: 10.2307/1128645. [DOI] [Google Scholar]
- Odendaal JSJ. Animal-assisted therapy—Magic or medicine? Journal of Psychosomatic Research. 2000;49:275–280. doi: 10.1016/S0022-3999(00)00183-5. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Jr, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyper-activity disorder. Journal of Clinical Child Psychology. 1998;27:190–205. doi: 10.1207/s15374424jccp2702_6. [DOI] [PubMed] [Google Scholar]
- Phelps EA, Le Doux JE. Contributions of the amygdala to motion processing: From animal models to human behavior. Neuron. 2005;48:175–187. doi: 10.1016/j.neu-ron.2005.09.025. [DOI] [PubMed] [Google Scholar]
- Phelps EA, Ling S, Carrasco M. Emotion facilitates perception and potentiates the perceptual benefits of attention. Psychological Science. 2006;17:292–299. doi: 10.1111/j.1467-9280.2006.01701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rydell A, Hagekull B, Bohlin G. Measurement of two social competence aspects in middle childhood. Developmental Psychology. 1997;33:824–833. doi: 10.1037/0012-1649.33.5.824. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Sonuga-Barke EJ. Psychological heterogeneity in AD/HD—A dual pathway model of behaviour and cognition. Behavioural Brain Research. 2002;10:29–36. doi: 10.1016/S0166-4328(01)00432-6. [DOI] [PubMed] [Google Scholar]
- Storebo OJ, Skoog M, Damm D, Thomson PH, Simonsen E, Gluud C. Social skills training for attention deficit hyperactivity disorder in children aged 5 to 18 years. Cochrane Database of Systematic Reviews. 2011;2011(12):Article CD008223. doi: 10.1002/14651858.CD008223.pub2. [DOI] [PubMed] [Google Scholar]
- Swanson JM, Baler RD, Volkow ND. Understanding the effects of stimulant medications on cognition in individuals with attention-deficit hyperactivity disorder: A decade of progress. Neuropsychopharmacology. 2011;36:207–226. doi: 10.1038/npp.2010.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamm L, Hughes C, Ames L, Pickering J, Silver CH, Stavinoha P, Emslie G. Attention training for school-aged children with ADHD: Results of an open trial. Journal of Attention Disorders. 2010;14:86–94. doi: 10.1177/1087054709347446. [DOI] [PubMed] [Google Scholar]
- Van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp PM. Efficacy of methylphenidate, psychosocial treatments and their combination in school-aged children with ADHD: A meta-analysis. Clinical Psychology Review. 2008;28:783–800. doi: 10.1016/j.cpr.2007.10.007. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ, Hammond M. Preventing conduct problems, promoting social competence: A parent and teacher training partnership in Head Start. Journal of Clinical Child Psychology. 2001;30:283–302. doi: 10.1207/S15374424JCCP3003_2. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- White LK, Helfinstein SM, Reeb-Sutherland BC, Degnan KA, Fox NA. Role of attention in the regulation of fear and anxiety. Developmental Neuroscience. 2009;31:309–317. doi: 10.1159/000216542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zylowska L, Ackerman DL, Yang MH, Futtrell JL, Horton NL, Hale TS, Smalley SL. Mindfulness meditation training in adults and adolescents with ADHD: A feasibility study. Journal of Attention Disorders. 2007;11:737–746. doi: 10.1177/1087054707308502. [DOI] [PubMed] [Google Scholar]