Abstract
Objective
The present study investigates the extent to which a refundable tax credit could be used to increase low income children's after-school physical activity levels.
Methods
An experimental study was conducted evaluating the effectiveness of an intervention offering a simulated refundable tax credit to parents of elementary school-age children (n=130) for enrollment in after-school physical activity programs. A randomized-controlled design was used, with data collected at baseline, immediately following the four month intervention (post-intervention), and six-weeks after the end of the intervention (follow-up). Evaluation measures included: (a) enrollment rate, time spent, weekly participation frequency, duration of enrollment and long term enrollment patterns in after-school physical activity programs; and (b) moderate-to-vigorous physical activity (MVPA).
Results
The simulated tax credits did not significantly influence low- income children's rates of enrollment in after-school physical activity programs, frequency of participation, time spent in after-school physical activity programs, and overall moderate-to-vigorous intensity physical activity at post-intervention or follow-up.
Conclusion
The use of refundable tax credits as incentives to increase participation in after-school physical activity programs in low-income families may have limited effectiveness. Lawmakers might consider other methods of fiscal policy to promote physical activity such as direct payment to after-school physical activity program providers for enrolling and serving a low- income child in a qualified program, or improvements to programming and infrastructure.
Keywords: obesity, children physical activity, tax credits
BACKGROUND
One-third of children and adolescents in California are either obese or overweight.1 Low-income children are particularly at excess risk of obesity,2 a phenomenon partly attributed to lower physical activity levels3 and increased sedentary behavior.4 A particular area of concern is the disparity in physical activity levels by income level in the after-school context. Children from lower income families are significantly less likely than children from higher income families to report involvement in organized after-school physical activity programs.5 Studies found the participation rate in after-school organized physical activity programs of children and youth in low-income urban areas is less than 20% compared to more than 80% for children and youth in more well off suburbs.6, 7 Enrollment in after-school physical activity programs is positively associated with physical activity, with children attending after-school programs engaging in twenty minutes of moderate-to-vigorous physical activity, on average, during that period.8 Thus, children enrolled in after-school physical activity programs have the potential to accumulate more total physical activity than children who are not enrolled in such programs.9
Financial incentives may be used to increase children's enrollment in after-school physical activity programs. To explore behavioral change of a financial incentive on children's level of physical activity in the after-school setting, this study utilized the economic theory of household production.10 Under the household production theory, individuals consume resources to produce household commodities (e.g. health status) that maximize well-being. By allocating different amounts of time to various activities (e.g., physical activity leisure vs. sedentary leisure), individuals are able to maximize their utility towards lifetime well-being.
Young children's time allocation is largely dependent on decisions made by their parents, thus, to affect children's time allocation it is necessary to influence parental decision making. However, the parents' decision regarding their children's time allocation is subject to budgetary constraints. If the price of an activity is altered, parents will reallocate expenditures and time. Similarly, if the price of after-school physical activity programs falls while the prices of other sedentary after-school leisure activities remain constant, we may expect parents to reallocate their budget in order to “buy” for their children more of the after-school physical activity programs and less of sedentary leisure time activities.11
Cost is considered one of the more significant barriers facing low income parents in supporting their children to engage in after-school physical activity.12, 13, 14, 15, 16 One way to reduce the cost barrier is to offer financial incentives for enrolling low income children in after-school physical activity programs. Facilitating financial incentives, particularly cash incentives, can significantly improve healthy behaviors.17 A financial incentive to engage in a certain behavior may be created through a tax legislation. Few studies have examined the impact of tax legislations on healthy eating habits of people.18, 19, 20 However, no study to date has examined the impact a refundable tax credit may have on the promotion of physical activity.11 This study explores a new and as yet untested approach for combating childhood obesity rates among low-income children by examining the potential impact refundable tax credits may have on these children's participation level in organized after-school physical activity program.
A refundable tax credit provides the taxpayer with a supplement payment when the tax credit amount exceeds the tax liability. Hence, a refundable tax credit is particularly helpful for taxpayers at the lowest end of the income spectrum.21 It enables low and moderate income taxpayers to receive a refund check from the government if the tax credit amount is larger than the taxpayer's income tax liability.22
Research Questions and Hypotheses
Our overall hypothesis is that tax legislation that offers a refundable tax credit to parents who enroll their children in organized after-school physical activity would reduce the cost barrier that currently deters some low-income parents from enrolling their children in such activities, and thus promote more children to engage in after-school physical activity programs. Our specific hypotheses are as follows:
Hypothesis 1: Rates of enrollment in after-school physical activity programs, maintenance of enrollment for the duration of the four-month intervention, and continuation of enrollment six weeks after the end of the intervention will be higher for children in the treatment group.
Hypothesis 2: Children in the treatment group will attend after-school physical activity programs at a significantly higher rate per week and will report a higher amount of time spent on after school physical activity than participants in the control group.
Hypothesis 3: Children in the treatment group will increase their daily moderate to vigorous physical activity level (MVPA).
METHODS
Data Collection Protocol
Data was collected at baseline, following the four month intervention, and six-weeks after the end of the intervention. A formal intervention was introduced between the first two measurement occasions. Participants that were randomly selected to take part in the treatment group were given a letter stating that they will receive up to $200 reimbursement following the enrollment of their elementary school-aged child in a qualified after-school physical activity program of their choice. This amount was chosen because a $200 reimbursement would cover approximately half of the average cost of a two day per week after school physical activity program over a four month period. Fifty percent refundable tax credit has been estimated previously to have a large impact on the behavior of low-income uninsured taxpayers in the context of health insurance acquisition.25 A qualified program for the purposes of our intervention was one that encourages children to strive towards at least 30 minutes of sustained moderate to vigorous physical activity per session, be supervised by an adult, and suitable for children. Eligible programs must last at least eight weeks, and meet at a minimum of one session per week. To receive the $200, parents must sign up their child to a qualified physical activity program, obtain a receipt from the organization providing the program, and complete, sign and submit a claim form. To simulate the burdens associated with receipt of a tax credit, the claim form that the parents were required to complete as part of this study was a one page form requiring similar information that they would be required to provide in a tax return seeking a tax credit. The form asked for the following set of information: child's name, organization name & address, type of physical activity program/s (soccer, swimming, etc.), dates of enrollment, and amount paid & date paid. Similar to a tax refund claim, the parents participating in the intervention, who fulfilled the requirements for reimbursements, receive their reimbursement within six to ten weeks after submitting the form. Children randomized to the control group received no invitation to the tax credit.
Sample
Our study population included low-income children between the age of 6 and 11 years old (1st through 5th grade). Eligibility in the federally funded free or reduced lunch program served as a proxy for low-income household, 23 and all 1st-5th grade students enrolled in the three schools receiving free or reduced lunch program were invited to participate in the study. This age group was selected because early childhood years are the most crucial years for shaping attitudes and behaviors,24 overweight status at that age is linked with an increased risk of coronary heart disease in adulthood,25 and because parental influence appears to be robust during that period in a child's life.26,27
Participants were recruited from three elementary schools in a suburb of Los Angeles. All three schools are public schools within the Los Angeles Unified School District, located only a few miles apart in the San Fernando Valley. The schools are Title 1 schools serving similar diverse student population: 30% Latino; 25% White; 14% Asians; and 13% Blacks. The student population is primarily low-income, with approximately half of enrolled students participating in the federally funded reduced or free lunch program. Students across schools are exposed to similar in-school physical education curriculum of one hour per week. One important distinction between the three schools is the availability and accessibility of after-school physical activity programs. In one school there was no after school physical activity programs available. In the second school, there was an after school physical activity program available for a fee. In the third school, there was an after school physical activity program that was free of charge. This allowed us to examine the effect of simulated tax incentive in different environments.
All those individuals, who were invited to participate in our study and who consented to participate, were allowed to join our study and were part of our sample. Students were aggregated in each of the three schools and then randomized. Randomization was performed within each schools using a randomization software, Research Randomizer.28 A total of 64 participants were assigned to the treatment group and 66 were assigned to the control group. The Human Subjects Protocol and Informed Consent was approved by the university's Human Subjects Committee.
Measures
Measures used to assess the efficacy of the simulated refundable tax credit were: (a) enrollment rate in after-school physical activity programs; (b) time spent participating in after-school physical activity programs; (c) weekly participation frequency in the after-school physical activity programs; (d) duration of enrollment (in weeks) in after-school physical activity programs; (e) moderate-to-vigorous physical activity (MVPA); and (f) long term enrollment patterns in after-school physical activity programs. With the exception of the MVPA, all measures were exclusively collected using self-reported data provided by the children's parents. MVPA was collected using time diaries completed by the children's parents and by data collected using accelerometers. Data were collected from the participants at baseline, post-intervention (four months after baseline) and follow up stage of the study (six weeks after post-intervention). In one school we were unable to collect follow up data because school year ended prior to the follow-up period.
Parents completed a survey at baseline asking demographic and family characteristics and their children's enrollment in after-school physical activity programs, including the frequency of attendance and the duration of the after school physical activity programs which they were enrolled. Demographic characteristics included race/ethnicity, child's age, parent's marital status, parent's level of education, acculturation, household size, vehicle ownership, and number of hours the parent worked per week. Acculturation was measured using the proxy of American citizenship to discern differences between recent immigrants and those who were either born in the United States or became naturalized citizens, which requires U.S. residence for at least five years. Marital status was dichotomized (1=married; 0=other) consistent with previous research that detected differences between married and non-married groups relative to their physical activity level.29 Education was categorized into: less than high school graduate, high school graduate, some college/associate's degree, college graduate, and post-graduate education. The number of hours worked by the parent was divided into five categories: 1) 0 hours; 2) <35 hours; 3) 35-40 hours; 4) 41-50; and 5) >50 hours. The reference category was 35-40 hours worked per week.
Parents completed time diaries for a week to assess the allocation of their children's time. These time diaries were given to the parents to complete in privacy, asked questions about the child's activities over a 24-hour period beginning at midnight of a randomly designated day. These questions asked the primary activity that was going on at that time, when it began and when it ended. Substantial methodological work has established the validity and reliability of data collected in time-diary form for children.30 Primary activities of children were classified into 18 major categories previously used and validated.31 Exercise reported in the diaries were coded using the task codes and corresponding metabolic equivalent of task [MET] values established in The Compendium of Energy Expenditures for Youth.32 The research assistants (RAs) worked in teams of two to input the time engaged in an activity (in minutes) and the code and MET values that corresponds to the activity. Both members of the team had to agree on the code and MET value. If a team of RAs could not agree on a code, then the faculty director of the research lab was consulted. For the outcome of MVPA, MET values that were equal to or greater than 4.0 were averaged to compute an average energy expenditure for a weekday and for a weekend day were calculated. Each participant received a $10 gift certificate for completing the time-diary instrument and survey.
Assessment of the children's MVPA level was obtained from Actigraph GT2Maccelerometers, which have previously been validated for assessment of physical activity among elementary school-aged children.33 Baseline assessment was collected prior to the implementation of the intervention. Children wore the accelerometer for seven consecutive days. Children were asked to wear the accelerometers on their waist, on the right hand side during waking hours only. The participants did not complete an accelerometer log. Given the limited number of accelerometers available, only a third of children from the control group and the treatment group were asked to wear the accelerometer. The participants received $10 for each one week of accelerometer data retrieved.
Analysis of Accelerometer Data
A child's accelerometer record was included in the analysis if there were at least 4 complete days of data available, taken as the minimum needed to obtain a reliable measurement of habitual physical activity in children (reliability of 0.80).34 We defined a complete day as ≥7 hour of data, after excluding periods in the day when the accelerometer appeared not to have been worn. Although 10 hours of worn time is often used, the reliability between 7 and 10 hours is not substantially different.35 In practice, wear time was usually greater than 7 hours. Nonwear time was identified from the data by periods of ≥20 minutes of consecutive zero counts, making it unlikely that the monitor was worn.36 MVPA thresholds (in counts per minute) were defined using age-specific prediction equations posed by Freedson.37,38 A threshold for moderate activity of 4 METs was used for children to account for higher resting energy expenditure in children and youth.39,40
Analysis
Participant and family characteristics were described and reviewed for possible inconsistencies between groups. Attrition and missing data rates were examined and rate of attrition between groups was compared using Fisher's exact χ2 tests. Analyses were performed with SPSS v.21; a priori α = 0.05 for all analyses.
Due to the data structure of this randomized trial, whereby randomization and treatment assignment was at the family level, all analyses were performed using statistics appropriate for nested data to account for similarity within family members. Thus analyses were performed at the family level, not the individual level, though for most families, there was only a single child. To test difference by group in prevalence of enrollment and maintenance in after-school physical activity programs (Hypothesis 1), the rates of children (a) enrolled in after school activity, (b) maintained in the programs through 4 months, and (c) continued to enroll were compared using binary logistic and generalized estimating equations were computed. To test the difference by group in attendance of activity programs and (amount of time spent on after school activity), as well as moderate to vigorous physical activity (MVPA) (Hypothesis 2 & 3), repeated linear mixed effects modeling were applied, to account for the same nesting issues described above. A priori covariates included perceived child health status (ordinal), , and child and family characteristics (e.g., race/ethnicity (Latino/not Latino), child's age, parent's marital status (Married/not Married), Parent education (ordinal scale), family income, number of cars in the household, number of hours worked (ordinal), born in the USA. In addition to the primary factor (treatment group), school × group effects were tested. This effect modifier was important, as each school had different support for after school physical activities.
RESULTS
Retention
Across the three schools, 130 participants were randomized by family unit—64 into the intervention group 66 into the control group. Figure 1 shows the study flow through the three data collection points for the study for each group, and broken down by school. Six week follow-up data were only available for two out of the three schools (follow up data was not available in the school that offered a free after-school physical activity program). Through the post-intervention time point, there were comparable attrition rates between intervention and control groups. Fifteen percent of participants who were randomized did not return for baseline evaluation; attrition at post-intervention was 26% and 41% at 6-week follow up. Of those who participated in the baseline evaluation (Z = 0.3, p = 0.75), and 89% of intervention participants and 84% of control participants who completed the baseline also completed the post-intervention assessment (Z = 0.8, p = 0.44); at 6-week follow- up assessment participation within the control group was 77% versus 65% of intervention group participants (Z = 1.2, p = 0.24).
Figure 1.
Study Flow
Participant characteristics
Table 2 shows demographic and family characteristics by study group. The groups were comparable with the exception of Latino ethnicity: Seventy-five percent of parents in the intervention group reported being Latino, while 55% reported Latino ethnicity in the control group (Z = 2.1, p = 0.03).
Table 2.
Participant Characteristics by Treatment Group
| Control | Intervention | ||||
|---|---|---|---|---|---|
| N | % | N | % | ||
| School | Elementary School Offering no After School Physical Activity Program | 20 | 30.3% | 22 | 34.4% |
| Elementary School Offering After School Physical Activity Program for a Fee | 26 | 39.4% | 24 | 37.5% | |
| Elementary School Offering After School Physical Activity Program for Free | 20 | 30.3% | 18 | 28.1% | |
| Gender | Male | 24 | 41.4% | 26 | 47.3% |
| Female | 34 | 58.6% | 29 | 52.7% | |
| Student Grade | 1 | 7 | 12.3% | 8 | 14.5% |
| 2 | 16 | 28.1% | 8 | 14.5% | |
| 3 | 9 | 15.8% | 9 | 16.4% | |
| 4 | 21 | 36.8% | 19 | 34.5% | |
| 5 | 4 | 7.0% | 11 | 20.0% | |
| Sex of the student's parent who completed exercise diary | Male/Father | 7 | 13.2% | 6 | 11.8% |
| Female/Mother | 46 | 86.8% | 45 | 88.2% | |
| Marital status of the student's parent | Single | 12 | 23.1% | 15 | 28.8% |
| Married | 31 | 59.6% | 31 | 59.6% | |
| Divorced | 6 | 11.5% | 4 | 7.7% | |
| Separated | 3 | 5.8% | 2 | 3.8% | |
| Widowed | 0 | 0.0% | 0 | 0.0% | |
| Married/not married | Not Married | 21 | 40.4% | 21 | 40.4% |
| Married | 31 | 59.6% | 31 | 59.6% | |
| Parent's education level | No formal education | 0 | 0.0% | 0 | 0.0% |
| Some grade school | 0 | 0.0% | 0 | 0.0% | |
| Grade school | 3 | 5.6% | 2 | 3.8% | |
| Some middle school | 0 | 0.0% | 1 | 1.9% | |
| Middle school | 5 | 9.3% | 0 | 0.0% | |
| Some high school | 1 | 1.9% | 4 | 7.7% | |
| High school graduate | 11 | 20.4% | 11 | 21.2% | |
| Some college | 22 | 40.7% | 22 | 42.3% | |
| College graduate | 8 | 14.8% | 7 | 13.5% | |
| Some graduate school | 0 | 0.0% | 1 | 1.9% | |
| Graduate School | 4 | 7.4% | 4 | 7.7% | |
| Parental education | < High School graduate | 9 | 16.7% | 7 | 13.5% |
| High school graduate | 11 | 20.4% | 11 | 21.2% | |
| Some college | 22 | 40.7% | 22 | 42.3% | |
| College graduate | 8 | 14.8% | 7 | 13.5% | |
| Post-graduate | 4 | 7.4% | 5 | 9.6% | |
| Parent's race | African American/Black | 4 | 7.5% | 2 | 3.8% |
| Asian | 1 | 1.9% | 1 | 1.9% | |
| Hispanic/Latino | 28 | 52.8% | 38 | 73.1% | |
| White | 17 | 32.1% | 8 | 15.4% | |
| Other | 3 | 5.7% | 3 | 5.8% | |
| Latino | No | 23 | 45.1% | 13 | 25.5% |
| Yes | 28 | 54.9% | 38 | 74.5% | |
| Number of Cars | 0 | 2 | 3.7% | 0 | 0.0% |
| 1 | 26 | 48.1% | 17 | 33.3% | |
| 2 | 22 | 40.7% | 25 | 49.0% | |
| 3 | 3 | 5.6% | 8 | 15.7% | |
| 4 | 1 | 1.9% | 1 | 2.0% | |
| N | M±SD | N | M±SD | ||
| Child Age | 58 | 10.1±1.2 | 55 | 10.3±1.4 | |
| Family Income ($k) | 52 | 40.0±29.7 | 43 | 37.7±18.3 | |
| Work hours/week | 51 | 26±19 | 49 | 28±20 | |
| N | % | N | % | ||
| Work hours/week categories | 0 | 12 | 23.5% | 11 | 22.4% |
| <35 | 11 | 21.6% | 12 | 24.5% | |
| 35-40 | 21 | 41.2% | 18 | 36.7% | |
| 41 - 50 | 6 | 11.8% | 5 | 10.2% | |
| >50 | 1 | 2.0% | 3 | 6.1% | |
| Birth country | Foreign born | 30 | 55.6% | 26 | 54.2% |
| US Born | 24 | 44.4% | 22 | 45.8% | |
Enrollment in After-School Physical Activity Programs (Hypothesis 1)
Table 3 compares the rates of enrollment in after-school physical activity programs at post-intervention and follow-up between groups. After controlling for covariates, group differences in after-school physical activity program enrollment were not statistically significant for either time point. However, the OR was 1.8 (95% CI = 0.2–17.2) for after-school physical activity program enrollment at post-intervention suggesting that children in the intervention group were 80% more likely to be enrolled in an after-school physical activity program at the end of the intervention than the control group. The direction of effect shifted when examining continued after-school physical activity program enrollment at the 6-week follow-up (OR = 0.8, 95% CI = 0.6–9.7), with the intervention group being 20% less likely to continue to enroll after 6 weeks. Child health was a significant predictor of enrollment in a physical activity program at the post-intervention time point (OR = 2.0, 95% CI = 1.2–3.5).
Table 3.
Univariate predi ctorof outcomes in Hypothesis 1
| Hyp 1A: Enroll | Hyp 1B: Maintain enrollment | Hyp 1C: Continue to enroll | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | |||||||||||
| Categorical Predictors | N | % | N | % | P | N | % | N | % | P | N | % | N | % | P | |
| Group | Control | 22 | 33.3 | 44 | 66.7 | 0.45 | 46 | 69.7 | 20 | 30.3 | 0.20 | 51 | 77.3 | 15 | 22.7 | 0.67 |
| Intervention | 17 | 26.6 | 47 | 73.4 | 37 | 57.8 | 27 | 42.2 | 52 | 81.3 | 12 | 18.8 | ||||
| School | Elementary School Offering no After School Physical Activity Program | 12 | 28.6 | 30 | 71.4 | 0.93 | 26 | 61.9 | 16 | 38.1 | 0.48 | 30 | 71.4 | 12 | 28.6 | .53 |
| Elementary School Offering After School Physical Activity Program for a Fee | 16 | 32.0 | 34 | 68.0 | 35 | 70.0 | 15 | 30.0 | 35 | 70.0 | 15 | 30.0 | ||||
| Elementary School Offering After School Physical Activity Program for Free | 11 | 28.9 | 27 | 71.1 | 22 | 57.9 | 16 | 42.1 | – | – | – | – | ||||
| Sex | Male | 18 | 36.0 | 32 | 64.0 | 0.84 | 28 | 56.0 | 22 | 44.0 | 0.70 | 38 | 76.0 | 12 | 24.0 | 1.00 |
| Female | 21 | 33.3 | 42 | 66.7 | 38 | 60.3 | 25 | 49.7 | 48 | 76.2 | 15 | 23.8 | ||||
| Country of Birth | Not USA | 20 | 35.7 | 36 | 64.3 | 0.68 | 33 | 58.9 | 23 | 41.1 | 0.69 | 39 | 69.6 | 17 | 30.4 | 0.17 |
| USA | 19 | 41.3 | 27 | 58.7 | 25 | 54.3 | 21 | 45.7 | 38 | 82.6 | 8 | 17.4 | ||||
| Child Health Status | Fair | 1 | 2.6 | 2 | 3.0 | 0.27 | 2 | 66.7 | 1 | 33.3 | 0.01 | 3 | 100.0 | 0 | 0.0 | 0.08 |
| Good | 12 | 30.8 | 9 | 13.6 | 16 | 76.2 | 5 | 23.8 | 18 | 85.7 | 3 | 14.3 | ||||
| Very Good | 10 | 25.6 | 18 | 27.3 | 18 | 64.3 | 10 | 35.7 | 22 | 78.6 | 6 | 21.4 | ||||
| Excellent | 16 | 41.0 | 37 | 56.1 | 22 | 41.5 | 31 | 58.5 | 37 | 69.8 | 16 | 30.2 | ||||
| Parent marital Status | Not Married | 13 | 34.2 | 29 | 43.9 | 0.41 | 19 | 45.2 | 23 | 54.8 | 0.11 | 33 | 78.6 | 9 | 21.4 | 0.65 |
| Married | 25 | 65.8 | 37 | 56.1 | 38 | 61.3 | 24 | 38.7 | 46 | 74.2 | 16 | 25.8 | ||||
| Number of cars | 0 | 2 | 5.1 | 0 | 0.0 | 0.75 | 2 | 100.0 | 0 | 0.0 | 0.05 | 2 | 100.0 | 0 | 0.0 | 0.79 |
| 1 | 13 | 33.3 | 30 | 45.5 | 19 | 44.2 | 24 | 55.8 | 31 | 72.1 | 12 | 27.9 | ||||
| 2 | 17 | 43.6 | 30 | 45.5 | 28 | 59.6 | 19 | 40.4 | 35 | 74.5 | 12 | 25.5 | ||||
| 3 | 5 | 12.8 | 6 | 9.1 | 7 | 63.6 | 4 | 36.4 | 9 | 81.8 | 2 | 18.2 | ||||
| 4 | 2 | 5.1 | 0 | 0.0 | 2 | 100.0 | 0 | 0.0 | 2 | 100.0 | 0 | 0.0 | ||||
| Work hour per week | 0 | 9 | 23.7 | 14 | 22.6 | 0.96 | 12 | 52.2 | 11 | 47.8 | 038 | 16 | 69.6 | 7 | 30.4 | 0.30 |
| <35 | 10 | 26.3 | 13 | 21.0 | 12 | 52.2 | 11 | 47.8 | 17 | 73.9 | 6 | 26.1 | ||||
| 35-40 | 9 | 23.7 | 30 | 48.4 | 22 | 56.4 | 17 | 43.6 | 32 | 82.1 | 7 | 17.9 | ||||
| 41-50 | 7 | 18.4 | 4 | 6.5 | 7 | 63.6 | 4 | 36.4 | 9 | 81.8 | 2 | 18.2 | ||||
| >50 | 3 | 7.9 | 1 | 1.6 | 3 | 75.0 | 1 | 25.0 | 3 | 75.0 | 1 | 25.0 | ||||
| Parent education | <HS | 6 | 15.4 | 10 | 14.9 | 0.15 | 8 | 50.0 | 8 | 50.0 | 0.86 | 13 | 81.3 | 3 | 18.8 | 0.67 |
| HS | 9 | 23.1 | 13 | 19.4 | 13 | 59.1 | 9 | 40.9 | 16 | 72.7 | 6 | 27.3 | ||||
| Some College | 18 | 46.2 | 26 | 38.8 | 25 | 56.8 | 19 | 43.2 | 34 | 77.3 | 10 | 22.7 | ||||
| BA/BS | 3 | 7.7 | 12 | 17.9 | 7 | 46.7 | 8 | 53.3 | 11 | 73.3 | 4 | 26.7 | ||||
| Post-graduate | 3 | 7.7 | 6 | 9.0 | 6 | 66.7 | 3 | 33.3 | 6 | 66.7 | 3 | 33.3 | ||||
| Latino | Not Latino | 12 | 31.6 | 24 | 37.5 | 0.67 | 18 | 50.0 | 18 | 50.0 | 1.00 | 26 | 72.2 | 10 | 27.8 | 0.47 |
| Latino/Hispanic | 26 | 68.4 | 40 | 62.5 | 33 | 50.0 | 33 | 50.0 | 52 | 78.8 | 14 | 21.2 | ||||
| Continuous | M | SD | M | SD | OR | P | M | SD | M | SD | OR | P | M | SD | M | SD | OR | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyp 1A: Enroll | Hyp 1B: Maintain enrollment | Hyp 1C: Continue to enroll | ||||||||||||||||
| No | Yes | No | Yes | No | Yes | |||||||||||||
| Predictors | ||||||||||||||||||
| Age (yrs) | 10.3 | 1.2 | 10.1 | 1.4 | 0.91 | 0.51 | 10.12 | 1.33 | 10.28 | 1.32 | 1.10 | 0.50 | 10.27 | 1.32 | 9.93 | 1.32 | 0.83 | 0.25 |
| Number of Cars | 1.8 | 0.9 | 1.6 | 0.6 | 0.76 | 0.30 | 1.79 | 0.83 | 1.57 | 0.65 | 0.68 | 0.15 | 1.72 | 0.80 | 1.62 | 0.64 | 0.83 | 0.54 |
| Work Hours | 28.3 | 21.4 | 26.7 | 17.9 | 1.00 | 0.68 | 29.23 | 19.56 | 24.89 | 18.72 | 0.99 | 0.26 | 27.99 | 19.41 | 25.09 | 18.84 | 0.99 | 0.37 |
| Family Income ($k) | 35.9 | 19.8 | 40.7 | 27.7 | 1.01 | 0.36 | 37465 | 22155 | 40767 | 28423 | 1.00 | 0.52 | 37811 | 23335 | 42358 | 30023 | 1.00 | 0.44 |
Note. Categorical outcome were tested with  2 testsL Fisher's exact for dichotomous, and 1 Pearsons exact for 3+ categories; ordinal outcomes were testd with Somer's D if not symetrical; continuous outcomes were tested with logistic regression modeling.
2 testsL Fisher's exact for dichotomous, and 1 Pearsons exact for 3+ categories; ordinal outcomes were testd with Somer's D if not symetrical; continuous outcomes were tested with logistic regression modeling.
Frequency and Time Spent in After-School Physical Activity Programs (Hypothesis 2)
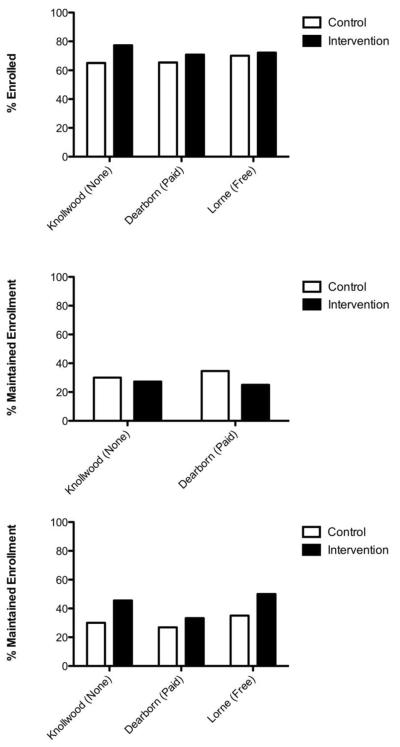
Table 4 compares the number of times children attended after school physical activity programs per week (i.e., attendance) and the total time spent (in minutes) in after-school physical activity programs between groups at the post-intervention and follow-up. After controlling for covariates, group differences in times per week of attendance to after-school physical activity programs were not statistically significant. However, there was a trend in the group x school interaction for times per week of attendance to after-school physical activity programs at the post-intervention assessment (F99 = 2.94, p = 0.06). As shown in Figure 2, the intervention group attended statistically more sessions per week than the control in the school with the fee-based after-school physical activity program than the school that did not offer any after-school physical activity programs (t1 = 2.36, p = .02), with the group differences in total time spent in after school physical activity programs during the intervention did not differ between groups.
Table 4.
Survey data by group across measurements
| Baseline | Post-Inter vention | Follow-Up | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | ||||||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||||||||
| How is your child's health? | |||||||||||||||||||
| Poor | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 1 | 3.8% | 0 | 0.0% | |||||||
| Fair | 3 | 5.7% | 0 | 0.0% | 3 | 6.8% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | |||||||
| Good | 11 | 20.8% | 10 | 19.2% | 6 | 13.6% | 10 | 23.3% | 8 | 30.8% | 6 | 26.1% | |||||||
| Very Good | 11 | 20.8% | 17 | 32.7% | 8 | 18.2% | 10 | 23.3% | 4 | 15.4% | 4 | 17.4% | |||||||
| Excellent | 28 | 52.8% | 25 | 48.1% | 27 | 61.4% | 23 | 53.5% | 13 | 50.0% | 13 | 56.5% | |||||||
| Over the past 30 days, has your child walked or bicycled as part of getting to and from school? | |||||||||||||||||||
| Yes | 17 | 32.1% | 5 | 10.0% | 17 | 38.6% | 10 | 23.3% | 11 | 42.3% | 2 | 9.1% | |||||||
| No | 36 | 67.9% | 45 | 90.0% | 27 | 61.4% | 33 | 76.7% | 15 | 57.7% | 20 | 90.9% | |||||||
| During the last four months, has yo ur child enrolled in an after -school physical activity program? | |||||||||||||||||||
| Yes | 29 | 53.7% | 32 | 61.5% | 24 | 54.5% | 30 | 68.2% | 18 | 69.2% | 16 | 69.6% | |||||||
| No | 25 | 46.3% | 20 | 38.5% | 20 | 45.5% | 14 | 31.8% | 8 | 30.8% | 7 | 30.4% | |||||||
| N | M | SD | N | M | SD | N | M | SD | N | M | SD | N | M | SD | N | M | SD | ||
| Howm any times per week did you child typically attend the after school physical activity program? | |||||||||||||||||||
| 28 | 3.4 | 1.9 | 32 | 2.8 | 1.3 | 24 | 3.7 | 1.5 | 29 | 2.9 | 1.6 | 18 | 2.7 | 1.3 | 16 | 3.7 | 1.1 | ||
| On each of the times that the program meets, how long does it last? | |||||||||||||||||||
| 29 | 81.8 | 33.7 | 30 | 86.0 | 52.4 | 24 | 117.3 | 86.6 | 29 | 85.9 | 43.7 | 18 | 108.1 | 53.1 | 15 | 99.7 | 50.7 | ||
| Number of weeks child attended after school physical activity program over the past4 months | |||||||||||||||||||
| 28 | 11.0 | 5.9 | 30 | 10.5 | 5.3 | 24 | 11.5 | 4.7 | 30 | 12.0 | 4.1 | 17 | 13.3 | 4.5 | 15 | 12.0 | 5.6 | ||
| Dose for 4 Months (times perw week × length of time × number of weeks): | |||||||||||||||||||
| 27 | 3775 | 3979 | 29 | 2632 | 3160 | 24 | 5339 | 5203 | 29 | 3244 | 3378 | 17 | 4844 | 4502 | 14 | 5468 | 4336 | ||
Figure 2.
Hypothesis 1 by School and Group
MVPA (Hypothesis 3)
Group comparisons in descriptive statistics for average MVPA min·day−1 (measured by accelerometer) at the post-intervention and follow-up time points are shown in Table 5. After controlling for covariates, group differences in average MVPA min·day−1 were not statistically significant for either time point. However, average MVPA min·day−1 was significantly lower among children whose parents were not married (β =−39.4, β =−54.4, p = .08) and at post-intervention and follow-up, respectively.
Table 5.
Moderate - Vigorous Activity (Mets) by group across measurements
| Baseline | Post-Intervention | Follow -Up | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | |||||||||||||
| N | M | SD | N | M | SD | N | M | SD | N | M | SD | N | M | SD | N | M | SD | |
| Exercise Diary (Mets) | ||||||||||||||||||
| Week | 40 | 3158 | 1790 | 39 | 3049 | 1598 | 25 | 4105 | 2332 | 30 | 4002 | 2236 | 16 | 50 94 | 1858 | 13 | 4141 | 2513 |
| Weekday | 43 | 1853 | 1138 | 41 | 1895 | 1150 | 26 | 2741 | 1615 | 32 | 2377 | 1596 | 17 | 27 42 | 1571 | 13 | 2513 | 1521 |
| Weekend | 40 | 1315 | 934 | 40 | 1164 | 816 | 25 | 1457 | 1042 | 30 | 1609 | 900 | 16 | 21 81 | 1084 | 13 | 1628 | 1577 |
| Accelerometer (min/day) | ||||||||||||||||||
| Daily Averaqe | ||||||||||||||||||
| Week | 30 | 86.7 | 26.1 | 28 | 79.5 | 31.4 | 18 | 71.9 | 27.8 | 10 | 83.7 | 24.9 | 14 | 76. 6 | 29.6 | 10 | 71.9 | 29.4 |
| Weekday | 37 | 83.7 | 26.1 | 33 | 79.1 | 33.5 | 20 | 80.0 | 37.3 | 17 | 83.0 | 25.6 | 21 | 73. 8 | 30.8 | 15 | 75.9 | 29.1 |
| Weekend | 26 | 78.5 | 45.4 | 21 | 74.8 | 35.7 | 17 | 78.2 | 45.9 | 9 | 77.3 | 28.7 | 15 | 75. 5 | 37.8 | 10 | 69.1 | 41.1 |
| Percent per week | ||||||||||||||||||
| Week | 30 | 3.4% | 1.5% | 28 | 3.3% | 1.3% | 18 | 2.9% | 0.9% | 10 | 3.4% | 1.1% | 14 | 3.0% | 1.2% | 10 | 3.3% | 1.6% |
| Weekday | 37 | 3.4% | 1.6% | 33 | 3.2% | 1.3% | 20 | 3.1% | 1.3% | 17 | 4.0% | 1.6% | 21 | 3.3% | 1.4% | 15 | 3.7% | 1.6% |
| After School | ||||||||||||||||||
| Average | 33 | 38.0 | 13.1 | 30 | 38.4 | 19.0 | 19 | 39.8 | 32.8 | 16 | 41.6 | 23.9 | 19 | 38. 5 | 19.9 | 12 | 40.3 | 20.3 |
| Percent | 33 | 3.5% | 1.4% | 30 | 3.7% | 2.0% | 19 | 3.7% | 3.4% | 16 | 4.1% | 2.2% | 19 | 3.9% | 2.3% | 12 | 3.9% | 2.1% |
Note. Daily minimum for Accelerometers are as follows 4 days for week and weekday, and 2 days for weekend. After school minimum was 2 days.
DISCUSSION
This study used a randomized controlled trial design to test the effectiveness of a simulated tax incentive program at increasing low-income children's participation in organized after-school physical activity. A number of national- and state-level governing bodies have either proposed or implemented the use of tax incentives to promote physical activity.41,42 However, only one study to date has directly evaluated the impact of a non-refundable tax incentive on physical activity, but results did not offer support for its effectiveness.43 Results of the current study indicate that the simulated tax credits did not significantly influence low-income children's rates of enrollment in after-school physical activity programs, frequency of participation and time spent in after-school physical activity programs, or overall moderate-to-vigorous intensity physical activity at post-intervention or follow-up. However, there was a post-intervention trend suggesting that children eligible for the simulated tax credits were 80% more likely than children in the control group to have enrolled in an after-school physical activity program. Given that our post-hoc power was rather low, these findings are in line with a small yet emerging body of evidence suggesting that low-income families may not benefit from tax credit programs to promote children's physical activity.42,44 In a recent analysis of the Children's Fitness Tax Credit (CFTC) system in Canada, a federal policy implemented in 2007 offering a non-refundable tax credit of up to $500 to register a child in an eligible physical activity program, low-income families were less aware of and less likely to claim the tax credit.43 Post-hoc analyses of the current study, found that 21% of families submitted the paperwork to receive the $200 in monetary credit to cover the costs of enrollment in physical activity programs. This rate is similar to the 28% of families in the lowest income quartile claiming the CFTC in the 2007 tax years in the large Canadian study.43
The simulated refundable tax credit examined in this study may have placed an undue burden on the participants because the estimated sufficiency of covering half of the anticipated costs of the programs may not have been enough of a financial relief to the participants. Families were required to cover the costs of the physical activity program out of pocket up front. For many low-income families, these initial costs might have been prohibitive, regardless of the opportunity for delayed reimbursement. While prior studies have found cash subsidies to have an impact on certain health behaviors,17 those studies have only looked at direct assistance to the individual where the individual did not have to front the money in order to engage in the targeted health behavior. The 2007 Canadian CFTC study concluded that tax credits appear to only benefit taxpayers who are wealthy enough to afford to pay upfront costs of a physical activity program and wait for reimbursement following the end of the tax year.
An important finding in the current study was the observed difference in the effectiveness of the simulated tax credit program across schools. The simulated tax credit intervention appeared to be the most effective in the school that only offered a fee-based after-school physical activity program. As compared with schools that offered free or no after-school physical activity programs, there were larger group differences observed in the school offering fee-based programming, with the simulated tax incentive intervention group showing greater participation in after-school physical activity programs in terms of the number of sessions attended per week and the total number of sessions attended. These findings suggest that in order for tax credits to be incentivizing, reimbursable physical activity programs may need to be readily available (e.g., offered on site) and not necessarily require additional time and transportation costs, as suggested by economic models.41
Taken together, these findings may have some relevant implications for future tax policies to promote physical activity. First, as also suggested by others, tax credit policies for participation in qualified physical activity programs utilizing delayed reimbursement (i.e., refundable tax credit) or income tax reduction methods (i.e., tax deduction) may do little to ultimately reduce income-related disparities in physical activity and obesity.4,2,43 Some have argued that these types of programs may even go so far as to increase inequities because higher income families, with more expendable income up front and higher income tax payments, may be more likely to take advantage of them.43 Instead, it has been recommended that funds may be better spent subsidizing physical activity programming to lower or eliminate up-front costs through direct payments to the service providers, and building new and improving existing physical activity infrastructure such as parks and playgrounds.43 However, the current study is the first known to test the effectiveness of a simulated tax credit program to promote children's physical activity through a rigorous RCT. Results need to be replicated in other studies before any definitive conclusions can be made.
Despite the strengths of the study design, including a randomized control group; multiple follow-up measurements; and objective physical activity and anthropometric measures; this study had a few limitations. First, it was not adequately powered to detect some of the small effect sizes that were observed. A priori power analyses were based on the sample size (N = 144) necessary to detect a medium effect size of .5 (assuming 80% power and a two-sided significance level of 0.05), which had been observed in previous school- and community-based interventions to increase physical activity.45 Also, challenges with recruitment and greater attrition than expected further reduced the sample size at the follow-up time point (n = 54) from what was planned in the original power calculation (n = 128 after attrition). Furthermore, accelerometers could only be used in a subsample due to cost restrictions, further limiting the ability to detect significant group difference in objectively-measured physical activity level. The limited use of accelerometers also increased the reliance on self- and parent-reported physical activity outcomes, which may be prone to recall errors and biases46,47Another potential limitation was the use of simulated instead of actual tax credits. It is not known whether families would behave differently in response to the implementation of a true tax credit system. Also, the study was limited in exploring a single tax credit amount. Future studies may test different amounts of tax credits, thereby determining whether a behavior response may result from a different incentive level. Lastly, this study was conducted in primarily low-income, Hispanic families residing in Southern California. While we did manage to target an at-risk population, the extent to which results generalize to other populations, settings, and regions of the country is unknown.
Results from the current study suggest that the use of refundable tax credits as incentives to increase participation in after-school physical activity programs in low-income families may have limited effectiveness. It appears that the promise of reducing parents' taxes in the future is not enough to encourage their children to exercise now. Lawmakers might consider other methods of fiscal policy to promote physical activity such as direct payment to an after-school physical activity program provider for enrolling and serving a low-income child in a qualified program, or improvements to programming and infrastructure.
Table 1.
Number of Classrooms and Participants in Each of the Three Schools
| Elementary School Offering no After School Physical Activity Program | Elementary School Offering After School Physical Activity Program for a Fee | Elementary School Offering After School Physical Activity Program for Free | |
|---|---|---|---|
| 1st Grade | 3 (n=6) | 2 (n=4) | 3 (n=5) |
| 2nd Grade | 3 (n=10) | 3 (n=11) | 2 (n=3) |
| 3rd Grade | 1 (n=3) | 4 (n=9) | 5 (n=6) |
| 4th Grade | 3 (n=15) | 4 (n=11) | 5 (n=14) |
| 5th Grade | 3 (n=6) | 2 (n=3) | 4 (n=5) |
| Total | 13 (n=40) | 13 (n=38) | 19 (n=35) |
ACKNOWLDEGMENTS
The authors would like to gratefully acknowledge the support and hard work of the following research assistants: Swati Swati, Mandeep Kaur, Sally Ghasemi, James Hernandez, Jessica Hernandez, Marbella Lupercio, and Galina Yankulovska.
FUNDING SOURCE This study was supported through a grant from the Robert Wood Johnson Foundation (Grant number: 68492), California State University, Northridge's Research Fellowship Program, and by NIH Research Infrastructure in Minority Institutions (RIMI) from the National Institute of Minority Health and Health Disparities, P20 MD003938.
REFERENCES
- 1.Levy J, Vinter S, Richardson L, Laurent R, Segal LM. F As in fat: how obesity policies are failing in America. Trust for America's Health; Washington D.C.: 2009. [Google Scholar]
- 2.Polhamus B, Dalenius K, Mackintosh H, Smith B, Grummer-Strawn L. Pediatric Nutrition Surveillance 2008 Report. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta: 2009. [Google Scholar]
- 3.Hanson MD, Chen E. Socioeconomic status and health behaviors in adolescence: a review of the literature. J Behav Med. 2007;30(3):263–85. doi: 10.1007/s10865-007-9098-3. [DOI] [PubMed] [Google Scholar]
- 4.Janssen I, Boyce WF, Simpson K, Pickett W. Influence of individual-and-are-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. Am J Clin Nutr. 2006;83:139–145. doi: 10.1093/ajcn/83.1.139. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Physical activity levels among children aged 9–13 years- United States, 2002. MMWR CDC Surveillance Summaries. 2003;52:785–788. [PubMed] [Google Scholar]
- 6.Edmunson K, Dithmer BL. Developing opportunities for participation in structured activities for children and youth. 1997. [Google Scholar]
- 7.Romero AJ. Low-income neighborhood barriers and resources for adolescents' physical activity. J Adolesc Health. 2005;36:253–259. doi: 10.1016/j.jadohealth.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 8.Trost SG, Rosenkranz RR, Dzewaltowski D. Physical activity levels among children attending after-school programs. Medicine & Science in Sports & Exercise. 2008;40:622–629. doi: 10.1249/MSS.0b013e318161eaa5. [DOI] [PubMed] [Google Scholar]
- 9.Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, Pruitt LA, Powell TM, Owens AS, Thompson NS, Flint-Moore NM, Davis GJ, Emig KA, Brown RT, Rochon J, Green S, Varady A. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis. 2003;13:S65–77. [PubMed] [Google Scholar]
- 10.Becker GS. A theory of allocation of time. Econ. J. 1965;75:493–517. [Google Scholar]
- 11.Faulkner GE, Grootendorst P, Nguyen VH, Andreyeva T, Arbour-Nicitopoulos K, Auld MC, Cash SB, Cawley J, Donnelly P, Drewnowski A, Dubé L, Ferrence R, Janssen I, Lafrance J, Lakdawalla D, Mendelsen R, Powell LM, Traill WB, Windmeijer F. Economic instruments for obesity prevention: results of a scoping review and modified Delphi survey. Int J Behav Nutr Phys Act. 2011;8:109–121. doi: 10.1186/1479-5868-8-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzgibbon ML, Stolley MR. Environmental changes may be needed for prevention of overweight in minority children. Pediatr Ann. 2004;33:45–49. doi: 10.3928/0090-4481-20040101-12. [DOI] [PubMed] [Google Scholar]
- 13.HSC Foundation . Preventing childhood obesity in lower-income communities: a focus group report of African-American and Latino families' understanding of healthy lifestyles, barriers, and challenges. 2007. [Google Scholar]
- 14.Grier S, Kumanyika S. Targeting interventions for ethnic minority and low income populations. The Future of Children. 2006;16:187–207. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- 15.Holt NL, Cunningham CT, Sehn ZL, Spence JC, Newton AS, Ball GD. Neighborhood physical activity opportunities for inner-city children and youth. Health Place. 2009;15(4):1022–8. doi: 10.1016/j.healthplace.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Humbert ML, Chad KE, Spink KS, Muhajarine N, Anderson KD, Bruner MW, Girolami TM, Odnokon P, Gryba CR. Factors that influence physical activity participation among high- and low- SES youth. Qualitative Health Research. 2006;16:467–483. doi: 10.1177/1049732305286051. [DOI] [PubMed] [Google Scholar]
- 17.Kane RL, Johnson PE, Town RJ, Butler M. A structured review of the effect of economic incentives on consumers' preventive behavior. Am J Prev Med. 2004;27(4):327–52. doi: 10.1016/j.amepre.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Mytton O, Gray A, Rayner M, Rutter H. Could targeted food taxes improve health? J Epidemiol Community Health. 2007;61:689–694. doi: 10.1136/jech.2006.047746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuchler F, Tegene A, Harris MJ. Taxing snack foods: what to expect for diet and tax revenues. Review of Agricultural Economics. 2005;27(1):4–20. [Google Scholar]
- 20.Jeffrey RW, French S, Raether C, Baxter JE. An environmental intervention to increase fruit and salad purchases in a cafeteria. Prev Med. 1994;23:788–792. doi: 10.1006/pmed.1994.1135. [DOI] [PubMed] [Google Scholar]
- 21.Winstanley CL. A health food tax credit: moving away from the fax tax and its fault based paradigm. Oregon Law Review. 2007;86:1152–1200. [Google Scholar]
- 22.Johnson N. A hand up: how state earned income tax credits help working families escape poverty in 2001. Center on Budget and Policy Priorities; Washington D.C.: 2001. pp. 1–48. [Google Scholar]
- 23.Vieweg VR, Johnston CH, Lanier JO, Fernandez A, Pandurangi AK. Correlation between high risk obesity groups and low socioeconomic status in school children. South Med J. 2007;100(1):8–13. doi: 10.1097/01.smj.0000253479.03665.6f. [DOI] [PubMed] [Google Scholar]
- 24.California Department of Education . Health framework for California public schools: kindergarten through grade twelve. 2002. [Google Scholar]
- 25.Baker JL, Olsen LW, Sørensen TIA. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–2337. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brustad RJ. Who will go out and play? parental and psychological influences on children's attraction to physical activity. Pediatr Exercise Sci. 1993;5:210–223. [Google Scholar]
- 27.Welk GJ, Wood K, Morss G. Parental influences on physical activity in children: an exploration of potential mechanisms. Pediatr Exerc Sci. 2003;15:19–33. [Google Scholar]
- 28.Urbaniak GC, Plous S. Research Randomizer (Version 4.0) [Computer software] 2013 Retrieved on June 22, 2013, from http://www.randomizer.org/
- 29.King AC, Kiernan M, Ahn DK, Wilcox S. The effects of marital transitions on changes in physical activity: Results from a 10-year community study. Annals of Behavioral Medicine. 1999;20:64–69. doi: 10.1007/BF02884450. [DOI] [PubMed] [Google Scholar]
- 30.Juster F, Stafford FP. Time, goods, and well-being. Institute for Social Research; Ann Arbor, MI: 1985. [Google Scholar]
- 31.Timmer SG, Eccles J, O'Brien K. How children use time. In: Juster FP, editor. Time, Goods, and Well-Being. Institute for Social Research; Ann Arbor, MI: 1985. pp. 353–382. [Google Scholar]
- 32.Ridley K, Ainsworth BE, Olds TS. Development of a compendium of energy expenditures for youth. Int J Behav Nutr Phys Act. 2008;5:45. doi: 10.1186/1479-5868-5-45. DOI: http://dx.doi.org/10.1186/1479-5868-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reilly JJ, Kelly LA, Montgomery C, Jackson DM, Slater C, Grant S, Paton JY. Validation of Actigraph accelerometer estimates of total energy expenditure in young children. Int J Pediatr Obes. 2006;1:161–167. doi: 10.1080/17477160600845051. [DOI] [PubMed] [Google Scholar]
- 34.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11):S531–43. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 35.Corder K, Ekelund U, Steele RM, Wareham NJ, Brage S. Assessment of physical activity in youth. J Appl Physiol. 2008;105:977–987. doi: 10.1152/japplphysiol.00094.2008. [DOI] [PubMed] [Google Scholar]
- 36.Treuth MS, Sherwood NE, Butte NF, McClanahan B, Obarzanek E, Zhou A, Ayers C, Adolph A, Jordan J, Jacobs DR, Rochon J. Validity and reliability of activity measures in African-American girls for GEMS. Med Sci Sports Exerc. 2003;35(3):532–9. doi: 10.1249/01.MSS.0000053702.03884.3F. [DOI] [PubMed] [Google Scholar]
- 37.Freedson PS, Melanson E, Sirard J. Calibration of the computer science and applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–81. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 38.Freedson P, Pober D, Janz KF. Calibration of accelerometer output for children. Med Sci Sports Exerc. 2005;37(11):S523–S30. doi: 10.1249/01.mss.0000185658.28284.ba. [DOI] [PubMed] [Google Scholar]
- 39.Harrell JS, McMurray RG, Baggett CD, Pennell ML, Pearce PF, Bangdiwala SI. Energy costs of physical activities in children and adolescents. Med Sci Sports Exerc. 2005;37(2):329–36. doi: 10.1249/01.mss.0000153115.33762.3f. [DOI] [PubMed] [Google Scholar]
- 40.Roemmich JN, Clark PA, Walter K, Patrie J, Weltman A, Rogol AD. Pubertal alterations in growth and body composition. V. Energy expenditure, adiposity, and fat distribution. American Journal of Physiology-Endocrinology and Metabolism. 2000;279(6):E1426–E36. doi: 10.1152/ajpendo.2000.279.6.E1426. [DOI] [PubMed] [Google Scholar]
- 41.Pratt M, Macera CA, Sallis JF, O'Donnell M, Frank LD. Economic interventions to promote physical activity: application of the SLOTH model. Am J Prev Med. 2004;27(suppl 3):136–145. doi: 10.1016/j.amepre.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 42.von Tigerstrom B, Larre T, Sauder J. Using the tax system to promote physical activity: critical analysis of Canadian initiatives. Am J Public Health. 2011;101(8):e10–6. doi: 10.2105/AJPH.2011.300201. doi: 10.2105/AJPH.2011.300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spence JC, Holt NL, Dutove JK, Carson V. BMC Public Health. 2010. Uptake and effectiveness of the children's fitness tax credit in Canada: the rich get richer; p. 356. doi: 10.1186/1471-2458-10-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spence JC, Holt NL, Sprysak CJ, Spencer-Cavaliere N, Caulfield T. Non-refundable tax credits are an inequitable policy instrument for promoting physical activity among Canadian children. Can J Public Health. 2012;103(3):175–7. doi: 10.1007/BF03403808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holtzman J, Schmitz K, Babes G, Kane RL, Duval S, Wilt TJ, MacDonald RM, Rutks I. Effectiveness of behavioral interventions to modify physical activity behaviors in general populations and cancer patients and survivors. evidence report/technology assessment No.102 (Prepared by the Minnesota Evidence-based Practice Center, under Contract No. 290-02-0009.) AHRQ Publication No. 04-E027-2. Agency for Healthcare Research and Quality; Rockville, MD: Jun, 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sirard JR, Pate RR. Physical activity assessment in children and adolescents. Sports Med. 2001;31:439–454. doi: 10.2165/00007256-200131060-00004. [DOI] [PubMed] [Google Scholar]
- 47.Sallis JF. Self-report measures of children's physical activity. J Sch Health. 1991;61:215–219. doi: 10.1111/j.1746-1561.1991.tb06017.x. [DOI] [PubMed] [Google Scholar]