Abstract
Cancer self-efficacy (CSE) and spiritual well-being (SWB) have been associated with better self-rated health (SRH) among breast cancer survivors (BCS), but have not been well studied among Latina BCS (LBCS). Multivariate logistic regression analyses of secondary data from a cross-sectional population-based telephone survey of 330 LBCS explored relationships of language acculturation, CSE, and SWB subdomains of inner peace and faith with SRH. English proficiency was associated with SRH, independent of other covariates (OR=2.26, 95% CI 1.15, 4.45). Cancer self-efficacy attenuated this effect and was positively associated with SRH (OR=2.24, 95% CI 1.22, 4.10). Adding inner peace (a SWB subscale) attenuated the association of CSE and SRH (OR=1.67, 95% CI 0.88, 3.18). Inner peace remained associated with SRH (OR= 2.44, 95% CI 1.30, 4.56), controlling for covariates. Findings support the importance of a sense of inner peace and control over breast cancer to LBCS' perceived health.
Keywords: Latinas/Hispanics, breast cancer, acculturation, cancer self-efficacy, spiritual well-being, self-rated health
Latina breast cancer survivors (LBCS) experience marked health disparities compared with their non-Latino White counterparts. Specifically, LBCS are diagnosed at later stages of disease, with larger tumors, and are 20% more likely to die of breast cancer (accounting for age and stage).1,2 Furthermore, LBCS experience greater psychosocial distress and poorer health related quality of life (HRQOL) than non-Latina White women with breast cancer.3,4
Ethnic disparities in HRQOL persist for LBCS relative to non-Latino White women after accounting for socioeconomic and treatment differences, suggesting cultural or other factors may be operating.4–7 Most research on LBCS is descriptive. Few studies have identified factors that may account for HRQOL differences within LBCS. Acculturation has received some attention with findings indicating that greater acculturation is associated with better HRQOL among LBCS.8–10 Acculturation captures the fluid, multidimensional nature of culture and is measured by proxies of nativity, generation, and language proficiency.11,12 Language proficiency is a particularly useful acculturation measure in health disparities research because of its central role in seeking, understanding, and applying health information.13 Acculturation has also been associated positively with self-rated health (SRH)14–16 among Latinos in general. Among cancer survivors, SRH is a better predictor of survival than HRQOL.17–19
Despite these findings, the relationship between acculturation and SRH among LBCS has not been elucidated. Among LBCS a potential mediator of the association of acculturation with SRH is confidence in one's ability to manage the effects of cancer (cancer self-efficacy). Greater cancer self-efficacy has been associated with better HRQOL or less depressive symptoms in people with cancer,20–22 less distress among multiethnic breast cancer survivors,23 and better SRH and fewer functional limitations among LBCS.24 However, among LBCS, no one has examined intragroup variability in cancer self-efficacy or if it mediates the effects of acculturation on SRH.
Another potential mediator of the relationship between level of acculturation and SRH among LBCS is spirituality. Spiritual well-being is a measure of spirituality that captures religious and non-religious sources of faith and inner peace; it has been shown to be independently associated with HRQOL.25 Qualitative studies of Latinos with cancer, including breast cancer, have identified spiritual well-being as an important culturally-based cancer coping strategy.26–29 One study among LBCS found a positive association of spirituality and SRH.24 However, studies of the associations between acculturation and spiritual well-being among LBCS are lacking. Additionally, the relative impact of two subdomains of spiritual well-being, faith (religious aspects of spirituality) and inner peace (non-religious aspects of spirituality), on SRH have not been explored. Clearly, more studies of this culturally salient theme in the context of breast cancer are needed.25
Theoretical framework
Psychosocial models of adaptation to cancer combine social-cognitive 30 and coping theories,31–33 and posit multidimensional social, cultural, cognitive, and spiritual facets of adaptation processes. The constructs of cancer self-efficacy and spiritual well-being, often included in these frameworks, may be rooted in cultural beliefs and thus can differ by ethnicity and level of acculturation. Guided by psychosocial models of coping, this study aimed to assess whether cancer self-efficacy and spiritual well-being (religious and non-religious aspects) are associated with acculturation, and whether they mediate the relationship between acculturation and SRH among LBCS. We hypothesized that greater acculturation is associated positively with SRH, and that this relationship is partially mediated by cancer self-efficacy and spiritual well-being.
Methods
Population studied
The study in which these data were collected aimed to identify predictors of cancer support group utilization among LBCS through a cross-sectional telephone survey conducted between April and September of 2004, recruiting patients from the Greater Bay Area Cancer Registry of the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program. ⋆ Recruitment is described elsewhere.34 The population studied included women of any age and national origin; women were eligible to participate if they: 1) self-identified as Latina; 2) were diagnosed with their first in-situ, localized, or regional stage breast cancer between 1999–2002 (within five years of the original survey); and 3) resided in one of four Northern California counties. Women were ineligible if they had metastatic (Stage IV) breast cancer or cognitive impairment compromising the interview quality (by interviewer judgment).
Data collection
Two weeks after mailing of an initial contact packet, women who did not return a refusal postcard were phoned by an experienced bilingual-bicultural interviewer who obtained verbal informed consent prior to the interview. The interview was conducted in Spanish or English, depending on the preference of the respondent. This secondary data project used a de-identified dataset so the University of California San Francisco Institutional Review Board determined it did not constitute human subjects research. All procedures for the original study were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5), and informed consent was obtained from all participants.
Measures
Variables were self-reported unless otherwise stated. Covariates included education level (6th grade or less, 7th grade to high school diploma/GED, more than high school), employment status (employed versus unemployed), health insurance (private, public only, or none), age at time of interview in years, comorbid chronic health conditions (yes or no), type of surgery (breast conserving surgery versus mastectomy), and tumor registry reported stage at diagnosis.
Predictor variables included acculturation indicators of English proficiency, language acculturation, and country of origin. English proficiency was based on the item “How well do you speak English?” and dichotomized as English proficient (very well/well) versus limited English proficient (LEP) (fairly well/poorly/not at all). Language acculturation was assessed using a four-item version of the previously validated Short Acculturation Scale for Hispanics (SASH)35 that asked the language they read and speak in general, speak at home, usually think in, and speak with friends (1=only Spanish; 2=Spanish better/more than English; 3=both equally; 4=English better/more than Spanish; and 5=English only)35. The validity of the SASH has been demonstrated among Latinos in the U.S. by its strong correlations with respondent's generation, length of time in the U.S. and age at arrival in the U.S.35 Cronbach's alpha for the acculturation scale was .95 in our sample. Mean language acculturation scores were dichotomized as ≤2.99 = “less acculturated” and >2.99 = “more acculturated.” 35 Country of origin was assessed by asking, “In what country were you born?” with response options of “U.S.” and “Other.”
Potential mediators included cancer self-efficacy and spiritual well-being. Cancer self-efficacy was measured with a 6-item scale adapted from the Cancer Behavior Inventory-Breast Cancer (CBI-B) version 2 36 that assessed confidence in seeking and understanding medical information, accepting cancer, maintaining a positive attitude, and seeking social support. The scale score (possible range=1–4) was the mean of non-missing items; a higher score = greater cancer self-efficacy. The cancer self-efficacy scale demonstrated good convergent validity (i.e., all item-scale correlations were greater than .4) and good divergent validity (i.e., the correlation of an item with its hypothesized scale was at least two standard errors greater than its correlation with other scales). Cronbach's alpha was .80 in our sample.34 For the multivariate models, the cancer self-efficacy score was dichotomized at the median split; a score ≤3.5 was considered “lower self-efficacy” and >3.5 “higher self-efficacy.”
Spiritual well-being was assessed using the previously validated 12-item Functional Assessment of Cancer Therapy Quality of Life Measurement System-Spiritual Well-being Scale (FACIT-Sp, version 4).37 Validity of the FACIT-Sp was supported by its strong correlations with similar measures of religion and spirituality.37 Cronbach's alpha for the scale was 0.82 in our sample.34 The FACIT-Sp can be scored as two subscales: eight-item Peace and four-item Faith scales. Peace assesses a sense of meaning, inner peace, and purpose in life, independent of religious beliefs. Faith assesses the relation between illness and one's faith/spiritual beliefs (e.g., finding comfort and strength in spiritual beliefs). Scores were calculated as the mean of non-missing items with a higher score indicating greater peace or faith. For multivariate analyses, Peace and Faith scores were dichotomized at the median split. Peace scores (range=0– 32) ≤27 were considered “lower sense of peace” and >27 “higher sense of peace.” Faith scores (range=0–16) <16 were considered “lower sense of faith” and =16 “higher sense of faith.”
The outcome variable, SRH, was measured by the item “In general, how would you rate your health?” (1=poor; 2=fair; 3=good; 4=very good; or 5=excellent), dichotomized as fair/poor versus good/very good/excellent. This global self-rated health item is a well-validated measure of self-perceived general health status, demonstrating consistent associations with health risk behaviors, disease states, and mortality.38
Analysis
Descriptive statistics were used to characterize the sample. Simple logistic regression was used to examine bivariate relationships of acculturation with the outcome (SRH), covariates, and potential mediators (cancer self-efficacy, peace, and faith).
Mediation analyses were conducted as recommended by Baron and Kenny.39 According to Baron and Kenny, mediation analysis requires four steps to establish mediation (Figure 1): 1) significant association between the predictor and outcome, without the mediator of interest in the model, (Figure 1, path C); 2) significant association between the predictor and mediator without the outcome in the model (Figure 1, path A); 3) significant association between the mediator and outcome with the predictor in the model (Figure 1, path B); and 4) the relationship between the predictor and outcome should be attenuated when the mediator is included in the model (Figure 1, path C′). Models establishing each of these criteria should include the same covariates. Using multivariate logistic regression, the four mediation steps were modeled separately for each mediator of interest that was related to SRH at p <.15 in bivariate analyses; these models used the same set of predictors and covariates, namely, those associated with SRH in bivariate analyses at p <.15 (except for the acculturation indicators due to problems with co-linearity described below).
Figure 1.
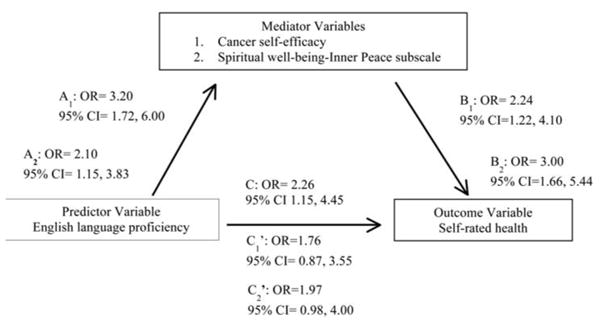
Mediation analysis model illustrating predictor, outcome, and mediator variable relationships with parameter estimates adjusted for odds ratios.
Based on the bivariate and mediation analyses results, a final multivariate logistic regression model estimated the odds of better (good/very good/excellent) SRH. This final model included confirmed mediators and the set of predictors and covariates used in the mediation analyses.
Results
Participant characteristics
The sampling frame consisted of 1,133; 29% (n=333) were unable to be contacted, 22% (n=249) were ineligible, 14% (n=161) declined, and 6% (n=60) were deceased/too ill. Of 491 women who were eligible and reached by telephone, 330 women completed the survey for a 67% response rate (29% of the sampling frame). Compared with non-participants, participants were younger at time of diagnosis (mean=55.8 versus 58.2 years, p<.001) and less likely to have well-differentiated tumors (14% versus 19%, p<.05). There were no significant differences between participants and non-participants by county of residence or stage at diagnosis.
Participants' mean age was 58.3 years (range=30–90 years; SD 11.9) and most had a high school education or less. About sixty percent were foreign-born and 62% were English proficient (Table 1). Approximately 70% were of Mexican origin. Most were within two to three years of diagnosis (86%). Two-hundred-and-six of the surveys were conducted in Spanish and 124 in English. Mean cancer self-efficacy, inner peace, and faith scores were high.
Table 1. Sample Characteristics, Coping Resources and Self-rated Health by English Proficiency, San Francisco Bay Area, 2004, N=330 Latina Breast Cancer Survivors.
| Characteristic | Total Sample N = 330 |
Limited English proficienta n = 126 |
English proficienta n = 204 |
p-value |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age in years, mean (SD) | 58.25 (11.89) | 57.23 (12.56) | 58.89 (11.44) | .219 |
| Education (%)b | ||||
| 6th grade or less | 27 | 57 | 8 | <.001 |
| 7th grade-H.S. diploma/GED | 42 | 31 | 50 | |
| More than high school | 31 | 12 | 42 | |
| Employed (%) | 40 | 28 | 47 | <.01 |
| Type of health insurance (%)c | ||||
| Private | 66 | 41 | 81 | <.001 |
| Public only | 31 | 53 | 18 | |
| No health insurance | 3 | 6 | 1 | |
| Acculturation characteristics | ||||
| Foreign born (%) | 59 | 98 | 35 | <.001 |
| Language acculturation (%) | ||||
| Less acculturated | 49 | 99 | 18 | <.001 |
| More acculturated | 51 | 1 | 82 | |
| Clinical characteristics | ||||
| Stage at diagnosis (%) | ||||
| In situ/localized | 70 | 66 | 72 | .23 |
| Regional | 30 | 34 | 28 | |
| Surgical treatment (%) | ||||
| Breast conserving surgery | 40 | 26 | 47 | <.001 |
| Mastectomy | 60 | 71 | 49 | |
| Has a comorbid chronic condition (%) | 18 | 25 | 13 | <.01 |
| Mediators: intrapersonal coping (mean SD) | ||||
| Cancer self-efficacy (1–4 scale) | 3.43 (0.59) | 3.08 (0.68) | 3.62 (0.45) | <.001 |
| Inner Peace scale (0–32 scale) | 26.60 (5.31) | 28.76 (6.70) | 31.42 (5.45) | <.001 |
| Faith scale (0–16 scale) | 14.20 (2.99) | 14.21 (2.84) | 14.20 (3.09) | .99 |
| Outcome: Self-rated health (%) | ||||
| Good/very good/excellent | 73 | 62 | 80 | <.001 |
| Poor/fair | 27 | 38 | 20 |
Limited English proficient = Speaks English “fairly well/poorly/not at all;” English proficient = speaks English “very well/well.”
Mean language acculturation scores (scale: 1=only Spanish; 2=Spanish better/more than English; 3=both equally; 4=English better/more than Spanish; and 5=English only) were dichotomized as ≤ 2.99 = “less acculturated” and scores > 2.99 = “more acculturated” using a 4-item adapted version of the Short Acculturation Scale for Hispanics (35)
Functional Assessment of Cancer Therapy Quality of Life Measurement System- Spiritual Well-being Scale (FACIT-Sp, version 4) subscales of Inner Peace and Faith.
Bivariate analyses
Only the English proficiency acculturation measure was used in the multivariate models due to its co-linearity with country of origin (r=.61) and SASH language acculturation score (r=.80), and its stronger association with the outcome in bivariate analysis (p<.001, versus p=.14 for country of origin and p<.05 for SASH score). Regarding covariates, age at time of interview and stage at diagnosis were not included in the multivariate analyses because they were not significantly associated with either self-reported English proficiency (p=.22 for age and p=.23 for stage at diagnosis) (Table 1) or SRH (p=.67 for age and p=.90 for stage at diagnosis) in bivariate analyses (Table 2). Regarding hypothesized mediators, the Faith score was not included in the multivariate analyses due to lack of significant associations with English proficiency (p=.99) (Table 1) or SRH (p=.48) in bivariate analyses (Table 2).
Table 2. Sample Characteristics and Coping Resources by Self-Rated Health, San Francisco Bay Area, 2004, N=330 Latina Breast Cancer Survivors.
| Characteristic | Poor/Fair Self-rated Health n = 89 |
Good/Very Good/Excellent Self-rated Healtha n = 241 |
p-value |
|---|---|---|---|
| Age in years, mean (SD) | 57.79 (11.42) | 58.43 (12.08) | .665 |
| Education (%) | |||
| 6th grade or less | 37 | 23 | <.05 |
| 7th grade-H.S. diploma/GED | 41 | 43 | |
| More than high school | 22 | 34 | |
| Employed (%) | 30 | 43 | <.05 |
| Type of health insurance (%) | |||
| Private | 59 | 68 | .115 |
| Public only | 40 | 28 | |
| No health insurance | 1 | 3 | |
| Acculturation characteristics | |||
| Limited English proficiencya (%) | 54 | 32 | <.001 |
| Foreign born (%) | 66 | 57 | .139 |
| Language acculturationb (%) | |||
| Less acculturated | 59 | 45 | <.05 |
| More acculturated | 41 | 55 | |
| Clinical characteristics | |||
| Stage at diagnosis (%) | .897 | ||
| In situ/localized | 69 | 70 | |
| Regional | 27 | 30 | |
| Surgical treatment (%) | 31 | 42 | .241 |
| Breast conserving surgery | 64 | 55 | |
| Mastectomy | 5 | 3 | |
| No surgery | |||
| Has a comorbid chronic condition (%) | 34 | 12 | <.001 |
| Mediators: intrapersonal coping (mean SD) | |||
| Cancer self-efficacy (1–4 scale) | 3.04 (0.74) | 3.55 (0.48) | <.001 |
| Inner Peace scalec (0–32 scale) | 27.43 (7.33) | 31.47 (5.18) | <.001 |
| Faith scalec (0–16 scale) | 14.0 (3.15) | 14.27 (2.93) | .482 |
Limited English proficient = speaks English “fairly well/poorly/not at all.”
Mean language acculturation scores (scale: 1=only Spanish; 2=Spanish better/more than English; 3=both equally; 4=English better/more than Spanish; and 5=English only) were dichotomized as ≤2.99 = “less acculturated” and scores > 2.99 = “more acculturated” using a 4-item adapted version of the Short Acculturation Scale for Hispanics (35).
Functional Assessment of Cancer Therapy Quality of Life Measurement System- Spiritual Well-being Scale (FACIT-Sp, version 4) subscales of Inner Peace and Faith.
In bivariate analyses, higher level of education, being employed, having health insurance, being born in the U.S., greater language acculturation, not having comorbid conditions, having breast-conserving surgery, greater cancer self-efficacy (vs. less), greater inner peace (vs. less), and better self-rated health were associated positively with English proficiency (vs. LEP) (Table 1).
In bivariate analyses, education level and employment status (p=.03 for both) were positively associated with SRH. Having insurance (p=.12) and breast-conserving surgery (p=.11) were also significantly associated with better SRH at p<.15 and were retained in the multivariate models. Not having comorbidities, greater cancer self-efficacy, and greater inner peace were associated with better SRH at p ≤.001 (Table 2).
Mediation analysis
Mediation analysis first established a significant association between English proficiency and SRH, controlling for education, employment status, type of health insurance, comorbid conditions, and type of surgery. English proficient women were more than twice as likely as LEP women to rate their health as good/very good/excellent (OR= 2.26, 95% CI= 1.15, 4.45; Table 3, Model 2; Figure 1, path C).
Table 3. Adjusted Odds Ratios of Good, Very Good or Excellent Self-rated Health, San Francisco Bay Area, 2004, N=330 Latina Breast Cancer Survivorsa.
| Model 1 AOR (95% CI) |
Model 2 AOR (95% CI) |
Model 3 AOR (95% CI) |
Model 4 AOR (95% CI) |
|
|---|---|---|---|---|
| Covariates | ||||
| Education | ||||
| 6th grade or less | 1 | 1 | 1 | 1 |
| 7th grade-H.S. diploma/GED | 1.41 (0.72, 2.74) | 0.98 (0.47, 2.05) | 0.95 (0.45, 2.03) | 1.03 (0.48, 2.23) |
| More than high school | 1.78 (0.81, 3.96) | 1.16 (0.48, 2.80) | 1.08 (0.4, 2.66) | 1.10 (0.44, 2.75) |
| Employment status | ||||
| Unemployed | 1 | 1 | 1 | 1 |
| Employed | 1.25 (0.66, 2.35) | 1.31 (0.69, 2.47) | 1.28 (0.67, 2.45) | 1.37 (0.70, 2.67) |
| Clinical characteristics | ||||
| Presence of comorbid conditions | ||||
| Yes | 1 | 1 | 1 | 1 |
| No | 3.51 (1.79, 6.87) | 3.35 (1.70, 6.60) | 3.27(1.63, 6.57) | 3.56 (1.74, 7.26) |
| Surgical treatment | ||||
| Mastectomy | 1 | 1 | 1 | 1 |
| Breast conserving therapy | 1.22 (0.68, 2.21) | 1.16 (0.64, 2.10) | 1.00 (0.55, 1.85) | 0.93 (0.50, 1.72) |
| Health insurance | ||||
| None | 1 | 1 | 1 | 1 |
| Public only | 0.45 (0.05, 3.90) | 0.39 (0.04, 3.37) | 0.40 (0.04, 3.53) | 0.36 (0.04, 3.29) |
| Private | 0.41 (0.05, 3.50) | 0.29 (0.03, 2.51) | 0.31 (0.04, 2.79) | 0.26 (0.03, 2.40) |
| Language acculturation | ||||
| English proficiencyb | ||||
| Limited English proficient | — | 1 | 1 | 1 |
| English proficient | — | 2.26 (1.15, 4.45) | 1.76 (0.87, 3.55) | 1.71 (0.83, 3.50) |
| Intrapersonal resources | ||||
| Cancer self-efficacyc | ||||
| Lower | — | — | 1 | 1 |
| Higher | — | — | 2.24 (1.22, 4.10) | 1.67 (0.88, 3.18) |
| Spiritual Well-being- Inner Peace subscaled | ||||
| Lower | — | — | — | 1 |
| Higher | — | — | — | 2.44 (1.30, 4.56) |
Adjusted for other variables in the model.
Limited English proficient = speaks English “fairly well/poorly/not at all;” English proficient = speaks English “very well/well.”
Mean Cancer Self-efficacy score ranged from 1–4 and was dichotomized at the median split (≤ 3.5 = “lower cancer self-efficacy”; > 3.5 = “higher cancer self-efficacy”).
Mean Inner Peace scale score ranged from 0–32 and was dichotomized at the median split (≤27 = “lower”; > 27 = “higher”).
AOR=Average Odds Ratio
CI=Confidence Intervals
Next, a significant association between English proficiency and each mediator (cancer self-efficacy and inner peace) had to be established. Controlling for covariates mentioned, English proficiency was associated with cancer self-efficacy; English proficient women were more than three times as likely to have greater cancer self-efficacy than LEP women (OR= 3.20, 95% CI= 1.72, 6.00; results not tabled; Figure 1, path A1). In a separate model not including cancer self-efficacy, but including covariates, English proficiency was significantly associated with inner peace (OR= 2.10, 95% CI= 1.15, 3.83; results not tabled; Figure 1, path A2); English proficient women were twice as likely as LEP women to report greater inner peace.
The third step established significant relationships between the mediators and SRH, controlling for covariates and English proficiency. When cancer self-efficacy was in the model that included covariates and English proficiency (without inner peace), it was positively associated with SRH (OR = 2.24, 95% CI = 1.22, 4.10; Table 3, Model 3; Figure 1, path B1) and English proficiency was no longer significantly associated with SRH (OR = 1.76, 95% CI = 0.87, 3.55; Table 3, Model 3; Figure 1, path C'1). When inner peace was in the model that included covariates and English proficiency (without cancer self-efficacy), it was also significantly associated with SRH (OR= 3.00, 95% CI=1.66, 5.44; not shown on tables; Figure 1, path B2), and English proficiency was no longer significantly associated with SRH (OR = 1.97, 95% CI = 0.98, 4.00; not tabled; Figure 1, path C'2). In each model, cancer self-efficacy and inner peace attenuated the effect of English proficiency on SRH. This satisfied the fourth step of the Baron and Kenny mediation analysis (Figure 1).
Final multivariate model
The final model included covariates and both confirmed mediators. When both cancer self-efficacy and inner peace were in the final multivariate model, along with English proficiency and covariates, cancer self-efficacy was not significantly associated with SRH, but inner peace remained positively associated (OR=2.44, 95% CI=1.30, 4.56) (Table 3, Model 4).
Discussion
This study examined complex relationships between acculturation (English proficiency), cancer self-efficacy, inner peace, and faith, with self-rated health (SRH) among LBCS. English proficiency was positively associated with SRH. Cancer self-efficacy and inner peace mediated this relationship, with inner peace being more strongly related to SRH than cancer self-efficacy. Faith, however, was not associated with English proficiency or SRH, and was relatively high among English- and Spanish-speaking Latinas. Spanish-speaking LBCS were at increased risk of poor SRH and less likely to perceive inner peace and an ability to manage their cancer, emphasizing their need for distress screening and support interventions.
Consistent with the general Latino population,16 acculturation was found to influence SRH such that English proficient LBCS were more likely than LEP LBCS to report better SRH. Cancer self-efficacy was positively associated with SRH, a finding consistent with previous studies among both non-Latino White women and Latinas,20–22 and partially explained the relationship between English proficiency and SRH.
Though spiritual well-being was associated with SRH in a prior study,24 the sub-domains (inner peace and faith) of this construct had not been explored, nor had differences by level of acculturation. In this study assessing these subscales yielded unique findings. While inner peace was associated with language ability and SRH, faith was not. This distinction between religious and non-religious aspects of spirituality among LBCS has not been made in prior research. More importantly, inner peace was a mediator of the relationship between language and SRH, and it attenuated the effect of cancer self-efficacy on this relationship. Studies utilizing the full spiritual well-being scale have shown its association with SRH, and postulated spiritual well-being may act on health status through cancer self-efficacy. The results of this study suggest cancer self-efficacy may act on self-rated health through components of spiritual well-being related to inner peace and meaning in one's life. These findings are consistent with a prior study that found that benefit-finding (sense of meaning after cancer) was associated with better health.40
As mentioned, having a sense of inner peace/meaning in life was associated with better SRH, but a religious source of spiritual well-being was not. Examination of the content of the spiritual well-being subscales provides some insights. While the Peace subscale items inquire about feeling peaceful, having reasons for living, feeling productive in life, and having a sense of purpose in life, the Faith subscale items inquire about comfort and strength garnered through faith/religion. A possible explanation with face validity is that a sense of peace and meaning are outcomes of one's religious faith, therefore, faith is no longer significantly related to SRH once inner peace is taken into account. This interpretation is consistent with anecdotal evidence from the experience of one of the authors (CO) as a cancer support provider, in which Latinas reach an acceptance of their diagnosis, largely due to their religious beliefs. For some cultural groups, this sense of “quiet acceptance” of a breast cancer diagnosis reflects a woman's religious beliefs and cultural upbringing,41 and may represent a cultural construct independent of fatalism that merits further investigation. Fatalism is often characterized as a barrier to positive health behaviors. For example, among Latinas it has been associated inversely with knowledge of cancer risk factors and receipt of cancer screening examinations.42 However, in the face of cancer, quiet acceptance may serve as a positive coping behavior that is distinct from, although related to fatalism.
If these results can be replicated in a longitudinal design, they would support development of interventions that promote increased inner peace and cancer self-efficacy, especially for those with limited English proficiency. Potential interventions include culturally and linguistically appropriate meditation or mindfulness-based practices for LBCS, either individually or in groups. Such interventions that increase positive emotions about life meaning and peace have been found to reduce cancer symptoms and medical visits for cancer- related morbidities.43
The current study had several limitations. Data were collected from less than one third of the sampling frame, thus findings may not be representative. Because the sample was mostly Mexican/Mexican American, the results may only be applicable to this Latino sub-group. Finally, the data come from a cross-sectional survey. Because the temporal sequence of the cancer coping resources and health status is unknown, causation cannot be inferred. Alternative explanations for the mediation findings are reverse causation, (better self-rated health causes a greater sense of peace), that an omitted variable may be causing both inner peace and SRH, or measurement error.
Despite these limitations, this study breaks new ground by revealing relationships between language acculturation, religious and non-religious components of spiritual well-being and cancer self-efficacy, and their effects on self-rated health among LBCS. These findings have important implications for the cancer care of Latinas. They suggest that due to their increased risk of psychosocial morbidity due to cancer, Spanish-speaking Latinas may benefit from routine distress screening in oncology settings, so that timely interventions can be delivered that may decrease and even prevent psychosocial morbidity. Stress management interventions and cognitive-behavioral approaches that seek to improve cancer self-efficacy have resulted in improved HRQOL among White women with breast cancer. Such improvements may be especially marked among high-risk Latinas with breast cancer, although to date these types of psychosocial interventions have not been adequately tested in this population. Interventions that target stress reduction and self-efficacy for managing cancer may help promote an improved sense of inner peace and control among Latinas, which, in turn, could contribute substantially to addressing ethnic and language disparities in HRQOL.44
Acknowledgments
This work was supported by a 2011 Arnold P. Gold Foundation Student Summer Fellowship, the University of California Berkeley-University of California San Francisco (UCSF) Joint Medical Program Schoeneman Award, a 2012 UCSF PROF-PATH Summer Research Award funded by the National Institute on Minority Health and Health Disparities grant no. R25MD006832, the National Cancer Institute grant nos. 1 UO1 CA86117 and U54CA1531511, and the National Institute on Aging grant no. 1 P30-AG15272. Cancer incidence data were collected by the Greater Bay Area Cancer Registry of the Cancer Prevention Institute of California (NCI contract N01-PC–35136), with support from the California Cancer Registry, Cancer Surveillance Section of the California Department of Health Services (Public Health Institute subcontract 1006128). The content of this article does not necessarily reflect the views or policies of the Cancer Prevention Institute of California, the California Public Health Institute, or the U.S. Department of Health and Human Services. This work would not have been possible without the general support of Ndola Prata, M.D., M.Sc. at the University of California Berkeley.
Footnotes
We conducted a thorough search on Pub Med on June 13th, 2014, using the keywords self-rated health, Latinas, and breast cancer. The search yielded only four publications since 2004:
1) Racial/ethnic differences in quality of life after diagnosis of breast cancer. Janz NK, et al. J Cancer Surviv. 2009 Dec;3(4):212–22.
2) Racial and ethnic differences in health status and health behavior among breast cancer survivors—Behavioral Risk Factor Surveillance System 2009. White A, et al. J Cancer Surviv. 2013 Mar;7(1):93–103.
3) Coping resources and self-rated health among Latina breast cancer survivors. Nápoles AM, et al. Oncol Nurs Forum. 2011 Sep;38(5):523–31.
4) The religiosity/spirituality of Latina breast cancer survivors and influence on health-related quality of life. Wildes KA, et al. Psychooncology. 2009 Aug;18(8):831–40.
Although our data date to 2004, there are several key features that distinguish the contributions of our paper from these other papers. First, none of the articles above examined acculturation, spiritual well-being, cancer self-efficacy and self-rated health (SRH) simultaneously as our paper does. Spiritual well-being has been shown to be positively correlated with SRH in low-income Mexican women14 and cancer self-efficacy has been shown to be positively correlated with SRH among Latina breast cancer survivors,24 but whether they may mediate the relationship of acculturation to SRH among Latinas with breast cancer has not been explored. Our prior article did not distinguish between low and high acculturated Latinas, did not test mediation hypotheses, and did not examine the subscales of the spiritual well-being measure as does our current manuscript. Second, only one of the articles distinguished between high and low acculturated Latinas with breast cancer;9 that article used data from 2005– 2007 and only examined mean differences in breast-cancer specific quality of life controlling for sociodemographic, clinical and treatment factors. Third, only our prior article24 from the same study as the current manuscript used the outcome of SRH; two of the others used breast cancer-specific quality of life scales and another compared the health behaviors of breast cancer survivors by ethnicity (without distinguishing between low and high acculturated Latinas). SRH is a widely accepted and well-validated measure of self-perceived general health status and has been found to be an independent predictor of clinical and mortality outcomes among individuals with chronic disease [Layes A, Asada Y, Kepart G. Whiners and deniers—what does self-rated health measure? Soc Sci Med. 2012 Jul;75(1):1–9. Epub 2011 Dec 3]. Among cancer patients, SRH is a better predictor of survival than performance status or quality of life measures,17–19 thus merits further investigation as an outcome. Fourth, none of these articles, with the exception of our prior article, examined cancer self-efficacy. Fifth, only one of the articles (Wildes, 2009) examined spirituality; for that paper, the investigators used a 15-item measure that had been tested only in Latinas in a Mexico City hospital. The measure of religiosity/spirituality that they used differed in definitions and domains of spirituality from the measure used in our study, which has been validated in U.S. Latinas. Finally, our study continues to be one of a few population-based studies of U.S. Latina breast cancer survivors.
In sum, our paper examines: the complex interplay between acculturation; coping resources of cancer self-efficacy, faith and sense of inner peace; and self-rated health among Latinas with breast cancer. Given that no other articles could be found that address all of these factors in a population-based sample of Latinas with breast cancer, the present paper fills a significant gap in the literature.
Disclosures: María García-Jimenez, Jasmine Santoyo-Olsson, Carmen Ortiz, Maureen Lahiff, Karen Sokal-Gutierrez, and Anna María Nápoles disclose that they have no conflict of interest.
Contributor Information
María García-Jimenez, University of California Berkeley-University of California San Francisco Joint Medical Program
Jasmine Santoyo-Olsson, Division of General Internal Medicine and the Center for Aging in Diverse Communities, Department of Medicine, University of California San Francisco
Carmen Ortiz, Círculo de Vida Cancer Support and Resource Center
Maureen Lahiff, Division of Biostatistics, School of Public Health, University of California Berkeley
Karen Sokal-Gutierrez, University of California, Berkeley, School of Public Health and the University of California Berkeley-University of California San Francisco Joint Medical Program
Anna María Nápoles, Division of General Internal Medicine and the Center for Aging in Diverse Communities, Department of Medicine, University of California San Francisco
References
- 1.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national databases. Hum Biol. 2002 Feb;74(1):83–109. doi: 10.1353/hub.2002.0011. http://dx.doi.org/10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Cokkinides V, Jemal A, et al. Cancer facts and figures for Hispanics/Latinos 2009–2011. Atlanta, GA: American Cancer Society; 2009. [Google Scholar]
- 3.Lopez-Class M, Perret-Gentil M, Kreling B, et al. Quality of life among immigrant Latina breast cancer survivors: realities of culture and enhancing cancer care. J Cancer Educ. 2011 Dec;26:724–33. doi: 10.1007/s13187-011-0249-4. http://dx.doi.org/10.1007/s13187-011-0249-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yanez B, Thompson E, Stanton A. Quality of life among Latina breast cancer patients: a systemic review of the literature. J Cancer Surviv. 2010 Jun;5(2):191–207. doi: 10.1007/s11764-011-0171-0. Epub 2011 Jan 28. http://dx.doi.org/10.1007/s11764-011-0171-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kagawa-Singer M. Socioeconomic and cultural influences on cancer care of women. Semin Oncol Nurs. 1995 May;11(2):109–19. doi: 10.1016/s0749-2081(05)80018-x. http://dx.doi.org/10.1016/S0749-2081(05)80018-X. [DOI] [PubMed] [Google Scholar]
- 6.Spencer SM, Lehman JM, Arena P, et al. Concerns about breast-cancer and relations to psychosocial well-being in a multiethnic sample of early-stage patients. Health Psychol. 1999 Mar;18(2):159–68. doi: 10.1037//0278-6133.18.2.159. http://dx.doi.org/10.1037/0278-6133.18.2.159. [DOI] [PubMed] [Google Scholar]
- 7.Eversley R, Estrin D, Dibble S, et al. Post-treatment symptoms among ethnic minority breast cancer survivors. Oncol Nurs Forum. 2005 Mar 5;32(2):250–6. doi: 10.1188/05.ONF.250-256. http://dx.doi.org/10.1188/05.ONF.250-256. [DOI] [PubMed] [Google Scholar]
- 8.Ashing- Giwa K, Rosales M, Lai L, et al. Depressive symptomatology among Latina breast cancer survivors. Psychooncology. 2013 Apr;22(4):845–53. doi: 10.1002/pon.3084. http://dx.doi.org/10.1002/pon.3084. [DOI] [PubMed] [Google Scholar]
- 9.Janz NK, Mujahid MS, Hawley ST, et al. Racial/ethnic differences in quality of life after diagnosis of breast cancer. J Cancer Surviv. 2009 Dec;3(4):212–22. doi: 10.1007/s11764-009-0097-y. http://dx.doi.org/10.1007/s11764-009-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez-Class M, Gomez-Duarte J, Graves K, et al. A contextual approach to understanding breast cancer survivorship among Latinas. Psychooncology. 2012 Feb;21(2):115–24. doi: 10.1002/pon.1998. http://dx.doi.org/10.1002/pon.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phinney J, Flores J. “Unpackaging” acculturation: aspects of acculturation as predictors of traditional sex role attitudes. J Cross-Cult Psychol. 2002 May;33(3):320–31. http://dx.doi.org/10.1177/0022022102033003007. [Google Scholar]
- 12.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systemic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009 Oct;69(7):983–91. doi: 10.1016/j.socscimed.2009.05.011. Epub 2009 jun 13. http://dx.doi.org/10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 13.Carter-Pokras O, Bethune L. Defining and measuring acculturation: a systemic review of public health studies with Hispanic populations in the United States (a commentary on Thomson and Hoffman-Goetz) Soc Sci Med. 2009 Oct;69(7):992–5. doi: 10.1016/j.socscimed.2009.06.042. http://dx.doi.org/10.1016/j.socscimed.2009.06.042. [DOI] [PubMed] [Google Scholar]
- 14.Franzini L, Fernandez-Esquer ME. Socioeconomic, cultural, and personal influences on health outcomes in low income Mexican-origin individuals in Texas. Soc Sci Med. 2004 Oct;59(8):1629–46. doi: 10.1016/j.socscimed.2004.02.014. http://dx.doi.org/10.1016/j.socscimed.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 15.Kandula N, Lauderdale D, Baker D. Differences in self-reported health among Asians, Latinos, and Non-Hispanic Whites: the role of language and nativity. Ann Epidemiol. 2007 Mar;17:191–8. doi: 10.1016/j.annepidem.2006.10.005. http://dx.doi.org/10.1016/j.annepidem.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Shetterly SM, Baxter J, Mason LD, et al. Self-rated health among Hispanic vs Non-Hispanic White adults: the San Luis Valley health and aging study. Am J Public Health. 1996 Dec;86:1789–801. doi: 10.2105/ajph.86.12.1798. http://dx.doi.org/10.2105/AJPH.86.12.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fayers PM, Sprangers MAG. Understanding self-rated health. Lancet. 2002 Jan 19;359(9302):187–8. doi: 10.1016/S0140-6736(02)07466-4. http://dx.doi.org/10.1016/S0140-6736(02)07466-4. [DOI] [PubMed] [Google Scholar]
- 18.Johnson KL, Caroll JF, Fulda KG, et al. Acculturation and self-reported health among Hispanics using a socio-behavioral model: the North Texas healthy heart study. BMC Public Health. 2010 Feb 2;10(53):1–9. doi: 10.1186/1471-2458-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shadbolt B, Barresi J, Craft P. Self-rated health as a predictor of survival among patients with advanced cancer. J Clin Oncol. 2002 May;20(10):2514–9. doi: 10.1200/JCO.2002.08.060. http://dx.doi.org/10.1200/JCO.2002.08.060. [DOI] [PubMed] [Google Scholar]
- 20.Cunningham AJ, Lockwood GA, Cunningham JA. A relationship between perceived self-efficacy and quality of life in cancer patients. Patient Educ Couns. 1991 Feb;17(1):71–8. doi: 10.1016/0738-3991(91)90052-7. http://dx.doi.org/10.1016/0738-3991(91)90052-7. [DOI] [PubMed] [Google Scholar]
- 21.Kreitler S, Peleg D, Ehrenfeld M. Stress, self-efficacy and quality of life in cancer patients. Psychooncology. 2007 Apr;16(4):329–41. doi: 10.1002/pon.1063. http://dx.doi.org/10.1002/pon.1063. [DOI] [PubMed] [Google Scholar]
- 22.Philip EJ, Merluzzi TV, Zhang Z, et al. Depression and cancer survivorship: importance of coping self-efficacy in post-treatment survivors. Psychooncology. 2013 May;22(5):987–94. doi: 10.1002/pon.3088. Epub 2012 May 10. http://dx.doi.org/10.1002/pon.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mosher CE, Duhamel KN, Egert J, et al. Self-efficacy for coping with cancer in a multiethnic sample of breast cancer patients: Associations with barriers to pain management and distress. Clin J Pain. 2010 Mar-Apr;26(3):227–34. doi: 10.1097/AJP.0b013e3181bed0e3. http://dx.doi.org/10.1097/AJP.0b013e3181bed0e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Napoles AM, Ortiz C, O'Brien H, et al. Coping resources and self-rated health among Latina breast cancer survivors. Oncol Nurs Forum. 2011 Sep;38(5):523–31. doi: 10.1188/11.ONF.523-531. http://dx.doi.org/10.1188/11.ONF.523-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brady MJ, Peterman AH, Fitchett G, et al. A case for including spirituality in quality of life measurement in oncology. Psychooncology. 1999 Sep-Oct;8(5):417–28. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. http://dx.doi.org/10.1002/(SICI)1099-1611(199909/10)8:5≤417::AID-PON398≥3.0.CO.2-4. [DOI] [PubMed] [Google Scholar]
- 26.Ashing-Giwa KT, Padilla GV, Bohorquez DE, et al. Understanding the breast cancer experience of Latina women. J Psychosoc Oncol. 2006;24(3):19–52. doi: 10.1300/J077v24n03_02. http://dx.doi.org/10.1300/J077v24n03_02. [DOI] [PubMed] [Google Scholar]
- 27.Juarez G, Ferrell B, Borneman T. Perceptions of quality of life in Hispanic patients with cancer. Cancer Pract. 1998 Nov-Dec;6(6):318–24. doi: 10.1046/j.1523-5394.1998.006006318.x. http://dx.doi.org/10.1046/j.1523-5394.1998.006006318.x. [DOI] [PubMed] [Google Scholar]
- 28.Taylor EJ. Spirituality, culture, and cancer care. Semin Oncol Nurs. 2001 Aug;17(3):197–205. doi: 10.1053/sonu.2001.25949. http://dx.doi.org/10.1053/sonu.2001.25949. [DOI] [PubMed] [Google Scholar]
- 29.Culver JL, Arena PL, Antoni MH, et al. Coping and distress among women under treatment for early stage breast cancer: comparing African Americans, Hispanics and non-Hispanic Whites. Psychooncology. 2002 Nov-Dec;11(6):495–504. doi: 10.1002/pon.615. http://dx.doi.org/10.1002/pon.615. [DOI] [PubMed] [Google Scholar]
- 30.Bandura A. self-efficacy: the exercise of control. 9th. New York, NY: W H Freeman and Company; 1997. Developmental analysis of self-efficacy. [Google Scholar]
- 31.Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993 May-Jun;55(3):234–47. doi: 10.1097/00006842-199305000-00002. http://dx.doi.org/10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Brennan J. Adjustment to cancer-coping or personal transition? Psychooncology. 2001 Nov-Dec;10(3):1–18. doi: 10.1002/1099-1611(200101/02)10:1<1::aid-pon484>3.0.co;2-t. http://dx.doi.org/10.1002/1099-1611(200101/02)10:1≤1::AID-PON484≥3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 33.Kagawa-Singer M, Padilla G, Ashing-Giwa K. Health related quality of life and culture. Semin Oncol Nurs. 2010 Feb;26(1):59–67. doi: 10.1016/j.soncn.2009.11.008. http://dx.doi.org/10.1016/j.soncn.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 34.Napoles-Springer AM, Ortiz C, O'Brien H, et al. Use of cancer support groups among Latina breast cancer survivors. J Cancer Surviv. 2007 Sep;1(3):193–204. doi: 10.1007/s11764-007-0029-7. http://dx.doi.org/10.1007/s11764-007-0029-7. [DOI] [PubMed] [Google Scholar]
- 35.Marin G, Sabogal F, VanOss Marin B, et al. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Science. 1987 Apr;9(2):183–205. http://dx.doi.org/10.1177/07399863870092005. [Google Scholar]
- 36.Merluzzi T, Nairn R, Hedge K. Self-efficacy for coping with cancer: revision of the Cancer Behavior Inventory (version 2.0) Psychooncology. 2001 Nov-Dec;10(2):206–17. doi: 10.1002/pon.511. http://dx.doi.org/10.1002/pon.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peterman A, Fischett G, Brady MJ, et al. Measuring spiritual well-being in people with cancer: the Functional Assessment of Chronic Illness Therapy-Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002 Winter;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. http://dx.doi.org/10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 38.Haddock CK, Poston WS, Pyle SA, et al. The validity of self-rated health as a measure of health status among young military personnel: evidence from a cross-sectional survey. Health Qual Life Outcomes. 2006 Aug;4:1–57. doi: 10.1186/1477-7525-4-57. http://dx.doi.org/10.1186/1477-7525-4-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baron RM, Kenny Da. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986 Dec;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. http://dx.doi.org/10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 40.Antoni M, Lehman JM, Kilbourn K, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and increases benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001 Aug;20(1):20–32. doi: 10.1037//0278-6133.20.1.20. http://dx.doi.org/10.1037/0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 41.Singh- Carlson S, Wong F, Martin L, et al. Breast cancer survivorship and South Asian women: understanding about the follow-up care plan and perspectives and preferences for information post treatment. Curr Oncol. 2013 Apr;20(2):e63–79. doi: 10.3747/co.20.1066. http://dx.doi.org/10.3747/co.20.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramirez AS. Fatalism and cancer risk knowledge among a sample of highly acculturated Latinas. J Canc Educ. 2014 Aug;29(2):50–5. doi: 10.1007/s13187-013-0541-6. http://dx.doi.org/10.1007/s13187-013-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Perez-Stable EJ, Sabogal F, Otero-Sabogal R, et al. Misconceptions about cancer among Latinos and Anglos. JAMA. 1992 Dec 9;268:3219–23. doi: 10.1001/jama.1992.03490220063029. http://dx.doi.org/10.1001/jama.1992.03490220063029. [DOI] [PubMed] [Google Scholar]
- 44.Napoles AM, Santoyo-Olsson J, Ortiz C, et al. Randomized controlled trial of Nuevo Amanecer: a peer-delivered stress management intervention for Spanish-speaking Latinas with breast cancer. Clin Trials. 2014 Apr;11(2):230–8. doi: 10.1177/1740774514521906. Epub 2014 Feb 26. http://dx.doi.org/10.1177/1740774514521906. [DOI] [PMC free article] [PubMed] [Google Scholar]


