Abstract
Duchenne muscular dystrophy (DMD) is a progressive muscle-wasting disorder. It is caused by loss-of-function mutations in the dystrophin gene. Currently, there is no cure. A highly promising therapeutic strategy is to replace or repair the defective dystrophin gene by gene therapy. Numerous animal models of DMD have been developed over the last 30 years, ranging from invertebrate to large mammalian models. mdx mice are the most commonly employed models in DMD research and have been used to lay the groundwork for DMD gene therapy. After ~30 years of development, the field has reached the stage at which the results in mdx mice can be validated and scaled-up in symptomatic large animals. The canine DMD (cDMD) model will be excellent for these studies. In this article, we review the animal models for DMD, the pros and cons of each model system, and the history and progress of preclinical DMD gene therapy research in the animal models. We also discuss the current and emerging challenges in this field and ways to address these challenges using animal models, in particular cDMD dogs.
KEY WORDS: Duchenne muscular dystrophy, Dystrophin, Animal model, Canine DMD, Gene therapy
Introduction
Duchenne muscular dystrophy (DMD) is the most common muscular dystrophy, with a worldwide incidence of one in 5000 live male births according to newborn screening (Emery and Muntoni, 2003; Mendell and Lloyd-Puryear, 2013). It is caused by the lack of dystrophin, a critical muscle protein that connects the cytoskeleton and the extracellular matrix (ECM) (Bonilla et al., 1988; Hoffman et al., 1987). The 2.4-Mb dystrophin gene was discovered in 1986 (Kunkel, 2005; Monaco et al., 1986). It contains 79 exons and encodes a ~14-kb cDNA (Koenig et al., 1987). The full-length protein has four functional domains: the N-terminal (NT), rod, cysteine-rich (CR) and C-terminal (CT) domains. Dystrophin assembles several transmembrane (dystroglycan, sarcoglycan, sarcospan) and cytosolic [syntrophin, dystrobrevin and neuronal nitric oxide synthase (nNOS)] proteins into a dystrophin-associated glycoprotein complex (DAGC) at the sarcolemma (Fig. 1; Box 1 for a glossary of terms) (Ervasti, 2007). Frame-shift mutations of the dystrophin gene abolish protein expression and lead to DMD (Box 1). In-frame deletions often generate truncated dystrophin and result in the milder Becker muscular dystrophy (BMD) (Fig. 2A) (Beggs et al., 1991; Hoffman and Kunkel, 1989; Monaco et al., 1988).
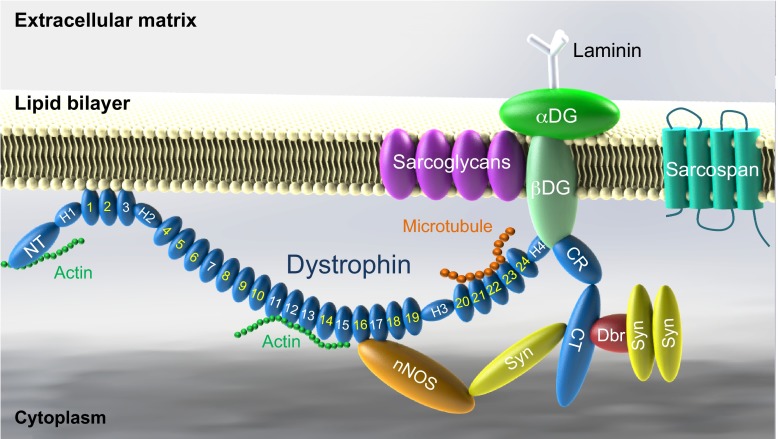
Fig. 1.
Schematic outline of dystrophin and the dystrophin-associated glycoprotein complex (DAGC). Dystrophin contains N-terminal (NT), middle rod, cysteine-rich (CR) and C-terminal (CT) domains. The middle rod domain is composed of 24 spectrin-like repeats (numerical numbers in the cartoon, positively charged repeats are marked in white color) and four hinges (H1, H2, H3 and H4). Dystrophin has two actin-binding domains located at NT and repeats 11–15, respectively. Repeats 1–3 interact with the negatively charged lipid bilayer. Repeats 16 and 17 form the neuronal nitric oxide synthase (nNOS)-binding domain. Dystrophin interacts with microtubule through repeats 20–23. Part of H4 and the CR domain bind to the β-subunit of dystroglycan (βDG). The CT domain of dystrophin interacts with syntrophin (Syn) and dystrobrevin (Dbr). Dystrophin links components of the cytoskeleton (actin and microtubule) to laminin in the extracellular matrix. Sarcoglycans and sarcospan do not interact with dystrophin directly but they strengthen the entire DAGC, which consists of dystrophin, DG, sarcoglycans, sarcospan, Syn, Dbr and nNOS.
Box 1. Glossary.
- Adeno-associated virus (AAV):
a single-stranded DNA virus identified in 1965. AAV has a ~4.7-kb genome and encodes at least three open reading frames (ORFs), one for viral capsid proteins, one for replication proteins and a third one for the assembly-activating protein. In recombinant AAV vectors, viral ORFs are replaced by a reporter or therapeutic expression cassette. An up to 5-kb vector genome can be packaged in an AAV vector. At least 13 different AAV serotypes have been reported. Hundreds of genetically modified AAV capsids have also been developed. AAV can efficiently transduce post-mitotic tissues and wild-type AAV does not cause human disease. Because of these features, AAV has been used in numerous clinical trials.
- Dual and tri-AAV vectors:
engineered AAV vector systems that can deliver a 10-kb (dual vector) or 15-kb (tri-vector) expression cassette. Specifically, a large expression cassette is divided into two pieces (dual vectors) or three pieces (tri-vector). An individual piece contains either a region that overlaps with another piece and/or is engineered with splicing signals. Each piece is packaged in a single viral particle. Co-delivery of vectors containing different pieces of the expression cassette results in reconstitution of the original expression cassette in vivo by cellular recombination mechanisms.
- Exon skipping:
a phenomenon in which one or multiple exons are spliced out and eliminated from the mature mRNA.
- Frame-shift mutation:
a mutation that disrupts the open reading frame of an mRNA transcript.
- Freezing response:
a reflex defense mechanism observed in prey animals where they freeze or completely stop moving when scared.
- Hydrodynamic intravascular delivery:
a technique used for gene delivery where the hydrostatic pressure is applied to increase the permeability of the vascular wall. This allows efficient penetration of gene therapy plasmids into the tissue parenchyma.
- Liposome:
an artificially created lipid-bilayer sphere. A DNA plasmid can be incorporated inside the lipid sphere. The fusion of the lipid bilayer with cell membrane allows delivery of the DNA plasmid into a cell.
- Microspheres:
generic name given to a nanoscale spherical object that can be made out of a variety of materials, including lipids, polymers and metal oxides. They can be used to deliver a DNA plasmid to the cell.
- Nuclease-based gene editing:
DNA gene editing technique that uses endonucleases to make double-stranded breaks in the DNA at a user-specified location to initiate error-prone DNA repair. As a consequence, the DNA sequence at the site of break is altered. These endonucleases are often linked to sequence-specific targeting proteins, such as zinc fingers.
- Phosphorodiamidate morpholino oligomer (PMO):
a synthetic oligonucleotide in which the ribose or deoxyribose backbone is replaced by a morpholine ring and the phosphate replaced by phosphorodiamidate. Any one of the four nucleobases can be attached to the morpholine ring. Because of the unnatural backbone, PMO is more resistant than the ordinary antisense oligonucleotide (AON) to nuclease digestion.
- Revertant fibers:
rarely occurring dystrophin-positive myofibers found in animals that carry a null mutation in the dystrophin gene. The molecular mechanisms underlying the formation of revertant fibers are not completely clear. They might arise from sporadic alternative splicing that eliminates the mutation from the dystrophin transcript and/or a second mutation that corrects the original mutation on the DNA.
- Sarcolemma:
muscle-cell plasma membrane.
- Vivo-morpholino:
a morpholino oligomer that has been covalently linked to an octa-guanidine dendrimer moiety. Conjugation with octa-guanidine increases cell penetration.
- WW domain:
a protein module of approximately 40 amino acids. It contains two preserved tryptophan (W) residues that are spaced 20 to 22 amino acids apart. The WW domain folds into a stable, triple-stranded β-sheet and mediates protein-protein interaction.
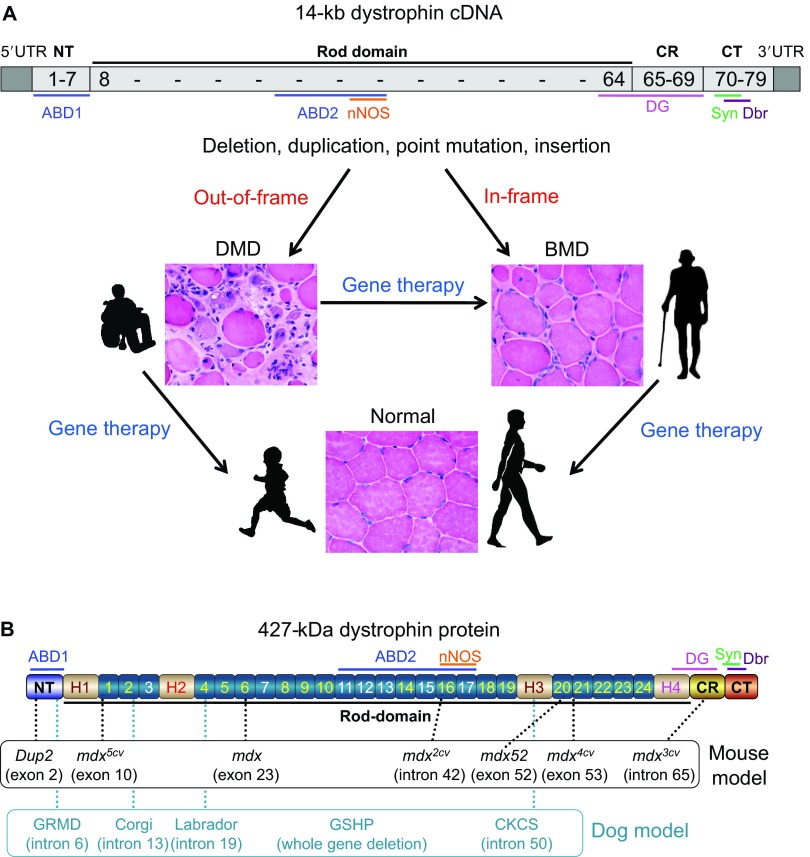
Fig. 2.
DMD gene therapy and dystrophin mutations in animal models. (A) The 14-kb dystrophin cDNA and the principle of DMD gene therapy. The numbers in the cDNA refers to exon number. The DNA sequence position of the main dystrophin domains and of the dystrophin-associated protein-binding sites (see Fig. 1) is also shown. Frame-interrupting (out-of-frame) mutation leads to severe DMD. In-frame mutation results in mild Becker muscular dystrophy (BMD). The primary goal of DMD gene therapy is to ameliorate muscle pathology and to improve muscle function. Gene therapy can convert the DMD phenotype to the benign BMD phenotype. Gene therapy might also prevent or slow down the development of muscle disease if affected individuals are treated early enough. (B) Domain structure of dystrophin and location of the mutations in representative mouse and dog models. ABD, actin-binding domain; CKCS, Cavalier King Charles spaniel; CR, cysteine-rich domain; CT, C-terminal domain; Dbr, dystrobrevin; DG, dystroglycan; GRMD, golden retriever muscular dystrophy; GSHP, German shorthaired pointer; nNOS, neuronal nitric oxide synthase; NT, N-terminal domain; Syn, syntrophin; UTR, untranslated region. See supplementary material Table S1 for a description on each model.
The identification of the disease-causing gene and the molecular basis for the DMD and BMD phenotypes establishes the foundation for DMD gene therapy (Fig. 2A). To mitigate muscle disease, one can either restore the full-length transcript or express a truncated but in-frame dystrophin gene (Duan, 2011; Goyenvalle et al., 2011; Konieczny et al., 2013; Mendell et al., 2012; Verhaart and Aartsma-Rus, 2012). Several gene therapy strategies are currently under development. They include replacing the mutated gene with a functional candidate gene (gene replacement) or repairing the defective gene by targeted correction and exon skipping (gene repair). Currently, adeno-associated virus (AAV)-mediated gene replacement and antisense oligonucleotide (AON)-mediated exon skipping are at the forefront (see Box 1).
In this Review, we discuss existing DMD animal models and their application in preclinical gene therapy research. We also discuss how to use these models to address the current and emerging challenges in DMD gene therapy.
Animal modeling of dystrophin deficiency
Both naturally occurring and laboratory-generated animal models are available to study the pathobiology of dystrophin deficiency and to develop innovative therapies for treating DMD. Currently, there are nearly 60 different animal models for DMD, and the list keeps growing (supplementary material Table S1). Non-mammalian (such as Caenorhabditis elegans, Drosophila melanogaster and zebrafish) and the feline (either hypertrophic or non-hypertrophic) DMD models are rarely used in gene therapy studies (Berger and Currie, 2012; Chamberlain and Benian, 2000; Kunkel et al., 2006; Lloyd and Taylor, 2010; Shelton and Engvall, 2005; Smith, 2011; Winand et al., 1994a), and the newly developed rat and pig DMD models have yet to be used in such research (Hollinger et al., 2014; Klymiuk et al., 2013; Nakamura et al., 2014; Nonneman et al., 2012). As such, we focus this Review on the mouse and dog models (Fig. 2B). We discuss the pros and cons of each system and their use in gene therapy (Table 1).
Table 1.
Comparison of disease severity and gene therapy status in dystrophin-null mice, dogs and humans
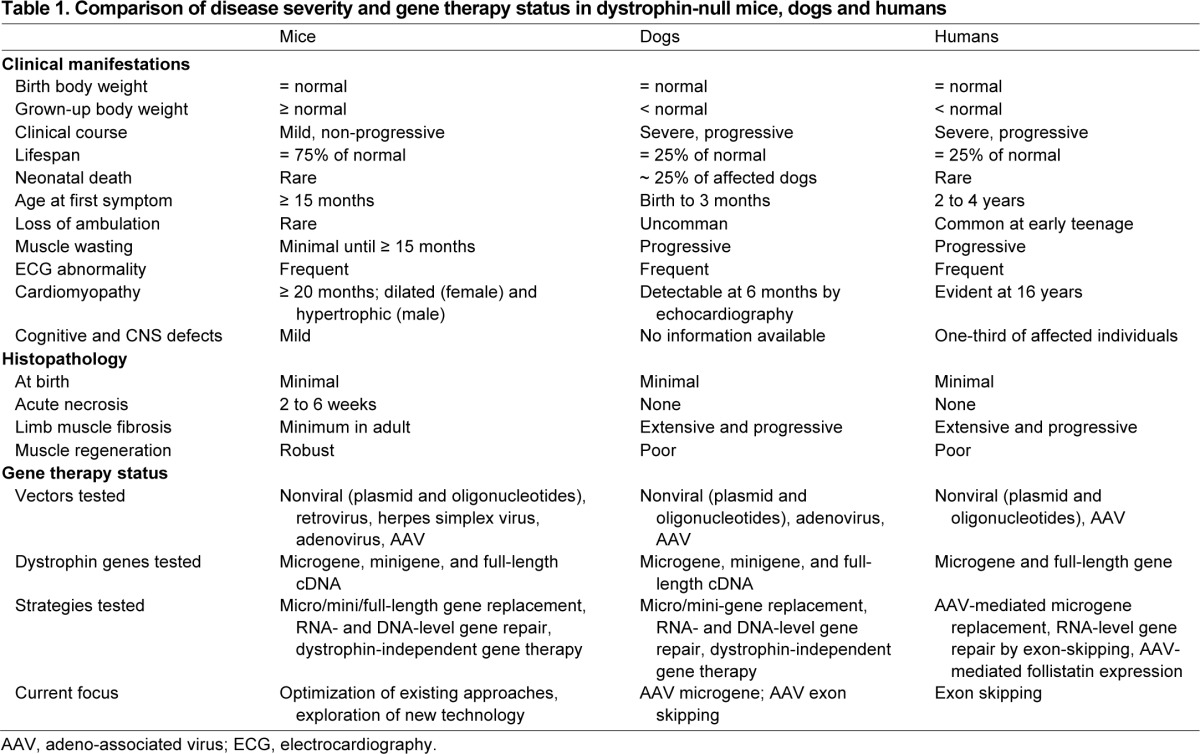
Dystrophin-deficient mice
The most widely used animal model for DMD research is the mdx mouse. It was discovered in the early 1980s in a colony of C57BL/10ScSn mice due to elevated serum creatine kinase (CK) and histological evidence of myopathy (Bulfield et al., 1984). The mutation in the mdx mouse is a nonsense point mutation (C-to-T transition) in exon 23 that aborted full-length dystrophin expression (Fig. 2B) (Sicinski et al., 1989).
Despite being deficient for dystrophin, mdx mice have minimal clinical symptoms and their lifespan is only reduced by ~25% (Fig. 3; Table 1) (Chamberlain et al., 2007; Li et al., 2009). In contrast, the lifespan of individuals with DMD is reduced by ~75% (Box 2; Fig. 3B). mdx skeletal muscle disease has several distinctive phases. In the first 2 weeks, mdx muscle is indistinguishable from that of normal mice. Between 3 to 6 weeks, it undergoes startling necrosis. Subsequently, the majority of skeletal muscle enters a relatively stable phase owing to robust regeneration. mdx limb muscles often become hypertrophic during this phase. The only exception is the diaphragm, which shows progressive deterioration, as is also seen in affected humans (Box 2) (Stedman et al., 1991). Severe dystrophic phenotypes, such as muscle wasting, scoliosis and heart failure, do not occur until mice are 15 months or older (Bostick et al., 2008b; Bostick et al., 2009; Hakim et al., 2011; Lefaucheur et al., 1995; Lynch et al., 2001; Pastoret and Sebille, 1995). A significant portion of aged mdx mice also develops spontaneous sarcoma (Fig. 3A) (Chamberlain et al., 2007; Schmidt et al., 2011; Wang et al., 2014).
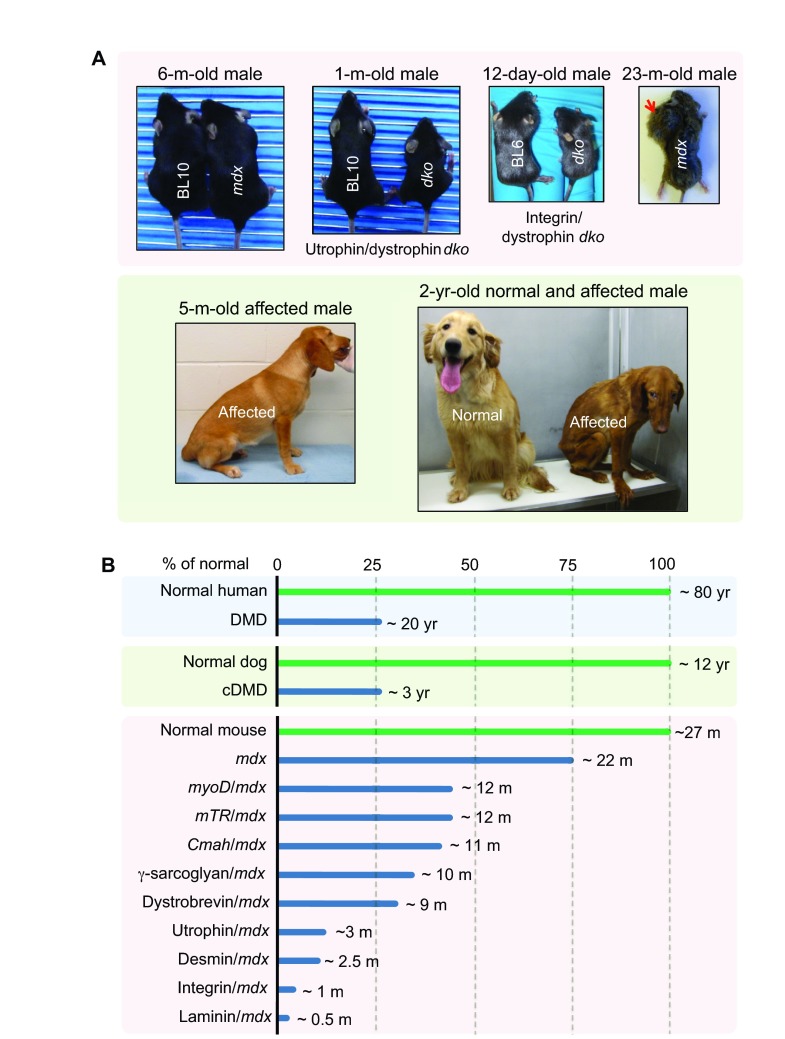
Fig. 3.
Representative animal models for DMD. (A) Representative pictures of selected DMD mouse and dog models. mdx mice do not show symptoms (see 6-month-old photo) until very old (see 23-month-old photo). Aged mdx mice are also prone to rhabdomyosarcoma (a tumor of muscle origin; red arrow). Utrophin/dystrophin and integrin/dystrophin double-knockout (dko) mice are much smaller than the age-matched wild-type (BL10 and BL6) mice. A 5-month-old affected dog shows limb muscle atrophy and is reluctant to exercise. At the age of 2 years old, the affected dog displays severe clinical disease, whereas its normal sibling remains healthy. (B) Lifespan comparison among affected humans, affected dogs and various mouse models.
Box 2. Clinical features of DMD.
Large-scale population studies have outlined the natural disease progression in affected humans (Table 1) (Bushby and Connor, 2011; Henricson et al., 2013; Magri et al., 2011; McDonald et al., 2013a; McDonald et al., 2013b; Spurney et al., 2014). The first clinical sign usually appears around age 3. Between ages 5 and 8, symptoms are often stabilized or even slightly improved (known as the ‘honeymoon’ period) in the absence of any treatment (Bushby and Connor, 2011; McDonald et al., 2013a; McDonald et al., 2010). Rapid clinical deterioration starts around 7 to 8 years of age (Mercuri and Muntoni, 2013). Individuals with DMD lose their ambulation at approximately age 10, develop cardiomyopathy at about age 16 and die around age 20 (life expectancy is reduced by ~75%). With the use of steroids, symptom management and multidisciplinary care (especially nocturnal ventilation), the lifespan of an affected individual is now extended to 30 to 40 years of age. In these individuals, cardiac complications (cardiomyopathy and/or cardiac arrhythmia) have emerged as a major source of morbidity and mortality. Despite the overall trend of disease progression throughout life, affected individuals actually show heterogeneity in clinical manifestations. One retrospective study of 75 drug-naïve affected individuals classified DMD into four distinctive groups (infantile, classical, moderate pure motor and severe pure motor) based on the intellectual and motor outcome (Desguerre et al., 2009).
The mdx mouse has been crossed to several different genetic backgrounds, including the albino, BALB/c, C3H, C57BL/6, DBA/2 and FVB strains, and several immune-deficient strains. Phenotypic variation has been observed in different backgrounds (supplementary material Table S1). For example, albino-mdx mice show more severe neurological dysfunction and higher circulating cytokines (Stenina et al., 2013). BALB/c-mdx and C3H-mdx mice are less susceptible to sarcoma (Krivov et al., 2009; Schmidt et al., 2011; Stenina et al., 2013). Immune-deficient nude-mdx and scid-mdx mice show less fibrosis (Farini et al., 2007; Morrison et al., 2000). The DBA/2-mdx mice are thought to better represent human disease because they display more fibrosis and less regeneration (Fukada et al., 2010). However, according to The Jackson Laboratory, the DBA/2 strain is a challenging breeder and it also carries mutations in a variety of genes that cause hearing loss and eye abnormalities (http://jaxmice.jax.org/strain/000671.html).
In 1989, four chemical variant (cv) mdx strains were published (Chapman et al., 1989). These mice were generated on the C57BL/6 background using the mutagen N-ethyl-N-nitrosourea (ENU) and they are named as mdx2cv, mdx3cv, mdx4cv and mdx5cv. Each of these strains carries a different point mutation (Fig. 2B; supplementary material Table S1) (Cox et al., 1993b; Im et al., 1996). Although the overall clinical presentation of these mice differs very little from that of mdx mice, each line has unique features. Specifically, mdx3cv mice still express ~5% of a near-full-length dystrophin protein (Cox et al., 1993b; Li et al., 2008). mdx5cv mice have a more severe skeletal muscle phenotype (Beastrom et al., 2011). Revertant fibers (see Box 1) are rarely seen in mdx4cv and mdx5cv mice (Danko et al., 1992; Partridge and Lu, 2008). In addition to these four strains, several new ENU-induced dystrophin-null lines have been recently generated (supplementary material Table S1) (Aigner et al., 2009).
In addition to the above-mentioned strains, several other dystrophin-deficient lines (Dup2, MD-null, Dp71-null, mdx52 and mdx βgeo) have been created using various genetic engineering techniques (see supplementary material Table S1 for details).
Immune-deficient mdx strains are dystrophin-null mice that have been crossed to the immune-deficient background. These mice can be used to study cell or gene therapy without the compounding effects of the host immune response. Besides the commonly used nude-mdx and scid-mdx mice (Farini et al., 2007; Morrison et al., 2000), several new lines (NSG-mdx4cv, Rag2−IL2rb−Dmd− and W41 mdx) have recently been developed (supplementary material Table S1) (Arpke et al., 2013; Bencze et al., 2012; Vallese et al., 2013; Walsh et al., 2011). These new lines carry additional mutations that further compromise the immune system.
Mouse models that recapitulate the DMD phenotype
Dystrophin-deficient mice show minimal clinical disease. This could be due to the upregulation of compensatory mechanisms or to a species-specific property of the muscle. Elimination of compensatory mechanisms or humanization of mdx mice results in mouse models that recapitulate the dystrophic phenotype of human with DMD. A major function of dystrophin is to strengthen the sarcolemma by cross-linking the ECM with the cytoskeleton. Two other proteins, utrophin and α7β1-integrin fulfil the same function and their expression is upregulated in mdx mice. The genetic elimination of utrophin and α7-integrin in mdx mice creates utrophin/dystrophin and integrin/dystrophin double-knockout (dko) mice, respectively (Deconinck et al., 1997a; Grady et al., 1997; Guo et al., 2006; Rooney et al., 2006). These dko mice are significantly smaller than their single-gene null parents and show much more severe muscle disease (similar to or even worse than that of humans with DMD) (Fig. 3A). However, they are difficult to generate and care for, and they often die prematurely (compared with the single knockouts; Fig. 3B). Recent studies suggest that utrophin heterozygous mdx mice might represent an intermediate model between the extreme dko mice and mildly affected mdx mice (Rafael-Fortney et al., 2011; van Putten et al., 2012b; Zhou et al., 2008).
Robust skeletal muscle regeneration also explains the slowly progressive phenotype of mdx mice. Two different approaches have been used to reduce muscle regeneration in mdx mice. Megeney et al. eliminated MyoD, a master myogenic regulator, from mdx mice (Megeney et al., 1996). The resulting MyoD/dystrophin double-mutant mouse shows marked myopathy, dilated cardiomyopathy and premature death (Fig. 3B) (Megeney et al., 1996; Megeney et al., 1999). Compared with normal muscle, the length of telomere is reduced in DMD muscle (Decary et al., 2000). Sacco et al. hypothesized that the long telomere length in mouse myogenic stem cells contributes to the high regenerative capacity of mouse muscle (Mourkioti et al., 2013; Sacco et al., 2010). Telomerase RNA (mTR) is required for the maintenance of the telomere length. To reduce telomere length in dystrophin-null mice, Sacco et al. crossed mdx4cv mice with mTR-null mice. These mTR/mdx double-mutant mice show more severe muscle wasting and cardiac defects (Mourkioti et al., 2013; Sacco et al., 2010). Their lifespan is reduced to ~12 months (Fig. 3B).
Other symptomatic dko strains (supplementary material Table S1) have also been generated by mutating genes involved in: (1) cytoskeleton-ECM interactions (such as desmin, laminin and like-glycosyltransferase) (Banks et al., 2014; Gawlik et al., 2014; Martins et al., 2013), (2) the DAGC (such as dystrobrevin and δ-sarcoglycan) (Grady et al., 1999; Li et al., 2009), (3) muscle repair (such as dysferlin) (Grady et al., 1999; Han et al., 2011; Hosur et al., 2012; Li et al., 2009) and (4) inflammation and fibrosis [such as interleukin-10, a disintegrin and metalloproteinase protein (ADAM)-8, and plasminogen activator inhibitor-1) (Ardite et al., 2012; Nishimura et al., 2015; Nitahara-Kasahara et al., 2014).
Humanization is another method of increasing mdx disease severity. The gene encoding cytidine monophosphate sialic acid hydroxylase (Cmah) is naturally inactivated in humans but not in mice (Varki, 2010). Cmah converts cell-surface sialic acid N-acetylneuraminic acid (Neu5Ac) to N-glycolylneuraminic acid (Neu5Gc). Hence, human cells only have Neu5Ac but no Neu5Gc. Genetic elimination of Cmah humanizes the cell-surface glycan profile in mice (Hedlund et al., 2007). Interestingly, Cmah-deficient mdx mice show a more severe phenotype (Fig. 3B). This humanization process renders Cmah/mdx mice a better model because they more closely recapitulate human disease (Chandrasekharan et al., 2010).
In summary, the large collection of symptomatic double-mutant mouse lines has greatly expanded the armory of potential mouse models for preclinical studies. Accelerated disease progression in these dko mice provides an excellent opportunity not only to obtain results from experimental therapies more rapidly but also to confirm whether a therapy can indeed ameliorate clinically relevant manifestations and increase lifespan. Nevertheless, there are also important limitations. For example, most dko mice are difficult to breed and are often not commercially available. Importantly, unlike in humans with DMD, all dko mice carry a mutation not only in the dystrophin gene but also in another gene (although because the gene encoding Cmah is inactivated in humans this is not an issue for Cmah/mdx mice). This is not the case in affected humans. How this additional mutation influences data interpretation remains incompletely understood.
To study DMD pathogenesis and/or to test effectiveness of certain therapies, mdx mice have also been crossed with many other gene-knockout strains that are deficient for additional genes (supplementary material Table S1). It should be noted that these dko mice show milder or similar disease phenotypes as that of mdx mice (see supplementary material Table S1 for details).
Dystrophin-deficient dogs
Two major barriers hinder translational DMD gene therapy research. The first is the host cellular and humoral immune responses to the viral capsid and/or therapeutic proteins expressed from the gene therapy vector. The second is the ability to scale-up vector production and to deliver large-scale-produced vector to patients. Unfortunately, mice are not good models for addressing either issue; however, canine models might bridge this gap. Canine X-linked muscular dystrophy has been described in the literature for over 50 years (Duan, 2011; Funkquist et al., 1980; Innes, 1951; Wentink et al., 1972). Confirmed dystrophin deficiency has been reported in ~20 different dog breeds (see supplementary material Table S1 for details). Generally, the clinical phenotype of canine Duchenne muscular dystrophy (cDMD) is considered more severe than that of mdx (see below for an in-depth discussion) and, as such, cDMD is regarded as a better model of human DMD.
Dystrophin gene mutations have been mapped in nine cDMD breeds (although only four mutations have been published in peer-reviewed research articles). Point mutations have been found in the Cavalier King Charles spaniel muscular dystrophy dogs (CKCS-MD, intron 50), golden retriever muscular dystrophy dogs (GRMD, intron 6) and Rottweiler muscular dystrophy dogs (exon 52) (Sharp et al., 1992; Walmsley et al., 2010; Winand et al., 1994b). Deletion mutations have been found in three breeds, including a small four-nucleotide deletion in exon 65 (Cocker spaniel), an exon 8–29 deletion in the Tibetan terrier, and a whole-gene deletion in the German shorthaired pointer (Kornegay et al., 2012; Schatzberg et al., 1999). Repetitive element insertions are rarely seen in humans with DMD. However, they have been identified in two dog breeds, including the Pembroke Welsh corgi and the Labrador retriever (Fig. 2B; supplementary material Table S1) (Smith et al., 2007; Smith et al., 2011). A recent genome-walking study suggests that the mutation in Japanese Spitz dystrophic dogs is chromosome inversion (Atencia-Fernandez et al., 2015).
Despite abundant documentation of dystrophin deficiency in dogs, most studies are limited to case reports. Experimental colonies have only been established with a few breeds. The GRMD model is the first and the most widely used cDMD model. It was initially identified by deLahunta and colleagues (Cornell University) and then characterized by Drs Cooper and Kornegay at Cornell University and North Carolina State University, USA, respectively (Cooper et al., 1988b; Hoffman and Gorospe, 1991; Kornegay et al., 1988; Valentine et al., 1986). Subsequent molecular, histological and clinical studies validated GRMD dogs as an authentic model for human DMD (Cooper et al., 1990; Cooper et al., 1988a; Cozzi et al., 2001; Kornegay et al., 1988; Lanfossi et al., 1999; McCully et al., 1991; Moise et al., 1991; Nguyen et al., 2002; Sharp et al., 1992; Valentine et al., 1989a; Valentine et al., 1990a; Valentine et al., 1991; Valentine and Cooper, 1991; Valentine et al., 1990b; Valentine et al., 1986; Valentine et al., 1988; Valentine et al., 1989b; Valentine et al., 1989c; Valentine et al., 1989d; Valentine et al., 1992). Currently, GRMD dogs are maintained in several colonies throughout the USA (including the University of Missouri and Texas A&M University, among others), and in France, Brazil and Australia. The GRMD mutation has also been crossed to the Beagle background and a colony is now maintained in Japan; these dogs are called canine X-linked muscular dystrophy in Japan or CXMDJ (Shimatsu et al., 2003; Valentine et al., 1988). Recently, we and others have created hybrid strains that are on mixed genetic backgrounds and/or contain mutations of different breeds (Cotten et al., 2013; Fine et al., 2011; Miyazato et al., 2011; Shin et al., 2013a; Yang et al., 2012). Besides GRMD-based colonies, research colonies have also been generated from affected Pembroke Welsh corgis and Labrador retrievers (Auburn University and University of Missouri), and CKCS-MD (Royal Veterinary College, UK) (Smith et al., 2007; Smith et al., 2011; Walmsley et al., 2010). The CKCS-MD model is especially interesting because the mutation in this breed corresponds to a major deletion hot spot (exons 45–53) in humans with DMD (Aartsma-Rus et al., 2006; Flanigan et al., 2009b; Tuffery-Giraud et al., 2009).
Affected dogs share a remarkably similar clinical course to that of DMD boys (Box 2; Fig. 3; Table 1) (Shimatsu et al., 2005; Smith et al., 2011; Valentine et al., 1988). Limb weakness and exercise intolerance start around 2 to 3 months of age (analogous to ~3 years of age in humans) (Valentine et al., 1988). Muscle atrophy, joint contracture, hypersalivation, dysphagia, abnormal gait and signs of cardiac involvement become apparent at ~6 months (Fig. 3A; Table 1) (Fan et al., 2014; Fine et al., 2011; Valentine et al., 1988; Valentine et al., 1989c; Yugeta et al., 2006). At around 6 to 10 months, disease progression enters a relatively stable ‘honeymoon’ period (Fan et al., 2014; Shimatsu et al., 2005; Valentine et al., 1988). Death often occurs around 3 years of age (a ~75% reduction of the lifespan) (Fig. 3B). Humans with DMD show heterogeneity in their clinical manifestation (Box 2) (Ashwath et al., 2014; Desguerre et al., 2009; Sifringer et al., 2004). cDMD dogs also show variation in their symptoms. In extreme cases, affected subjects are essentially asymptomatic despite the lack of dystrophin in their muscles (Ambrósio et al., 2008; Dubowitz, 2006; Hattori et al., 1999; Wakefield et al., 2009; Zatz et al., 2014; Zucconi et al., 2010).
Besides clinical resemblance, cDMD dogs also have histological lesions similar to affected humans. For example, limb muscle fibrosis is a salient disease feature in humans with DMD and in affected dogs but not in mdx mice (C.H.H. and D.D., unpublished observations). Vigorous regeneration in mouse muscle contributes substantially to the mild phenotype of mdx mice. This regeneration is evident by high proportions of centrally nucleated myofibers in mdx mice. Similar to humans with DMD, cDMD dogs have much fewer myofibers containing central nucleation (Cozzi et al., 2001; Shin et al., 2013b; Smith et al., 2011; Yang et al., 2012).
It should be noted that the clinical presentation of cDMD dogs is not identical to that of humans with DMD (Table 1). About 20–30% of cDMD puppies die within 2 weeks of birth likely due to diaphragm failure (Ambrósio et al., 2008; Nakamura et al., 2013; Shimatsu et al., 2005; Valentine et al., 1988). However, this neonatal death is not seen in newborn DMD boys. Growth retardation is another canine-specific symptom (West et al., 2013). Body weight at birth is similar between normal and affected cDMD puppies (Smith et al., 2011). However, at 1 and 6 months of age, the body weight of affected puppies reaches only ~80% and ~60% of normal, respectively (C.H.H. and D.D., unpublished observation from n>50 dogs). Finally, untreated humans with DMD usually lose ambulation during the early teenage years. However, complete loss of ambulation is not a clinical feature in young cDMD dogs (Duan et al., 2015; Valentine et al., 1988).
Overall, cDMD dogs share many features with that of humans with DMD. These features make cDMD dogs an excellent model to conduct preclinical gene therapy studies (Duan, 2011; Duan, 2015). Nevertheless, mdx mice remain the most commonly used model in DMD gene therapy studies owing to the low cost and easy access. Any discussion of DMD models in gene therapy that lacked mention of mdx mice would not be complete.
Establishing the foundations of gene therapy: transgenic mdx mice
The successful development of a gene therapy requires research to identify the therapeutic candidate gene, the level of expression needed to produce a therapeutic effect and the tissue that should be targeted (Chamberlain, 2002; Duan, 2006). As we discuss in this section, for DMD gene therapy research, these fundamental questions have been addressed using transgenic mdx mice.
Therapeutic potential of truncated dystrophin genes
Naturally occurring small dystrophin isoforms
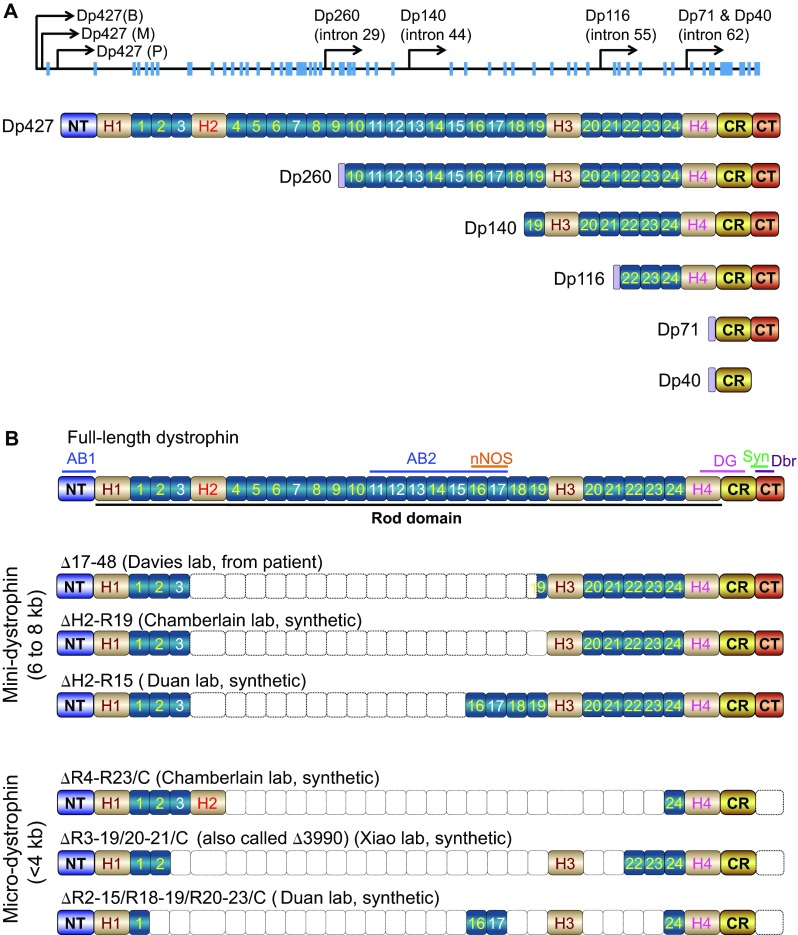
The enormous size of the full-length dystrophin gene poses one of the biggest challenges for gene therapy because it exceeds the packaging limit of most viral vectors. For this reason, identifying a smaller but functional gene has been an ongoing goal in the development of a dystrophin gene-replacement therapy. Early studies showed that, besides the 427-kDa full-length protein, the dystrophin gene also encodes a number of smaller N-terminal-truncated non-muscle isoforms (Ahn and Kunkel, 1993; Blake et al., 2002; Ervasti, 2007). These include Dp260, Dp140, Dp116, Dp71 and Dp40 (numbers refer to the molecular weight) (Fig. 4A). With the exception of Dp40 (Fujimoto et al., 2014), they all contain the CT and CR domains but are missing the NT actin-binding domain. To determine whether these miniature isoforms are therapeutically relevant, the Chamberlain lab, as well as others, made transgenic mdx mice for Dp260, Dp116 and Dp71 (see supplementary material Table S1 for details) (Cox et al., 1994; Gaedigk et al., 2006; Greenberg et al., 1994; Judge et al., 2011; Judge et al., 2006; Warner et al., 2002).
Fig. 4.
Structure of abbreviated dystrophins. (A) Naturally occurring dystrophin isoforms. In the topmost schematic, blue boxes denote exons. The full-length dystrophin (Dp427) transcripts have three isoforms, including brain Dp427 (B), muscle Dp427 (M) and Purkinje cell Dp427 (P). Smaller dystrophin isoforms are produced from promoters located in different introns (intron positions are marked for each isoform). Dp260 is expressed in the retina, Dp140 in the brain and kidney, Dp116 in Schwann cells, and Dp71 and Dp40 are expressed from the same promoter except Dp71 is ubiquitously expressed whereas Dp40 only exists in the brain. Except for Dp140, all other dystrophin isoforms have unique N-terminal sequences not present in the full-length protein. (B) Structure of representative mini- and micro-dystrophins. The full-length dystrophin protein is shown uppermost, and features the same terminology as that used in Fig. 1.
Dp71 is the most abundant non-muscle dystrophin isoform. It contains only the CR and CT domains (Fig. 4A). Because the CT domain carries the binding sites for syntrophin and dystrobrevin, it was initially thought that Dp71 might restore some of the signaling functions of dystrophin. Surprisingly, however, transgenic overexpression of Dp71 results in more severe muscle disease in mdx mice (Cox et al., 1994; Greenberg et al., 1994) and myopathy in normal mice (Leibovitz et al., 2002). The WW domain of hinge 4 (H4; see Fig. 1A and Box 1), which is partially truncated in Dp71, participates in dystrophin-dystroglycan interaction (Huang et al., 2000). To fully appreciate the contribution of dystroglycan binding and dystrophin signaling in DMD pathogenesis, Judge et al. generated Dp116 transgenic mdx mice. Dp116 is a Schwann-cell-specific dystrophin isoform. It contains the last three spectrin-like repeats, H4, and the CR and CT domains (Fig. 4A). Dp116 expression does not improve muscle disease in mdx4cv mice nor does it reduce the histopathology in utrophin/dystrophin dko mice (Judge et al., 2011; Judge et al., 2006). Interestingly, the lifespan of utrophin/dystrophin dko mice was significantly increased by transgenic Dp116 expression (Judge et al., 2011).
Two independent strains of Dp260 transgenic mice have been studied (Gaedigk et al., 2006; Warner et al., 2002). Although Dp260 (also known as the retinal isoform of dystrophin) does not carry the NT domain, it contains the ABD2 domain (Fig. 2B; Fig. 4A). Its overexpression significantly reduces the dystrophic phenotype of mdx and utrophin/dystrophin dko mice but does not completely prevent muscle degeneration, inflammation and fibrosis (Gaedigk et al., 2006; Warner et al., 2002). In summary, transgenic analyses of naturally occurring dystrophin isoforms suggest that the N-terminal domain is required for maximum muscle protection and that a complete dystroglycan-binding domain (including the WW domain in H4 and the CR domain) is important.
Synthetic mini- and micro-dystrophin genes
An alternative approach to developing a smaller but functional dystrophin gene is through genetic engineering. To achieve this, one needs to know which regions of the dystrophin gene are dispensable for its normal functions. The first clue about this came from a mildly affected individual, who was ambulant at age 61 (England et al., 1990). This person carries a large in-frame deletion (Δ17–48) in the rod domain, which eliminates 46% of the coding sequence. Transgenic expression of the Δ17–48 minigene in mdx mice significantly reduced skeletal muscle pathology and increased specific muscle force (Phelps et al., 1995; Wells et al., 1995). Subsequent optimization by removing residue repeat 19 in the Δ17–48 minigene resulted in a more protective ΔH2-R19 minigene (Fig. 4B) (Harper et al., 2002).
An important function of dystrophin is to recruit nNOS to the sarcolemma. Failure to do so results in functional ischemia and aggravates muscle disease (Thomas, 2013). We recently identified the dystrophin nNOS-binding site at R16/17 of the rod domain (Fig. 1; Fig. 2B) (Lai et al., 2009; Lai et al., 2013). Inclusion of this binding site in synthetic dystrophins (Fig. 4B) significantly enhances muscle protection and exercise capacity (Lai et al., 2009; Zhang et al., 2013).
The mini-dystrophin gene is ~6 to 8 kb. One drawback is that it cannot fit into the 5-kb packaging limit of AAV, the most efficient muscle gene-transfer vector. A pivotal transgenic study from the Chamberlain lab opened the door to further reducing the size of the dystrophin gene by deleting the entire CT domain (Crawford et al., 2000). Specifically, Chamberlain and colleagues showed that a C-terminal-truncated dystrophin gene successfully restored syntrophin and dystrobrevin to the sarcolemma and completely protected young adult mdx mice (Crawford et al., 2000). Consistent with this transgenic study, a subset of affected individuals who have partial or complete CT-domain deletion also show mild disease (Aartsma-Rus et al., 2006; McCabe et al., 1989; Patria et al., 1996; Tuffery-Giraud et al., 2009). Collectively, the existing data suggest that the majority of the rod domain (except for R16/17) and the entire C-terminal domain are not essential for dystrophin function. Based on this understanding, several versions of highly abbreviated synthetic micro-dystrophin genes (<4 kb) have been engineered (Fig. 4B) (Harper et al., 2002; Lai et al., 2009; Wang et al., 2000). These microgenes greatly prevent muscle damage in transgenic mdx mice (Hakim and Duan, 2013; Harper et al., 2002; Li et al., 2011).
Level of expression
Two essential questions in DMD gene therapy are: (1) how much dystrophin is too much, and (2) how much dystrophin is enough to ameliorate disease? In transgenic mdx mice, Chamberlain and colleagues found that 50-fold overexpression of full-length dystrophin was not toxic to skeletal muscle, thus providing a high safety margin (Cox et al., 1993a). Studies in transgenic mdx mice have also revealed the threshold for histological and physiological protection (Phelps et al., 1995; Wells et al., 1995). Dystrophin expression at ~20% of the wild-type level significantly mitigated muscle pathology and enhanced muscle contractility (Phelps et al., 1995; Wells et al., 1995). mdx3cv mice express ~5% of a near-full-length dystrophin protein and mdx-XistΔhs mice express variable low levels of dystrophin (supplementary material Table S1) (Cox et al., 1993b; van Putten et al., 2012a). Recent studies in mdx3cv and mdx-XistΔhs mice suggest that dystrophin expression at a 5% level still preserves some muscle function in mdx mice and extends the lifespan of utrophin/dystrophin dko mice (Li et al., 2008; Li et al., 2010; van Putten et al., 2012a; van Putten et al., 2013). A clear correlation between the dystrophin level and clinical manifestation has also been noticed in humans with DMD (Nicholson et al., 1993a; Nicholson et al., 1993b). Affected individuals with ≥20% wild-type dystrophin protein expression are often ambulant beyond age 20 (Bulman et al., 1991; Byers et al., 1992; Hoffman et al., 1989). An affected individual with 30% dystrophin protein expression, measured through western blot, was even free of skeletal muscle disease at age 23 (Neri et al., 2007). Where gene therapy is concerned, there is no doubt that restoring ≥20% protein expression will be needed to achieve clinically meaningful improvement. Nonetheless, mouse data suggest that even a low level of expression (~5%) might still be beneficial.
Target tissue: skeletal muscle versus heart
Humans with DMD suffer from both skeletal muscle disease and cardiomyopathy. It thus seems obvious that both skeletal and heart muscle should be treated. However, many existing gene therapy approaches (such as some AONs used for exon skipping and AAV serotype-9-mediated systemic gene transfer in newborn dogs) cannot efficiently reach the heart (Alter et al., 2006; Hakim et al., 2014; Yokota et al., 2009; Yue et al., 2008). Will skeletal-muscle-centered therapy benefit individuals with DMD? An early study in young (4- to 5-month-old) transgenic mdx4cv mice suggests that targeted repair of skeletal muscle accelerates heart disease (Townsend et al., 2008). However, the interpretation of the heart function data in this study has been questioned (Wasala et al., 2013). Using a different approach, Crisp et al. reached a completely opposite conclusion in adult (6- to 9-month-old) mdx mice and neonatal (10-day-old) utrophin/dystrophin dko mice (Crisp et al., 2011). They concluded that skeletal muscle rescue can prevent cardiomyopathy (Crisp et al., 2011). Because mdx mice do not develop clinically evident cardiomyopathy until they are 21-months old (Bostick et al., 2008b; Bostick et al., 2009), we recently re-evaluated this issue in a similar transgenic strain used by Townsend et al. (Townsend et al., 2008; Wasala et al., 2013). Surprisingly, skeletal-muscle-rescued mdx mice showed the identical heart disease as that of non-transgenic mdx mice at the age of 23 months (Wasala et al., 2013). In summary, skeletal muscle rescue might neither aggravate nor completely alleviate cardiomyopathy. As such, we believe that gene therapy should treat both skeletal and cardiac muscles.
Gene replacement therapy
A straightforward approach to treating DMD is to add back a functional dystrophin gene. This can be achieved using a variety of gene-transfer vectors, including nonviral, retroviral, adenoviral, herpes simplex viral and AAV vectors. The candidate gene can be the full-length cDNA or an abbreviated synthetic gene.
Replacement with the full-length dystrophin coding sequence
Several strategies have been explored to deliver the 14-kb, full-length dystrophin cDNA. Direct plasmid injection was tested in mdx mice soon after the discovery of the dystrophin gene (Acsadi et al., 1991). A number of different nonviral delivery approaches have since been evaluated in mdx mice. These include the use of liposomes, microspheres, electroporation and hydrodynamic intravascular delivery (see Box 1). Direct plasmid injection has also been tested in the GRMD model and in a Phase 1 human trial (Braun, 2004; Duan, 2008). However, poor transduction and transient expression have limited further development of these plasmid-based therapeutic strategies.
The gutted adenoviral vector does not carry any viral genes and can package a 35-kb genome. It has been used to express the full-length dystrophin cDNA (Haecker et al., 1996; Kochanek et al., 1996; Kumar-Singh and Chamberlain, 1996). Tests conducted in mdx and utrophin/dystrophin dko mice have yielded promising results (Clemens et al., 1996; DelloRusso et al., 2002; Ishizaki et al., 2011; Kawano et al., 2008). The current challenges are the host immune response to the adenoviral capsid and the contaminating wild-type adenovirus. Herpes simplex virus also has an extremely large capacity (~150 kb) and has been used to package the full-length dystrophin cDNA (Akkaraju et al., 1999; Liu et al., 2006). However, there have been very few animal studies performed with it due to the toxicity of the virus.
Recently, tri-AAV vectors were used to deliver the full-length dystrophin cDNA (see Box 1) (Koo et al., 2014; Lostal et al., 2014). In this system, the full-length cDNA expression cassette is split into three fragments and separately packaged in an AAV vector. Coinfection with all three AAV vectors results in the production of a full-length dystrophin protein. This approach has been tested in mdx and mdx4cv mice by direct muscle injection. The therapeutic benefits of this system await substantial improvement in transduction efficiency.
Replacement with small synthetic dystrophin genes
The 6- to 8-kb minigenes discussed earlier in the Review have been tested with plasmid, retrovirus, adenovirus and AAV. Retroviral delivery is very inefficient because the virus does not transduce post-mitotic muscle cells (Dunckley et al., 1993). The first-generation E1-deleted adenovirus was used to deliver the Δ17–48 minigene to mdx mice and GRMD dogs (Howell et al., 1998; Ragot et al., 1993). Although this vector is more efficient than a retroviral vector, it induces a strong cellular immune response in mdx mice (Howell et al., 1998; Ragot et al., 1993). The Chamberlain and Duan labs have tested dual-AAV-vector-mediated mini-dystrophin therapy in mdx mice using local and systemic gene transfer (see Box 1) (Ghosh et al., 2008; Lai et al., 2005; Odom et al., 2011; Zhang and Duan, 2012; Zhang et al., 2013). In the dual AAV vector system, mini-dystrophin expression is achieved with a pair of AAV vectors, each carrying half of the minigene. These studies have shown a significant improvement of histology and function in treated mdx mice. Noticeably, the use of the R16/17-containing mini-dystrophin dual AAV vectors has successfully restored sarcolemmal nNOS expression and ameliorated functional ischemia (Zhang and Duan, 2012; Zhang et al., 2013).
AAV-mediated, micro-dystrophin gene therapy is currently at the cutting edge of DMD gene-replacement therapy. Local injection studies performed in the Chamberlain, Dickson, Duan, Takeda and Xiao laboratories suggest that a rationally designed dystrophin microgene can protect limb muscles and the heart in mdx mice despite the absence of ~70% of the coding sequence (Harper et al., 2002; Wang et al., 2000; Yoshimura et al., 2004; Yue et al., 2003). Using the newly developed AAV serotype-6 and -8 vectors (Gao et al., 2002; Rutledge et al., 1998), the Chamberlain and Xiao labs achieved widespread whole-body muscle gene transfer in the rodent models of muscular dystrophies (Gregorevic et al., 2004; Wang et al., 2005). Later, it was found that AAV serotype-9 can also provide efficient systemic muscle delivery (Bostick et al., 2007; Pacak et al., 2006). More recent studies suggest that AAV-8 and AAV-9 can also produce robust body-wide muscle gene transfer in neonatal dogs (Hakim et al., 2014; Kornegay et al., 2010; Pan et al., 2013; Yue et al., 2008).
The first systemic gene therapy test was performed in mdx mice by Gregorevic et al. (Gregorevic et al., 2004) and subsequently in utrophin/dystrophin and myoD/dystrophin dko mice (Gregorevic et al., 2006; Lai et al., 2009). In these studies, micro-dystrophin gene therapy significantly ameliorated the histological and physiological signs of muscular dystrophy, reduced CK levels and extended lifespan. To further improve therapeutic efficacy, several labs made additional changes to the existing micro-dystrophin constructs. Dickson and colleagues found that codon-optimization and inclusion of the syntrophin/dystrobrevin-binding site resulted in better rescue (Foster et al., 2008; Koo et al., 2011a). The Chamberlain lab found that the rigid poly-proline site in hinge 2 compromised micro-dystrophin function (Banks et al., 2010). Our studies have suggested that R16/17 should be incorporated in the microgene design to normalize nNOS expression (Harper, 2013; Lai et al., 2009; Lai et al., 2013; Li et al., 2011; Shin et al., 2013b).
In an effort to translate AAV microgene therapy to large mammals, several groups have extended research into cDMD models (Koo et al., 2011b; Kornegay et al., 2010; Shin et al., 2012a; Shin et al., 2012b; Wang et al., 2007). These studies uncovered two important issues that were not encountered during mouse studies. First, intramuscular injection results in a strong cellular immune response (Ohshima et al., 2009; Wang et al., 2007; Yuasa et al., 2007; Yue et al., 2008). As a result, transient immune suppression is necessary for persistent transduction in dog muscle (Shin et al., 2012b; Wang et al., 2007). Second, a microgene that reduces muscle disease in mice might not work effectively in dogs (Kornegay et al., 2010; Sampaolesi et al., 2006). Specifically, the ΔR4-23/C dystrophin microgene did not improve muscle histology when tested in a cell therapy study (Sampaolesi et al., 2006). Newborn GRMD dogs developed more severe disease after treatment with the ΔR3-19/20–21/C (also called Δ3990) microgene (Kornegay et al., 2010). Currently, convincing physiological improvement has only been demonstrated in the ΔR2-15/R18-19/R20-23/C microgene-treated dogs (Shin et al., 2013b).
Gene repair therapy
Therapeutic approaches that aim to repair or correct a DMD gene mutation have been conducted at both the RNA and DNA level using oligonucleotides or engineered endonucleases (Aartsma-Rus, 2012; Bertoni, 2014). Although AON-mediated exon skipping has already reached Phase 3 human trials, endonuclease-based gene repair has just begun to emerge (Koo and Wood, 2013; Lu et al., 2011).
Repairing the dystrophin transcript
Therapeutic RNA targeting using exon skipping is by far the most advanced DMD gene therapy technology developed to date. In exon skipping, AONs are used to modulate the splicing of the RNA transcript such that one or several exons are excluded. As a result, an out-of-frame mRNA is converted into an in-frame transcript or an exon that contains a premature stop codon is removed from the transcript (Spitali and Aartsma-Rus, 2012). An internally deleted but partially functional dystrophin produced from exon skipping is expected to convert severe DMD to the milder Becker phenotype. This approach represents an excellent example of how a rationally designed strategy can rapidly move from bench to bedside.
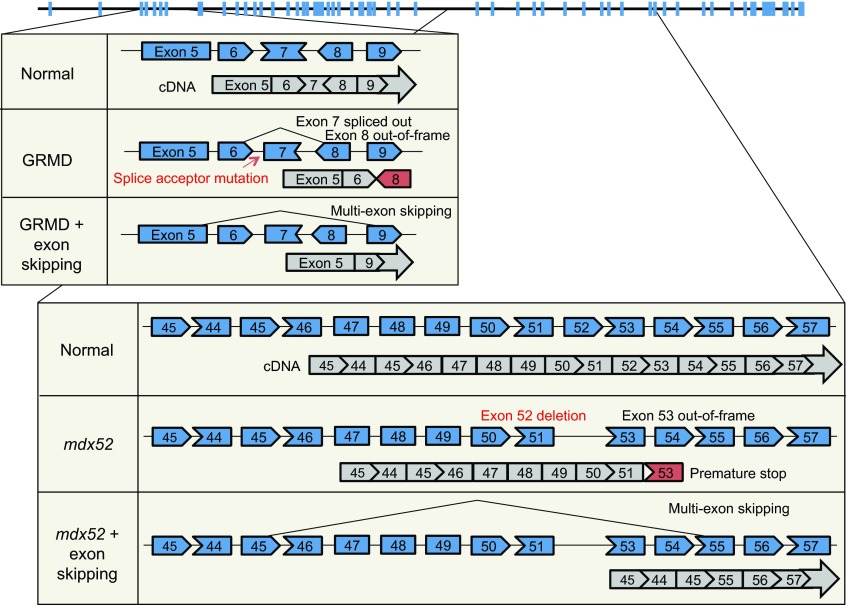
The initial proof-of-principle study for exon skipping was conducted in cultured mdx mouse muscle cells (Dunckley et al., 1998). Subsequent in vivo tests in mdx mice showed that this approach produced a highly efficient restoration of dystrophin expression and improved muscle function, following local or systemic injection (Alter et al., 2006; Gebski et al., 2003; Lu et al., 2003; Lu et al., 2005; Mann et al., 2001). Similarly, exon skipping (Fig. 5) has been achieved in cultured cDMD muscle cells and in CXMDJ dogs by local and systemic delivery (McClorey et al., 2006; Walmsley et al., 2010; Yokota et al., 2009). Several clinical trials have been initiated based on the results of animal studies (Koo and Wood, 2013; Opar, 2012). Data from the Phase 1 and 2 trials are highly promising (Cirak et al., 2011; Goemans et al., 2011; Kinali et al., 2009; Mendell et al., 2013; van Deutekom et al., 2007). However, the expected efficacy remains to be confirmed in a Phase 3 study (Hoffman and McNally, 2014; Wood, 2013).
Fig. 5.
Multiple-exon skipping. The uppermost diagram is the intron/exon structure of the dystrophin gene. Blue boxes denote exons. The top box shows the golden retriever muscular dystrophy dog (GRMD) mutation and exon skipping for GRMD. A point mutation in intron 6 alters normal splicing, and the resulting transcript (gray) is out-of-frame. Skipping exons 6, 7 and 8 yields an in-frame transcript. The bottom box shows the mdx52 mutation and exon skipping in mdx52. Deletion of exon 52 disrupts the reading frame and results in a premature stop. Removing exons 45 to 55 from the mutated transcript generates an in-frame transcript.
Early exon-skipping studies used AONs based on 2′-O-methylated phosphorothioate (2OMe-PS) or phosphorodiamidate morpholino oligomers (PMOs) (Box 1). An important limitation of these AONs is that they cannot reach the heart. To overcome this hurdle, a variety of conjugated PMOs have been developed (Aoki et al., 2012; Jearawiriyapaisarn et al., 2008; Wu et al., 2009; Wu et al., 2008; Yin et al., 2008; Yin et al., 2011). In these PMOs, oligonucleotides are covalently linked to a cell-penetrating peptide or an octa-guanidine dendrimer, which can enhance cell penetration (the octa-guanidine-modified PMO is called vivo-morpholino; see Box 1). Systemic delivery of conjugated AONs in mdx mice produced robust exon skipping in the heart and the restoration of cardiac function (Wu et al., 2008; Wu et al., 2011). Another drawback of AON therapy is the rapid turnover of the therapeutic oligonucleotides. To solve this problem, investigators have begun to use the AAV vector to achieve persistent AON delivery in vivo in mdx mice (Denti et al., 2006; Goyenvalle et al., 2004). Recently, AAV-based exon skipping has been shown to significantly improve the dystrophic phenotype in utrophin/dystrophin dko mice and in GRMD dogs (Barbash et al., 2013; Bish et al., 2012; Goyenvalle et al., 2012; Le Guiner et al., 2014; Vulin et al., 2012).
mdx mice and GRMD dogs carry point mutations in the dystrophin gene. However, ~ 60% of DMD is due to deletions in exons 45–53 or duplications in exon 2 (Flanigan et al., 2009b). mdx52 and dup2 mice carry mutations that resemble the deletions and duplications in affected humans, respectively. Hence, they are excellent models for preclinical testing. Aoki et al. delivered a cocktail of ten vivo-morpholino AONs to mdx52 mice and achieved efficient multiple-exon skipping (exons 45–55) (Fig. 5) (Aoki et al., 2012). The resulting Δ45–55 dystrophin transcript is highly protective and significantly improves muscle strength and histology without causing any toxicity (Aoki et al., 2012). The duplication of exon 2 is a more challenging error to correct because a complete skipping of exon 2 leads to an out-of-frame transcript. Wein et al. recently tested exon 2 skipping in the dup2 model using an AAV-based exon-skipping system (Wein et al., 2014). The treatment generated a Δ2 transcript with a premature stop codon in exon 3. Surprisingly, however, the dystrophic phenotype was significantly ameliorated. Further investigation suggests that the removal of exon 2 activates a downstream internal ribosome entry site in exon 5. Translation from this site yields a highly functional protein (Wein et al., 2014). The results of the Aoki et al. and Wein et al. studies are especially appealing because humans who carry similar transcripts are often asymptomatic (Ferreiro et al., 2009; Flanigan et al., 2009a; Nakamura et al., 2008). Therapies based on the same principle might therefore yield dramatic clinical improvement in boys with DMD.
Repair at the DNA level
Compared to exon skipping, approaches to correct the mutated dystrophin gene are less developed (Bertoni, 2014). Initial DNA-repair strategies used oligonucleotides that are homologous to the target DNA. This approach has resulted in gene correction in mdx and mdx5cv mice, and in one GRMD dog, but the efficiency was too low for clinical application (Bartlett et al., 2000; Kayali et al., 2010; Rando et al., 2000). Nuclease-based gene editing is a powerful technology to correct DNA defects (Box 1). Briefly, a nuclease is used as a pair of molecular scissors to cut DNA at the target site. When a double-strand DNA break is repaired by cellular mechanisms, insertions and/or deletions are introduced at the break point. Some of these modifications yield the wild-type sequence, hence gene correction. Four families of engineered nucleases have been recently developed, including meganuclease, zinc-finger nuclease, TALEN (transcription activator-like effector nuclease) and the CRISPR/Cas (clustered regularly interspaced short palindromic repeat/CRISPR-associated nuclease/helicase) system. These have all been explored for use in DMD therapy; however, the majority of the studies are currently limited to cultured cells (Chapdelaine et al., 2010; Long et al., 2014; Ousterout et al., 2014; Ousterout et al., 2013; Rousseau et al., 2011). Future studies are needed to validate these highly promising gene-editing strategies in animal models of DMD.
Gene therapy for cardiomyopathy and neuronal defects
Cardiomyopathy and neuronal defects are two other prominent clinical features of DMD. Gene therapy for the heart and central nervous system (CNS) requires special consideration (Anderson et al., 2002; Duan, 2006; Lai and Duan, 2012; Nardes et al., 2012; Ricotti et al., 2011; Shin et al., 2010; Snow et al., 2013) because these organs differ from skeletal muscle in their anatomy and physiology. Importantly, dystrophin deficiency produces a unique disease profile in the heart and CNS.
Duchenne cardiomyopathy gene therapy
The characteristic cardiac manifestation of DMD is dilated cardiomyopathy (Duan, 2006; Finsterer and Cripe, 2014). Heart damage is also a prominent phenotype in various strains of dko mice, including the utrophin/dystrophin dko, α7-integrin/dystrophin dko, myoD/dystrophin dko and mTR/dystrophin dko mice (Grady et al., 1997; Guo et al., 2006; Megeney et al., 1999; Mourkioti et al., 2013) (supplementary material Table S1). However, aged female mdx mice are by far the best mouse models for studying Duchenne dilated cardiomyopathy because they are genetically and phenotypically identical to affected humans (Bostick et al., 2010; Bostick et al., 2008b).
Most Duchenne cardiomyopathy gene therapy studies have been conducted in the mdx model. Using dystrophin heterozygous mice, Duan and colleagues demonstrated that dystrophin expression in 50% of cardiomyocytes was sufficient to mitigate heart injury in mdx mice (Bostick et al., 2008b; Yue et al., 2004). The first cardiac gene therapy study was performed in neonatal mdx mice using an AAV-5 ΔR4-23/ΔC microgene vector in our laboratory (Fig. 4B). This micro-dystrophin gene therapy restores the DAGC and increases the strength of the cardiomyocyte membrane (Yue et al., 2003). Subsequent studies using the same microgene normalized the electrocardiography (ECG) defects and improved cardiac hemodynamics in young and adult mdx mice (Bostick et al., 2008a; Schinkel et al., 2012; Shin et al., 2011b; Townsend et al., 2007). To further explore the therapeutic potential, Bostick et al. treated aged female mdx mice with an AAV-9 ΔR4-23/ΔC microgene vector (Bostick et al., 2011; Bostick et al., 2012). They achieved efficient whole-heart gene transfer despite the presence of extensive myocardial fibrosis. In near-terminal-age mice (16- to 20 months old), fibrosis was significantly reduced and hemodynamic performance significantly enhanced (Bostick et al., 2011). However, such improvements were not observed in terminal-age mice (>21 months old) (Bostick et al., 2012). The cardiac protection of the mini-dystrophin gene has only been examined using the 6-kb ΔH2-R19 minigene in transgenic mdx mice (Fig. 4B) (Bostick et al., 2009). This minigene completely normalizes skeletal muscle force in transgenic mdx mice (Harper et al., 2002). However, it does not lead to a full recovery of heart function (Bostick et al., 2009).
Exon skipping has also been explored for treating mdx heart disease. The original 2OMe-PS and PMO AONs cannot reach the heart (Alter et al., 2006). However, conjugated PMOs developed in the Lu and Wood labs have significantly increased cardiac exon skipping and heart contractility in mdx mice (Wu et al., 2009; Wu et al., 2008; Wu et al., 2011; Yin et al., 2008; Yin et al., 2011). Recently, two groups tested AAV-based exon skipping in GRMD dogs. Sweeney and colleagues delivered the vector to the heart via fluoroscopy-guided trans-endocardial injection (Bish et al., 2012). This treatment restored dystrophin expression in the heart, reduced fibrosis and improved left ventricular function (Bish et al., 2012). Using X-ray-fused magnetic resonance, Barbash et al. have further improved the transendocardial gene-delivery method and achieved dystrophin expression in the GRMD heart (Barbash et al., 2013).
Correcting neuronal defects with gene therapy
About one-third of individuals with DMD display cognitive deficiency and other CNS symptoms (Anderson et al., 2002; D’Angelo and Bresolin, 2006; Nardes et al., 2012; Ricotti et al., 2011; Snow et al., 2013). Although all dystrophin isoforms have been detected in the nervous system (Lidov, 1996; Tozawa et al., 2012), only Dp140 and Dp71 have been implicated in neuronal abnormalities in humans with DMD (Bardoni et al., 2000; Bardoni et al., 1999; Daoud et al., 2009a; Daoud et al., 2009b; Felisari et al., 2000; Moizard et al., 1998; Moizard et al., 2000; Pane et al., 2012; Taylor et al., 2010). Among all DMD models, only mdx3cv and mdx βgeo mice do not express Dp140 and Dp70. Surprisingly, neurocognitive behaviors of mdx3cv mice are only slightly different from those of mdx mice (Muntoni et al., 1991; Vaillend et al., 1998; Vaillend et al., 2004; Vaillend et al., 1995; Vaillend and Ungerer, 1999; Yamamoto et al., 2010). Dp71-specific knockout mice have also been generated and, interestingly, they show more severe learning impairment than mdx mice (Daoud et al., 2009b; Sarig et al., 1999). It is very likely that none of the existing mouse models can fully recapitulate the neurocognitive impairments of humans with DMD (D’Angelo and Bresolin, 2006). Nevertheless, most investigators have used mdx mice to dissect the molecular and cellular consequences of dystrophin deficiency in the brain. Collectively, these studies have revealed abnormalities in the hippocampus and in several other regions of the brain (Ghedini et al., 2012; Graciotti et al., 2008; Miranda et al., 2011; Miranda et al., 2009; Parames et al., 2014; Vaillend et al., 2004; Vaillend et al., 1999). So far, only exon skipping has been explored to treat CNS defects. Vaillend and colleagues injected an AAV exon-skipping vector to the mdx brain and found improvement of hippocampus function (Dallérac et al., 2011; Vaillend et al., 2010). Sekiguchi et al. ameliorated the abnormal freezing response (see Box 1) seen in mdx mice by injecting PMO AON to the ventricles of the brain (Sekiguchi et al., 2009). Utrophin has been considered as a highly promising replacement for dystrophin (see next section for details). Interestingly, a recent study suggested that utrophin upregulation in the brain might not rescue behavioral deficiency in mdx mice (Perronnet et al., 2012).
Dystrophin-independent gene therapy for DMD: lessons from animal models
The striking phenotypic differences between dystrophin-deficient mice and affected humans have stimulated much interest in identifying the genes that modify DMD phenotypes. Compared with dystrophin-based therapy, the modulation of genes that already exist in the body has clear immunological advantages; the therapeutic expression of these genes is unlikely to induce immune rejection because they are considered as self (Ebihara et al., 2000).
Utrophin and α7β1-integrin are among the most obvious candidates to consider because: (1) similarly to dystrophin, they strengthen the sarcolemma by cross-linking the ECM and the cytoskeleton; (2) their expression is upregulated in mdx mice; (3) genetic elimination of either gene aggravates dystrophic manifestations in mdx mice; and (4) overexpression of either gene ameliorates muscle disease in mdx mice (Burkin et al., 2005; Burkin et al., 2001; Deconinck et al., 1997a; Deconinck et al., 1997b; Grady et al., 1997; Guo et al., 2006; Rafael et al., 1998; Rooney et al., 2006; Tinsley et al., 1998; Tinsley et al., 1996). As a result, gene therapy studies have been conducted in dystrophic mice (and some dogs) using full-length utrophin (Deol et al., 2007), mini-utrophin (Cerletti et al., 2003; Gilbert et al., 1999; Wakefield et al., 2000), micro-utrophin (Odom et al., 2008) and α7-integrin (Heller et al., 2013). As predicted from knockout and transgenic experiments, the dystrophic phenotype was significantly reduced by utrophin or integrin gene therapy.
Myostatin inhibition is another example of dystrophin-independent therapy for DMD. Myostatin is an endogenous muscle-growth inhibitor (Lee, 2004; McPherron et al., 1997). Mutations in the myostatin gene cause hypermuscularity in mouse, cattle, sheep, dog and humans (Stinckens et al., 2011). Elimination of the myostatin gene protects mdx mice by reducing fibrosis and increasing muscle strength (Wagner et al., 2002). These observations provide compelling justification to explore myostatin inhibition gene therapy in animal models and, more recently, in BMD patients (Mendell et al., 2015; Rodino-Klapac et al., 2009).
Evidence from preclinical studies is opening up new lines of investigation concerning how other endogenous genes could be used in DMD gene therapy. These include genes encoding cytotoxic T-cell GalNAc transferase (Xu et al., 2007), nNOS (Lai et al., 2014), sarcoplasmic reticulum calcium ATPase 2a (Shin et al., 2011a), peroxisome proliferator-activated receptor gamma coactivator 1-alpha (Selsby et al., 2012) and sarcospan (Marshall et al., 2013).
Conclusions and perspective
Animal models have greatly enriched our understanding of the biological function of dystrophin and the pathology of DMD, providing excellent platforms for investigating the efficacy and toxicity of experimental gene therapies. Considerable progress has been made in model development in the last three decades. We now have a large (and still expanding) collection of animal models (supplementary material Table S1). Although this offers an unprecedented opportunity for cross-species comparison and translation (Poussin et al., 2014), it also adds complexity and difficulty in model selection for preclinical studies. The advantages and limitations of each model system can vary depending on the study question. Some aspects of the DMD pathology (such as neurocognitive deficiency) remain difficult to model. Furthermore, animals are not humans. The findings from animal studies may guide but not completely predict the outcome of clinical studies. Nevertheless, the value of animal models should never be underestimated. The development of an effective gene therapy for DMD has relied heavily, and will continue to rely, on animal models (Duan, 2011). Animal studies not only establish the proof-of-principle, they are also crucial for protocol optimization before and during human tests. Certain studies that cannot be performed in affected individuals (such as necropsy, in situ and ex vivo single-muscle force measurement) will have to be carried out in animal models. The field has surmounted many obstacles in the development of DMD models. The mild mdx mice are now complemented by numerous background and mutation variants that can better mimic affected humans. However, as therapies that have been in development for the last decade enter clinical trials, new questions are emerging. Many of these new questions (such as the immune response to the AAV vector and scaling-up of systemic gene transfer) might be better answered with cDMD dogs, a model that remains to be fully characterized (Duan, 2011; Duan, 2015).
Supplementary Material
Acknowledgments
We thank Mitchell C. Tarka for help with the Fig. 1 illustration.
Footnotes
Competing interests
D.D. is a member of the scientific advisory board for Solid GT, a subsidiary of Solid Ventures.
Funding
DMD research in the Duan lab is supported by the National Institutes of Health (AR-49419, HL-91883), Department of Defense (MD-13), Muscular Dystrophy Association, Parent Project Muscular Dystrophy, Jesse’s Journey-The Foundation for Gene and Cell Therapy, Hope for Javier, Kansas City Area Life Sciences Institute and the University of Missouri.
Supplementary material
Supplementary material available online at http://dmm.biologists.org/lookup/suppl/doi:10.1242/dmm.018424/-/DC1
References
- Aartsma-Rus A. (2012). Overview on DMD exon skipping. Methods Mol. Biol. 867, 97–116. [DOI] [PubMed] [Google Scholar]
- Aartsma-Rus A., Van Deutekom J. C., Fokkema I. F., Van Ommen G. J., Den Dunnen J. T. (2006). Entries in the Leiden Duchenne muscular dystrophy mutation database: an overview of mutation types and paradoxical cases that confirm the reading-frame rule. Muscle Nerve 34, 135–144. [DOI] [PubMed] [Google Scholar]
- Acsadi G., Dickson G., Love D. R., Jani A., Walsh F. S., Gurusinghe A., Wolff J. A., Davies K. E. (1991). Human dystrophin expression in mdx mice after intramuscular injection of DNA constructs. Nature 352, 815–818. [DOI] [PubMed] [Google Scholar]
- Ahn A. H., Kunkel L. M. (1993). The structural and functional diversity of dystrophin. Nat. Genet. 3, 283–291. [DOI] [PubMed] [Google Scholar]
- Aigner B., Rathkolb B., Klaften M., Sedlmeier R., Klempt M., Wagner S., Michel D., Mayer U., Klopstock T., de Angelis M. H., et al. (2009). Generation of N-ethyl-N-nitrosourea-induced mouse mutants with deviations in plasma enzyme activities as novel organ-specific disease models. Exp. Physiol. 94, 412–421. [DOI] [PubMed] [Google Scholar]
- Akkaraju G. R., Huard J., Hoffman E. P., Goins W. F., Pruchnic R., Watkins S. C., Cohen J. B., Glorioso J. C. (1999). Herpes simplex virus vector-mediated dystrophin gene transfer and expression in mdx mouse skeletal muscle. J. Gene Med. 1, 280–289. [DOI] [PubMed] [Google Scholar]
- Alter J., Lou F., Rabinowitz A., Yin H., Rosenfeld J., Wilton S. D., Partridge T. A., Lu Q. L. (2006). Systemic delivery of morpholino oligonucleotide restores dystrophin expression bodywide and improves dystrophic pathology. Nat. Med. 12, 175–177. [DOI] [PubMed] [Google Scholar]
- Ambrósio C. E., Valadares M. C., Zucconi E., Cabral R., Pearson P. L., Gaiad T. P., Canovas M., Vainzof M., Miglino M. A., Zatz M. (2008). Ringo, a Golden Retriever Muscular Dystrophy (GRMD) dog with absent dystrophin but normal strength. Neuromuscul. Disord. 18, 892–893. [DOI] [PubMed] [Google Scholar]
- Anderson J. L., Head S. I., Rae C., Morley J. W. (2002). Brain function in Duchenne muscular dystrophy. Brain 125, 4–13. [DOI] [PubMed] [Google Scholar]
- Aoki Y., Yokota T., Nagata T., Nakamura A., Tanihata J., Saito T., Duguez S. M., Nagaraju K., Hoffman E. P., Partridge T., et al. (2012). Bodywide skipping of exons 45–55 in dystrophic mdx52 mice by systemic antisense delivery. Proc. Natl. Acad. Sci. USA 109, 13763–13768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardite E., Perdiguero E., Vidal B., Gutarra S., Serrano A. L., Muñoz-Cánoves P. (2012). PAI-1-regulated miR-21 defines a novel age-associated fibrogenic pathway in muscular dystrophy. J. Cell Biol. 196, 163–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpke R. W., Darabi R., Mader T. L., Zhang Y., Toyama A., Lonetree C. L., Nash N., Lowe D. A., Perlingeiro R. C., Kyba M. (2013). A new immuno-, dystrophin-deficient model, the NSG-mdx4cv mouse, provides evidence for functional improvement following allogeneic satellite cell transplantation. Stem Cells 31, 1611–1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashwath M. L., Jacobs I. B., Crowe C. A., Ashwath R. C., Super D. M., Bahler R. C. (2014). Left ventricular dysfunction in Duchenne muscular dystrophy and genotype. Am. J. Cardiol. 114, 284–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atencia-Fernandez S., Shiel R. E., Mooney C. T., Nolan C. M. (2015). Muscular dystrophy in the Japanese Spitz: an inversion disrupts the DMD and RPGR genes. Anim. Genet. [Epub ahead of print] 10.1111/age.12266. [DOI] [PubMed] [Google Scholar]
- Banks G. B., Judge L. M., Allen J. M., Chamberlain J. S. (2010). The polyproline site in hinge 2 influences the functional capacity of truncated dystrophins. PLoS Genet. 6, e1000958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks G. B., Combs A. C., Odom G. L., Bloch R. J., Chamberlain J. S. (2014). Muscle structure influences utrophin expression in mdx mice. PLoS Genet. 10, e1004431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbash I. M., Cecchini S., Faranesh A. Z., Virag T., Li L., Yang Y., Hoyt R. F., Kornegay J. N., Bogan J. R., Garcia L., et al. (2013). MRI roadmap-guided transendocardial delivery of exon-skipping recombinant adeno-associated virus restores dystrophin expression in a canine model of Duchenne muscular dystrophy. Gene Ther. 20, 274–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardoni A., Sironi M., Felisari G., Comi G. P., Bresolin N. (1999). Absence of brain Dp140 isoform and cognitive impairment in Becker muscular dystrophy. Lancet 353, 897–898. [DOI] [PubMed] [Google Scholar]
- Bardoni A., Felisari G., Sironi M., Comi G., Lai M., Robotti M., Bresolin N. (2000). Loss of Dp140 regulatory sequences is associated with cognitive impairment in dystrophinopathies. Neuromuscul. Disord. 10, 194–199. [DOI] [PubMed] [Google Scholar]
- Bartlett R. J., Stockinger S., Denis M. M., Bartlett W. T., Inverardi L., Le T. T., thi Man N., Morris G. E., Bogan D. J., Metcalf-Bogan J., et al. (2000). In vivo targeted repair of a point mutation in the canine dystrophin gene by a chimeric RNA/DNA oligonucleotide. Nat. Biotechnol. 18, 615–622. [DOI] [PubMed] [Google Scholar]
- Beastrom N., Lu H., Macke A., Canan B. D., Johnson E. K., Penton C. M., Kaspar B. K., Rodino-Klapac L. R., Zhou L., Janssen P. M., et al. (2011). Mdx5cv mice manifest more severe muscle dysfunction and diaphragm force deficits than do mdx Mice. Am. J. Pathol. 179, 2464–2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beggs A. H., Hoffman E. P., Snyder J. R., Arahata K., Specht L., Shapiro F., Angelini C., Sugita H., Kunkel L. M. (1991). Exploring the molecular basis for variability among patients with Becker muscular dystrophy: dystrophin gene and protein studies. Am. J. Hum. Genet. 49, 54–67. [PMC free article] [PubMed] [Google Scholar]
- Bencze M., Negroni E., Vallese D., Yacoub-Youssef H., Chaouch S., Wolff A., Aamiri A., Di Santo J. P., Chazaud B., Butler-Browne G., et al. (2012). Proinflammatory macrophages enhance the regenerative capacity of human myoblasts by modifying their kinetics of proliferation and differentiation. Mol. Ther. 20, 2168–2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger J., Currie P. D. (2012). Zebrafish models flex their muscles to shed light on muscular dystrophies. Dis. Model. Mech. 5, 726–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertoni C. (2014). Emerging gene editing strategies for Duchenne muscular dystrophy targeting stem cells. Front. Physiol. 5, 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bish L. T., Sleeper M. M., Forbes S. C., Wang B., Reynolds C., Singletary G. E., Trafny D., Morine K. J., Sanmiguel J., Cecchini S., et al. (2012). Long-term restoration of cardiac dystrophin expression in golden retriever muscular dystrophy following rAAV6-mediated exon skipping. Mol. Ther. 20, 580–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake D. J., Weir A., Newey S. E., Davies K. E. (2002). Function and genetics of dystrophin and dystrophin-related proteins in muscle. Physiol. Rev. 82, 291–329. [DOI] [PubMed] [Google Scholar]
- Bonilla E., Samitt C. E., Miranda A. F., Hays A. P., Salviati G., DiMauro S., Kunkel L. M., Hoffman E. P., Rowland L. P. (1988). Duchenne muscular dystrophy: deficiency of dystrophin at the muscle cell surface. Cell 54, 447–452. [DOI] [PubMed] [Google Scholar]
- Bostick B., Ghosh A., Yue Y., Long C., Duan D. (2007). Systemic AAV-9 transduction in mice is influenced by animal age but not by the route of administration. Gene Ther. 14, 1605–1609. [DOI] [PubMed] [Google Scholar]
- Bostick B., Yue Y., Lai Y., Long C., Li D., Duan D. (2008a). Adeno-associated virus serotype-9 microdystrophin gene therapy ameliorates electrocardiographic abnormalities in mdx mice. Hum. Gene Ther. 19, 851–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostick B., Yue Y., Long C., Duan D. (2008b). Prevention of dystrophin-deficient cardiomyopathy in twenty-one-month-old carrier mice by mosaic dystrophin expression or complementary dystrophin/utrophin expression. Circ. Res. 102, 121–130. [DOI] [PubMed] [Google Scholar]
- Bostick B., Yue Y., Long C., Marschalk N., Fine D. M., Chen J., Duan D. (2009). Cardiac expression of a mini-dystrophin that normalizes skeletal muscle force only partially restores heart function in aged mdx mice. Mol. Ther. 17, 253–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostick B., Yue Y., Duan D. (2010). Gender influences cardiac function in the mdx model of Duchenne cardiomyopathy. Muscle Nerve 42, 600–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostick B., Shin J.-H., Yue Y., Duan D. (2011). AAV-microdystrophin therapy improves cardiac performance in aged female mdx mice. Mol. Ther. 19, 1826–1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostick B., Shin J. H., Yue Y., Wasala N. B., Lai Y., Duan D. (2012). AAV micro-dystrophin gene therapy alleviates stress-induced cardiac death but not myocardial fibrosis in >21-m-old mdx mice, an end-stage model of Duchenne muscular dystrophy cardiomyopathy. J. Mol. Cell. Cardiol. 53, 217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun S. (2004). Naked plasmid DNA for the treatment of muscular dystrophy. Curr. Opin. Mol. Ther. 6, 499–505. [PubMed] [Google Scholar]
- Bulfield G., Siller W. G., Wight P. A., Moore K. J. (1984). X chromosome-linked muscular dystrophy (mdx) in the mouse. Proc. Natl. Acad. Sci. USA 81, 1189–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulman D. E., Murphy E. G., Zubrzycka-Gaarn E. E., Worton R. G., Ray P. N. (1991). Differentiation of Duchenne and Becker muscular dystrophy phenotypes with amino- and carboxy-terminal antisera specific for dystrophin. Am. J. Hum. Genet. 48, 295–304. [PMC free article] [PubMed] [Google Scholar]
- Burkin D. J., Wallace G. Q., Nicol K. J., Kaufman D. J., Kaufman S. J. (2001). Enhanced expression of the alpha 7 beta 1 integrin reduces muscular dystrophy and restores viability in dystrophic mice. J. Cell Biol. 152, 1207–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkin D. J., Wallace G. Q., Milner D. J., Chaney E. J., Mulligan J. A., Kaufman S. J. (2005). Transgenic expression of alpha7beta1 integrin maintains muscle integrity, increases regenerative capacity, promotes hypertrophy, and reduces cardiomyopathy in dystrophic mice. Am. J. Pathol. 166, 253–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bushby K., Connor E. (2011). Clinical outcome measures for trials in Duchenne muscular dystrophy: report from International Working Group meetings. Clin. Investig. (Lond) 1, 1217–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers T. J., Neumann P. E., Beggs A. H., Kunkel L. M. (1992). ELISA quantitation of dystrophin for the diagnosis of Duchenne and Becker muscular dystrophies. Neurology 42, 570–576. [PubMed] [Google Scholar]
- Cerletti M., Negri T., Cozzi F., Colpo R., Andreetta F., Croci D., Davies K. E., Cornelio F., Pozza O., Karpati G., et al. (2003). Dystrophic phenotype of canine X-linked muscular dystrophy is mitigated by adenovirus-mediated utrophin gene transfer. Gene Ther. 10, 750–757. [DOI] [PubMed] [Google Scholar]
- Chamberlain J. S. (2002). Gene therapy of muscular dystrophy. Hum. Mol. Genet. 11, 2355–2362. [DOI] [PubMed] [Google Scholar]
- Chamberlain J. S., Benian G. M. (2000). Muscular dystrophy: the worm turns to genetic disease. Curr. Biol. 10, R795–R797. [DOI] [PubMed] [Google Scholar]
- Chamberlain J. S., Metzger J., Reyes M., Townsend D., Faulkner J. A. (2007). Dystrophin-deficient mdx mice display a reduced life span and are susceptible to spontaneous rhabdomyosarcoma. FASEB J. 21, 2195–2204. [DOI] [PubMed] [Google Scholar]
- Chandrasekharan K., Yoon J. H., Xu Y., deVries S., Camboni M., Janssen P. M., Varki A., Martin P. T. (2010). A human-specific deletion in mouse Cmah increases disease severity in the mdx model of Duchenne muscular dystrophy. Sci. Transl. Med. 2, 42ra54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapdelaine P., Pichavant C., Rousseau J., Pâques F., Tremblay J. P. (2010). Meganucleases can restore the reading frame of a mutated dystrophin. Gene Ther. 17, 846–858. [DOI] [PubMed] [Google Scholar]
- Chapman V. M., Miller D. R., Armstrong D., Caskey C. T. (1989). Recovery of induced mutations for X chromosome-linked muscular dystrophy in mice. Proc. Natl. Acad. Sci. USA 86, 1292–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirak S., Arechavala-Gomeza V., Guglieri M., Feng L., Torelli S., Anthony K., Abbs S., Garralda M. E., Bourke J., Wells D. J., et al. (2011). Exon skipping and dystrophin restoration in patients with Duchenne muscular dystrophy after systemic phosphorodiamidate morpholino oligomer treatment: an open-label, phase 2, dose-escalation study. Lancet 378, 595–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemens P. R., Kochanek S., Sunada Y., Chan S., Chen H. H., Campbell K. P., Caskey C. T. (1996). In vivo muscle gene transfer of full-length dystrophin with an adenoviral vector that lacks all viral genes. Gene Ther. 3, 965–972. [PubMed] [Google Scholar]
- Cooper B. J., Valentine B. A., Wilson S., Patterson D. F., Concannon P. W. (1988a). Canine muscular dystrophy: confirmation of X-linked inheritance. J. Hered. 79, 405–408. [DOI] [PubMed] [Google Scholar]
- Cooper B. J., Winand N. J., Stedman H., Valentine B. A., Hoffman E. P., Kunkel L. M., Scott M. O., Fischbeck K. H., Kornegay J. N., Avery R. J., et al. (1988b). The homologue of the Duchenne locus is defective in X-linked muscular dystrophy of dogs. Nature 334, 154–156. [DOI] [PubMed] [Google Scholar]
- Cooper B. J., Gallagher E. A., Smith C. A., Valentine B. A., Winand N. J. (1990). Mosaic expression of dystrophin in carriers of canine X-linked muscular dystrophy. Lab. Invest. 62, 171–178. [PubMed] [Google Scholar]
- Cotten S. W., Kornegay J. N., Bogan D. J., Wadosky K. M., Patterson C., Willis M. S. (2013). Genetic myostatin decrease in the golden retriever muscular dystrophy model does not significantly affect the ubiquitin proteasome system despite enhancing the severity of disease. Am. J. Transl. Res. 6, 43–53. [PMC free article] [PubMed] [Google Scholar]
- Cox G. A., Cole N. M., Matsumura K., Phelps S. F., Hauschka S. D., Campbell K. P., Faulkner J. A., Chamberlain J. S. (1993a). Overexpression of dystrophin in transgenic mdx mice eliminates dystrophic symptoms without toxicity. Nature 364, 725–729. [DOI] [PubMed] [Google Scholar]
- Cox G. A., Phelps S. F., Chapman V. M., Chamberlain J. S. (1993b). New mdx mutation disrupts expression of muscle and nonmuscle isoforms of dystrophin. Nat. Genet. 4, 87–93. [DOI] [PubMed] [Google Scholar]
- Cox G. A., Sunada Y., Campbell K. P., Chamberlain J. S. (1994). Dp71 can restore the dystrophin-associated glycoprotein complex in muscle but fails to prevent dystrophy. Nat. Genet. 8, 333–339. [DOI] [PubMed] [Google Scholar]
- Cozzi F., Cerletti M., Luvoni G. C., Lombardo R., Brambilla P. G., Faverzani S., Blasevich F., Cornelio F., Pozza O., Mora M. (2001). Development of muscle pathology in canine X-linked muscular dystrophy. II. Quantitative characterization of histopathological progression during postnatal skeletal muscle development. Acta Neuropathol. 101, 469–478. [DOI] [PubMed] [Google Scholar]
- Crawford G. E., Faulkner J. A., Crosbie R. H., Campbell K. P., Froehner S. C., Chamberlain J. S. (2000). Assembly of the dystrophin-associated protein complex does not require the dystrophin COOH-terminal domain. J. Cell Biol. 150, 1399–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crisp A., Yin H., Goyenvalle A., Betts C., Moulton H. M., Seow Y., Babbs A., Merritt T., Saleh A. F., Gait M. J., et al. (2011). Diaphragm rescue alone prevents heart dysfunction in dystrophic mice. Hum. Mol. Genet. 20, 413–421. [DOI] [PubMed] [Google Scholar]
- D’Angelo M. G., Bresolin N. (2006). Cognitive impairment in neuromuscular disorders. Muscle Nerve 34, 16–33. [DOI] [PubMed] [Google Scholar]
- Dallérac G., Perronnet C., Chagneau C., Leblanc-Veyrac P., Samson-Desvignes N., Peltekian E., Danos O., Garcia L., Laroche S., Billard J. M., et al. (2011). Rescue of a dystrophin-like protein by exon skipping normalizes synaptic plasticity in the hippocampus of the mdx mouse. Neurobiol. Dis. 43, 635–641. [DOI] [PubMed] [Google Scholar]
- Danko I., Chapman V., Wolff J. A. (1992). The frequency of revertants in mdx mouse genetic models for Duchenne muscular dystrophy. Pediatr. Res. 32, 128–131. [DOI] [PubMed] [Google Scholar]
- Daoud F., Angeard N., Demerre B., Martie I., Benyaou R., Leturcq F., Cossée M., Deburgrave N., Saillour Y., Tuffery S., et al. (2009a). Analysis of Dp71 contribution in the severity of mental retardation through comparison of Duchenne and Becker patients differing by mutation consequences on Dp71 expression. Hum. Mol. Genet. 18, 3779–3794. [DOI] [PubMed] [Google Scholar]
- Daoud F., Candelario-Martínez A., Billard J. M., Avital A., Khelfaoui M., Rozenvald Y., Guegan M., Mornet D., Jaillard D., Nudel U., et al. (2009b). Role of mental retardation-associated dystrophin-gene product Dp71 in excitatory synapse organization, synaptic plasticity and behavioral functions. PLoS ONE 4, e6574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decary S., Hamida C. B., Mouly V., Barbet J. P., Hentati F., Butler-Browne G. S. (2000). Shorter telomeres in dystrophic muscle consistent with extensive regeneration in young children. Neuromuscul. Disord. 10, 113–120. [DOI] [PubMed] [Google Scholar]
- Deconinck A. E., Rafael J. A., Skinner J. A., Brown S. C., Potter A. C., Metzinger L., Watt D. J., Dickson J. G., Tinsley J. M., Davies K. E. (1997a). Utrophin-dystrophin-deficient mice as a model for Duchenne muscular dystrophy. Cell 90, 717–727. [DOI] [PubMed] [Google Scholar]
- Deconinck N., Tinsley J., De Backer F., Fisher R., Kahn D., Phelps S., Davies K., Gillis J. M. (1997b). Expression of truncated utrophin leads to major functional improvements in dystrophin-deficient muscles of mice. Nat. Med. 3, 1216–1221. [DOI] [PubMed] [Google Scholar]
- DelloRusso C., Scott J. M., Hartigan-O’Connor D., Salvatori G., Barjot C., Robinson A. S., Crawford R. W., Brooks S. V., Chamberlain J. S. (2002). Functional correction of adult mdx mouse muscle using gutted adenoviral vectors expressing full-length dystrophin. Proc. Natl. Acad. Sci. USA 99, 12979–12984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denti M. A., Rosa A., D’Antona G., Sthandier O., De Angelis F. G., Nicoletti C., Allocca M., Pansarasa O., Parente V., Musarò A., et al. (2006). Body-wide gene therapy of Duchenne muscular dystrophy in the mdx mouse model. Proc. Natl. Acad. Sci. USA 103, 3758–3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deol J. R., Danialou G., Larochelle N., Bourget M., Moon J. S., Liu A. B., Gilbert R., Petrof B. J., Nalbantoglu J., Karpati G. (2007). Successful compensation for dystrophin deficiency by a helper-dependent adenovirus expressing full-length utrophin. Mol. Ther. 15, 1767–1774. [DOI] [PubMed] [Google Scholar]
- Desguerre I., Christov C., Mayer M., Zeller R., Becane H. M., Bastuji-Garin S., Leturcq F., Chiron C., Chelly J., Gherardi R. K. (2009). Clinical heterogeneity of duchenne muscular dystrophy (DMD): definition of sub-phenotypes and predictive criteria by long-term follow-up. PLoS ONE 4, e4347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan D. (2006). Challenges and opportunities in dystrophin-deficient cardiomyopathy gene therapy. Hum. Mol. Genet. 15, R253–R261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan D. (2008). Myodys, a full-length dystrophin plasmid vector for Duchenne and Becker muscular dystrophy gene therapy. Curr. Opin. Mol. Ther. 10, 86–94. [PubMed] [Google Scholar]
- Duan D. (2011). Duchenne muscular dystrophy gene therapy: lost in translation? Res. Rep. Biol. 2011, 31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan D. (2015). Duchenne muscular dystrophy gene therapy in the canine model. Hum. Gene Ther. Clin. Dev. [Epub ahead of print] 10.1089/hum.2015.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan D., Hakim C. H., Ambrosio C. E., Smith B. F., Sweeney H. L. (2015). Early loss of ambulation is not a representative clinical feature in Duchenne muscular dystrophy dogs: remarks on the article of Barthélémy et al. Dis. Model. Mech. 8, 193–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz V. (2006). Enigmatic conflict of clinical and molecular diagnosis in Duchenne/Becker muscular dystrophy. Neuromuscul. Disord. 16, 865–866. [DOI] [PubMed] [Google Scholar]
- Dunckley M. G., Wells D. J., Walsh F. S., Dickson G. (1993). Direct retroviral-mediated transfer of a dystrophin minigene into mdx mouse muscle in vivo. Hum. Mol. Genet. 2, 717–723. [DOI] [PubMed] [Google Scholar]
- Dunckley M. G., Manoharan M., Villiet P., Eperon I. C., Dickson G. (1998). Modification of splicing in the dystrophin gene in cultured mdx muscle cells by antisense oligoribonucleotides. Hum. Mol. Genet. 7, 1083–1090. [DOI] [PubMed] [Google Scholar]
- Ebihara S., Guibinga G. H., Gilbert R., Nalbantoglu J., Massie B., Karpati G., Petrof B. J. (2000). Differential effects of dystrophin and utrophin gene transfer in immunocompetent muscular dystrophy (mdx) mice. Physiol. Genomics 3, 133–144. [DOI] [PubMed] [Google Scholar]
- Emery A. E. H., Muntoni F. (2003). Duchenne muscular dystrophy. Oxford; New York, NY: Oxford University Press. [Google Scholar]
- England S. B., Nicholson L. V., Johnson M. A., Forrest S. M., Love D. R., Zubrzycka-Gaarn E. E., Bulman D. E., Harris J. B., Davies K. E. (1990). Very mild muscular dystrophy associated with the deletion of 46% of dystrophin. Nature 343, 180–182. [DOI] [PubMed] [Google Scholar]
- Ervasti J. M. (2007). Dystrophin, its interactions with other proteins, and implications for muscular dystrophy. Biochim. Biophys. Acta 1772, 108–117. [DOI] [PubMed] [Google Scholar]
- Fan Z., Wang J., Ahn M., Shiloh-Malawsky Y., Chahin N., Elmore S., Bagnell C. R., Jr, Wilber K., An H., Lin W., et al. (2014). Characteristics of magnetic resonance imaging biomarkers in a natural history study of golden retriever muscular dystrophy. Neuromuscul. Disord. 24, 178–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farini A., Meregalli M., Belicchi M., Battistelli M., Parolini D., D’Antona G., Gavina M., Ottoboni L., Constantin G., Bottinelli R., et al. (2007). T and B lymphocyte depletion has a marked effect on the fibrosis of dystrophic skeletal muscles in the scid/mdx mouse. J. Pathol. 213, 229–238. [DOI] [PubMed] [Google Scholar]
- Felisari G., Martinelli Boneschi F., Bardoni A., Sironi M., Comi G. P., Robotti M., Turconi A. C., Lai M., Corrao G., Bresolin N. (2000). Loss of Dp140 dystrophin isoform and intellectual impairment in Duchenne dystrophy. Neurology 55, 559–564. [DOI] [PubMed] [Google Scholar]
- Ferreiro V., Giliberto F., Muñiz G. M., Francipane L., Marzese D. M., Mampel A., Roqué M., Frechtel G. D., Szijan I. (2009). Asymptomatic Becker muscular dystrophy in a family with a multiexon deletion. Muscle Nerve 39, 239–243. [DOI] [PubMed] [Google Scholar]
- Fine D. M., Shin J. H., Yue Y., Volkmann D., Leach S. B., Smith B. F., McIntosh M., Duan D. (2011). Age-matched comparison reveals early electrocardiography and echocardiography changes in dystrophin-deficient dogs. Neuromuscul. Disord. 21, 453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finsterer J., Cripe L. (2014). Treatment of dystrophin cardiomyopathies. Nat. Rev. Cardiol. 11, 168–179. [DOI] [PubMed] [Google Scholar]
- Flanigan K. M., Dunn D. M., von Niederhausern A., Howard M. T., Mendell J., Connolly A., Saunders C., Modrcin A., Dasouki M., Comi G. P., et al. (2009a). DMD Trp3X nonsense mutation associated with a founder effect in North American families with mild Becker muscular dystrophy. Neuromuscul. Disord. 19, 743–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanigan K. M., Dunn D. M., von Niederhausern A., Soltanzadeh P., Gappmaier E., Howard M. T., Sampson J. B., Mendell J. R., Wall C., King W. M., et al. United Dystrophinopathy Project Consortium (2009b). Mutational spectrum of DMD mutations in dystrophinopathy patients: application of modern diagnostic techniques to a large cohort. Hum. Mutat. 30, 1657–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster H., Sharp P. S., Athanasopoulos T., Trollet C., Graham I. R., Foster K., Wells D. J., Dickson G. (2008). Codon and mRNA sequence optimization of microdystrophin transgenes improves expression and physiological outcome in dystrophic mdx mice following AAV2/8 gene transfer. Mol. Ther. 16, 1825–1832. [DOI] [PubMed] [Google Scholar]
- Fujimoto T., Itoh K., Yaoi T., Fushiki S. (2014). Somatodendritic and excitatory postsynaptic distribution of neuron-type dystrophin isoform, Dp40, in hippocampal neurons. Biochem. Biophys. Res. Commun. 452, 79–84. [DOI] [PubMed] [Google Scholar]
- Fukada S., Morikawa D., Yamamoto Y., Yoshida T., Sumie N., Yamaguchi M., Ito T., Miyagoe-Suzuki Y., Takeda S., Tsujikawa K., et al. (2010). Genetic background affects properties of satellite cells and mdx phenotypes. Am. J. Pathol. 176, 2414–2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funkquist B., Haraldsson I., Stahre L. (1980). Primary progressive muscular dystrophy in the dog. Vet. Rec. 106, 341–343. [DOI] [PubMed] [Google Scholar]
- Gaedigk R., Law D. J., Fitzgerald-Gustafson K. M., McNulty S. G., Nsumu N. N., Modrcin A. C., Rinaldi R. J., Pinson D., Fowler S. C., Bilgen M., et al. (2006). Improvement in survival and muscle function in an mdx/utrn(−/−) double mutant mouse using a human retinal dystrophin transgene. Neuromuscul. Disord. 16, 192–203. [DOI] [PubMed] [Google Scholar]
- Gao G. P., Alvira M. R., Wang L., Calcedo R., Johnston J., Wilson J. M. (2002). Novel adeno-associated viruses from rhesus monkeys as vectors for human gene therapy. Proc. Natl. Acad. Sci. USA 99, 11854–11859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawlik K. I., Holmberg J., Durbeej M. (2014). Loss of dystrophin and β-sarcoglycan significantly exacerbates the phenotype of laminin α2 chain-deficient animals. Am. J. Pathol. 184, 740–752. [DOI] [PubMed] [Google Scholar]
- Gebski B. L., Mann C. J., Fletcher S., Wilton S. D. (2003). Morpholino antisense oligonucleotide induced dystrophin exon 23 skipping in mdx mouse muscle. Hum. Mol. Genet. 12, 1801–1811. [DOI] [PubMed] [Google Scholar]
- Ghedini P. C., Avellar M. C., De Lima T. C., Lima-Landman M. T., Lapa A. J., Souccar C. (2012). Quantitative changes of nicotinic receptors in the hippocampus of dystrophin-deficient mice. Brain Res. 1483, 96–104. [DOI] [PubMed] [Google Scholar]
- Ghosh A., Yue Y., Lai Y., Duan D. (2008). A hybrid vector system expands adeno-associated viral vector packaging capacity in a transgene-independent manner. Mol. Ther. 16, 124–130. [DOI] [PubMed] [Google Scholar]
- Gilbert R., Nalbantoglu J., Petrof B. J., Ebihara S., Guibinga G. H., Tinsley J. M., Kamen A., Massie B., Davies K. E., Karpati G. (1999). Adenovirus-mediated utrophin gene transfer mitigates the dystrophic phenotype of mdx mouse muscles. Hum. Gene Ther. 10, 1299–1310. [DOI] [PubMed] [Google Scholar]
- Goemans N. M., Tulinius M., van den Akker J. T., Burm B. E., Ekhart P. F., Heuvelmans N., Holling T., Janson A. A., Platenburg G. J., Sipkens J. A., et al. (2011). Systemic administration of PRO051 in Duchenne’s muscular dystrophy. N. Engl. J. Med. 364, 1513–1522. [DOI] [PubMed] [Google Scholar]
- Goyenvalle A., Vulin A., Fougerousse F., Leturcq F., Kaplan J. C., Garcia L., Danos O. (2004). Rescue of dystrophic muscle through U7 snRNA-mediated exon skipping. Science 306, 1796–1799. [DOI] [PubMed] [Google Scholar]
- Goyenvalle A., Seto J. T., Davies K. E., Chamberlain J. (2011). Therapeutic approaches to muscular dystrophy. Hum. Mol. Genet. 20, R69–R78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyenvalle A., Babbs A., Wright J., Wilkins V., Powell D., Garcia L., Davies K. E. (2012). Rescue of severely affected dystrophin/utrophin-deficient mice through scAAV-U7snRNA-mediated exon skipping. Hum. Mol. Genet. 21, 2559–2571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graciotti L., Minelli A., Minciacchi D., Procopio A., Fulgenzi G. (2008). GABAergic miniature spontaneous activity is increased in the CA1 hippocampal region of dystrophic mdx mice. Neuromuscul. Disord. 18, 220–226. [DOI] [PubMed] [Google Scholar]
- Grady R. M., Teng H., Nichol M. C., Cunningham J. C., Wilkinson R. S., Sanes J. R. (1997). Skeletal and cardiac myopathies in mice lacking utrophin and dystrophin: a model for Duchenne muscular dystrophy. Cell 90, 729–738. [DOI] [PubMed] [Google Scholar]
- Grady R. M., Grange R. W., Lau K. S., Maimone M. M., Nichol M. C., Stull J. T., Sanes J. R. (1999). Role for alpha-dystrobrevin in the pathogenesis of dystrophin-dependent muscular dystrophies. Nat. Cell Biol. 1, 215–220. [DOI] [PubMed] [Google Scholar]
- Greenberg D. S., Sunada Y., Campbell K. P., Yaffe D., Nudel U. (1994). Exogenous Dp71 restores the levels of dystrophin associated proteins but does not alleviate muscle damage in mdx mice. Nat. Genet. 8, 340–344. [DOI] [PubMed] [Google Scholar]
- Gregorevic P., Blankinship M. J., Allen J. M., Crawford R. W., Meuse L., Miller D. G., Russell D. W., Chamberlain J. S. (2004). Systemic delivery of genes to striated muscles using adeno-associated viral vectors. Nat. Med. 10, 828–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregorevic P., Allen J. M., Minami E., Blankinship M. J., Haraguchi M., Meuse L., Finn E., Adams M. E., Froehner S. C., Murry C. E., et al. (2006). rAAV6-microdystrophin preserves muscle function and extends lifespan in severely dystrophic mice. Nat. Med. 12, 787–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo C., Willem M., Werner A., Raivich G., Emerson M., Neyses L., Mayer U. (2006). Absence of alpha 7 integrin in dystrophin-deficient mice causes a myopathy similar to Duchenne muscular dystrophy. Hum. Mol. Genet. 15, 989–998. [DOI] [PubMed] [Google Scholar]
- Haecker S. E., Stedman H. H., Balice-Gordon R. J., Smith D. B., Greelish J. P., Mitchell M. A., Wells A., Sweeney H. L., Wilson J. M. (1996). In vivo expression of full-length human dystrophin from adenoviral vectors deleted of all viral genes. Hum. Gene Ther. 7, 1907–1914. [DOI] [PubMed] [Google Scholar]
- Hakim C. H., Duan D. (2013). Truncated dystrophins reduce muscle stiffness in the extensor digitorum longus muscle of mdx mice. J. Appl. Physiol. 114, 482–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakim C. H., Grange R. W., Duan D. (2011). The passive mechanical properties of the extensor digitorum longus muscle are compromised in 2- to 20-mo-old mdx mice. J. Appl. Physiol. 110, 1656–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakim C. H., Yue Y., Shin J. H., Williams R. R., Zhang K., Smith B. F., Duan D. (2014). Systemic gene transfer reveals distinctive muscle transduction profile of tyrosine mutant AAV-1, -6, and -9 in neonatal dogs. Mol Ther Methods Clin Dev 1, 14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han R., Rader E. P., Levy J. R., Bansal D., Campbell K. P. (2011). Dystrophin deficiency exacerbates skeletal muscle pathology in dysferlin-null mice. Skelet Muscle 1, 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S. Q. (2013). Molecular dissection of dystrophin identifies the docking site for nNOS. Proc. Natl. Acad. Sci. USA 110, 387–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S. Q., Hauser M. A., DelloRusso C., Duan D., Crawford R. W., Phelps S. F., Harper H. A., Robinson A. S., Engelhardt J. F., Brooks S. V., et al. (2002). Modular flexibility of dystrophin: implications for gene therapy of Duchenne muscular dystrophy. Nat. Med. 8, 253–261. [DOI] [PubMed] [Google Scholar]
- Hattori N., Kaido M., Nishigaki T., Inui K., Fujimura H., Nishimura T., Naka T., Hazama T. (1999). Undetectable dystrophin can still result in a relatively benign phenotype of dystrophinopathy. Neuromuscul. Disord. 9, 220–226. [DOI] [PubMed] [Google Scholar]
- Hedlund M., Tangvoranuntakul P., Takematsu H., Long J. M., Housley G. D., Kozutsumi Y., Suzuki A., Wynshaw-Boris A., Ryan A. F., Gallo R. L., et al. (2007). N-glycolylneuraminic acid deficiency in mice: implications for human biology and evolution. Mol. Cell. Biol. 27, 4340–4346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller K. N., Montgomery C. L., Janssen P. M., Clark K. R., Mendell J. R., Rodino-Klapac L. R. (2013). AAV-mediated overexpression of human α7 integrin leads to histological and functional improvement in dystrophic mice. Mol. Ther. 21, 520–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henricson E. K., Abresch R. T., Cnaan A., Hu F., Duong T., Arrieta A., Han J., Escolar D. M., Florence J. M., Clemens P. R., et al. CINRG Investigators (2013). The cooperative international neuromuscular research group Duchenne natural history study: glucocorticoid treatment preserves clinically meaningful functional milestones and reduces rate of disease progression as measured by manual muscle testing and other commonly used clinical trial outcome measures. Muscle Nerve 48, 55–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman E. P., Gorospe J. R. M. (1991). The animal models of Duchenne muscular dystrophy: windows on the pathophsiological consequences of dystrophin deficiency. Curr. Top. Membr. 38, 113–154. [Google Scholar]
- Hoffman E. P., Kunkel L. M. (1989). Dystrophin abnormalities in Duchenne/Becker muscular dystrophy. Neuron 2, 1019–1029. [DOI] [PubMed] [Google Scholar]
- Hoffman E. P., McNally E. M. (2014). Exon-skipping therapy: a roadblock, detour, or bump in the road? Sci. Transl. Med. 6, 230fs14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman E. P., Brown R. H., Jr, Kunkel L. M. (1987). Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell 51, 919–928. [DOI] [PubMed] [Google Scholar]
- Hoffman E. P., Kunkel L. M., Angelini C., Clarke A., Johnson M., Harris J. B. (1989). Improved diagnosis of Becker muscular dystrophy by dystrophin testing. Neurology 39, 1011–1017. [DOI] [PubMed] [Google Scholar]
- Hollinger K., Yang C. X., Montz R. E., Nonneman D., Ross J. W., Selsby J. T. (2014). Dystrophin insufficiency causes selective muscle histopathology and loss of dystrophin-glycoprotein complex assembly in pig skeletal muscle. FASEB J. 28, 1600–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosur V., Kavirayani A., Riefler J., Carney L. M., Lyons B., Gott B., Cox G. A., Shultz L. D. (2012). Dystrophin and dysferlin double mutant mice: a novel model for rhabdomyosarcoma. Cancer Genet 205, 232–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell J. M., Lochmüller H., O’Hara A., Fletcher S., Kakulas B. A., Massie B., Nalbantoglu J., Karpati G. (1998). High-level dystrophin expression after adenovirus-mediated dystrophin minigene transfer to skeletal muscle of dystrophic dogs: prolongation of expression with immunosuppression. Hum. Gene Ther. 9, 629–634. [DOI] [PubMed] [Google Scholar]
- Huang X., Poy F., Zhang R., Joachimiak A., Sudol M., Eck M. J. (2000). Structure of a WW domain containing fragment of dystrophin in complex with beta-dystroglycan. Nat. Struct. Biol. 7, 634–638. [DOI] [PubMed] [Google Scholar]
- Im W. B., Phelps S. F., Copen E. H., Adams E. G., Slightom J. L., Chamberlain J. S. (1996). Differential expression of dystrophin isoforms in strains of mdx mice with different mutations. Hum. Mol. Genet. 5, 1149–1153. [DOI] [PubMed] [Google Scholar]
- Innes J. R. (1951). Myopathies in animals; a record of some cases including progressive muscular dystrophy (pseudo-hypertrophic) (dog), “weisses Fleisch” (lamb), neuropathic muscular atrophy (sheep) and lymphocytic/histiocytic myositis, neuritis, radiculitis (dog). Br. Vet. J. 107, 131–143. [DOI] [PubMed] [Google Scholar]
- Ishizaki M., Maeda Y., Kawano R., Suga T., Uchida Y., Uchino K., Yamashita S., Kimura E., Uchino M. (2011). Rescue from respiratory dysfunction by transduction of full-length dystrophin to diaphragm via the peritoneal cavity in utrophin/dystrophin double knockout mice. Mol. Ther. 19, 1230–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jearawiriyapaisarn N., Moulton H. M., Buckley B., Roberts J., Sazani P., Fucharoen S., Iversen P. L., Kole R. (2008). Sustained dystrophin expression induced by peptide-conjugated morpholino oligomers in the muscles of mdx mice. Mol. Ther. 16, 1624–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judge L. M., Haraguchiln M., Chamberlain J. S. (2006). Dissecting the signaling and mechanical functions of the dystrophin-glycoprotein complex. J. Cell Sci. 119, 1537–1546. [DOI] [PubMed] [Google Scholar]
- Judge L. M., Arnett A. L., Banks G. B., Chamberlain J. S. (2011). Expression of the dystrophin isoform Dp116 preserves functional muscle mass and extends lifespan without preventing dystrophy in severely dystrophic mice. Hum. Mol. Genet. 20, 4978–4990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawano R., Ishizaki M., Maeda Y., Uchida Y., Kimura E., Uchino M. (2008). Transduction of full-length dystrophin to multiple skeletal muscles improves motor performance and life span in utrophin/dystrophin double knockout mice. Mol. Ther. 16, 825–831. [DOI] [PubMed] [Google Scholar]
- Kayali R., Bury F., Ballard M., Bertoni C. (2010). Site-directed gene repair of the dystrophin gene mediated by PNA-ssODNs. Hum. Mol. Genet. 19, 3266–3281. [DOI] [PubMed] [Google Scholar]
- Kinali M., Arechavala-Gomeza V., Feng L., Cirak S., Hunt D., Adkin C., Guglieri M., Ashton E., Abbs S., Nihoyannopoulos P., et al. (2009). Local restoration of dystrophin expression with the morpholino oligomer AVI-4658 in Duchenne muscular dystrophy: a single-blind, placebo-controlled, dose-escalation, proof-of-concept study. Lancet Neurol. 8, 918–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klymiuk N., Blutke A., Graf A., Krause S., Burkhardt K., Wuensch A., Krebs S., Kessler B., Zakhartchenko V., Kurome M., et al. (2013). Dystrophin-deficient pigs provide new insights into the hierarchy of physiological derangements of dystrophic muscle. Hum. Mol. Genet. 22, 4368–4382. [DOI] [PubMed] [Google Scholar]
- Kochanek S., Clemens P. R., Mitani K., Chen H. H., Chan S., Caskey C. T. (1996). A new adenoviral vector: Replacement of all viral coding sequences with 28 kb of DNA independently expressing both full-length dystrophin and beta-galactosidase. Proc. Natl. Acad. Sci. USA 93, 5731–5736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig M., Hoffman E. P., Bertelson C. J., Monaco A. P., Feener C., Kunkel L. M. (1987). Complete cloning of the Duchenne muscular dystrophy (DMD) cDNA and preliminary genomic organization of the DMD gene in normal and affected individuals. Cell 50, 509–517. [DOI] [PubMed] [Google Scholar]
- Konieczny P., Swiderski K., Chamberlain J. S. (2013). Gene and cell-mediated therapies for muscular dystrophy. Muscle Nerve 47, 649–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo T., Wood M. J. (2013). Clinical trials using antisense oligonucleotides in Duchenne muscular dystrophy. Hum. Gene Ther. 24, 479–488. [DOI] [PubMed] [Google Scholar]
- Koo T., Malerba A., Athanasopoulos T., Trollet C., Boldrin L., Ferry A., Popplewell L., Foster H., Foster K., Dickson G. (2011a). Delivery of AAV2/9-microdystrophin genes incorporating helix 1 of the coiled-coil motif in the C-terminal domain of dystrophin improves muscle pathology and restores the level of α1-syntrophin and α-dystrobrevin in skeletal muscles of mdx mice. Hum. Gene Ther. 22, 1379–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo T., Okada T., Athanasopoulos T., Foster H., Takeda S., Dickson G. (2011b). Long-term functional adeno-associated virus-microdystrophin expression in the dystrophic CXMDj dog. J. Gene Med. 13, 497–506. [DOI] [PubMed] [Google Scholar]
- Koo T., Popplewell L., Athanasopoulos T., Dickson G. (2014). Triple trans-splicing adeno-associated virus vectors capable of transferring the coding sequence for full-length dystrophin protein into dystrophic mice. Hum. Gene Ther. 25, 98–108. [DOI] [PubMed] [Google Scholar]
- Kornegay J. N., Tuler S. M., Miller D. M., Levesque D. C. (1988). Muscular dystrophy in a litter of golden retriever dogs. Muscle Nerve 11, 1056–1064. [DOI] [PubMed] [Google Scholar]
- Kornegay J. N., Li J., Bogan J. R., Bogan D. J., Chen C., Zheng H., Wang B., Qiao C., Howard J. F., Jr, Xiao X. (2010). Widespread muscle expression of an AAV9 human mini-dystrophin vector after intravenous injection in neonatal dystrophin-deficient dogs. Mol. Ther. 18, 1501–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornegay J. N., Bogan J. R., Bogan D. J., Childers M. K., Li J., Nghiem P., Detwiler D. A., Larsen C. A., Grange R. W., Bhavaraju-Sanka R. K., et al. (2012). Canine models of Duchenne muscular dystrophy and their use in therapeutic strategies. Mamm. Genome 23, 85–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krivov L. I., Stenina M. A., Yarygin V. N., Polyakov A. V., Savchuk V. I., Obrubov S. A., Komarova N. V. (2009). A new genetic variant of mdx mice: study of the phenotype. Bull. Exp. Biol. Med. 147, 625–629. [DOI] [PubMed] [Google Scholar]
- Kumar-Singh R., Chamberlain J. S. (1996). Encapsidated adenovirus minichromosomes allow delivery and expression of a 14 kb dystrophin cDNA to muscle cells. Hum. Mol. Genet. 5, 913–921. [DOI] [PubMed] [Google Scholar]
- Kunkel L. M. (2005). 2004. William Allan award address. cloning of the DMD gene. Am. J. Hum. Genet. 76, 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunkel L. M., Bachrach E., Bennett R. R., Guyon J., Steffen L. (2006). Diagnosis and cell-based therapy for Duchenne muscular dystrophy in humans, mice, and zebrafish. J. Hum. Genet. 51, 397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y., Duan D. (2012). Progress in gene therapy of dystrophic heart disease. Gene Ther. 19, 678–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y., Yue Y., Liu M., Ghosh A., Engelhardt J. F., Chamberlain J. S., Duan D. (2005). Efficient in vivo gene expression by trans-splicing adeno-associated viral vectors. Nat. Biotechnol. 23, 1435–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y., Thomas G. D., Yue Y., Yang H. T., Li D., Long C., Judge L., Bostick B., Chamberlain J. S., Terjung R. L., et al. (2009). Dystrophins carrying spectrin-like repeats 16 and 17 anchor nNOS to the sarcolemma and enhance exercise performance in a mouse model of muscular dystrophy. J. Clin. Invest. 119, 624–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y., Zhao J., Yue Y., Duan D. (2013). α2 and α3 helices of dystrophin R16 and R17 frame a microdomain in the α1 helix of dystrophin R17 for neuronal NOS binding. Proc. Natl. Acad. Sci. USA 110, 525–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y., Zhao J., Yue Y., Wasala N. B., Duan D. (2014). Partial restoration of cardiac function with ΔPDZ nNOS in aged mdx model of Duchenne cardiomyopathy. Hum. Mol. Genet. 23, 3189–3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanfossi M., Cozzi F., Bugini D., Colombo S., Scarpa P., Morandi L., Galbiati S., Cornelio F., Pozza O., Mora M. (1999). Development of muscle pathology in canine X-linked muscular dystrophy. I. Delayed postnatal maturation of affected and normal muscle as revealed by myosin isoform analysis and utrophin expression. Acta Neuropathol. 97, 127–138. [DOI] [PubMed] [Google Scholar]
- Le Guiner C., Montus M., Servais L., Cherel Y., Francois V., Thibaud J. L., Wary C., Matot B., Larcher T., Guigand L., et al. (2014). Forelimb treatment in a large cohort of dystrophic dogs supports delivery of a recombinant AAV for exon skipping in Duchenne patients. Mol. Ther. 22, 1923–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. J. (2004). Regulation of muscle mass by myostatin. Annu. Rev. Cell Dev. Biol. 20, 61–86. [DOI] [PubMed] [Google Scholar]
- Lefaucheur J. P., Pastoret C., Sebille A. (1995). Phenotype of dystrophinopathy in old mdx mice. Anat. Rec. 242, 70–76. [DOI] [PubMed] [Google Scholar]
- Leibovitz S., Meshorer A., Fridman Y., Wieneke S., Jockusch H., Yaffe D., Nudel U. (2002). Exogenous Dp71 is a dominant negative competitor of dystrophin in skeletal muscle. Neuromuscul. Disord. 12, 836–844. [DOI] [PubMed] [Google Scholar]
- Li D., Yue Y., Duan D. (2008). Preservation of muscle force in Mdx3cv mice correlates with low-level expression of a near full-length dystrophin protein. Am. J. Pathol. 172, 1332–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Long C., Yue Y., Duan D. (2009). Sub-physiological sarcoglycan expression contributes to compensatory muscle protection in mdx mice. Hum. Mol. Genet. 18, 1209–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Yue Y., Duan D. (2010). Marginal level dystrophin expression improves clinical outcome in a strain of dystrophin/utrophin double knockout mice. PLoS ONE 5, e15286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Yue Y., Lai Y., Hakim C. H., Duan D. (2011). Nitrosative stress elicited by nNOSμ delocalization inhibits muscle force in dystrophin-null mice. J. Pathol. 223, 88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidov H. G. (1996). Dystrophin in the nervous system. Brain Pathol. 6, 63–77. [DOI] [PubMed] [Google Scholar]
- Liu Q., Perez C. F., Wang Y. (2006). Efficient site-specific integration of large transgenes by an enhanced herpes simplex virus/adeno-associated virus hybrid amplicon vector. J. Virol. 80, 1672–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd T. E., Taylor J. P. (2010). Flightless flies: Drosophila models of neuromuscular disease. Ann. N. Y. Acad. Sci. 1184, e1–e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long C., McAnally J. R., Shelton J. M., Mireault A. A., Bassel-Duby R., Olson E. N. (2014). Prevention of muscular dystrophy in mice by CRISPR/Cas9-mediated editing of germline DNA. Science 345, 1184–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lostal W., Kodippili K., Yue Y., Duan D. (2014). Full-length dystrophin reconstitution with adeno-associated viral vectors. Hum. Gene Ther. 25, 552–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Q. L., Mann C. J., Lou F., Bou-Gharios G., Morris G. E., Xue S. A., Fletcher S., Partridge T. A., Wilton S. D. (2003). Functional amounts of dystrophin produced by skipping the mutated exon in the mdx dystrophic mouse. Nat. Med. 9, 1009–1014. [DOI] [PubMed] [Google Scholar]
- Lu Q. L., Rabinowitz A., Chen Y. C., Yokota T., Yin H., Alter J., Jadoon A., Bou-Gharios G., Partridge T. (2005). Systemic delivery of antisense oligoribonucleotide restores dystrophin expression in body-wide skeletal muscles. Proc. Natl. Acad. Sci. USA 102, 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Q. L., Yokota T., Takeda S., Garcia L., Muntoni F., Partridge T. (2011). The status of exon skipping as a therapeutic approach to duchenne muscular dystrophy. Mol. Ther. 19, 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch G. S., Hinkle R. T., Chamberlain J. S., Brooks S. V., Faulkner J. A. (2001). Force and power output of fast and slow skeletal muscles from mdx mice 6–28 months old. J. Physiol. 535, 591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magri F., Govoni A., D’Angelo M. G., Del Bo R., Ghezzi S., Sandra G., Turconi A. C., Sciacco M., Ciscato P., Bordoni A., et al. (2011). Genotype and phenotype characterization in a large dystrophinopathic cohort with extended follow-up. J. Neurol. 258, 1610–1623. [DOI] [PubMed] [Google Scholar]
- Mann C. J., Honeyman K., Cheng A. J., Ly T., Lloyd F., Fletcher S., Morgan J. E., Partridge T. A., Wilton S. D. (2001). Antisense-induced exon skipping and synthesis of dystrophin in the mdx mouse. Proc. Natl. Acad. Sci. USA 98, 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J. L., Kwok Y., McMorran B. J., Baum L. G., Crosbie-Watson R. H. (2013). The potential of sarcospan in adhesion complex replacement therapeutics for the treatment of muscular dystrophy. FEBS J. 280, 4210–4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins P. C., Ayub-Guerrieri D., Martins-Bach A. B., Onofre-Oliveira P., Malheiros J. M., Tannus A., de Sousa P. L., Carlier P. G., Vainzof M. (2013). Dmdmdx/Largemyd: a new mouse model of neuromuscular diseases useful for studying physiopathological mechanisms and testing therapies. Dis. Model. Mech. 6, 1167–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe E. R., Towbin J., Chamberlain J., Baumbach L., Witkowski J., van Ommen G. J., Koenig M., Kunkel L. M., Seltzer W. K. (1989). Complementary DNA probes for the Duchenne muscular dystrophy locus demonstrate a previously undetectable deletion in a patient with dystrophic myopathy, glycerol kinase deficiency, and congenital adrenal hypoplasia. J. Clin. Invest. 83, 95–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClorey G., Moulton H. M., Iversen P. L., Fletcher S., Wilton S. D. (2006). Antisense oligonucleotide-induced exon skipping restores dystrophin expression in vitro in a canine model of DMD. Gene Ther. 13, 1373–1381. [DOI] [PubMed] [Google Scholar]
- McCully K., Giger U., Argov Z., Valentine B., Cooper B., Chance B., Bank W. (1991). Canine X-linked muscular dystrophy studied with in vivo phosphorus magnetic resonance spectroscopy. Muscle Nerve 14, 1091–1098. [DOI] [PubMed] [Google Scholar]
- McDonald C. M., Henricson E. K., Han J. J., Abresch R. T., Nicorici A., Atkinson L., Elfring G. L., Reha A., Miller L. L. (2010). The 6-minute walk test in Duchenne/Becker muscular dystrophy: longitudinal observations. Muscle Nerve 42, 966–974. [DOI] [PubMed] [Google Scholar]
- McDonald C. M., Henricson E. K., Abresch R. T., Florence J. M., Eagle M., Gappmaier E., Glanzman A. M., Spiegel R., Barth J., Elfring G., et al. PTC124-GD-007-DMD Study Group (2013a). The 6-minute walk test and other endpoints in Duchenne muscular dystrophy: longitudinal natural history observations over 48 weeks from a multicenter study. Muscle Nerve 48, 343–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald C. M., Henricson E. K., Abresch R. T., Han J. J., Escolar D. M., Florence J. M., Duong T., Arrieta A., Clemens P. R., Hoffman E. P., et al. Cinrg Investigators (2013b). The cooperative international neuromuscular research group Duchenne natural history study—a longitudinal investigation in the era of glucocorticoid therapy: design of protocol and the methods used. Muscle Nerve 48, 32–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherron A. C., Lawler A. M., Lee S. J. (1997). Regulation of skeletal muscle mass in mice by a new TGF-beta superfamily member. Nature 387, 83–90. [DOI] [PubMed] [Google Scholar]
- Megeney L. A., Kablar B., Garrett K., Anderson J. E., Rudnicki M. A. (1996). MyoD is required for myogenic stem cell function in adult skeletal muscle. Genes Dev. 10, 1173–1183. [DOI] [PubMed] [Google Scholar]
- Megeney L. A., Kablar B., Perry R. L., Ying C., May L., Rudnicki M. A. (1999). Severe cardiomyopathy in mice lacking dystrophin and MyoD. Proc. Natl. Acad. Sci. USA 96, 220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendell J. R., Lloyd-Puryear M. (2013). Report of MDA muscle disease symposium on newborn screening for Duchenne muscular dystrophy. Muscle Nerve 48, 21–26. [DOI] [PubMed] [Google Scholar]
- Mendell J. R., Rodino-Klapac L., Sahenk Z., Malik V., Kaspar B. K., Walker C. M., Clark K. R. (2012). Gene therapy for muscular dystrophy: lessons learned and path forward. Neurosci. Lett. 527, 90–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendell J. R., Rodino-Klapac L. R., Sahenk Z., Roush K., Bird L., Lowes L. P., Alfano L., Gomez A. M., Lewis S., Kota J., et al. Eteplirsen Study Group (2013). Eteplirsen for the treatment of Duchenne muscular dystrophy. Ann. Neurol. 74, 637–647. [DOI] [PubMed] [Google Scholar]
- Mendell J. R., Sahenk Z., Malik V., Gomez A. M., Flanigan K. M., Lowes L. P., Alfano L. N., Berry K., Meadows E., Lewis S., et al. (2015). A phase 1/2a follistatin gene therapy trial for Becker muscular dystrophy. Mol. Ther. 23, 192–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercuri E., Muntoni F. (2013). Muscular dystrophy: new challenges and review of the current clinical trials. Curr. Opin. Pediatr. 25, 701–707. [DOI] [PubMed] [Google Scholar]
- Miranda R., Sébrié C., Degrouard J., Gillet B., Jaillard D., Laroche S., Vaillend C. (2009). Reorganization of inhibitory synapses and increased PSD length of perforated excitatory synapses in hippocampal area CA1 of dystrophin-deficient mdx mice. Cereb. Cortex 19, 876–888. [DOI] [PubMed] [Google Scholar]
- Miranda R., Nudel U., Laroche S., Vaillend C. (2011). Altered presynaptic ultrastructure in excitatory hippocampal synapses of mice lacking dystrophins Dp427 or Dp71. Neurobiol. Dis. 43, 134–141. [DOI] [PubMed] [Google Scholar]
- Miyazato L. G., Moraes J. R., Beretta D. C., Kornegay J. N. (2011). Muscular dystrophy in dogs: does the crossing of breeds influence disease phenotype? Vet. Pathol. 48, 655–662. [DOI] [PubMed] [Google Scholar]
- Moise N. S., Valentine B. A., Brown C. A., Erb H. N., Beck K. A., Cooper B. J., Gilmour R. F. (1991). Duchenne’s cardiomyopathy in a canine model: electrocardiographic and echocardiographic studies. J. Am. Coll. Cardiol. 17, 812–820. [DOI] [PubMed] [Google Scholar]
- Moizard M. P., Billard C., Toutain A., Berret F., Marmin N., Moraine C. (1998). Are Dp71 and Dp140 brain dystrophin isoforms related to cognitive impairment in Duchenne muscular dystrophy? Am. J. Med. Genet. 80, 32–41. [DOI] [PubMed] [Google Scholar]
- Moizard M. P., Toutain A., Fournier D., Berret F., Raynaud M., Billard C., Andres C., Moraine C. (2000). Severe cognitive impairment in DMD: obvious clinical indication for Dp71 isoform point mutation screening. Eur. J. Hum. Genet. 8, 552–556. [DOI] [PubMed] [Google Scholar]
- Monaco A. P., Neve R. L., Colletti-Feener C., Bertelson C. J., Kurnit D. M., Kunkel L. M. (1986). Isolation of candidate cDNAs for portions of the Duchenne muscular dystrophy gene. Nature 323, 646–650. [DOI] [PubMed] [Google Scholar]
- Monaco A. P., Bertelson C. J., Liechti-Gallati S., Moser H., Kunkel L. M. (1988). An explanation for the phenotypic differences between patients bearing partial deletions of the DMD locus. Genomics 2, 90–95. [DOI] [PubMed] [Google Scholar]
- Morrison J., Lu Q. L., Pastoret C., Partridge T., Bou-Gharios G. (2000). T-cell-dependent fibrosis in the mdx dystrophic mouse. Lab. Invest. 80, 881–891. [DOI] [PubMed] [Google Scholar]
- Mourkioti F., Kustan J., Kraft P., Day J. W., Zhao M. M., Kost-Alimova M., Protopopov A., DePinho R. A., Bernstein D., Meeker A. K., et al. (2013). Role of telomere dysfunction in cardiac failure in Duchenne muscular dystrophy. Nat. Cell Biol. 15, 895–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntoni F., Mateddu A., Serra G. (1991). Passive avoidance behaviour deficit in the mdx mouse. Neuromuscul. Disord. 1, 121–123. [DOI] [PubMed] [Google Scholar]
- Nakamura A., Yoshida K., Fukushima K., Ueda H., Urasawa N., Koyama J., Yazaki Y., Yazaki M., Sakai T., Haruta S., et al. (2008). Follow-up of three patients with a large in-frame deletion of exons 45–55 in the Duchenne muscular dystrophy (DMD) gene. J. Clin. Neurosci. 15, 757–763. [DOI] [PubMed] [Google Scholar]
- Nakamura A., Kobayashi M., Kuraoka M., Yuasa K., Yugeta N., Okada T., Takeda S. (2013). Initial pulmonary respiration causes massive diaphragm damage and hyper-CKemia in Duchenne muscular dystrophy dog. Sci. Rep. 3, 2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura K., Fujii W., Tsuboi M., Tanihata J., Teramoto N., Takeuchi S., Naito K., Yamanouchi K., Nishihara M. (2014). Generation of muscular dystrophy model rats with a CRISPR/Cas system. Sci. Rep. 4, 5635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nardes F., Araújo A. P., Ribeiro M. G. (2012). Mental retardation in Duchenne muscular dystrophy. J. Pediatr. (Rio J.) 88, 6–16. [DOI] [PubMed] [Google Scholar]
- Neri M., Torelli S., Brown S., Ugo I., Sabatelli P., Merlini L., Spitali P., Rimessi P., Gualandi F., Sewry C., et al. (2007). Dystrophin levels as low as 30% are sufficient to avoid muscular dystrophy in the human. Neuromuscul. Disord. 17, 913–918. [DOI] [PubMed] [Google Scholar]
- Nguyen F., Cherel Y., Guigand L., Goubault-Leroux I., Wyers M. (2002). Muscle lesions associated with dystrophin deficiency in neonatal golden retriever puppies. J. Comp. Pathol. 126, 100–108. [DOI] [PubMed] [Google Scholar]
- Nicholson L. V., Johnson M. A., Bushby K. M., Gardner-Medwin D. (1993a). Functional significance of dystrophin positive fibres in Duchenne muscular dystrophy. Arch. Dis. Child. 68, 632–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson L. V., Johnson M. A., Bushby K. M., Gardner-Medwin D., Curtis A., Ginjaar I. B., den Dunnen J. T., Welch J. L., Butler T. J., Bakker E., et al. (1993b). Integrated study of 100 patients with Xp21 linked muscular dystrophy using clinical, genetic, immunochemical, and histopathological data. Part 1. Trends across the clinical groups. J. Med. Genet. 30, 728–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimura D., Sakai H., Sato T., Sato F., Nishimura S., Toyama-Sorimachi N., Bartsch J. W., Sehara-Fujisawa A. (2015). Roles of ADAM8 in elimination of injured muscle fibers prior to skeletal muscle regeneration. Mech. Dev. 135, 58–67. [DOI] [PubMed] [Google Scholar]
- Nitahara-Kasahara Y., Hayashita-Kinoh H., Chiyo T., Nishiyama A., Okada H., Takeda S., Okada T. (2014). Dystrophic mdx mice develop severe cardiac and respiratory dysfunction following genetic ablation of the anti-inflammatory cytokine IL-10. Hum. Mol. Genet. 23, 3990–4000. [DOI] [PubMed] [Google Scholar]
- Nonneman D. J., Brown-Brandl T., Jones S. A., Wiedmann R. T., Rohrer G. A. (2012). A defect in dystrophin causes a novel porcine stress syndrome. BMC Genomics 13, 233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odom G. L., Gregorevic P., Allen J. M., Finn E., Chamberlain J. S. (2008). Microutrophin delivery through rAAV6 increases lifespan and improves muscle function in dystrophic dystrophin/utrophin-deficient mice. Mol. Ther. 16, 1539–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odom G. L., Gregorevic P., Allen J. M., Chamberlain J. S. (2011). Gene therapy of mdx mice with large truncated dystrophins generated by recombination using rAAV6. Mol. Ther. 19, 36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohshima S., Shin J. H., Yuasa K., Nishiyama A., Kira J., Okada T., Takeda S. (2009). Transduction efficiency and immune response associated with the administration of AAV8 vector into dog skeletal muscle. Mol. Ther. 17, 73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opar A. (2012). Exon-skipping drug pulls ahead in muscular dystrophy field. Nat. Med. 18, 1314. [DOI] [PubMed] [Google Scholar]
- Ousterout D. G., Perez-Pinera P., Thakore P. I., Kabadi A. M., Brown M. T., Qin X., Fedrigo O., Mouly V., Tremblay J. P., Gersbach C. A. (2013). Reading frame correction by targeted genome editing restores dystrophin expression in cells from Duchenne muscular dystrophy patients. Mol. Ther. 21, 1718–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ousterout D. G., Kabadi A. M., Thakore P. I., Perez-Pinera P., Brown M. T., Majoros W. H., Reddy T. E., Gersbach C. A. (2014). Correction of dystrophin expression in cells from Duchenne Muscular Dystrophy patients through genomic excision of Exon 51 by zinc finger nucleases. Mol. Ther. [Epub ahead of print] 10.1038/mt.2014.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacak C. A., Mah C. S., Thattaliyath B. D., Conlon T. J., Lewis M. A., Cloutier D. E., Zolotukhin I., Tarantal A. F., Byrne B. J. (2006). Recombinant adeno-associated virus serotype 9 leads to preferential cardiac transduction in vivo. Circ. Res. 99, e3–e9. [DOI] [PubMed] [Google Scholar]
- Pan X., Yue Y., Zhang K., Lostal W., Shin J. H., Duan D. (2013). Long-term robust myocardial transduction of the dog heart from a peripheral vein by adeno-associated virus serotype-8. Hum. Gene Ther. 24, 584–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pane M., Lombardo M. E., Alfieri P., D’Amico A., Bianco F., Vasco G., Piccini G., Mallardi M., Romeo D. M., Ricotti V., et al. (2012). Attention deficit hyperactivity disorder and cognitive function in Duchenne muscular dystrophy: phenotype-genotype correlation. J. Pediatr. 161, 705–709e1. [DOI] [PubMed] [Google Scholar]
- Parames S. F., Coletta-Yudice E. D., Nogueira F. M., Nering de Sousa M. B., Hayashi M. A., Lima-Landman M. T., Lapa A. J., Souccar C. (2014). Altered acetylcholine release in the hippocampus of dystrophin-deficient mice. Neuroscience 269, 173–183. [DOI] [PubMed] [Google Scholar]
- Partridge T., Lu Q. L. (2008). The enigma of the ‘dystrophin revertant’ muscle fibre. In Recent Advances in Skeletal Muscle Differentiation (ed. Kunihiro T., Takeda S.), pp. 93–107 Kerala: Research Signpost. [Google Scholar]
- Pastoret C., Sebille A. (1995). Mdx mice show progressive weakness and muscle deterioration with age. J. Neurol. Sci. 129, 97–105. [DOI] [PubMed] [Google Scholar]
- Patria S. Y., Alimsardjono H., Nishio H., Takeshima Y., Nakamura H., Matsuo M. (1996). A case of Becker muscular dystrophy resulting from the skipping of four contiguous exons (71–74) of the dystrophin gene during mRNA maturation. Proc. Assoc. Am. Physicians 108, 308–314. [PubMed] [Google Scholar]
- Perronnet C., Chagneau C., Le Blanc P., Samson-Desvignes N., Mornet D., Laroche S., De La Porte S., Vaillend C. (2012). Upregulation of brain utrophin does not rescue behavioral alterations in dystrophin-deficient mice. Hum. Mol. Genet. 21, 2263–2276. [DOI] [PubMed] [Google Scholar]
- Phelps S. F., Hauser M. A., Cole N. M., Rafael J. A., Hinkle R. T., Faulkner J. A., Chamberlain J. S. (1995). Expression of full-length and truncated dystrophin mini-genes in transgenic mdx mice. Hum. Mol. Genet. 4, 1251–1258. [DOI] [PubMed] [Google Scholar]
- Poussin G., Mathis C., Alexopoulos L. G., Messinis D. E., Dulize R. H. J., Belcastro V., Melas I. N., Sakellaropoulos T., Rhrissorrakrai K., Bilal E., et al. (2014). The species translation challenge – a systems biology perspective on human and rat bronchial epithelial cells. Sci. Data 1, 140009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafael J. A., Tinsley J. M., Potter A. C., Deconinck A. E., Davies K. E. (1998). Skeletal muscle-specific expression of a utrophin transgene rescues utrophin-dystrophin deficient mice. Nat. Genet. 19, 79–82. [DOI] [PubMed] [Google Scholar]
- Rafael-Fortney J. A., Chimanji N. S., Schill K. E., Martin C. D., Murray J. D., Ganguly R., Stangland J. E., Tran T., Xu Y., Canan B. D., et al. (2011). Early treatment with lisinopril and spironolactone preserves cardiac and skeletal muscle in Duchenne muscular dystrophy mice. Circulation 124, 582–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ragot T., Vincent N., Chafey P., Vigne E., Gilgenkrantz H., Couton D., Cartaud J., Briand P., Kaplan J. C., Perricaudet M., et al. (1993). Efficient adenovirus-mediated transfer of a human minidystrophin gene to skeletal muscle of mdx mice. Nature 361, 647–650. [DOI] [PubMed] [Google Scholar]
- Rando T. A., Disatnik M. H., Zhou L. Z. (2000). Rescue of dystrophin expression in mdx mouse muscle by RNA/DNA oligonucleotides. Proc. Natl. Acad. Sci. USA 97, 5363–5368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricotti V., Roberts R. G., Muntoni F. (2011). Dystrophin and the brain. Dev. Med. Child Neurol. 53, 12. [DOI] [PubMed] [Google Scholar]
- Rodino-Klapac L. R., Haidet A. M., Kota J., Handy C., Kaspar B. K., Mendell J. R. (2009). Inhibition of myostatin with emphasis on follistatin as a therapy for muscle disease. Muscle Nerve 39, 283–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooney J. E., Welser J. V., Dechert M. A., Flintoff-Dye N. L., Kaufman S. J., Burkin D. J. (2006). Severe muscular dystrophy in mice that lack dystrophin and alpha7 integrin. J. Cell Sci. 119, 2185–2195. [DOI] [PubMed] [Google Scholar]
- Rousseau J., Chapdelaine P., Boisvert S., Almeida L. P., Corbeil J., Montpetit A., Tremblay J. P. (2011). Endonucleases: tools to correct the dystrophin gene. J. Gene Med. 13, 522–537. [DOI] [PubMed] [Google Scholar]
- Rutledge E. A., Halbert C. L., Russell D. W. (1998). Infectious clones and vectors derived from adeno-associated virus (AAV) serotypes other than AAV type 2. J. Virol. 72, 309–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco A., Mourkioti F., Tran R., Choi J., Llewellyn M., Kraft P., Shkreli M., Delp S., Pomerantz J. H., Artandi S. E., et al. (2010). Short telomeres and stem cell exhaustion model Duchenne muscular dystrophy in mdx/mTR mice. Cell 143, 1059–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampaolesi M., Blot S., D’Antona G., Granger N., Tonlorenzi R., Innocenzi A., Mognol P., Thibaud J. L., Galvez B. G., Barthélémy I., et al. (2006). Mesoangioblast stem cells ameliorate muscle function in dystrophic dogs. Nature 444, 574–579. [DOI] [PubMed] [Google Scholar]
- Sarig R., Mezger-Lallemand V., Gitelman I., Davis C., Fuchs O., Yaffe D., Nudel U. (1999). Targeted inactivation of Dp71, the major non-muscle product of the DMD gene: differential activity of the Dp71 promoter during development. Hum. Mol. Genet. 8, 1–10. [DOI] [PubMed] [Google Scholar]
- Schatzberg S. J., Olby N. J., Breen M., Anderson L. V., Langford C. F., Dickens H. F., Wilton S. D., Zeiss C. J., Binns M. M., Kornegay J. N., et al. (1999). Molecular analysis of a spontaneous dystrophin ‘knockout’ dog. Neuromuscul. Disord. 9, 289–295. [DOI] [PubMed] [Google Scholar]
- Schinkel S., Bauer R., Bekeredjian R., Stucka R., Rutschow D., Lochmüller H., Kleinschmidt J. A., Katus H. A., Müller O. J. (2012). Long-term preservation of cardiac structure and function after adeno-associated virus serotype 9-mediated microdystrophin gene transfer in mdx mice. Hum. Gene Ther. 23, 566–575. [DOI] [PubMed] [Google Scholar]
- Schmidt W. M., Uddin M. H., Dysek S., Moser-Thier K., Pirker C., Höger H., Ambros I. M., Ambros P. F., Berger W., Bittner R. E. (2011). DNA damage, somatic aneuploidy, and malignant sarcoma susceptibility in muscular dystrophies. PLoS Genet. 7, e1002042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekiguchi M., Zushida K., Yoshida M., Maekawa M., Kamichi S., Yoshida M., Sahara Y., Yuasa S., Takeda S., Wada K. (2009). A deficit of brain dystrophin impairs specific amygdala GABAergic transmission and enhances defensive behaviour in mice. Brain 132, 124–135. [DOI] [PubMed] [Google Scholar]
- Selsby J. T., Morine K. J., Pendrak K., Barton E. R., Sweeney H. L. (2012). Rescue of dystrophic skeletal muscle by PGC-1α involves a fast to slow fiber type shift in the mdx mouse. PLoS ONE 7, e30063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp N. J., Kornegay J. N., Van Camp S. D., Herbstreith M. H., Secore S. L., Kettle S., Hung W. Y., Constantinou C. D., Dykstra M. J., Roses A. D., et al. (1992). An error in dystrophin mRNA processing in golden retriever muscular dystrophy, an animal homologue of Duchenne muscular dystrophy. Genomics 13, 115–121. [DOI] [PubMed] [Google Scholar]
- Shelton G. D., Engvall E. (2005). Canine and feline models of human inherited muscle diseases. Neuromuscul. Disord. 15, 127–138. [DOI] [PubMed] [Google Scholar]
- Shimatsu Y., Katagiri K., Furuta T., Nakura M., Tanioka Y., Yuasa K., Tomohiro M., Kornegay J. N., Nonaka I., Takeda S. (2003). Canine X-linked muscular dystrophy in Japan (CXMDJ). Exp. Anim. 52, 93–97. [DOI] [PubMed] [Google Scholar]
- Shimatsu Y., Yoshimura M., Yuasa K., Urasawa N., Tomohiro M., Nakura M., Tanigawa M., Nakamura A., Takeda S. (2005). Major clinical and histopathological characteristics of canine X-linked muscular dystrophy in Japan, CXMDJ. Acta Myol. 24, 145–154. [PubMed] [Google Scholar]
- Shin J.-H., Bostick B., Yue Y., Duan D. (2010). Duchenne cardiomyopathy gene therapy. In Muscle Gene Therapy (ed. Duan D.), pp. 141–162 New York, NY: Springer Science + Business Media, LLC. [Google Scholar]
- Shin J. H., Bostick B., Yue Y., Hajjar R., Duan D. (2011a). SERCA2a gene transfer improves electrocardiographic performance in aged mdx mice. J. Transl. Med. 9, 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J. H., Nitahara-Kasahara Y., Hayashita-Kinoh H., Ohshima-Hosoyama S., Kinoshita K., Chiyo T., Okada H., Okada T., Takeda S. (2011b). Improvement of cardiac fibrosis in dystrophic mice by rAAV9-mediated microdystrophin transduction. Gene Ther. 18, 910–919. [DOI] [PubMed] [Google Scholar]
- Shin J. H., Yue Y., Smith B., Duan D. (2012a). Humoral immunity to AAV-6, 8, and 9 in normal and dystrophic dogs. Hum. Gene Ther. 23, 287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J. H., Yue Y., Srivastava A., Smith B., Lai Y., Duan D. (2012b). A simplified immune suppression scheme leads to persistent micro-dystrophin expression in Duchenne muscular dystrophy dogs. Hum. Gene Ther. 23, 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J. H., Greer B., Hakim C. H., Zhou Z., Chung Y. C., Duan Y., He Z., Duan D. (2013a). Quantitative phenotyping of Duchenne muscular dystrophy dogs by comprehensive gait analysis and overnight activity monitoring. PLoS ONE 8, e59875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin J. H., Pan X., Hakim C. H., Yang H. T., Yue Y., Zhang K., Terjung R. L., Duan D. (2013b). Microdystrophin ameliorates muscular dystrophy in the canine model of duchenne muscular dystrophy. Mol. Ther. 21, 750–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sicinski P., Geng Y., Ryder-Cook A. S., Barnard E. A., Darlison M. G., Barnard P. J. (1989). The molecular basis of muscular dystrophy in the mdx mouse: a point mutation. Science 244, 1578–1580. [DOI] [PubMed] [Google Scholar]
- Sifringer M., Uhlenberg B., Lammel S., Hanke R., Neumann B., von Moers A., Koch I., Speer A. (2004). Identification of transcripts from a subtraction library which might be responsible for the mild phenotype in an intrafamilially variable course of Duchenne muscular dystrophy. Hum. Genet. 114, 149–156. [DOI] [PubMed] [Google Scholar]
- Smith K. (2011). Feline muscular dystrophy: parallels between cats and people. Vet. Rec. 168, 507–508. [DOI] [PubMed] [Google Scholar]
- Smith B. F., Kornegay J. N., Duan D. (2007). Independent canine models of Duchenne muscular dystrophy due to intronic insertions of repetitive DNA. Mol. Ther. 15, S51. [Google Scholar]
- Smith B. F., Yue Y., Woods P. R., Kornegay J. N., Shin J. H., Williams R. R., Duan D. (2011). An intronic LINE-1 element insertion in the dystrophin gene aborts dystrophin expression and results in Duchenne-like muscular dystrophy in the corgi breed. Lab. Invest. 91, 216–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow W. M., Anderson J. E., Jakobson L. S. (2013). Neuropsychological and neurobehavioral functioning in Duchenne muscular dystrophy: a review. Neurosci. Biobehav. Rev. 37, 743–752. [DOI] [PubMed] [Google Scholar]
- Spitali P., Aartsma-Rus A. (2012). Splice modulating therapies for human disease. Cell 148, 1085–1088. [DOI] [PubMed] [Google Scholar]
- Spurney C., Shimizu R., Morgenroth L. P., Kolski H., Gordish-Dressman H., Clemens P. R., CINRG Investigators (2014). Cooperative International Neuromuscular Research Group Duchenne Natural History Study demonstrates insufficient diagnosis and treatment of cardiomyopathy in Duchenne muscular dystrophy. Muscle Nerve 50, 250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stedman H. H., Sweeney H. L., Shrager J. B., Maguire H. C., Panettieri R. A., Petrof B., Narusawa M., Leferovich J. M., Sladky J. T., Kelly A. M. (1991). The mdx mouse diaphragm reproduces the degenerative changes of Duchenne muscular dystrophy. Nature 352, 536–539. [DOI] [PubMed] [Google Scholar]
- Stenina M. A., Krivov L. I., Voevodin D. A., Yarygin V. N. (2013). Phenotypic differences between mdx black mice and mdx albino mice. Comparison of cytokine levels in the blood. Bull. Exp. Biol. Med. 155, 376–379. [DOI] [PubMed] [Google Scholar]
- Stinckens A., Georges M., Buys N. (2011). Mutations in the myostatin gene leading to hypermuscularity in mammals: indications for a similar mechanism in fish? Anim. Genet. 42, 229–234. [DOI] [PubMed] [Google Scholar]
- Taylor P. J., Betts G. A., Maroulis S., Gilissen C., Pedersen R. L., Mowat D. R., Johnston H. M., Buckley M. F. (2010). Dystrophin gene mutation location and the risk of cognitive impairment in Duchenne muscular dystrophy. PLoS ONE 5, e8803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas G. D. (2013). Functional muscle ischemia in Duchenne and Becker muscular dystrophy. Front. Physiol. 4, 381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinsley J. M., Potter A. C., Phelps S. R., Fisher R., Trickett J. I., Davies K. E. (1996). Amelioration of the dystrophic phenotype of mdx mice using a truncated utrophin transgene. Nature 384, 349–353. [DOI] [PubMed] [Google Scholar]
- Tinsley J., Deconinck N., Fisher R., Kahn D., Phelps S., Gillis J. M., Davies K. (1998). Expression of full-length utrophin prevents muscular dystrophy in mdx mice. Nat. Med. 4, 1441–1444. [DOI] [PubMed] [Google Scholar]
- Townsend D., Blankinship M. J., Allen J. M., Gregorevic P., Chamberlain J. S., Metzger J. M. (2007). Systemic administration of micro-dystrophin restores cardiac geometry and prevents dobutamine-induced cardiac pump failure. Mol. Ther. 15, 1086–1092. [DOI] [PubMed] [Google Scholar]
- Townsend D., Yasuda S., Li S., Chamberlain J. S., Metzger J. M. (2008). Emergent dilated cardiomyopathy caused by targeted repair of dystrophic skeletal muscle. Mol. Ther. 16, 832–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tozawa T., Itoh K., Yaoi T., Tando S., Umekage M., Dai H., Hosoi H., Fushiki S. (2012). The shortest isoform of dystrophin (Dp40) interacts with a group of presynaptic proteins to form a presumptive novel complex in the mouse brain. Mol. Neurobiol. 45, 287–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuffery-Giraud S., Béroud C., Leturcq F., Yaou R. B., Hamroun D., Michel-Calemard L., Moizard M. P., Bernard R., Cossée M., Boisseau P., et al. (2009). Genotype-phenotype analysis in 2,405 patients with a dystrophinopathy using the UMD-DMD database: a model of nationwide knowledgebase. Hum. Mutat. 30, 934–945. [DOI] [PubMed] [Google Scholar]
- Vaillend C., Ungerer A. (1999). Behavioral characterization of mdx3cv mice deficient in C-terminal dystrophins. Neuromuscul. Disord. 9, 296–304. [DOI] [PubMed] [Google Scholar]
- Vaillend C., Rendon A., Misslin R., Ungerer A. (1995). Influence of dystrophin-gene mutation on mdx mouse behavior. I. Retention deficits at long delays in spontaneous alternation and bar-pressing tasks. Behav. Genet. 25, 569–579. [DOI] [PubMed] [Google Scholar]
- Vaillend C., Billard J. M., Claudepierre T., Rendon A., Dutar P., Ungerer A. (1998). Spatial discrimination learning and CA1 hippocampal synaptic plasticity in mdx and mdx3cv mice lacking dystrophin gene products. Neuroscience 86, 53–66. [DOI] [PubMed] [Google Scholar]
- Vaillend C., Ungerer A., Billard J. M. (1999). Facilitated NMDA receptor-mediated synaptic plasticity in the hippocampal CA1 area of dystrophin-deficient mice. Synapse 33, 59–70. [DOI] [PubMed] [Google Scholar]
- Vaillend C., Billard J. M., Laroche S. (2004). Impaired long-term spatial and recognition memory and enhanced CA1 hippocampal LTP in the dystrophin-deficient Dmd(mdx) mouse. Neurobiol. Dis. 17, 10–20. [DOI] [PubMed] [Google Scholar]
- Vaillend C., Perronnet C., Ros C., Gruszczynski C., Goyenvalle A., Laroche S., Danos O., Garcia L., Peltekian E. (2010). Rescue of a dystrophin-like protein by exon skipping in vivo restores GABAA-receptor clustering in the hippocampus of the mdx mouse. Mol. Ther. 18, 1683–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine B. A., Cooper B. J. (1991). Canine X-linked muscular dystrophy: selective involvement of muscles in neonatal dogs. Neuromuscul. Disord. 1, 31–38. [DOI] [PubMed] [Google Scholar]
- Valentine B. A., Cooper B. J., Cummings J. F., deLahunta A. (1986). Progressive muscular dystrophy in a golden retriever dog: light microscope and ultrastructural features at 4 and 8 months. Acta Neuropathol. 71, 301–310. [DOI] [PubMed] [Google Scholar]
- Valentine B. A., Cooper B. J., de Lahunta A., O’Quinn R., Blue J. T. (1988). Canine X-linked muscular dystrophy. An animal model of Duchenne muscular dystrophy: clinical studies. J. Neurol. Sci. 88, 69–81. [DOI] [PubMed] [Google Scholar]
- Valentine B. A., Blue J. T., Cooper B. J. (1989a). The effect of exercise on canine dystrophic muscle. Ann. Neurol. 26, 588. [DOI] [PubMed] [Google Scholar]
- Valentine B. A., Cooper B. J., Gallagher E. A. (1989b). Intracellular calcium in canine muscle biopsies. J. Comp. Pathol. 100, 223–230. [DOI] [PubMed] [Google Scholar]
- Valentine B. A., Cummings J. F., Cooper B. J. (1989c). Development of Duchenne-type cardiomyopathy. Morphologic studies in a canine model. Am. J. Pathol. 135, 671–678. [PMC free article] [PubMed] [Google Scholar]
- Valentine B. A., Kornegay J. N., Cooper B. J. (1989d). Clinical electromyographic studies of canine X-linked muscular dystrophy. Am. J. Vet. Res. 50, 2145–2147. [PubMed] [Google Scholar]
- Valentine B. A., Blue J. T., Shelley S. M., Cooper B. J. (1990a). Increased serum alanine aminotransferase activity associated with muscle necrosis in the dog. J. Vet. Intern. Med. 4, 140–143. [DOI] [PubMed] [Google Scholar]
- Valentine B. A., Cooper B. J., Cummings J. F., de Lahunta A. (1990b). Canine X-linked muscular dystrophy: morphologic lesions. J. Neurol. Sci. 97, 1–23. [DOI] [PubMed] [Google Scholar]
- Valentine B. A., Chandler S. K., Cummings J. F., Cooper B. J. (1991). In vitro characteristics of normal and dystrophic skeletal muscle from dogs. Am. J. Vet. Res. 52, 104–107. [PubMed] [Google Scholar]
- Valentine B. A., Winand N. J., Pradhan D., Moise N. S., de Lahunta A., Kornegay J. N., Cooper B. J. (1992). Canine X-linked muscular dystrophy as an animal model of Duchenne muscular dystrophy: a review. Am. J. Med. Genet. 42, 352–356. [DOI] [PubMed] [Google Scholar]
- Vallese D., Negroni E., Duguez S., Ferry A., Trollet C., Aamiri A., Vosshenrich C. A., Füchtbauer E. M., Di Santo J. P., Vitiello L., et al. (2013). The Rag2−Il2rb−Dmd− mouse: a novel dystrophic and immunodeficient model to assess innovating therapeutic strategies for muscular dystrophies. Mol. Ther. 21, 1950–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Deutekom J. C., Janson A. A., Ginjaar I. B., Frankhuizen W. S., Aartsma-Rus A., Bremmer-Bout M., den Dunnen J. T., Koop K., van der Kooi A. J., Goemans N. M., et al. (2007). Local dystrophin restoration with antisense oligonucleotide PRO051. N. Engl. J. Med. 357, 2677–2686. [DOI] [PubMed] [Google Scholar]
- van Putten M., Hulsker M., Nadarajah V. D., van Heiningen S. H., van Huizen E., van Iterson M., Admiraal P., Messemaker T., den Dunnen J. T., ’t Hoen P. A., et al. (2012a). The effects of low levels of dystrophin on mouse muscle function and pathology. PLoS ONE 7, e31937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Putten M., Kumar D., Hulsker M., Hoogaars W. M., Plomp J. J., van Opstal A., van Iterson M., Admiraal P., van Ommen G. J., ’t Hoen P. A., et al. (2012b). Comparison of skeletal muscle pathology and motor function of dystrophin and utrophin deficient mouse strains. Neuromuscul. Disord. 22, 406–417. [DOI] [PubMed] [Google Scholar]
- van Putten M., Hulsker M., Young C., Nadarajah V. D., Heemskerk H., van der Weerd L., ’t Hoen P. A., van Ommen G. J., Aartsma-Rus A. M. (2013). Low dystrophin levels increase survival and improve muscle pathology and function in dystrophin/utrophin double-knockout mice. FASEB J. 27, 2484–2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varki A. (2010). Colloquium paper: uniquely human evolution of sialic acid genetics and biology. Proc. Natl. Acad. Sci. USA 107 Suppl. 2, 8939–8946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhaart I. E., Aartsma-Rus A. (2012). Gene therapy for Duchenne muscular dystrophy. Curr. Opin. Neurol. 25, 588–596. [DOI] [PubMed] [Google Scholar]
- Vulin A., Barthélémy I., Goyenvalle A., Thibaud J. L., Beley C., Griffith G., Benchaouir R., le Hir M., Unterfinger Y., Lorain S., et al. (2012). Muscle function recovery in golden retriever muscular dystrophy after AAV1-U7 exon skipping. Mol. Ther. 20, 2120–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner K. R., McPherron A. C., Winik N., Lee S. J. (2002). Loss of myostatin attenuates severity of muscular dystrophy in mdx mice. Ann. Neurol. 52, 832–836. [DOI] [PubMed] [Google Scholar]
- Wakefield P. M., Tinsley J. M., Wood M. J., Gilbert R., Karpati G., Davies K. E. (2000). Prevention of the dystrophic phenotype in dystrophin/utrophin-deficient muscle following adenovirus-mediated transfer of a utrophin minigene. Gene Ther. 7, 201–204. [DOI] [PubMed] [Google Scholar]
- Wakefield S. E., Dimberg E. L., Moore S. A., Tseng B. S. (2009). Dystrophinopathy presenting with arrhythmia in an asymptomatic 34-year-old man: a case report. J. Med. Case Rep. 3, 8625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walmsley G. L., Arechavala-Gomeza V., Fernandez-Fuente M., Burke M. M., Nagel N., Holder A., Stanley R., Chandler K., Marks S. L., Muntoni F., et al. (2010). A Duchenne muscular dystrophy gene hot spot mutation in dystrophin-deficient Cavalier King Charles spaniels is amenable to exon 51 skipping. PLoS ONE 5, e8647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh S., Nygren J., Pontén A., Jovinge S. (2011). Myogenic reprogramming of bone marrow derived cells in a W41Dmd(mdx) deficient mouse model. PLoS ONE 6, e27500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Li J., Xiao X. (2000). Adeno-associated virus vector carrying human minidystrophin genes effectively ameliorates muscular dystrophy in mdx mouse model. Proc. Natl. Acad. Sci. USA 97, 13714–13719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Zhu T., Qiao C., Zhou L., Wang B., Zhang J., Chen C., Li J., Xiao X. (2005). Adeno-associated virus serotype 8 efficiently delivers genes to muscle and heart. Nat. Biotechnol. 23, 321–328. [DOI] [PubMed] [Google Scholar]
- Wang Z., Kuhr C. S., Allen J. M., Blankinship M., Gregorevic P., Chamberlain J. S., Tapscott S. J., Storb R. (2007). Sustained AAV-mediated dystrophin expression in a canine model of Duchenne muscular dystrophy with a brief course of immunosuppression. Mol. Ther. 15, 1160–1166. [DOI] [PubMed] [Google Scholar]
- Wang Y., Marino-Enriquez A., Bennett R. R., Zhu M., Shen Y., Eilers G., Lee J. C., Henze J., Fletcher B. S., Gu Z., et al. (2014). Dystrophin is a tumor suppressor in human cancers with myogenic programs. Nat. Genet. 46, 601–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner L. E., DelloRusso C., Crawford R. W., Rybakova I. N., Patel J. R., Ervasti J. M., Chamberlain J. S. (2002). Expression of Dp260 in muscle tethers the actin cytoskeleton to the dystrophin-glycoprotein complex and partially prevents dystrophy. Hum. Mol. Genet. 11, 1095–1105. [DOI] [PubMed] [Google Scholar]
- Wasala N. B., Bostick B., Yue Y., Duan D. (2013). Exclusive skeletal muscle correction does not modulate dystrophic heart disease in the aged mdx model of Duchenne cardiomyopathy. Hum. Mol. Genet. 22, 2634–2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wein N., Vulin A., Falzarano M. S., Szigyarto C. A., Maiti B., Findlay A., Heller K. N., Uhlén M., Bakthavachalu B., Messina S., et al. (2014). Translation from a DMD exon 5 IRES results in a functional dystrophin isoform that attenuates dystrophinopathy in humans and mice. Nat. Med. 20, 992–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells D. J., Wells K. E., Asante E. A., Turner G., Sunada Y., Campbell K. P., Walsh F. S., Dickson G. (1995). Expression of human full-length and minidystrophin in transgenic mdx mice: implications for gene therapy of Duchenne muscular dystrophy. Hum. Mol. Genet. 4, 1245–1250. [DOI] [PubMed] [Google Scholar]
- Wentink G. H., van der Linde-sipman J. S., Meijer A. E. F. H., Kamphuisen H. A. C., van Vorstenbosch C. J. A. H. V., Hartman W., Hendriks H. J. (1972). Myopathy with a possible recessive X-linked inheritance in a litter of Irish Terriers. Vet. Pathol. 9, 328–349. [DOI] [PubMed] [Google Scholar]
- West N. A., Yang M. L., Weitzenkamp D. A., Andrews J., Meaney F. J., Oleszek J., Miller L. A., Matthews D., DiGuiseppi C. (2013). Patterns of growth in ambulatory males with Duchenne muscular dystrophy. J. Pediatr. 163, 1759–1763e1. [DOI] [PubMed] [Google Scholar]
- Winand N. J., Edwards M., Pradhan D., Berian C. A., Cooper B. J. (1994a). Deletion of the dystrophin muscle promoter in feline muscular dystrophy. Neuromuscul. Disord. 4, 433–445. [DOI] [PubMed] [Google Scholar]
- Winand N. J., Pradhan D., Cooper B. J. (1994b). Molecular characterization of severe Duchenne-type muscular dystrophy in a family of Rottweiler dogs. In Molecular Mechanism of Neuromuscular Disease. Tucson, AZ: Muscular Dystrophy Association. [Google Scholar]
- Wood M. J. (2013). To skip or not to skip: that is the question for Duchenne muscular dystrophy. Mol. Ther. 21, 2131–2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu B., Moulton H. M., Iversen P. L., Jiang J., Li J., Li J., Spurney C. F., Sali A., Guerron A. D., Nagaraju K., et al. (2008). Effective rescue of dystrophin improves cardiac function in dystrophin-deficient mice by a modified morpholino oligomer. Proc. Natl. Acad. Sci. USA 105, 14814–14819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu B., Li Y., Morcos P. A., Doran T. J., Lu P., Lu Q. L. (2009). Octa-guanidine morpholino restores dystrophin expression in cardiac and skeletal muscles and ameliorates pathology in dystrophic mdx mice. Mol. Ther. 17, 864–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu B., Xiao B., Cloer C., Shaban M., Sali A., Lu P., Li J., Nagaraju K., Xiao X., Lu Q. L. (2011). One-year treatment of morpholino antisense oligomer improves skeletal and cardiac muscle functions in dystrophic mdx mice. Mol. Ther. 19, 576–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R., Camboni M., Martin P. T. (2007). Postnatal overexpression of the CT GalNAc transferase inhibits muscular dystrophy in mdx mice without altering muscle growth or neuromuscular development: evidence for a utrophin-independent mechanism. Neuromuscul. Disord. 17, 209–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto K., Yamada D., Kabuta T., Takahashi A., Wada K., Sekiguchi M. (2010). Reduction of abnormal behavioral response to brief restraint by information from other mice in dystrophin-deficient mdx mice. Neuromuscul. Disord. 20, 505–511. [DOI] [PubMed] [Google Scholar]
- Yang H. T., Shin J. H., Hakim C. H., Pan X., Terjung R. L., Duan D. (2012). Dystrophin deficiency compromises force production of the extensor carpi ulnaris muscle in the canine model of Duchenne muscular dystrophy. PLoS ONE 7, e44438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin H., Moulton H. M., Seow Y., Boyd C., Boutilier J., Iverson P., Wood M. J. (2008). Cell-penetrating peptide-conjugated antisense oligonucleotides restore systemic muscle and cardiac dystrophin expression and function. Hum. Mol. Genet. 17, 3909–3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin H., Saleh A. F., Betts C., Camelliti P., Seow Y., Ashraf S., Arzumanov A., Hammond S., Merritt T., Gait M. J., et al. (2011). Pip5 transduction peptides direct high efficiency oligonucleotide-mediated dystrophin exon skipping in heart and phenotypic correction in mdx mice. Mol. Ther. 19, 1295–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokota T., Lu Q. L., Partridge T., Kobayashi M., Nakamura A., Takeda S., Hoffman E. (2009). Efficacy of systemic morpholino exon-skipping in Duchenne dystrophy dogs. Ann. Neurol. 65, 667–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshimura M., Sakamoto M., Ikemoto M., Mochizuki Y., Yuasa K., Miyagoe-Suzuki Y., Takeda S. (2004). AAV vector-mediated microdystrophin expression in a relatively small percentage of mdx myofibers improved the mdx phenotype. Mol. Ther. 10, 821–828. [DOI] [PubMed] [Google Scholar]
- Yuasa K., Yoshimura M., Urasawa N., Ohshima S., Howell J. M., Nakamura A., Hijikata T., Miyagoe-Suzuki Y., Takeda S. (2007). Injection of a recombinant AAV serotype 2 into canine skeletal muscles evokes strong immune responses against transgene products. Gene Ther. 14, 1249–1260. [DOI] [PubMed] [Google Scholar]
- Yue Y., Li Z., Harper S. Q., Davisson R. L., Chamberlain J. S., Duan D. (2003). Microdystrophin gene therapy of cardiomyopathy restores dystrophin-glycoprotein complex and improves sarcolemma integrity in the mdx mouse heart. Circulation 108, 1626–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue Y., Skimming J. W., Liu M., Strawn T., Duan D. (2004). Full-length dystrophin expression in half of the heart cells ameliorates beta-isoproterenol-induced cardiomyopathy in mdx mice. Hum. Mol. Genet. 13, 1669–1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue Y., Ghosh A., Long C., Bostick B., Smith B. F., Kornegay J. N., Duan D. (2008). A single intravenous injection of adeno-associated virus serotype-9 leads to whole body skeletal muscle transduction in dogs. Mol. Ther. 16, 1944–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yugeta N., Urasawa N., Fujii Y., Yoshimura M., Yuasa K., Wada M. R., Nakura M., Shimatsu Y., Tomohiro M., Takahashi A., et al. (2006). Cardiac involvement in Beagle-based canine X-linked muscular dystrophy in Japan (CXMDJ): electrocardiographic, echocardiographic, and morphologic studies. BMC Cardiovasc. Disord. 6, 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatz M., Pavanello R. C., Lazar M., Yamamoto G. L., Lourenço N. C., Cerqueira A., Nogueira L., Vainzof M. (2014). Milder course in Duchenne patients with nonsense mutations and no muscle dystrophin. Neuromuscul. Disord. 24, 986–989. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Duan D. (2012). Novel mini-dystrophin gene dual adeno-associated virus vectors restore neuronal nitric oxide synthase expression at the sarcolemma. Hum. Gene Ther. 23, 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Yue Y., Li L., Hakim C. H., Zhang K., Thomas G. D., Duan D. (2013). Dual AAV therapy ameliorates exercise-induced muscle injury and functional ischemia in murine models of Duchenne muscular dystrophy. Hum. Mol. Genet. 22, 3720–3729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L., Rafael-Fortney J. A., Huang P., Zhao X. S., Cheng G., Zhou X., Kaminski H. J., Liu L., Ransohoff R. M. (2008). Haploinsufficiency of utrophin gene worsens skeletal muscle inflammation and fibrosis in mdx mice. J. Neurol. Sci. 264, 106–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucconi E., Valadares M. C., Vieira N. M., Bueno C. R., Jr, Secco M., Jazedje T., da Silva H. C., Vainzof M., Zatz M. (2010). Ringo: discordance between the molecular and clinical manifestation in a golden retriever muscular dystrophy dog. Neuromuscul. Disord. 20, 64–70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.