Abstract
Microsoft's Kinect for Xbox 360 virtual reality (VR) video games are promising rehabilitation options because they involve motivating, full-body movement practice. However, these games were designed for recreational use, which creates challenges for clinical implementation. Busy clinicians require decision-making support to inform game selection and implementation that address individual therapeutic goals. This article describes the development and preliminary evaluation of a knowledge translation (KT) resource to support clinical decision making about selection and use of Kinect games in physical therapy. The knowledge-to-action framework guided the development of the Kinecting With Clinicians (KWiC) resource. Five physical therapists with VR and video game expertise analyzed the Kinect Adventure games. A consensus-building method was used to arrive at categories to organize clinically relevant attributes guiding game selection and game play. The process and results of an exploratory usability evaluation of the KWiC resource by clinicians through interviews and focus groups at 4 clinical sites is described. Subsequent steps in the evaluation and KT process are proposed, including making the KWiC resource Web-based and evaluating the utility of the online resource in clinical practice.
The rapidly developing field of virtual reality (VR) offers substantial promise for rehabilitation research and clinical practice. Virtual reality systems use hardware and software to create interactive simulations that engage users in realistic environments.1 Platforms range from expensive, immersive, laboratory-based systems to low-cost, off-the-shelf video games. Therapy that incorporates the use of VR is currently used to target clinical outcomes in many patient populations. Systematic reviews summarizing the evidence in this diverse field support the use of VR in upper limb rehabilitation2,3 and call for ongoing, high-quality methodological research to support its optimal use in practice.4–8 Yet, evidence for effectiveness is only one relevant piece of the puzzle. Clinicians also require support in the form of knowledge translation (KT) resources to inform decisions about how to use VR in clinical practice.9,10 Developing accessible, clinically relevant KT resources may enhance integration of VR systems into rehabilitation.
Using KT to address the evidence-to-practice gap is a key priority for both the National Institute on Disability and Rehabilitation Research (NIDRR)11,12 and the Canadian Institutes of Health and Research (CIHR). Knowledge translation is defined by CIHR as “a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically-sound application of knowledge to improve the health of Canadians, provide more effective health services and products and strengthen the health care system.”13 Traditional KT strategies include the use of printed educational materials, audit and feedback, and tailored interventions.14 Although little is known about which specific KT strategies are most effective in physical therapy,15 active strategies involving multiple methods have the greatest support.14,16 In addition, using the Internet as a platform for KT resources or tools is becoming increasingly popular because of the potential to lead large numbers of individuals through self-paced, self-directed learning of up-to-date multimedia content.17,18
Accessible, user-friendly KT resources to support clinical decision making about VR integration into practice are needed because clinicians worldwide are embracing the use of these systems.19–21 A focus group reported that video gaming is the most prevalent assistive technology used by therapists in stroke rehabilitation in the United Kingdom.21 In Australia, 76% of stroke rehabilitation units have access to the Nintendo Wii (Nintendo, Redmond, Washington).19 A survey of occupational therapist and physical therapists working in a Canadian rehabilitation hospital showed that 76% of respondents believed the Wii to be beneficial for inpatient clients, with 73% agreeing that its use could enhance client adherence to intervention programs.20 However, platforms and games are released at a pace surpassing that at which research exploring their utility can be conducted and disseminated. For example, the Wii was released in 2007, with the first case report with application to rehabilitation published in 200822 and a game analysis to guide clinical decision making disseminated in 2011.23 However, the evidence for this system compared with standard of care is only recently becoming available20,24–34 and is inconclusive.
The newest game console in the clinical environment is Microsoft's Kinect (Microsoft Inc, Redmond, Washington). Its infrared sensor allows full-body, motion-controlled play. The Kinect sensor, designed for use with Xbox 360 games, removes the potential for “cheating” inherent to the Wiimote (Wii remote), although it has limitations recognizing users in seated positions. Evidence is emerging for use of the Kinect Xbox games as rehabilitation interventions for diverse populations, including adults with stroke28,35 and multiple sclerosis,36 children with cerebral palsy (CP)37 and ataxia,38 and adolescents with ankle sprains.39 This early literature demonstrates benefits for individuals undergoing training using the Kinect toward a variety of short-term outcomes related to upper limb use, balance, and mobility.
Despite the growing evidence in support of the Kinect and other VR systems as an adjunct to physical therapy, many factors affect translation of this technology into practice.40 Physical therapists and occupational therapists in brain injury rehabilitation identified barriers in knowledge and time as constraints to using the Interactive Rehabilitation Exercise System (IREX).9 Even though they perceived the IREX as useful and applicable, they had difficulty with implementation into practice. Increased use of this VR system was facilitated by knowledge translation initiatives.9 Levac and Miller10 found that physical therapists using the Wii in a pediatric brain injury setting felt a strong responsibility to learn how to use the system appropriately and wanted education on how to do so. Lack of time and knowledge appear to be the main barriers to implementing VR video games in practice.
Given the history of difficulties adopting previous VR and video game technologies, we sought to proactively address these barriers with the creation of a knowledge resource pertaining to the Kinect with the aim of reducing the knowledge barrier directly and the time barrier indirectly. We focused on the Kinect because we speculate that its hands-free, camera-based interaction will appeal to clinicians who may be inspired to integrate these games into clinical practice if they had support to inform decisions about game use within goal-oriented rehabilitation programs. Skills in any VR implementation include decision making about matching the intervention to the client, implementation of treatment parameters, and progression through different levels of the game or task.41 A KT resource to support development of these competencies may maximize the potential benefits of VR use for clients.9,41 Importantly, we view the knowledge resource as a tool to bridge the gap between the technology and its implementation in physical therapy.
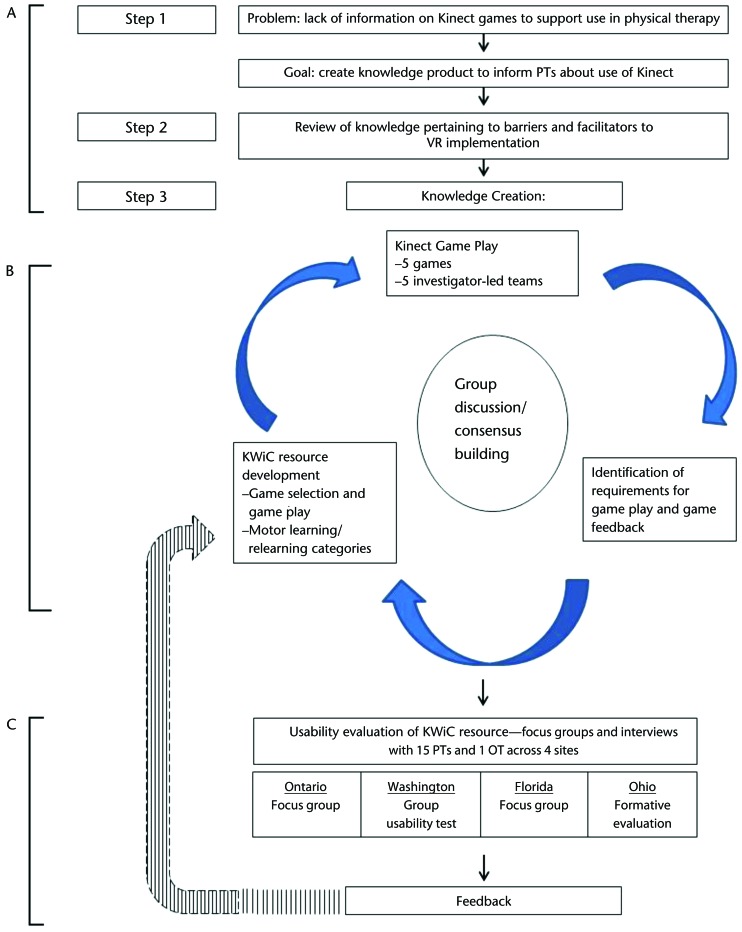
Indeed, successful translation of an innovative technology such as VR into clinical practice depends partially on the availability and quality of appropriate KT resources for that new technology. Creation of those KT resources may best be accomplished with a framework to guide development and evaluation.42,43 The knowledge-to-action (KTA) cycle42 (Fig. 1) guides researchers in the process of creating, implementing, and evaluating sustainable KT initiatives. In this article, we describe our use of the KTA framework to guide the development, preliminary usability evaluation, and proposed evaluation of a resource designed to support clinical decision making about selection and implementation of Kinect games for rehabilitation.
Figure 1.
The knowledge-to-action framework. Reprinted with permission of John Wiley & Sons from: Strauss SE, Tetroe J, Graham ID, eds. Knowledge Translation in Health Care: Moving From Evidence to Practice. 2nd ed. Chichester, United Kingdom: John Wiley & Sons Ltd; 2013.
Methods
The KTA cycle guided our approach to the development and planned eventual integration into practice of a knowledge resource about Kinect games in rehabilitation. The KTA framework contains 2 components. The first is a knowledge creation cycle in which information is synthesized to create knowledge products, resources, or tools that are directed toward the needs of specific end users. Next, an action cycle outlines distinct steps in activities inherent to translating the knowledge product into practice, including monitoring and evaluating knowledge use.42 The KTA framework is illustrated in Figure 1. The specific methodology we used for the assessment of the knowledge resource was 4 usability studies conducted as either focus groups or formative evaluations with subject matter experts. The KTA application, namely identifying the problem and creating a knowledge resource, is presented in Figure 2 (parts A and B) and the usability methodology is presented in Figure 2C.
Figure 2.
Knowledge translation-to-action cycle and study method: (A) identifying the problem, (B) creating the knowledge resource, and (C) usability methodology. VR=virtual reality, KWiC=Kinecting With Clinicians, PT=physical therapist, OT=occupational therapist.
Identifying the Problem
Our approach began with the first step in the action cycle: identifying the problem (Figs. 1A and 2A). In this case, the problem was a lack of information to support use of Kinect for Xbox 360 games in physical therapy toward a variety of clinical goals. When we surveyed the literature, there was no resource to support clinicians' use of Kinect in practice. The authors, a group of physical therapists with VR and video game expertise and publication histories in different areas of this field, were invited by one researcher (J.E.D.) to collaborate on this project. We had all observed anecdotal interest in Kinect use among our clinician colleagues and valued its potential in rehabilitation. However, we were familiar with the literature identifying barriers to VR adoption, which suggests that overburdened clinicians were unlikely to have the time or guidance to fully explore the potential of this gaming platform.9,10 Our goal, therefore, was to create an accessible and clinically relevant knowledge product to inform physical therapists about integrating the Kinect system into practice. Recognizing that the information needed to be applicable across a range of practice settings and client populations, an iterative process to product development was planned, understanding that final content and format would emerge through our team interactions and feedback from end users.44
We then sought to identify and review the knowledge relevant to the problem. This knowledge included information described earlier about barriers and facilitators to VR implementation, which motivated our vision of the product as being easily accessible and providing synthesized, clinically relevant knowledge about Kinect game play in written and video formats.
Creating the Knowledge Resource
The knowledge creation component (Figs. 1 and 2B) began with synthesizing the knowledge and experience from previous work in this area, including a Wii game analysis,23 a classification framework of pediatric VR systems,45,46 experimental studies using and adapting the Kinect games for rehabilitation,47,48 and a systematic framework to guide clinical decision making in gaming choices for therapeutic use.49 We then familiarized ourselves with Kinect game play. Three Kinect games believed to be representative of a variety of movements and virtual environments were selected: Soccer (Sports Season One), Boxing (Sports Season One), and 20,000 Leaks (Adventures). The games were played individually and with each investigator's clinical or research teams. We documented the movements required, the type of feedback provided by the games, and other details that we thought would be relevant to clinicians. These initial observations informed the early version of the content and format of the knowledge product, which we called the Kinecting With Clinicians (KWiC) resource.
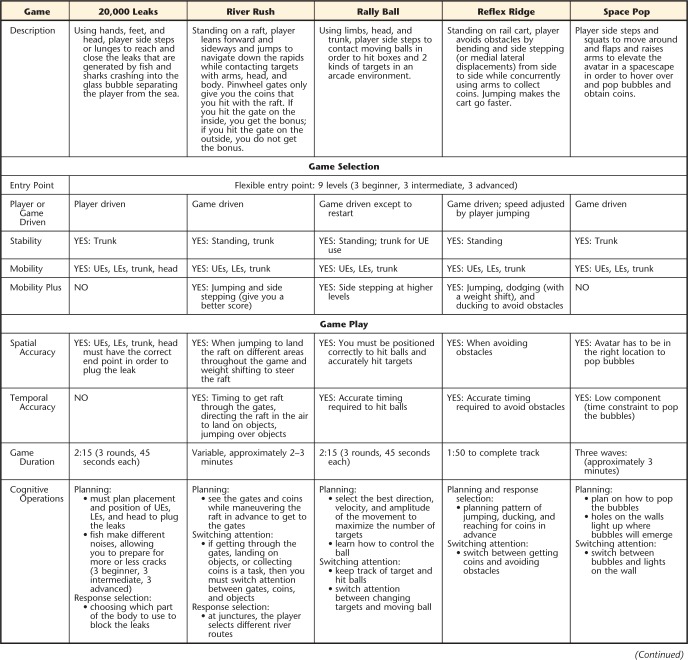
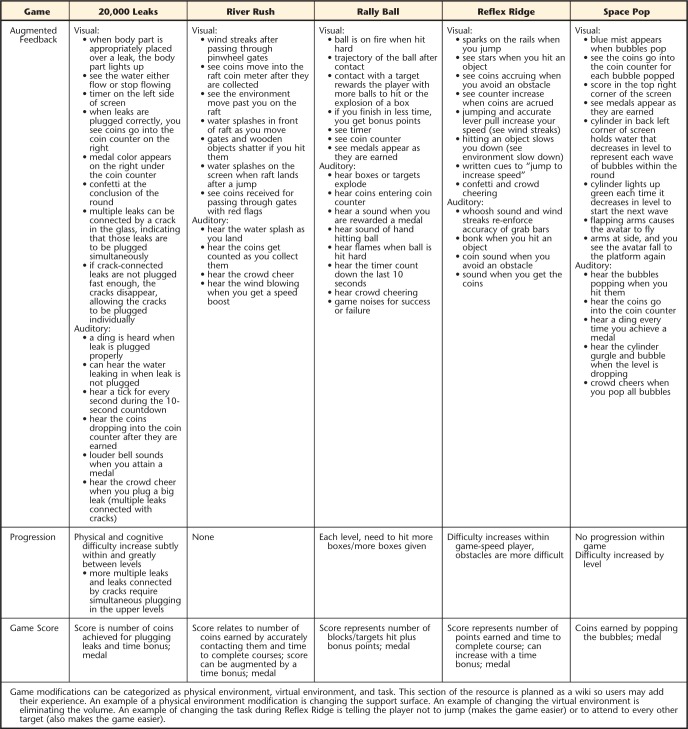
We organized the KWiC resource (Appendix 1) into 2 sections: (1) information to inform game selection (ie, what game would a clinician select as most relevant for a particular goal or client) and (2) information to inform game play (ie, specific details about playing an individual game). We then decided on a list of operationally defined game characteristics by which to organize the information in the resource (Tab. 1). Next, we analyzed the 5 Kinect Adventure games, as they come bundled with the purchase of the console and offer a variety of game play options. We developed a print version of the KWiC resource as well as videos illustrating game play of each of the 5 games at beginner and advanced levels.
Table 1.
Operational Definitions for Categories in the Kinecting With Clinicians (KWiC) Resource
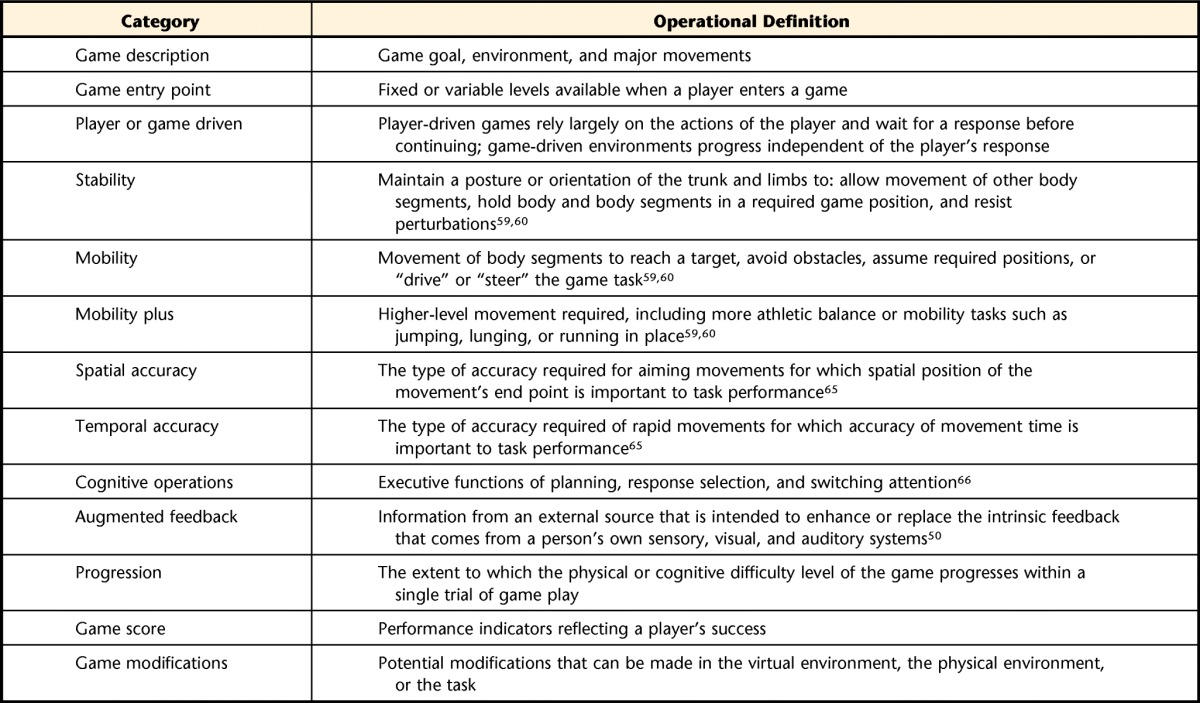
Resource categories whose therapeutic importance became apparent to us through iterations of game analysis were agreed on after discussion and consensus among the group: game description, entry point, player or game driven, game score, game modifications, and progression. Typically, one member would suggest a category, then the team would discuss their understanding of that construct, its potential importance for clinicians, and how to name, define, and structure it. Each author scrutinized the consensus definition during the next iteration of game analysis, and any needed changes were discussed and agreed on at the following meeting (Fig. 2B).
Other specific therapeutic components of video games were derived from previous work9,20,42–44 following the same iterative and consensus forming approach (Fig. 2B,) but, in this case, informed by motor learning and motor control principles.50 Virtual reality, including off-the-shelf games, is appealing as a therapeutic tool, in part, because it can mimic many of the task and environmental features one would modulate in a motor learning treatment approach.51,52 This approach emphasizes, among other things, active involvement by the patient, the interrelatedness of posture and movement, context (person, task or environment)–specific training or retraining, and appropriate feedback.53,54 This approach originated in neurological rehabilitation, but its application has been advocated across practice areas55 and across the life span.56,57
The KWiC categories “Stability” and “Mobility” recognize the importance of the interrelatedness of posture and movement53,58 and were defined from Gentile's constructs of body stability versus body transport,59 the idea that gait and other human mobility require both stability (not falling) and mobility (moving in the desired direction),60 and the construct of proximal stability to allow more effective distal mobility.60 “Mobility plus” was a term we coined to describe those motions that we felt were more demanding than stepping or walking, such as jumping, lunging, and tasks performed in single-leg stance. Motor learning also emphasizes that practice should be structured around analysis of the person and the task or environment and with attention to feedback.53,58,61 Spatial and temporal accuracy are crucial regulatory conditions of the environment that must be structured appropriately into relearning of motor skills,58 making the accuracy demands inherent to individual games important information for clinicians. The definitions we agreed on were taken from the motor control literature50 (Tab. 1). The ability to augment feedback beyond the means available in more typical therapy sessions has been recognized as a powerful therapeutic advantage of virtual reality,51,62,63 thus its inclusion as a consideration in this resource. Likewise, the additional cognitive demands imposed by game play are recognized64 and thus were included.
Usability Evaluation of the KWiC Knowledge Resource
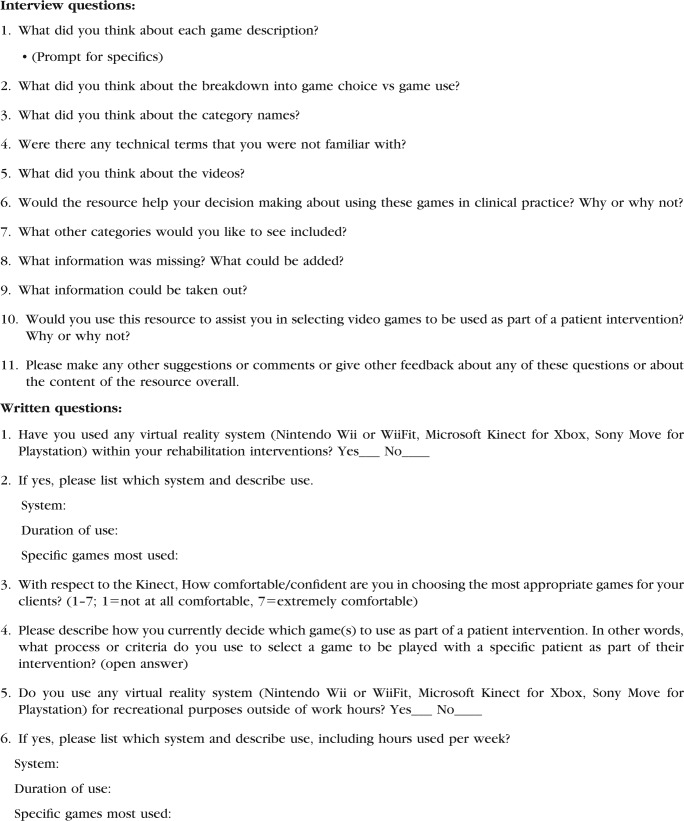
Although the subsequent steps of the KTA action cycle focus on integrating knowledge into practice, we first needed to get feedback from end users about the print and video content of the KWiC product. This is an important step in the development of a new knowledge product, particularly because we had not consulted with end users thus far. We used an exploratory, preliminary usability evaluation44 methodology with institutional review board/research ethics board approval from our respective institutions. The exploratory usability evaluation involved seeking feedback about the resource from end users through interviews and focus groups at each of our sites.
The 4 sites used the same questionnaire to obtain written demographic information from all participants. Participants were provided with a paper or electronic copy of the KWiC resource and access to the game play videos (hosted on a private YouTube channel). Although all sites used the same questions, the process of familiarizing participants with the resource and obtaining feedback varied slightly. At each site, researchers documented feedback during the session. The list of questions asked during the focus groups or interviews is presented in Appendix 2. The sites differed in their methodology; Figure 2C outlines the process. Ontario and Florida used focus groups, and Washington and Ohio conducted individual interviews. Ohio used a formative evaluation methodology67 with experts in game analysis.
At 2 sites (Ohio and Ontario), participants perused the resource and videos on their own prior to meeting with the researcher. At the Florida site, participants were provided with the video links prior to the meeting, and Kinect games were played in person with the researcher prior to introducing and obtaining feedback on the resource. At the Washington site, participants were provided with the resource and shown the videos at the focus group. Participants were asked to read through the game descriptions on the paper resource and select a game that they thought would be most appropriate for a typical client who they may see in their practice prior to participating in the facilitated discussion.
Following the focus groups or interviews, each researcher summarized the feedback obtained per question. Three group discussions were used to synthesize the findings across sites. These findings were then consolidated into Tables 2, 3, and 4. User responses to the quality and clarity of the KWiC were coded as changes to the resource or verification of existing plans. Decisions about changes to the resource were based on the frequency of comments. When there was controversy regarding the comments, the group decided to evaluate that aspect in future studies.
Table 2.
Participant Demographicsa
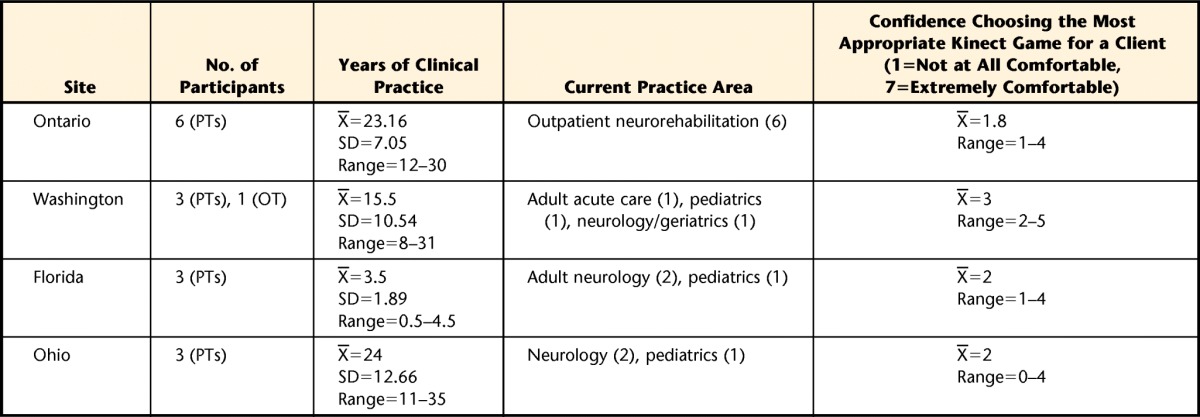
PT=physical therapist, OT=occupational therapist.
Table 3.
Responses to Specific Questions
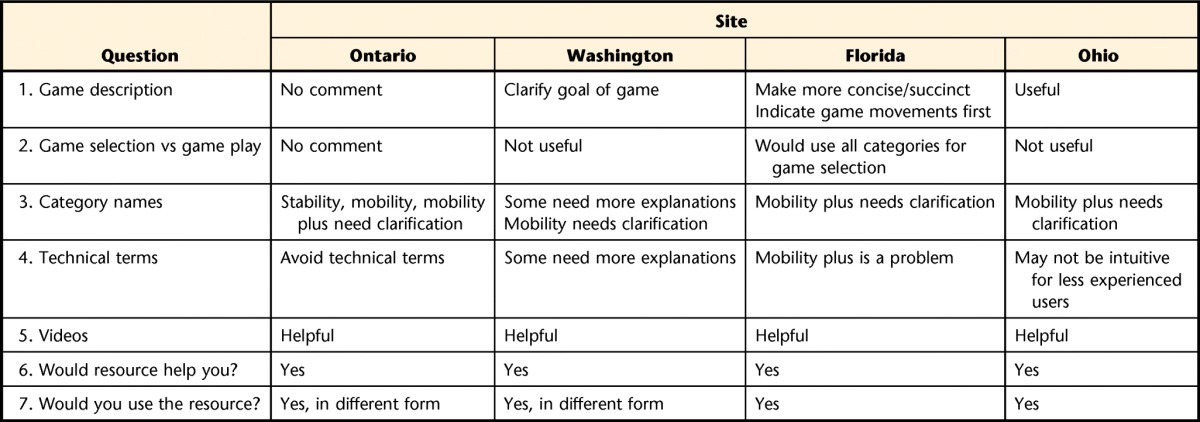
Table 4.
Responses to Open-Ended Questions

Results of the Exploratory Usability Evaluation
Participant Demographics
Feedback was obtained from 16 participants. Their demographics are summarized in Table 2. Participants had an average of 17.75 years of clinical experience (SD=11.52).
Participants had greater experience using the Wii and relatively little expertise implementing Kinect games in clinical practice. At the Ontario site, 3 therapists had previously used the Wii with clients in clinical practice, and the same therapists had experience using Wii games recreationally. Two participants had used the Kinect recreationally. However, none had used this system with their rehabilitation clients. Ohio site participants were more familiar with Wii than Kinect, although 1 participant did use Kinect recreationally. All participants reported that their method of game choice was clinical reasoning based on how well the games matched the clients' goals and therapeutic needs. In Florida, all participants had familiarity with VR video games. Two of the 3 therapists had used VR in the clinic, and 1 participant had previously used the Kinect in the clinic. Participants reported that their current method of decision making to use games is to determine patient impairments and select games that appear to meet these needs. Washington site therapists were all familiar with the Wii, and only 1 therapist had used the Kinect for recreational purposes. These therapists reported that they consider patient safety, interest in games, and their own prior experience with the games when making decisions.
Feedback Summaries by Site
Decisions About Changes to the KWiC Resource
In deciding how to interpret the feedback across the 4 sites, we focused primarily on the comments that were similar across the groups.
Changes
Game description: will be standardized by the order and detail of information across each (in terms of starting with goal of the game or the movements required).
Game selection versus game play: will be further evaluated using the Web interface when the resource will be tested in the context of clinical decision making.
Category names: the labels and definitions of “Stability,” “Mobility,” and “Mobility plus” need to be renamed and revised for clarity using labels that are consistent with clinicians' terminology.68
Verification and Enhancements
Videos were uniformly viewed as an important component of the KWiC resource. Advanced-level videos will be reviewed to better illustrate the movement potential of this challenge level. Filming more videos illustrating players having difficulty with movements required for the games will be considered in order to facilitate clinician problem solving.
Participants uniformly reported positive responses about using the KWiC resource. It is anticipated that the Web implementation will make it user-friendly.
Comments regarding categories and information that could be added were numerous and specific. Clinicians requested ranking information for the games in the different categories, as well as including a decision-making algorithm in the online resource to facilitate finding the games that might best fit a particular goal or client population.
Discussion
Given the rapid development of motion capture technology and the decline in the cost of video game consoles, we identified a need to support clinicians in their efforts to adopt these technologies into practice. This need is specifically relevant for off-the shelf consoles such as the Kinect for Xbox 360, where the games were not designed for rehabilitation. We used the KTA framework to inform the development and eventual evaluation of a knowledge product to facilitate clinical integration of Kinect games into practice. This article describes the first step in this research program, a preliminary usability evaluation of the KWiC resource, with clinicians at 4 clinical sites. Our assumption that clinicians want a knowledge resource was universally supported by the participants, solidifying our plans to create a Web-based, video-enhanced resource. We learned the importance of using familiar and standardized terminology. The feedback obtained through this evaluation will guide decisions about changes to be made to the KWiC resource. We now discuss the methodological advantages and disadvantages of the usability evaluation used in this study as a way to inform future research. Finally, we outline how the KTA framework will guide our subsequent research plans.
Methodological Advantages and Disadvantages
Obtaining feedback in slightly differing ways from a variety of clinicians was both advantageous and problematic with respect to summarizing and utilizing that feedback to make changes to the KWiC resource. We discuss how feedback was obtained according to relevant features of our process.
Participants and their relationship to investigators.
Our participants had varied clinical and VR experience. This range of experience was potentially advantageous as it allowed us to obtain richer feedback on the resource and was potentially representative of future users of the resource. However, participants practiced primarily in neurologic and pediatric settings. Inclusion of clinicians working with clients with orthopedic and geriatric conditions will enhance the generalizability of the KWiC. The participants had a professional association with the researchers. The advantage of this prior association was reflected in the depth of discussion regarding the resource and the apparent interest the participants had in contributing to improvements in the resource. The limitation or disadvantage is the potential reluctance of the participants to provide highly critical feedback to a colleague.
Familiarization with the resource.
Our initial aim was to provide the resource ahead of time for review by participants. We assumed that participants would familiarize themselves with the resource, but this did not always occur. This lack of familiarization resulted in less rich feedback than we had anticipated, as some participants needed to familiarize themselves with the resource during the brief interview time. Some sites anticipated this limitation and allowed time during the focus group to review the resource and discuss it, but others did not.
Differing methods.
Slight differences in terms of whether participants were interviewed alone or in a focus group as well as whether games were played during the focus group may have had an impact on the depth of feedback provided. In addition, users in a group setting may influence each other, resulting in some data loss from a user study perspective.69 Methodological differences were largely in an effort to individualize the process for the participants and to obtain the most useful feedback. Another limitation is that the way we asked participants to consult the resource was not particularly context-based in that it was isolated from a clinical sense. Clinicians may have been able to give more feedback had they been asked to think about a particular client (as was done at the Washington site) and consider whether the resource would be helpful in making decisions about that particular client.
In a true user-centered design, we would have involved users from the beginning of the study.44 We chose instead to use our experiences and perspectives, as we all had worked with clinicians and or physical therapist students to implement games in practice. We acknowledge this as a limitation in our process.
Subsequent Research Plans
The action cycle of the KTA framework will structure the next steps in the research process. First, we will make the changes described above to the KWiC resource. We will then adapt the new version to an online format. Online KT resources aim to disseminate research findings or translate evidence-based knowledge into practice with the goal of increasing awareness and stimulating practice change.70 Using the Internet as a platform for KT resources or tools is becoming increasingly popular because of its potential to lead large numbers of individuals through flexible self-paced, self-directed learning of up-to-date multimedia content.71,72 Evidence supporting the use of online resources to translate knowledge in rehabilitation is emerging.18,73–75 Best practice guidelines for the development of online KT resources in rehabilitation were proposed by Levac et al70; these guidelines will be followed in creating the website. An online resource may be an efficient method of achieving KT aims across geographic boundaries while applying adult learning principles to promote self-paced and self-directed ongoing learning. The online KWiC resource will include a “wiki” component, allowing clinicians to contribute their knowledge by suggesting therapeutic adaptations to games, analyzing new games, and providing ongoing feedback on resource content.
Next Steps
Mixed-method evaluation of content and format of the new Web-based KWiC resource.
This step will involve a larger sample size that is more representative of different practice areas. The method will be an online survey with a qualitative content analysis.76 We will first present participants with a selection of 1 of 4 case scenarios representative of use of the Kinect in different physical therapy practice areas. Participants will peruse the KWiC resource in the context of making a decision about which game to select for that particular client. They will provide feedback about content and format of the resource through an online questionnaire. The next phase of the KTA action cycle—assessing barriers to knowledge use—will be targeted through the questionnaire by asking participants questions about factors that would influence their use of an online KWiC resource to inform their clinical practice.
Tailor the intervention.
We will then tailor the intervention by making subsequent changes to KWiC resource based on feedback received from this questionnaire. We also will expand the resource to include more Kinect games.
Implement intervention, monitor knowledge use, and evaluate outcomes.
Once we have completed the usability evaluations and are confident that the content and format of the resource meets clinicians' needs, we will evaluate the impact of use of the KWiC resource on clinical decision making. Possible research methods could include a comparative study evaluating clinicians who use the KWiC to inform their Kinect intervention programs and those who are not exposed to the resource.
Sustain knowledge use.
This phase of the KTA action cycle will be targeted following successful and effective integration of the KWiC resource into practice by continually adding new games as they become available, summarizing emergent research evidence, monitoring the wiki, facilitating a discussion forum, and uploading additional video content to the resource, including short videos illustrating tips and techniques related to Kinect use with different patient populations.
Conclusion
Kinect for Xbox 360 games are accessible, motivating, and potentially challenging options for a variety of rehabilitation clients. The diversity of the games and their development for healthy populations implies that busy clinicians may require resources to support decision making about integration into rehabilitation clinical practice. Rather than simply deciding to use a new technology because it is popular, clinicians can learn to match the features of the system and the game characteristics to the needs of individual clients to achieve therapeutic benefit. It is important for clinicians to be comfortable enough with the technology to evaluate its effectiveness and to adapt it to changing needs. These goals informed the development and exploratory usability evaluation of a KT resource (ie, KWiC) designed to meet these goals. This article described the process and feedback received from the usability evaluation and outlined subsequent research plans for improving and further evaluating the KWiC resource using the KTA framework to guide the proposed research methods. We believe that an online KT resource that incorporates multimedia content and contains a discussion forum is the ideal format. After further user-based evaluation and feedback, we will explore the clinical utility of the KWiC resource by monitoring and evaluating outcomes related to its use.
Appendix 1.
Appendix 1.
Kinecting With Clinicians (KWiC) Resourcea
a UE=upper extremity, LE=lower extremity.
Appendix 2.
Appendix 2.
Focus Group Interview and Written Questions
Footnotes
All authors provided concept/idea/project design, writing, data analysis, and facilities/equipment. Dr Levac, Dr Espy, Dr Fox, and Dr Pradhan provided data collection and participants. Dr Levac and Dr Deutsch provided project management and consultation (including review of the manuscript before submission). The authors acknowledge Univerity of Florida undergraduate student research assistants for assistance with data collection at the Florida site and Bryan Barker, PT, PhD, and Andrew Grando, PT, PhD, research assistants in the Rivers Lab, for extensive work on game analysis at the New Jersey site.
Funding for this project was provided by the Rutgers Foundation and the Rivers Lab. Dr Levac is supported by a postdoctoral fellowship from the Canadian Institutes of Health Research.
References
- 1. Wilson PN, Foreman N, Stanton D. Virtual reality, disability and rehabilitation. Disabil Rehabil. 1997;19:213–220. [DOI] [PubMed] [Google Scholar]
- 2. Laver K, George S, Thomas S, et al. Cochrane review: virtual reality for stroke rehabilitation. Eur J Phys Rehabil Med. 2012;48:523–530. [PubMed] [Google Scholar]
- 3. Saposnik G, Levin M. Virtual reality in stroke rehabilitation: a meta-analysis and implications for clinicians. Stroke. 2011;42:1380–1386. [DOI] [PubMed] [Google Scholar]
- 4. Mumford N, Wilson PH. Virtual reality in acquired brain injury upper limb rehabilitation: evidence-based evaluation of clinical research. Brain Inj. 2009;23:179–191. [DOI] [PubMed] [Google Scholar]
- 5. Galvin J, McDonald R, Catroppa C, Anderson V. Does intervention using virtual reality improve upper limb function in children with neurological impairment: a systematic review of the evidence. Brain Inj. 2011;25:435–442. [DOI] [PubMed] [Google Scholar]
- 6. Parsons TD, Rizzo AA, Rogers S, York P. Virtual reality in paediatric rehabilitation: a review. Dev Neurorehabil. 2009;12:224–238. [DOI] [PubMed] [Google Scholar]
- 7. Sandlund M, McDonough S, Hager-Ross C. Interactive computer play in rehabilitation of children with sensorimotor disorders: a systematic review. Dev Med Child Neurol. 2009;51:173–179. [DOI] [PubMed] [Google Scholar]
- 8. Biddiss E. Should we integrate video games into home-based rehabilitation therapies for cerebral palsy? Future Neurol. 2012;7:515–518. [Google Scholar]
- 9. Glegg SM, Holsti L, Velikonja D, et al. Factors influencing therapists' adoption of virtual reality for brain injury rehabilitation. Cyberpsychol Behav Soc Netw. 2013;16:385–401. [DOI] [PubMed] [Google Scholar]
- 10. Levac DE, Miller PA. Integrating virtual reality video games into practice: clinicians' experiences. Physiother Theory Pract. 2013;29:504–512. [DOI] [PubMed] [Google Scholar]
- 11. Office of Special Education and Rehabilitative Services. National Institute on Disability and Rehabilitation Research long-range plan for fiscal years 2013–2017. Fed Regist. 2013;78:20299–20311. [Google Scholar]
- 12. National Center for the Dissemination of Disability Research. Knowledge translation. Available at: http://www.ncddr.org/knowledge_trans_over.html Accessed December 10, 2013.
- 13. Canadian Institutes of Health Research. About knowledge translation and commercialization. Available at: http://www.cihr-irsc.gc.ca/e/29418.html Accessed October 9, 2013.
- 14. Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implement Sci. 2012;7:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zidarov D, Thomas A, Poissant L. Knowledge translation in physical therapy: from theory to practice. Disabil Rehabil. 2013;35:1571–1577. [DOI] [PubMed] [Google Scholar]
- 16. Grimshaw JM, Eccles MP, Walker AE, Thomas RE. Changing physicians' behavior: what works and thoughts on getting more things to work. J Contin Educ Health Prof. 2002;22:237–243. [DOI] [PubMed] [Google Scholar]
- 17. Curran VR, Fleet L. A review of evaluation outcomes of Web-based continuing medical education. Med Educ. 2005;39:561–567. [DOI] [PubMed] [Google Scholar]
- 18. David I, Poissant L, Rochette A. Clinicians' expectations of Web 2.0 as a mechanism for knowledge transfer of stroke best practices. J Med Internet Res. 2012;14:e121–e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. National Stroke Foundation. National stroke audit: rehabilitation services report 2012. Melbourne, Australia: Available at: http://www.strokefoundation.com.au Accessed October 9, 2013. [Google Scholar]
- 20. Fung V, Ho A, Shaffer J, et al. Use of Nintendo Wii Fit™ in the rehabilitation of outpatients following total knee replacement: a preliminary randomised controlled trial. Physiotherapy. 2012;98:183–188. [DOI] [PubMed] [Google Scholar]
- 21. Demain S, Burridge J, Ellis-Hill C, et al. Assistive technologies after stroke: self-management or fending for yourself? A focus group study. BMC Health Serv Res. 2013;13:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Deutsch JE, Borbely M, Filler J, et al. Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Phys Ther. 2008;88:1–12. [DOI] [PubMed] [Google Scholar]
- 23. Deutsch JE, Brettler A, Smith C, et al. Nintendo Wii Sports and Wii Fit game analysis, validation, and application to stroke rehabilitation. Top Stroke Rehabil. 2011;18:701–719. [DOI] [PubMed] [Google Scholar]
- 24. Herz NB, Mehta SH, Sethi KD, et al. Nintendo Wii rehabilitation (“Wii-hab”) provides benefits in Parkinson's disease. Parkinsonism Relat Disord. 2013;19:1039–1042. [DOI] [PubMed] [Google Scholar]
- 25. Mombarg R, Jelsma D, Harman E. Effect of Wii-intervention on balance of children with poor motor performance. Res Dev Disabil. 2013;34:2996–3003. [DOI] [PubMed] [Google Scholar]
- 26. Mhatre PV, Vilares I, Stibb SM, et al. Wii Fit balance board playing improves balance and gait in Parkinson disease. PM&R. 2013;5:769–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Prosperini L, Fortuna D, Giannì C, et al. Home-based balance training using the Wii balance board: a randomized, crossover pilot study in multiple sclerosis. Neurorehabil Neural Repair. 2013;27:516–525. [DOI] [PubMed] [Google Scholar]
- 28. Rajaratnam BS, Gui Kaien J, Lee Jilin K, et al. Does the inclusion of virtual reality games within conventional rehabilitation enhance balance retraining after a recent episode of stroke? Rehabil Res Pract. 2013;2013:649561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Conyers JK, Malkin MJ, Yang H. An exploratory study on the effects of Nintendo Wii® Fit balance board on balance retraining and body mass index of adolescents with a traumatic brain injury. Am J Recreation Ther. 2011;10:38–48. [Google Scholar]
- 30. Heick JD, Flewelling S, Blau R, et al. Wii Fit and balance: does the Wii Fit improve balance in community-dwelling older adults? Top Geriatr Rehabil. 2012;28:217–222. [Google Scholar]
- 31. Jorgensen MG, Laessoe U, Hendriksen C, et al. Efficacy of Nintendo Wii training on mechanical leg muscle function and postural balance in community-dwelling older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2013;68:845–852. [DOI] [PubMed] [Google Scholar]
- 32. Sparker-Griffin C. Wii-habilitation: using Wii as an effective intervention tool for seniors. OT Practice. 2013;18:18–19. [Google Scholar]
- 33. Baltaci G, Harput G, Haksever B, et al. Comparison between Nintendo Wii Fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sport Traumatol Arthrosc. 2012;21:880–887. [DOI] [PubMed] [Google Scholar]
- 34. Sims J, Cosby N, Saliba EN, et al. Exergaming and static postural control in individuals with a history of lower limb injury. J Athl Train. 2013;48:314–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sin H, Lee G. Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am J Phys Med Rehabil. 2013;92:871–880. [DOI] [PubMed] [Google Scholar]
- 36. Gutiérrez RO, Gálan Del Rio F, Cano de la Cuerda R, et al. A telerehabilitation program by virtual reality video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation. 2013;33:545–554. [DOI] [PubMed] [Google Scholar]
- 37. Luna-Oliva L, Ortiz-Gutiérrez RM, Cano-de la Cuerda R, et al. Kinect Xbox 360 as a therapeutic modality for children with cerebral palsy in a school environment: a preliminary study. NeuroRehabilitation. 2013;33:513–521. [DOI] [PubMed] [Google Scholar]
- 38. Ilg W, Schatton C, Schicks J, et al. Video game-based coordinative training improves ataxia in children with degenerative ataxia. Neurology. 2012;79:2056–2060. [DOI] [PubMed] [Google Scholar]
- 39. Vernadakis N, Derri V, Tsitskari E, Antoniou P. The effect of Xbox Kinect intervention on balance ability for previous injured young competitive male athletes: a preliminary study. Phys Ther Sports. 2014;15:148–155. [DOI] [PubMed] [Google Scholar]
- 40. Laver K, George S, Ratcliffe J, Crotty M. Virtual reality stroke rehabilitation: hype or hope? Aust Occup Ther J. 2011;58:215–219. [DOI] [PubMed] [Google Scholar]
- 41. Levac DE, Galvin J. When is virtual reality “therapy”? Arch Phys Med Rehabil. 2013;94:795–798. [DOI] [PubMed] [Google Scholar]
- 42. Straus SE, Tetroe J, Graham ID. Introduction: knowledge translation—what it is and what it isn't. In: Straus SE, Tetroe J, Graham ID, eds. Knowledge Translation in Health Care: Moving From Evidence to Practice. 2nd ed Chichester, United Kingdom: John Wiley & Sons Ltd; 2013. [Google Scholar]
- 43. Sudsawad P. Knowledge Translation: Introduction to Models, Strategies, and Measures. Austin, TX: Southwest Educational Development Laboratory, National Center for the Dissemination of Disability Research; 2007. [Google Scholar]
- 44. Rubin J, Chasnell D. Handbook of Usability Testing: How to Plan, Design, and Conduct Effective Tests. 2nd ed Indianapolis, IN: Wiley Publishing Inc; 2008. [Google Scholar]
- 45. Levac DE, Galvin J. Facilitating clinical decision-making about the use of virtual reality within paediatric motor rehabilitation: application of a classification framework. Dev NeuroRehabilitation. 2011;14:177–184. [DOI] [PubMed] [Google Scholar]
- 46. Galvin J, Levac DE. Facilitating clinical decision-making about the use of virtual reality within paediatric motor rehabilitation: describing and classifying virtual reality systems. Dev NeuroRehabilitation. 2011;14:112–122. [DOI] [PubMed] [Google Scholar]
- 47. Rademaker M, Fox EJ, Lange B, et al. Made for rehab: feasibility and effect of a clinician-adapted video game using the Kinect™ on balance and falls in a woman with parkinsonism. Poster presented at: Combined Sections Meeting of the American Physical Therapy Association; January 21–24, 2013; San Diego, California. [Google Scholar]
- 48. Pradhan SD, Mortiz C. The use of a gaming device for a multimodal exercise intervention in individuals with Parkinson disease. Poster presented at: Combined Sections Meeting of the American Physical Therapy Association; January 21–24, 2013; San Diego, California. [Google Scholar]
- 49. Espy D, Reinthal A, Dal Bello-Haas V. A systematic framework to guide clinical decision-making in gaming choices for therapeutic use. Poster presented at: Combined Sections Meeting of the American Physical Therapy Association; January 21–24, 2013: San Diego, California. [Google Scholar]
- 50. Schmidt RA, Lee TD. Motor Control and Learning: A Behavioral Emphasis. 5th ed Champaign, IL: Human Kinetics; 2011. [Google Scholar]
- 51. Holden MK. Virtual environments for motor rehabilitation: review. Cyberpsychol Behav. 2005;8:187–211. [DOI] [PubMed] [Google Scholar]
- 52. Imam B, Jarus T. Virtual reality rehabilitation from social cognitive and motor learning theoretical perspectives in stroke population. Rehabil Res Pract. 2014;2014:594540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Pollock A, Baer G, Langhorne P, Pomeroy V. Physiotherapy treatment approaches for the recovery of postural control and lower limb function following stroke: a systematic review. Clin Rehabil. 2007;21:395–410. [DOI] [PubMed] [Google Scholar]
- 54. Zelaznik H. The past and future of motor learning and control: what is the proper level of description and analysis? Kin Rev. 2014;3:38–43. [Google Scholar]
- 55. Snodgrass SJ, Heneghan NR, Tsao H, et al. Recognising neuroplasticity in musculoskeletal rehabilitation: a basis for greater collaboration between musculoskeletal and neurological physiotherapists. Man Ther. 2014;19:614–617. [DOI] [PubMed] [Google Scholar]
- 56. Sullivan KJ, Kantak SS, Burtner PA. Motor learning in children: feedback effects on skill acquisition. Phys Ther. 2008;88:720–732. [DOI] [PubMed] [Google Scholar]
- 57. Cai L, Chan JSY, Yan JH, Peng K. Brain plasticity and motor practice in cognitive aging. Frontiers Aging Neurosci. 2014;6:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Carr JH, Shepard R, eds. Movement Science: Foundations for Physical Therapy in Rehabilitation. Gaithersberg, MD: Aspen Pubishers Inc; 2000. [Google Scholar]
- 59. Gentile AM. Skill acquisition: action, movement, and neuromotor processes. In: Carr JH, Shepard R, eds. Movement Science: Foundations for Physical Therapy in Rehabilitation. Gaithersberg, MD: Aspen Publishers Inc; 2000. [Google Scholar]
- 60. Shumway-Cook A, Woollacott MH. Motor Control: Theory and Practical Applications. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 61. Winstein CJ. Knowledge of results and motor learning: implications for physical therapy. Phys Ther. 1991;71:140–149. [DOI] [PubMed] [Google Scholar]
- 62. Levin MF. Can virtual reality offer enriched environments for rehabilitation? Expert Rev Neurother. 2011;11:153–155. [DOI] [PubMed] [Google Scholar]
- 63. Lohse K, Shirzad N, Verster A, et al. Video games and rehabilitation: using design principles to enhance engagement in physical therapy. J Neurol Phys Ther. 2013;37:166–175. [DOI] [PubMed] [Google Scholar]
- 64. dos Santos Mendes FA, Pompeu JE, Modenesi Lobo A, et al. Motor learning, retention and transfer after virtual-reality-based training in Parkinson's disease—effect of motor and cognitive demands of games: a longitudinal, controlled clinical study. Physiotherapy. 2012;98:217–223. [DOI] [PubMed] [Google Scholar]
- 65. Schmidt RA, Wrisberg CA. Motor Learning and Performance. 2nd ed Champaign, IL: Human Kinetics; 2000. [Google Scholar]
- 66. Jurado MB, Rosselli M. The elusive nature of executive functions: a review of our current understanding. Neuropsychol Rev. 2007;17:213–233. [DOI] [PubMed] [Google Scholar]
- 67. Hix D, Gabbard JL. Usability engineering of virtual environments. In: Stanney K, ed. Handbook of Virtual Environments: Design, Implementation, and Applications. Mahwah, NJ: Lawrence Erlbaum Associates; 2002:681–699. [Google Scholar]
- 68. Preece J, Rogers Y, Sharp H. Interaction Design: Beyond Human-Computer Interaction. New York, NY: John Wiley & Sons Inc; 2002. [Google Scholar]
- 69. Sullivan P. Multiple methods and the usability of interface prototypes: the complementarity of laboratory and focus groups. In: Proceedings of the ACM Conference on Systems Documentation; New York, NY; 1991 1991:106–118. [Google Scholar]
- 70. Levac D, Glegg S, Camden C, et al. Best practice guidelines for the development, implementation, and evaluation of online knowledge translation resources in rehabilitation. Phys Ther. doi: 10.2522/ptj.20130500. [DOI] [PubMed] [Google Scholar]
- 71. Mathur S, Stanton S, Reid WD. Canadian physical therapists' interest in Web-based and computer-assisted continuing education. Phys Ther. 2005;85:226–237. [PubMed] [Google Scholar]
- 72. Stockley D, Beyer W, Hutchinson N, et al. Using interactive technology to disseminate research findings to a diverse population. Can J Learning Technol. 2009;35:1. [Google Scholar]
- 73. MacDonald CJ, Stodel EJ, Farres LJ, et al. The demand-driven learning model: a framework for Web-based learning. Internet Higher Ed. 2001;4:9–30. [Google Scholar]
- 74. Dieleman C, Duncan EAS. Investigating the purpose of an online discussion group for health professionals: a case example from forensic occupational therapy. BMC Health Serv Res. 2013;13:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hoffmann T, Desha L, Verrall K. Evaluating an online occupational therapy community of practice and its role in supporting occupational therapy practice. Aust Occup Ther J. 2011;58:337–345. [DOI] [PubMed] [Google Scholar]
- 76. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. [DOI] [PubMed] [Google Scholar]