Abstract
Liposarcomas of the larynx are extremely rare tumors, with only 37 cases reported in the English or French literature to date. The first two cases of laryngeal liposarcomas were reported respectively by Kapur and Dockerty in 1968 [1, 2]. Liposarcoma of the larynx is at high risk of local recurrence and seldom has metastatic potential. Prognosis for this tumor is better than that of non laryngeal liposarcoma. The present case is the first patient of primary liposarcoma of the larynx reported from China. A review of the literature was performed, and the presentation, position, pathological diagnosis, treatment and prognosis of the patients with liposarcoma of the larynx of the reported cases before are analyzed.
Keywords: Larynx, liposarcoma, surgery, radiotherapy, chemotherapy
Introduction
Liposarcoma is one of common soft tissue malignant tumor and is often found in the lower extremities and retro peritoneum. Only about 5.6% of liposarcomas are found in the head and neck, and most of the tumors arise from the soft tissues of the neck. Laryngeal liposarcoma (LLS) is extremely rare, with only 37 cases reported in the English or French language literature. In the present study, we report a case of LLS and analyze the 37 cases of LLS.
Case report
A 53-year-old man had a history of heavy smoking for 20 years and chronic laryngitis for 2 years, with airway obstruction that had developed over 3 months. A so-called laryngeal polyp had been removed from the right arytenoid region, aryepiglottic fold (AEF) and false vocal fold (FVF) 3 months before by surgical excision in a county hospital. According to the clinic doctor, the neoplasm was a yellow-grey 1×1 cm polypoid mass and was unencapsulated. The patient did not take the pathological examination in the country hospital. One week before, the tumor recurred. A laryngoscopic examination disclosed the irregular tumor mass in the right arytenoid region, AEF and FVF (Figure 1). We received irregular scattered masses excised from the focus with a size of 0.8×1 cm in large diameter.
Figure 1.
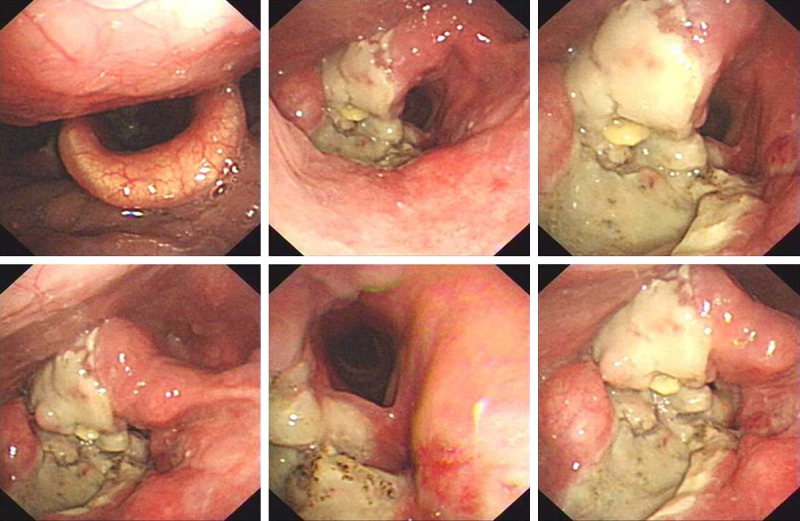
Laryngoscope showed the tumor mass in the right arytenoid region, aryepiglottic fold (AEF) and false vocal fold (FVF).
The specimen was examined histologically and immunohistochemically. The tumor was composed of fat lobules with a few fibrous tissues. The adipocytes were of different size with scattered lipoblasts. At high-power view, well differentiated liposarcoma was characterized by adipocytes with a great variation in size and multivacuolated lipoblasts (Figure 2A-C). No mitotic figures in the areas of well-differentiated liposarcoma and no atypical spindled cells were seen. Immunohistochemistry on formalin-fixed paraffin-embedded tissue revealed positivity of the tumor cells for vimentin, S-100 and MDM2 protein (Figure 2D-F). Tumor cells were negative for AE1/AE3 cytokeratin, myoglobin, and CD68 immunostains. Final pathological diagnosis, suggested by the histological appearance and immunohistochemical profile, was atypical lipomatous tumor/well-defferentiated liposarcoma.
Figure 2.
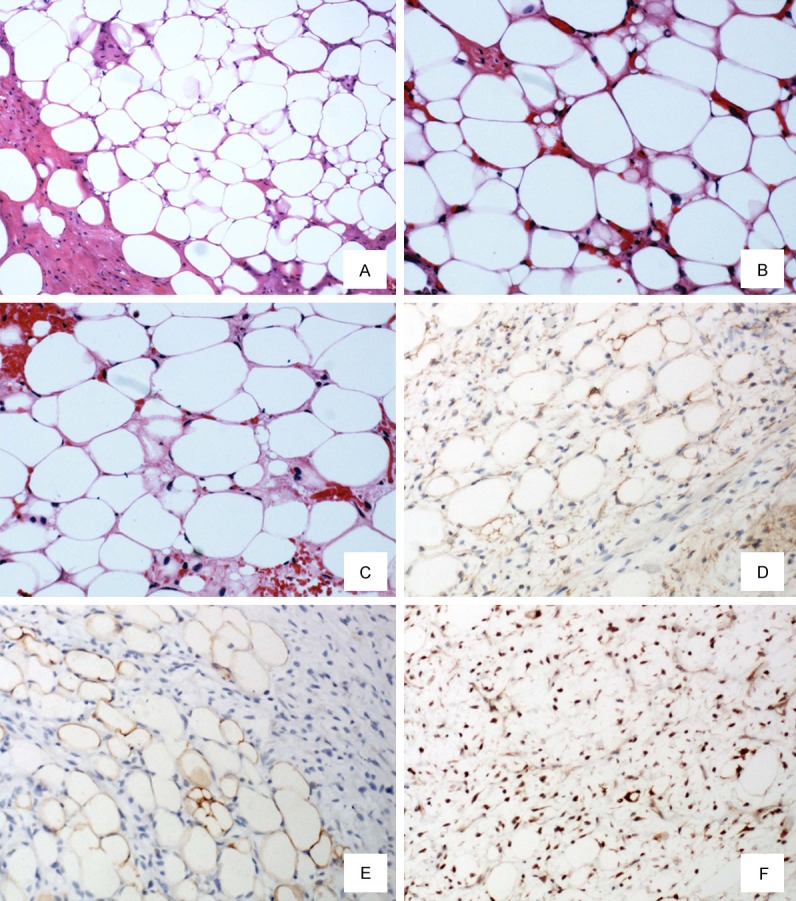
Microscopically, the tumor consisted of well-differentiated liposarcoma (A, hematoxylin-eosin, ×100). At high-power view, well-differentiated liposarcoma was characterized by multivacuolated lipoblasts (B and C, hematoxylin-eosin, ×200). On immunohistochamical analysis lipogenic areas showed positivity for vimentin (D, ×200), S100 (E, ×200) and MDM2 (F, ×200).
As a consequence, total laryngectomy was performed. The study of the latter specimen revealed tumor infiltration of the tumor margin. The patient did not receive radiotherapy and chemotherapy. Today, 13 months after laryngectomy, he is alive and well, without any evidence of recurrence or metastases.
Discussion
Liposarcoma, which is much less frequent than lipoma, was first described by Virchow in 1857 [26]. Laryngeal liposarcomas (LLS) are exceedingly rare, with only 37 cases been reported in the English or French language literature to date. Having reviewed the 37 cases of LLS reported (see Table 1), we summarize the clinical features are as follows: LLS are more common in men, and only 4 cases have been reported in women (male to female ratio is 8:1). The mean age of the patients is 55 years (ranged from 28 to 83 years) in the reported cases. Most of the reported cases affected the supraglottic area. There are only 4 cases affecting the true vocal cords. The most frequent complaints at presentation are airway obstruction, snoring or dysphagia, although some patients present because of hoarsenessor throat discomfort. Smoking has been suggested as an environmental factor in the development of this neoplasm.
Table 1.
Clinical and pathological features of 37 cases of laryngeal liposarcoma
| Authors | Age | Sex | Location | WHO Histology | Treatment | Rec | Follow-Up | year | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Dockerty [26] | 33 | M | left AEF | Pleo | surgery | Y | DOD | 1968 |
| 2 | Kapur [1] | 61 | M | Larynx, left PS | Myxoid WD | surgery | Y 3 Rec | DOD within 12 m | 1968 |
| 3 | Miller [3] | 43 | M | right FVF | Myxoid WD | TL | N | NED 72 m | 1975 |
| 4 | Velek [4] | 68 | M | right supraglottis | WD | TL | N | NED 80 m | 1976 |
| 5 | Krausen [5] | 67 | M | Epiglottis, right AEF | PD | SL. pRT | N | DOD 72 m | 1977 |
| 6 | Ferlito [6] | 52 | M | left FVF+TVF | Pleo | HL, pRT/TL | Y | NED 72 m | 1978 |
| 7 | Tobey [7] | 61 | M | right vocal cord | PD | SL, Chem | Y | DOD 13 m | 1979 |
| 8 | Gaynor [8] | 59 | M | right AEF, Epiglottis | MX/RDC | SL | N | NED 36 m | 1984 |
| 9 | Shah [9] | 28 | M | Epiglottis | MX/RDC | SL | Y | 32 m | 1984 |
| 10 | Gaynor [8] | 59 | M | Epiglottis, AEF | MX/RDC | SL | Y | 36 m | 1984 |
| 11 | Narula [10] | 45 | M | Larynx | MX/RDC | TL | N | DOD 30 m | 1985 |
| 12 | Allsbrook [11] | 45 | M | left arytenoid | WD | EE/LP×2, EE | Y | 48 m | 1985 |
| 13 | Gadomski [12] | 28 | M | Epiglottis | WD | SE | N | NED 48 m | 1986 |
| 14 | Meis [13] | 54 | M | right AEF | WD | EE/EE, SL, ND, pRT | Y | NED 58 m | 1986 |
| 15 | Gertner [14] | 37 | M | left arytenoid | WD | TL, pRT | N | DOD 24 m | 1988 |
| 16 | Wenig [15] | 49 | M | AEF | WD, 3 cm | SE/SE | Y | NED 72 m | 1990 |
| 17 | Wenig [15] | 65 | F | Epiglottis | WD, 2×2×1.5 cm | SE/SE | Y | NED 480 m | 1990 |
| 18 | Wenig [15] | 57 | M | Epiglottis | WD | SE/SE×2, TL | Y | NED 33 m | 1990 |
| 19 | Wenig [15] | 68 | M | Epiglottis | WD, 3×2×1.5 cm | TL | N | NED 168 m | 1990 |
| 20 | Wenig [15] | 55 | M | right FVF | WD, 6×3 cm, polyp | SE/SE×4, pRT | Y | NED 120 m | 1990 |
| 21 | Esclamado [16] | 34 | M | left AEF | WD | SL | N | NED 15 m | 1994 |
| 22 | McCormick [17] | 62 | M | Larynx | DD | Not doc | Y | Rec 276 m | 1994 |
| 23 | Hurtado [18] | 83 | F | left TVF | WD | EE | N | NED 24 m | 1994 |
| 24 | Wenig [19] | 76 | F | Epiglottis | MX/RDC | LP/TL | Y | DND 12 m | 1995 |
| 25 | Wenig [19] | 44 | M | Epiglottis | MX/RDC | EE/EE, LP | Y | NED 72 m | 1995 |
| 26 | Wenig [19] | 56 | M | right TVF | Pleo | EE/SE | Y | NED 60 m | 1995 |
| 27 | Wenig [19] | 72 | M | Epiglottis | WD | EE/EE×7, LP | Y | NED 120 m | 1995 |
| 28 | Wenig [19] | 56 | M | left AEF | WD | EE/EE×3 | Y | NED 108 m | 1995 |
| 29 | Wenig [19] | 63 | M | right AEF | WD | SL | N | NED 36 m | 1995 |
| 30 | Gal [20] | 63 | M | Larynx | WD | SE | Not doc | Not doc | 1998 |
| 31 | Mandell [21] | 37 | M | left arytenoid | WD | EE/EE | N | RD 122 m | 1999 |
| 32 | Mestre de Juan [22] | 62 | M | right AEF | WD | SL | N | NED 14 m | 1999 |
| 33 | Acharki [23] | 50 | M | FVF | MX/RDC | TL, pRT (50 Gy) | N | NED 18 m | 1999 |
| 34 | Brauchle [24] | 51 | M | Epiglottis | WD | LP | N | NED 18 m | 2001 |
| 35 | Yaqoob [25] | 60 | F | right TVF | MX/RDC | Not doc | Not doc | Not doc | 2006 |
| 36 | Powitzky [2] | 63 | M | left AEF, PS | DD, NOS | LP | N | NED 12 m | 2007 |
| 37 | Present case | 53 | M | right AEF, FVF | WD, 2×1 cm | TL | Y | NED 13 m | 2014 |
Abbreviations: AEF, aryepiglottic fold; Chem, chemotherapy; DD, dedifferentiated; DND, dead of causes other than disease; DOD, dead of disease; EE, endoscopic excision; F, female; FVF, false vocal fold; HL, hemilaryngectomy; LP, laleral pharyngetomy; m, months; M, male; MX, mxyoid; ND, neck disseciion; NED, alive with no evidence of disease; Not doc, not documented in report; PD, poor differentiated; Pleo, pleomorphic; Prt, postoperative radiotherapy; PS, pyriform sinus; RDC, round cell; Rec, recurrence; RT, radiation therapy; SE, simple excision; SL, supragiottic laryngectomy; TL, tolal laryngectomy; TVF, true vocal fold; WD, well differentiated; WHO, World Health Organization.
The World Health Organization pathological classification (WHO 2013) identifies four histological subtypes of liposarcoma: well differentiated/atypical lipomatous tumor, myxoid/round cell, pleomorphic and dedifferentiated. We present a case of a laryngeal well differentiated liposarcoma. To our knowledge, this is the first case of laryngeal liposarcoma reported from China.
Histologically, most of the LLS are low grade tumors (either well-differentiated or myxoid liposarcomas), with only few reports describing high grade tumors (pleomorphic, myxoid/round-cell or dedifferentiated liposarcomas) [2,5,6,17].
The main differential diagnosis of LLS is lipoma and myxoid chondrosarcoma. Immunohistochemistry cannot distinguish them, because both lipoma and chondrosarcoma are positive for S100 protein. Therefore, pathologists should find the typical histological features of liposarcoma (mainly the presence of lipoblasts) and make sure that there are no chondromatous areas. Lipomas are usually well-demarcated, encapsulated lesions which have no tendency to infiltrate into the surrounding normal tissues, show no lipoblasts and allow a simple excision without recurrences.
Most LLSs are indolent with low-grade histology. They are locally aggressive but have no tendency to spread to regional lymph nodes. Moreover, distant metastases are very rare. The locally aggressive behavior of the tumor is underscored by its tendency to recur after surgery. Summarize all published cases, 19/37 patients had recurrence (51%) to date, regional nodal metastasis has not been reported, while distant metastases have been reported in 3/37 patients (8.1%) [2]. The high grade tumors have spread to the skin and the bone, causing the patient’s death [6,16].
The recommended treatment for LLS is wide surgical excision [2], i.e. excision of the lesion with a sufficient cuff of surrounding tissues generally free of disease. In fact, the high recurrence rate of laryngeal liposarcomas seems to be related more to treatment than to the histological type [2]. There appears to be no justification for the use of radiotherapy or chemotherapy in these patients, for these adjuvant techniques do not improve the results obtained by complete resection alone. Radiotherapy has been used only occasionally as adjuvant to surgery or for recurrent lesions following surgery [4,15]. LLS has a better prognosis compared to their counterparts in extremities or retroperitoneum, for the symptoms of airway obstruction occur early resulting in early medical examination.
Acknowledgements
We thank Mr. Li-Chao Wang who provided valuable clinical history and data.
Disclosure of conflict of interest
None.
References
- 1.Kapur TR. Recurrent lipomata of the larynx and the pharynx with late malignant change. J Laryngol Otol. 1968;82:761–768. doi: 10.1017/s0022215100069425. [DOI] [PubMed] [Google Scholar]
- 2.Powitzky R, Powitzky ES, Garcia R. Liposarcoma of the larynx. Ann Otol Rhinol Laryngol. 2007;116:418–424. doi: 10.1177/000348940711600605. [DOI] [PubMed] [Google Scholar]
- 3.Miller D, Goodman M, Weber A, Goldstein A. Primary liposarcoma of the larynx. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol. 1975;80:444–447. [PubMed] [Google Scholar]
- 4.Velek JP. Liposarcoma of the larynx. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol. 1976;82:569–570. [PubMed] [Google Scholar]
- 5.Krausen AS, Gall AM, Garza R, Spector GJ, Ansel DG. Liposarcoma of the larynx: a multicentric or a metastatic malignancy. Laryngoscope. 1977;87:1116–1124. doi: 10.1288/00005537-197707000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Ferlito A. Primary pleomorphic liposarcoma of the larynx. J Otolaryngol. 1978;7:161–166. [PubMed] [Google Scholar]
- 7.Tobey DN, Wheelis RF, Yarington CT Jr. Electron microscopy in the diagnosis of liposarcoma and fibrosarcoma of the larynx. Ann Otol Rhinol Laryngol. 1979;88:867–871. doi: 10.1177/000348947908800623. [DOI] [PubMed] [Google Scholar]
- 8.Gaynor EB, Raghausan U, Weisbrot IM. Primary myxoid liposarcoma of the larynx. Otolaryngol Head Neck Surg. 1984;92:476–480. doi: 10.1177/019459988409200418. [DOI] [PubMed] [Google Scholar]
- 9.Shah MC, Lowry LD. Primary liposarcoma of the larynx. Trans Pa Acad Ophthalmol Otolaryngol. 1984;37:49–52. [PubMed] [Google Scholar]
- 10.Narula A, Jefferis AF. Squamous cell carcinoma and liposarcoma of the larynx occurring metachronously. J Laryngol Otol. 1985;99:509–511. doi: 10.1017/s0022215100097140. [DOI] [PubMed] [Google Scholar]
- 11.Allsbrook WC Jr, Harmon JD, Chongchitnant N, Erwin S. Liposarcoma of the larynx. Arch Pathol Lab Med. 1985;109:294–296. [PubMed] [Google Scholar]
- 12.Gadomski SP, Zwillenberg D, Choi HY. Non-epidermoid carcinoma of the larynx: the Thomas Jefferson University experience. Otolaryngol Head Neck Surg. 1986;95:558–565. doi: 10.1177/019459988609500507. [DOI] [PubMed] [Google Scholar]
- 13.Meis JM, Mackay B, Goepfert H. Liposarcoma of the larynx. Case report and literature review. Arch Otolaryngol Head Neck Surg. 1986;112:1289–1292. doi: 10.1001/archotol.1986.03780120053010. [DOI] [PubMed] [Google Scholar]
- 14.Gertner R, Podoshin L, Fradis M, Misselevitch I, Boss J. Liposarcoma of the larynx. J Laryngol Otol. 1988;102:838–841. doi: 10.1017/s0022215100106620. [DOI] [PubMed] [Google Scholar]
- 15.Wenig BM, Weiss SW, Gnepp DR. Laryngeal and hypopharyngeal liposarcoma. A clinicopathologic study of 10 cases with a comparison to soft-tissue counterparts. Am J Surg Pathol. 1990;14:134–141. doi: 10.1097/00000478-199002000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Esclamado RM, Disher MJ, Ditto JL, Rontal E, McClatchey KD. Laryngeal liposarcoma. Arch Otolaryngol Head Neck Surg. 1994;120:422–426. doi: 10.1001/archotol.1994.01880280050009. [DOI] [PubMed] [Google Scholar]
- 17.McCormick D, Mentzel T, Beham A, Fletcher CD. Dedifferentiated liposarcoma. Clinicopathologic analysis of 32 cases suggesting a better prognostic subgroup among pleomorphic sarcomas. Am J Surg Pathol. 1994;18:1213–1223. doi: 10.1097/00000478-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Hurtado JF, Lopez JJ, Aranda FI, Talavera J. Primary liposarcoma of the larynx. Case report and literature review. Ann Otol Rhinol Laryngol. 1994;103:315–318. doi: 10.1177/000348949410300409. [DOI] [PubMed] [Google Scholar]
- 19.Wenig BM, Heffner DK. Liposarcomas of the larynx and hypopharynx: a clinicopathologic study of eight new cases and a review of the literature. Laryngoscope. 1995;105:747–756. doi: 10.1288/00005537-199507000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Gal TJ, Agnello PF, Muro-Cacho CA. Pathologic quiz case 2. Liposarcoma of the larynx. Arch Otolaryngol Head Neck Surg. 1998;124:1171, 1173. [PubMed] [Google Scholar]
- 21.Mandell DL, Brandwein MS, Woo P, Som PM, Biller HF, Urken ML. Upper aerodigestive tract liposarcoma: report on four cases and literature review. Laryngoscope. 1999;109:1245–1252. doi: 10.1097/00005537-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Mestre de Juan MJ, Fernandez-Acenero MJ. Laryngeal liposarcoma: report of a case. Pathol Res Pract. 1999;195:125–128. doi: 10.1016/S0344-0338(99)80085-5. [DOI] [PubMed] [Google Scholar]
- 23.Acharki A, Sahraoui S, Benider A, Samlali R, Kahlain A. [Liposarcoma of the larynx. Review of the literature apropos of a case] . Cancer Radiother. 1999;3:245–248. doi: 10.1016/s1278-3218(99)80059-6. [DOI] [PubMed] [Google Scholar]
- 24.Brauchle RW, Farhood AI, Pereira KD. Well-differentiated liposarcoma of the epiglottis. J Laryngol Otol. 2001;115:593–595. doi: 10.1258/0022215011908342. [DOI] [PubMed] [Google Scholar]
- 25.Yaqoob N, Pervez S, Ahmed I. A 60-year-old woman with history of hoarseness and dysphagia. Laryngeal liposarcoma. Arch Pathol Lab Med. 2006;130:115–116. doi: 10.5858/2006-130-115-AYWWHO. [DOI] [PubMed] [Google Scholar]
- 26.Virchow R. Einfall von bosartigen, zum theil in der form des neurons quftretenden fettgeschwullsten. Virchows Arch. 1857;11:281–288. [Google Scholar]


