Abstract
In this brief report, we have described a rare case of schwannoma of the parotid gland in a young female who presented to us with a 3 cm diameter parotid swelling. The fine-needle aspiration cytology showed small fascicles, clusters and discrete spindle-shaped cells with long wavy nuclei. The cytological diagnosis of schwannoma of the parotid gland was offered and later confirmed by excision and histopathology.
Keywords: Fine-needle aspiration cytology, parotid, schwannoma
Introduction
Schwannomas of the parotid gland are rare neoplasms.[1] Preoperative diagnosis of these tumors helps in the proper surgical excision of this tumor. Fine-needle aspiration cytology (FNAC) of schwannoma of the parotid glands are rarely been described.[2] Most of the times the lesions are misinterpreted on FNAC of parotid.[3] Herein, we present a rare case of schwannoma of the parotid gland, diagnosed on FNAC and subsequently confirmed on histopathology.
Case Report
A 29-year-old female presented with a painless, gradually progressive swelling in right preauricular region for 3 years. Patient denied any facial weakness, twitching or pain. On examination, there was a well-defined 3 cm × 2 cm, firm, nontender, mobile swelling in right parotid region. Facial nerve function was normal. Contrast-enhanced computed tomography revealed a well-defined heterogeneously enhancing soft tissue density involving right superficial lobe of the parotid gland. FNAC was performed, and the cytology smears were moderately cellular having cohesive clusters, small fascicles, and the singly scattered spindle-shaped tumor cells. Most of the cell clusters were of low cellularity representing Antoni B areas [Figure 1]. These cells showed mild pleomorphism, elongated wavy nuclei with pointed ends, bland nuclear chromatin, inconspicuous nucleoli and a moderate amount of cytoplasm. The cells were embedded in a fibrillary eosinophilic matrix. A diagnosis of benign nerve sheath tumor (BNST), consistent with schwannoma was reported. Surgical excision of the tumor showed an encapsulated firm tumor measuring 3 cm × 2cm × 2 cm. Cut surface was whitish with focal areas of hemorrhage. Microscopy revealed a well-encapsulated tumor having hypercellular (Antoni A) and hypocellular (Antoni B) areas composed of spindle-shaped cells having elongated nuclei with pointed ends and eosinophilic cytoplasm [Figure 2]. Focal nuclear palisading was seen. Final histopathologic diagnosis of schwannoma was made. Post-operatively the patient was asymptomatic without any features of nerve palsy.
Figure 1.

Small fascicle of tumor cells in cytology smear of schwannoma (H and E, ×440)
Figure 2.
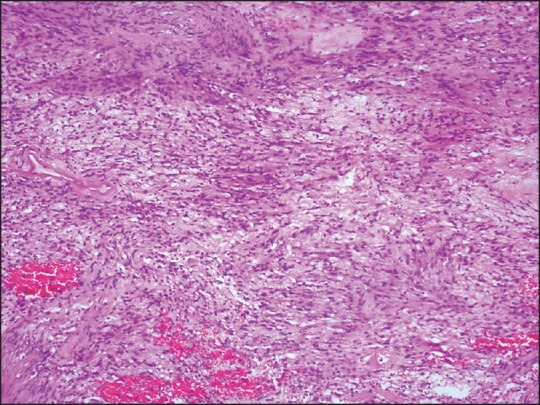
Histopathology section of schwannoma of the parotid gland showing bundles of spindle cells with cellular and hypocellular areas (H and E, ×240)
Discussion
Schwannoma (neurilemmoma) is a slow growing encapsulated tumor of neuroectodermal derivation that originates from the Schwann cells of the neural sheath. Approximately, 25-30% of all reported schwannomas occur in the head and neck and most of these in the eighth nerve.[4] Among 802 parotid tumors, Eneroth and Hamberger[5] could demonstrate two cases with neurogenic origin and in a review of 700 parotidectomies Nussbaum[6] found only one case of neurilemmoma of the facal nerve. Although these tumors may arise at any age, the peak incidence is between the third and sixth decades.[7] Many patients present with a painless, palpable facial mass. The presence of facial paralysis is variable.
The difficulty in establishing a correct preoperative diagnosis has been pointed out by Conley and Janecka[8] because this tumor is infrequent and generally unsuspected as preoperative facial nerve paresis is unusual. FNAC is frequently used preoperatively to evaluate the salivary gland lesions with reasonable sensitivity and specificity, ranging from 60-100% to 90-100%, respectively.[2] Most of the parotid tumors have characteristic cytomorphologic features that aid indefinite preoperative diagnosis, however, a few lesions, both benign and malignant, can cause problems in interpretation.
Distinctive pathologic features of schwannoma include a dimorphic growth pattern comprising of cellular (Antoni A) and loose-textured (Antoni B) areas, Verocay bodies and hyaline blood vessels.[9] FNAC in the present case has characteristic morphology of a benign peripheral nerve sheath tumor, but the location was unusual and clinically also it was unsuspected. Differential diagnosis of pleomorphic adenoma (with predominant stromal component) was considered. However, this possibility was ruled out due to lack of epithelial elements and chondromyxoid stroma. An erroneous diagnosis of a pleomorphic adenoma on fine-needle aspiration had been made in the past where histopathology confirmed benign schwannoma.[3] In contrast pleomorphic adenoma was misinterpreted as BNST in two cases and authors recommended a diligent search for epithelial elements prior to diagnosing BNST in the head and neck region.[10] Other mimickers include the predominant spindle cell myoepitheliomas[11] and some of the low-grade sarcomas that may arise from the parotid gland. The schwannoma like mixed tumor of the parotid gland[12] must be also considered.
With early diagnosis of parotid schwannoma by FNAC, management of patient can be planned and ultimately, facial nerve function can be optimized. Enucleation with nerve preservation is preferred choice to offer better facial function, whereas nerve excision with cable graft may be performed with satisfactory results.[13]
In brief, schwannoma of the parotid gland is rare and may be mistaken as pleomorphic adenoma. Cytological features such as small fascicles of cells and wavy spindle-shaped nuclei are helpful features to distinguish this tumor from pleomorphic adenoma.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Falcioni M, Russo A, Taibah A, Sanna M. Facial nerve tumors. Otol Neurotol. 2003;24:942–7. doi: 10.1097/00129492-200311000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Layfield LJ, Tan P, Glasgow BJ. Fine-needle aspiration of salivary gland lesions. Comparison with frozen sections and histologic findings. Arch Pathol Lab Med. 1987;111:346–53. [PubMed] [Google Scholar]
- 3.Mair S, Leiman G. Benign neurilemmoma (schwannoma) masquerading as a pleomorphic adenoma of the submandibular salivary gland. Acta Cytol. 1989;33:907–10. [PubMed] [Google Scholar]
- 4.Putney FJ, Moran JJ, Thomas GK. Neurogenic tumors of the head and neck. Laryngoscope. 1964;74:1037–59. doi: 10.1288/00005537-196408000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Eneroth CM, Hamberger CA. Principles of treatment of different types of parotid tumors. Laryngoscope. 1974;84:1732–40. doi: 10.1288/00005537-197410000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Nussbaum M, Cho HT, Som ML. Parotid space tumors of non-salivary origin. Ann Surg. 1976;183:10–2. doi: 10.1097/00000658-197601000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stout AP. Tumors of the Peripheral Nervous System. Section II Fascicle 6. Washington DC: AFIP; 1949. Atlas of Tumor Pathology; pp. 15–6. [Google Scholar]
- 8.Conley J, Janecka I. Neurilemmoma of the facial nerve. Plast Reconstr Surg. 1973;52:55–60. doi: 10.1097/00006534-197307000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Kurtkaya-Yapicier O, Scheithauer B, Woodruff JM. The pathobiologic spectrum of Schwannomas. Histol Histopathol. 2003;18:925–34. doi: 10.14670/HH-18.925. [DOI] [PubMed] [Google Scholar]
- 10.Kapila K, Mathur S, Verma K. Schwannomas: A pitfall in the diagnosis of pleomorphic adenomas on fine-needle aspiration cytology. Diagn Cytopathol. 2002;27:53–9. doi: 10.1002/dc.10121. [DOI] [PubMed] [Google Scholar]
- 11.Siddaraju N, Badhe BA, Goneppanavar M, Mishra MM. Preoperative fine needle aspiration cytologic diagnosis of spindle cell myoepithelioma of the parotid gland: A case report. Acta Cytol. 2008;52:495–9. doi: 10.1159/000325561. [DOI] [PubMed] [Google Scholar]
- 12.Kajor M, Gierek T, Markowski J, Pajak J. Schwannomalike mixed tumor of the parotid gland: A case report. Acta Cytol. 2006;50:529–30. doi: 10.1159/000326007. [DOI] [PubMed] [Google Scholar]
- 13.Chong KW, Chung YF, Khoo ML, Lim DT, Hong GS, Soo KC. Management of intraparotid facial nerve schwannomas. Aust N Z J Surg. 2000;70:732–4. doi: 10.1046/j.1440-1622.2000.01941.x. [DOI] [PubMed] [Google Scholar]


