Abstract
Background:
Designing effective vocational programs for persons with spinal cord injury (SCI) is essential for improving return to work outcome following injury. The relationship between specific vocational services and positive employment outcome has not been empirically studied.
Objective:
To examine the association of specific vocational service activities as predictors of employment.
Method:
Secondary analysis of a randomized, controlled trial of evidence-based supported employment (EBSE) with 12-month follow-up data among 81 Veteran participants with SCI.
Results:
Primary activities recorded were vocational counseling (23.9%) and vocational case management (23.8%). As expected, job development and employment supports were the most time-consuming activities per appointment. Though the amount of time spent in weekly appointments did not differ by employment outcome, participants obtaining competitive employment averaged significantly more individual activities per appointment. Further, for these participants, job development or placement and employment follow-along or supports were more likely to occur and vocational counseling was less likely to occur. Community-based employment services, including job development or placement and employment follow-along or supports as part of a supported employment model, were associated with competitive employment outcomes. Office-based vocational counseling services, which are common to general models of vocational rehabilitation, were associated with a lack of employment.
Conclusions:
Vocational services that actively engage Veterans with SCI in job seeking and acquisition and that provide on-the-job support are more likely to lead to employment than general vocational counseling that involves only job preparation.
Keywords: employment, supported, rehabilitation, vocational, social reintegration, spinal cord injury, unemployment, Veterans, vocational services
Despite advances in medical care and legislative efforts aimed at improving employment for persons with disabilities, rates of return to work following spinal cord injury (SCI) have remained low.1–3 Although rehabilitation professionals and consumers acknowledge that vocational issues need careful consideration as part of a comprehensive rehabilitation program, there is no standard in the field for what type of vocational rehabilitation (VR) programs should be included or which vocational services are most effective for persons with SCI who wish to return to employment. Despite the critical need for effective services, there is a notable lack of controlled studies to inform the field on best VR practices for persons with SCI. Furthermore, wide variability in the availability, access, and quality of services and in the terms used to describe them across and within health care settings poses a significant challenge to understanding the critical features that lead to successful outcomes.
Commonly used to refer to state or federal programs, vocational rehabilitation is a broad term that encompasses an array of services to help a person become employed or re-enter the workforce after illness or disability. Examples of services include assessment to determine eligibility and needed supports, job skills training or education, social skills training, job development, determination of supports necessary to secure employment, assistance with placement and retention, observation or supervision of the employed person, and follow-up support to reinforce and stabilize job placement.4 Also, services are typically provided on a time-limited basis in 3 phases: assessment, job placement, and follow-along support. Traditionally in VR for persons with disabilities, contact and affiliation with the health care team treating the illness or injury are limited. One retrospective study of a large cohort of persons with SCI served by state VR agencies examined the types of vocational service patterns associated with employment outcomes.5 Of 16 vocational services analyzed, job placement best predicted a positive employment outcome. Results also found that this service was underutilized.
Individual placement and support (IPS), often referred to as evidence-based supported employment (EBSE) in the Veterans Health Administration (VHA), is a standardized approach to integrating vocational services into clinical care to better help persons with disabilities find employment in the community.6 In this model, specific principles strictly guide service delivery and, unlike traditional VR, the client plays a much larger role in job choice and development and many more services are provided in the field – that is, the client’s community.7 Randomized clinical trials have demonstrated the effectiveness of IPS for patients with serious mental illness. Compared with other forms of VR, IPS has been found to be more than twice as effective in obtaining competitive employment (CE), a job in the community paying minimum wage or higher that is not set aside only for persons with disabilities. IPS also shortens the time to first employment and increases the number of annualized weeks worked.8 The effectiveness of the IPS model for persons with SCI was tested in a multisite, randomized controlled trial that compared EBSE with vocational treatment as usual (TAU) in VHA SCI Centers.9 The trial was an example of early integration of EBSE into medical rehabilitation. This trial showed that, even with only “fair” implementation of the model, EBSE was 2.5 times more likely than TAU to result in CE (25.9% vs 10.5%, respectively). The implications and impact of specific VR activities, however, remain unclear. The purpose of this analysis was to determine whether, among a cohort of Veterans with SCI undergoing EBSE, the type or amount of EBSE services would predict attainment of CE.
Methods
Study population
The present research was part of a larger 3-year randomized control trial comparing EBSE to TAU provided for 12 months each to unemployed Veterans with SCI who were 18 to 65 years of age and receiving medical and/or rehabilitation health care services at 1 of 6 VHA SCI Centers.3,9 Individuals with substance abuse or psychotic disorders who were not being actively treated for these mental health conditions were excluded. Individuals with other mental health conditions and medical co-morbidities, including traumatic brain injury, were allowed to enroll in the study as long as they had the capacity to provide informed consent. Given the clear success of the EBSE intervention in the trial and the relatively small number of competitive jobs obtained in the other groups, this analysis was restricted to the EBSE group (N = 81).
Study condition
Participants in the EBSE condition received the IPS model of EBSE without modification, as the model is considered disability neutral. The study sought to follow the evidence-based principles of supported employment as closely as possible, including integrated vocational and medical rehabilitation treatment, rapid engagement in job finding, competitive employment, inclusion regardless of severity or type of disability, ongoing job support, and focus on participant preferences. Services were primarily provided in the community, rather than in hospital or office settings. Access to personalized benefits counseling was included.
Services were provided by vocational rehabilitation counselors hired specifically for the study. After being trained both in EBSE and in information about the basic care and management of SCI, the counselors were integrated into the existing SCI interdisciplinary care team in the SCI Centers.
Measures
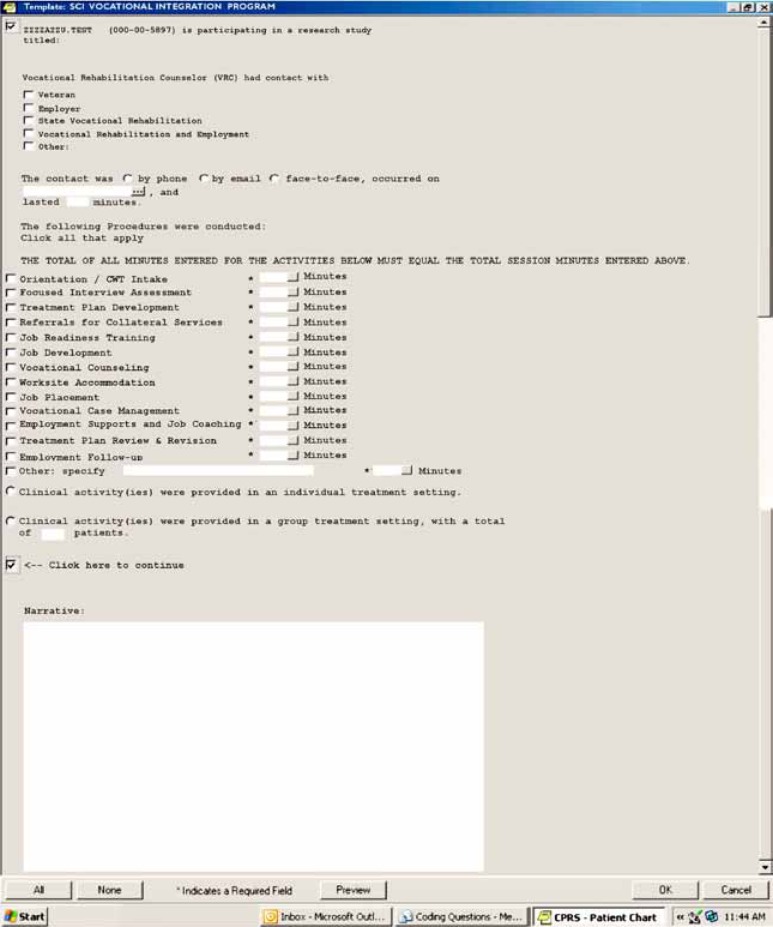
Demographic data, medical data, social security benefits information, and prior employment data were obtained through subject interviews and medical chart extraction. The IPS Fidelity Scale was used to measure the study’s adherence to the supported employment model.10 To enable vocational counselors across study sites to document service activities at the time they were delivered in a standardized and efficient manner, they recorded vocational service activities using a progress note form that was integrated into the patients’ electronic medical record. As part of their initial training, counselors were provided a documentation manual and were trained in using the electronic medical record form to document EBSE services per study definitions (Table 1). Ongoing training on documenting service delivery was provided at monthly conference calls and at annual meetings over the 3 years of the study. Using the electronic form (Figure 1), counselors provided details on both the types of services they provided and the time spent on each. In summary, the services included face-to-face interviews and counseling, telephone counseling, and meetings with potential and actual employers both in person and on the phone with or without the participant being present.
Table 1. Types and definitions of vocational service activities.
| Vocational service activity | Definition |
| Orientation/CWT intake | Provide Veteran with an understanding of how the program works and what supports the vocational rehabilitation counselor will provide |
| Focused interview assessment | Establish a working plan for the ongoing assessment process that will lead to community networking and job development |
| Treatment plan development | Integrate the information gained in the orientation, through focused assessment and through the initial community exploration and networking, into the primary clinical team treatment plan format |
| Referrals for collateral services | Refer to nonintegrated, clinical team programs to address job placement or training |
| Job readiness training | Provide services, supports, training programs, and/or referrals to other interventions that are intended to get the Veteran ready to go to work versus direct job placement with support |
| Job development | Employer networking and negotiation based on the Veteran’s interests and preferences |
| Vocational counseling | Provide office-based or telephone guidance to the Veteran on how to get and keep jobs; sometimes includes interview training and interpersonal skills training |
| Worksite accommodation | Provide information, resources, equipment, or modifications to aid productivity, eg, schedules, workspace, equipment, personnel support |
| Job placement | Advocacy, actions, and negotiations with personnel in the employment setting to secure the job and make arrangements for the Veteran to start the job |
| Vocational case management | Actions and supports specific to the Veteran’s job development preferences intended to enhance employability, eg, help in getting work clothing, advocate with family or community resources to assist with transportation to and from work |
| Employment supports and job coaching | Hands-on, face-to-face training and support in the workplace to improve the Veteran’s comfort, mobility, relationships, personal care, and overall work function |
| Treatment plan review and revision | Return to the employment plan and treatment plan to update and reflect on better strategies to attain the stated goal of job placement or job retention support |
| Employment follow-up | Support to both the Veteran and employer/co-workers to safeguard Veteran’s productivity, safety, and satisfaction in addition to employer’s satisfaction |
Note: CWT = compensated work therapy.
Figure 1. Vocational service activity form integrated in participants’ electronic medical record.
Statistical analysis
Data are presented as mean ± standard deviation or frequency and percent, where appropriate. The primary dependent variable for all models was CE (yes/no) defined as a paying job earning at least minimum wage in the community. Volunteer work and sheltered employment did not qualify as employment. Comparisons were made between those participants obtaining CE and those who did not using Student’s t test or chi-square test, where appropriate. Rates of CE are presented as percent employed per group with 95% Wald confidence intervals (CIs) with normal approximation and were performed with an intent-to-treat approach. All randomly assigned participants for whom data are available contributed to employment analyses. All analyses were performed with SAS (Version 9.2; SAS Inc., Cary, NC).
Results
Participant characteristics
The 81 EBSE participants were primarily men, middle aged, with a high school education, and Caucasian (about 50%) (Table 2). Over half of the study sample received any VA benefits (61.7%; n = 50); of those participants, 62.0% (n = 31) received service-connected benefits, meaning financial compensation based on their disability being related to their military service (a benefit not affected by income earned). Among those receiving VA benefits, 23.8% (n = 19) were receiving service-connected benefits for SCI. Time since injury varied widely as did the levels of impairment, which were described by combining the American Spinal Injury Association Impairment Scale (AIS) ratings and neurologic levels.11 The cause of SCI was mainly motor vehicle accident (35.0%; n = 30) or gunshot wound (18.5%; n = 15).
Table 2. Demographic characteristics of persons with spinal cord injury who received evidence-based supported employment serivices.
| Characteristicss | EBSE (n=81) |
| Age, mean years (SD) | 48.7 (9.8) |
| Education, mean years (SD) | 13.1 (2.3) |
| Race, n (%) | |
| White | 37 (45.7) |
| African American | 29 (35.8) |
| Hispanic | 5 (6.2) |
| Marital status, n (%) | |
| Married | 30 (37.0) |
| Divorced | 28 (34.6) |
| Time since injury, mean years (SD) | 11.7 (11.2) |
| AIS and neurologic status, n (%) | |
| High tetraplegia, AIS A,B,C | 12 (15.0) |
| Low tetraplegia, AIS A,B,C | 5 (6.3) |
| Paraplegia, AIS A,B,C | 38 (47.5) |
| AIS D/E | 25 (31.3) |
| A | 26 (32.5) |
| B | 11 (13.8) |
| C | 18 (22.5) |
| D | 25 (31.3) |
| E | 0 (0.0) |
Note. AIS = American Spinal Injury Association Impairment Scale.
Results of the 15-item IPS Fidelity Scale that was administered every 6 months showed that scores did not differ over time or between sites (F7,18 = 0.8, P < .619; range, 59-68). Site scores on the Fidelity Scale across the 3-year study enrollment period averaged 63.4 ± 2.5, which falls within the upper portion of the “fair” range for implementation of the IPS model. During the 12 months of the study, attrition was 17.3% (14 of 81). Reasons for withdrawal were early exit/loss to follow-up (64.3%; n = 9) or withdrawal by investigator (35.7%; n = 5).
Employment and vocational service activities
The employment rate was greater than 25% (95% CI, 20.8-40.4) (Table 3). Average weekly wages and weekly hours worked were $233.9 ± 279.0 and 22.0 ± 14.6 hours, respectively. Appointments were conducted face to face for 56%, by telephone for 38.6%, and by e-mail for 3.9%; this information was missing for 1.7%. Individual appointments were preferred (98.8%) over group appointments (1.2%).
Table 3. Competitive employment (CE) rates during 1 year of evidence-based supported employment for persons with spinal cord injury (N = 81).
| Employment | CE rates |
| Total jobs, n (%) | 50 (NA) |
| Unique participants with job, n (%) | 21 (25.9) |
| Employment rate (95% CI) | 25.9 (17.6-36.5) |
Note: No percentages (NA) are given for total jobs as participants were allowed to have multiple jobs and there is no expressed denominator.
Vocational activities are delineated in Tables 4 and 5. Table 4 shows weekly vocational activities per quarter visit for participants obtaining CE versus none. As expected, the number of vocational activities declined over time. Study participants averaged 1.2 ± 0.5 vocational activities per visit, with no statistically significant changes (P < .753) observed from quarter 1 to 4 between either group.
Table 4. Weekly recorded vocational service activity for participants receiving evidence-based supported employment for 1 year who did or did not obtain competitive employment (CE).
|
Quarter 1 (N = 81) |
Quarter 2 (N = 75) |
Quarter 3 (N = 68) |
Quarter 4 (N = 57) |
|||||
| Parameter |
No CE (n = 60) |
CE (n = 21) |
No CE (n = 54) |
CE (n = 21) |
No CE (n = 49) |
CE (n = 19) |
No CE (n = 41) |
CE (n = 16) |
| Number of recorded VS activities | 745 | 273 | 672 | 264 | 593 | 232 | 499 | 186 |
| VS activity, mean ± SD | 1.2 ± 0.5 | 1.3 ± 0.6 | 1.2 ± 0.5 | 1.2 ± 0.5 | 1.2 ± 0.4 | 1.3 ± 0.6 | 1.2 ± 0.5 | 1.2 ± 0.4 |
Note. Participants only included if ≥ 1 vocational service activity occurred per quarter. VS activity, mean ± SD
Table 5. Distribution of vocational service activities and average time spent on that activity for participants receiving evidence-based supported employment (EBSE).
|
All EBSE participants (N = 81) |
No competitive employment (n = 60) |
Competitive employment (n = 21) |
||||
| Activity | n (%) | Mean ± SD | n (%) | Mean ± SD | n (%) | Mean ± SD |
| Orient/CWT intake | 150 (2.4) | 32.9 ± 20.0 | 108 (2.7) | 32.3 ± 19.5 | 42 (2.0) | 34.5 ± 21.4 |
| Focused interview | 407 (6.6) | 37.0 ± 31.7 | 273 (6.8) | 34.5 ± 24.3* | 134 (6.3) | 41.9 ± 42.6 |
| Treatment plan development | 120 (1.9) | 43.2 ± 22.9 | 66 (1.6) | 39.5 ± 19.3 | 54 (2.5) | 47.5 ± 26.2 |
| Referral for collateral services | 62 (1.0) | 38.3 ± 75.3 | 44 (1.1) | 35.0 ± 87.7 | 18 (0.8) | 46.7 ± 26.6 |
| Job readiness | 139 (2.3) | 49.6 ± 36.6 | 89 (2.2) | 49.7 ± 39.6 | 50 (2.3) | 49.3 ± 31.3 |
| Job development | 1,402 (22.7) | 57.9 ± 44.8 | 835 (20.7)*** | 56.8 ± 44.3 | 567 (26.6) | 59.5 ± 45.6 |
| Vocational counseling | 1,475 (23.9) | 33.1 ± 24.9 | 1,149 (28.4)*** | 32.2 ± 25.2** | 326 (15.3) | 36.3 ± 23.2 |
| Worksite accommodations | 13 (0.2) | 31.1 ± 30.8 | 6.0 (0.1)* | 25.0 ± 18.2 | 7.0 (0.3) | 35.8 ± 38.3 |
| Job placement | 42 (0.7) | 50.5 ± 38.6 | 14 (0.3)*** | 59.1 ± 49.2 | 28 (1.3) | 46.1 ± 32.0 |
| Vocational case management | 1,470 (23.8) | 22.2 ± 20.8 | 946 (23.4) | 21.7 ± 20.2 | 524 (24.6) | 23.1 ± 21.8 |
| Employment supports | 169 (2.7) | 55.8 ± 42.4 | 41 (1.0)*** | 45.6 ± 31.3 | 128 (6.0) | 59.2 ± 45.1 |
| Treatment plan | 137 (2.2) | 37.0 ± 18.1 | 84 (2.1) | 38.7 ± 17.7 | 53 (2.5) | 34.5 ± 18.5 |
| Employment follow-up | 266 (4.3) | 35.6 ± 23.2 | 87 (2.2)*** | 39.8 ± 22.5 | 179 (8.4) | 33.5 ± 23.4 |
| Other activities | 1,398 (22.6) | 21.5 ± 15.0 | 908 (22.5) | 20.0 ± 13.2*** | 490 (23.0) | 24.4 ± 17.5 |
| Avg. number of activities | – | 1.17 ± 0.5 | – | 1.15 ± 0.5*** | – | 1.22 ± 0.5 |
| Avg. minutes of activity | – | 42.5 ± 40.5 | – | 39.9 ± 39.1*** | – | 47.4 ± 42.7 |
Note. Percentage reflects documented endorsed vocational service (VS) activity, if reported, and time spent on that activity. Per subject, the maximum number of weekly VS activities was 14, with each potential VS activity endorsed 52 times over the course of 1 year (1 per week). Mean time reflects average time per documented activity. CWT = compensated work therapy. Comparisons are between employment groups.
P < .05.
P .01.
P < .001.
When vocational activities are stratified by those participants obtaining CE or not (Table 5), numerous patterns emerge. Primary activities recorded were vocational counseling (23.9%) and vocational case management (23.8%). As expected, job development (57.9 ± 44.8 minutes) and employment supports (55.8 ± 42.4 minutes) were the most time-consuming activities per appointment. There was not a statistically significant difference observed in participants obtaining CE for minutes per weekly appointment (42.7 ± 13.71 vs 39.9 ± 39.9; P < .153), but there was a statistically significant difference observed for individual activities per appointment (1.1 ± 0.5 vs 1.2 ± 0.5; P < .038). Further, participants obtaining CE were more likely to receive job development (26.6% vs 20.7%), job placement (1.3% vs 0.3%), and employment follow-up (8.4% vs. 2.2%) and less likely to receive vocational counseling (15.3% vs 28.4%)
Discussion
This study examined how the amount and the type of vocational activities delivered within the context of an EBSE program for Veterans with SCI were related to employment outcomes. Although the time spent on vocational services was the same for those who did and did not obtain CE, a greater variety of services on a weekly basis was received by those who did obtain CE than those who did not. Moreover, the data suggest that the percentage of time spent engaging in specific vocational activities had a distinct relationship to employment outcomes, with certain activities more likely to be associated with positive outcomes than others. Specifically, job development, job placement, employment supports, job coaching, and follow-up occurred more often for those who obtained CE than those who did not, whereas vocational counseling and interviews occurred more often for those who did not obtain CE. No association with CE was detected for other more generic vocational activities such as orientation/ intake, treatment planning, or referrals for other services.
Of the documented activities examined, community-based vocational activities were more likely to be associated with CE. These activities align closely with the IPS model of EBSE, which uses assertive community engagement to rapidly find work in the individuals’ desired setting. Specifically, job development and placement activities, which involved vocational providers networking with community employers and then negotiating appropriate work placement and conditions with and on behalf of the person with SCI, were effective in securing CE. Support of persons as they transition into the workplace is also critical to successful CE. In this study, employment supports involved hands-on training and problem solving in the workplace to ensure the ongoing satisfaction of the Veteran employee with productivity and the employer with the placement. Vocational counselors were encouraged to involve the SCI treatment team in providing employment supports including activities such as worksite evaluations and accommodations.
The finding of the importance of job development and placement to CE outcomes is consistent with previous research examining vocational services in the state VR system among persons with SCI5 and other disabilities.12 There is certainly some variation in how these services are delivered between specific IPS programs and state VR. In our study, job development and placement was a direct patient care service provided by the vocational counselor as part of an integrated program of EBSE in SCI care. The activity often involved working with the employer to “carve out” a new position where one did not previously exist, in order to use the unique skills of the Veteran with SCI to fill an unmet business need. In state VR systems, job placement is often obtained by referral to another service provider, such as a private employment agency, and has more of a job-matching focus, where the person with the disability is matched to an available position. Notwithstanding these differences, the data suggest that persons with SCI as well as other disabilities benefit from a skilled professional who can access community employers on behalf of clients. This advocacy function is strengthened when the vocational counselors can act as a liaison with health care providers following a change in physical or mental functioning. In the IPS EBSE for SCI program described here, this service was provided directly by the vocational counselor who was part of the interdisciplinary care team. As such, the vocational counselor had direct access to the clinical team to address concerns, limitations, or barriers that the Veterans and employers might identify in the workplace. By integrating vocational services within the medical rehabilitation health care setting, barriers could be addressed with Veterans as they began a job search and after the job was obtained as new issues emerged. In more traditional VR models, a referral to an outside VR service provider is made at the conclusion of a health care episode, with little or no linkage between VR and the teams to address the health care needs of persons with SCI.
Collectively, these research findings argue for a paradigm shift away from conventional wisdom that holds that a person with a significant catastrophic disability, such as SCI, needs to spend time in prevocational activities such as independent living and/or “work hardening” programs that focus on job readiness. Instead, rehabilitation programs and the persons they serve would garner a greater return on investment with time spent in a variety of vocational activities that focus on rapidly finding real jobs and obtaining appropriate supports in the community. While a small number of individuals who have certain characteristics such as less severe injuries, higher educational attainment, and the ability to return to their pre-injury field of employment1–3 may be able to return to work with minimal vocational assistance, the majority of persons who are living with SCI and chronic unemployment, particularly those who also experience other mental, physical or cognitive impairments, require a more intensive and integrated approach to VR.
Limitations
A potential limitation of the present study is that data on vocational services were extracted from the vocational counselors’ clinical progress notes, which annotated the amount and type of vocational services delivered for each patient encounter in the Veterans’ electronic medical record. Although the vocational counselors received training on clinical documentation of service activities, had a manual to refer to, and had refresher trainings on a recurring basis, there is no interrater reliability available for the tool itself, and it is possible that there was variance between providers in how services were recorded.
Another potential limitation may be sample size. Although our study was sufficiently powered to detect an overall treatment effect between groups, no power analysis was conducted for further subanalyses. Initial analyses focused on demographic data and clinical injury characteristics such as medical comorbidities as univariate predictors of CE with the intent of identifying significant parameters to be included in a subsequent multivariate model to examine the effect of EBSE on CE, after controlling for potential confounding and modifying effects. However, no univariate associations were found, thus making multivariate comparisons unnecessary. For future studies, larger sample sizes will be needed to determine significant clinical and demographic predictors aside from the strong treatment effect of EBSE itself.
Conclusions and implications
The results of this study strongly suggest the importance of designing vocational programs for persons with SCI that include actionoriented, community-based services such as job development or placement, employment supports, and follow-up in the workplace. Optimally, these services are integrated with ongoing SCI medical rehabilitation care and delivered by a skilled vocational provider who is either a member of the clinical team or is willing to work closely with the team throughout the employment process. VR efforts that are primarily office-based, such as interviewing, assessments, and general counseling, are less likely to yield results in terms of CE in the community. Although these basic vocational activities may be a part of most vocational programs, the time spent in them should be minimized to that which is necessary to build rapport and formulate an informed, consumerdriven treatment plan to actively search for a job in the community for the person with SCI. Adopting IPS EBSE programs in SCI rehabilitation is a means of including integrated community-based services that have been shown to be effective for this specialized population.
Acknowledgments
Financial support/disclosures: This material is based on work supported by the Office of Research and Development, Rehabilitation Research and Development Service, Department of Veterans Affairs, VA RR&D grant B3773R. Contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government.
Ethics and reporting requirements: The trial was approved by the IRB of the Research and Development Committee of the James A. Haley Veterans’ Hospital, and each participating study site obtained approval from its respective IRB.
Conflicts of interest: The authors declare no conflicts of interest.
Additional contributions: We gratefully acknowledge the site investigators, study coordinators, and counselors who contributed to this study and Lynn Dirk, MAMC, for editorial assistance with this manuscript.
Clinical Trial Registration: NCT00117806.
References
- 1.Krause JS, Terza JV, Dismuke CE.Factors associated with labor force participation after spinal cord injury. J Vocational Rehabil. 2010;33(2):89–99. [Google Scholar]
- 2.Krause J, Kewman D, DeVivo M, et al. Employment after spinal cord injury: An analysis of cases from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil. 1999;80(11):1492–1500. [DOI] [PubMed] [Google Scholar]
- 3.Ottomanelli L, Lind L.Review of critical factors related to employment after spinal cord injury: Implications for research and vocational services. J Spinal Cord Med. 2009;32(5):503–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rehabilitation Act of 1973. Pub. L. 93-112. http://www.usbr.gov/cro/pdfsplus/rehabact.pdf Accessed August28, 2014.
- 5.Marini I, Lee GK, Chan F, Chapin MH, Romero MG.Vocational rehabilitation service patterns related to successful competitive employment outcomes of persons with spinal cord injury. J Vocational Rehabil. 2008;28(1):1–13. [Google Scholar]
- 6.Bond GR.Supported employment: Evidence for an evidence-based practice. Psychiatric Rehabil J. 2004;27(4):345–359. [DOI] [PubMed] [Google Scholar]
- 7.Bond GR, Becker DR, Drake RE, et al. Implementing supported employment as an evidence-based practice. Psychiatr Serv. 2001;52(3):313–322. [DOI] [PubMed] [Google Scholar]
- 8.Bond GR, Drake RE, Becker DR.An update on randomized controlled trials of evidence-based supported employment. Psychiatr Rehabil J. 2008;31(4):280–290. [DOI] [PubMed] [Google Scholar]
- 9.Ottomanelli L, Goetz LL, Suris A, et al. Effectiveness of supported employment for veterans with spinal cord injuries: results from a randomized multisite study. Arch Phys Med Rehabil. 2012;93(5):740–747. [DOI] [PubMed] [Google Scholar]
- 10.Bond GR, Becker DR, Drake RE, Vogler KM.A fidelity scale for the individual placement and support model of supported employment. Rehabil Couns Bull. 1997;40:265–284. [Google Scholar]
- 11.Marino R, ed. International Standards for Neurological Classification of Spinal Cord Injury. 5th ed. Chicago, IL: American Spinal Injury Association; 2000. [Google Scholar]
- 12.Bolton BF, Bellini JL, Brookings JB.Predicting client employment outcomes from personal history, functional limitations, and rehabilitation services. Rehabil Couns Bull. 2000;44(1):10–21. [Google Scholar]