Abstract
Subclavius posticus is a rare anomalous muscle that traverses from the costal cartilage of the first rib posterolaterally to the superior border of the scapula. We present an athlete who presented with incapacitating suprascapular nerve compression associated with a subclavius posticus diagnosed by MRI. Symptoms were relieved, and function was restored by decompression of the nerve and excision of the anomalous muscle. We present this case to bring awareness of the subclavius posticus as an anatomic variant and a potential additional source for compression in suprascapular neuropathy. We recommend high-resolution magnetic resonance imaging to evaluate cases of isolated suprascapular neuropathy.
Level of Evidence: V
Introduction
Subclavius posticus (SP) is a rare anomalous muscle that traverses from the costal cartilage of the first rib posterolaterally to the superior border of the scapula. First described by Rosenmuller in 1800 [1], SP travels cephalad to the brachial plexus and subclavian artery and vein. Akita reported an incidence of 8.9 % in 124 cadaver dissections [1].
A number of cadaveric studies have speculated that subclavius posticus can be a potential cause of thoracic outlet syndrome [1, 4]. It has also been suggested that the anomalous muscle may be a factor causing Paget-von Schroetter syndrome [1].
We present a 49-year-old male who presented with signs and symptoms of suprascapular nerve compression 5 months after a fall from his bicycle. Magnetic resonance imaging identified a subclavius posticus surrounding his suprascapular nerve. Excision of the anomalous muscle led to rapid resolution of his weakness.
Case Report
A 49-year-old right hand-dominant male “iron man” triathlete fell from his bike during training in September 2011 and sustained a left distal clavicle fracture, left rib fractures, and left pneumothorax. His clavicular fracture was treated with a sling for comfort, followed by formal physical therapy after 4 weeks. He reported an uneventful recovery. In December, he noted new onset of weakness and stiffness about his left shoulder with no additional trauma. He initiated his own therapy by swimming but was unable to maintain his preinjury pace or endurance. He sought evaluation for his left shoulder. His chief complaint was a loss of shoulder range of motion and pain at the extremes of motion.
Upon evaluation, his left shoulder elevation measured 130°, abduction 140°, external rotation (ER) 30°, and internal rotation (IR) to L1. By comparison, he had full overhead elevation on the right, ER of 80°, and IR to T6. Strength of ER was 3/5, IR 5/5, and abduction 4/5. He had obvious atrophy about the scapular spine with no winging. He did have signs of impingement with a positive Hawkins and Neer test.
An outside MRI of the left shoulder was consistent with rotator cuff tendonopathy and a healed distal clavicle fracture. No masses or other anomalies were identified by an independent reading from our chief of MR radiology. Because of suboptimal spatial resolution of the nerves, we recommended a high-resolution MRI tailored to optimize imaging of the upper trunk and suprascapular nerve. Of note, the outside MRI utilized fat suppression in three planes, which obscured the muscle fat contrast resolution. The new MRI acquired oblique coronal MR images from the axial images directly in the plane of the plexus, using relatively high spatial resolution (390 μm in the frequency direction) as well as good through plane resolution (2 mm with no interslice gap). Fat suppression was only applied in one plane to assess for any perineural edema. The study revealed an anomalous muscle that traversed the plexus, originating on the superolateral cartilaginous margin of the first rib and inserting upon the superior border of the scapula (Figs. 1 and 2). The suprascapular nerve was identified, entering the muscle and exiting just prior to the suprascapular notch. No distinct notch compression or soft tissue mass could be identified. There was also a hypertrophic nonunion of the distal clavicle with thickening and interstitial injury of the coracoclavicular ligament as well as edema about the posterior margin of the serratus anterior. Changes about the serratus anterior were presumed to be related to scapular dyskinesia and overuse.
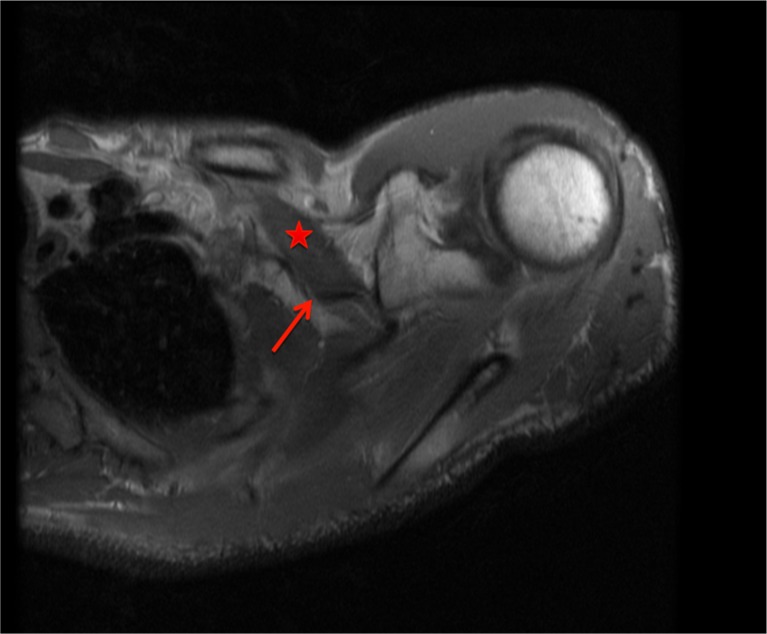
Fig. 1.
Axial MRI cross section at the level of the coracoid process demonstrating a large muscle (star) obliquely traversing the brachial plexus in an anteroposterior direction. The suprascapular nerve is visualized coursing immediately medial to the muscle and entering the muscle belly (arrow)
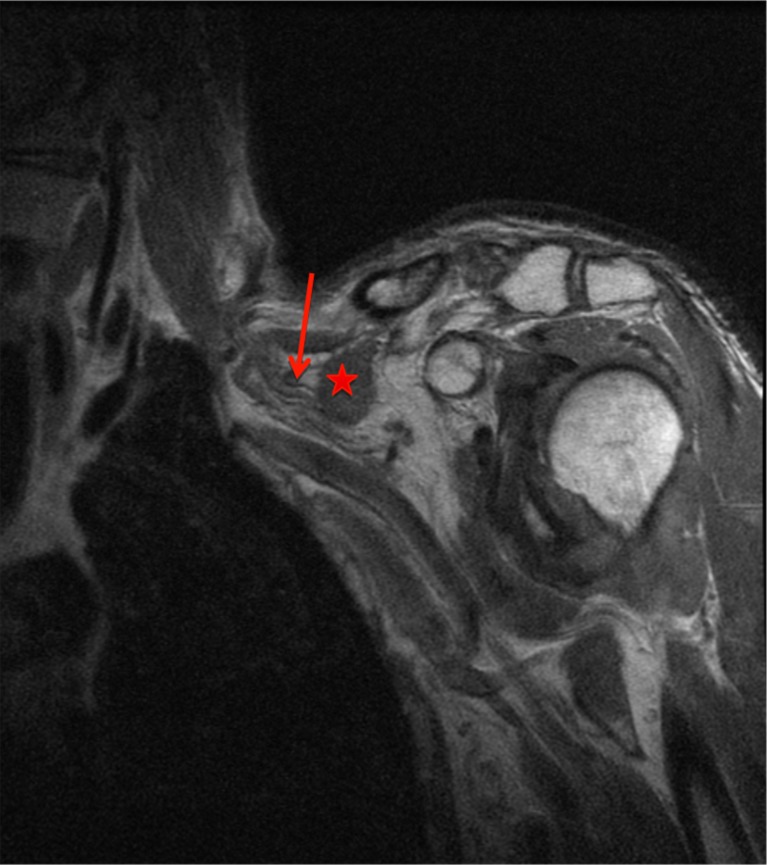
Fig. 2.
Coronal section demonstrating the muscle in cross section (star) just medial to the coracoid process and the suprascapular nerve immediately medial to the muscle (arrow)
Electrodiagnostic testing was performed to evaluate the acuity of the weakness, conduction along the suprascapular nerve, as well as any electromyographic findings in the periscapular musculature. This revealed complete denervation of the supra- and infraspinatus muscles, with moderate to severe abnormal spontaneous activity and no detectable motor units. There was no evidence of axonal regeneration, and all other periscapular muscles were normal.
Given the clinical presentation, lack of improvement at 5 months following injury, complete denervation shown on the EMG, and MRI findings of an anomalous muscle potentially compressing the suprascapular nerve, we recommended exploration and decompression of the suprascapular nerve with excision of the anomalous muscle.
The patient was taken to the operating room and placed in a beach chair position with a rolled gel pad medial to the left scapula. The initial dissection was performed from a standard superior approach to the brachial plexus. The omohyoid and large neighboring anomalous muscles were immediately identified. Dissection medially revealed a normal suprascapular nerve at its takeoff from the upper trunk. We followed the nerve a few centimeters distally to reveal its entry into the subclavius posticus. Due to the size of the muscle, we were unable to visualize the distal portion of the muscle and nerve from the superior approach. We extended the incision with a 5-cm “T” across the clavicle and just medial to the coracoid process and made an anterior, subclavicular approach to the suprascapular nerve [3]. This approach enabled improved visualization of the inferior and posterior aspect of the subclavius posticus as well as the exit of the suprascapular nerve (SSN) from the muscle belly. There was no apparent encroachment by fracture callus of the distal clavicle. The muscle was removed in its entirety by visualizing and sparing the nerve (Fig. 3). We could not, however, visualize the scapular notch through the combined approach with sufficient clarity to divide the suprascapular notch ligament, which appeared to be circumferentially ossified. The final portion of the decompression was performed from a posterior approach to allow direct access to the suprascapular notch. A 5-cm transverse incision was made just superior to the scapular spine. The transverse fibers of the trapezius were split to identify the atrophied supraspinatus, and the superior border of the scapula was palpated and traced to the base of the coracoid process. The suprascapular artery was identified to be superior to the notch, and the ossified transverse scapular ligament was released using Kerrison rongeurs. Despite the ossification of the ligament, the diameter of the notch appeared grossly normal. There appeared to be no kinking, traction, or compression of the nerve at the notch.
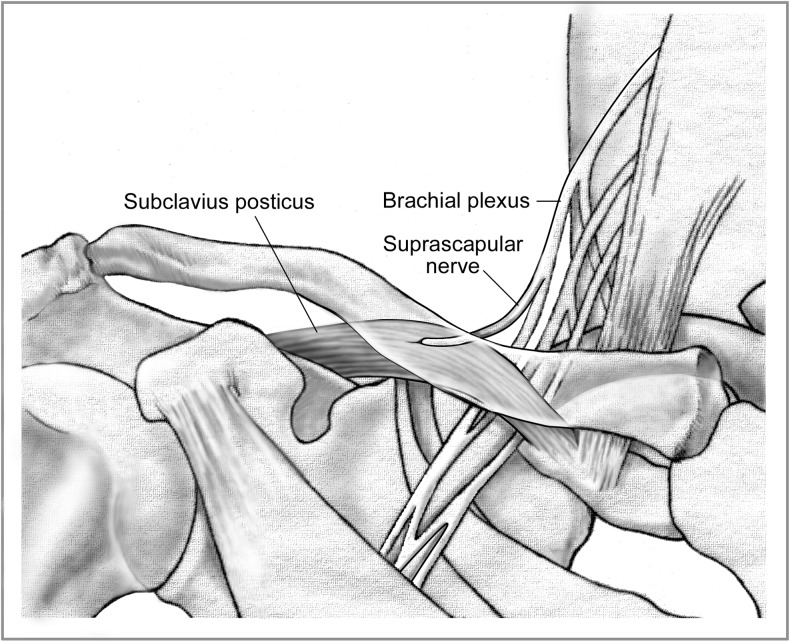
Fig. 3.
Drawing demonstrating the relationship of the SP to the first rib, scapular spine, and neurovascular structures of the thoracic outlet (Benjamin Goode, bengoode@charter.net)
At the first follow-up visit 2 weeks following surgery, our patient reported alleviation of all preoperative pain. His shoulder range of motion was unchanged. At 6 weeks postoperatively, he reported an increase in range of motion and subjectively increased strength. Shoulder elevation and abduction measured 130°. He could externally rotate against 4/5 resistance to 60° from neutral. Scaption strength (fully extended elbow, shoulder abduction to 90° in the plane of the scapula with thumb pointing toward the floor) measured 4/5. Both the supra- and infraspinati were actively contracting. There was no tenderness over the wounds. An EMG of the infra- and supraspinatus muscles at 3 months postoperatively showed evidence of significant axonal regeneration of both muscles with nascent units. At 6 months follow-up, he had regained full range of motion through his left shoulder, strength had returned to 5/5 in all muscle groups, and he was pain free. He had normal bulk and contour of the supra- and infraspinatus muscles. He also returned to triathlete competitions and recorded his personal best time.
Discussion
Previous reports of the subclavius posticus (SP) muscle come predominantly from cadaveric dissections [5, 10, 13]. There are few reported cases in the literature about this muscle causing clinical symptoms. Ozcakar et al. reported on an instance of subclavius posticus in a 30-year-old man who presented with traumatic brachial plexopathy with underlying thoracic outlet syndrome. Resection of a rudimentary rib, the first rib, and SP resulted in alleviation of pain and improved muscle strength [8].
Anatomic studies on SP define the origin at the first rib and insertion on the superior border of the scapula, adjacent to the insertion site of the omohyoid muscle just medial to the suprascapular notch. In a Weister rat study in 1998, Tanaka found that the muscle might develop from an anlage of the hypobranchial musculature near and/or in the junctional region between the hypobranchial and pectoral regions at midline. It was proposed that this region might phylogenetically and ontogenetically undergo remarkable changes, concomitantly with the development of the heart and lungs, to which variations of this muscle and its innervation could be attributed [14].
The innervation that has been described in the literature is variable and corroborates Tanaka’s study. Some cadaveric studies have shown the innervation as coming from the subclavius [2], others describe it from the nerve to the omohyoid from the ansa cervicalis [1], and others have shown the suprascapular nerve as the source of innervation [4, 8, 13]. Our muscle appeared to be innervated by the suprascapular nerve, though we do not have formal electrodiagnostic testing.
Given SP’s intimate relationship to the brachial plexus and subclavian artery and vein, the SP muscle has been suggested as a potential source of compression (Fig. 3). It could be a factor causing Paget-von Schroetter syndrome, which is recognized as spontaneous or effort-related thrombosis of the axillo-subclavian vein [10, 12]. Subclavian vascular compression has been described by several authors in association with the SP [4, 9, 11], though to our knowledge, excision of the muscle has not been reported in the literature to relieve the condition. SP has also been reported as a potential factor in thoracic outlet syndrome, as first suggested by Akita et al. [1]. Forcada et al. reported an instance of SP in a cadaver in which the surface of the brachial plexus in contact with the anomalous muscle showed a groove, which could be interpreted as compression [4].
Suprascapular neuropathy in athletes has been reported in a number of case reports. Niemann et al. reported on a 20-year-old baseball pitcher who developed right posterior shoulder pain during throwing [7]. After attempting conservative treatment, electrodiagnostic testing showed decreased nerve conduction of the suprascapular nerve. Twenty-two weeks after SSN release, the patient was able to return to pitching. In a recent literature review of suprascapular neuropathy, Moen et al. associate SSN injuries with overhead athletes, particularly volleyball players and baseball players [6]. To our knowledge, no cases of SSN neuropathy in a triathlete have been reported.
We present this case to bring awareness of the subclavius posticus as an anatomic variant and a potential source for compression in brachial plexus or suprascapular neuropathy. We recommend high-resolution magnetic resonance imaging to evaluate complex cases of nerve entrapment, as in this case of suprascapular neuropathy.
Acknowledgments
Conflict of Interest
Ashley C. Cogar declares that she has no conflict of interest.
Parker H. Johnsen declares that he has no conflict of interest.
Hollis G. Potter declares that she has no conflict of interest.
Scott W. Wolfe declares that he has no conflict of interest.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 [10].
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
Footnotes
None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
Contributor Information
Ashley C. Cogar, Email: ashleyccogar@gmail.com
Parker H. Johnsen, Phone: 212 606 1529, Email: johnsenp@hss.edu
Hollis G. Potter, Phone: 212 606 1023, Email: potterh@hss.edu
Scott W. Wolfe, Phone: 212 606 1529, Email: wolfes@hss.edu
References
- 1.Akita K, Ibukuro K, Yamaguchi K, Heima S, Sato T. The subclavius posticus muscle: a factor in arterial, venous or brachial plexus compression? Surg Radiol Anat. 2000;22(2):111–5. doi: 10.1007/s00276-000-0111-6. [DOI] [PubMed] [Google Scholar]
- 2.Akita K, Tsuboi Y, Sakamoto H, Sato T. A case of muscle subclavius posticus with special reference to its innervation. Surg Radiol Anat. 1996;18(4):335–7. doi: 10.1007/BF01627613. [DOI] [PubMed] [Google Scholar]
- 3.Bodily KD, Spinner RJ, Sin AY, Bishop AT. Clinical significance of suprascapular nerve mobilization. Clin Anat. 2005;18(8):573–9. doi: 10.1002/ca.20165. [DOI] [PubMed] [Google Scholar]
- 4.Forcada P, Rodriguez-Niedenfuhr M, Liusa M, Carrera A. Subclavius posticus muscle: supernumerary muscle as a potential cause for thoracic outlet syndrome. Clin Anat. 2001;14(1):55–7. doi: 10.1002/1098-2353(200101)14:1<55::AID-CA1010>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 5.Kutoglu T, Ulucam E, Gurbuz H. A case of the subclavius posticus muscle. Trakia J Sci. 2005;3(1):77–8. [Google Scholar]
- 6.Moen TC, Babatunde OM, Hsu SH, Ahmad CS, Levine WN. Suprascapular neuropathy: what does the literature show? J Shoulder Elbow Surg. 2012;21(6):835–46. doi: 10.1016/j.jse.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 7.Niemann AJ, Juzeszyn LS, Kahanov L, Eberman LE. Suprascapular neuropathy in collegiate baseball player. Asian J Sports Med. 2013;4(1):76–81. [PMC free article] [PubMed] [Google Scholar]
- 8.Ozcakar L, Guney MS, Ozdag F, Alay S, Kiralp MZ, Gorur R, et al. A sledgehammer on the brachial plexus: thoracic outlet syndrome, subclavius posticus muscle, and traction in aggregate. Arch Phys Med Rehabil. 2010;91:656–8. doi: 10.1016/j.apmr.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 9.Roos D. Congenital anomalies associated with thoracic outlet syndrome. Anatomy, symptoms, diagnosis and treatment. Am J Surg. 1976;132:771–8. doi: 10.1016/0002-9610(76)90456-6. [DOI] [PubMed] [Google Scholar]
- 10.Sarikcioglu L, Sindel M. A case with subclavius posticus muscle. Folia Morphol. 2001;60(3):229–31. [PubMed] [Google Scholar]
- 11.Shetty YP, Pai MM, Prabhu LV, Vadgaonkar R, Nayak SR, Shivanandan R. The subclavius posticus muscle: its phylogenetic retention and clinical relevance. Int J Morphol. 2006;24(4):599–600. doi: 10.4067/S0717-95022006000500014. [DOI] [Google Scholar]
- 12.Sievert T, Maike HW, Wildmeister W. Paget-von Schroetter syndrome: case description in the light of the literature. Z Gesamte Inn Med. 1991;46:375–80. [PubMed] [Google Scholar]
- 13.Singhal S, Rao V, Manjunath KY. Subclavius posticus muscle—a case report. Int J Morphol. 2008;26(4):813–5. doi: 10.4067/S0717-95022008000400005. [DOI] [Google Scholar]
- 14.Tanaka S, Zukeran C, Nakagawa S. A macroscopical study of the subclavius muscle of rat. Anat Anz. 1998;165(5):417–24. [PubMed] [Google Scholar]