Abstract
Background
Headless compression screws have been used for arthrodesis of the distal interphalangeal joint with good clinical results. However, some distal phalanges are too small, thus precluding their use, or increasing complication rates.
Methods
In order to validate our digital measurements, radiographs of five cadaveric hands were obtained. The distal phalanges of these fingers were measured using our institution’s digital radiograph software. The cadavers were then dissected, and the actual phalanges were measured to confirm the accuracy of the digital measurements; 200 consecutive hand radiographs were then measured to obtain average width and heights of the narrowest measurements of the distal phalanx of each finger. Subgroup analysis of each finger for age and gender was completed.
Results and Conclusions
Females were routinely smaller than their male counterparts. No age-related differences were seen. A substantial number of fingers were found to be too small to allow for use of headless compression screws; 42 % of small finger distal phalanges are too small to accommodate 2.8-mm threads, and that number increases to 81 % with 3.2-mm threads and 97 % with 3.5-mm threads. Few distal phalanges, regardless of which finger, are large enough to accommodate 3.5-mm-diameter threads; 22% of female ring finger distal phalanges are smaller than 2.8 mm, and 66 % of ring fingers are smaller than 3.2 mm. Based on our measurements, a surprising number of distal phalanges are smaller than the trailing thread diameter of commonly commercially available headless screws. Care must be taken in selecting implants for distal interphalangeal (DIP) fusion.
Keywords: Distal phalanx, DIP, Arthrodesis, Headless compression screw
Introduction
The distal interphalangeal (DIP) joint can be a source of pain and instability for a variety of reasons. Rheumatoid arthritis, degenerative arthritis, post-traumatic arthritis, and nonunion are common causes. Arthrodesis of the DIP joint is the gold standard of definitive treatment, and a variety of techniques have been described [1–4, 6–10, 12, 14]. Complication rates of DIP joint fusion have been reported from 0–22 % [2, 4, 5, 9].
The use of headless compression screws for DIP joint arthrodesis has increased recently and has the benefits of compression and convenience to patient with no need for hardware removal. It has been noted that some distal phalanges are so small that precision must be used when placing the screw to avoid cutout and nonunion. Tomaino describes an antegrade-retrograde method of fusion with a headless compression screw and mentions that some small fingers may be too small [12]. Wyrsch et al. measured 30 distal phalanges, excluding the small fingers, and found the average height of 3.55 mm to be less than the diameter of the lagging threads of a Herbert screw (3.90 mm). However, they identified no differences based on gender or based on the index, middle, or ring fingers [13]. We believe there are a significant number of distal phalanges that are too small to accept certain screws without potentially cutting through the cortex, fracturing the phalanx, or damaging the overlying nail bed. This is a descriptive anatomic study to characterize the dimensions of the distal phalanx with regard to retrograde placement of a headless compression screw.
Methods
Validation of Digital Measurements
Five frozen cadaver hands were obtained. First, standard posterior-anterior (PA) and lateral radiographs of each hand and of each digit (index, long, ring, and small) were obtained through our medical center’s radiology department. Radiology technicians using roentgenogram machines that are used for regular patient care performed the radiographs. Radiographs of both the hand and individual digits were obtained using our institution’s standard protocols, which control the distance from beam to plate and hand position, thus standardizing magnification issues for both the cadaveric radiographs and for the clinical radiographs utilized in the study. The images were then burned onto a CD and erased from the workstation.
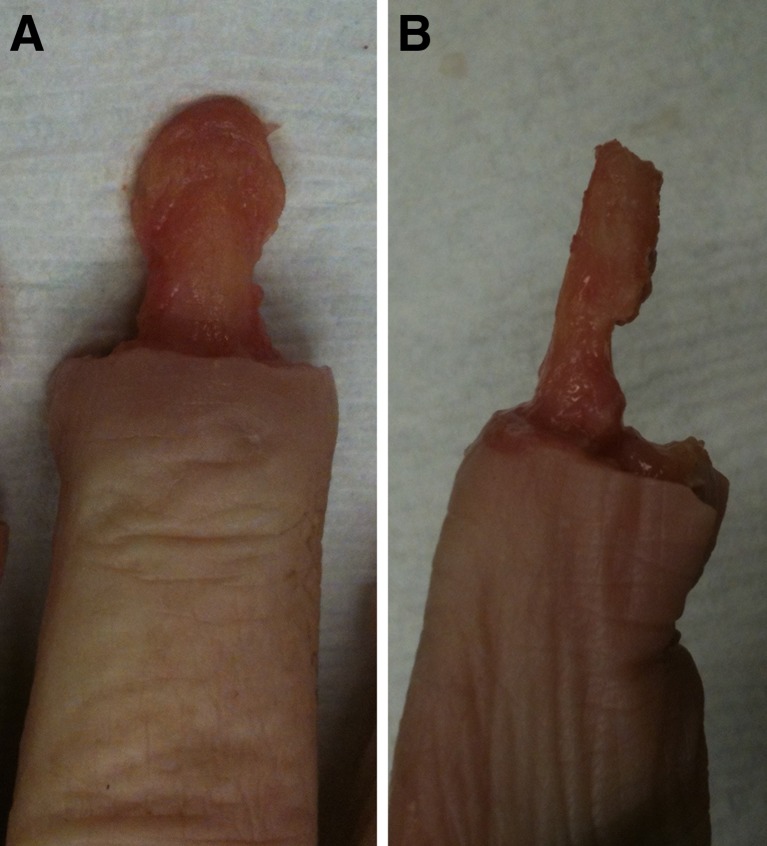
Next, the distal phalanges of the index, long, ring, and small digits were removed of all soft tissue (Fig. 1a, b). The thumb was not included due to the relatively large size of the thumb phalanges, which often require alternative methods of fusion, as a solitary headless compression screw does not achieve acceptable purchase in the capacious thumb phalanges. Using calipers, two separate investigators measured the dorsal-volar (height) and radial-ulnar (width) dimensions of each distal phalanx at the thinnest portion just proximal to the tuft. The measurements were taken on three separate occasions by the two investigators. The intra-observer correlation was excellent by Intraclass Correlation Coefficient (ICC = 0.991), and the inter-observer correlation was found to have excellent agreement (ICC = 0.983).
Fig. 1.
Cadaveric dissection of the distal phalanx. After removing the overlying soft tissues, calipers were used to measure the phalanx in both the dorsal-volar and radial-ulnar dimensions at its narrowest point
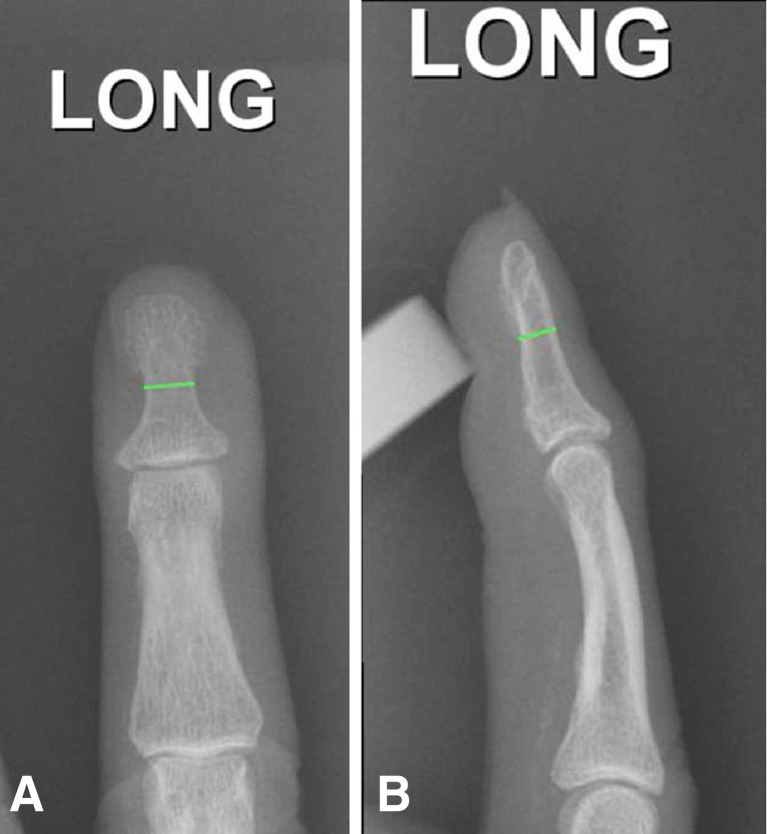
These measurements were compared to the corresponding radiographic values for each distal phalanx as measured using Pixmeo OsiriX v4.1.2 32-bit imaging software (Fig. 2a, b). The radiographic measurements from both the hand as well as the digit radiographs were shown to have excellent agreement with the physical measurements (ICC 0.983). In order to validate the accuracy of the imaging software to be used for the remainder of the study, five deidentified clinical hand radiographs from the General Electric Imagecast PACS, v3.6.101.0, were exported to the OsiriX software. Measurements of the distal phalanges were shown to have excellent agreement between the two imaging software clients (ICC 0.994).
Fig. 2.
Distal phalanx as measured using Pixmeo OsiriX v4.1.2 32-bit imaging software
Obtaining Data
Radiographs of 200 consecutive hands performed at our institution using GE Imagecast PACS were selected and reviewed (Fig. 3a, b). Portable radiographs were excluded, as standard radiographic techniques and beam-plate distances could not be controlled for with these examinations. Inclusion criteria were patient age ≥18, atraumatic distal phalanges, and adequate visualization of each distal phalanx on PA and lateral radiographs. The latest 200 radiographs at the time of the search were chosen. Dorsal-volar and radio-ulnar dimensions of each distal phalanx were measured and recorded at the narrowest portion of the shaft. Descriptive analyses were then performed for gender, age groups, and digit.
Fig. 3.
Radiographic measurements of the distal phalanx using GE Imagecast PACS
Statistical Analysis
The Intraclass Correlation Coefficient (ICC) is a reliability index often used to assess agreement among observers [11]. There are six different versions of the ICC based on the specific variables involved. For our purposes, we used the ICC 3.1 for comparing the measurements made by both observers of all digits and radiographs, in the manner described by Shrout and Fleiss. A value of 0.95 was chosen as “excellent” agreement. Additionally, cutoff dimensions of 3.5, 3.2, and 2.8 mm (the diameter of trailing threads of commonly used headless compression screws) were used to determine the percent of distal phalanges which could not accommodate each screw.
Results
A total of 200 hands were analyzed from 200 individuals from age 18 to 97, mean 47. For descriptive purposes, age groups were chosen as follows: <40 (79 hands), 40–60 (65 hands), 61–75 (41 hands), and >75 (15 hands). There were 117 females and 83 males, 106 right hands and 94 left hands. Table 1 shows the overall mean for each measurement. The largest mean dimension was the width of the long finger distal phalanx at 5.3 mm, and the smallest mean dimension was the height of small finger distal phalanx at 2.9 mm.
Table 1.
Mean dimension by finger
| Finger | Measurement | Dimension (mm) |
|---|---|---|
| Index | Width | 4.8 |
| Height | 3.4 | |
| Long | Width | 5.3 |
| Height | 3.6 | |
| Ring | Width | 4.8 |
| Height | 3.3 | |
| Small | Width | 3.7 |
| Height | 2.9 |
The measurements were then grouped based on gender as seen in Table 2. The female distal phalanges were consistently smaller than their male counterparts. Furthermore, the measurements were grouped according to age groups as seen in Table 3. There was not a large variability among the age groups, but the general trend was that the age group with the smallest dimensions was 40–60 years old, and the age group with the largest was >75 years old.
Table 2.
Mean dimension by finger and gender
| Finger | Measurement | Gender | Dimension (mm) |
|---|---|---|---|
| Index | Width | F | 4.4 |
| M | 5.3 | ||
| Height | F | 3.2 | |
| M | 3.8 | ||
| Long | Width | F | 4.9 |
| M | 5.8 | ||
| Height | F | 3.4 | |
| M | 3.9 | ||
| Ring | Width | F | 4.5 |
| M | 5.3 | ||
| Height | F | 3.1 | |
| M | 3.6 | ||
| Small | Width | F | 3.4 |
| M | 4.1 | ||
| Height | F | 2.7 | |
| M | 3.2 |
Table 3.
Measurement means by finger and age group
| Finger | Measurement | Age group | Mean in mm |
|---|---|---|---|
| Index | Width | <40 | 4.8 |
| 40–60 | 4.7 | ||
| 61–75 | 4.8 | ||
| >75 | 5.1 | ||
| Height | <40 | 3.4 | |
| 40–60 | 3.4 | ||
| 61–75 | 3.4 | ||
| >75 | 3.6 | ||
| Long | Width | <40 | 5.3 |
| 40–60 | 5.2 | ||
| 61–75 | 5.2 | ||
| >75 | 5.4 | ||
| Height | <40 | 3.6 | |
| 40–60 | 3.5 | ||
| 61–75 | 3.6 | ||
| >75 | 3.7 | ||
| Ring | Width | <40 | 4.9 |
| 40–60 | 4.8 | ||
| 61–75 | 4.8 | ||
| >75 | 5.0 | ||
| Height | <40 | 3.4 | |
| 40–60 | 3.3 | ||
| 61–75 | 3.3 | ||
| >75 | 3.5 | ||
| Small | Width | <40 | 3.7 |
| 40–60 | 3.7 | ||
| 61–75 | 3.7 | ||
| >75 | 3.9 | ||
| Height | <40 | 2.9 | |
| 40–60 | 2.8 | ||
| 61–75 | 2.9 | ||
| >75 | 3.1 |
Table 4 shows the percent of distal phalanges that have dimensions below the size of various screw trailing diameters; 42 % of small finger distal phalanges are too small to accommodate 2.8-mm threads, and that number increases to 81 % with 3.2-mm threads and 97 % with 3.5-mm threads. Few distal phalanges, regardless of which finger, are large enough to accommodate 3.5-mm-diameter threads. As demonstrated, the female distal phalanges are consistently and sometimes dramatically smaller than their male counterparts, thus increasing the likelihood of their dimensions falling below the critical threshold.
Table 4.
Percent of digits with dimensions based on commonly used headless compression screws
| Finger | Group | % of fingers <2.8 mm | % of fingers <3.2 mm | % of fingers <3.5 mm |
|---|---|---|---|---|
| Index | Overall | 16 | 48 | 66 |
| Female | 26 | 68 | 83 | |
| Male | 2 | 19 | 40 | |
| Long | Overall | 4 | 24 | 51 |
| Female | 6 | 39 | 72 | |
| Male | 0 | 4 | 22 | |
| Ring | Overall | 14 | 43 | 69 |
| Female | 22 | 66 | 88 | |
| Male | 1 | 11 | 41 | |
| Small | Overall | 42 | 81 | 97 |
| Female | 65 | 95 | 100 | |
| Male | 8 | 62 | 93 |
Discussion
Arthrodesis of the distal interphalangeal joint using a headless compression screw is a very effective treatment for a variety of DIP joint pathologies. A retrograde technique is commonly utilized. However, the size of the distal phalanx must be large enough to accept the chosen implant. Wyrsch et al. found that the average height of distal phalanges was less than the diameter of the lagging threads of a 3.0 Herbert screw. However, their study was limited in that they only measured the index, middle, and ring distal phalanges in ten hands [13]. Our current study measured the index, middle, ring, and small distal phalanges in 200 hands. In addition, since their study was published in 1996, smaller diameter headless compression screws have become commercially available for use.
There are currently over a dozen different variations of headless compression screws. When placed in a standard retrograde fashion across the DIP, the trailing diameter of the screw (the widest portion of the screw) ends up at the narrowest portion of the distal phalanx. The trailing diameter of the smallest option implant for each company is usually around 2.5–3.0 mm (ranging from 2.2 to 3.6 mm). For our study, we chose to evaluate phalanx size based on the diameters of the trailing threads of commonly used commercially available headless compression screws: 2.8 mm (Acutrak 2 Micro 2.5, OrthoHelix MiniMax Torque 2.5), 3.2 mm (Acutrak Mini 2.8, OrthoHelix MiniMax Torque 3.1, Herbert Mini 2.5), and 3.5 mm (Acutrak Fusion 2.8, Synthes HCS 3.0) (Table 5).
Table 5.
Diameter of trailing threads of selected commercially available headless screws
| Manufacturer | Model | Leading thread diameter (mm) | Trailing thread diameter (mm) |
|---|---|---|---|
| Acumed | Acutrak 2 Micro | 2.5 | 2.8 |
| Acutrak 2 Mini | 3.5 | 3.6 | |
| Integra | Kompressor Mini | 2.8 | 3.6 |
| OrthoHelix | Mini MaxTorque | 2.5 | 2.8 |
| 3.1 | 3.2 | ||
| OsteoMed | ExtremiFix | 2.0 | 2.5 |
| 2.4 | 2.9 | ||
| 3.0 | 3.6 | ||
| Trimed | Compression Screw | 1.7 | 2.6 |
| 2.3 | 3.3 | ||
| Stryker | TwinFix | 3.2 | 4.1 |
| Synthes | HCS | 1.5 | 2.2 |
| 2.4 | 3.1 | ||
| 3.0 | 3.5 | ||
| Zimmer | Herbert Mini | 2.5 | 3.2 |
| Herbert Standard | 3.0 | 3.9 |
Based on our measurements, there are a considerable number of distal phalanges that at their smallest dimension are too small to accommodate some of the most commonly used headless compression screws. The surgeon must always know the limitations of the implants available, especially when considering an arthrodesis involving a bone as small as the distal phalanx. Within this cohort, when using implants with 2.8 mm trailing diameters, 65 % of the female small fingers, and as many as a quarter of the female index and ring distal phalanges, are too small to contain the trailing threads within bone. However, no male finger group had more than 8 % too small to accept a 2.8 mm diameter screw.
Age does not seem to be a significant factor when considering size. In fact, the oldest distal phalanges in this study were consistently larger. This may be a result of altered morphology from degenerative arthritis, though not all individuals hypertrophy with osteoarthritis.
Based on the information from this study, we recommend careful planning prior to performing distal interphalangeal joint arthrodesis. Extreme caution should be used when considering DIP joint arthrodesis in females and in the small finger, both in implant choice and technique used. Consideration for alternative fixation techniques may be required, either using an antegrade or oblique screw placement technique or alternative implant selection.
Acknowledgments
This work was supported by an Orthopaedic Research Initiation Grant from the Department of Orthopaedics and Rehabilitation of the Penn State Milton S. Hershey Medical Center.
Conflict of Interest
Rodney Brenneman has no conflicts of interest to disclose.
Justin Bigger has no conflicts of interest to disclose.
Michael Darowish has no conflicts of interest to disclose.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
No informed consent was obtained; 200 consecutive deidentified hand radiographs were used. The study was approved by the institutional IRB.
References
- 1.Arata J, Ishikawa K, Soadea H, Kitayama T. Arthrodesis of the distal interphalangeal joint using a bioabsorbable rod as an intramedullary nail. Scand J Plast Reconstr Surg Hand Surg. 2003;37:228–231. doi: 10.1080/02844310310016403. [DOI] [PubMed] [Google Scholar]
- 2.Brutus JP, Palmer AK, Mosher JF, Harley BJ, Loftus JB. Use of a headless compressive screw for distal interphalangeal joint arthrodesis in digits: clinical outcome and review of complications. J Hand Surg [Am] 2006;31:85–89. doi: 10.1016/j.jhsa.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Cobb T. Arthroscopic distal interphalangeal joint arthrodesis. Tech Hand Upper Extrem Surg. 2008;12:266–269. doi: 10.1097/BTH.0b013e3181902091. [DOI] [PubMed] [Google Scholar]
- 4.Henry M. Variable pitch headless compression screw treatment of distal phalangeal nonunions. Tech Hand Upper Extrem Surg. 2010;14:230–233. doi: 10.1097/BTH.0b013e3181e35361. [DOI] [PubMed] [Google Scholar]
- 5.Kocak E, Carruthers K, Kobus R. Distal interphalangeal joint arthrodesis with the Herbert headless compression screw: outcomes and complications in 64 consecutively treated joints. Hand. 2011;6:56–59. doi: 10.1007/s11552-010-9295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lamas-Gomez C, Proubasta I, Escriba I, Itarte J, Caceres E. Distal interphalangeal joint arthrodesis: treatment with Herbert screw. J South Orthop Assoc. 2003;12:154–159. [PubMed] [Google Scholar]
- 7.Leibovic S. Internal fixation for small joint arthrodesis in the hand. The interphalangeal joints. Hand Clin. 1997;13:601–613. [PubMed] [Google Scholar]
- 8.Leibovic S. Instructional course lecture. Arthrodesis of the interphalangeal joints with headless compression screws. J Hand Surg [Am] 2007;32:1113–1119. doi: 10.1016/j.jhsa.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Olivier L, Gensigk F, Board T, Kendoff, Krehmeier U, Wolfhard U. Arthrodesis of the distal interphalangeal joint: description of a new technique and clinical follow-up at 2 years. Arch Orthop Trauma Surg. 2008;128:307–311. doi: 10.1007/s00402-007-0457-x. [DOI] [PubMed] [Google Scholar]
- 10.Sabbagh W, Grobbelaar A, Clarke C, Smith P, Harrison D. Long-term results of digital arthrodesis with the Harrison-Nicolle peg. J Hand Surg (Br) 2001;26:568–571. doi: 10.1054/jhsb.2001.0649. [DOI] [PubMed] [Google Scholar]
- 11.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psych Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 12.Tomaino MM. Distal interphalangeal joint arthrodesis with screw fixation: why and how. Hand Clin. 2006;22:207–210. doi: 10.1016/j.hcl.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 13.Wyrsch B, Dawson J, Aufranc S, Weikert D, Milek M. Distal interphalangeal joint arthrodesis comparing tension-band wire and Herbert screw: a biomechanical and dimensional analysis. J Hand Surg [Am] 1996;21:438–443. doi: 10.1016/S0363-5023(96)80360-1. [DOI] [PubMed] [Google Scholar]
- 14.Zavitsanos G, Watkins F, Britton E, Somia N, Gupta A, Kleinbert G. Distal interphalangeal joint arthrodesis using intramedullary and interosseus fixation. Hand Surg. 1999;4:51–55. doi: 10.1142/S0218810499000125. [DOI] [PubMed] [Google Scholar]