Abstract
An acquired brain injury (ABI) is an injury to the brain, which is not hereditary, congenital, degenerative, or induced by birth trauma. In India, rapid urbanization, economic growth and changes in lifestyle have led to a tremendous increase in the incidence of ABI, so much so that it is being referred to as a ‘silent epidemic’. Unlike developed countries, there is no well-established system for collecting and managing information on various diseases in India. Thus it is a daunting task to obtain reliable information about acquired brain injury. In the course of conducting a systematic review on the epidemiology of ABI in India, we recognized several challenges which hampered our effort. Inadequate case definition, lack of centralized reporting mechanisms, lack of population based studies, absence of standardized survey protocols and inadequate mortality statistics are some of the major obstacles. Following a standard case definition, linking multiple hospital-based registries, initiating a state or nationwide population-based registry, conducting population-based studies that are methodologically robust and introducing centralized, standard reporting mechanisms for ABI, are some of the strategies that could help facilitate a thorough investigation into the epidemiology and understanding of ABI. This may help improve policies on prevention and management of acquired brain injury in India.
Keywords: Acquired brain injury, challenges, epidemiology, India
What is Acquired Brain Injury?
An acquired brain injury (ABI) is an injury to the brain, which is not hereditary, congenital, degenerative, or induced by birth trauma. It is an injury to the brain that has occurred after birth.[1] The causes of ABI can be broadly categorized into two main types: ‘Traumatic’ and ‘Non-traumatic’ causes. “Traumatic brain injury is damage to the brain resulting from an external mechanical force, such as rapid acceleration, impact, blast waves, or penetration by a projectile”.[2] Non-traumatic brain injury is caused by an illness or disease of the brain (not due to trauma). It results from internal forces such as infections and malignancies.[3] Some of the non-traumatic causes of ABI include cerebro-vascular accident (stroke) which is “A focal (or at times global) neurological impairment of sudden onset, and lasting more than 24 hours (or leading to death), and of presumed vascular origin”[4], tumor, vascular malformations and cerebral infections.[5]
Understanding the Epidemiology of ABI
ABI is an important public health problem with a significant global impact. However, the problem experienced by those affected, such as impairments in cognition and perception, are often not visible. Hence it has been referred to as a ‘silent epidemic’.[6] Among the various causes of ABI, traumatic brain injury and stroke are the leading causes of death and disability worldwide.[7] Traumatic brain injury (TBI) and stroke are the two main causes of ABI that have reached epidemic proportions and are regarded as important public health problems in India. Rapid urbanization, economic growth and life style changes are the reasons for the growing burden of ABI in India.[8] In India, over 100,000 people die due to road traffic accidents each year[9] and nearly 50-60% of them are hospitalized for brain injury.[10] The increasing prevalence of hypertension in the country has resulted in an increase in the number of stroke cases by 17.5% during the past 15 years.[11] Thus, understanding the epidemiology of ABI in India could help plan appropriate interventions and address the burden accordingly.
Our systematic review identified eight studies on stroke[12,13,14,15,16,17,18,19], two studies on traumatic brain injury,[20,21] two studies on brain tumor[22,23] and one study on neurological disorders that included brain infections and stroke.[12] Of the 13 studies, eight studies on stroke were population based, cross-sectional studies. All the remaining studies were hospital based longitudinal registries or cross-sectional studies. None of the identified studies looked at the incidence and prevalence of ABI resulting from all the causes together. Two studies estimated the incidence and prevalence of stroke exclusively.[24,25] One study looked at the prevalence of brain infections and stroke together with other neurological disorders.[12]
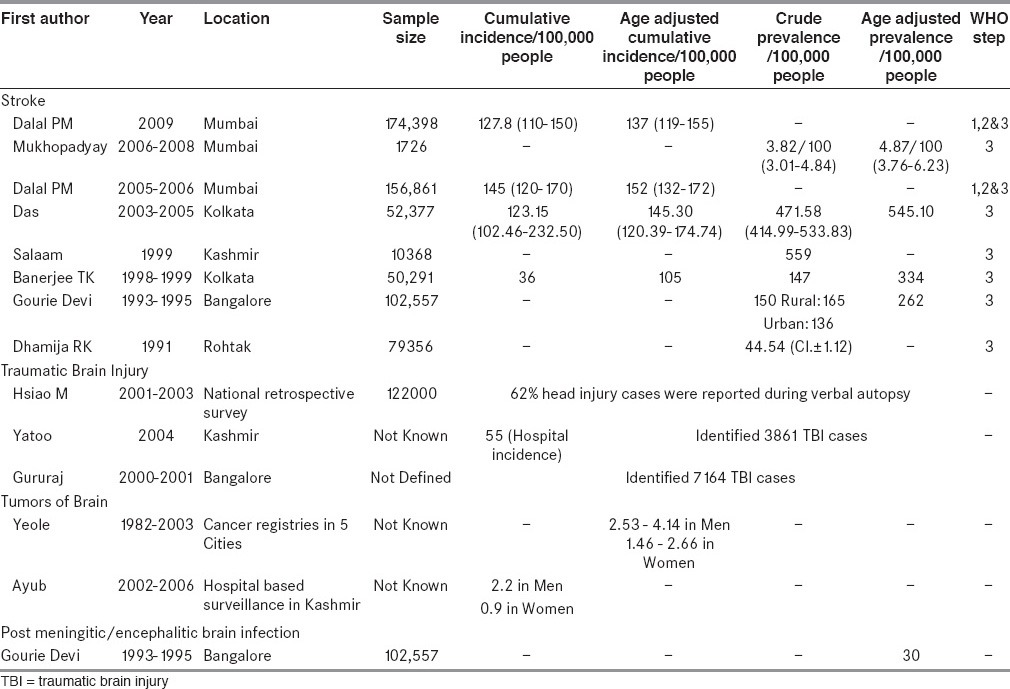
Table 1 depicts the heterogeneity among the studies identified and included for the review[12,24,25,26,27,28,29,30,31,32,33,34]. We did not find any population based study on acquired brain injuries except for stroke. Each study has looked at a specific cause of ABI at various states and cities within India, using different study methods. Given these methodological challenges, it is difficult to combine the estimates from individual epidemiological studies to understand the exact magnitude of ABI in India.
Table 1.
Incidence and prevalence of ABI in India—Details from included studies
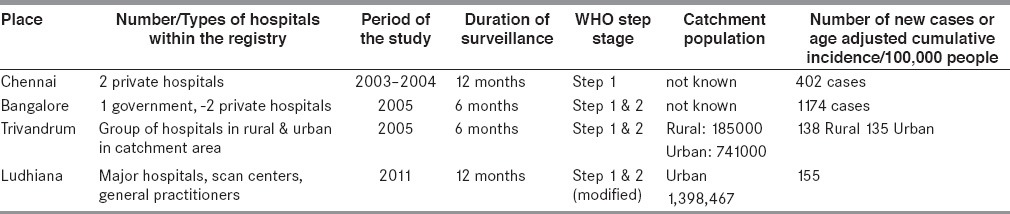
In our systematic review, we identified several hospital based studies [Table 2][14,15,16,35]. Every hospital based study had assumed that the maximum number of ABI cases would report only to the hospitals involved in the study. However, it is difficult to define the catchment population in any of the hospital based studies. People affected by ABI might end up in any hospital outside the geographic location of the study or they might reach the hospitals from an entirely different state or district outside the study location as there is no structured referral pathway in India. Thus, it implies a gross under-estimation of the incident cases and it is highly unlikely that findings from these studies reflect true estimates.
Table 2.
Age-adjusted cumulative stroke incidence and the number of new stroke cases from stroke registries
Challenges in Understanding the Epidemiology of ABI in India
Unlike developed countries, there is no well-established system for collecting and managing information on various diseases in India. Many factors hamper the efforts to precisely quantify the burden of acquired brain injury in India. Let alone the lack of reliable reporting systems, it is difficult to discover reliable statistics even from routinely collected data.[11] Hence we would like to highlight some of the barriers to understanding the epidemiology of ABI in India.
By definition, ABI includes brain injuries of both traumatic and non-traumatic etiology. A wide range of causes contribute to the burden of acquired brain injury. Until now, the burden imposed by various causes had only been studied individually rather than in totality in India. Each study has looked at a specific cause of ABI at various places within India, using different study methods. Case ascertainment strategies and sample size in these studies also differed widely. Only one population based study conducted in Bangalore, looked at stroke and brain infections together with other neurological disorders.[12] However, even this study did not adopt the definition of ABI strictly. The study considered neurodegenerative diseases and did not include traumatic brain injury. Given these methodological challenges, it is difficult to estimate the magnitude of ABI in the community from individual epidemiological studies.
Mortality statistics of India do not have information on the cause of death.[13] Unless someone dies in a hospital that could provide information about the cause of death to these death registries in India, it is not possible to identify the exact cause of death from the mortality registers available in India. For example, TBI contribute to a significant proportion of deaths due to road traffic accidents (RTAs).[36,37] In India, RTA investigation is carried out by the police/crime department and the information about the RTA is maintained by the National Crime Records Bureau (NCRB). But it does not collect information on cause of death. Given the context, under-reporting of RTA deaths by the police department have been reported in many studies.[38,39] The recently published million death study on road injuries and death have highlighted the under-reporting of crude death rates by the NCRB which ranged from < 1% to about 80%.[31]
Majority of the information on epidemiology of ABI is from hospital based studies. It is difficult to define the catchment population in any of the hospital based studies. Details from the hospital based stroke registries have been depicted in Table 2.
There is a lack of population based studies on the incidence and prevalence of ABI in India. There are no cohort studies on any of the causes of ABI.[17] Cohort studies are vital to establish the incidence and impact of ABI in the community. Unfortunately, there has been no effort at the state, or the national level, to initiate such a study. Because of this, epidemiological parameters are often estimated from cross-sectional studies and these estimates may not be reflecting the true magnitude of the problem.
-
Lack of standardized survey protocols for assessing the incidence and prevalence of ABI in totality or from individual causes is also a challenge. Although the WHO STEP wise approach to surveillance for stroke is widely used in many countries including India[18], the feasibility of using such a tool in the Indian context and the necessary revisions, to enhance feasibility of such protocols in the Indian context have not been optimally explored. Information from Table 2 highlights the variation in sample size, WHO surveillance STEPs, and whether catchment population was defined in each study. For example, studies have followed different WHO STEPs to their stroke surveillance which makes it difficult to arrive at the precise estimate of the incidence or prevalence from these studies. The estimates may vary among these studies because each study had followed only selective steps of the WHO STEPs surveillance procedures.
Each of the population based studies [Table 1] had very different sample sizes. In some studies the catchment population was not defined. Hence, arriving at an estimate for incidence or prevalence was not possible in these studies.
A limitation of the million death study is the use of lay person narratives to conduct the survey which may have led to inaccurate reporting.[31] Similarly in some of the stroke studies, only first ever strokes were considered as a case. In some studies people with stroke who have died during the study have not been included as a case. This makes estimation of incidence and prevalence of ABI very difficult.
Ascertainment of cases for ABI studies in India doesn’t ensure confirmatory radio-diagnosis. Case ascertainment strategies in most of the cross-sectional studies aimed at assessing the prevalence of ABI in India are based on questionnaire surveys and neurological examination.[19] Confirmatory diagnosis through computerized tomography (CT) and magnetic resonance imaging (MRI) were not used as the basis for case ascertainment in many studies. Hence objectivity of the case ascertainment strategies used in epidemiological surveys of ABI in India is questionable.
Information from population-based registries is limited to very few hospitals in India. Some of the hospital-based registries in India propose themselves to be population based registers for certain causes of ABI. For example, the stroke registry and the cancer registry.[20] However, these are sustained by voluntary contributions from a few hospitals from a defined catchment area. There are no regulations by concerned authorities to ensure compulsory documentation and reporting of epidemiological data on ABI to these registries.
There is a lack of data sharing and linkage between the existing registries to consolidate the available information and to regularly update it at a state, regional or country level. This reduces the actual utility of such registries since a single hospital cannot catch a significant proportion of the population within a target area. Unlike developed countries, we do not have linkages between various government departments gathering information about ABI in India. For example. Information about RTAs from NCRB is not linked to the hospitals collecting longitudinal data on TBI in India in hospitals such as NIMHANS.[19] Registries themselves are independently managed at present. There is no linkage between the registry for stroke, TBI and brain tumors in the country.
There is a lack of centralized reporting mechanism, to allow streamlined documentation and utilization of epidemiological data on ABI in India. Such mechanisms could potentially enhance consolidation of epidemiological information on ABI from various hospital or population based registries located in different districts or states. It could also help integrate the information from various registries for stroke, brain tumor, TBI and cerebral infections such as encephalitis (especially Japanese encephalitis), meningitis and cerebral malaria. This creates an urgent need for policies and regulation for a centralized information management organization or system in the country that could aid robust epidemiological investigations on ABI.
The Documentation of disease related information in most of the hospitals in India is not performed by utilizing a generic method. International classification of diseases (ICD) is a commonly used method in many hospitals for documentation worldwide. However, many hospitals in India do not practice documentation based on ICD. Even in those few hospitals that practice ICD based documentation, there exist significant discrepancies in coding between individuals and hospitals.[21] Practice of a generic system of paper or computer based documentation of ABI could be made compulsory in government and private hospitals. Health professionals can be trained to start documenting disease related information in a standardized format right from their academic sessions and practice placements.
Lack of electronic documentation and dependence on printed records makes the task of documentation and consolidation of existing data on ABI from various hospitals and registries cumbersome. Paper based records are also prone to duplication and human errors, which can be significantly reduced by electronic documentation. In addition, paper based documentation does not allow quick retrieval and analysis of data.[22] There is a strong potential for this to happen if the existing framework for electronic documentation from national aids control program and revirecd national tuberculosis control program is utilized to develop a similar system for ABI too.
How do we Proceed Further?
ABI is a heterogeneous health condition encompassing multiple etiologies leading on to some common effects of diverse severities. Understanding the epidemiology of ABI will help evaluate the impact of such a neurologic injury in the community. Translating this understanding into public health practice will not only help in prevention of ABIs but will also help policymakers plan programs and pathways for managing the disability experienced by those affected. As discussed above, there are multiple challenges that hinder our approach to understanding epidemiology of ABI. Inadequate case definition and case ascertainment, lack of centralized reporting mechanisms and the lack of population based studies are some of the major obstacles.
The authors urge for a radical change in the way epidemiological data on ABI is collected, managed and utilized. Following a standard case definition, using the existing mechanisms such as telemedicine to screen for cases in rural areas and not just limiting studies to cities and urban areas, linking multiple hospital-based registries, initiating a state or nationwide population-based registry, conducting population-based studies that are methodologically robust and introducing centralized and standard reporting mechanisms for ABI could be some of the strategies that will facilitate a thorough investigation into the epidemiology and understanding of ABI, which in turn will help improve policies on management of acquired neurologic diseases. It may also help in facilitating mechanisms to understand and address other health conditions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Brain injury association of America (BIAUSA). What is the difference between acquired brain injury and traumatic brain injury? [Last accessed on 2012 Apr 30]. Available from: http://www.biausa.org/FAQRetrieve.aspx?ID=43913 .
- 2.Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–41. doi: 10.1016/S1474-4422(08)70164-9. [DOI] [PubMed] [Google Scholar]
- 3.Headway. Types of acquired brain injury. [Lsat accessed on 2012 Apr 30]. Available from: http://www.headway.ie .
- 4.Toronto Acquired Brain Injury Network (TABIN). Definition of acquired brain injury. [Last accessed on 2012 Apr 30]. Available from: http://www.abinetwork.ca/definition.htm .
- 5.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: A brief overview. J Head Trauma Rehabil. 2006;21:375–8. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Mar J, Arrospide A, Begiristain JM, Larranaga I, Elosegui E, Oliva-Moreno J. The impact of acquired brain damage in terms of epidemiology, economics and loss in quality of life. BMC Neurol. 2011;11:46. doi: 10.1186/1471-2377-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prabhakaran VR. Non-communicable diseases in India: Transitions, burden of disease and risk factors - A short story. India health beat. 2012 Jun;6(No: 1) [Google Scholar]
- 8.Gururaj R. Road traffic deaths, injuries and disabilities in India: Current scenario. Natl Med J India. 2008;21:14–20. [PubMed] [Google Scholar]
- 9.Dandona R, Kumar GA, Ameer MA, Ahmed GM, Dandona L. Incidence and burden of road traffic injuries in urban India. Inj Prev. 2008;14:354–9. doi: 10.1136/ip.2008.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.New Delhi: Ministry of Health and Family Welfare, Government of India; 2005. Burden of disease in India, Background papers for the National Commission on Macroeconomics. [Google Scholar]
- 11.Jennett B. Epidemiology of head injury. J Neurol Neurosurg Psychiatry. 1996;60:362–9. doi: 10.1136/jnnp.60.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gourie-Devi M, Gururaj G, Satishchandra P, Subbakrishna DK. Prevalence of neurological disorders in Bangalore, India: A community-based study with a comparison between urban and rural areas. Neuroepidemiology. 2004;23:261–8. doi: 10.1159/000080090. [DOI] [PubMed] [Google Scholar]
- 13.Kotabgi RB, Chaturvedi RK, Banerjee A. Medical Certification of Cause of Death. [Last accessed on 2014 May 21];Med J Armed Forces India. 2004 60:261–72. doi: 10.1016/S0377-1237(04)80060-1. Available from: http://medind.nic.in/maa/t04/i3/maat04i3p261.pdf . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arjundas D, Pandiyan U, Arjundas G, Baux H. Surveillance of stroke: WHO Stepwise approach: A Chennai stroke Unit report. Ann Indian Acad Neurol. 2007;10:154–9. [Google Scholar]
- 15.Nagaraja D, Gururaj G, Girish N, Panda S, Roy AK, Sarma GR, et al. Feasibility study of stroke surveillance: Data from Bangalore, India. Indian J Med Res. 2009;130:396–403. [PubMed] [Google Scholar]
- 16.Verma SJ, Singh G, Singla M, Gill JS, Brar RS, Gill AS, et al. Brazil: Presented at the world stroke congress; 2012. Feasibility of population based stroke registry in Ludhiana City, India. [Google Scholar]
- 17.Taylor FC, Sureshkumar K. Stroke fact sheet India. [Last accessed on 2014 May 22]. Available from: http://www.sancd.org/Updated%20Stroke%20Fact%20sheet%202012.pdf .
- 18.Das SK. WHO Steps stroke surveillance system: Feasibility in India. Indian J Med Res. 2009;130:359–60. [PubMed] [Google Scholar]
- 19.Gururaj G, Kolluri SV, Chandramouli BA, Subbakrishna DK, Kraus JF. Bangalore: National Institute of Mental Health and Neurosciences; 2005. [Last accessed on 2014 May 19]. Traumatic brain injury. Available from: www.nimhans.kar.nic.in/epidemiology/doc/ep_ft25.pdf . [Google Scholar]
- 20.Indian Council of Medical Research. About National Cancer Registry Program. [Last accessed on 2014 May 21]. Available from: http://www.ncrpindia.org/About_NCRP.aspx .
- 21.New Delhi: Nirman Bhavan; 2006. Mortality Statistics in India. Status of mortality reporting in India. Central Bureau of Health Intelligence (CBHI). Directorate General of Health Services. Ministry of Health and Family Welfare. [Google Scholar]
- 22.Thomas J. Medical records and issues in negligence. Indian J Urol. 2009;25:384–8. doi: 10.4103/0970-1591.56208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yeole BB. Trends in the brain cancer incidence in India. Asian Pac J Cancer Prev. 2008;9:267–70. [PubMed] [Google Scholar]
- 24.Banerjee TK, Mukherjee CS, Sarkhel A. Stroke in the urban population of Calcutta: An epidemiological study. Neuroepidemiology. 2001;20:201–7. doi: 10.1159/000054788. [DOI] [PubMed] [Google Scholar]
- 25.Das SK, Banerjee TK, Biswas A, Roy T, Raut DK, Mukherjee CS, et al. A prospective community-based study of stroke in Kolkata, India. Stroke. 2007;38:906–10. doi: 10.1161/01.STR.0000258111.00319.58. [DOI] [PubMed] [Google Scholar]
- 26.Dalal PM, Bhattacharjee MA, Vairale JY. WHO-global stroke initiative-Mumbai stroke registry: A report on incidence of first-ever-stroke during re-survey 2009. Int J Stroke. 2012;7:E3. doi: 10.1111/j.1747-4949.2012.00873.x. [DOI] [PubMed] [Google Scholar]
- 27.Mukhopadhyay A, Sundar U, Adwani S, Pandit D. Prevalence of stroke and post-stroke cognitive, impairment in the elderly in Dharavi, Mumbai. J Assoc Physicians India. 2012;60:29–32. [PubMed] [Google Scholar]
- 28.Dalal P, Bhattacharjee M, Vairale J, Bhat P. International Stroke Society-WHO Global Stroke initiative: A report on population based Mumbai Stroke registry (2005-2006), India. Int J Stroke. 2009;4:239–40. doi: 10.1111/j.1747-4949.2009.00313.x. [DOI] [PubMed] [Google Scholar]
- 29.Salaam A. Epidemiology of neurological disorders in Kashmir. J Health Adm. 2002;13-14:15–24. [Google Scholar]
- 30.Dhamija RK, Mittal S, Bansal BC. Trends in clinico-epidemiological correlates of stroke in the community. J Indian Acad Clin Med. 2000;5:27–31. [Google Scholar]
- 31.Hsiao M, Malhotra A, Thakur JS, Sheth JK, Nathens AB, Dhingra N, et al. Million Death Study Collaborators. Road traffic injury mortality and its mechanisms in India: Nationally representative mortality survey of 1.1 million homes. BMJ Open. 2013;3:e002621. doi: 10.1136/bmjopen-2013-002621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yattoo G, Tabish A. The profile of head injuries and traumatic brain injury deaths in Kashmir. J Trauma Manag Outcomes. 2008;2:5. doi: 10.1186/1752-2897-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gururaj G. Background Papers: Burden of Disease. New Delhi: The National Commission on Macroeconomics and Health, Ministry of Health and Family Welfare; Injuries in India: A national perspective; pp. 325–47. [Google Scholar]
- 34.Ayub SG, Ayub T, Khan SN, Rasool S, Mahboob-ul-Hussain, Wani KA, et al. Epidemiological distribution and incidence of different cancers in Kashmir Valley- 2002–2006. Asian Pac J Cancer Prev. 2011;12:1867–72. [PubMed] [Google Scholar]
- 35.Sridharan SE, Unnikrishnan JP, Sukumaran S, Sylaja PN, Nayak SD, Sarma PS, et al. Incidence, types, risk factors and outcome of stroke in a developing country: The Trivandrum Stroke Registry. Stroke. 2009;40:1212–8. doi: 10.1161/STROKEAHA.108.531293. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization; 2008. World Health Organization. The global burden of disease: 2004 Update. [Google Scholar]
- 37.Mathers CD, Bernard C, Moesgaard Iburg K, Inoue M, Fat DM, Shibuya K, et al. World Health Organization; 2003. Global burden of disease in 2002: Data sources, methods, and results. Global Programme on Evidence for Health Policy Discussion Paper No. 54. [Google Scholar]
- 38.Dandona R, Kumar GA, Ameer MA, Reddy GB, Dandona L. Under-reporting of road traffic injuries to the police: Results from two data sources in urban India. Inj Prev. 2008;14:360–5. doi: 10.1136/ip.2008.019638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Naci H, Chisholm D, Baker TD. Distribution of road traffic deaths by road user group: A global comparison. Inj Prev. 2009;15:55–9. doi: 10.1136/ip.2008.018721. [DOI] [PubMed] [Google Scholar]


