Abstract
A twenty-one-year old primigravida presented two weeks postpartum with new onset of behavioral alteration and irrelevant talking without fever, headache, or seizures. Magnetic resonance imaging (MRI) of brain showed a lesion with diffusion restriction in splenium of corpus callosum. A possibility of postpartum psychosis was considered after ruling out various etiologies for splenium hyperintense lesion. Near complete resolution of symptoms was noted after initiation of antipsychotic medications. Literature has described multiple etiologies for lesions involving splenium of corpus callosum on brain imaging. We present this case as a unique clinical presentation of splenial pathology in the form of postpartum psychosis.
Keywords: MRI, postpartum psychosis, reversible splenium lesion, splenium hyperintensity
Introduction
Corpus callosum is a midline structure of the cerebrum and is composed of connecting white matter fibers. Isolated involvement of corpus callosum on magnetic resonance imaging (MRI) is well known, but it is a non-specific observation. Corpus callosum involvement has been described in a variety of disorders that involve demyelination, infection, inflammation, trauma, and metabolic, vascular, and malignant pathologies. A relatively new entity known as Mild Encephalopathy with Reversible Splenial lesions (MERS) has been described, which includes cases with mild encephalitis-like presentation and clearing of corpus callosum lesions on follow-up imaging study.[1] To the best of our knowledge, association of radiological splenial involvement presenting as postpartum psychosis has not been described earlier.
Case Report
A twenty-one–year-old primigravida with an uneventful antenatal period presented two weeks postpartum with new onset of behavioral abnormalities and irrelevant talking since prior five to seven days. She underwent hospital-based normal delivery at full term. She was noticed by her family to behave abnormally in the form of crying spells, anger outbursts, irrelevant talking, ideas of persecution, wandering behavior, and disturbed sleep. She was observed being detached and disinterested in the baby, and having unexplained fear. She did not have fever, headache, vomiting, seizures, or trauma. In her past, she never had similar episodes and her family denied any depressive features or use of any long-term medications prior to onset of the symptoms. She was admitted at a local hospital where she progressively lapsed in to a state of near akinetic mutism.
On examination, her vital parameters were normal. She looked apathetic with no spontaneous limb movements or vocalization. She seemed to be muttering to herself with occasional crying spells and did not obey any commands. In view of negativism, orientation to time, place, or person could not be assessed. Tone in extremities and deep tendon reflexes were normal. There were no signs of waxy flexibility or meningeal irritation. Remaining neurological and systemic examination, including fundus, was unremarkable.
Magnetic resonance imaging (MRI) of brain at admission showed isolated diffusion restriction and low apparent diffusion coefficient (ADC) values in splenium of corpus callosum, extending into the body of corpus callosum. There was mild edema in T2 and Fluid Attenuated Inversion Recovery (FLAIR) sequences. The lesion did not enhance after gadolinium administration [Figure 1]. Specifically, no lesions were observed in other cortical or subcortical white matter and posterior circulation territory. Cerebral angiogram and venogram were normal. Her hemogram, metabolic panel, erythrocyte sedimentation rate, thyroid profile, autoimmune panel, urine routine, and chest x-ray were normal. Serum vitamin B12 level was 218 pg/ml. Blood and urine cultures did not grow any organisms. She tested negative for Salmonella, Tuberculosis, Dengue, HIV, and respiratory infections. Her history, clinical examination, and investigations did not show any evidence of infective or metabolic diseases. Electroencephalography was negative for any epileptiform discharges or slowing of background activity. Cerebrospinal fluid (CSF) analysis showed normal proteins, sugar, and cell count. CSF Polymerase Chain Reaction (PCR) for tuberculosis and herpes were negative. Visual evoked potential (VEP) and Brainstem Auditory Evoked Potential (BAER) were within normal limits.
Figure 1.
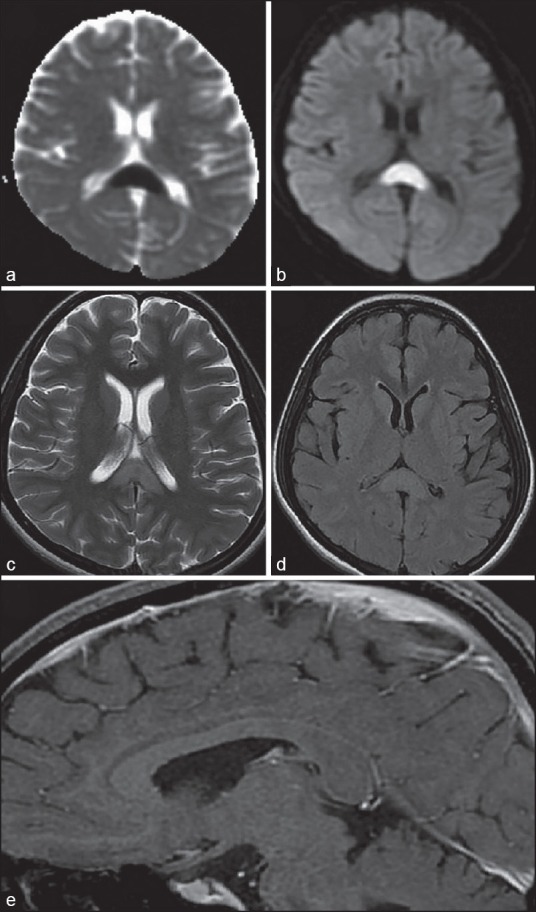
MRI of Brain showing low ADC value (a) and diffusion restriction (b) in splenium of corpus callosum with hyperintensity on axial T2 (c) and FLAIR (d) sequences. No enhancement noted in post gadolinium T1 sagittal image (e)
She was initially managed empirically with Ceftraixone and Acyclovir. With normal CSF picture, these medications were stopped and psychiatry consultation was sought. She was diagnosed to have postpartum psychosis and was started on Lorazepam, Escitalopram, and Olanzepine, along with behavioral counseling. Following these medications, progressive improvement was noted in her clinical status. Her symptoms of crying spells, persecution, and wandering recovered. She became oriented with normal vocalization and sleep. She was discharged after ten days of hospital stay and is awaited for follow up.
Discussion
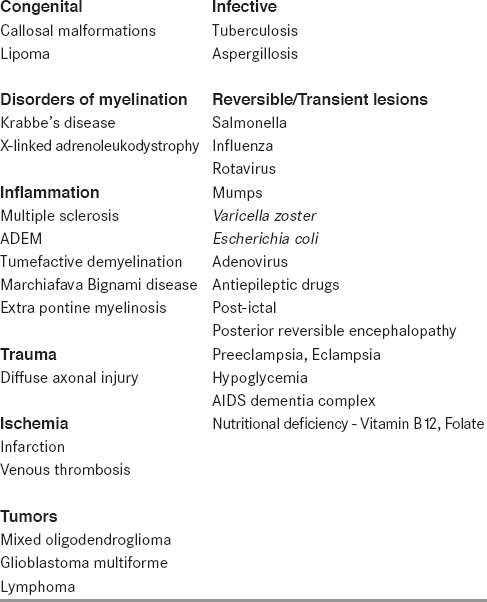
Corpus callosum is the largest commissure consisting of white matter tracts connecting the two cerebral hemispheres. It comprises rostrum, genu, body, and splenium. It has a rich vascular supply. Lesions of corpus callosum present clinically as disconnection syndromes. Solitary involvement of corpus callosum on MRI has been a well described entity and is associated with variety of diseases [Table 1].[2] Isolated involvement of corpus callosum does not have a specific radiological diagnosis. Lesion of splenium area of corpus callosum, resulting in diffusion restriction, has been described as “Boomerang sign”.[3]
Table 1.
Differential diagnosis of Corpus Callosum lesions on MRI
Acute disseminated encephalomyelitis (ADEM) should be considered as a differential diagnosis in lesions of corpus callosum. ADEM lesions, however, are multiple and with variable contrast enhancement. In addition, CSF analysis in ADEM shows pleocytosis. The lesions in MRI were not typical of multiple sclerosis (MS) or tumefactive demyelination (TD). MS and TD can be isolated but have characteristic contrast enhancement with abnormal CSF.
Corpus callosum has a rich blood supply from anterior and posterior vascular territories. Infarction of corpus callosum is generally secondary to large vessel ischemia. Focal infarction of a part of corpus callosum is uncommon since the blood supply is through small perforating vessels running perpendicular to the parent vessel. It is difficult for the emboli to enter these branches and lead to infarction. Hence, corpus callosum infarcts are associated with involvement of other areas in corresponding vascular territory.[2] However, ischemia due to hypoxia, especially in neonates, produces typical corpus callosum lesions. Cerebral venous sinus thrombosis, involving the deep venous system, leads to vasogenic edema and infarction of corpus callosum.
Tumors involving corpus callosum show a heterogeneous morphology and variable edema, contrast enhancement with or without multiple lesions affecting other areas of brain. Nutritional deficiencies, especially vitamin B12, folic acid, and thiamine, have been shown to cause splenial involvement.[4] These lesions are transient and are reversible with nutritional supplementation.
Infections such as tuberculosis and aspergillosis have propensity to involve the corpus callosum. Tuberculosis is an important differential diagnosis, especially in endemic countries such as India. Tuberculoma shows central necrosis with peripheral contrast enhancement. It may mimic glioma; spectroscopy helps to differentiate between the two conditions.
Transient lesions involving corpus callosum have been covered under the umbrella of MERS (Mild Encephalitis with Reversible Splenial lesion). Many cases with transient splenium lesions have been described with a variety of pathology, which include infections, post-seizure, drugs, and metabolic/nutritional and preeclampsia/eclampsia [Table 1]. The time interval for repeat neuroimaging is variable among the reports, but the reversibility interval ranges from few days to months. Antiviral or steroid medications are ineffective in these lesions and are managed with supportive medications. Tada et al. described case series of fifteen patients having similar presentation and radiological features, all of which resolved within one month duration.[1]
Post-seizure splenium hyper intense lesions on MRI are well recognized.[5] The mechanisms proposed are vasogenic or cytotoxic edema. Corpus callosum is usually not an origin focus but rather a pathway for seizure propagation for generalization. Moreover, rapid alterations in dose of antiepileptic medications have also been shown to lead to splenium lesion, probably through disturbance in the arginine–vasopressin homeostasis.[6]
In peri-partum cases, important etiologies for splenial involvement to be considered are cerebral venous sinus thrombosis, post-seizure, and preeclampsia-eclampsia. Preeclampsia and other conditions associated with uncontrolled hypertension commonly affect the posterior white matter. There are descriptions of a more subtle presentation of late postpartum preeclampsia, made unusual due to a lack of classic signs such as edema, proteinuria, and hypertension.[7] A case report by Curtis et al. described a benign postpartum splenial lesion presenting as visual symptoms that underwent expectant management and resolution by six weeks.[8] Probable etiology for the lesion was considered to be post-partum subclinical preeclampsia.
Despite the large number of possible etiologies, the exact pathogenesis of the reversible splenial lesions is not well understood. With reversibility of the lesions and the absence of any other lesions in vascular distributions, it is unlikely that the splenial abnormalities are the result of ischemia. Other etiological hypotheses are presence of elevated level of interleukin-6 and cross-reaction to viral antigens. Vasogenic or cytogenic edema has been proposed as possible reasons for infective, post-infectious, and post-seizure involvement. Disturbance in arginine–vasopressin system is probably responsible for lesions following antiepileptic medication withdrawal.
The relationship between corpus callosum and behavior is well known. Occurrence of neuropsychological disorders likely secondary to lesions of corpus callosum have been described in literature.[9] Isolated cases presenting with neuropsychiatric manifestations following corpus callosum lesions have been reported by Durst and Rosca-Rebaudengo,[10] Tanaghow et al.,[11] Fersten et al.,[12] and Pavesi et al.[13] It has been proposed that corpus callosum pathologies increase the risk for psychiatric symptoms by interfering with corticocortical interhemispheric activity.[13]
In our case, most of the etiologies described above were ruled out through clinical history, examination, and investigations. There was no evidence of infective or metabolic pathology. Clinically, she was diagnosed with postpartum psychosis. Antipsychotic medications resulted in remarkable improvement of symptoms and near complete recovery. The role of subclinical preeclampsia, nutritional deficiency, or unidentified viral infection could not be ruled out with certainty in this case. However, clinical diagnosis of psychosis and response to antipsychotic medications makes this case a unique clinical presentation of a radiological splenial lesion. However, whether the clinical picture is a consequence to the MRI lesion is not certain since we do not have follow-up imaging.
In conclusion, splenial involvement in MRI is a well-described finding but is non-specific and associated with numerous conditions. We came across a unique association of postpartum psychosis with splenium lesion not described previously in literature. This case exemplifies variability in clinical presentation of splenium involvement and denotes the importance of diagnostic consideration of psychiatric disease with an abnormal brain imaging study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Tada H, Takanashi J, Barkovich AJ, Oba H, Maeda M, Tsukahara H, et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology. 2004;63:1854–8. doi: 10.1212/01.wnl.0000144274.12174.cb. [DOI] [PubMed] [Google Scholar]
- 2.Kazi AZ, Joshi PC, Kelkar AB, Mahajan MS, Ghawate AS. MRI evaluation of pathologies affecting the corpus callosum: A pictorial essay. Indian J Radiol Imaging. 2013;23:321–32. doi: 10.4103/0971-3026.125604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malhotra HS, Garg RK, Vidhate MR, Sharma PK. Boomerang sign: Clinical significance of transient lesion in splenium of corpus callosum. Ann Indian Acad Neurol. 2012;15:151–7. doi: 10.4103/0972-2327.95005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kosugi T, Isoda H, Imai M, Sakahara H. Reversible focal splenial lesion of the corpus callosum on MR images in a patient with malnutrition. Magn Reson Med Sci. 2004;3:211–4. doi: 10.2463/mrms.3.211. [DOI] [PubMed] [Google Scholar]
- 5.Polster T, Hoppe M, Ebner A. Transient lesion in the splenium of the corpus callosum: Three further cases in epileptic patients and a pathophysiological hypothesis. J Neurol Neurosurg Psychiatry. 2001;70:459–63. doi: 10.1136/jnnp.70.4.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim SS, Chang KH, Kim ST, Suh DC, Cheon JE, Jeong SW, et al. Focal lesion in the splenium of the corpus callosum in epileptic patients: Antiepileptic drug toxicity? AJNR Am J Neuroradiol. 1999;20:125–9. [PubMed] [Google Scholar]
- 7.Dziewas R, Stögbauer F, Freund M, Lüdemann P, Imai T, Holzapfel C, et al. Late onset postpartum eclampsia: A rare and difficult diagnosis. J Neurol. 2002;249:1287–91. doi: 10.1007/s00415-002-0840-z. [DOI] [PubMed] [Google Scholar]
- 8.Curtis R, Winder T, Scott J, Hill MD. Benign post-partum reversible restricted diffusion lesion of the splenium. Can J Neurol Sci. 2013;40:89–90. doi: 10.1017/s0317167100013019. [DOI] [PubMed] [Google Scholar]
- 9.Devinsky O, Laff R. Callosal lesions and behavior: History and modern concepts. Epilepsy Behav. 2003;4:607–17. doi: 10.1016/j.yebeh.2003.08.029. [DOI] [PubMed] [Google Scholar]
- 10.Durst R, Rosca-Rebaudengo P. Koro secondary to a tumour of the corpus callosum. Br J Psychiatry. 1988;153:251–4. doi: 10.1192/bjp.153.2.251. [DOI] [PubMed] [Google Scholar]
- 11.Tanaghow A, Lewis J, Jones GH. Anterior tumour of the corpus callosum with atypical depression. Br J Psychiatry. 1989;155:854–6. doi: 10.1192/bjp.155.6.854. [DOI] [PubMed] [Google Scholar]
- 12.Fersten E, Łuczywek E, Głowacki M, Czernicki Z. Paranoid syndrome in a patient with tumor in anterior part of corpus callosum. Case report. Neurol Neurochir Pol. 2001;35:741–7. [PubMed] [Google Scholar]
- 13.Pavesi G, Causin F, Feletti A. Cavernous angioma of the corpus callosum presenting with acute psychosis. Behav Neurol 2014. 2014 doi: 10.1155/2014/243286. 243286. [DOI] [PMC free article] [PubMed] [Google Scholar]


