Abstract
INTRODUCTION
The aim of the present study was to investigate the challenges faced by physicians during shift handovers in a university hospital that has a high handover sender/recipient ratio.
METHODS
We adopted a multifaceted approach, comprising recording and analysis of handover information, rating of handover quality, and shadowing of handover recipients. Data was collected at the general medical ward of a university hospital in Singapore for a period of three months. Handover information transfer (i.e. senders’ and recipients’ verbal communication, and recipients’ handwritten notes) and handover environmental factors were analysed. The relationship between ‘to-do’ tasks and information transfer, handover quality and handover duration was examined using analysis of variance.
RESULTS
Verbal handovers for 152 patients were observed. Handwritten notes on 102 (67.1%) patients and handover quality ratings for 98 (64.5%) patients were collected. Although there was good task prioritisation (information transfer: p < 0.005, handover duration: p < 0.01), incomplete information transfer and poor implementation of non-modifiable identifiers were observed. The high sender/recipient ratio of the hospital made face-to-face and/or bedside handover difficult to implement. Although the current handover method (i.e. use of telephone communication) allowed for interactive communication, it resulted in systemic information loss due to the lack of written information. The handover environment was chaotic in the high sender/recipient ratio setting, and the physicians had no designated handover time or location.
CONCLUSION
Handovers in high sender/recipient ratio settings are challenging. Efforts should be made to improve the handover processes in such situations, so that patient care is not compromised.
Keywords: communication breakdown, handoff, handover, sender/recipient ratio
INTRODUCTION
Hospitals today provide healthcare services 24 hours a day. In order to achieve seamless continuity of patient care, primary medical teams routinely transfer patients to on-call teams. This transfer process is referred to as a ‘handover’; its primary objective is to ensure that the information about a patient’s state and plan of care is accurately transferred.(1) Despite their pivotal role in ensuring patient safety, handovers have been identified as one of the most poorly regulated practices in hospitals. Breakdown in handover communication contributes to increased clinical errors, delayed treatment, longer patient stays and wasted clinical resources.(2,3)
The majority of research on patient handover has investigated the handover practices in Europe, the United States and Australia. There is little research on the handover practices in Asia. In fact, none of the studies reported in two recently published literature review articles was conducted in Asia.(4,5) One exception is a study that examined resident physicians’ handover practices in a public hospital in Singapore;(6) the authors showed that the handover sender/recipient ratio in Singapore was a few times higher than that reported in other countries or settings (20 vs. 3–4 handover senders to one handover recipient).(7,8)
The sender/recipient ratio is a decisive factor in handover practices, as it directly influences the resources available for each handover. A high sender/recipient ratio and the resulting large number of patients handled by each recipient impose more constraints on the amount of time and effort that can be invested in each patient,(9) leading to some distinctive practices. For example, in a high sender/recipient ratio setting, it would be difficult to coordinate shift handovers among medical teams and to conduct face-to-face or bedside handovers, which are recommended as the proper methods.(10)
Despite the large variability in sender/recipient ratios, there is limited understanding on how handover occurs in high sender/recipient ratio settings and how its accompanying complexities are managed. Therefore, the present study aimed to investigate the strengths and pitfalls of shift handover practices in a university hospital with a high sender/recipient ratio. This was done in an attempt to highlight the challenges of implementing handover recommendations in high sender/recipient ratio settings.
METHODS
The present study was undertaken at the general medical ward of a 943-bed university hospital with Joint Commission International accreditation in Singapore. We adopted a multifaceted approach, which included: (a) recording and analysis of handover conversations and handover notes; (b) evaluation of the quality of the handover; and (c) shadowing of handover recipients.
At the time of the study, the Department of Medicine ran a shift system with a total of three handovers daily (day-evening, evening-night and night-day handovers). Starting from 1730 hours, approximately 20 primary medical teams transferred inpatients to one evening on-call team. The evening on-call team finished their shift at 2230 hours and handed the inpatients over to two night on-call teams. The night on-call teams completed the shift by transferring the inpatients back to the primary teams at 0800 hours the next morning.
Each primary medical team and on-call team consisted of one consultant, one registrar, one medical officer (MO) and one or two house officers (HOs). The majority of the handovers between the two shifts were performed between two MOs and occasionally, between a registrar and an MO. The common handover method adopted by the MOs/registrars was telephone communication. The handover sender would call the handover recipient prior to the change of shift, and the handover recipient would usually write down critical patient information on a blank piece of paper and carry it around during the shift. The day-evening handover was identified by the department as the most problematic, due to the high sender/recipient ratio. Therefore, the present study focused on only the day-evening handover.
Data collection was conducted from 1730 hours to 1900 hours on weekdays, over a three-month period. When a participant was on evening call, we provided the person with a smart phone, through which handover conversations were recorded and time stamped. After each handover call, the participant was requested to rate the handover quality on a 5-point Likert scale (1: very poor, 5: excellent) and to share their handwritten notes. Submission of the handover quality ratings and notes was voluntary, and the participant may opt out for any reason. A human factors researcher shadowed the participants during the time of handover and collected information regarding the handover (e.g. handover location and the level of ambient noise) on a shadowing log file. Due to the exploratory nature of the present study, no formal sample size calculation was undertaken. Instead, at least 20 handover sessions over 20 days was expected to provide enough data points, in accordance with benchmarks of past studies.(8,11,12)
The Domain-Specific Review Boards of the National Healthcare Group, Singapore, approved the present study and all participants gave their informed consent. A panel of subject matter experts (SMEs), comprising two consultants and one registrar, was formed to guide the study and provide medical input. Prior to data analysis, the registrar from the SME panel reviewed the handover recordings and handwritten notes, and removed all identifiable information, including the patient name and identity card number.
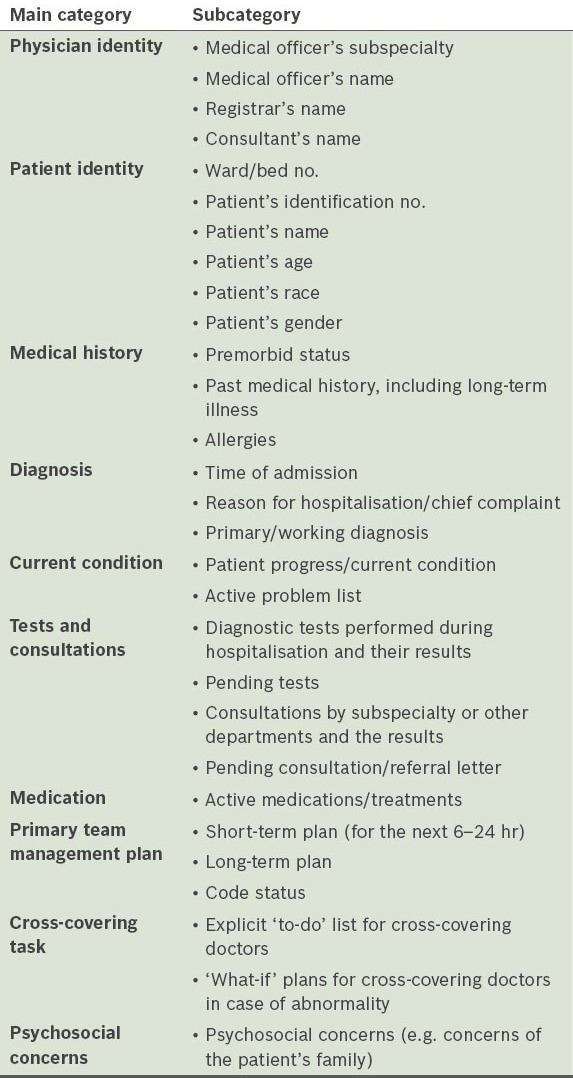
The main outcome measures were coverage of patient information, quality of the handover, and handover duration, time and location. As a first step of data analysis, we developed a coding scheme to categorise the various types of patient information. The coding scheme developed was based on four recently published coding systems.(8,11-13) It was further refined by the SME panel, resulting in 10 main categories and 29 subcategories (Table I).
Table I.
Coding scheme for patient information.
The handover recordings were transcribed using the Transcriber® software (http://trans.sourceforge.net/). For the purpose of coding the communication transcripts and handwritten notes, the registrar from the SME panel trained the human factors researcher on how to classify patient information. An information category was considered to have been addressed in the discussion if the participants made comments belonging to that category. For example, the comment, “No, we did not perform a CT brain scan” was regarded as a discussion on ‘diagnostic tests performed and their results’, even though the test was not performed. The registrar and human factors researcher each independently coded a set of 30 randomly selected transcripts, and the inter-rater reliability(14) between the two coders revealed a high consistency (k = 0.852). The rest of the transcripts and handwritten notes were subsequently evaluated by the human factors researcher.
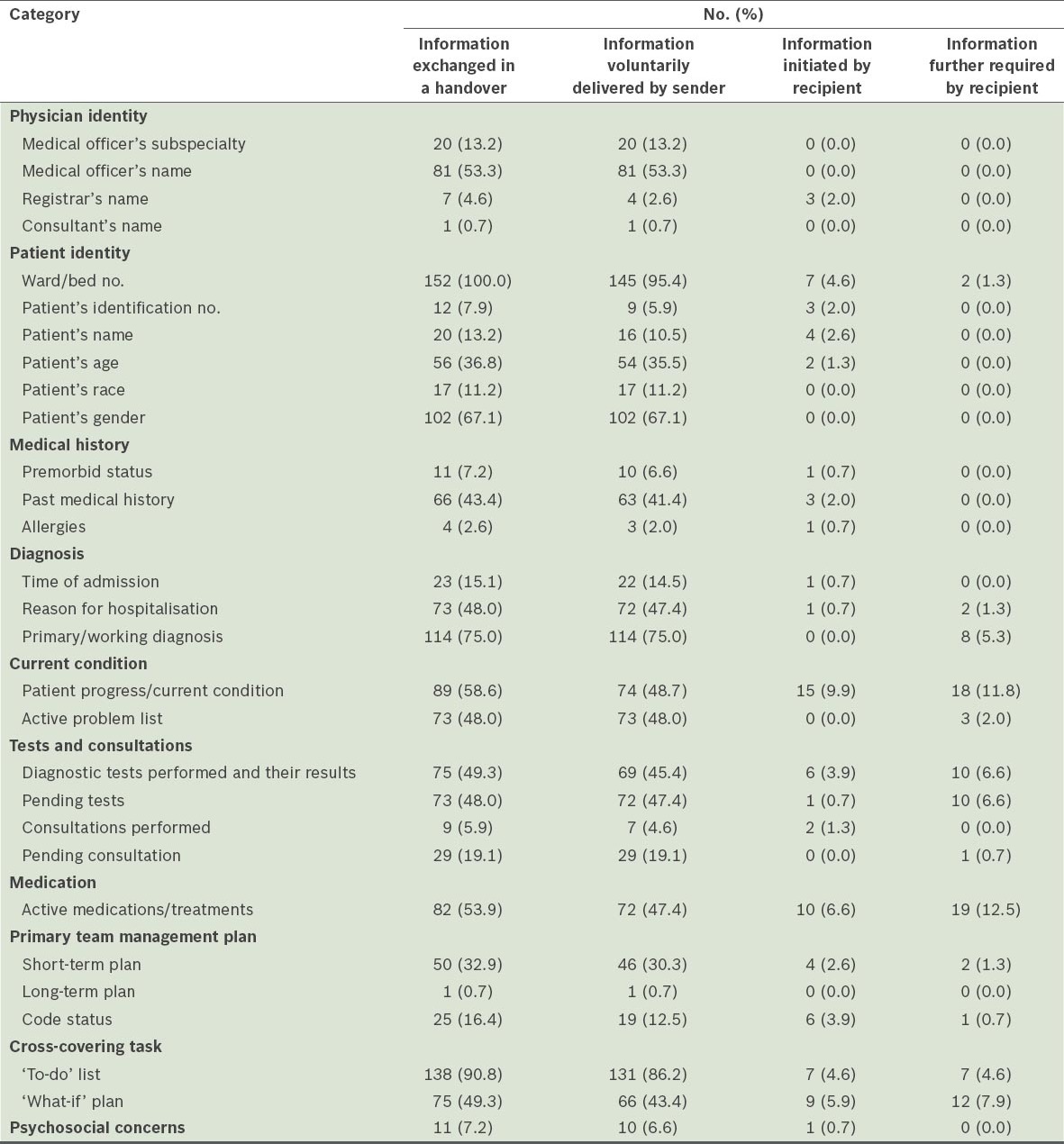
In the second step of our data analysis, each patient information item was coded according to the person who initiated the transfer of that item. ‘Information voluntarily delivered by sender’ was information that was voluntarily transferred by a primary team physician to an on-call physician. ‘Information initiated by recipient’ was information that was obtained through the prompting of an on-call physician, and not delivered voluntarily by the primary team physician. These two types of information were mutually exclusive and their sum equalled to ‘information exchanged in a handover’. ‘Information further required by recipient’ was information that an on-call physician further required, after voluntary information was delivered by a primary team physician (Table II). In the final step of our data analysis, the shadowing log files were analysed following a grounded theory approach,(15) to categorise the environmental factors.
Table II.
Verbal information transfer between primary team physicians (i.e. the senders) and on-call physicians (i.e. the recipients) for 152 patients.
RESULTS
A total of 23 physicians (all MOs; 14 female and 9 male) participated in the present study. The mean duration of their experience as MOs was 2.5 ± 1.2 (range 0.5–4) years and their mean age was 27.3 ± 2.0 (range 24–33) years. Over the duration of the study, 96 handover calls covering 152 patient cases were recorded. Handover quality ratings were collected for the handovers of 98 (64.5%) patients and handwritten notes were collected for the handover of 102 (67.1%) patients. To examine the information transfer during the handovers, we analysed the coverage of each information category in: (a) the senders’ and recipients’ verbal communication; and (b) the recipients’ written handover notes.
Table II shows the frequency of each information category in the senders’ and recipients’ verbal communication. Only information regarding the subcategory, ward/bed number, was exchanged for all 152 patient cases. Other subcategories of information that were exchanged frequently were ‘to-do’ list (90.8%), primary/working diagnosis (75.0%), patient’s gender (67.1%), patient progress/current condition (58.6%), active medications/treatments (53.9%), medical officer’s name (53.3%), ‘what-if’ plan (49.3%), and diagnostic test performed and their results (49.3%).
The primary team physicians initiated the majority of the discussions. Five subcategories of information were voluntarily delivered in more than half of the cases – ward/bed number (95.4%), ‘to-do’ list (86.2%), primary/working diagnosis (75.0%), patient’s gender (67.1%) and medical officer’s name (i.e. the sender) (53.3%). The on-call physicians commonly initiated questions related to patient progress/current condition (9.9%), active medications/treatments (6.6%), ‘what-if’ plan (5.9%) and ‘to-do’ list (4.6%). The subcategories that on-call physicians frequently requested further information included active medications/treatments (12.5%), patient progress/current condition (11.8%), ‘what-if’ plan (7.9%), diagnostic tests performed and their results (6.6%), pending tests (6.6%), primary/working diagnosis (5.3%) and ‘to-do’ list (4.6%).
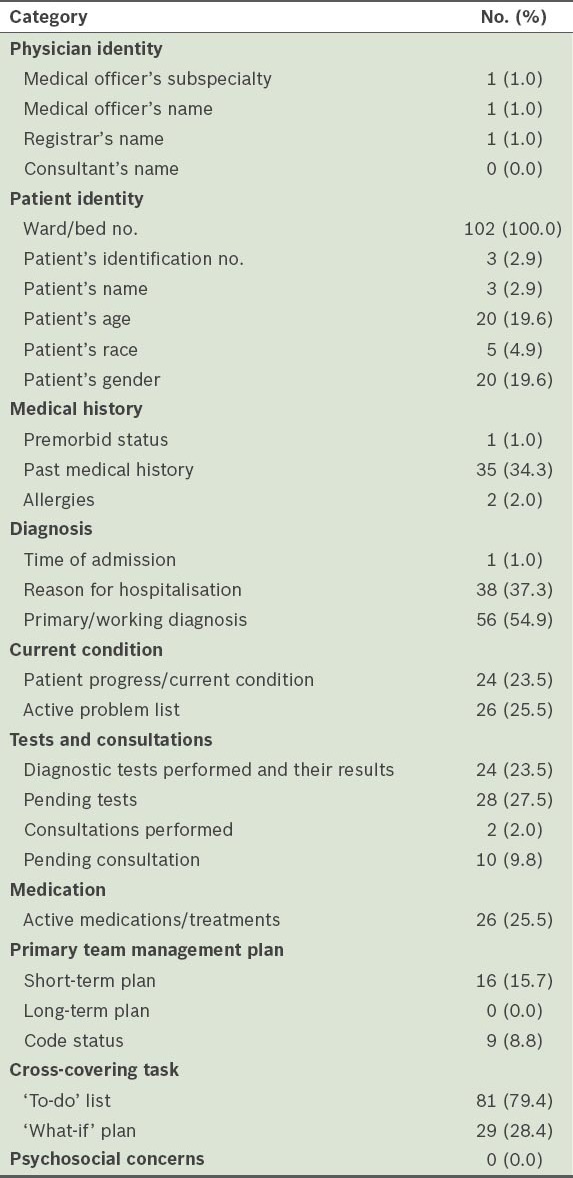
Table III lists the frequency of each information category in the on-call physicians’ handwritten notes. Only one information item, ward/bed number, was written down by the on-call physicians for every patient. The following information items were also frequently written down by the on-call physicians: ‘to-do’ list (79.4%), primary/working diagnosis (54.9%), reason for hospitalisation (37.3%), past medical history (34.3%), pending tests (27.5%), active problem list (25.5%), active medications/treatments (25.5%) and patient progress/current condition (23.5%).
Table III.
Information recorded in the handwritten notes of the on-call physicians for 102 patients.
In-depth analysis of the tasks in the ‘to-do’ list showed that there were five major types of tasks: (a) review sick patients (n = 42, 27.6%); (b) trace diagnostic test results (n = 71, 46.7%); (c) trace referral letter replies (i.e. a primary team physician referred a patient to another staff) (n = 15, 9.9%); (d) note for patients (i.e. a primary team physician informed an on-call physician of patients with a high possibility of deteriorating during the on-call period) (n = 17, 11.2%); and (e) others (n = 7, 4.6%). ‘Others’ included tasks related to administrative matters, such as obtaining a signature from the patient. There were 13 cases without an explicit statement regarding the ‘to do’ tasks; these cases were classified based on the other information discussed during the handover conversation.
As it was postulated that information transfer, handover duration and handover quality may differ across the different task types, we tabulated the number of information categories exchanged, the handover duration and the handover quality rating per handover, for each task type (Table IV). The mean rate of information exchange was 9.8 categories of information per handover. The primary team physicians voluntarily delivered a mean of 9.2 categories of information per handover, while the on-call physicians prompted a mean of 0.6 categories of information per handover. The mean number of categories where further information was required was 0.6 and the mean number of categories where information was written down was 5.5. The handover of a patient took a mean duration of 80 s. The quality of the majority of handovers was perceived as good, with a mean score of 3.6 (1: very poor, 5: excellent).
Table IV.
Information transfer, duration and perceived handover quality of each type of task.
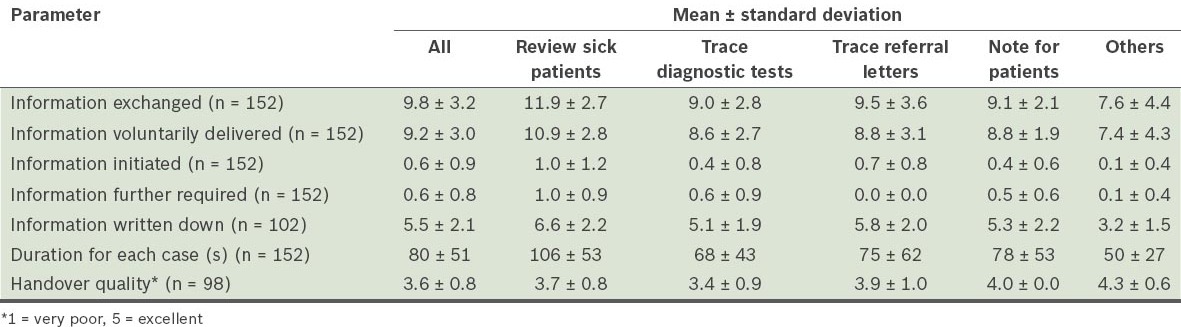
One-way analysis of variance was used to examine the effect of task type on the number of information categories transferred, the handover duration and the handover quality. We found that task type significantly affected the number of information categories (a) exchanged in a handover (p < 0.001); (b) voluntarily delivered by the sender (p < 0.001); (c) initiated by the recipient (p < 0.005); (d) further requested by the recipient (p < 0.005); and (e) written down by the recipient (p < 0.001). The task type ‘review sick patients’ had the highest number of information categories exchanged in all the four types of information transfer, while ‘others’ had the lowest. In addition, there was a significant difference in the handover duration (p < 0.01) between the task types ‘review sick patients’ and ‘others’ (the former took the longest time, while the latter took the shortest time). There was no significant difference in handover quality.
To examine the environmental factors during shift handovers, we analysed the handover call time stamps and shadowing log files. The results showed that the on-call physicians had no designated time or place for handovers. They received 34.1% of the handover calls within the first 30 minutes after their shift started, 40.8% during 1800–1830 hours and 25.0% during 1830–1900 hours. The on-call physicians received handover calls at three locations: (a) the resident room (42.3%); (b) the nurse station (35.4%); and (c) in transit (i.e. while the physician was moving from one place to another) (18.3%), and others (4.0%). When participants received handover calls in the nurse station or in transit, they were subject to high ambient noises. However, when they received handover calls in the resident room, they were subject to high ambient noises only occasionally. It should be noted that although the majority of handover calls were received when the on-call physicians were at the resident room/nurse station, it did not necessarily mean that they had attended to the call in the same resident room/nurse station throughout the handover period. On the contrary, the on-call physicians were constantly moving from one place to another.
DISCUSSION
The results of the present study revealed that physicians allocated their time and effort according to the severity level and care demands of patients; ‘review sick patients’ had the highest number of information categories transferred and the longest handover duration. This is consistent with our SME panel’s opinion that the task ‘review sick patients’ usually involved patients with high severity, and should therefore be given priority over the other four types of tasks. It supports the hypothesis proposed by Nemeth et al,(16) which states that “the greatest amount of attention would be paid to the patients who require the greatest amount of care.” Since the condition of patients in general medical wards are varied (from soon-to-be-discharged patients to those who are scheduled to be sent to an intensive care unit), task prioritisation is necessary for physicians to cope with the variability of care demands.
Our analysis of handover information revealed two major problems, namely poor implementation of non-modifiable patient identifiers and inadequate transfer of critical information. Despite World Health Organization’s recommendation to use at least two non-modifiable patient identifiers,(17) the physicians in the present study depended mainly on one modifiable identifier, i.e. ‘ward/bed number’ (100%). The coverage of ‘patient’s identification number’ (7.9%) and ‘patient’s name’ (13.2%) was much lower than that in previous studies.(8,12) This finding is disconcerting, as patients might be moved to other locations due to reasons such as medical conditions, and therefore, the sole dependence on ‘ward/bed number’ would increase the risk of identification errors.
The present study also showed that even in the case of certain critical information categories, such as ‘primary/working diagnosis’ (75.0%) and ‘‘to-do’ list’ (90.8%), the handover of patient information was not perfect. Although inadequate patient information transfer has been reported in previous studies,(18,19) it should be highlighted that this inadequacy could be exacerbated in high sender/recipient ratio settings due to tighter constraints on time and effort for each patient. This is observed in the mean handover duration per patient in the present study, which was conducted in a high sender/recipient setting; the duration was shorter than that reported in low sender/recipient ratio settings (80 s vs. 148 s).(12)
The Joint Commission recommends that handovers include an opportunity for questions to be asked and answered.(20) This recommendation is supported by experimental studies on technology-mediated communication; one study showed that adding interactive channels enabled conversation parties for clarifying doubts and suggesting alternatives, thus contributing to the participants’ understanding of a situation.(21) The synchronous verbal handover methods, which was adopted in the present study, enabled interaction and feedback in real time. As a result, the primary team physicians and on-call physicians worked together to build a good representation of the patient. The result is consistent with a study by Horwitz et al.(22)
Despite the advantage of synchronous feedback, the present study revealed that systemic information loss occurred in pure verbal communication. This was observed when on-call physicians transferred verbally delivered information into written notes. On average, the primary team physicians and on-call physicians discussed 9.8 information categories per patient case; however, on-call physicians wrote down an average of only 5.5 information categories out of the 9.8 delivered (Table IV). There were large discrepancies between information exchanged verbally and information written down, even for categories bearing critical patient information (e.g. ‘active problem list’ and ‘‘what-if’ plans’). Such discrepancies may result in a strong negative impact on handover quality and patient safety. As memory retention without written documentation is extremely low,(23,24) it is highly likely that the on-call physicians would be unable to recall information that is not written down. In other words, potentially up to 40% of the handover information communicated could be lost during the transfer of information from the primary physicians to the on-call physicians.
One potential reason is the increased mental workload required from the recipient during a handover that is conducted over the telephone. The high sender/recipient ratio in the present study made it difficult for face-to-face or bedside handovers to be conducted, thus hindering the physical transfer of written handover notes. The shortage of written handover notes increases the mental workload of on-call physicians during handovers.(25) The on-call physicians have to record down vital patient information, in addition to perceiving and understanding the transferred information, probing for more details when necessary, and synthesising all given information into an accurate mental model of the patient. Under such high mental workloads, it is not surprising that a high percentage of information is lost from the sender to the recipient during the handover.
In the present study, the physicians did not have a designated time or place for handovers. The handovers happened throughout the entire shadowing period (1730–1900 hours), and with only 35% of the handover calls received within the first 30 minutes of the start of the shift. Due to the prolonged handover period, it was not possible for the on-call physician to stay in one location or to find a conducive environment for the handover. In fact, more than half of the calls were received in a noisy environment. Interruptions, ambient noise and other distractions may work as distractors that decrease the handover quality and discourage the on-call physicians from further communication to clarify doubts.(10)
According to our SME panel, it was difficult to coordinate shift handovers among the various medical teams due to the dynamic nature of clinical work. The high sender/recipient ratio further worsened the situation, as the larger number of handover senders translates to a larger variation in handover time. The prolonged handover period made it impossible for the on-call physicians to be stationed at a specific location for the purpose of receiving handover information, as they had to spend time caring for patients.
In the present study, we investigated the handover practices in a general medical ward of a university hospital in Singapore, which has a handover sender/recipient ratio of up to 20. We identified the effective handover strategies that were adopted by physicians under the extreme condition of a high sender/recipient ratio, as well as the vulnerabilities that were unique or exacerbated in such a setting. Alarmingly, poor implementation of non-modifiable patient identifiers and inadequate transfer of critical information were identified as the two major vulnerabilities in handover content. Despite the advantage of synchronous feedback in the use of telephone communication, the present study revealed systemic information loss in pure verbal communication. In addition, the physicians had no designated time or place for handovers.
Based on the identified deficiencies, we suggest several possible interventions for the improvement of handover quality. First, we propose the implementation of a standardised handover dataset. This would provide a structure for the handover materials, helping the handover senders to plan in advance, thus reducing the possibility of inadequate information transfer. Second, the implementation of both written and verbal handovers could reduce the information loss from handover senders to handover recipients, ensuring the intended patient information is successfully received and recorded. Third, in an effort to ensure a conductive environment for handovers, institutional enforcement may be needed to coordinate and regulate the practices.
The present study is one of the pioneering studies on shift handovers in Asia. It contributes to the medical literature through its report of handover practices in a high sender/recipient ratio setting and its examination of the challenges of implementing existing handover recommendations in a high sender/recipient ratio setting. However, the present study was not without limitations. The findings of the present study cannot be generalised to all situations, as it is based on the practices of only one department in a single institution. However, it is likely that many hospitals in Asia have higher sender/recipient ratios than their western counterparts, largely due to the prevalent shortage of physicians.(26) In other words, the findings of the present study may be generalised to most hospitals in Asia. Another shortcoming is that the measurement of handover quality was based on subjective ratings. These ratings may have been influenced by other factors, such as the level of familiarity between the participants. However, since anonymity of evaluation was emphasised throughout the study and the submission of handover ratings was voluntary, the impact of these factors is expected to be minor.
In conclusion, clinical handover is an area deserving further research. The recommendations and solutions to address the unique challenges of shift handovers in high sender/recipient ratio settings should be evaluated in further studies.
ACKNOWLEDGEMENTS
We are grateful to the Department of Medicine, National University Hospital System, Singapore, for its support in the present study. This study was also supported by the Health Systems Competitive Research Grant (HSRCRG09/01) from the Ministry of Health, Singapore.
REFERENCES
- 1.Patterson ES, Roth EM, Woods DD, Chow R, Gomes JO. Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16:125–32. doi: 10.1093/intqhc/mzh026. [DOI] [PubMed] [Google Scholar]
- 2.Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. Consequences of inadequate sign-out for patient care. Arch Intern Med. 2008;168:1755–60. doi: 10.1001/archinte.168.16.1755. [DOI] [PubMed] [Google Scholar]
- 3.Singh H, Thomas EJ, Petersen LA, Studdert DM. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167:2030–6. doi: 10.1001/archinte.167.19.2030. [DOI] [PubMed] [Google Scholar]
- 4.Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identifiedin an extensive review. Qual Saf Health Care. 2010;19:493–7. doi: 10.1136/qshc.2009.033480. [DOI] [PubMed] [Google Scholar]
- 5.Raduma-Tomàs MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospitals: a literature review. BMJ Qual Saf. 2011;20:128–33. doi: 10.1136/bmjqs.2009.034389. [DOI] [PubMed] [Google Scholar]
- 6.Yang X, Koh RY, Tay BT, et al. Las Vegas, USA. CA: Sage Publications; 2011. Clinical shift handoffs in Singapore: A three-phase prospective. In Proceedings of the Human Factors and Ergonomics Society 55th Annual Meeting, 19-23 September. [Google Scholar]
- 7.Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM. Adequacy of information transferred at resident sign-out (in-hospital handover of care): a prospective survey. Qual Saf Health Care. 2008;17:6–10. doi: 10.1136/qshc.2006.019273. [DOI] [PubMed] [Google Scholar]
- 8.Alem L, Joseph M, Kethers S, Steele C, Wilkinson R. Information environments for supporting consistent registrar medical handover. HIM J. 2008;37:9–25. doi: 10.1177/183335830803700102. [DOI] [PubMed] [Google Scholar]
- 9.Wears RL, Perry SJ, Patterson ES. Handoffs and Transitions of Care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. CRC Press; 2011. [Google Scholar]
- 10.Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80:1094–9. doi: 10.1097/00001888-200512000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ye K, McD Taylor D, Knott JC, Dent A, MacBean CE. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas. 2007;19:433–41. doi: 10.1111/j.1742-6723.2007.00984.x. [DOI] [PubMed] [Google Scholar]
- 12.Sledd R, Bass EJ, Borowitz S, Waggoner-Fountain L. San Francisco, CA: Proceeding of the 50th Annual Meeting of the Human Factors and Ergonomics Society; October 16-20 2006; 2006. Characterization of sign-out in pediatric acute care wards to inform process improvement. [Google Scholar]
- 13.Flanagan ME, Patterson ES, Frankel RM, Doebbeling BN. Evaluation of a physician informatics tool to improve patient handoffs. J Am Med Inform Assoc. 2009;16:509–15. doi: 10.1197/jamia.M2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carletta J. Assessing agreement on classification tasks: The kappa statistic. Comput Ling. 1996;22:249–54. [Google Scholar]
- 15.Martin PY, Turner BA. Grounded Theory and Organizational Research. J Appl Behavioral Sci. 1986;22:141–57. [Google Scholar]
- 16.Nemeth CP, Kowalsky J, Brandwijk M, et al. Between Shifts: Healthcare Communication in the PICU. In: Nemeth CP, editor. Improving Healthcare Team Communication: Building on Lessons from Aviation and Aerospace. Ashgate; 2008. pp. 135–53. [Google Scholar]
- 17.WHO Collaborating Centre for Patient Safety Solutions. Patient Identification. Patient Safety Solutions 2007 [online] [Accessed January 7 2013]. Available at: http://www.ccforpatientsafety.org/common/pdfs/fpdf/presskit/PS-Solution2.pdf .
- 18.Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14:401–7. doi: 10.1136/qshc.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79:186–94. doi: 10.1097/00001888-200402000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Joint Commission. 2006 Critical Access Hospital and Hospital National Patient Safety Goals 2006 [online] [Accessed January 7 2013]. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsg_cah.htm .
- 21.Clark HH, Krych MA. Speaking while monitoring addressees for understanding. J Mem Lang. 2004;50:62–81. [Google Scholar]
- 22.Horwitz LI, Parwani V, Shah NR, et al. Evaluation of an asynchronous physician voicemail sign-out for emergency department admissions. Ann Emerg Med. 2009;54:368–78. doi: 10.1016/j.annemergmed.2009.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhabra G, Mackeith S, Monteiro P, Pothier DD. An experimental comparison of handover methods. Ann R Coll Surg Engl. 2007;89:298–300. doi: 10.1308/003588407X168352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pothier D, Monteiro P, Mooktiar M, Shaw A. Pilot study to show the loss of important data in nursing handover. Br J Nurs. 2005;14:1090–3. doi: 10.12968/bjon.2005.14.20.20053. [DOI] [PubMed] [Google Scholar]
- 25.Harvey CM, Schuster RJ, Durso FT, Matthews AL, Surabattula D. Human Factors of Transition of Care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Lawrence Erlbaum Associates; 2006. [Google Scholar]
- 26.World Health Organization. Global Health Observatory Data Repository, Density per 1000. [Accessed November 15 2012];2012 [Google Scholar]


