Abstract
Nigeria has the world's 10th largest tuberculosis (TB) burden. Targeted community-based interventions can potentially help reduce TB incidence. We designed an intervention in a periurban community where 10 community volunteers were trained to provide community TB education and also detect and refer TB suspects to a nearby clinic. To determine the effect of the intervention on knowledge, attitude, and preventive practices of TB, we compared results from a pre-intervention survey with those of a post-intervention survey. Pre-intervention, respondents had a mean knowledge score of 10.6 ± 7.0 of a possible 34, a mean attitude score of 5.8 ± 3.3 of a possible 10, and a mean practice score of 5.3 ± 1.4 of a possible 7. The intervention significantly increased the mean knowledge score to 16 ± 5.4 (P < 0.001) and mean attitude score to 7.0 ± 1.8 (P < 0.001); however, there was no statistically significant difference in the mean practice score. Eight TB suspects were referred to the clinic, and one suspect was subsequently diagnosed with TB. The use of trained community volunteers to share information on TB improved the overall knowledge and attitudes of respondents. Continued empowerment of the community should be encouraged to promote TB prevention and care.
Introduction
Nigeria has the world's 10th largest tuberculosis (TB) burden, with 180,000 estimated new cases in 2012.1 Although the Stop TB intervention reduced prevalence from an estimated 521 cases per 100,000 population in 2007 to 270 cases per 100,000 population by 2012, this remains close to double the 2015 Global Plan to Stop TB target of 141 cases per 100,000 population.1,2 It is likely that the current data on TB are underestimated, because transmission is ongoing within communities with high numbers of undetected smear-positive cases.3
National TB programs (NTPs) in most countries, which had hitherto promoted access to effective TB care through government health facilities, are now placing more emphasis on TB care through other health service providers, including the community. The promotion of community contribution to TB care is particularly urgent in sub-Saharan African countries, like Nigeria, where human immunodeficiency virus (HIV) is fuelling the TB epidemic and stretching the limited capacity of government health service providers.4 Communities can contribute to TB care by participating in direct observation of treatment, supporting and motivating TB patients, detecting cases, and increasing community awareness and access to drugs.4,5
Empowering communities to actively participate in TB prevention has been identified as one of the key areas of focus for prevention and reduction of missed cases; this has led to the adoption and implementation of community directly observed treatment, short-course (DOTS) programs that involve the recruitment and training of community members as treatment supporters as well as the identification and referral of TB suspects.6 International control efforts have recognized the need to engage communities through public communication campaigns to educate people about symptoms and facilities for care as well as reduce stigma.7
Community health workers and community volunteers (CVs) can carry out community-based TB activities based on national and local contexts. Although community health workers have formal health training and are often compensated with financial incentives, CVs are community members who are systematically sensitized about community TB care through short, specific training or repeated contact with professional health workers, and they are often not compensated financially.8
Successes in TB case detection and subsequent treatment have been documented when community care providers have been trained to provide community TB care.9–11 Specifically, programs that used CVs observed comparable successes with programs that used health workers.12,13 However, there is a dearth of information from intervention studies with outcome indicators that include change in community TB knowledge, attitude, and preventive practices after training community care providers.
In Nigeria, community TB care is implemented within the National Strategic Plan for Tuberculosis and Leprosy Control; it aims to increase community awareness of TB as a means of eliminating the stigma associated with TB as well as improving case detection, early diagnosis, and uptake of treatment.14 At the end of 2012, it was reported that less than 5% of TB patients were cared for by CVs and that wide variations existed between the states.15
Lack of TB knowledge and stigmatizing attitudes have been identified in previous community-based studies in Nigeria as detrimental to TB prevention and control.16,17 This study, therefore, aimed to determine the effect of a community-based intervention on improving TB knowledge, attitudes, and preventive practices among adults in Idi Araba, a periurban community in Lagos state, Nigeria.
Materials and Methods
Study area.
This quasiexperimental study was carried out in Idi Araba, 1 of 19 wards in Mushin local government area (LGA) of Lagos state (an urban LGA). It houses the College of Medicine, University of Lagos (CMUL) and Lagos University Teaching Hospital (LUTH), a tertiary facility with a functional DOTS clinic. Idi Araba is made up of four zones, with a total of about 47 streets that are well-demarcated with street signs. The community has an estimated population of 42,000 who live in a largely congested residential area with inadequate sanitation and low-quality housing, which is characteristic of periurban communities in the state. The study population was adults ages 18 years and over living in Idi Araba.
Sampling.
A sample size of 252 was calculated using the formula for comparison of proportions,18 which ensured a power of 80% to detect a 20% increase in TB knowledge after intervention. Before the intervention, the research team visited with the community development association (CDA) of each zone, where the goals and objectives of the study were explained. A multistage sampling technique was used to select 252 respondents pre-intervention. In the Idi Araba community, there are four zones; the streets in each zone were collected from the zonal CDA representative, and this information was followed by simple random sampling (lottery method) to select four streets from each zone. For each of the streets, community mapping and counting of habitable houses were carried out. Systematic random sampling was then used to select houses for inclusion. Typically, each house had several apartment units representing separate households; one household was selected, and one eligible respondent was then selected per household by simple random sampling. The same procedure was repeated to select another sample of 252 respondents post-intervention.
Data collection.
Six trained field interviewers with post-secondary education who were fluent in the local languages collected data using a pre-tested, structured questionnaire, which was adapted from the World Health Organization (WHO) sample Advocacy, Communication and Social Mobilization Knowledge, Attitudes and Practice (KAP) survey questionnaire.19 The tool contained sections on personal characteristics; living conditions and health-seeking behavior; TB knowledge and awareness; TB attitudes and care-seeking behavior; TB attitudes and stigma; and TB information and preventive practices. The survey was administered pre-intervention and repeated at 6 months post-intervention. Monthly data on referrals of TB suspects from the community were collected from the patient registry at the DOTS clinic at LUTH.
Study intervention.
Ten CVs were nominated by the CDA after a meeting to explain the criteria for selection of CVs. The criteria for selection of CVs included recommended by the community, willingness to participate in community TB care, residing in the community, and ability to speak the local language fluently.14 The intervention was a 2-day training on community TB care for the CVs. The researchers (M.B., A.S., O.O., and O.L.-P.) served as the facilitators and were guided by a training manual developed by the Federal Ministry of Health.14 The CVs were trained to sensitize the community on TB, detect cases of TB, and link suspect TB cases to the DOTS clinic at LUTH. To standardize the health education discussions in which CVs would engage, they were trained using role play as a methodology to include core aspects of TB information (cause, signs/symptoms, transmission, risk factors, and preventive measures) in all of their health talks. Their knowledge of core areas of TB increased from a mean score of 16.9 ± 5.1 (of a possible score of 29) at the pre-test evaluation to 24.6 ± 3.7 at the post-test evaluation. After the training, the CVs organized health talks in the market, church, and mosque and targeted households and different occupational groups, such as hairdressers and charcoal sellers. They also had one-on-one discussions with friends, neighbors, and other community members. The CVs organized two health education activities as a group within each month of the intervention phase and had individual daily discussions with at least five community members each. They delivered educational pamphlets door to door and hung up posters on every street to aid their health talks. They also held a rally to create awareness along the streets in Idi Araba using a band and songs on TB and had health talks with groups of people along the way. There were monthly monitoring and evaluation meetings between the researchers and the CVs in the community to monitor progress, address challenges, and collect reports, such as notebook records and video recordings of health education activities, TB suspects, referral registers, and feedback of referral forms from the DOTS clinic.
Ethical consideration.
The study proposal was approved by the Health Research and Ethics Committee of LUTH. Written informed consent was obtained from the respondents before the administration of questionnaires, and confidentiality was maintained by not using identifiers.
Data analysis.
Data collected were analyzed using Epi Info Statistical Software, version 3.5.1 (Centers for Disease Control and Prevention, Atlanta, GA) and Statistical Package for Social Sciences (SPSS), version 15 (SPSS Inc., Chicago, IL). Significant differences in pre- and post-intervention values were evaluated using χ2, Fisher's exact, and Student's t tests where appropriate. Level of significance was set at 0.05.
The overall knowledge, attitude, and practice of respondents were assessed. For knowledge, a score of 1 was given to correct responses, and the possible scores ranged from 0 to 34. Ten questions on attitude were scored, and the positive responses were each given a score of 1; the maximum score obtainable was 10. For preventive practices, four questions were scored, three of which were on a 3-point scale graded 0–2; the maximum score obtainable was 7. For multivariate analyses, the cutoff for what was considered to be good knowledge, positive attitude, and good practice was 50%. The outcomes measured included differences in community knowledge, attitude, and preventive practices.
To control for possible confounders to the outcome variables that may have resulted from difference in pre- and post-intervention sampling, demographic variables with statistical differences at P < 0.2 were considered for inclusion in logistic regression analyses. These demographic variables were entered into the model using a block entry approach. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were produced for each predictor variable. There was no colinearity among the variables included in the final model.
Results
The respondents in both pre- and post-intervention groups ranged in age from 18 to 80 years old, with a mean age of 36.2 ± 13.7 years old in the pre-intervention group and 34.5 ± 10.0 years old in the post-intervention group. The pre- and post-intervention respondents were mostly female (59.9% versus 51.2%), were married (62.3% versus 69%), and had secondary education (41.3% versus 44.4%). About one-half (48.9% versus 53.4%) of the jobs in both groups were semiskilled. The pre- and post-intervention respondents differed in age; there were higher proportions of older age groups in the pre-intervention group (P = 0.003) (Table 1).
Table 1.
Sociodemographic characteristics of respondents before and after intervention
| Variables | Pre-intervention (N = 252) frequency (%) | Post-intervention (N = 252) frequency (%) | P value |
|---|---|---|---|
| Age group (years) | |||
| < 25 | 49 (19.4) | 32 (12.7) | 0.003 |
| 25–34 | 85 (33.7) | 110 (43.7) | |
| 35–44 | 58 (23.0) | 72 (28.6) | |
| 45–54 | 29 (11.5) | 27 (10.7) | |
| 55–64 | 19 (7.5) | 8 (3.2) | |
| > 64 | 12 (4.8) | 3 (1.2) | |
| Mean age | 36.2 ± 13.7 | 34.5 ± 10.0 | 0.120 |
| Sex | |||
| Female | 151 (59.9) | 129 (51.2) | 0.060 |
| Male | 101 (40.1) | 123 (48.8) | |
| Marital status | |||
| Single | 72 (28.6) | 61 (24.2) | 0.289 |
| Married | 157 (62.3) | 174 (69.0) | |
| Cohabiting | 3 (1.2) | 0 (0.0) | |
| Separated | 7 (2.8) | 4 (1.6) | |
| Divorced | 2 (0.8) | 4 (1.6) | |
| Widowed | 11 (4.4) | 9 (3.6) | |
| Education | |||
| No formal | 42 (17.7) | 30 (12.0) | 0.054 |
| Primary | 50 (19.8) | 69 (27.4) | |
| Secondary | 104 (41.3) | 112 (44.4) | |
| Post-secondary | 56 (22.2) | 41 (16.3) | |
| Religion | |||
| Christianity | 118 (46.8) | 98 (38.9) | 0.228 |
| Islam | 133 (52.8) | 151 (59.9) | |
| Traditional | 1 (0.4) | 2 (0.8) | |
| Other | 0 (0.0) | 1 (0.4) | |
| Ethnicity | |||
| Yoruba | 134 (53.2) | 152 (60.3) | 0.223 |
| Hausa | 66 (26.2) | 61 (24.2) | |
| Igbo | 33 (13.1) | 29 (11.5) | |
| Others | 19 (7.5) | 10 (4.0) | |
| Employment status | |||
| Employed | 186 (73.8) | 204 (81.0) | 0.070 |
| Unemployed | 66 (26.2) | 48 (19.0) | |
| Occupation N | 186 | 204 | |
| Senior professional | 3 (1.6) | 3 (1.5) | 0.126 |
| Intermediate professional | 21 (11.3) | 14 (6.9) | |
| Junior professional/skilled | 43 (23.1) | 60 (29.4) | |
| Semiskilled | 91 (48.9) | 109 (53.4) | |
| Unskilled | 28 (15.1) | 18 (8.8) | |
| Status of the unemployed N | 66 | 48 | |
| Housewife | 28 (42.4) | 24 (50.0) | 0.310 |
| Student | 25 (37.9) | 14 (29.2) | |
| Apprentice | 6 (9.1) | 8 (16.7) | |
| Retired | 7 (10.6) | 2 (4.2) | |
In total, 201 (79.8%) respondents had heard about TB before the survey, and this value increased significantly to 245 (97.2%) respondents post-intervention (P < 0.001); 40.1% and 48.4% of the pre- and post-intervention respondents, respectively, knew a person with TB.
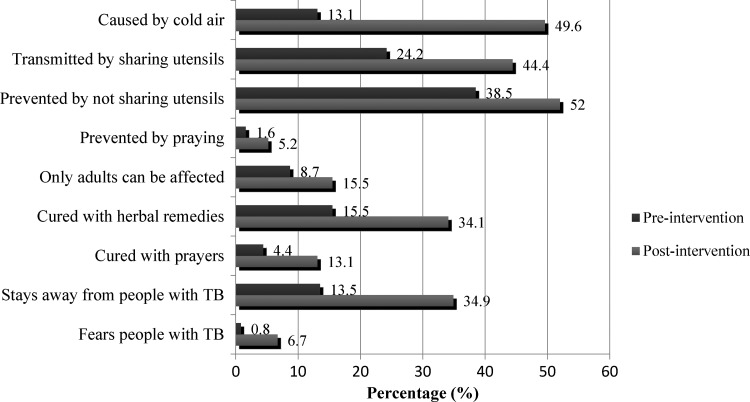
Post-intervention, there was a statistically significant increase (34.5% increase) in the proportion of respondents who knew that TB was caused by a germ. However, the increase in the proportion that mentioned cold air as a cause of TB was also significant (P < 0.001) (Figure 1). After the intervention, there were statistically significant increases in proportions of respondents who recognized cough, coughing up sputum, coughing up blood, weight loss, fever, chest pain, and fatigue as symptoms of TB. Also, a significantly higher proportion of post-intervention respondents knew that a 2-week duration of cough was regarded as suspicious for TB (P < 0.001).
Figure 1.
Significant persistence of misconceptions and stigmatizing attitudes among respondents (N = 252; P values < 0.05).
Significantly higher proportions of post-intervention respondents knew TB to be transmissible (22.2% increase) and mentioned the correct mode of transmission (37.7% increase) compared with pre-intervention respondents. However, the increases in the proportions that mentioned sharing eating utensils and living in the same house as modes of transmission also increased significantly (Figure 1). The proportion of respondents who mentioned mouth/nose covering when coughing/sneezing as a way to prevent TB also increased significantly (from 23.4% to 71.4% from pre- to post-intervention, respectively; P < 0.001). There was improvement in the knowledge that homeless people, drug users, people living with HIV/acquired immunodeficiency syndrome (AIDS), prisoners, smokers, passive smokers, and people who live with people with TB were at greater risk of acquiring TB. The knowledge of a cure for TB with drugs given at health centers (21.4% increase) also improved significantly (P < 0.001), although few respondents mentioned DOTS at pre- (3.6%) and post-intervention (2.8%). There were statistically significant increases in the proportions of respondents who also mentioned herbal remedies and prayer as ways of curing TB at post-intervention versus pre-intervention (Figure 1). The increases in the proportions of respondents who were aware of a health facility for TB diagnosis and treatment in the LGA (34.3% increase) and knew that TB diagnosis (23.9% increase) and treatment (28.3% increase) were free post-intervention versus pre-intervention were all statistically significant (P < 0.001) (Table 2).
Table 2.
Knowledge of TB before and after intervention
| Knowledge of TB | Pre-intervention (N = 252) frequency (%) | Post-intervention (N = 252) frequency (%) | P value |
|---|---|---|---|
| Cause of TB | |||
| A germ | 42 (16.7) | 129 (51.2) | < 0.001 |
| Signs and symptoms of TB | |||
| Cough | 158 (62.7) | 202 (80.2) | < 0.001 |
| Coughing up sputum | 9 (3.6) | 57 (22.6) | < 0.001 |
| Coughing up blood | 60 (23.8) | 141 (56.0) | < 0.001 |
| Weight loss | 91 (36.1) | 132 (52.4) | < 0.001 |
| Fever | 12 (4.8) | 25 (9.9) | 0.026 |
| Night sweats | 4 (1.6) | 1 (0.4) | 0.373 |
| Chest pain | 18 (7.1) | 64 (25.4) | < 0.001 |
| Shortness of breath | 13 (5.2) | 24 (9.5) | 0.060 |
| Loss of appetite | 10 (4.0) | 15 (6.0) | 0.305 |
| Fatigue | 8 (3.2) | 30 (11.9) | < 0.001 |
| Duration of cough regarded as suspicious for TB | |||
| 2+ weeks | 33 (13.1) | 115 (45.6) | < 0.001 |
| Transmission of TB | |||
| TB is transmissible | 164 (65.1) | 220 (87.3) | < 0.001 |
| Transmitted through air when person with TB coughs/sneezes | 81 (32.1) | 176 (69.8) | < 0.001 |
| Transmitted through air when a person with TB talks/sings | 30 (11.9) | 46 (18.3) | 0.046 |
| Mode of prevention of TB | |||
| Covering mouth/nose when coughing/sneezing | 59 (23.4) | 180 (71.4) | < 0.001 |
| Avoid overcrowding | 28 (11.1) | 53 (21.0) | 0.002 |
| Cross-ventilation at home | 15 (6.0) | 13 (5.2) | 0.697 |
| Good nutrition | 11 (4.4) | 11 (4.4) | |
| BCG immunization in children | 10 (4.0) | 17 (6.7) | 0.166 |
| Age group and gender affected | |||
| Adults and children | 173 (68.7) | 203 (80.6) | 0.002 |
| Men and women | 193 (76.6) | 235 (93.3) | < 0.001 |
| Persons at greater risk of TB* | |||
| Poor people | 102 (40.5) | 114 (45.2) | 0.280 |
| Homeless people | 117 (46.4) | 177 (70.2) | < 0.001 |
| Alcoholics | 115 (45.6) | 131 (52.0) | 0.154 |
| Drug users | 119 (47.2) | 183 (72.6) | < 0.001 |
| People living with HIV/AIDS | 99 (39.2) | 131 (52.0) | 0.004 |
| Prisoners | 128 (50.8) | 171 (67.9) | < 0.001 |
| Smokers | 160 (63.5) | 206 (81.7) | < 0.001 |
| People who stay around smokers | 128 (50.8) | 167 (66.3) | < 0.001 |
| People who live with people with TB | 144 (57.1) | 220 (87.3) | < 0.001 |
| People with diabetes | 38 (15.1) | 32 (12.7) | 0.440 |
| TB treatment | |||
| TB can be cured | 177 (70.2) | 214 (84.9) | < 0.001 |
| Cured with specific drugs given at health facility | 154 (61.1) | 208 (82.5) | < 0.001 |
| Cured with DOTS | 9 (3.6) | 7 (2.8) | 0.611 |
| Aware of health facility for TB diagnosis and treatment in LGA | 76 (30.2) | 177 (70.2) | < 0.001 |
| Aware of free TB diagnosis in LGA | 30 (11.9) | 96 (38.1) | < 0.001 |
| Aware of free TB treatment in LGA | 26 (10.3) | 102 (40.5) | < 0.001 |
BCG = Bacillus Calmette-Guerin.
Prompted questions (each with yes/no/do not know options).
In comparisons of attitudes toward TB, there were no statistically significant differences in the respondents' self-perceived risk of TB and perception of TB as a serious problem in Nigeria post-intervention (Table 3). Also, more respondents (21.4% increase) post-intervention responded that they would feel compassion but would stay away from people with TB than those interviewed pre-intervention (Figure 1). It was also found that, among respondents post- versus pre-intervention, higher proportions would go to the health facility if they had TB symptoms (90.5% versus 75.8%; P < 0.001), felt that HIV-positive people should be concerned about TB (59.1% versus 35.7%; P < 0.001), and were willing to get more information about TB (95.2% versus 75.0%; P < 0.001).
Table 3.
Attitudes toward TB before and after intervention
| Questions on attitudes | Responses | Pre-intervention (N = 252) frequency (%) | Post-intervention (N = 252) frequency (%) | P value |
|---|---|---|---|---|
| In your opinion, how serious a disease is TB? | Very serious | 168 (66.7) | 208 (82.5) | < 0.001 |
| How serious a problem do you think TB is in Nigeria? | Very serious | 146 (57.9) | 156 (61.9) | 0.363 |
| Do you think you can get TB? | Yes | 66 (26.2) | 73 (29.0) | 0.485 |
| Who would you talk to about your illness if you had TB? | Doctor or other medical worker | 128 (50.8) | 176 (69.8) | < 0.001 |
| What would you do if you thought you had symptoms of TB? | Go to health facility | 191 (75.8) | 228 (90.5) | < 0.001 |
| If you had symptoms of TB, when would you go to health facility? | As soon as I realized that symptoms might be TB | 159 (63.1) | 174 (69.0) | 0.158 |
| Do you support BCG immunization for children? | Yes | 198 (78.6) | 241 (95.6) | < 0.001 |
| How expensive do you think TB diagnosis and treatment are in Nigeria? | Free | 29 (11.5) | 86 (34.1) | < 0.001 |
| Which statement is closest to your feeling about people with TB disease? | I feel compassion and desire to help | 153 (60.7) | 105 (41.7) | 0.659 |
| Do you think HIV+ people should be concerned about TB? | Yes | 90 (35.7) | 149 (59.1) | < 0.001 |
| Would you like to get more information about TB? | Yes | 189 (75.0) | 240 (95.2) | < 0.001 |
BCG = Bacillus Calmette-Guerin.
Regarding post-intervention respiratory etiquette, there was no statistically significant difference in the self-reported practice of covering one's mouth when coughing compared with pre-intervention, but there was a statistically significant reduction in the proportion of those who never covered their nose/mouth when sneezing (Table 4). Additionally, higher proportions of the post-intervention group reported use of their hands (90.5% versus 76.2%; P < 0.001), crook of the elbow (6.7% versus 0.8%; P < 0.001), and part of their clothing (15.1% versus 3.2%; P < 0.001) to cover their mouth/nose when coughing/sneezing in the post- versus pre-intervention groups. There was also a significant increase in the self-reported practice of always ensuring cross-ventilation in homes in the post- versus pre-intervention groups (69.0% versus 64.7%; P < 0.001).
Table 4.
Respondents' preventive practices before and after intervention
| Variables | Pre-intervention (N = 252) frequency (%) | Post-intervention (N = 252) frequency (%) | P value |
|---|---|---|---|
| Covers mouth when coughing | 0.300 | ||
| Not at all | 7 (2.8) | 4 (1.6) | |
| Yes, sometimes | 73 (29.0) | 87 (34.5) | |
| Yes, always | 172 (68.3) | 161 (63.9) | |
| Covers nose/mouth when sneezing | 0.038 | ||
| Not at all | 10 (4.0) | 2 (0.8) | |
| Yes, sometimes | 82 (32.5) | 96 (38.1) | |
| Yes, always | 160 (63.5) | 154 (61.1) | |
| Object(s) used to cover mouth | |||
| Hand | 192 (76.2) | 228 (90.5) | < 0.001 |
| Handkerchief | 131 (52.0) | 124 (49.2) | 0.533 |
| Crook of elbow | 2 (0.8) | 17 (6.7) | < 0.001 |
| Part of clothes | 8 (3.2) | 38 (15.1) | < 0.001 |
| Ensures cross-ventilation in home | < 0.001 | ||
| Not at all | 27 (10.7) | 5 (2.0) | |
| Yes, sometimes | 62 (24.6) | 73 (29.0) | |
| Yes, always | 163 (64.7) | 174 (69.0) | |
The mean knowledge score of the respondents increased from 10.6 ± 7.0 at baseline to 16 ± 5.4 post-intervention (P < 0.001). There was also a 20.3% increase in respondents with a positive attitude and a significant increase in mean attitude score (P < 0.001). However, there was no significant difference in the overall practices in the pre- versus post-intervention comparison (Table 5).
Table 5.
Change in overall knowledge, attitude, and practice before and after intervention
| Variables | Pre-intervention (N = 252) frequency (%) | Post-intervention (N = 252) frequency (%) | P value |
|---|---|---|---|
| Overall knowledge | < 0.001 | ||
| Poor | 192 (76.2) | 128 (50.8) | |
| Good | 60 (23.8) | 124 (49.2) | |
| Mean knowledge score | 10.6 ± 7.0 | 16 ± 5.4 | < 0.001 |
| Overall attitude | < 0.001 | ||
| Negative | 68 (27.0) | 17 (6.7) | |
| Positive | 184 (73.0) | 235 (93.3) | |
| Mean attitude score | 5.8 ± 3.3 | 7.0 ± 1.8 | < 0.001 |
| Overall practice | 0.460 | ||
| Poor | 28 (11.1) | 23 (9.1) | |
| Good | 224 (88.9) | 229 (90.9) | |
| Mean practice score | 5.3 ± 1.4 | 5.4 ± 1.3 | 0.584 |
In multivariate analyses, there was a positive association between respondent age and TB knowledge (OR = 1.03, 95% CI = 1.01–1.05), and post-secondary education was associated with positive attitudes (OR = 4.99, 95% CI = 1.86–13.41) pre-intervention. None of the predictor variables were significantly associated with post-intervention outcomes (Table 6).
Table 6.
Multivariate analysis of characteristics associated with good knowledge, positive attitude, and good practice before and after intervention
| Characteristic | Pre-intervention | Post-intervention | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Good knowledge* | ||||||
| Age (years) | 1.03 | 1.01–1.05 | 0.008 | 0.99 | 0.97–1.02 | 0.555 |
| Sex | ||||||
| Female | Reference | Reference | ||||
| Male | 1.11 | 0.60–2.05 | 0.735 | 1.01 | 0.61–1.69 | 0.964 |
| Education | ||||||
| More than post-secondary | Reference | Reference | ||||
| Post-secondary | 1.12 | 0.54–2.30 | 0.767 | 0.87 | 0.44–1.74 | 0.697 |
| Employment status | ||||||
| Unemployed | Reference | Reference | ||||
| Employed | 0.76 | 0.36–1.64 | 0.488 | 0.84 | 0.42–1.67 | 0.614 |
| Occupation | ||||||
| Non-professional | Reference | Reference | ||||
| Professional | 1.45 | 0.69–3.03 | 0.327 | 0.93 | 0.51–1.69 | 0.813 |
| Positive attitude† | ||||||
| Age (years) | 1.01 | 0.99–1.04 | 0.225 | 1.02 | 0.96–1.07 | 0.590 |
| Sex | ||||||
| Female | Reference | Reference | ||||
| Male | 1.24 | 0.68–2.28 | 0.487 | 1.13 | 0.40–3.23 | 0.819 |
| Education | ||||||
| More than post-secondary | Reference | Reference | ||||
| Post-secondary | 4.99 | 1.86–13.41 | 0.001 | 3.83 | 0.48–30.32 | 0.204 |
| Employment status | ||||||
| Unemployed | Reference | Reference | ||||
| Employed | 1.48 | 0.72–3.01 | 0.285 | 1.53 | 0.40–5.82 | 0.534 |
| Occupation | ||||||
| Non-professional | Reference | Reference | ||||
| Professional | 1.48 | 0.68–3.24 | 0.329 | 0.58 | 0.18–1.90 | 0.367 |
| Good practice‡ | ||||||
| Age (years) | 0.99 | 0.96–1.02 | 0.535 | 1.01 | 0.96–1.05 | 0.812 |
| Sex | ||||||
| Female | Reference | Reference | ||||
| Male | 0.69 | 0.31–1.55 | 0.370 | 1.33 | 0.53–3.34 | 0.551 |
| Education | ||||||
| More than post-secondary | Reference | Reference | ||||
| Post-secondary | 0.96 | 0.35–2.58 | 0.928 | 1.34 | 0.41–4.31 | 0.629 |
| Employment status | ||||||
| Unemployed | Reference | Reference | ||||
| Employed | 1.05 | 0.40–2.76 | 0.921 | 3.36 | 0.93–12.1 | 0.063 |
| Occupation | ||||||
| Non-professional | Reference | Reference | ||||
| Professional | 1.83 | 0.61–5.51 | 0.283 | 0.20 | 0.06–0.62 | 0.005 |
Poor knowledge.
Negative attitude.
Poor practice.
Clinic records showed that 8 of 12 referred TB suspects came to the DOTS clinic in LUTH during the intervention phase (6 were male, and 2 were female). One was positive for sputum acid-fast bacilli, whereas the others were negative.
Discussion
As part of community-based TB care, communication and social mobilization organized by community members are known to be the most effective tools for addressing wrong beliefs and stigma.20 Community members in the developing world have indicated their acceptability of CVs in TB control,21 and their contribution to treatment has also been shown to be effective.13 Some previous studies showed improved knowledge using other interventional strategies among housewives after mass media campaigns22 and immigrants and refugees after exposure to an educational video.23 Also, health workers' TB knowledge improved and stigma was eliminated after a training workshop.24 However, no prior studies have evaluated knowledge gains after using CVs to communicate TB information. This study showed that using CVs as health educators improved overall knowledge of and attitude toward TB. The specific knowledge increases in understanding of the cause, modes of transmission, and prevention of TB; knowledge of the signs and symptoms of TB; and awareness of a facility offering free TB services were particularly encouraging; this is an important finding, because increased knowledge reduces diagnostic delays among people at risk and those around them.25 Some of the improvement in attitude was also related to a more positive disposition to proper health-seeking behavior in the event of acquiring TB (Table 3).
Some misconceptions persisted among the study participants post-intervention. For example, there was persistence in the belief that TB is caused by cold air. Also, post-intervention respondents still believed that TB could be transmitted through sharing eating utensils. Such misconceptions about the cause and transmission of TB have been reported in previous studies.16,17,21,26 The misconception that only adults could be affected by TB increased significantly (Figure 1), and the implication of this is that childhood symptoms of TB could be ignored, therefore delaying case detection and care among this group, which remains the most vulnerable to the disease.27
Use of herbal remedies and prayer were mentioned by people as a cure for TB; cultural and spiritual dispositions of people can influence health decisions,28,29 and these obviously persisted, despite the intervention. Although a high proportion of the respondents (82.5%) knew that special drugs are given to cure TB in health facilities, the term DOTS was mentioned by just 2.8% of respondents after the intervention. It is recommended that future community interventions should place emphasis on the directly observed nature of TB treatment and the inability of herbal remedies to cure TB.
Misconceived ideas regarding causes, signs, and/or treatments for TB have the potential to create the foundation for increased stigmatization of TB patients and subsequently, decrease the TB case detection rate.26 A reason for increased misconceptions could be because of the fact that CVs, who are not trained health workers, received a large amount of new knowledge themselves during the 2-day training and may not have fully understood the cause, transmission, signs, and cure of TB. These unexpected findings underscore the need for multiple training sessions with CVs in future programs and interventions.
Despite the gains in overall knowledge and attitude from this intervention, the seriousness of the burden of TB in Nigeria was not better appreciated in the community possibly because more than one-half of the respondents did not know anyone with TB. Rather, the stigmatizing attitude actually worsened with increases in proportions of respondents with negative attitudes toward people with TB (Figure 1). The persistence of misconceptions in the community could be responsible for the stigma, which has been highlighted in another developing country.30 There is also the possibility that the CVs who gave unsupervised health talks passed on partial information to community members. This coupled with the brevity of messages on educational pamphlets and posters used for health education may not satisfactorily influence the alleviation of stigma. Another important consideration is the varying cultures within the community, which has a mix of ethnic groups, and this has been found to have an influence on stigma.31 It may have helped if all the ethnic tribes were represented among the CVs chosen by the CDA, but this was not the case; they were all from the Yoruba ethnic group, which is the most populous in the community (Table 1). Future intervention studies aimed at reducing stigma will need to consider such cultural variations.
The intervention improved the practice of ensuring cross-ventilation in homes; this practice is bound to reduce TB transmission risk in the community.32 However, it did not improve the practice of appropriately covering of the mouth when coughing, and a higher proportion of people reported the use of hands to cover their mouths instead of the more appropriate handkerchief/tissue or in the absence of that, the crook of the elbow post- versus pre-intervention. Although a recent observational cough etiquette study did not find these commonly publicized respiratory hygiene methods to satisfactorily block droplets that result in transmission of respiratory diseases, like TB,33 they are still widely advocated by national and international health organizations34,35 and may remain principal means of prevention of airborne diseases in poorer communities, like Idi Araba. Emphasis should, thus, be placed on encouraging these practices in future community intervention studies.
This study had some limitations. First, we did not assess baseline numbers of persons in the community attending clinics with suspected TB; therefore, we could not satisfactorily measure the effect of the intervention on the yield of TB suspects in this study, and this narrowed the scope of the study. Moreover, previous studies assessing TB case detection had much longer intervention timeframes that extended into several years.9–11 Second, this study used self-reported means to determine preventive practices, which are subject to respondents' desire to provide socially desirable answers. Third, the level of exposure to the community intervention for each of the post-intervention respondents was not ascertained objectively; therefore, knowledge change vis-à-vis level of exposure could not be assessed.
In summary, the use of trained CVs to share information on TB improved the overall knowledge and attitudes of respondents. Continued empowerment of the community should be encouraged to promote sustainable TB prevention and care. Role model educators can be used in the community to promote proper preventive practices. Additional analytic and intervention studies that compare the effectiveness of the use of CVs and other methods in improving community knowledge as well as cost-effective analyses are recommended to guide future policies and programs on TB control.
ACKNOWLEDGMENTS
The authors express their appreciation to the study participants and community of Idi Araba, who graciously provided their time to provide us with important information on the impact of the intervention program. The authors are also indebted to Mojisola Odupitan, Omotanwa Assu, Ayoade Shobowale, Rilwan Muhammed, Oluwaseun Shabi, Ahmed Akinola, Funmilayo Olayinka, Omolara Iginla, Oluwaseyi Akande, and Mariam Bello for their efforts as community volunteers. The authors are grateful to Olufunmilayo Oke, the Tuberculosis and Leprosy Control Officer for the Mushin local government area, for her support during community entry and training of community volunteers.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations.
Footnotes
Financial support: The project described was supported by the Medical Education Partnership Initiative in Nigeria (MEPIN) funded by the Fogarty International Center, the Office of AIDS Research, and the National Human Genome Research Institute of the National Institute of Health; the Health Resources and Services Administration (HRSA); and Office of the US Global AIDS Coordinator Award R24TW008878.
Authors' addresses: Mobolanle Balogun, Adekemi Sekoni, Oluwakemi Odukoya, and Adebayo Onajole, Department of Community Health and Primary Care, College of Medicine of the University of Lagos, Lagos, Nigeria, E-mails: mbalogun@cmul.edu.ng, aosekoni@cmul.edu.ng, drolukemiodukoya@yahoo.com, and aonajole@cmul.edu.ng. Seema Thakore Meloni and Phyllis J. Kanki, Department of Immunology and Infectious Diseases, Harvard School of Public Health, Boston, MA, E-mails: sthakore@hsph.harvard.edu and pkanki@hsph.harvard.edu. Olukemi Longe-Peters, Department of Community Health, Lagos University Teaching Hospital, Lagos, Nigeria, E-mail: peterskemi@yahoo.com. Folasade Ogunsola, Department of Medical Microbiology and Parasitology, College of Medicine of the University of Lagos, Lagos, Nigeria, E-mail: sade.ogunsola@gmail.com.
References
- 1.World Health Organization Global Tuberculosis Report. 2013. www.who.int/tb/data Available at. Accessed February 20, 2014.
- 2.World Health Organization Global Tuberculosis Control Report 2009: Country Profile for Nigeria. 2009. www.who.int/tb/data Available at. Accessed February 20, 2014.
- 3.World Health Organization Countdown to 2015, Global Tuberculosis Report 2013 Supplement. 2013. www.who.int/tb/data Available at. Accessed February 20, 2014.
- 4.Maher D. The role of the community in the control of tuberculosis. Tuberculosis (Edinb) 2003;83:177–182. doi: 10.1016/s1472-9792(02)00066-5. [DOI] [PubMed] [Google Scholar]
- 5.Hadley M, Maher D. Community involvement in tuberculosis control lessons from other health care programmes. Int J Tuberc Lung Dis. 2000;4:401–408. [PubMed] [Google Scholar]
- 6.World Health Organization Community TB Care in Africa: Report on a “Lessons Learned” Meeting in Harare, Zimbabwe, 27–29 September 2000 (WHO/CDS/TB/2001.291) 2001. www.who.int/tb/people_and_communities/commcare Available at. Accessed November 5, 2013.
- 7.Castro KG, LoBue P. Bridging implementation, knowledge, and ambition gaps to eliminate tuberculosis in the United States and globally. Emerg Infect Dis. 2011;17:337–342. doi: 10.3201/eid1703.110031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Engage-TB: Integrating Community-Based Tuberculosis Activities into the Work of Nongovernmental and Other Civil Society Organizations: Operational Guidance. 2012. www.who.int/tb/people_and_communities/en/ Available at. Accessed September 30, 2014.
- 9.Islam S, Harries AD, Malhotrad S, Zaman K, Husain A, Islam A, Ahmed F. Training of community healthcare providers and TB case detection in Bangladesh. Int Health. 2013;5:223–227. doi: 10.1093/inthealth/iht012. [DOI] [PubMed] [Google Scholar]
- 10.Lorent N, Choun K, Thai S, Kim T, Huy S, Pe R. Community-based active tuberculosis case finding in poor urban settlements of Phnom Penh, Cambodia: a feasible and effective strategy. PLoS ONE. 2014;9:e92754. doi: 10.1371/journal.pone.0092754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delai MY, Gounder S, Tayler-Smith K, Van den Bergh R, Harries AD. Relationship between education and training activities and tuberculosis case detection in Fiji, 2008–2011. Public Health Action. 2012;2:142–144. doi: 10.5588/pha.12.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barker RD, Millard FJC, Nthangeni ME. Unpaid community volunteers - effective providers of directly observed therapy (DOT) in rural South Africa. S Afr Med J. 2002;92:291–294. [PubMed] [Google Scholar]
- 13.Singh AA, Parasher D, Shekhavat GS, Sahu S, Wares DF, Granich R. Effectiveness of urban community volunteers in directly observed treatment of tuberculosis patients: a field report from Haryana, North India. Int J Tuberc Lung Dis. 2004;8:800–802. [PubMed] [Google Scholar]
- 14.Federal Ministry of Health Nigeria . National Tuberculosis and Leprosy Control Program Module for Training of Community Volunteers on Tuberculosis Control. Abuja, Nigeria: Federal Ministry of Health; 2011. [Google Scholar]
- 15.Federal Ministry of Health Nigeria . National Tuberculosis and Leprosy Control Programme 2012 Annual Report. Abuja, Nigeria: Federal Ministry of Health; 2013. [Google Scholar]
- 16.Anochie PI, Onyeneke EC, Onyeozirilla AC, Igbolekwu LC, Onyeneke BC, Ogu AC. Evaluation of public awareness and attitude to pulmonary tuberculosis in a Nigerian rural community. Germs. 2013;3:52–62. doi: 10.11599/germs.2013.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tobin EA, Okojie P-W, Isah EC. Community knowledge and attitude to pulmonary tuberculosis in rural Edo state, Nigeria. Ann Afr Med. 2013;12:148–154. doi: 10.4103/1596-3519.117623. [DOI] [PubMed] [Google Scholar]
- 18.Prabhakara GN. Biostatistics. New Delhi, India: Jaypee Brothers Medical; Publishers Ltd; 2006. pp. 110–119. [Google Scholar]
- 19.World Health Organization . Advocacy, Communication and Social Mobilization for TB Control: A Guide to Developing Knowledge, Attitude and Practice Surveys (WHO/HTM/STB/2008.46) Geneva: World Health Organization; 2008. [Google Scholar]
- 20.CORE Group TB Working Group . Community-Based Tuberculosis Prevention and Care: Why—and How—to Get Involved. An International Handbook for Nongovernmental Organizations and Civil Society Organizations. Washington, DC: CORE Group; 2013. [Google Scholar]
- 21.Mesfin MM, Tasew TW, Tareke IG, Mulugeta GWM, Richard MJ. Community knowledge, attitudes and practices on pulmonary tuberculosis and their choice of treatment supervisor in Tigray, northern Ethiopia. Ethiop J Health Dev. 2005;19:21–27. [Google Scholar]
- 22.Sharma AK, Sharma R. Impact of mass media on knowledge about tuberculosis control among homemakers in Delhi. Int J Tuberc Lung Dis. 2007;11:893–897. [PubMed] [Google Scholar]
- 23.Wieland ML, Nelson J, Palmer T, O'Hara C, Weis JA, Nigron JA, Sia IG. Evaluation of a tuberculosis education video among immigrants and refugees at an adult education center: a community-based participatory approach. J Health Commun. 2013;18:343–353. doi: 10.1080/10810730.2012.727952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu PS, Chou P, Chang NT, Sun WJ, Kuo HS. Assessment of changes in knowledge and stigmatization following tuberculosis training workshops in Taiwan. J Formos Med Assoc. 2009;108:377–385. doi: 10.1016/S0929-6646(09)60081-4. [DOI] [PubMed] [Google Scholar]
- 25.Roy A, Ibrahim A, Yates S, Chapman A, Lipman M, Monk P, Catchpole M. Evaluating knowledge gain from TB leaflets for prison and homeless sector staff: the National Knowledge Service TB pilot. Eur J Public Health. 2008;18:600–603. doi: 10.1093/eurpub/ckn096. [DOI] [PubMed] [Google Scholar]
- 26.Esmael A, Ali I, Agonafir M, Desale A, Yaregal Z, Desta K. Assessment of patients' knowledge, attitude, and practice regarding pulmonary tuberculosis in eastern Amhara regional state, Ethiopia: cross-sectional study. Am J Trop Med Hyg. 2013;88:758–788. doi: 10.4269/ajtmh.12-0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brent AJ. Childhood TB surveillance: bridging the knowledge gap to inform policy. J Trop Med. 2012;2012(865436) doi: 10.1155/2012/865436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mandell DS, Novak M. The role of culture in families' treatment decisions for children with autism spectrum disorders. Ment Retard Dev Disabil Res Rev. 2005;11:110–115. doi: 10.1002/mrdd.20061. [DOI] [PubMed] [Google Scholar]
- 29.Sulmasy DP. Spirituality, religion, and clinical care. Chest. 2009;135:1634–1642. doi: 10.1378/chest.08-2241. [DOI] [PubMed] [Google Scholar]
- 30.Matthew AS, Takalkar AM. Living with tuberculosis: the myths and the stigma from the Indian perspective. Clin Infect Dis. 2007;45:1247. doi: 10.1086/522312. [DOI] [PubMed] [Google Scholar]
- 31.Chang S-H, Cataldo JK. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. Int J Tuberc Lung Dis. 2014;18:168–173. doi: 10.5588/ijtld.13.0181. [DOI] [PubMed] [Google Scholar]
- 32.Lygizos M, Shenoi SV, Brooks RP, Bhushan A, Brust JCM, Zelterman D, Deng Y, Northrup V, Moll AP, Friedland GH. Natural ventilation reduces high TB transmission risk in traditional homes in rural KwaZulu-Natal, South Africa. BMC Infect Dis. 2013;13:300. doi: 10.1186/1471-2334-13-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zayas G, Chiang MC, Wong E, MacDonald F, Lange CF, Senthilselvan A, King M. Effectiveness of cough etiquette maneuvers in disrupting the chain of transmission of infectious respiratory diseases. BMC Public Health. 2013;13:811. doi: 10.1186/1471-2458-13-811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Center for Disease Control and Prevention . Draft Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC). Respiratory Hygiene/Cough Etiquette in Health Care Settings. Atlanta, GA: Center for Disease Control and Prevention; 2009. [Google Scholar]
- 35.World Health Organization . Interim Guidelines: Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Diseases in Health Care. Geneva: World Health Organization; 2007. [PubMed] [Google Scholar]