Abstract
Objective
Less-than-annual cervical cancer screening is now recommended for most US women, raising questions about the need for routine annual bimanual pelvic examinations. Little is known about clinicians’ bimanual pelvic examination practices, their beliefs about its importance or the reasoning underlying its performance in asymptomatic women.
Study Design
We conducted a nationwide survey of US obstetrician-gynecologists. Respondents (n=521) reported their examination practices and beliefs based on vignettes for asymptomatic women across the lifespan.
Results
Nearly all obstetrician-gynecologists perform bimanual pelvic examinations in asymptomatic women across the lifespan, although it is viewed as less important for a newly sexually active 18-year-old. Reasons cited as very important included adherence to standard medical practices (45%), patient reassurance (49%), detection of ovarian cancer (47%) and identification of benign uterine (59%) and ovarian conditions (54%).
Conclusions
Obstetrician-gynecologists perform bimanual pelvic examinations in the vast majority of asymptomatic women, but the importance placed on the examinations and reasons for conducting them vary.
Keywords: bimanual pelvic examination, clinical practice, cancer screening, provider views
Introduction
Recent recommendations by the American Cancer Society and the US Preventive Services Task Force endorse less-than-annual cervical cancer screening for most women in the United States. Subsequently, the need for annual bimanual pelvic examinations among asymptomatic women has been questioned.1 The Institute of Medicine report on Clinical Preventive Services for Women include annual well-woman visits,2 but whether or not these visits should include a routine bimanual pelvic examination has not been established. In August 2012, the American Congress of Obstetricians and Gynecologists (ACOG) issued a Committee Opinion on well-woman visits and reaffirmed its recommendation that pelvic examinations, including bimanual examination, be included in the annual assessment for women aged 21 years and older.3
Despite its prominent position in well-woman care, little is known about the clinical circumstances under which clinicians perform bimanual pelvic examinations, the reasons these examinations are being performed and the importance clinicians place on them. To address these uncertainties, we surveyed a random sample of practicing obstetrician-gynecologists to obtain estimates on their practices and beliefs regarding bimanual pelvic examinations in asymptomatic women.
Materials and Methods
Sample
A national probability sample of obstetrician-gynecologists currently working in the United States was drawn from the American Medical Association’s (AMA) Physician Masterfile, a comprehensive database of nearly one million physicians that includes both members and non-members of the AMA and is updated weekly. A sample of at least 500 eligible respondents was targeted to achieve population estimates with at least ± 5% precision. A simple random sample of 1,020 practicing gynecologists (i.e., not retired, not in residency, currently providing patient care, specializing in obstetrics and gynecology or gynecology alone) was drawn using a random number generator. The response rate was calculated using a standard formula in which ineligible clinicians were subtracted and adjustments made for an estimated proportion of eligible participants among unknown respondents.4
Data collection and measurement
Clinicians were sent a letter introducing the study, followed 10 days later by a survey and cover letter, postage-paid return envelope and $10 in cash. A reminder postcard was mailed one week later. A second cover letter, copy of the survey and postage-paid return envelope was sent two weeks after the postcard if the original survey had not yet been returned. If mail was returned as undeliverable, research staff used online state medical boards, directories, and search engines to locate current information and confirm a correct mailing address. After the final mailing, recruitment efforts were continued by telephone. Data were collected from May 2010 through January 2011. The Committee on Human Research at the University of California, San Francisco approved the study protocol.
Outcome variables
Clinicians were asked to indicate whether they would conduct a bimanual examination (with or without rectal examination) in patient vignettes of women aged 18, 35, 55, and 70 years (Table 1). Their characteristics were defined such that, according to current (at the time of survey) guidelines, they were not in need of a Pap test at the visit.5 The vignettes are described in Table 1. For each, clinicians were asked about a number of components of gynecological examination, and then asked about their importance, rated with four response categories: very important, moderately important, a little important, and not important. The clinical services listed were: a) Pap test, b) HPV test, c) visual inspection of the external genitalia, d) speculum examination, e) bimanual pelvic examination without rectal examination and, f) bimanual pelvic examination with rectal examination. We created an outcome variable to compare those clinicians who would conduct bimanual pelvic examination (with or without rectal examination) for the patient vignette and considered it very important, compared to all other responses.
Table 1.
Patient vignettes1
| Patient 1 | An 18-year-old woman presents to you for a routine health visit. She became sexually active one month ago. She has no history of dysplasia, is not immuno-compromised, has no symptoms, and is not pregnant. |
| Patient 2 | A 35-year-old woman with no new sexual partners in the last 5 years presents for a routine health visit. She has had 3 consecutive normal annual Pap tests with you, the last of which was one year ago. She has no history of dysplasia, is not immuno-compromised, has no symptoms, and is not pregnant. |
| Patient 3 | A 55-year-old woman presents to you for a routine health visit. Her cervix and ovaries were removed last year at the time of hysterectomy for symptomatic fibroids. She has no history of dysplasia, is not immuno-compromised, and has no symptoms. |
| Patient 4 | A healthy 70-year-old woman presents to you for a routine health visit. She has had annual Pap tests with normal findings for the past 30 years. She has not been sexually active for the last 10 years. She has no history of dysplasia, is not immuno-compromised, and has no symptoms. |
For each vignette, respondents were instructed, “For this patient, please indicate whether you would perform each of the following.” And, “For this patient, please indicate your opinion about the importance of each of the following.” The clinical services listed were: a) Pap test, b) HPV test, c) visual inspection of the external genitalia, d) speculum examination, e) bimanual pelvic examination without rectal examination and, f) bimanual pelvic examination with rectal examination.
Clinicians also were asked to rate potential reasons for conducting bimanual pelvic examinations for asymptomatic women using the same 4-point importance response scale to answer the question: “In your opinion, how important is the bimanual pelvic examination in women without symptoms?” Its importance for detection of ovarian cancer, uterine cancer, cervical cancer, subclinical pelvic inflammatory disease, benign uterine or ovarian conditions, uterine position, adherence to standard medical practice, and non-clinical reasons such as accommodating patient expectations, reassuring patients of their health and ensuring adequate compensation was measured. The questions were designed to evaluate general reasoning underlying the performance of these exams and were not related specifically to the vignettes.
Provider characteristics
Measures of the characteristics of clinicians included age, gender, and race/ethnicity. The practice setting was measured with an item that permitted multiple responses; these were coded hierarchically as follows: university-based, solo or stand-alone practice, group practice, and hospital-based or other (community or family planning clinic, locum tenums, health-maintenance organization). Additional measures describing the practice setting include clinic volume, the proportion of patients having public health insurance (e.g., Medicaid, Medicare), region of the country, and whether the practice was in a metropolitan area, according to zip-code based Rural-Urban Commuting Area codes.
Analysis
Comparisons for categorical variables were conducted with Fisher’s Exact tests. Adjusted odds ratios and 95% confidence intervals from multivariable logistic regression models examining the independent associations of provider characteristics with reasons for conducting the examination for asymptomatic women were computed. Variables relevant to clinical practices were included in the model, and parsimony was achieved by excluding some variables that were not significant in bivariate models (e.g., race/ethnicity, teaching hospital admitting privileges, urban location, proportion of patients low-income). All analyses were conducted with STATA statistical software version 11.1 (Stata Corp, College Station, TX).
Results
Of 1,020 surveys mailed, eligibility could be determined for 716. Of these, 590 were eligible, 63 declined participation and 6 submitted incomplete surveys. Assuming a similar proportion of eligible respondents among the unknowns (82%), 250 eligible respondents were added to the denominator for the response rate calculation (590+250). The survey response rate, therefore, was 62%, with 521 eligible respondents. Respondents were no different than non-respondents by region of the country, urban location, or gender, but were younger (34% of non-respondents age 60 or older versus 23% of respondents). Ninety percent of respondents were members of the American College of Obstetricians and Gynecologists. Seventy percent of physicians performed over 30 gynecological exams per week and the mean number of gynecologic patients per week was 85 (Table 2).
Table 2.
Demographic and practice characteristics of sample (n=521)
| Characteristic | % (n) |
|---|---|
| Gender: | |
| Male | 54.7 (285) |
| Female | 45.3 (236) |
| Age: | |
| 30–39 | 20.0 (104) |
| 40–49 | 31.1 (162) |
| 50–59 | 27.1 (141) |
| 60+ | 21.9 (114) |
| Race/ethnicity: | |
| White, non-Hispanic | 74.0 (376) |
| Black, non-Hispanic | 7.5 (38) |
| Hispanic/Latino | 8.3 (42) |
| Other | 10.2 (52) |
| Region of country: | |
| West | 25.1 (131) |
| Midwest | 22.3 (116) |
| South | 30.9 (161) |
| Northeast | 21.7 (113) |
| Urban location | 86.4 (449) |
| Member of ACOGa | 89.6 (466) |
| Specialty: | |
| Obstetrician-Gynecologist | 81.2 (422) |
| Gynecologist only | 18.9 (98) |
| Number of gynecologic exams per week: | |
| <30 | 30.6 (159) |
| 30+ | 69.4 (361) |
| Mean number of patients per week (SD) | 85.2 (46.6) |
| Proportion of patients using public insurance: | |
| < 25% | 49.9 (259) |
| 25–50% | 32.4 (168) |
| More than 50% | 17.7 (92) |
| Proportion of patients low-income: | |
| < 25% | 54.6 (283) |
| 25–50% | 28.2 (146) |
| More than 50% | 17.2 (89) |
| Practice setting: | |
| Solo or stand-alone | 24.6 (128) |
| Group | 42.2 (219) |
| University-based | 11.0 (57) |
| Hospital-based, community, family planning clinic, or other | 23.3 (116) |
| Admitting privileges at a teaching hospital | 55.7 (289) |
American College of Obstetricians and Gynecologists
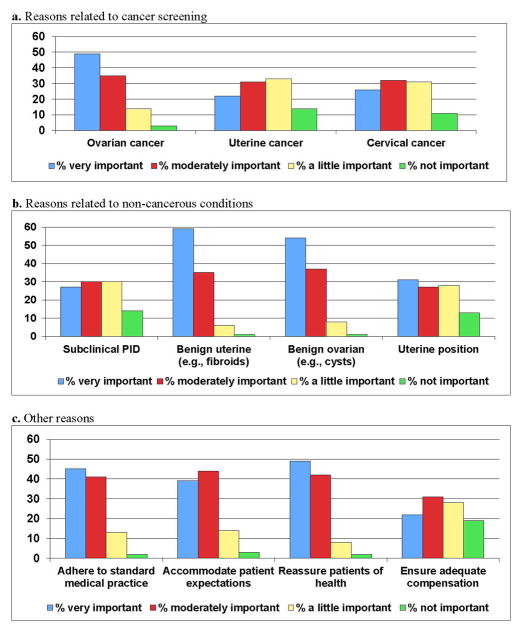
Nearly all obstetrician-gynecologists would conduct bimanual pelvic examinations in routine visits with asymptomatic women across the lifespan for the vignettes presented (Figure 1). Nearly all respondents indicated that they would perform the examination in the 55-year-old despite the absence of her ovaries, uterus and cervix, and over half believed it to be very important for this woman. The proportion believing the examination to be very important varied by age: about one-third (36%) viewed the examination as very important for the 18-year-old compared with 69% believing the same for the 70-year-old. For the 18-year-old patient, older physicians were significantly more likely to place high importance on the examination than younger physicians (data not shown). Respondents practicing in the Northeast and the South were more likely than those in the West to consider the examination very important for each of the patients (Table 3). Clinicians in solo practice were also more likely to place high importance on the examination.
Figure 1.
Clinicians who would perform bimanual pelvic examination and consider it very important, by vignette
Table 3.
Characteristics associated with reasons for considering bimanual examination purposes very important in asymptomatic women, multivariable logistic regression
| Provider characteristics | Identify cancers of the ovaries OR (95% CI) | Detect benign uterine conditions OR (95% CI) | Reassure patients of their health OR (95% CI) | Accommodate patient expectations OR (95% CI) | Ensure adequate compensation OR (95% CI) |
|---|---|---|---|---|---|
|
| |||||
| Age | |||||
| 30–39 | REF | REF | REF | REF | REF |
| 40–49 | 0.6 (0.3, 1.0) | 0.7 (0.4, 1.2) | 1.0 (0.6, 1.7) | 1.0 (0.6, 1.7) | 0.9 (0.5, 1.6) |
| 40–59 | 1.2 (0.6, 2.0) | 1.0 (0.5, 1.7) | 1.2 (0.7, 2.2) | 1.3 (0.7, 2.3) | 0.7 (0.4, 1.4) |
| 60+ | 1.3 (0.7, 2.5) | 1.0 (0.5, 1.9) | 1.4 (0.8, 2.7) | 1.5 (0.8, 2.8) | 0.7 (0.3, 1.6) |
| Female gender | 1.1 (0.7, 1.6) | 0.9 (0.6, 1.3) | 0.7 (0.5, 1.1) | 0.8 (0.5, 1.2) | 0.6 (0.4, 1.0) |
| Region: | |||||
| West | REF | REF | REF | REF | REF |
| Midwest | 1.1 (0.7, 1.9) | 1.1 (0.7, 1.9) | 1.5 (0.9, 2.6) | 1.5 (0.9, 2.6) | 1.4 (0.7, 2.8) |
| South | 0.9 (0.6, 1.5) | 1.1 (0.7, 1.8) | 1.9 (1.2, 3.1)* | 1.5 (0.9, 2.4) | 1.9 (1.0, 3.5)* |
| Northeast | 1.4 (0.8, 2.4) | 1.5 (0.9, 2.5) | 2.3 (1.3, 4.0)** | 1.8 (1.1, 3.2)* | 1.8 (0.9, 3.4) |
| Clinical setting: | |||||
| Solo practice | REF | REF | REF | REF | REF |
| Group practice | 0.6 (0.4, 1.0)* | 0.6 (0.4, 1.0)* | 0.4 (0.3, 0.7)** | 0.8 (0.5, 1.3) | 0.7 (0.4, 1.2) |
| University-based | 0.4 (0.2, 0.7)** | 0.4 (0.2, 0.7)** | 0.3 (0.1, 0.5)*** | 0.8 (0.4, 1.7) | 0.9 (0.4, 2.0) |
| Hospital/clinic, other | 0.4 (0.2, 0.7)** | 0.6 (0.4, 1.1) | 0.4 (0.2, 0.7)** | 0.8 (0.5, 1.4) | 0.7 (0.4, 1.4) |
| Patients with public insurance <25% | 0.8 (0.6, 1.2) | 1.1 (0.8, 1.6) | 1.0 (0.7, 1.4) | 1.5 (1.0, 2.2)* | 1.3 (0.8, 2.0) |
OR indicates odds ratio. CI indicates confidence interval.
p <.05,
p<.01,
p<.001
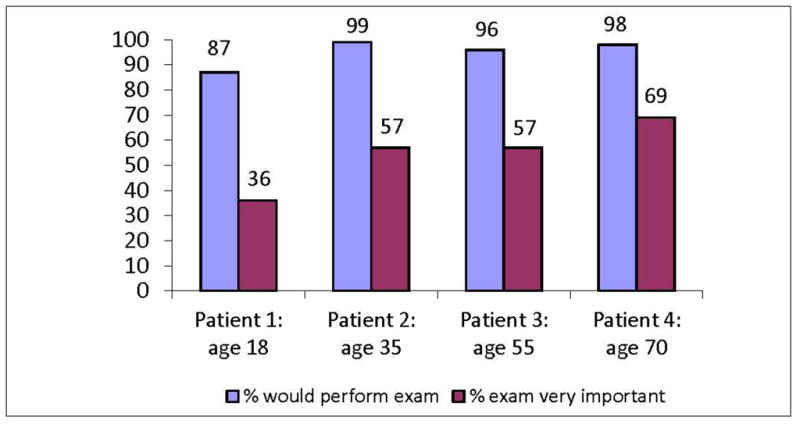
When asked to rate the importance of different reasons for conducting bimanual pelvic examinations in asymptomatic patients, the detection of ovarian cancer was a very or moderately important reason among 84% of respondents, with nearly half considering it very important (Figure 2a). The detection of benign conditions of the uterus and ovaries were the reasons considered very important by the highest proportion of respondents (Figure 2b). A high proportion of respondents also ascribed to non-clinical reasons for conducting the examination in asymptomatic patients (Figure 2c); nearly half considered it very important for reassuring patients of their health (49%). Although only 1 in 5 considered it very important for ensuring adequate compensation for routine gynecologic care, over half considered compensation a very or moderately important reason. In supplemental adjusted analyses, we found clinicians that considered bimanual pelvic examinations very important for detection of ovarian, uterine, and cervical cancer were nearly 5 times more likely to consider it very important in the 18-year-old patient vignette. Identifying benign conditions of the uterus and ovaries and reassuring patients of their health were also more strongly associated with placing high importance on the examination across all vignettes.
Figure 2.
Importance of different reasons for bimanual pelvic examinations in asymptomatic women
a. Reasons related to cancer screening
b. Reasons related to non-cancerous conditions
c. Other reasons
In multivariable analysis of predictors of different reasons for bimanual pelvic examinations for asymptomatic women, clinicians practicing in the Northeast and serving patient populations with fewer publicly insured patients were more likely to consider accommodation of patient expectations a very important reason (Table 3). Clinicians in the Northeast and South, and those in solo practice were most likely to indicate that bimanual pelvic examinations are important for reassuring patients of their health. The only covariate associated with placing high importance on the examination for detection of ovarian cancer and for benign conditions was whether clinicians were in a solo practice versus some other practice setting. Model fit was adequate in all multivariable analyses according to the log-likelihood ratios.
Comment
The vast majority of practicing obstetrician-gynecologists surveyed would perform bimanual pelvic examinations in asymptomatic women, regardless of clinical scenario, but their beliefs about the importance of the examinations and reasons for conducting them varied. Our study is novel in that it was designed to provide national estimates of the proportion of obstetrician-gynecologists that perform bimanual pelvic examinations for healthy women across the lifespan. Unlike prior studies exploring only the purposes of pelvic examinations using a web-based survey,6,7 we constructed clinical vignettes to define more specifically the circumstances under which bimanual examinations are being performed. Further, we clearly defined and focused on the bimanual pelvic examination to avoid confusion with other components of the pelvic examination, including the speculum examination and visual inspection of the external genitalia. These other aspects of pelvic examination also deserve study, as their clinical importance and provider perceived value may differ from our findings for the bimanual examination. The recent ACOG Committee Opinion by the Committee on Gynecologic Practice details clinical aspects of a contemporary well-woman visit, defines the elements of pelvic examination, and gives guidance as to who should receive the examinations. The College recommends annual pelvic examinations in all women aged 21 and older, stating that “no evidence supports or refutes” performance of the examination in asymptomatic, low-risk women; the reasoning behind performance of the examination is not defined.3 The recommendations clarify that the pelvic examination is not a routine part of the annual assessment in asymptomatic females younger than age 21 years. The vast majority of respondents to our survey (87%) would perform a bimanual examination in an asymptomatic 18-year-old, suggesting a need to educate clinicians about the appropriateness of pelvic examinations for young women. Of note, nearly all of the clinicians in our study would routinely perform the examination in an asymptomatic 55-year-old woman who has had a total hysterectomy and bilateral oophorectomy and no risk factors that would warrant continued cervical cancer screening; such women would be candidates to end cervical screening under current guidelines, suggesting a future need to educate clinicians about the appropriateness of offering discontinuation of pelvic examinations to some women. It is notable that clinicians believed that the examination gains importance as women age, with 69% believing it to be “very important” in a 70-year-old whose history suggests cervical cancer screening can end. For older patients, ACOG guidelines allow for discontinuation of routine pelvic examinations “if the patient would not intervene on detected conditions”, although these conditions are not specified.
That most clinicians considered the bimanual pelvic examination very important for identifying benign uterine conditions was of note, given that the value of identifying lesions such as uterine leiomyomata in asymptomatic women is unclear. Some survey respondents may have considered the detection of benign ovarian masses useful to avoid future surgical emergencies such as torsion and rupture; evidence derived from clinical studies concerning the utility of the examination in detecting these conditions and averting adverse health outcomes would be useful.
Our finding that characteristics of the clinical practice setting, including geographical location, were independently related to the degree of importance placed on the bimanual pelvic examination for different patients and purposes was notable. Regional differences in practices related to cancer screening have been found in other studies, with clinicians practicing in the West less likely to conduct unnecessary tests.8,9 Clinicians in solo practice were more likely to consider the examination very important, highlighting the importance of health system factors on provider practice patterns and attitudes. Nearly half of the gynecologists placed high importance on the bimanual examination for reassuring women of their health. Studies examining whether women share this perspective are needed. Prior studies on cervical cancer screening preferences suggest that some women place importance on the examination even if it is not effective for cancer screening,10,11 but others may prefer not to undergo the examination, especially if it could lead to unnecessary intervention or interfere with access to contraception.8,12–14
Our study has both strengths and limitations. We were able to achieve a relatively high response rate for a physician survey and had little evidence for meaningfully differences between responders and non-responders in most demographic variables assessed. Respondents, however, were somewhat younger than non-respondents, so our findings may underestimate the proportions conducting and placing a high level of importance on bimanual pelvic examinations for the vignettes. Data from this survey is subject to measurement bias, such as social desirability, when clinicians believe certain responses more acceptable or consistent with their professional identity (e.g., not linking clinical practices to concerns about compensation). In addition, the responses to our survey are not direct measures of clinical practice; studies relying on mailed surveys of clinicians, however, have been successfully employed to learn about knowledge, attitudes and practices regarding a range of preventive practices, with survey techniques and response rates similar to ours.15–17 Patient vignettes have been validated for accurately measuring provider practices when compared to chart review and standardized patients for a variety of health conditions.18,19
The belief among obstetrician-gynecologists that the bimanual pelvic examination is important for detecting ovarian cancer is consistent with findings by others6,7 and is noteworthy given that ovarian cancer screening is not recommended by ACOG. In addition, the USPSTF has consistently, and with ongoing evidence review, given ovarian cancer screening a D rating, indicating harms outweigh benefits.20 Of note, a recent, large (n=78,216) multi-centered randomized trial funded by the National Cancer Institute-- the Prostate, Lung, Colorectal and Ovarian Cancer Screening Randomized Controlled Trial-- found that transvaginal sonography and serum CA-125 are ineffective in reducing ovarian cancer mortality compared to usual care.21 Screening did, however, lead to harms from the surgical evaluation of false-positive tests. Bimanual examination of the ovaries was part of the original screening protocol but was discontinued because no cancers were detected by ovarian palpation alone, suggesting that the examination would not confer a clinically significant benefit in terms of ovarian cancer mortality. The potential harms of bimanual examination of the ovaries may include the same as those noted with sonography and CA-125: false-positive testing, additional radiological evaluation and the potential for unnecessary surgical exploration.
Our study serves as an important baseline for nationwide practices immediately prior to a time when the well-woman visit is being re-defined. Our survey calls attention to areas for practice improvement, specifically in clarifying its role in ovarian cancer screening. Further research would be useful in determining optimal ways to educate providers and patients about the appropriate use of this examination in asymptomatic woman.
Clinical Implications.
Our study serves as an important baseline for nationwide bimanual pelvic examination practices immediately prior to a time when the well-woman visit is being re-defined.
The results call attention to areas for practice improvement, specifically clarifying the role of bimanual pelvic examination in ovarian cancer screening. Further research would be useful in determining optimal ways to educate providers and patients about the appropriate use of this examination in asymptomatic woman
Acknowledgments
Funding for this study was provided by a grant from the UCSF Mt. Zion Health Foundation, Dr. Henderson’s Mentored Research Scientist Development Award in Population Research (K01HD054495), and resources from the NIH/NCRR/OD UCSF-CTSI (KL2 RR024130) program. We thank Ms. Cait Quinlivan and Ms. Lily Loew for their assistance with data collection. Dr. Henderson had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The contents of this paper do not necessarily represent the official position of the NIH or the Centers for Disease Control and Prevention.
Footnotes
Disclosure: None of the authors have a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jillian T. HENDERSON, Email: HendersonJ@obgyn.ucsf.edu.
Cynthia C. HARPER, Email: HarperC@obgyn.ucsf.edu.
Sarah GUTIN, Email: Sarah.Gutin@ucsf.edu.
Mona SARAIYA, Email: MSaraiya@cdc.gov.
Jocelyn CHAPMAN, Email: ChapmanJS@obgyn.ucsf.edu.
George F. SAWAYA, Email: SawayaG@obgyn.ucsf.edu.
References
- 1.Westhoff CL, Jones HE, Guiahi M. Do new guidelines and technology make the routine pelvic examination obsolete? J Womens Health. 2011;20(1):5–10. doi: 10.1089/jwh.2010.2349. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Clinical Preventive Services for Women. Closing the Gaps. Washington, DC: The National Academies Press; 2011. [Google Scholar]
- 3.American College of Obstetrics and Gynecology, Committee Opinion No 534. Well-woman visit. Obstet Gynecol. 2012;120(2):421–424. doi: 10.1097/AOG.0b013e3182680517. [DOI] [PubMed] [Google Scholar]
- 4.The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 7. AAPOR; 2011. [Google Scholar]
- 5.American College of Obstetrics and Gynecology, Practice Bulletin No 109. Cervical Cytology Screening. Obstet Gynecol. 2009;114(6):1409–1420. doi: 10.1097/AOG.0b013e3181c6f8a4. [DOI] [PubMed] [Google Scholar]
- 6.Stormo AR, Hawkins NA, Cooper CP, Saraiya M. The pelvic examination as a screening tool: practices of US physicians. Arch Intern Med. 2011;171(22):2053–4. doi: 10.1001/archinternmed.2011.575. [DOI] [PubMed] [Google Scholar]
- 7.Stormo AR, Cooper CP, Hawkins NA, Saraiya M. Physician characteristics and beliefs associated with use of pelvic examinations in asymptomatic women. Prev Med. 2012;54(6):415–421. doi: 10.1016/j.ypmed.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Henderson JT, Sawaya GF, Blum M, Stratton L, Harper CC. Pelvic examinations and access to oral hormonal contraception. Obstet Gynecol. 2010;116(6):1257–1264. doi: 10.1097/AOG.0b013e3181fb540f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walter LC, Bertenthal D, Lindquist K, Konety BR. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296(19):2336–2342. doi: 10.1001/jama.296.19.2336. [DOI] [PubMed] [Google Scholar]
- 10.Huang AJ, Pérez-Stable EJ, Kim SE, Wong ST, Kaplan CP, Walsh JME, et al. Preferences for human papillomavirus testing with routine cervical cancer screening in diverse older women. J Gen Intern Med. 2008;23(9):1324–9. doi: 10.1007/s11606-008-0633-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sawaya GF, Iwaoka-Scott AY, Kim S, Wong ST, Huang AJ, Washington AE, et al. Ending cervical cancer screening: attitudes and beliefs from ethnically diverse older women. Am J Obstet Gynecol. 2009;200(1):40.e1–7. doi: 10.1016/j.ajog.2008.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keirns CC, Goold SD. Patient-centered care and preference-sensitive decision making. JAMA. 2009;302(16):1805–6. 1. doi: 10.1001/jama.2009.1550. [DOI] [PubMed] [Google Scholar]
- 13.Weitlauf JC, Finney JW, Ruzek JI, Lee TT, Thrailkill A, Jones S, et al. Distress and pain during pelvic examinations: effect of sexual violence. Obstet Gynecol. 2008;112(6):1343–50. doi: 10.1097/AOG.0b013e31818e4678. [DOI] [PubMed] [Google Scholar]
- 14.Harper C, Balistreri E, Boggess J, Leon K, Darney P. Provision of hormonal contraceptives without a mandatory pelvic examination: the first stop demonstration project. Fam Plann Perspect. 2001;33(1):13–8. [PubMed] [Google Scholar]
- 15.DesRoches CM, Rao SR, Fromson JA, Birnbaum RJ, Iezzoni L, Vogeli C, et al. Physicians’ perceptions, preparedness for reporting, and experiences related to impaired and incompetent colleagues. JAMA. 2010;304(2):187–93. doi: 10.1001/jama.2010.921. [DOI] [PubMed] [Google Scholar]
- 16.Kahn JM, Asch RJ, Iwashyna TJ, Haynes K, Rubenfeld GD, Angus DC, et al. Physician attitudes toward regionalization of adult critical care: a national survey. Crit Care Med. 2009;37(7):2149–54. doi: 10.1097/CCM.0b013e3181a009d0. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence RE, Curlin FA. Physicians’ beliefs about conscience in medicine: A national survey. Acad Med. 2009;84(9):1276–1282. doi: 10.1097/ACM.0b013e3181b18dc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000;283(13):1715–22. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- 19.Peabody JW, Luck J, Glassman P, Jain S, Hansen J, Spell M, et al. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med. 2004;141(10):771–80. doi: 10.7326/0003-4819-141-10-200411160-00008. [DOI] [PubMed] [Google Scholar]
- 20.Screening for ovarian cancer: U S Preventive Services Task Force recommendation statement. Ann Fam Med. 2004;2(3):260–2. doi: 10.1370/afm.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buys SS, Partridge E, Black A, et al. Effect of screening on ovarian cancer mortality. JAMA. 2011;305(22):2295–2303. doi: 10.1001/jama.2011.766. [DOI] [PubMed] [Google Scholar]