Abstract
Background/Aims
The efficacy of surveillance for esophageal squamous cell neoplasia (ESCN) in patients with head and neck squamous cell carcinoma (HNSCC) remains controversial. Our study aimed to provide clinical data concerning the necessity of surveillance for detecting early ESCN in patients with HNSCC.
Methods
We retrospectively reviewed the data from 714 patients who were pathologically confirmed as having HNSCC (n=236 oral cavity cancers, 137 oropharyngeal cancers, 87 hypopharyngeal cancers, and 254 laryngeal cancers).
Results
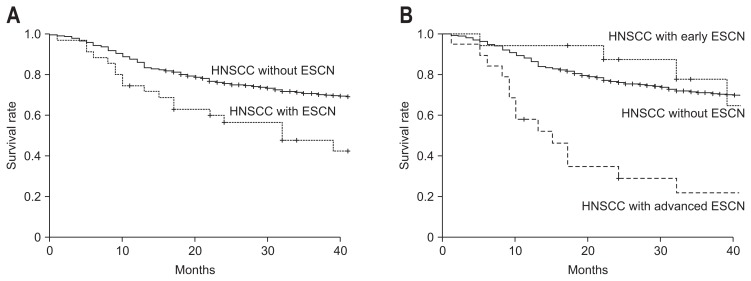
Of 714 patients, during a median follow-up of 31 months, 48 ESCNs (37 synchronous and 11 metachronous) were detected in 36 patients (5%). Fifteen synchronous lesions (40.3%) were early ESCN, whereas nine metachronous lesions (81.8%) were early ESCN. The 3-year survival rates of HNSCC only and HNSCC combined with ESCN were 71.2% and 48.2%, respectively (p<0.001). Among 36 patients with ESCN, the 3-year survival rates for early and advanced ESCN were 77.7% and 21.7%, respectively (p=0.01). In the multivariate analysis, alcohol consumption and hypopharyngeal cancer were significant factors associated with the development of ESCN.
Conclusions
HN-SCC patients with early ESCN were similar in prognosis with patients without ESCN, in contrast to patients with advanced ESCN. Therefore, surveillance for the early detection of ESCN in patients with HNSCC, especially in alcohol drinkers and those with hypopharyngeal cancer, is warranted.
Keywords: Esophageal neoplasms, Head and neck neoplasms, Early detection of cancer, Prognosis
INTRODUCTION
Patients with head and neck squamous cell carcinoma (HN-SCC) often have a second primary tumor (SPT) in their upper aerodigestive tract, most commonly in the head and neck, lung, and esophagus.1,2 It has been explained by field cancerization, whereby environmental carcinogens can induce changes in a region of mucosa that are linked with premalignant disease and that might increase the risk of epithelial cancer throughout the upper aerodigestive tract.3 The incidence of SPT in patients with HNSCC varies from 16% to 36%.4,5 The occurrence of SPT is the leading cause of mortality, accounting for one-third of HN-SCC deaths, because they are usually detected at an advanced stage.6,7
Esophageal squamous cell neoplasia (ESCN) is the most common SPT of the digestive tract in patients with HNSCC.5,8–14 Several studies report that SPT in the esophagus is the leading cause of treatment failure and death in patients with HNSCC.14,15 Among primary gastrointestinal cancers, ESCN has one of the worst prognoses: over 90% of patients are diagnosed at an advanced stage. On the other hand, the prognosis of patients with ESCN confined within the intraepithelium or mucosal layer is excellent, with 5-year survival rates of 85% to 100%.16 Therefore, early detection of ESCN appears warranted for improving the prognosis of patients with HNSCC. However, the efficacy of surveillance for ESCN in patients with HNSCC remains controversial and its impact on prognosis is not fully determined.13,17
The aims of this study were to provide clinical data on the necessity of surveillance to detect early ESCN in patients with HNSCC by analyzing the incidence, stage, and prognosis of the patients, and to investigate the risk factors associated with the development of ESCN.
MATERIALS AND METHODS
1. Patients
We retrospectively reviewed the data of patients who were diagnosed with primary HNSCC at Asan Medical Center, Seoul, Korea, between May 2005 and May 2010, and met the following criteria: (1) HNSCC with confirmed pathology, (2) no history of previous surgery, chemotherapy, or radiotherapy for other cancers during the previous 5 years, (3) no evidence of synchronous or metachronous cancer except ESCN. Data reviewed included age, gender, alcohol consumption, smoking, location of index HNSCC, stage of HNSCC, histological differentiation of HNSCC, treatment methods for HNSCC, presence of ESCN, stage of ESCN, date of diagnosis of HNSCC and ESCN, and date of death or last follow-up.
All patients underwent diagnostic work-ups with endoscopic and imaging analysis during initial staging as well as during follow-up after treatment. Initial staging work-ups included oral cavity inspection, endoscopic examinations of the pharynx and larynx, computed tomography (CT) and/or magnetic resonance imaging (MRI) of the head and neck, whole body 18F-FDG positron emission tomography (PET) and esophagogastroduodenoscopy (EGD). During follow-up after treatment, routine CT and/or MRI of the head and neck region and whole body 18F-FDG PET was carried out every 6 to 12 months up to the second year and alternatively checked annually thereafter. EGD was performed annually or biennially.
Alcohol consumption was estimated as the average number of grams of pure alcohol ingested per drinking day. Smoking was calculated as the number of cigarettes smoked per day multiplied by the number of total smoking years. Ex-smokers and former drinkers were defined as those who quit smoking or alcohol consumption for 5 or more years prior to index tumor diagnosis. Nonsmokers and nondrinkers were defined as patients who never used or who only rarely used tobacco and alcohol, respectively. The index primary tumor was defined as the first malignancy diagnosed, grouped by location (oral cavity, oropharynx, hypopharynx, or larynx). Tumor stage was classified according to the American Joint Committee on Cancer 7th edition.18 Diagnosis of the second primary ESCN was based on the criteria defined by Warren and Gates: (1) the tumor must be clearly malignant on histological examination, (2) the tumor must be separated by normal mucosa, and (3) the possibility that the second tumor represents a metastasis must be excluded.19 ESCN was defined as synchronous if it occurred within 1 year of the diagnosis of the HNSCC, or metachronous if it occurred over 1 year from the diagnosis of the HNSCC. Early ESCN was defined as a tumor limited to the mucosa or submucosa, and without lymph node metastasis or distant metastasis. Advanced ESCN was defined as a tumor that invaded beyond the submucosa of the esophagus, or a tumor that had lymph node or distant metastasis. In cases of HNSCC combined with multiple ESCNs, ESCN stage was defined according to the most advanced lesion.
2. Statistical analysis
The primary endpoint was overall survival (OS), defined as the time from the date of initial diagnosis of HNSCC to the date of death, and was calculated using the Kaplan-Meier method. Survival was compared using the log-rank test. Logistic regression model was carried out to determine risk factors associated with the development of SPT in the esophagus. All potential prognostic factors with p-values <0.05 on univariate analyses were entered into the multivariate analyses. The final models were determined using the backward elimination method. The SPSS for Windows version 18.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. This study was approved by the Institutional Review Board of Asan Medical Center (2010-0045).
RESULTS
1. Baseline characteristics of patients with HNSCC
A total of 714 patients who met inclusion criteria were enrolled. The median age was 59 years (range, 18 to 87 years), and 590 patients (82.6%) were male (Table 1). Five hundred forty-five patients (76.3%) were current or ex-smokers and 463 patients (64.8%) had a history of alcohol consumption. Considering HNSCC location, 236 lesions (33.1%) were in the oral cavity, 137 lesions (19.2%) were in the oropharynx, 87 lesions (12.2%) were in the hypopharynx, and 254 lesions (35.5%) were in the larynx. Two hundred forty-seven patients (34.6%) had localized disease (stage 0 to II), and 467 patients (65.4%) had locally advanced or metastatic disease (stage III to IV).
Table 1.
Baseline Characteristics for Patients with Head and Neck Squamous Cell Carcinoma
| HNSCC without ESCN (n=678) | HNSCC with ESCN (n=36) | p-value | |
|---|---|---|---|
| Age, median (range), yr | 59 (18–87) | 63 (40–83) | 0.041 |
| Male sex | 555 (81.8) | 35 (97.2) | 0.016 |
| Smoking | 0.028 | ||
| Nonsmoker | 167 (24.6) | 2 (5.6) | |
| Ex-smoker | 103 (15.2) | 8 (22.2) | |
| Current smoker | 408 (60.2) | 26 (72.2) | |
| Smoking index, median (IQR), pack-year | 24.0 (1.0–40.0) | 25.0 (18.0–45.0) | 0.256 |
| Alcohol consumption | 0.001 | ||
| Nondrinker | 248 (36.6) | 3 (8.3) | |
| Former drinker | 31 (4.6) | 4 (11.1) | |
| Current drinker | 399 (58.8) | 29 (80.6) | |
| Amount of daily alcohol intake, median (IQR), g | 9.6 (0.0–19.1) | 23.9 (9.6–67.0) | 0.019 |
| Location of HNSCC | <0.001 | ||
| Oral cavity | 232 (34.2) | 4 (11.1) | |
| Oropharynx | 134 (19.8) | 3 (8.3) | |
| Hypopharynx | 69 (10.2) | 18 (50) | |
| Larynx | 243 (35.8) | 11 (30.6) | |
| Histological differentiation of HNSCC | 0.071 | ||
| Well differentiated | 252 (37.2) | 7 (19.4) | |
| Moderately differentiated | 328 (48.4) | 24 (66.7) | |
| Poorly differentiated | 98 (14.4) | 5 (13.9) | |
| Clinical stage of HNSCC (AJCC 7th) | 0.718 | ||
| Stage 0 or I | 179 (26.4) | 7 (19.4) | |
| Stage II | 58 (8.6) | 3 (8.3) | |
| Stage III | 109 (16.1) | 5 (13.9) | |
| Stage IV | 332 (48.9) | 21 (58.4) | |
| Treatment methods of HNSCC | <0.001 | ||
| Surgery alone | 219 (32.3) | 4 (11.1) | |
| Surgery combined chemotherapy or radiotherapy | 260 (38.3) | 8 (22.2) | |
| Radiotherapy alone | 31 (4.6) | 3 (8.3) | |
| Chemotherapy alone | 20 (29.5) | 3 (8.3) | |
| Concurrent chemoradiotherapy | 127 (18.7) | 16 (44.4) | |
| Supportive care | 21 (3.0) | 2 (5.5) |
Data are presented as median (range) or number (%).
HNSCC, head and neck squamous cell carcinoma; ESCN, esophageal squamous cell neoplasia; IQR, interquartile range; AJCC, American Joint Committee on Cancer.
2. Comparison of baseline characteristics of patients with HNSCC according to the existence of ESCN and stage of ESCN
Of the 714 patients with HNSCC, 36 patients (5%) had SPTs in the esophagus. Comparing baseline characteristics of HN-SCC patients according to the existence of ESCN, median age (63 years vs 59 years, p=0.041), male gender (97.2% vs 81.8%, p=0.016), current or ex-smoker (94.4% vs 75.4%, p=0.028), former or current drinker (91.7% vs 63.4%, p=0.001), amount of daily alcohol intake (23.9 g vs 9.6 g, p=0.019), and hypopharyngeal location (50% vs 10.2%, p<0.001) were significantly greater in patients with ESCN compared to without ESCN (Table 1). Surgical resection (70.5% vs 33.3%, p<0.001) was performed more in patients without ESCN.
Of the 36 patients with ESCN, 17 patients had early ESCN (stage 0 to I) and 19 patients had advanced ESCN (stage IIA to IVB). However, in comparison of baseline characteristics of HNSCC patients according to the stage of ESCN, there were no significant differences in baseline characteristics between the groups, except smoking (p=0.002) and amount of daily alcohol intake (p=0.028) (Table 2).
Table 2.
Baseline Characteristics of Patients with Esophageal Squamous Cell Neoplasia
| Early ESCN (n=17) | Advanced ESCN (n=19) | p-value | |
|---|---|---|---|
| Age, median (range), yr | 65.4 (53–83) | 62.1 (40–80) | 0.288 |
| Male sex | 17 (100) | 18 (94.4) | 0.999 |
| Smoking | 0.002 | ||
| Nonsmoker | 0 | 2 (10.5) | |
| Ex-smoker | 0 | 8 (42.1) | |
| Current smoker | 17 (100) | 9 (47.4) | |
| Smoking index, median (IQR), pack-year | 27.5 (18.5–42.5) | 25.0 (16.0–49.5) | 0.521 |
| Alcohol consumption | 0.231 | ||
| Nondrinker | 0 | 3 (15.8) | |
| Former drinker | 2 (5.9) | 2 (10.5) | |
| Current drinker | 15 (94.1) | 14 (73.7) | |
| Amount of daily alcohol intake, median (IQR), g | 47.9 (21.5–67.0) | 9.6 (4.8–33.5) | 0.028 |
| Intervals between HNSCC and ESCN, mo | 9.59 (0–72) | 6.16 (0–54) | 0.547 |
| Location of HNSCC | 0.535 | ||
| Oral cavity | 1 (5.8) | 3 (15.9) | |
| Oropharynx | 1 (5.8) | 2 (10.5) | |
| Hypopharynx | 10 (58.9) | 8 (42.1) | |
| Larynx | 5 (29.5) | 6 (31.5) | |
| Histological differentiation of HNSCC | 0.581 | ||
| Well differentiated | 4 (23.5) | 3 (15.7) | |
| Moderately differentiated | 11 (64.7) | 13 (68.4) | |
| Poorly differentiated | 2 (11.7) | 3 (15.7) | |
| Clinical stage of HNSCC (AJCC 7th) | 0.437 | ||
| Stage 0 or I | 4 (23.5) | 3 (15.7) | |
| Stage II | 1 (5.8) | 2 (10.5) | |
| Stage III | 4 (23.5) | 1 (5.3) | |
| Stage IV | 8 (47.1) | 13 (68.4) | |
| Treatment methods of HNSCC | 0.868 | ||
| Surgery alone | 3 (17.6) | 1 (5.3) | |
| Surgery combined chemotherapy or radiotherapy | 3 (17.6) | 5 (26.3) | |
| Radiotherapy alone | 3 (17.6) | 0 | |
| Chemotherapy alone | 0 | 3 (15.9) | |
| Concurrent chemoradiotherapy | 7 (41.3) | 9 (47.2) | |
| Supportive care | 1 (5.9) | 1 (5.3) |
Data are presented as median (range) or number (%).
ESCN, esophageal squamous cell neoplasia; IQC, interquartile range; HNSCC, head and neck squamous cell carcinoma; AJCC, American Joint Committee on Cancer.
3. Overall survival rate for patients with HNSCC according to the existence of ESCN and stage of ESCN
At a median follow-up of 31 months (range, 1 to 76 months), median OS was 55.5 months (95% confidence interval [CI], 53.3 to 57.7 months). The overall 3-year survival rate was 69.6%. The OS rates of patients with HNSCC according the existence of ESCN and stage of ESCN are shown in Fig. 1. The 3-year OS rates in HNSCC patients with or without ESCN were 48.2% and 71.2%, respectively (p<0.001) (Fig. 1A). The 3-year OS rates for patients with early and advanced ESCN were 77.7% and 21.7%, respectively (p=0.01) (Fig. 1B). However, there was no significant difference between patients without ESCN (71.2%) and patients with early ESCN (77.7%) (p=0.42).
Fig. 1.
Kaplan-Meier survival curves for patients with head and neck squamous cell carcinoma (HNSCC) according to the existence (A) and stage of esophageal squamous cell neoplasia (ESCN) (B).
4. Characteristics of combined ESCN lesions
The characteristics of combined ESCN lesions are shown in Table 3. Forty-eight ESCNs were detected in 36 patients: 26 patients had one lesion; eight patients had two lesions; and two patients had three lesions. The median interval time between the diagnosis of HNSCC and ESCN was 7.8 months (range, 0 to 72 months). Thirty-seven lesions (77.1%) were synchronous and 11 lesions (22.9%) were metachronous. Among 37 synchronous ESCNs, 15 lesions (40.3%) were early ESCN and 22 lesions (59.7%) were advanced ESCN. However, in case of metachronous ESCN, nine lesions (81.8%) were early ESCN and two lesions (18.2%) were advanced ESCN. Of the 15 synchronous early ESCNs, 12 lesions were detected during initial diagnostic work-up and the others were detected during follow-up. Of the 22 synchronous advanced ESCNs, 21 lesions were detected during initial diagnostic work-up and one lesion was detected during follow-up. Of the nine metachronous early ESCNs, seven lesions were detected by annual EGD surveillance and the others were detected by biennial EGD surveillance. However, all metachronous advanced ESCN were detected by biennial EGD surveillance. Seven lesions (14.5%) were located in the cervical or upper thoracic esophagus, 17 (35.4%) in the middle thoracic esophagus, and 24 (50%) in the lower thoracic esophagus.
Table 3.
Characteristics of Combined Esophageal Squamous Cell Neoplasia
| Characteristic | No. of lesions (%) |
|---|---|
| No. of ESCN | |
| Single | 26 (72.2) |
| Double | 8 (22.2) |
| Triple | 2 (5.6) |
| Location of ESCN | |
| Cervical and upper thoracic esophagus | 7 (14.5) |
| Middle thoracic esophagus | 17 (35.4) |
| Lower thoracic esophagus | 24 (50.0) |
| Histological differentiation of ESCN | |
| High grade dysplasia | 8 (16.6) |
| SCC, well differentiated | 12 (25.0) |
| SCC, moderately differentiated | 22 (45.7) |
| SCC, poorly differentiated | 6 (12.5) |
| Clinical stage of ESCN (AJCC 7th) | |
| Stage 0 or I | 17 (47.2) |
| Stage II | 6 (16.7) |
| Stage III | 9 (25.0) |
| Stage IV | 4 (11.1) |
ESCN, esophageal squamous cell neoplasia; SCC, squamous cell carcinoma; AJCC, American Joint Committee on Cancer.
5. Risk factors associated with the development of ESCN
The results from the logistic regression model to analyze the risk factor associated with the development of ESCN are shown in Table 4. In univariate analysis, age, gender, smoking, alcohol consumption, amount of daily alcohol intake, HNSCC location, and histological differentiation of HNSCC were associated with development of ESCN. In multivariate analysis, among them, alcohol consumption (former drinker: odds ratio [OR], 8.42, 95% confidence interval (CI), 1.49 to 47.59, p=0.016; current drinker: OR, 4.37, 95% CI, 1.12 to 17.07, p=0.034), and hypopharyngeal cancer (OR, 15.85; 95% CI, 4.20 to 59.81; p<0.001) were the significant factors associated with development of ESCN.
Table 4.
Analysis of Factors Associated with the Development of Esophageal Squamous Cell Neoplasia
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age | 1.04 (1.01–1.07) | 0.036 | 1.01 (0.96–1.05) | 0.799 |
| Male sex | 7.76 (1.05–57.16) | 0.044 | 1.76 (0.18–17.61) | 0.631 |
| Smoking | ||||
| Nonsmoker | 1 | 1 | ||
| Ex-smoker | 6.49 (1.35–31.14) | 0.02 | 2.78 (0.43–18.16) | 0.285 |
| Current smoker | 5.32 (1.25–22.67) | 0.024 | 1.19 (0.21–6.66) | 0.847 |
| Smoking index | 1.007 (0.99–1.02) | 0.256 | ||
| Alcohol consumption | ||||
| Nondrinker | 1 | 1 | ||
| Former drinker | 10.67 (2.28–49.9) | 0.003 | 8.42 (1.49–47.59) | 0.016 |
| Current drinker | 6.01 (1.81–19.93) | 0.003 | 4.37 (1.12–17.07) | 0.034 |
| Amount of daily alcohol intake | 1.01 (1.01–1.02) | 0.001 | 1.00 (0.99–1.01) | 0.887 |
| Location of HNSCC | ||||
| Oral cavity | 1 | 1 | ||
| Oropharynx | 0.43 (0.05–3.86) | 0.448 | 0.44 (0.044–4.43) | 0.486 |
| Hypopharynx | 17.31 (5.72–52.41) | <0.001 | 15.85 (4.20–59.81) | <0.001 |
| Larynx | 2.63 (0.82–8.36) | 0.102 | 2.42 (0.62–9.51) | 0.205 |
| Histological differentiation of HNSCC | ||||
| Well differentiated | 1 | 1 | ||
| Moderately differentiated | 2.64 (1.14–6.21) | 0.027 | 2.31 (0.87–6.12) | 0.092 |
| Poorly differentiated | 1.84 (0.57–5.93) | 0.309 | 3.85 (0.97–15.33) | 0.056 |
| Stage of HNSCC (AJCC 7th) | ||||
| Stage 0 or I | 1 | - | ||
| Stage II | 1.32 (0.33–5.28) | 0.692 | - | - |
| Stage III | 1.17 (0.36–3.79) | 0.790 | - | - |
| Stage IV | 1.62 (0.68–3.88) | 0.281 | - | - |
OR, odds ratio; CI, confidence interval; HNSCC, head and neck squamous cell carcinoma; AJCC, American Joint Committee on Cancer.
DISCUSSION
In the present study, we investigated the incidence of second primary ESCN, prognosis according to the existence and stage of ESCN, and risk factors associated with the development of ESCN in patients with HNSCC, and aimed to provide clinical data on the necessity of surveillance for detecting early ESCN. Among 714 patients, the overall incidence of second primary ESCN was 5.0%. The OS rate of HNSCC patients with early ESCN represented a significantly improved prognosis over patients with advanced ESCN. Alcohol consumption and hypopharyngeal cancer were significant factors associated with the development of ESCN.
SPT in patients with HNSCC illustrate the concept of field cancerization, in which environmental carcinogens, such as tobacco and alcohol, may induce a field of mucosa afflicted with premalignant disease and elevate epithelial cancer risk throughout the upper aerodigestive tract.3 Of the various SPTs, ESCN is one of the most frequent SPT associated with HNSCC. The incidence of ESCN in patients with HNSCC has been reported to range from 0.8% to 21.9%, with differences in occurrences attributed to both geographic location and the anatomical location of the primary HNSCC.5,8–14 In our study, the incidence of ESCN was 5.0% and similar with that observed in the previous reports. These incidences are higher than the estimated incidence of HNSCC in the general population of Korea, which is 1.1%.20 Our result showed that patients with HNSCC are at increased risk of developing ESCN.
The introduction of new surgical techniques, improved radiotherapy techniques, and the use of chemotherapy has led to a significant improvement in locoregional control of HNSCC over the previous few decades; however, OS from HNSCC have not greatly improved.21,22 This is likely to be due to the frequent development of SPT that occur more often in patients with HNSCC than in patients with cancers of other sites. Among the SPT, ESCN is the most common SPT of the digestive tract and is one of leading causes of treatment failure and death with a median survival after the development of ESCN of less than 1 year, regardless of the site of the index tumor.23 Therefore, early detection of ESCN, utilizing modalities such as endoscopy, in patients with HNSCC appears critical for improving their prognosis.16 However, the efficacy of surveillance for ESCN remains controversial and its impact on prognosis has not been fully determined. We found that patients with ESCN and, in particular, advanced stage ESCN, had significant reductions in OS. The 3-year OS of HNSCC patients with early ESCN represented a significantly improved prognosis over patients with advanced ESCN. And, among 11 metachronous ESCNs detected by surveillance, ratio of early ESCN was 81.8%. Our results lend support to the argument that early detection of ESCN is critical and surveillance in patients with HNSCC is warranted.
To improve protocols for follow-up screening and identify at-risk patients, factors associated with the development of ESCN in patients with HNSCC must be identified. We found that two factors were associated with the development of ESCN: alcohol consumption and hypopharyngeal cancer. Alcohol consumption generally accepted as major behavioral risk factors for occurrence of HNSCC or ESCN.24,25 We demonstrated that the habit of drinking alcohol was an independent risk factor for development of ESCN. However, contrary to our expectations, smoking did not show any association with the development of ESCN. Smoking is closely associated with alcohol consumption, making it difficult to separate their effects. The reason for this result is unclear, and further studies are needed to clarify this issue.
Location of index tumors is associated with further development of SPT along the aerodigestive tract: the tumor had a tendency to follow either a respiratory (larynx-lung) or a digestive (pharynx-esophagus) axis.26,27 In our study, the incidence of second primary ESCN in patients with hypopharyngeal caner was 20.7% (18/87) and hypopharyngeal cancer was the significant factor associated with development of ESCN. This finding reinforces the concept that susceptibility to tumor formation lies primarily along the digestive axis (pharynx-esophagus), given an index tumor in the tract.
This study had several potential limitations. First, patients were reviewed in a retrospective manner, which introduces the possibility of publication, exclusion, and selection bias. Second, we did not routinely perform image-enhanced endoscopy, such as narrow band image and Lugol chromoendoscopy, enable early detection of ESCN and precancerous lesions. So, the incidence of synchronous or metachronous ESCN was likely to be underestimated although endoscopy was performed by experienced endoscopists. Third, this study was conducted in a single center; however, this center is major referral center in Korea. Multicenter studies should be performed to confirm the results of the current study.
In conclusion, patients with HNSCC have a high risk of developing ESCN. Patients with early ESCN were similar in prognosis with those without ESCN, in contrast to advanced ESCN. We recommended that optimal surveillance should be performed to detect early ESCN in patients with HNSCC, especially in those who have history of alcohol consumption and hypopharyngeal cancer. These efforts may substantially improve the prognosis of patients with HNSCC. And, further studies for optimal methods and interval of surveillance are needed to improve the detection rate of early ESCN.
Footnotes
See editorial on page 131.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Chuang SC, Scelo G, Tonita JM, et al. Risk of second primary cancer among patients with head and neck cancers: a pooled analysis of 13 cancer registries. Int J Cancer. 2008;123:2390–2396. doi: 10.1002/ijc.23798. [DOI] [PubMed] [Google Scholar]
- 2.Morris LG, Sikora AG, Patel SG, Hayes RB, Ganly I. Second primary cancers after an index head and neck cancer: subsite-specific trends in the era of human papillomavirus-associated oropharyngeal cancer. J Clin Oncol. 2011;29:739–746. doi: 10.1200/JCO.2010.31.8311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer. 1953;6:963–968. doi: 10.1002/1097-0142(195309)6:5<963::AID-CNCR2820060515>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 4.Muto M, Hironaka S, Nakane M, Boku N, Ohtsu A, Yoshida S. Association of multiple Lugol-voiding lesions with synchronous and metachronous esophageal squamous cell carcinoma in patients with head and neck cancer. Gastrointest Endosc. 2002;56:517–521. doi: 10.1016/S0016-5107(02)70436-7. [DOI] [PubMed] [Google Scholar]
- 5.Shiozaki H, Tahara H, Kobayashi K, et al. Endoscopic screening of early esophageal cancer with the Lugol dye method in patients with head and neck cancers. Cancer. 1990;66:2068–2071. doi: 10.1002/1097-0142(19901115)66:10<2068::AID-CNCR2820661005>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 6.Sturgis EM, Miller RH. Second primary malignancies in the head and neck cancer patient. Ann Otol Rhinol Laryngol. 1995;104:946–954. doi: 10.1177/000348949510401206. [DOI] [PubMed] [Google Scholar]
- 7.Vikram B. Changing patterns of failure in advanced head and neck cancer. Arch Otolaryngol. 1984;110:564–565. doi: 10.1001/archotol.1984.00800350006003. [DOI] [PubMed] [Google Scholar]
- 8.Jones AS, Morar P, Phillips DE, Field JK, Husband D, Helliwell TR. Second primary tumors in patients with head and neck squamous cell carcinoma. Cancer. 1995;75:1343–1353. doi: 10.1002/1097-0142(19950315)75:6<1343::AID-CNCR2820750617>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 9.Scherübl H, von Lampe B, Faiss S, et al. Screening for oesophageal neoplasia in patients with head and neck cancer. Br J Cancer. 2002;86:239–243. doi: 10.1038/sj.bjc.6600018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petit T, Georges C, Jung GM, et al. Systematic esophageal endoscopy screening in patients previously treated for head and neck squamous-cell carcinoma. Ann Oncol. 2001;12:643–646. doi: 10.1023/A:1011191720336. [DOI] [PubMed] [Google Scholar]
- 11.Ina H, Shibuya H, Ohashi I, Kitagawa M. The frequency of a concomitant early esophageal cancer in male patients with oral and oropharyngeal cancer: screening results using Lugol dye endoscopy. Cancer. 1994;73:2038–2041. doi: 10.1002/1097-0142(19940415)73:8<2038::AID-CNCR2820730804>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 12.León X, Quer M, Diez S, Orus C, Lopez-Pousa A, Burgues J. Second neoplasm in patients with head and neck cancer. Head Neck. 1999;21:204–210. doi: 10.1002/(SICI)1097-0347(199905)21:3<204::AID-HED4>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 13.Atabek U, Mohit-Tabatabai MA, Rush BF, Ohanian M, Rovelli P. Impact of esophageal screening in patients with head and neck cancer. Am Surg. 1990;56:289–292. [PubMed] [Google Scholar]
- 14.Leon X, Ferlito A, Myer CM, 3rd, et al. Second primary tumors in head and neck cancer patients. Acta Otolaryngol. 2002;122:765–778. doi: 10.1080/003655402/000028048. [DOI] [PubMed] [Google Scholar]
- 15.Cohn AM, Peppard SB. Multiple primary malignant tumors of the head and neck. Am J Otolaryngol. 1980;1:411–417. doi: 10.1016/S0196-0709(80)80022-6. [DOI] [PubMed] [Google Scholar]
- 16.Roth JA, Putnam JB., Jr Surgery for cancer of the esophagus. Semin Oncol. 1994;21:453–461. [PubMed] [Google Scholar]
- 17.Hirota WK, Zuckerman MJ, Adler DG, et al. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 2006;63:570–580. doi: 10.1016/j.gie.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL. AJCC cancer staging manual. 7th ed. New York: Springer; 2010. [Google Scholar]
- 19.Warren S, Gates O. Multiple primary malignant tumors: a survey of the literature and a statistical study. Am J Cancer. 1932;16:1358–1414. [Google Scholar]
- 20.Statistics Korea. Korean statistical information service [Internet] Daejeon: Statistics Korea; 2009. [cited 2013 Aug 2]. Available from: http://kosis.kr. [Google Scholar]
- 21.Sant M, Aareleid T, Berrino F, et al. EUROCARE-3: survival of cancer patients diagnosed 1990–94--results and commentary. Ann Oncol. 2003;14(Suppl 5):v61–v118. doi: 10.1093/annonc/mdg754. [DOI] [PubMed] [Google Scholar]
- 22.Berrino F, Gatta G. Variation in survival of patients with head and neck cancer in Europe by the site of origin of the tumours. EUROCARE Working Group. Eur J Cancer. 1998;34:2154–2161. doi: 10.1016/S0959-8049(98)00328-1. [DOI] [PubMed] [Google Scholar]
- 23.Chen MC, Huang WC, Chan CH, Chen PT, Lee KD. Impact of second primary esophageal or lung cancer on survival of patients with head and neck cancer. Oral Oncol. 2010;46:249–254. doi: 10.1016/j.oraloncology.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 24.Erkal HS, Mendenhall WM, Amdur RJ, Villaret DB, Stringer SP. Synchronous and metachronous squamous cell carcinomas of the head and neck mucosal sites. J Clin Oncol. 2001;19:1358–1362. doi: 10.1200/JCO.2001.19.5.1358. [DOI] [PubMed] [Google Scholar]
- 25.Aaltonen LA, Hamilton SR. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press; 2000. p. 270. [Google Scholar]
- 26.Panosetti E, Luboinski B, Mamelle G, Richard JM. Multiple synchronous and metachronous cancers of the upper aerodigestive tract: a nine-year study. Laryngoscope. 1989;99:1267–1273. doi: 10.1288/00005537-198912000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Morimoto M, Nishiyama K, Nakamura S, et al. Significance of endoscopic screening and endoscopic resection for esophageal cancer in patients with hypopharyngeal cancer. Jpn J Clin Oncol. 2010;40:938–943. doi: 10.1093/jjco/hyq068. [DOI] [PubMed] [Google Scholar]