Abstract
BACKGROUND
The growing number of primary care physicians (PCPs) reducing their clinical work hours has raised concerns about meeting the future demand for services and fulfilling the continuity and access mandates for patient-centered care. However, the patient’s experience of care with part-time physicians is relatively unknown, and may be mediated by continuity and access to care outcomes.
OBJECTIVE
We aimed to examine the relationships between a physicians’ clinical full-time equivalent (FTE), continuity of care, access to care, and patient satisfaction with the physician.
DESIGN
We used a multi-level structural equation estimation, with continuity and access modeled as mediators, for a cross-section in 2010.
PARTICIPANTS
The study included family medicine (n = 104) and internal medicine (n = 101) physicians in a multi-specialty group practice, along with their patient satisfaction survey responses (n = 12,688).
MAIN MEASURES
Physician level FTE, continuity of care received by patients, continuity of care provided by physician, and a Press Ganey patient satisfaction with the physician score, on a 0–100 % scale, were measured. Access to care was measured as days to the third next-available appointment.
KEY RESULTS
Physician FTE was directly associated with better continuity of care received (0.172 % per FTE, p < 0.001), better continuity of care provided (0.108 % per FTE, p < 0.001), and better access to care (−0.033 days per FTE, p < 0.01), but worse patient satisfaction scores (−0.080 % per FTE, p = 0.03). The continuity of care provided was a significant mediator (0.016 % per FTE, p < 0.01) of the relationship between FTE and patient satisfaction; but overall, reduced clinical work hours were associated with better patient satisfaction (−0.053 % per FTE, p = 0.03).
CONCLUSIONS
These results suggest that PCPs who choose to work fewer clinical hours may have worse continuity and access, but they may provide a better patient experience. Physician workforce planning should consider these care attributes when considering the role of part-time PCPs in practice redesign efforts and initiatives to meet the demand for primary care services.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-3104-6) contains supplementary material, which is available to authorized users.
KEY WORDS: part-time work, continuity of care, access to care, patient satisfaction
INTRODUCTION
In the last decade, there has been a shift in the primary care workforce toward a higher proportion of physicians choosing to work part-time. The 2011 Physician Retention Survey by the American Medical Group Association found that 22 % of male physicians and 44 % of female physicians worked less than full-time, up from 7 % and 29 %, respectively, in 2005.1 Longer hours have been associated with greater dissatisfaction with work–life balance and an increased risk of burnout in primary care physicians (PCPs).2 Some of the fastest-growing physician demographic groups, e.g., women at the beginning or middle of their careers and men at the end, are increasing the demand for reduced clinical hours.3 At the same time, insurance expansion from health reform and an aging population are projected to dramatically increase the demand for primary care services.4–7
Part-time physicians have faced concerns about their ability to fulfill the goals of patient-centered primary care.8 Continuity of care and care coordination may be compromised when physicians work less than full-time,9–11 and part-time physicians “challenge traditional expectations about face-to-face continuity of care between patient and physician.”12 Additionally, access and enhanced access, such as expanded hours and same-day appointments,13,14 may be more difficult with reduced clinical hours.15 Despite these concerns, only one study included empirical evidence and found that PCPs working greater than 65 h/week had slightly higher continuity, but no difference in access.16
Furthermore, the patient perspective on being cared for by a part-time PCP is not well understood. One systematic review concluded that provider work hours had no relationship with patient satisfaction,16–18 yet because of the lack of well-designed studies, the authors could not make strong conclusions about these findings.13 However, there are several possible reasons why physicians with fewer clinical full time equivalents (FTEs) may have higher patient satisfaction scores. Studies have shown that part-time physicians experience higher work satisfaction and less burnout than full-time physicians,19,20 which may be attributed to an increased sense of control in setting one’s schedule,19 feeling less time pressure with patients,21 or better work–life balance.22,23 There is a well-established association between patient and physician satisfaction,21 perhaps because more satisfied physicians may communicate better,24 be more empathetic,24 and better address their patients’ concerns.25 Finally, longer clinical FTEs may contribute to job-related stress and exhaustion, which has been associated with lower quality communication in non-medical settings.26,27 One study found that patients of part-time physicians were 2.49 % more likely than those of full-time physicians to report better satisfaction with care.21
There are several limitations with the current literature associating a physician’s clinical work hours with patient satisfaction. A common limitation is the use of an arbitrary discrete cutoff to define part-time versus full-time,16,17,21 with cutoffs ranging from 20 clinical hours/week17 to 40 h/week of self-reported work.16 No study has yet controlled for either continuity of care or access, which have both been associated with patient satisfaction,28–31 or accounted for their potential mediating relationship, since continuity of care and access are also likely to be affected by a physician’s work hours.
We seek to understand the relationship between physicians’ clinical work hours and the patient experience by simultaneously estimating the association of a physician’s clinical FTE with continuity of care, access to care, and patient satisfaction with the provider. We hypothesize that physicians who work fewer clinical hours may have lower care continuity and access to care, which may be negatively associated with patient satisfaction. However, these physicians may also have other care attributes, such as communication style, that are positively associated with patient satisfaction, raising questions about the overall relationship between a physician’s clinical FTE and patient satisfaction. Findings from this study may inform the discussion about the role of part-time PCPs in practice redesign efforts and initiatives to meet the increasing demand for primary care services post-Affordable Care Act.
METHODS
Study Setting
The study was conducted at a large multi-specialty, mixed-payer, ambulatory care practice in northern California, which contracts with a group of nearly 1,000 physicians. This setting provides an example of a medical practice in which part-time physicians are more likely to work: physician-owned practices of 500 or more physicians, compared to practices that are hospital-based or have fewer than 50 physicians.32 The medical group provides care for more than 850,000 unique patients, whose demographic characteristics reflect the underlying population with respect to gender, age and race/ethnicity.33
Study Design
We conducted an observational study for the 12-month period from January 2010 through December 2010. The PCP was the unit of analysis. Two hundred and five physicians were nested within 22 departments [Family Medicine (n = 13) and Internal Medicine (n = 9)], nested within 13 clinics.
Conceptual Model
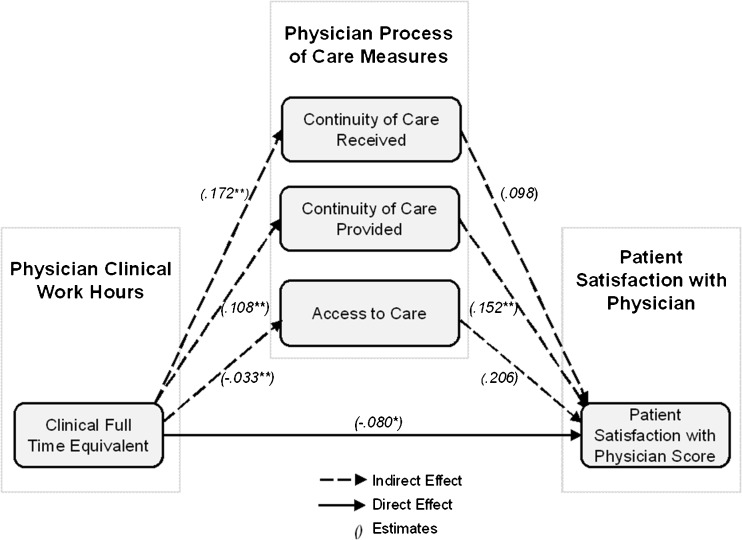
We conceptualized a model in which the total relationship between a physician’s clinical FTE and patient satisfaction includes both a direct and an indirect association. The direct association comes from the clinical FTE, care continuity,28,30 access to care,29,31 and other practice characteristics. The indirect association comes through continuity of care and access to care. The indirect association through the continuity of care, for example, may be understood as a combination of the relationship between a physician’s FTE and continuity and the relationship between continuity and patient satisfaction. Figure 1 provides a graphical illustration of these relationships.
Fig. 1.
Conceptual model of the relationship between physician clinical work hours, continuity of care, access to care, and patient satisfaction with the physician. Note: All variables in this diagram are measured at the physician level. Variable definitions are provided in the notes for Table 1. The estimates come from Table 2, ** indicates p < 0.01, and * indicates p < 0.05.
Variable Definitions
Clinical Full Time Equivalent (FTE)
The main variable of interest was a physician’s clinical FTE, which is a measure of clinical work hours. A 100 % clinical FTE corresponded to 34 clinical hours per week. The organization does not publish any estimates for the number of hours per week spent on non-clinical work or the total hours worked per week. The clinical FTE was measured as a continuous variable.
Continuity of Care
Continuity of care is measured by two variables: “continuity of care received,” which measures the patient experience and “continuity of care provided,” which measures the provider experience. Continuity of care received, also known as “see your own” in quality improvement literature,34 is defined as the percentage of primary care office visits made by a physician’s patients to their own PCPs in a year. Continuity of care provided is defined as the annual percentage of a physician’s office visits that were spent seeing the PCP’s own patients. This measure is commonly used jointly with the continuity of care received to monitor a physician’s panel size, because as the panel size increases, a physician’s continuity of care provided tends to increase, but, above an optimal point, their patients’ continuity of care received tends to decrease as more patients end up seeing other providers.35 Physicians who have a higher continuity of care provided or who see more of their own patients may have more patient satisfaction evaluations filled out by their own patients. Patients who see their own provider are more likely to report higher satisfaction.30
Access to Care
The third next-available appointment measures a PCP’s average number of days until the third next-available appointment. It is a widely used indicator of when an appointment is easily available to patients,36 and is a better reflection of the system availability than the time to the first or second next-available appointment, which may be available due to a cancellation. Physicians have the option to practice with ‘short’ and ‘long’ appointments that are either 15 min and 30 min or 20 min and 40 min, respectively. We constructed the access to care variable by averaging each PCP’s annualized third next-available short and long appointments.
Patients’ Experiences of Care
We used patient experiences of care obtained from the Press Ganey Patient Satisfaction Survey, and examined all ten items related to the provider, including the provider’s time spent with patient, concern for questions and worries, involvement in decision making, explanations about problems and conditions, information about medication, instructions for follow-up care, clarity of language, friendliness and courtesy, and the patient’s confidence in and likelihood of recommending the provider. The Press Ganey Survey provides patients with a five-point Likert scale ranging from “Very Poor” to “Very Good.” These data were aggregated at the provider level as the percentage of “Very Good” responses for each item. Exploratory factor analysis on the ten items revealed one distinct domain of patient satisfaction with the physician, which had an internal consistency estimate of 0.98 (appendices available online). We created an overall score for patient satisfaction with the physician by calculating the mean of the ten items to preserve the original scale range of 0–100 %. As the factor loadings and the uniqueness measures were roughly the same in the ten items, the reliability of the factor score would only be slightly higher than the mean score.
The surveys were mailed directly to patients and the response rate was 21.2 %, compared with the national Press Ganey response rate of 21.6 % for mailed surveys. There were an average of approximately 60 responses (SD = 15) per physician. Our final data set included about 12,688 patient responses matched to physicians.
Explanatory Variables
To account for the potential influences of other physician-level factors on patient satisfaction, we adjusted for variables that previous research suggests may influence patient satisfaction.37 An indicator variable was used to control for the different appointment lengths (15/30 min versus 20/40 min) practiced by the physicians, because some patients prefer more time with their provider.38 Physician gender has been associated with mixed results for patient satisfaction.37,39 The years-since-medical-school variable was measured from the graduation date and captures both physician age and experience dimensions, with evidence varying for these characteristics as well.39,40
We also included covariates to adjust for differences in department-level characteristics. The staff-to-physician ratio was the number of staff divided by the total FTE of the physicians in the department. Staff members included physician assistants, nurse practitioners, nurses, medical assistants, and patient services representatives. We also included department size, defined as the total number of staff plus the total FTE of physicians. A binary variable for internal versus family medicine was used to control for potential unmeasured differences in provider and patient characteristics between the specialties.
Lastly, to account for patient characteristics,41 we controlled for gender, age, ethnicity, insurance type, and average Charlson score42 of the patient panel. As the survey was based on random sampling, panel level characteristics approximate the characteristics of survey respondents. Since the organization is the product of a 2008 merger of three large multi-specialty physician groups, we included division indicators to account for the legacies of different organizational cultures.
Analysis
According to our conceptual model, we simultaneously estimated the association of a physician’s clinical FTE with four variables: continuity of care received, continuity of care provided, access to care, and the patient satisfaction with the physician score. A multi-level structural equations model was analyzed using Stata/MP 13.0 GSEM, with department level random effects and standard errors correlated at the clinic level.
RESULTS
The clinical FTE ranged from 50 % (the minimum required by the practice) to 103 % (Table 1). The average FTE was largely similar across the specialties (family medicine = 82.4 %, internal medicine = 78.0 %). Physicians working fewer clinical FTEs were more likely to be female (X2, p < 0.001), and to have a panel with more female (F test, p < 0.001) and non-Hispanic white (F test, p < 0.001) patients. In a sensitivity analysis, we examined gender concordance between the physician and patient as measured by the percentage of the panel with the same gender as the physician. We found that gender concordance was relatively constant across the five 10 % clinical FTE bands (F test, p =0.908) with a sample average (SD) of 72.2 % (6.9 %) of the panel. Including gender concordance had no effect on our results (available upon request to authors). Across the five 10 % clinical FTE bands, continuity of care received increased from 68.4 to 75.7 % (F test, p < 0.001), continuity of care provided displayed no relationship (F test, p = 0.83), access to care decreased from 6.2 days to 3.8 days (F test, p = 0.06), and the patient satisfaction score decreased from 82.4 to 77.4 % (F test, p < 0.01). See the appendices available online for the correlations of the physician-level independent variables.
Table 1.
Patient Panel, Physician, and Department Characteristics, and the Press Ganey Patient Satisfaction with Physician Score, 2010
| Characteristics | Sample | Physician clinical full-time equivalents | |||||
|---|---|---|---|---|---|---|---|
| 50–60 % (n = 33) | 61–70 % (n = 22) | 71–80 % (n = 51) | 81–90 % (n = 28) | 91–103 % (n = 71) | p value | ||
| Patient panel level (n = 205) | |||||||
| Charlson Score, mean (SD) | 0.33 (0.17) | 0.39 | 0.36 | 0.32 | 0.32 | 0.30 | 0.12 |
| % Female, mean (SD) | 56.8 (22.3) | 69.4 | 65.3 | 62.2 | 53.0 | 46.0 | < 0.001 |
| Age, mean (SD) | |||||||
| % Age ≤ 18 | 5.1 (6.1) | 3.5 | 4.5 | 5.4 | 4.9 | 6.0 | 0.42 |
| % 19 ≤ Age < 35 | 25.5 (11.9) | 20.3 | 25.4 | 25.1 | 28.1 | 27.2 | 0.26 |
| % 36 ≤ Age < 50 | 32.6 (7.6) | 31.0 | 32.7 | 33.7 | 34.4 | 31.8 | 0.95 |
| % 51 ≤ Age < 65 | 22.1 (8.7) | 26.7 | 20.9 | 22.7 | 20.3 | 20.5 | 0.05 |
| % Age ≥ 65 | 14.7 (9.8) | 18.6 | 16.4 | 13.1 | 12.3 | 14.5 | 0.95 |
| Race, mean (SD) | |||||||
| % Non-Hispanic White | 51.6 (16.7) | 60.5 | 49.0 | 53.5 | 48.5 | 48.2 | <0.01 |
| % Asian | 26.9 (16.8) | 20.3 | 31.0 | 24.9 | 30.4 | 28.7 | 0.06 |
| % Hispanic | 9.5 (7.1) | 7.5 | 8.3 | 9.9 | 9.1 | 10.5 | 0.30 |
| % Other | 12.0 (2.4) | 11.7 | 11.7 | 11.6 | 11.9 | 12.6 | 0.15 |
| Insurance, mean (SD) | |||||||
| % PPO | 49.7 (7.3) | 49.3 | 48.1 | 49.4 | 50.0 | 50.5 | 0.87 |
| % HMO | 22.5 (5.4) | 22.8 | 21.6 | 23.7 | 22.3 | 21.9 | 0.96 |
| % Medicare PPO | 8.7 (6.8) | 11.3 | 9.4 | 7.5 | 7.2 | 8.8 | 0.04 |
| % Medicare HMO | 3.0 (2.7) | 3.9 | 3.8 | 2.7 | 2.4 | 2.6 | 0.09 |
| % Other | 16.1 (5.2) | 12.6 | 17.0 | 16.7 | 18.1 | 16.2 | 0.65 |
| Physician level (n = 205) | |||||||
| Continuity of care received(%), mean (SD) | 73.1 (6.7) | 68.4 | 71.1 | 73.3 | 73.5 | 75.7 | <0.001 |
| Continuity of care provided (%), mean (SD) | 81.0 (14.0) | 79.6 | 83.7 | 80.2 | 82.1 | 80.9 | 0.83 |
| Access to care (days), mean (SD) | 5.0 (4.9) | 6.2 | 6.2 | 5.6 | 4.4 | 3.8 | 0.06 |
| 20/40 min appointment lengths*, no (%) | 169 (82.4 %) | 87.9 % | 86.4 % | 78.4 % | 85.7 % | 80.2 % | 0.75 |
| Years since medical school, mean (SD) | 16.2 (8.4) | 17.5 | 16.5 | 16.2 | 18.1 | 14.7 | 0.34 |
| Female, no (%) | 134 (65.4 %) | 90.1 % | 77.3 % | 76.5 % | 57.1 % | 45.1 % | <0.001 |
| Clinical full-time equivalent, mean (SD) | 80.2 (16.3) | – | – | – | – | – | |
| Specialty | |||||||
| Family medicine | 104 (50.7 %) | 33.3 % | 45.5 % | 52.9 % | 60.7 % | 54.9 % | 0.20 |
| Internal medicine | 101 (49.3 %) | 66.7 % | 54.5 % | 47.1 % | 39.3 % | 45.1 % | |
| Department level (n = 22) | |||||||
| Staff to physician ratio | 2.1 (0.7) | – | – | – | – | – | |
| Department Size | 24.3 (18.8) | – | – | – | – | – | |
| Patient satisfaction (n = 205) | |||||||
| Patient satisfaction with physician score (%) | 78.9 (8.2) | 82.4 | 77.8 | 80.9 | 75.8 | 77.4 | <0.01 |
Continuity of care received is defined as the annual percentage of all primary care office visits made by a physician’s patients to their own physician. Continuity of Care Provided is defined as the annual percentage of a physician’s office visits that were spent seeing their own patients. Access to Care was constructed by averaging each PCP’s annualized third next available short and long appointment. Staff to Physician Ratio measures the number of physician assistants, nurse practitioners, nurses, medical assistants, and patient services representatives divided by the total FTE of physicians in the department. The Department Size is defined as the total number of staff plus the total FTE of physicians. For the Overall Satisfaction with Physician Score, values indicate the percentage of respondents for each physician reporting “Very Good”
Table 2 displays the structural equation results illustrated by the conceptual model (Fig. 1). The physician’s clinical FTE was significantly associated with better continuity of care received (0.172 % per FTE, p < 0.001), better continuity of care provided (0.108 % per FTE, p < 0.001), and better access to care (−0.033 days per FTE, p < 0.01). This translates to a 8.60 % (percentage point) improvement in continuity of care received, 5.40 % improvement in continuity of care provided, and 1.7 day reduction in days to an appointment between a full-time physician (100 % FTE) compared to a part-time physician (50 % FTE).
Table 2.
Structural Equation Modeling Results of the Direct Association of a Physician’s Clinical Full-Time Equivalent with Continuity of Care, Access to Care, and the Press Ganey Patient Satisfaction with Physician Score, 2010
| Continuity of care received (%) | Continuity of care provided (%) | Access to care (days) | Patient satisfaction with physician score (%) | |||||
|---|---|---|---|---|---|---|---|---|
| Coeff | p value | Coeff | p value | Coeff | p value | Coeff | p value | |
| Physician level | ||||||||
| Continuity of care received | 0.098 | 0.31 | ||||||
| Continuity of care provided | 0.152 | <0.001 | ||||||
| Access to care | 0.206 | 0.09 | ||||||
| 20/40 min appointment lengths | −1.285 | 0.10 | 0.088 | 0.95 | −0.619 | 0.29 | 1.018 | 0.43 |
| Years since medical school | −0.033 | 0.54 | 0.137 | 0.09 | 0.037 | 0.32 | −0.136 | <0.001 |
| Female | 2.885 | 0.17 | −10.729 | 0.06 | 1.483 | 0.42 | 1.054 | 0.64 |
| Internal medicine | 2.564 | 0.03 | 3.448 | 0.19 | 0.685 | 0.51 | −0.665 | 0.28 |
| Clinical full-time equivalent | 0.172 | <0.001 | 0.108 | <0.001 | −0.033 | <0.01 | −0.080 | 0.03 |
| Department level | ||||||||
| Staff-to-physician ratio | −1.568 | 0.15 | 3.404 | 0.206 | 1.543 | 0.02 | −0.428 | 0.41 |
| Department size | −0.022 | 0.28 | 0.007 | 0.914 | −0.019 | 0.36 | −0.068 | 0.01 |
| Patient panel level | ||||||||
| Mean Charlson score | 4.464 | 0.39 | 16.837 | 0.02 | 12.831 | <0.001 | 5.007 | 0.15 |
| % Female | −0.051 | 0.23 | 0.267 | 0.02 | −0.015 | 0.69 | 0.007 | 0.90 |
| % Age ≤ 18 | 0.024 | 0.79 | 1.034 | <0.001 | 0.219 | <0.01 | 0.453 | <0.01 |
| % 36 ≤ Age < 50 | −0.166 | 0.03 | 1.008 | <0.001 | 0.122 | <0.01 | 0.150 | 0.52 |
| % 51 ≤ Age < 65 | 0.005 | 0.97 | 0.441 | 0.03 | 0.086 | 0.13 | 0.261 | 0.02 |
| % Age ≥ 65 | 0.029 | 0.84 | −0.192 | 0.59 | −0.200 | 0.04 | 0.221 | 0.45 |
| % Asian | 0.072 | 0.02 | 0.017 | 0.76 | −0.022 | 0.17 | −0.210 | <0.001 |
| % Hispanic | −0.272 | <0.001 | 0.031 | 0.71 | −0.076 | 0.06 | 0.096 | 0.24 |
| % other race | 0.105 | 0.71 | 0.121 | 0.71 | −0.188 | 0.10 | 0.087 | 0.61 |
| % HMO | −0.428 | 0.02 | 0.978 | <0.001 | 0.039 | 0.56 | −0.217 | 0.20 |
| % Medicare PPO | −0.622 | <0.01 | 1.016 | <0.01 | 0.397 | <0.001 | −0.106 | 0.76 |
| % Medicare HMO | 0.571 | 0.11 | 1.272 | 0.09 | −0.190 | 0.48 | −0.602 | 0.22 |
| % Other insurance | −0.225 | 0.12 | 1.016 | <0.001 | 0.247 | <0.01 | −0.116 | 0.69 |
| Division one indicator | −1.110 | 0.27 | −3.224 | 0.27 | −2.963 | <0.001 | 0.465 | 0.71 |
| Division three indicator | 11.245 | <0.001 | −4.023 | 0.05 | −5.778 | <0.001 | −4.946 | 0.09 |
| Constant | 82.493 | <0.001 | −41.504 | 0.003 | −2.413 | 0.26 | 63.246 | <0.001 |
| Log likelihood | −2,596.05 | |||||||
| Observations | 205 | |||||||
The physician was the unit of analysis. The left out variables include: % 19 ≤ Age < 35, % Non-Hispanic White, % PPO, and the Division Two Indicator. Definitions of the variables are provided in Table 1
Table 2 also includes the direct association of the clinical FTE with the patient satisfaction score. The physician’s clinical FTE had a negative significant association (−0.080 % per FTE, p < 0.03). This implies that patients of part-time physicians (50 % FTE) were 4.0 % more likely than the patients of full-time physician’s (100 % FTE) to answer with a “very good” response. Continuity of care provided (0.152 % per continuity %, p < 0.01) was the only other significant physician level process measure, with a one standard deviation (14.0 %) increase associated with a 2.1 % improvement in patient satisfaction scores. Physicians who worked fewer clinical FTEs and who cared for more of their own patients received higher patient satisfaction scores, regardless of their patient’s continuity of care received or access to care.
Table 3 displays the direct, indirect, and total association of a physician’s clinical FTE with the patient satisfaction score. We found that the indirect relationships through both the continuity of care received and access to care were not significant (p = 0.36 and p = 0.11, respectively), but the continuity of care provided was a significant mediator (0.016, p < 0.01). Therefore, the total relationship of the clinical FTE with patient satisfaction (−0.053 % per FTE, p = 0.03) was less than the direct association (−0.080 % per FTE, p = 0.03). See the appendices available online for sensitivity analyses results from simple linear regressions and multi-level models.
Table 3.
The Direct, Indirect, and Total Association of a Physician’s Clinical Full-Time Equivalent with the Press Ganey Patient Satisfaction with Physician Score, 2010
| Direct association | Indirect association | Total association | |||
|---|---|---|---|---|---|
| Continuity of care received | Continuity of care provided | Access to care | |||
| Coeff | −0.080 | 0.017 | 0.016 | −0.006 | −0.053 |
| p value | 0.03 | 0.36 | <0.01 | 0.11 | 0.03 |
These estimates are based on the results in Table 2. The total association is the sum of the direct and the indirect associations
DISCUSSION
This is the first study to simultaneously estimate the relationships between a physician’s clinical work hours, continuity of care measures, access to care, and patient satisfaction with the physician. We found empirical evidence consistent with the argument that full-time physicians provide better access and continuity of care.9–12,16 However, contrary to much of the previous literature,17–19 our findings also suggest that physicians with lower clinical FTEs had higher patient satisfaction scores, after accounting for direct and indirect associations with continuity and access to care measures. Overall, this work suggests that PCPs who choose to work fewer clinical hours may have worse continuity and access outcomes, but they may provide a better patient experience.
Study Limitations
A limitation of this research is the cross-sectional design, which only identifies associations. An alternative explanation of the observed relation between clinical FTE and patient satisfaction is that both are associated with some unmeasured physician characteristics, such as empathy or communication skills.
This study used physician panel level information of patient characteristics and not the respondents’ actual characteristics. This requires the assumption that both the patients who were sampled and who responded adequately represented the physician’s panel. If some response rates differed based on patient characteristics that are associated with patient satisfaction (e.g., race/ethnicity), our panel level adjustments may be insufficient. In studies of patient satisfaction with hospital care, response rates have varied according to patient demographics and disease.43 The response rate of 21.2 % (albeit similar to the national Press Ganey response rate) raises the possibility that nonresponse bias may impact these findings. We were not able to compare the characteristics of respondents with non-respondents in our sample.
Our results may be limited to larger medical practices that have already adopted policies supporting part-time physicians. In the 2010 AMGA survey, 37 % of PCPs in the medical group strongly agreed that the medical group is supportive of providers who choose to work part-time compared to the national average of 17 % for all providers. Shorter hours may raise additional difficulties for physicians in hospital-based or smaller practices, and may not produce the same patient satisfaction results.
Implications
In the face of the projected shortage of PCPs, employers could be more supportive of physicians choosing to work reduced clinical hours to increase provider supply. Physician recruitment and retention might be improved with greater options to work reduced clinical hours44,45 due to the changing demographic of physicians and the association between patient and physician satisfaction.21 An increasing number of medical societies and other stakeholders are becoming more publicly supportive of part-time physicians.44
The different care attributes associated with a provider’s clinical work hours raise questions for primary care redesign efforts. Continuity, access, and satisfaction are all important elements of patient-centered care and are associated with better clinical outcomes and lower costs.46 As more patients access the health system through electronic media, such as secure messaging, the association of fewer clinical office hours with worse continuity and access could be diminished. Team-based primary care models might also reduce the burden from caring for complex patients so that providers do not feel so overworked.12 Such efforts can foster an environment that allows physicians to better address their patients’ needs, at a lower personal cost.
Electronic supplementary material
(PDF 366 kb)
Acknowledgements
The work was generously funded by AHRQ R18 HS019167. The authors would like to thank Sonja Huang for her research assistance.
Conflict of Interest
The authors have no conflict of interest, financial or otherwise.
REFERENCES
- 1.Satiani B, Williams TE, Brod H, Way DP, Ellison EC. A review of trends in attrition rates for surgical faculty: a case for a sustainable retention strategy to cope with demographic and economic realities. J Am Coll Surg. 2013;216(5):944–953. doi: 10.1016/j.jamcollsurg.2012.12.052. [DOI] [PubMed] [Google Scholar]
- 2.Shanafelt T, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 3.Shiotani LM, Parkerton PH, Wenger NS, Needleman J. Internal medicine work hours: trends, associations, and implications for the future. Am J Med. 2008;121(1):80–85. doi: 10.1016/j.amjmed.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 4.New York Times. Don’t Quit This Day Job. Available at: http://www.nytimes.com/2011/06/12/opinion/12sibert.html?pagewanted=all&_r=0. Accessed October 29, 2014.
- 5.Petterson SM, Liaw WR, Phillips RL, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010–2025. Ann Fam Med. 2012;10(6):503–509. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berry-Millett R, Bandara S, Bodenheimer T. The health care problem no one’s talking about. J Fam Pract. 2009;35(12):633. [PubMed] [Google Scholar]
- 7.Bodenheimer T, Pham H. Primary care: current problems and proposed solutions. Health Aff. 2010;29(5):799. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 8.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953–957. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bodenheimer T. Coordinating care—a perilous journey through the health care system. N Engl J Med. 2008;358(10):8. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 10.Bodenheimer T. Transforming practice. N Engl J Med. 2008;359(20):2086–2089. doi: 10.1056/NEJMp0805631. [DOI] [PubMed] [Google Scholar]
- 11.Nutting PA, Crabtree BF, Stewart EE, et al. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med. 2010;8(Suppl 1):S33–S44. doi: 10.1370/afm.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grumbach K, Bodenheimer T. A primary care home for Americans: putting the house in order. JAMA. 2002;288(7):889–893. doi: 10.1001/jama.288.7.889. [DOI] [PubMed] [Google Scholar]
- 13.Kapinos KA, Fitzgerald P, Greer N, Rutks I, Wilt TJ. The Effect of working conditions on patient care: a systematic review. Department of Veterans Affairs; 2012. [PubMed]
- 14.Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–203. doi: 10.1056/NEJMp1211775. [DOI] [PubMed] [Google Scholar]
- 15.Egger MJ, Day J, Scammon DL, Li Y, Wilson A, Magill MK. Correlation of the Care by Design primary care practice redesign model and the principles of the patient-centered medical home. J Am Board Fam Med. 2012;25(2):216–223. doi: 10.3122/jabfm.2012.02.110159. [DOI] [PubMed] [Google Scholar]
- 16.Murray A, Safran DG, Rogers WH, Inui T, Chang H, Montgomery JE. Part-time physicians. Physician workload and patient-based assessments of primary care performance. Arch Fam Med. 2000;9(4):327. doi: 10.1001/archfami.9.4.327. [DOI] [PubMed] [Google Scholar]
- 17.Fairchild DG, McLoughlin KS, Gharib S, et al. Productivity, quality, and patient satisfaction. N Engl J Med. 2001;16(10):663–667. doi: 10.1111/j.1525-1497.2001.01111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parkerton PH, Wagner EH, Smith DG, Straley HL. Effect of part-time practice on patient outcomes. J Gen Intern Med. 2003;18(9):717–724. doi: 10.1046/j.1525-1497.2003.20401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mechaber HF, Levine RB, Manwell LB, Linzer M. Part-time physicians… prevalent, connected, and satisfied. J Gen Intern Med. 2008;23(3):300–303. doi: 10.1007/s11606-008-0514-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McMurray JE, Heiligers PJ, Shugerman RP, et al. Part-time medical practice: where is it headed? Am J Med. 2005;118(1):87–92. doi: 10.1016/j.amjmed.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15(2):122–128. doi: 10.1046/j.1525-1497.2000.02219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barnett RC, Gareis KC, Carr PL. Career satisfaction and retention of a sample of women physicians who work reduced hours. J Womens Health (Larchmt) 2005;14(2):146–153. doi: 10.1089/jwh.2005.14.146. [DOI] [PubMed] [Google Scholar]
- 23.Warde C. Time is of the essence. J Gen Intern Med. 2001;16(10):712–713. doi: 10.1046/j.1525-1497.2001.08020.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hall JA, Dornan MC. Patient sociodemographic characteristics as predictors of satisfaction with medical care: a meta-analysis. Soc Sci Med. 1990;30(7):811–818. doi: 10.1016/0277-9536(90)90205-7. [DOI] [PubMed] [Google Scholar]
- 25.Roter DL, Stewart M, Putnam SM, Lipkin M, Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA. 1997;277(4):350–356. doi: 10.1001/jama.1997.03540280088045. [DOI] [PubMed] [Google Scholar]
- 26.Roberts NA, Levenson RW. The remains of the workday: impact of job stress and exhaustion on marital interaction in police couples. J Marriage Fam. 2001;63(4):1052–1067. doi: 10.1111/j.1741-3737.2001.01052.x. [DOI] [Google Scholar]
- 27.Keller RT. Cross-functional project groups in research and new product development: diversity, communications, job stress, and outcomes. Acad Manag J. 2001;44(3):547–55.
- 28.Adler R, Vasiliadis A, Bickell N. The relationship between continuity and patient satisfaction: a systematic review. Fam Pract. 2010;27(2):171–178. doi: 10.1093/fampra/cmp099. [DOI] [PubMed] [Google Scholar]
- 29.Murray M, Bodenheimer T, Rittenhouse D, Grumbach K. Improving timely access to primary care: case studies of the advanced access model. JAMA. 2003;289(8):1042–1046. doi: 10.1001/jama.289.8.1042. [DOI] [PubMed] [Google Scholar]
- 30.Nutting PA, Goodwin MA, Flocke SA, Zyzanski SJ, Stange KC. Continuity of primary care: to whom does it matter and when? Ann Fam Med. 2003;1(3):149–155. doi: 10.1370/afm.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kroneman MW, Maarse H, van der Zee J. Direct access in primary care and patient satisfaction: a European study. Health Policy. 2006;76(1):72–79. doi: 10.1016/j.healthpol.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 32.Elliot VS. American Medical Association. More doctors work part time, flexible schedules. Available at: http://www.amednews.com/article/20120326/business/303269974/1/. Accessed October 29, 2014.
- 33.U.S. Census Bureau. Profiles of General Demographic Characteristics, 2000 Census of Population and Housing. 2001. Available at: http://www.census.gov/prod/cen2000/dp1/2khus.pdf. Accessed October 29, 2014.
- 34.Salisbury C, Sampson F, Ridd M, Montgomery AA. How should continuity of care in primary health care be assessed? Br J Gen Pract. 2009;59(561):e134–e141. doi: 10.3399/bjgp09X420257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murray M, Davies M, Boushon B. Panel size: how many patients can one doctor manage? Fam Pract Manag. 2007;14(4):44–51. [PubMed] [Google Scholar]
- 36.Murray M, Berwick D. Advanced access: reducing waiting and delays in primary care. JAMA. 2003;289(8):1035–1040. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- 37.Bertakis KD. The influence of gender on the doctor-patient interaction. Patient Educ Couns. 2009;76(3):356–360. doi: 10.1016/j.pec.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 38.Gross DA, Zyzanski SJ, Borawski EA, Cebul RD, Stange KC. Patient satisfaction with time spent with their physician. J Fam Pract. 1998;47(2):133–137. [PubMed] [Google Scholar]
- 39.Hall J, Irish J, Roter D, Ehrlich C, Miller L. Satisfaction, gender, and communication in medical visits. Med Care. 1994;32(12):1216–1231. doi: 10.1097/00005650-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Hall JA, Dornan MC. Meta-analysis of satisfaction with medical care: description of research domain and analysis of overall satisfaction levels. Soc Sci Med. 1988;27(6):637–644. doi: 10.1016/0277-9536(88)90012-3. [DOI] [PubMed] [Google Scholar]
- 41.Sixma HJ, Spreeuwenberg PM, van der Pasch MA. Patient satisfaction with the general practitioner: a two-level analysis. Med Care. 1998;36(2):212–229. doi: 10.1097/00005650-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 43.Spooner SH. Survey response rates and overall patient satisfaction scores: what do they mean? J Nurs Care Qual. 2003;18(3):162–174. doi: 10.1097/00001786-200307000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Linzer M, Warde C, Alexander RW, et al. Part-time careers in academic internal medicine: a report from the association of specialty professors part-time careers task force on behalf of the alliance for academic internal medicine. Acad Med. 2009;84(10):1395–1400. doi: 10.1097/ACM.0b013e3181b6bf8c. [DOI] [PubMed] [Google Scholar]
- 45.Satiani B, Williams T, Ellison E. The impact of employment of part-time surgeons on the expected surgeon shortage. J Am Coll Surg. 2011;213(3):345–351. doi: 10.1016/j.jamcollsurg.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 46.Paustian ML, Alexander JA, El Reda DK, Wise CG, Green LA, Fetters MD. Partial and incremental PCMH practice transformation: implications for quality and Costs. Health Serv Res. 2014;49(1):52–74. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 366 kb)