Abstract
BACKGROUND
Alcohol dependence results in multiple hospital readmissions, but no discharge planning protocol has been studied to improve outcomes. The inpatient setting is a frequently missed opportunity to discuss treatment of alcohol dependence and initiate medication-assisted treatment, which is effective yet rarely utilized.
AIM
Our aim was to implement and evaluate a discharge planning protocol for patients admitted with alcohol dependence.
SETTING
The study took place at the San Francisco General Hospital (SFGH), a university-affiliated, large urban county hospital.
PARTICIPANTS
Learner participants included Internal Medicine residents at the University of California, San Francisco (UCSF) who staff the teaching service at SFGH. Patient participants included inpatients with alcohol dependence admitted to the Internal Medicine teaching service.
PROGRAM DESCRIPTION
We developed and implemented a discharge planning protocol for patients admitted with alcohol dependence that included eligibility assessment and initiation of medication-assisted treatment.
PROGRAM EVALUATION
Rates of medication-assisted treatment increased from 0 % to 64 % (p value < 0.001). All-cause 30-day readmission rates to SFGH decreased from 23.4 % to 8.2 % (p value = 0.042). All-cause emergency department visits to SFGH within 30 days of discharge decreased from 18.8 % to 6.1 % (p value = 0.056).
DISCUSSION
Through implementation of a discharge planning protocol by Internal Medicine residents for patients admitted with alcohol dependence, there was a statistically significant increase in medication-assisted treatment and a statistically significant decrease in both 30-day readmission rates and emergency department visits.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-2968-9) contains supplementary material, which is available to authorized users.
KEY WORDS: alcoholism and addictive behavior, care transitions, medical student and residency education, substance abuse, medical education-clinical skills training
INTRODUCTION
Alcohol use disorders are a common problem in the United States and frequently go untreated. According to the National Survey on Drug Use and Health in 2012,1 only 13.5 % of people with alcohol use disorders received any type of treatment, most of which were in self-help groups. Less than 10 % reported treatment in a hospital or clinic based setting.
At San Francisco General Hospital (SFGH), a large urban county hospital, patients with alcohol dependence have high admission and readmission rates. From 1 July 2010 to 30 June 2011, 24.5 % (973/3,967) of patients discharged from the Internal Medicine service had at least one ICD-9 code related to alcohol. These patients were 1.58 times more likely to be readmitted to SFGH within 30 days (19 % versus 12 %). Alcohol-related complications sit atop the list of reasons for readmission to SFGH, alongside congestive heart failure, chronic obstructive pulmonary disease (COPD) and diabetes-related complications. While the development of discharge planning bundles and systematic approaches have been studied extensively to tackle readmission rates for these other top reasons for readmission,2–7 no such study exists for alcohol-related admissions. This is the first such paper to describe the design and implementation of a discharge planning protocol aimed to decrease readmission rates for those with alcohol dependence.
Inpatient hospitalization is a critical but frequently missed opportunity to discuss treatment of alcohol dependence. An inpatient stay addresses the acute illness, but often fails to tackle the underlying reason for admission: the alcohol dependence.8 Referrals to social services or behavioral counseling may be offered, but these are often insufficient to treat dependence and ensure a safe discharge. Medication-assisted treatment is one important component of alcohol dependence management. Compared to either alone, the addition of pharmacotherapy to psychosocial treatment improves outcomes.9 Medications can help relieve cravings and symptoms of protracted withdrawal and allow neurons to readapt to a nonalcoholic state.10 This helps patients increase motivational readiness for change, leading to longer periods of abstinence.11
The Food and Drug Administration (FDA) has approved four medications for the treatment of alcohol dependence: two forms of naltrexone (oral and extended-release injectable),12–17 acamprosate,18–21 and disulfiram.22,23 There are data to support the safety and efficacy of all of these medications.24 In particular, many experts consider naltrexone first-line therapy for alcohol dependence, given its proven efficacy and safety profile, both during supervised withdrawal and in the primary care setting.25,26
Despite availability, these medications are extremely underutilized. In a US Department of Veterans Affairs (VA) healthcare system, only 1.9 % of patients with alcohol dependence were prescribed naltrexone.27 A national survey of US physicians who treat addictions showed that only 3–13 % use pharmacotherapy for the treatment of alcohol dependence.28 Although physicians demonstrate low prescribing patterns, a majority of patients with alcohol dependence report an interest in medication-assisted treatment.29
Here we report on the design, implementation, and results of a discharge planning protocol that includes guidance on medication-assisted treatment, for Internal Medicine residents to use when discharging patients with alcohol dependence.
Setting and Participants
This study took place at the San Francisco General Hospital (SFGH), a 460-bed, university-affiliated, urban county hospital. Learner participants included Internal Medicine residents at the University of California, San Francisco (UCSF) who staff the teaching service at SFGH. Patient participants included SFGH patients with alcohol dependence admitted to the Internal Medicine teaching service in March 2012, when the discharge planning protocol was implemented. Admission data as well as data one month after discharge were collected for patients admitted to SFGH in June 2011 (pre-intervention) and March 2012 (post-intervention).
Project Description
Every month, 15 UCSF Internal Medicine residents admit an average of 275 patients to the teaching service at SFGH. As part of their ambulatory care didactics, residents receive a dedicated curriculum on Screening, Brief Intervention, and Referral to Treatment (SBIRT). SBIRT is an evidence-based, comprehensive, outpatient approach to identifying and treating persons with substance use disorders or those at risk of developing these disorders.30–32
To improve the treatment of alcohol dependence in the inpatient setting, a pilot educational intervention and discharge planning protocol was implemented in March 2012. This intervention was designed around information gathered during a focus group that sought to identify the biggest barriers to treatment of alcohol dependence in the inpatient setting. The focus group included Internal Medicine residents, attending physicians, pharmacists, medical social workers and substance abuse counselors in the community. The biggest barriers identified included lack of knowledge about efficacy and safety of medication options, availability of medications on hospital formulary, limited time to discuss with patients, and lack of primary care or follow-up.
To address these barriers, all 15 residents on the medicine service in March 2012 participated in an hour-long session, during regular didactic time, on treatment of alcohol dependence, including medication-assisted treatment. The education focused on the efficacy and safety of naltrexone, a medication already approved on formulary at SFGH. A partnership was also solidified with the Treatment Access Program (TAP), an assessment, referral and placement center in San Francisco for individuals with mental health and substance use disorders. If patients did not have a primary care provider or could not see their provider within 2 weeks, an appointment could be made with a TAP counselor for follow-up and medication refills.
During the month of March 2012, all residents were instructed to fill out the discharge planning tool (see online appendix) for all patients admitted with an alcohol-related diagnosis. The tool included an algorithm to prompt residents to discuss alcohol use, screen for naltrexone eligibility and contraindications (severe liver disease and opioid use/dependence), assess patient preferences and arrange follow-up. It included phone numbers to the Treatment Access Program for referrals and a detachable patient information sheet. Social workers also prompted the teams to complete these discharge planning tools during daily multidisciplinary/discharge planning rounds. As with all discharge medications at SFGH, a 30-day supply was given upon discharge to all patients who were prescribed naltrexone. The UCSF institutional review board approved of this study.
Program Evaluation
Patient data was gathered from the electronic health record and compared before and after implementation of the discharge planning protocol (June 2011 versus March 2012). Baseline patient characteristics were similar in both groups (see Table 1). Most of the patients were male and white, though Hispanic patients made up a large minority. More than half of patients were homeless or marginally housed. Most patients consumed greater than 21 drinks per week and more than 20 % had received prior alcohol treatment. Both groups had similar rates of comorbid disorders, including opioid and stimulant use disorders, mood or anxiety disorders, diabetes, hypertension, and human immunodeficiency virus (HIV).
Table 1.
Characteristics of the Patients at Baseline
| Characteristics | Pre-intervention Group (June 2011) N = 64 | Intervention Group (March 2012) N = 49 | p Values* |
|---|---|---|---|
| Age – year (mean +/− SD) | 47.1+/−11.2 | 48.9 +/− 10.5 | 0.23 |
| Male Sex – no. (%) | 53 (82.8) | 44 (89.8) | 0.43 |
| Race or ethnic group – no. (%) | 0.19 | ||
| Black | 12 (18.8) | 4 (8.2) | |
| Native American | 1 (1.6) | 4 (8.2) | |
| Asian or Pacific | 2 (3.1) | 3 (6.1) | |
| White | 34 (53.1) | 21 (42.9) | |
| Hispanic | 13 (20.3) | 14 (28.6) | |
| Other | 2 (3.1) | 3 (6.1) | |
| Housing – no. (%) | 0.99 | ||
| Housed | 23 (35.9) | 18 (36.7) | |
| Marginally Housed | 13 (20.3) | 10 (20.4) | |
| Homeless | 28 (43.8) | 21 (42.9) | |
| Alcohol use upon admission – no. (%) | 0.78 | ||
| < 7 drinks/week | 5 (7.8) | 2 (4.1) | |
| 7–14 drinks/week | 0 (0) | 0 (0) | |
| 14–21 drinks/week | 6 (9.4) | 3 (6.1) | |
| > 21 drinks/week | 44 (68.8) | 39 (79.6) | |
| Not Recorded | 9 (14.1) | 5 (10.2) | |
| Prior Alcohol Treatment†− no. (%) | 15 (23.4) | 11 (22.4) | 0.92 |
| Opioid abuse/dependence – no. (%) | |||
| Past | 8 (12.5) | 3 (6.1) | 0.49 |
| Current | 5 (7.8) | 3 (6.1) | |
| None | 51 (79.7) | 43 (87.8) | |
| Stimulant use – no. (%) | 0.36 | ||
| Past | 4 (6.3) | 2 (4.1) | |
| Current | 12 (18.8) | 5 (10.2) | |
| None | 48 (75.0) | 42 (85.7) | |
| Mood Disorder – no. (%) | 19 (29.7) | 12 (24.5) | 0.69 |
| Anxiety Disorder – no. (%) | 8 (12.5) | 5 (10.2) | 0.77 |
| Human immunodeficiency virus (HIV) – no (%) | 8 (12.5) | 4 (8.2) | 0.55 |
| Diabetes – no. (%) | 5 (7.8) | 9 (18.4) | 0.15 |
| Hypertension – no. (%) | 10 (15.6) | 13 (26.5) | 0.23 |
* p values are based on F-tests for the continuous variables and on Fisher’s exact tests or chi-square tests for the categorical variables
† Prior alcohol treatment includes pharmacotherapy, rehabilitation, peer support groups and/or other counseling specifically around alcohol use
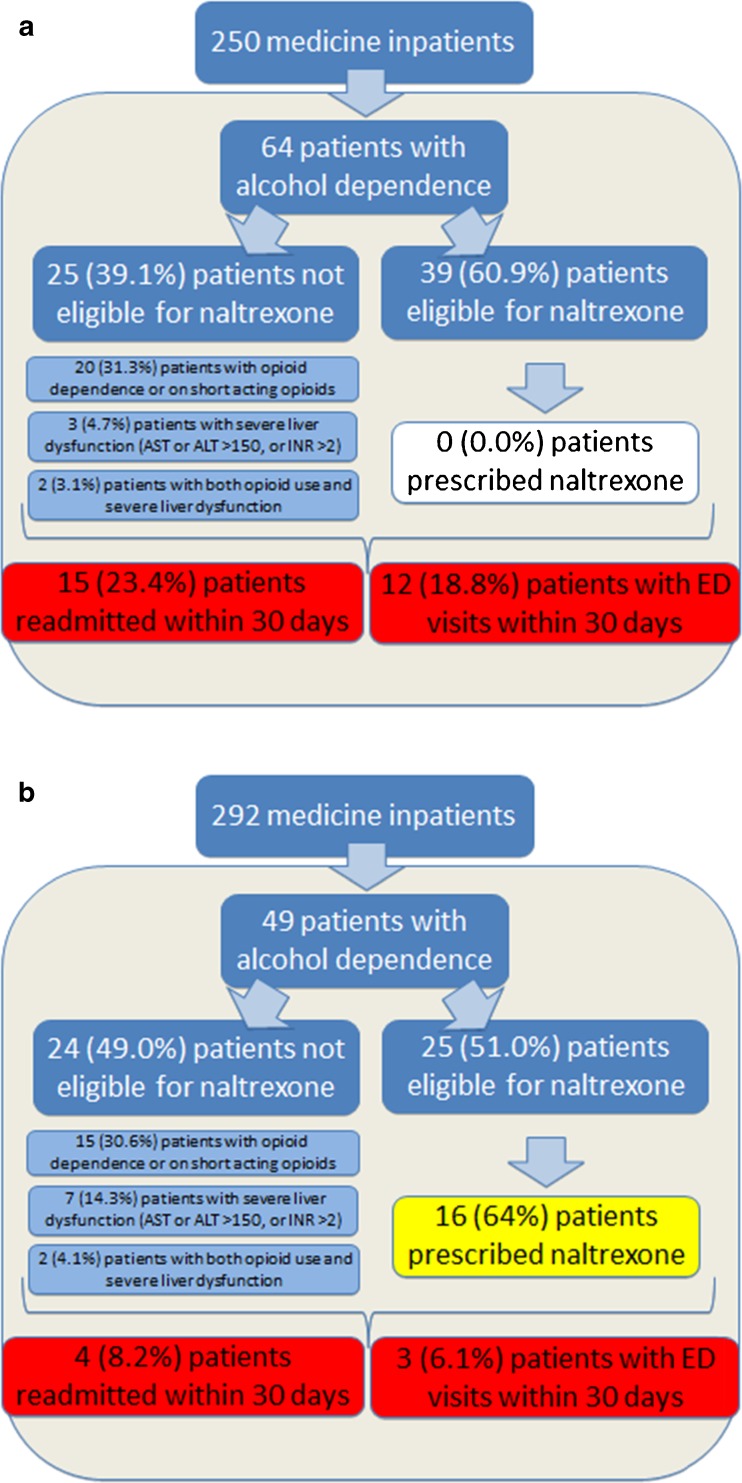
The total number of patients with alcohol dependence was identified through chart review according to the Diagnostic and Statistical Manual of Mental Disorders IV (DSM IV) criteria. Of those patients with alcohol dependence, the number of patients who would be candidates for naltrexone pharmacotherapy (based on documentation of liver function tests and no recent opioid use) was also compared before and after intervention. (see Fig. 1a). Pre-intervention, 39.1 % (25/64) of patients were not eligible for naltrexone (20 due to opioid dependence or short-term opioid use, three due to severe liver function test abnormalities, and two due to both contraindications). The remaining 60.9 % (39/64) of patients were eligible for naltrexone.
Figure 1.
Comparison of pre-intervention group (June 2011) (a), and post-intervention group (March 2012) (b). This figure breaks down the characteristics of all patients with alcohol dependence admitted during the two comparison months. Regarding eligibility criteria for treatment with naltrexone, over 50 % of patients in both groups were eligible for treatment. The primary process measure was the percent of those patients eligible for naltrexone who were prescribed naltrexone. This increased from 0 % to 64 % (p < 0.001) after the intervention. For the primary outcome measures, the rate of readmissions within 30 days decreased from 23.4 % to 8.2 % (p = 0.042) and the rate of patients with emergency department (ED) visits within 30 days decreased from 18.8 % to 6.1 % (p = 0.056).
After implementation of the discharge planning tool in March 2012 (see Fig. 1b), 49.0 % (24/49) of patients were not eligible for naltrexone (15 due to opioid dependence or short-term opioid use, seven due to severe liver function test abnormalities, and two due to both contraindications). The remaining 51.0 % (25/49) of patients were eligible for naltrexone.
The primary process measure compared the rate of prescription of naltrexone pharmacotherapy among those eligible patients. Pre-intervention, 0 % (0/39) of eligible patients were prescribed naltrexone during the inpatient stay or upon discharge. After the intervention, 64 % (16/25) of eligible patients were prescribed naltrexone (p < 0.001). All of the remaining eligible patients declined the medication, either because they preferred other treatment options or were not yet ready to change their alcohol use.
The primary outcome measures compared rates of all-cause emergency department (ED) visits and inpatient readmissions within 30 days of discharge. Of all patients with alcohol dependence discharged pre-intervention, 23.4 % (15/64) were readmitted to SFGH within 30 days of discharge, compared with 8.2 % (4/49) post-intervention (p value = 0.042). Before the intervention, 18.8 % (12/64) of patients had visits to the SFGH ED within 30 days (but were not readmitted), compared with 6.1 % (3/49) after intervention (p value = 0.056).
Of those patients who were eligible for naltrexone pre-intervention, 38.5 % (15/39) were readmitted or had an ED visit versus 12.0 % (3/25) post-intervention (p value = 0.025). Two of three in the latter group had been prescribed naltrexone. Of those patients who were not eligible for naltrexone pre-intervention, 48 % (12/25) were readmitted or had an ED visit versus 16.7 % (4/24) post-intervention (p value = 0.032).
Most of the reasons for readmission or presentation to the ED were alcohol-related: 74.1 % (20/27) in the pre-intervention group compared to 85.7 % (6/7) in the post-intervention group (p value = 1.0).
Among those with mood and/or anxiety disorders, high rates of readmission or ED visits within 30 days were seen both pre-intervention (44.4 %, 12/27) and post-intervention (46.2 %, 6/13) (p value = 1.0).
DISCUSSION
This is the first paper to describe an intervention in which Internal Medicine residents were able to implement a discharge planning protocol to improve treatment of alcohol dependence in the inpatient setting. After the intervention, rates of naltrexone prescription increased significantly, and readmission rates and ED visits within 30 days of discharge decreased by two-thirds. Although the decrease in readmissions and ED visits was greatest in the group eligible for naltrexone, there was a statistically significant decrease in those who were not eligible as well. This suggests that there were multiple factors contributing to improved outcomes. The protocol not only promoted increased rates of medication-assisted treatment, but also improved interdisciplinary collaboration and streamlined outpatient referrals. It enhanced patient–provider communication around alcohol use and allowed residents to employ motivational interviewing techniques learned during the SBIRT curriculum. A combination of all of these elements played a role in decreasing readmission rates and visits to the ED. This study, however, also shows that the discharge planning protocol was not as effective in improving outcomes for the subset of patients with mood and/or anxiety disorders, suggesting that these groups have unique needs that may require a modified discharge protocol.
This study has several limitations. First, this is not a randomized controlled trial, as we compared two groups at different points in time. Thus, the implementation of the discharge planning protocol and the decrease in readmission rates and ED visits cannot be proven as causally related. There were no statistically significant differences between the two groups based on measured baseline characteristics, but it is possible that there were unmeasured variables that may have contributed to the differences in outcomes. In addition, the outcomes were measured immediately after initiation of the intervention, which does not allow for extrapolation to a sustained or longer-term outcome. Finally, the primary outcome measures of readmission rates and visits to the ED only apply to SFGH. We were unable to determine if patients presented to other hospitals in San Francisco. Data, however, was collected using the SFGH electronic health records in the same way before and after intervention, presumably excluding similar data in both sets.
Despite these limitations, this study of a discharge planning protocol for alcohol dependent patients is one of the first to tackle the problem of alcohol dependence in the inpatient setting using the same systems-based approaches being studied for other leading reasons for hospital readmission. Our discharge planning protocol builds on the SBIRT curriculum to help teach Internal Medicine residents how to address alcohol dependence in the inpatient setting through combined use of counseling and pharmacotherapy. With these tangible tools in hand, providers can be a more active part of the solution. Alcohol dependence needs to be treated like other medical diseases, utilizing evidence-based approaches to treatment and prevention. This study is an additional step in that direction.
Electronic supplementary material
(DOCX 28 kb)
Acknowledgements
We would like to thank the University of California, San Francisco Internal Medicine residents for their participation. We would also like to thank Jenee Bryant, MSW, Katie Luttrell, MSW, Amy Logan, Pharm.D., David Hersh, MD, Paula Lum, MD, and Richard Brooks, MD for their support throughout this project.
Funders
None.
Prior Presentations
We presented an earlier version of the manuscript as a poster for the University of California, San Francisco Quality and Safety Symposium on 29 May 2012. This abstract was also presented for the Association of Medical Education and Research in Substance Abuse (AMERSA) conference on 3 November 2012.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality . Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2012. [Google Scholar]
- 2.Amarasingham R, Patel PC, Toto K, et al. Allocating scarce resources in real-time to reduce heart failure readmissions: a prospective, controlled study. BMJ Qual Saf. 2013;22(12):998–1005. doi: 10.1136/bmjqs-2013-001901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ryan J, Kang S, Dolacky S, Ingrassia J, Ganeshan R. Change in readmissions and follow-up visits as part of a heart failure readmission quality improvement initiative. Am J Med. 2013;126(11):989–994. doi: 10.1016/j.amjmed.2013.06.027. [DOI] [PubMed] [Google Scholar]
- 4.Lainscak M, Kadivec S, Kosnik M, et al. Discharge coordinator intervention prevents hospitalizations in patients with COPD: a randomized controlled trial. J Am Med Dir Assoc. 2013;14(6):450e1–6. doi: 10.1016/j.jamda.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Hopkinson NS, Englebretsen C, Cooley N, et al. Designing and implementing a COPD discharge care bundle. Thorax. 2012;67(1):90–2. doi: 10.1136/thoraxjnl-2011-200233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen JY, Ma Q, Chen H, Yermilov I. New bundled world: quality of care and readmission in diabetes patients. J Diabetes Sci Technol. 2012;6(3):563–71. doi: 10.1177/193229681200600311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Healy SJ, Black D, Harris C, Lorenz A, Dungan KM. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care. 2013;36(10):2960–7. doi: 10.2337/dc13-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stewart S, Swain S. Assessment and management of alcohol dependence and withdrawal in the acute hospital. Clin Med. 2012;12(3):266–71. doi: 10.7861/clinmedicine.12-3-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss RD, Kueppenbender KD. Combining psychosocial treatment with pharmacotherapy for alcohol dependence. J Clin Psychopharmacol. 2006;26(Suppl 1):S37–S42. doi: 10.1097/01.jcp.0000248604.58305.b3. [DOI] [PubMed] [Google Scholar]
- 10.Garbutt JC, West SL, Carey TS, Lohr KN, Crews FT. Pharmacological treatment of alcohol dependence. JAMA. 1999;281:1318–25. doi: 10.1001/jama.281.14.1318. [DOI] [PubMed] [Google Scholar]
- 11.O'Malley SS, Kosten TR. Pharmacotherapy of addictive disorders. In: Miller WR, Carroll KM, editors. Rethinking substance abuse: what the science shows, and what we should do about it. New York: The Guilford Press; 2006. pp. 240–56. [Google Scholar]
- 12.Kranzler HR, Van Kirk J. Efficacy of naltrexone and acamprosate for alcoholism treatment: a meta-analysis. Alcohol Clin Exp Res. 2001;25:1335–41. doi: 10.1111/j.1530-0277.2001.tb02356.x. [DOI] [PubMed] [Google Scholar]
- 13.Srisurapanont M, Jarusuraisin N. Opioid antagonists for alcohol dependence (Review) Cochrane Database Syst Rev. 2005;2(1) doi: 10.1002/14651858.CD001867.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Streeton C, Whelan G. Naltrexone: a relapse prevention maintenance treatment of alcohol dependence: a meta-analysis of randomized controlled trials. Alcohol. 2001;36:544–52. [DOI] [PubMed]
- 15.Pettinati HM, O’Brien CP, Rabinowitz AR, et al. The status of naltrexone in the treatment of alcohol dependence: specific effects on heavy drinking. J Clin Psychopharmacol. 2006;26(6):610–25. doi: 10.1097/01.jcp.0000245566.52401.20. [DOI] [PubMed] [Google Scholar]
- 16.Anton RF, O’Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–17. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- 17.Jones DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311(18):1889–900. doi: 10.1001/jama.2014.3628. [DOI] [PubMed] [Google Scholar]
- 18.Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: a clinical review. J Clin Psychiatry. 2001;62(Suppl 10):42–8. [PubMed] [Google Scholar]
- 19.Soyka M, Chick J. Use of acamprosate and opioid agonists in the treatment of alcohol dependence: a European perspective. Am J Addict. 2003;12(Suppl 1):S69–S80. doi: 10.1111/j.1521-0391.2003.tb00497.x. [DOI] [PubMed] [Google Scholar]
- 20.Yahn SL, Watterson LR, Olive MF. Safety and efficacy of acamprosate for the treatment of alcohol dependence. Subst Abus. 2013;6:1–12. doi: 10.4137/SART.S9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rösner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M. Acamprosate for alcohol dependence. Cochrane Database Syst Rev. 2010;9:1–118. doi: 10.1002/14651858.CD004332.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suh JJ, Pettinati HM, Kampman KM, O’Brien CP. The status of disulfiram: a half of a century later. J Clin Psychopharmacol. 2006;26(3):290–302. doi: 10.1097/01.jcp.0000222512.25649.08. [DOI] [PubMed] [Google Scholar]
- 23.Jorgensen CH, Pederson B, Tonnesen H. The efficacy of disulfiram for the treatment of alcohol use disorder. Alcohol Clin Exp Res. 2011;35(10):1749–58. doi: 10.1111/j.1530-0277.2011.01523.x. [DOI] [PubMed] [Google Scholar]
- 24.US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment . Incorporating Alcohol Pharmacotherapies Into Medical Practice, Treatment Improvement Protocol (TIP) Series, No. 49. Rockville, MD: Center for Substance Abuse Treatment; 2009. [PubMed] [Google Scholar]
- 25.Anton R. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715–21. doi: 10.1056/NEJMct0801733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedmann PD. Alcohol use in adults. N Engl J Med. 2013;368(4):365–73. doi: 10.1056/NEJMcp1204714. [DOI] [PubMed] [Google Scholar]
- 27.Petrakis IL, Leslie D, Rosenheck R. Use of naltrexone in the treatment of alcoholism nationally in the Department of Veterans Affairs. Alcohol Clin Exp Res. 2003;27:1780–4. doi: 10.1097/01.ALC.0000095861.43232.19. [DOI] [PubMed] [Google Scholar]
- 28.Mark TL, Kranzle HR, Song X. Understanding U.S. addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71(3):219–228. doi: 10.1016/S0376-8716(03)00134-0. [DOI] [PubMed] [Google Scholar]
- 29.Stewart SH, Connors GJ. Interest in pharmacotherapy and primary care alcoholism treatment among medically hospitalized, alcohol dependent patients. J Addict Dis. 2007;26(2):63–69. doi: 10.1300/J069v26n02_08. [DOI] [PubMed] [Google Scholar]
- 30.Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28(3):7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- 31.Davoudi M, Rawson RA, Davoudi M, Rawson RA. Screening, brief intervention, and referral to treatment (SBIRT) initiatives in California: notable trends, challenges, and recommendations. J Psychoactive Drugs. 2010;Suppl 6:239–48. doi: 10.1080/02791072.2010.10400547. [DOI] [PubMed] [Google Scholar]
- 32.Hettema JE, Ratanawongsa N, Manuel JK, et al. A SBIRT curriculum for medical residents: development of a performance feedback tool to build learner confidence. Subst Abus. 2012;33(3):241–50. doi: 10.1080/08897077.2011.640172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 28 kb)