Abstract
OBJECTIVE:
To evaluate the impact of a clinical pharmacy program on health outcomes in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital in Brazil.
METHOD:
A randomized controlled trial with a 6-month follow-up period was performed in 70 adults, aged 45 years or older, with type 2 diabetes who were taking insulin and who had an HbA1c level ≥8%. Patients in the control group (CG) (n = 36) received standard care, patients in the intervention group (IG) (n = 34) received an individualized pharmacotherapeutic care plan and diabetes education. The primary outcome measure was change in HbA1c. Secondary outcomes included diabetes and medication knowledge, adherence to medication, insulin injection and home blood glucose monitoring techniques and diabetes-related quality of life. Outcomes were evaluated at baseline and 6 months using questionnaires.
RESULTS:
Diabetes knowledge, medication knowledge, adherence to medication and correct insulin injection and home blood glucose monitoring techniques significantly improved in the intervention group but remained unchanged in the control group. At the end of the study, mean HbA1c values in the control group remained unchanged but were significantly reduced in the intervention group. Diabetes-related quality of life significantly improved in the intervention group but worsened significantly in the control group.
CONCLUSION:
The program improved health outcomes and resulted in better glycemic control in patients with type 2 diabetes undergoing insulin therapy.
Keywords: Diabetes Mellitus Type 2, Medication Adherence, Clinical Pharmacy Services, Self-Management, Outpatient Care
INTRODUCTION
Diabetes mellitus (DM) is one of the most common non-communicable diseases globally. In 2011, it was estimated that 366 million people worldwide had DM, corresponding to a global prevalence of 8.3%. Type 2 DM (T2DM) accounts for the majority of these cases and 80% of people with DM live in low- and middle-income countries (1). A recent study estimated the prevalence of DM in Brazil at 5.6% (2).
The management of T2DM is complex, requiring long-term continuous medical care and significant effort by the patient regarding self-management activities (3). To enable effective management of DM, multidisciplinary team approaches are necessary and must rely on a well-established relationship between an informed and involved patient and a proactive team (3,4).
It is essential in this collaborative and integrated team approach that individuals with diabetes assume an active role in their care. Various strategies and techniques should be used by professionals to provide adequate education on and to support the development of problem-solving skills in various aspects of diabetes management. Any plan should recognize diabetes self-management education and ongoing diabetes support as integral components of care. Diabetes self-management education is the continuous process of facilitating the knowledge, skills and abilities necessary for diabetes self-care. The objectives of this educational approach are to support informed decision-making, self-care behaviors, problem-solving and active collaboration with the health care team to improve clinical outcomes, health status and quality of life (3,4).
The expansion of the diabetes educator role to other professionals, such as pharmacists, has been recognized (3-6). Moreover, pharmacists are uniquely positioned to educate patients on the appropriate utilization of medication through the elaboration, implementation and monitoring of pharmacotherapeutic plans intended to produce specific outcome improvements (3,5,7).
MATERIALS AND METHODS
Study design
The study was a randomized controlled trial (RCT) with a 6-month follow-up period. It was performed in the diabetes outpatient clinic of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, which is a tertiary facility hospital located in the city of São Paulo, Brazil.
Patients were included in the study if they were aged 45 years or older, diagnosed with T2DM and on prescription insulin and if they had an HbA1c level exceeding 8%. Patients were not included if they were unable to develop self-management activities and/or they had participated in DM educational programs in the last 3 months.
Eligible patients were invited to participate and for those who accepted, additional information was provided before they were asked to sign the study's consent form. After recruitment, patients were randomly assigned to one of two groups: the control group (CG) or the intervention group (IG). The group allocations were assigned by simple randomization.
After randomization, all patients were individually interviewed to obtain socio-demographic information, a clinical history of diabetes and information on current medication use. Assessments of diabetes and medication knowledge, adherence to medication, insulin injection and home blood glucose monitoring techniques, HbA1c values and diabetes-related quality of life were also performed.
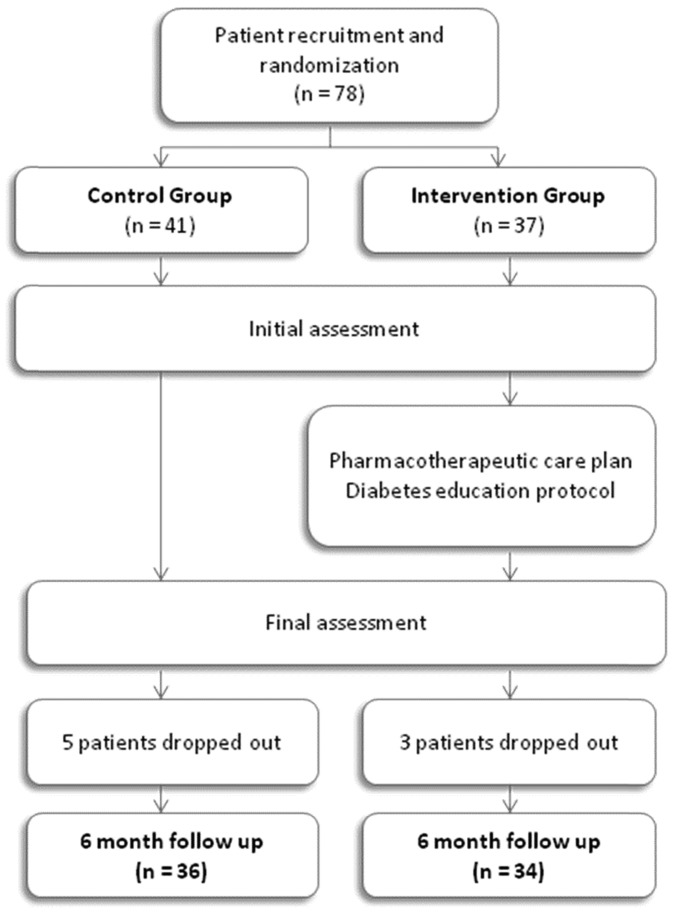
Patients in the IG had monthly individual appointments and those in the CG were observed at the initial and final assessments (Figure 1).
Figure 1.
Flow chart showing the various phases of the study.
Patients randomized to the CG received standard care during the study period. Although they did not receive advice from the clinical pharmacist, they were allowed to request information anytime during the study.
Interventions
For each patient randomized to the IG, an individualized pharmacotherapeutic care plan (PCP) was designed based on necessities identified in the first interview. Advice focused on indication, proper dosage, side effects and adequate storage of medication. Pill organizers were given to each patient along with verbal directions on their assembly. Written guidance on prescriptions was provided at each consult. Additionally, a diabetes education protocol was developed to provide basic information on acute and chronic complications, the importance of lifestyle changes (healthy diet, physical activity, smoking cessation), regular foot inspections, the importance of home blood glucose monitoring and other topics. Clinical pharmacist recommendations, such as insulin dose adjustments, were discussed with the physician when necessary.
Outcomes
The primary outcome measure was change in HbA1c level. HbA1c levels were measured using the high-performance liquid chromatography (HPLC) method.
Diabetes and medication knowledge was assessed using questionnaires developed based on previous publications (8,9). Self-reported adherence to medication was evaluated using the Morisky-Green questionnaire (10,11) and the Adherence to Medicines Questionnaire (AMQ), which has been validated in the Brazilian population (12). Insulin injection and home blood glucose monitoring techniques were assessed by instruments standardized in our practice (13) and diabetes-related quality of life was determined using the validated Brazilian version of Diabetes Quality of Life Measure (14).
Statistical analysis
Comparisons were made between the data at the initial and final assessments using appropriate statistical tests as follows: the chi-square test was used for categorical data and the paired t-test was utilized for normally distributed continuous data. Comparisons between HbA1c levels and other outcomes were performed using analysis of variance (ANOVA) and Bonferroni's correction.
All analyses were performed using the Statistical Analysis System (SAS) version 8.0 and the Statistical Package for the Social Sciences (SPSS) version 15.0.
Ethics
The study protocol was approved by the Research Ethics Committee of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo.
RESULTS
Seventy-eight patients were initially enrolled in the study, namely, 41 in the CG and 37 in the IG. During the study period, 8 patients were excluded (5 in the CG and 3 in the IG) because they missed appointments. Thirty-six patients in the CG and 34 in the IG completed the study (Figure 1).
The demographic characteristics of the patients are shown in Table 1; the two groups were homogeneous with respect to all variables.
Table 1.
Baseline demographics of the study participants.
| Variable | Control Group (n = 36) | Intervention Group (n = 34) | p | Total |
| Age (years) (mean (SD)) | 61.58 (8.14) | 61.91 (9.58) | 0.877 | 61.74 (8.81) |
| Male (n/total (%)) | 14/36 (38.9) | 13/34 (38.2) | 0.955 | 27/70 (38.6) |
| Duration of diabetes (years), (mean (SD)) | 14.92 (8.49) | 14.56 (7.40) | 0.852 | 14.74 (7.92) |
In the IG, the diabetes knowledge score increased from 9.91±2.69 to 15.74±3.03 and medication knowledge increased from 4.47±0.84 to 6.58±1.29. No changes were observed in the CG for either knowledge outcome (Table 2).
Table 2.
Outcome changes from baseline in the control and intervention groups.
| Variable | Assessment | Control Group (n = 36) | Intervention Group (n = 34) | p* |
| Diabetes knowledge (score, mean ± SD) | Initial | 9.72±2.71 | 9.91±2.69 | >0.999 |
| Final | 9.75±2.69 | 15.74±3.03 | <0.001 | |
| p# | >0.999 | <0.001 | ||
| Medication knowledge (score, mean ± SD) | Initial | 3.94±0.99 | 4.47±0.84 | 0.118 |
| Final | 3.85±0.99 | 6.58±1.29 | <0.001 | |
| p# | >0.999 | <0.001 | ||
| Adherence, Morisky-Green (% adherent patients) | Initial | 27.8% | 17.6% | 0.313 |
| Final | 25% | 70.6% | <0.001 | |
| p# | >0.999 | <0.001 | ||
| Adherence, AMQ (% adherent patients) | Initial | 30.6% | 47.1% | 0.917 |
| Final | 25% | 52.9% | 0.016 | |
| p# | 0.500 | 0.039 | ||
| Insulin injection technique (% correct) | Initial | 59.09±18.24 | 66.61±15.41 | 0.404 |
| Final | 57.68±18.21 | 87.81±10.89 | <0.001 | |
| p# | >0.999 | <0.001 | ||
| Home blood glucose monitoring technique (score, mean ± SD) | Initial | 6.31±1.41 | 6.85±0.93 | 0.364 |
| Final | 6.25±1.18 | 8.88±1.04 | <0.001 | |
| p# | >0.999 | <0.001 | ||
| HbA1c (%, mean ± SD) | Initial | 9.61±1.38 | 9.78±1.55 | >0.999 |
| Final | 9.53±1.68 | 9.21±1.41 | >0.999 | |
| p# | >0.999 | <0.001 | ||
| Diabetes-related quality of life (score, mean ± SD) | Initial | 162.53±9.71 | 157.21±13.28 | 0.354 |
| Final | 166.36±9.94 | 152.06±14.98 | <0.001 | |
| p# | <0.001 | <0.001 |
p* for comparisons between groups.
p# for analyses between the initial and final assessments within a group.
According to both questionnaires used to estimate adherence to medication, adherence in the IG improved significantly, namely, from 17.6% to 70.6% adherent patients according to the Morisky-Green questionnaire and from 41.7% to 52.9% adherent patients based on the AMQ responses. The percentage of adherent patients in the CG remained unchanged (Table 2).
The scores for insulin injection and blood glucose monitoring techniques significantly increased at the end of the study in the IG (66.61±15.41 to 87.81±10.89 and 6.85±0.93 to 8.88±1.04, respectively) but remained unchanged in the CG (Table 2).
The baseline mean serum HbA1c level was 9.61±1.38 in the CG and 9.78±1.55 in the IG. At the end of the study, the mean HbA1c level changed to 9.53±1.68 in the CG but decreased significantly to 9.21±1.41 in the IG, corresponding to a decrease of 0.57%.
Diabetes-related quality of life improved significantly in the IG by the end of the study, whereas there was a significant decrease in quality of life in the CG (Table 2).
No patients in the CG requested information during the study.
DISCUSSION
The practice of pharmaceutical care in Brazil has grown in recent years and in patients with diabetes, this care occurs mainly in primary and secondary health care settings (15-18).
This study was designed to evaluate the impact of pharmaceutical care in patients with T2DM treated at a tertiary health care facility, where patients are seen by a multidisciplinary team of physicians, nurses, psychologists, dieticians and podiatrists. Therefore, this study was unique because the clinical pharmacist worked directly with other professionals involved in patient care and participated in discussions regarding the best approach to patient treatment.
Few studies on pharmaceutical care have evaluated patients' diabetes knowledge. Similar to our study, significant increases in diabetes knowledge in the IG were reported by Fornos et al. (19) and by Mehuys et al. (20).
At the beginning of our study, patient knowledge of medications was low in both groups, mainly due to a lack of knowledge regarding the main adverse reactions and how to respond to missing a dose. The instructions regarding these aspects, as well as the medication names, indications and doses, most likely contributed to the significant increase in the scores at the end of the study in the IG. Other studies have reported similar results (19,21,22) and similar to our findings, Wermeille et al. attributed the minimal knowledge at baseline to not knowing the names of the medicines or how to respond to a missed dose (22).
Nonadherence to medications has been reported as the primary factor responsible for unscheduled consults and hospitalizations among patients with diabetes (23). Therefore, correct medication use is essential for treatment success among patients with this disease. Adherence is a complex component of treatment that is influenced by several factors directly related to patient behavior. Thus, both the questionnaires utilized to estimate self-reported adherence aim to identify and evaluate some of these aspects.
At the end of our study, 70.6% of the patients in the IG were adherent according to the Morisky-Green questionnaire and 52.9% were adherent according to the AMQ questionnaire. The percentage of adherent patients according to the Morisky-Green questionnaire in the IG at the end of the study is similar to the 72% reported by Jarab et al. (2012) using the same questionnaire (24). These values correspond to literature reports of compliance ranging from 36% to 85% for patients with diabetes (25), as well as to other studies evaluating adherence in pharmaceutical care programs (16,21).
Our study did not show significant inverse correlations between the number of prescribed medications and adherence, in contrast to observations in other studies (25,26).
T2DM is a progressive disease and several years after diagnosis, most patients develop secondary insulin deficiency and require daily insulin injections. Therefore, insulin injection and blood glucose self-monitoring techniques are important components of diabetes self-management in patients taking insulin (4).
At baseline, the most common errors regarding insulin use were related to the use of the insulin bottle for longer than recommended after opening (30 days), not washing hands before the injection, not homogenizing the NPH insulin before dispensing the dose and not waiting 5 seconds before removing the syringe after the injection. At the end of the study, the major improvements observed in the IG were related to proper homogenization of NPH insulin and appropriate reading of the graduation of the syringes. Regarding home blood glucose monitoring, the major technical improvement observed in the IG was related to the appropriate puncture site on the finger. Nevertheless, we did not identify previously published studies that evaluated these aspects in pharmaceutical care programs.
The significant reduction in mean HbA1c (0.57% decrease) in the IG was comparable to that reported in other randomized controlled trials with the same follow-up period; specifically, the decrease was similar to the 0.6% decrease reported by Mourão et al. (18) and Mehuys et al. (20) and slightly lower than the 0.8% decrease reported by Jarab et al. (24). Despite the similarities between the studies, it is worth noting that the study published by Mourão et al. (18) was conducted in a primary health care setting and included patients with HbA1c>7% who were only on oral antidiabetic medication. The study reported by Mehuys et al. (20) was performed in community pharmacies and only approximately 10% of the participants were on prescription insulin. The study performed by Jarab et al. (24) included patients with HbA1c levels above 7.5% who had a shorter duration of disease compared with our population, which may explain why approximately 70% of the patients were on insulin therapy. Additionally, the reduction in mean HbA1c observed in our study was similar to the 0.62% reduction in the IG described in a meta-analysis performed by Machado et al. (27), but it was lower than the 0.76% reduction found in the meta-analysis by Collins et al. (28).
A non-randomized study performed in the city of Ribeirão Preto, São Paulo, Brazil, with patients of similar age to those in our study revealed a significant reduction in mean HbA1c (0.9%) in the IG after 12 months of follow-up (16). Similarly to the study cited, other studies have reported greater reductions in HbA1c (1.3% and 3.4%), probably due to a longer follow-up period (usually 12 months) (19,29-31).
The differences between the reductions in HbA1c values reported in the aforementioned studies could also be due to the characteristics of the study population. The patients in this study had difficulty managing T2DM; a prolonged time had elapsed since disease diagnosis; and all the patients were on prescription insulin, most as intensive therapy. Furthermore, social and cultural aspects, such as low health literacy, partially explain the poor glycemic control and eventually presented as deficiencies in knowledge of diabetes, medications and necessary techniques for self-management at the beginning of the study.
Studies have shown that certain classes of antidiabetic medication, including the most recent glucagon-like peptide 1 (GLP-1) agonists and dipeptidyl peptidase 4 (DPP-4) inhibitors, reduce HbA1c by a mean of 0.5% to 1%. Thus, the 0.57% decrease reported in our study is clinically relevant (32).
The significant improvement in diabetes-related quality of life in the IG as well as the decreased diabetes-related quality of life in the CG were unexpected. As quality of life encompasses several dimensions, changes typically only become apparent in the medium or long term and are, therefore, difficult to detect in a six-month period or in a small cohort, such as was the case in our study. Indeed, Al Mazroui et al. reported a significant increase in quality of life in the IG after 12 months of intervention according to a general health-related quality of life questionnaire (SF36 Questionnaire) (21).
We can likely attribute the reduction in HbA1c in the IG patients to the positive results in the evaluated secondary outcomes (16,21,33).
The improvement in the outcomes measured in our study are a result of individualized instructions related to pharmacotherapy provided by a clinical pharmacist and the educational approach to diabetes self-management activities, as we consider pharmacists to be diabetes educators (34,35). This combination is intended to improve patient quality of life, which is consistent with the philosophy of pharmaceutical care (7).
This study had certain limitations, such as the small sample size, the short follow-up period and the inherent inability to control for all confounding factors in the outcome analysis.
ACKNOWLEDGMENTS
We acknowledge Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for providing financial support.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.International Diabetes Federation. 2011 IDF Diabetes Atlas, (cited 2011 Dec 12);5:(Available from: http://www.idf.org/diabetesatlas/5e/the-global-burden). [Google Scholar]
- 2.Brasil, Ministério da Saúde. Vigitel Brasil 2011, (cited 2012 Jul 12); (Available from: http://portalsaude.saude.gov.br/portalsaude/arquivos/pdf/2012/Mai/09/Vigitel_2011_diabetes_final.pdf). [Google Scholar]
- 3.Lindenmeyer A, Hearnshaw H, Vermeire E, Royen PV, Wens J, Biot Y. Interventions to improve adherence to medication in people with type 2 diabetes mellitus: a review of the literature on the role of pharmacists. J Clin Pharm Ther. 2006;31(5):409–19. doi: 10.1111/j.1365-2710.2006.00759.x. [DOI] [PubMed] [Google Scholar]
- 4.Standards of Medical Care in Diabetes. Diabetes Care. 2012;35(Suppl 1):S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sisson E, Kuhn C. Pharmacist roles in the management of patients with type 2 diabetes. J Am Pharm Assoc. 2009;49(Suppl 1):S41–5. doi: 10.1331/JAPhA.2009.09075. [DOI] [PubMed] [Google Scholar]
- 6.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National Standards for Diabetes Self-Management Education. Diabetes Care. 2012;35(Suppl 1):S101–8. doi: 10.2337/dc12-s101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43. [PubMed] [Google Scholar]
- 8.Rothman RL, Malone R, Bryant B, Wolfe C, Padgett P, DeWalt DA, et al. The Spoken Knowledge in Low Literacy in Diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Education. 2005;31(2):215–24. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- 9.McPherson ML, Smith SW, Powers A, Zuckerman IH. Association between diabetes patients' knowledge about medications and their blood glucose control. Res Social Adm Pharm. 2008;4(1):37–45. doi: 10.1016/j.sapharm.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Strelec MAAM, Pierin AMG, Mion D., Jr A influência do conhecimento sobre a doença e a atitude frente à tomada dos remédios no controle da hipertensão arterial. Arq Bras Cardiol. 2003;81(4):343–8. [Google Scholar]
- 12.Santa Helena ET, Nemes MI, Eluf J., Neto Development and validation of a multidimensional questionnaire assessing non-adherence to medicines. Rev Saude Publica. 2008;42(4):764–7. doi: 10.1590/s0034-89102008000400025. [DOI] [PubMed] [Google Scholar]
- 13.Kaneto LA, Fabri LRO, Damião EBC, Queiroz MS, Nery M. Diabetes Mellitus tipo 1: verificação do conhecimento sobre insulinoterapia e monitorização glicêmica. Arq Bras Endocrinol Metabol. 2009;53(8):S986. [Google Scholar]
- 14.Correr CJ, Rolo RP, Melchiors AC, Rossignoli P, Fernández-Llimós F, Radominski RB. Tradução para o Português e Validação do Instrumento Diabetes Quality of Life Measure (DQOL-Brasil) Arq Bras Endocrinol Metabol. 2008;52(3):515–22. doi: 10.1590/s0004-27302008000300012. [DOI] [PubMed] [Google Scholar]
- 15.Correr CJ, Pontarolo R, Souza RAP, Venson R, Melchiors AC, Wiens A. Effect of a Pharmaceutical Care Program on quality of life and satisfaction with pharmacy services in patients with type 2 diabetes mellitus. Braz J Pharm Sci. 2009;45(4):809–17. [Google Scholar]
- 16.Borges AP, Guidoni CM, Ferreira LD, de Freitas O, Pereira LR. The pharmaceutical care of patients with type 2 diabetes mellitus. Pharm World Sci. 2010;32(6):730–6. doi: 10.1007/s11096-010-9428-3. [DOI] [PubMed] [Google Scholar]
- 17.Correr CJ, Melchiors AC, Fernandez-Llimos F, Pontarolo R. Effects of a pharmacotherapy follow-up in community pharmacies on type 2 diabetes patients in Brazil. Int J Clin Pharm. 2011;33(2):273–80. doi: 10.1007/s11096-011-9493-2. [DOI] [PubMed] [Google Scholar]
- 18.Mourão AO, Ferreira WR, Martins MA, Reis AM, Carrillo MR, Guimarães AG, et al. Pharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trial. Int J Clin Pharm. 2013;35(1):79–86. doi: 10.1007/s11096-012-9710-7. [DOI] [PubMed] [Google Scholar]
- 19.Fornos JA, Andres NF, Andres JC, Guerra MM, Egea B. A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm World Sci. 2006;28(2):65–72. doi: 10.1007/s11096-006-9003-0. [DOI] [PubMed] [Google Scholar]
- 20.Mehuys E, Van Bortel L, De Bolle L, Van Tongelen I, Annemans L, Remon JP, Giri M. Effectiveness of a community pharmacist intervention in diabetes care: a randomized controlled trial. J Clin Pharm Ther. 2010;2011;36(5):602–13. doi: 10.1111/j.1365-2710.2010.01218.x. [DOI] [PubMed] [Google Scholar]
- 21.Al Mazroui NR, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with Type 2 diabetes mellitus. Br J Clin Pharmacol. 2009;67(5):547–57. doi: 10.1111/j.1365-2125.2009.03391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wermeille J, Bennie M, Brown I, McKnight J. Pharmaceutical care model for patients with type 2 diabetes: integration of the community pharmacist into the diabetes team-a pilot study. Pharm World Sci. 2004;26(1):18–25. doi: 10.1023/b:phar.0000013465.24857.a8. [DOI] [PubMed] [Google Scholar]
- 23.Irons BK, Lenz RJ, Anderson SL, Wharton BL, Habeger B, Anderson HG., Jr A retrospective cohort analysis of the clinical effectiveness of a physician-pharmacist collaborative drug therapy management diabetes clinic. Pharmacotherapy. 2002;22(10):1294–300. doi: 10.1592/phco.22.15.1294.33476. [DOI] [PubMed] [Google Scholar]
- 24.Jarab AS, Algudah SG, Mukattash TL, Shattat G, Al-Qirim T. Randomized Controlled Trial of Clinical Pharmacy Management of Patients with Type 2 Diabetes in an Outpatient Diabetes Clinic in Jordan. J Manag Care Pharm. 2012;18(7):516–26. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Odegard PS, Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabetes Educator. 2007;33(6):1014–29. doi: 10.1177/0145721707308407. [DOI] [PubMed] [Google Scholar]
- 26.Odegard PS, Lam A, Chun A, Blough D, Li MA, Wu J. Pharmacist provision of language-appropriate education for Asian patients with asthma. J Am Pharm Assoc. 2004;44(4):472–7. doi: 10.1331/1544345041475742. [DOI] [PubMed] [Google Scholar]
- 27.Machado M, Bajcar J, Guzzo GC, Einarson TR. Sensitivity of patient outcomes to pharmacist interventions. Part I: systematic review and meta-analysis in diabetes management. Ann Pharmacother. 2007;41(10):1569–82. doi: 10.1345/aph.1K151. [DOI] [PubMed] [Google Scholar]
- 28.Collins C, Limone BL, Scholle JM, Coleman CI. Effect of pharmacists intervention on glycemic control in diabetes. Diabetes Diabetes Res Clin Pract. 2011;92(2):145–52. doi: 10.1016/j.diabres.2010.09.023. [DOI] [PubMed] [Google Scholar]
- 29.Morello CM, Zadvorny EB, Cording MA, Suemoto RT, Skog J, Harari A. Development and clinical outcomes of pharmacist-managed diabetes care clinics. Am J Health Syst Pharm. 2006;15;63(14):1325–31. doi: 10.2146/ajhp050430. [DOI] [PubMed] [Google Scholar]
- 30.Clifford RM, Davis WA, Batty KT, Davis TM. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2005;28(4):771–6. doi: 10.2337/diacare.28.4.771. [DOI] [PubMed] [Google Scholar]
- 31.Cioffi ST, Caron MF, Kalus JS, Hill P, Buckley TE. Glycosylated hemoglobin, cardiovascular, and renal outcomes in a pharmacist-managed clinic. Ann Pharmacother. 2004;38(5):771–5. doi: 10.1345/aph.1D359. [DOI] [PubMed] [Google Scholar]
- 32.Nathan DM, Buse JB, Davison MB, Ferrannini E, Holman RR, Sherwin R, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. Diabetes Care. 2009;32(1):193–203. doi: 10.2337/dc08-9025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rhee MK, Slocum W, Ziemer DC, Culler SD, Cook CB, El-Kebbi IM, Gallina DL, et al. Patient adherence improves glycemic control. Diabetes Educ. 2005;31(2):240–50. doi: 10.1177/0145721705274927. [DOI] [PubMed] [Google Scholar]
- 34.Pepper MJ, Mallory N, Coker TN, Chaki A, Sando KR. Pharmacists' impact on improving outcomes in patients with type 2 diabetes mellitus. Diabetes Educ. 2012;38(3):409–16. doi: 10.1177/0145721712443291. [DOI] [PubMed] [Google Scholar]
- 35.Wubben DP, Vivian EM. Effects of pharmacists outpatients interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;28(4):421–36. doi: 10.1592/phco.28.4.421. [DOI] [PubMed] [Google Scholar]