Abstract
OBJECTIVES:
The aim of our study was to evaluate the total atrial conduction time and its relationship to subclinical atherosclerosis, inflammation and echocardiographic parameters in patients with type 2 diabetes mellitus.
METHODS:
A total of 132 patients with type 2 diabetes mellitus (mean age 54.5±9.6 years; 57.6% male) and 80 age- and gender-matched controls were evaluated. The total atrial conduction time was measured by tissue-Doppler imaging and the carotid intima-media thickness was measured by B-mode ultrasonography.
RESULTS:
The total atrial conduction time was significantly longer in the patients with type 2 diabetes mellitus than in the control group (131.7±23.6 vs. 113.1±21.3, p<0.001). The patients with type 2 diabetes mellitus had significantly increased carotid intima-media thicknesses, neutrophil to lymphocyte ratios and high-sensitivity C-reactive protein levels than those of the controls. The total atrial conduction time was positively correlated with the high-sensitivity C-reactive protein level, neutrophil to lymphocyte ratio, carotid intima-media thickness and left atrial volume index and negatively correlated with the early diastolic velocity (Em), Em/late diastolic velocity (Am) ratio and global peak left atrial longitudinal strain. A multiple logistic regression analysis demonstrated that the neutrophil to lymphocyte ratio, carotid intima-media thickness and global peak left atrial longitudinal strain were independent predictors of the total atrial conduction time.
CONCLUSIONS:
We suggest that subclinical atherosclerosis and inflammation may represent a mechanism related to prolonged total atrial conduction time and that prolonged total atrial conduction time and impaired left atrial myocardial deformation may be represent early subclinical cardiac involvement in patients with type 2 diabetes mellitus.
Keywords: Inflammation, Left Atrial Strain, Subclinical Atherosclerosis, Total Atrial Conduction Time
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is a chronic multisystem disease associated with a high risk of cardiovascular disease (1). In clinical practice, atrial fibrillation (AF) is the most frequently observed cardiac arrhythmia and is related to increased morbidity and mortality. Diabetes is significantly correlated with AF in both genders even after adjusting for age and other risk factors (2). However, the pathological mechanisms related to the initiation and maintenance of AF in patients with diabetes mellitus have not been well described.
In patients with T2DM, the carotid intima media thickness (CIMT), which is a well-established marker of subclinical atherosclerosis, is significantly greater than that in non-diabetic subjects (3). Subclinical chronic inflammation is widely known to play a key role in the initiation, propagation and development of diabetes (4). Both laboratory and epidemiological studies have suggested that subclinical atherosclerosis and inflammation can play a role in the development of AF (5-9). However, there are not sufficient data in the literature regarding the relationship between AF and subclinical atherosclerosis and inflammation in diabetic patients.
Electrical and structural atrial remodeling, the shortening of the atrial refractory period and the inhomogeneous propagation of sinus impulses are well-known electrophysiological characteristics of fibrillation-prone atria. The total atrial conduction time (TACT), measured via tissue Doppler imaging (PA-TDI Interval), is a novel echocardiographic parameter used to identify the presence and the extent of electrical and structural atrial remodeling (10). Previous studies have shown that a prolonged TACT is a strong and independent predictor of new-onset AF (11,12). In this study, we hypothesized that the relationship between DM and AF may be mediated by the effect of subclinical atherosclerosis and inflammation on atrial myocardial tissue.
High-sensitivity C-reactive protein (hsCRP) is an inflammatory biomarker that independently predicts the cardiovascular risk (13). The neutrophil to lymphocyte ratio (NLR), as an indicator of systemic inflammation, is an emerging marker for both cardiac and non-cardiac disorders (14-15). The CIMT is a widely accepted marker of subclinical atherosclerosis (3).
To date, no studies have investigated the effects of subclinical atherosclerosis and inflammation on the TACT, which is an early predictor of AF development, in patients with T2DM. In this study, we aimed to evaluate the effects of T2DM on the TACT and to investigate the possible relationship between the TACT and echocardiographic findings, the CIMT and the NLR and hsCRP levels in patients with T2DM.
METHODS
Study population
A total of 132 consecutive type 2 diabetic patients who were diagnosed at least one year prior and 80 sex- and age-matched healthy controls were enrolled in this observational, cross-sectional study. T2DM was diagnosed according to the American Diabetes Association criteria (16). Of the diabetic cases, 48 (36.3%) patients were receiving insulin and 84 (63.7%) patients were receiving an oral anti-diabetic treatment. The exclusion criteria for the patients were as follows: a history of coronary artery disease, left ventricular (LV) systolic dysfunction, moderate to severe valvular heart disease, arterial hypertension, AF, pre-excitation syndromes, atrioventricular conduction abnormalities, bundle branch block, previously implanted cardiac pacemakers, anti-arrhythmic medicine use, electrolyte imbalance, thyroid diseases, chronic renal or liver diseases, pulmonary disease, chronic inflammatory disorders, known infectious disease and a history of a hypoglycemic episode in the past month. The study protocol was approved by our local ethics committee and all patients provided their written informed consent to participate in the study.
Echocardiographic examination
Echocardiography was performed using a GE Vivid S5 system (GE Vingmed Ultrasound AS, Norten, Norway) with a 2.5-MHz phased-array transducer. All subjects were imaged in the left lateral decubitus position and underwent a complete transthoracic echocardiographic examination. All examinations were made by two experienced cardiologists blinded to the clinical data of the subjects. During the echocardiography, a 1-lead electrocardiogram (ECG) was continuously recorded. The LV size measurements and diastolic LV filling velocities were conducted in accordance with the American Society of Echocardiography guidelines (17). The left ventricular ejection fraction (LVEF) was calculated using Simpson's biplane method. The LV mass was calculated with the Devereux formula (18). The interventricular septal thickness (IVST), posterior wall thickness (PWT) and left atrial volumes were also measured. Both the LV mass and the left atrium (LA) volume were indexed according to the body surface area. Mitral inflow was assessed from the apical four-chamber view with pulsed-wave Doppler by placing a 1-2-mm sample volume between the tips of the mitral leaflets in diastole. From the mitral inflow E and A wave velocities, the E-deceleration time (DT) and E/A velocity ratio were obtained. TDI was performed in the apical 4-chamber view by placing a 1-2-mm sample volume at the lateral and septal mitral annulus. The measurements of the systolic (Sm), early diastolic (Em) and late diastolic (Am) velocities were obtained and averaged (19). The Em/Am and E/Em ratios were calculated. The myocardial performance index (MPI) was measured as previously defined by Tei (20).
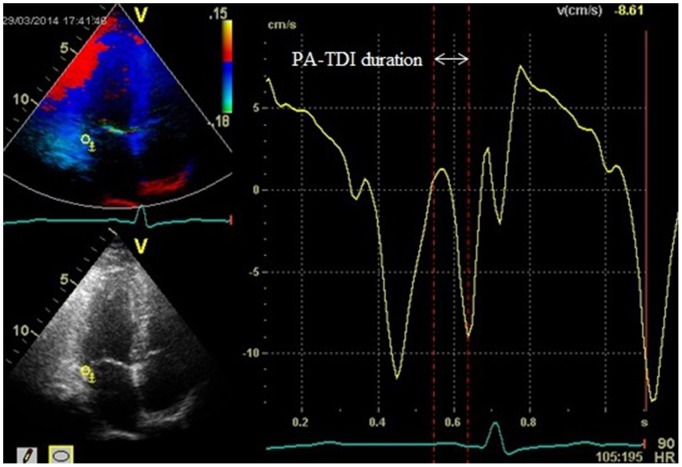
The PA-TDI duration is a novel echocardiographic parameter that can be used to estimate the TACT. The PA-TDI interval was defined as the time interval from the initiation of the P-wave on the surface ECG to the peak of the A wave on the TDI of the lateral wall of the LA, just above the mitral annulus (Figure 1) (21).
Figure 1.
Measurement of the total atrial conduction time (PA-TDI interval). The PA-TDI interval was defined as the time interval between the onset of the P-wave on the surface ECG and the peak Am wave on the tissue Doppler tracing. ECG: electrocardiogram; Am: tissue Doppler mitral annular late diastolic velocity.
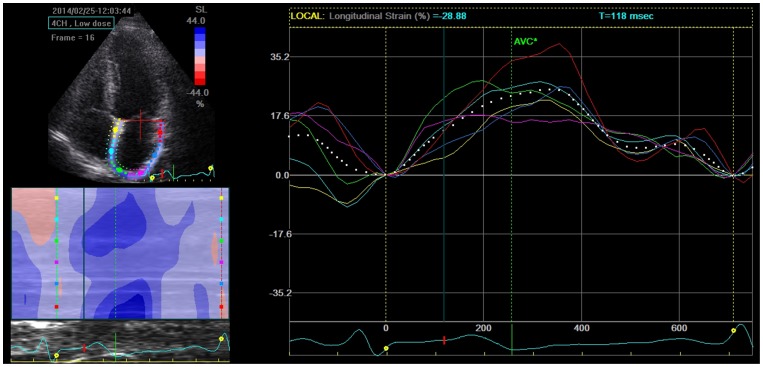
Two-dimensional echocardiography images for the LA were obtained from the apical two- and four-chamber views. All images were stored in a cine loop format from three consecutive beats during a breath hold with a stable electrocardiographic recording. The frame rate was set between 60 and 80 frames per second. Speckle-tracking analyses were performed offline using commercially available software (EchoPAC; GE Medical Systems). The endocardial border was manually defined and tracing was automatically performed by the software for each view. An image tracking algorithm automatically divided the LA wall into 6 segments and the peak LA longitudinal strain (PALS) values for each apical view were measured by averaging the values observed in all LA segments (Figure 2). The global PALS values were the averages of the values obtained for each apical view (22,23).
Figure 2.
Assessment of the peak atrial longitudinal strain by two-dimensional speckle-tracking echocardiography. The dashed curve represents the average atrial longitudinal strain along the cardiac cycle.
Assessment of the carotid intima-media thickness
The CIMT was measured using the Toshiba Diagnostic Ultrasound System (Aplio MX SSA-780A) with a 7.5-MHz transducer in patients lying in the supine position. The technique used was in accordance with the consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force (24). Briefly, the CIMT was defined as the distance between the leading edge of the lumen-intima interface and the media-adventitia interface on the far wall of the common carotid artery (CCA) (posterior wall). After examination of the transverse and longitudinal planes of the carotid arteries, the CIMT was measured in both arteries approximately 1 cm proximal to the carotid artery bifurcation in an area free of plaque. At least three measurements were performed on both sides and averaged. Then, the average of the measurements obtained from both CCAs was taken as the CIMT.
Analysis of blood samples
After fasting overnight for 12 h, venous blood samples were obtained for all patients from the antecubital space. Total and differential leukocyte counts were measured as part of the automated complete blood count using a Coulter LH 780 Hematology Analyzer (Beckman Coulter Inc., Miami, FL, USA). HsCRP and other biochemical parameters were measured by standard laboratory procedures. The NLR was obtained by dividing the total neutrophil count by the total lymphocyte count.
Statistical analysis
Continuous variables are presented as the mean + standard deviation or the median (interquartile range) values and categorical variables are presented as a percentage. The one-sample Kolmogorov-Smirnov test was used to evaluate whether the distribution of continuous variables was normal. Continuous variables between 2 groups were compared with Student's t test or the Mann-Whitney U test. Categorical variables were compared appropriately with the chi-square test or Fisher's exact test. The correlations between variables were tested by Pearson's correlation tests for normally distributed variables and with Spearman's correlation tests for non-normally distributed variables. The TACT was categorized into two groups, with the median as the cut-off point. To determine the independent predictors of supramedian TACT, parameters that were found to have significance (p<0.05) in the univariate analysis were evaluated by stepwise forward logistic regression analysis; 95% confidence intervals (CIs) and odds ratios (ORs) were presented together. Receiver–operating characteristic (ROC) analysis was used to compare the performance and prognostic power of the NLR, CIMT and PALS for supramedian TACT. The predictive validities were quantified as the area under the ROC curves (c statistics) and the comparisons of c statistics were performed using the MedCalc statistical software (version 11.3.8.0, Mariakerke, Belgium). To assess the reproducibility of the CIMT, TACT and global PALS measurements, 20 patients were randomly selected. For the interobserver and intraobserver variability, Bland-Altman analysis and intraclass correlation coefficient were used, respectively. A 2-sided p value <0.05 was considered significant in all analyses. Data were analyzed using SPSS version 15.0 (SPSS Inc., Chicago, Illinois).
RESULTS
The study population comprised 132 T2DM patients (mean age 54.5±9.6 years; 57.6% male) and 80 controls (mean age 53.2±9.0 years; 62.5% male). The demographic findings and laboratory values of the study groups are presented in Table 1). The age, sex, body mass index, smoking status, systolic and diastolic blood pressures and heart rate were similar between the 2 groups (p>0.05). In patients with T2DM, the mean HbA1c level was 8.4%±2.7% and the mean disease duration was 83.4±52.5 months. The patients with T2DM had a significantly increased CIMT compared with the controls (0.80±0.25 vs. 0.66±0.13 mm, p<0.001). When the laboratory findings were compared, T2DM patients had significantly higher NLRs and hsCRP levels (3.7±1.4 vs. 2.5±1.2, p<0.001; 1.0±0.4 vs. 0.8±0.4, p = 0.003, respectively).
Table 1.
Clinical and laboratory characteristics of the study population.
| Patients with DM | Controls | ||
| (n = 132) | (n = 80) | p | |
| Age, years | 54.5±9.6 | 53.2±9.0 | 0.315 |
| Gender, Male (%) | 76(57.6%) | 50(62.5%) | 0.479 |
| BMI (kg/m2) | 23.5±5.8 | 22.1±6.1 | 0.116 |
| Smoking (%) | 50(37.9%) | 27(33.8%) | 0.545 |
| SBP (mmHg) | 116.8±12.9 | 114.8±14.6 | 0.315 |
| DBP (mmHg) | 68.6±8.5 | 67.9±8.7 | 0.608 |
| Heart rate (beats/min) | 73.2±10.2 | 74.7±11.6 | 0.339 |
| Disease duration (mo) | 83.4±52.5 | - | - |
| NLR | 3.7±1.4 | 2.5±1.2 | <0.001 |
| HsCRP (mg/L) | 1.0±0.4 | 0.8±0.4 | 0.003 |
| CIMT | 0.80±0.25 | 0.66±0.13 | <0.001 |
BMI: body mass index; SDP: systolic blood pressure; DBP: diastolic blood pressure; NLR: neutrophil to lymphocyte ratio; hsCRP: high-sensitivity C-reactive protein; CIMT: carotid intima-media thickness.
The LV echocardiographic findings in the subjects are shown in Table 2). The E/A ratio was significantly decreased in the patients with T2DM. The tissue Doppler Am was higher in the diabetic group; consequently, the average Em/Am ratio was significantly decreased in this group. The left atrial volume index (LAVI) was significantly increased in the diabetic patients (32.7±6.4 vs. 23.6±5.6, p<0.001). Global PALS was found to be significantly decreased in the patients with T2DM compared with the control group (24.5±6.6 vs. 33.4±8.2, p<0.001). TACT was significantly longer in the patients with T2DM than in healthy subjects (131.7±23.6 vs. 113.1±21.3, p<0.001). The LVEF, IVST, PWT, LV mass index, Mitral E and A velocities, DT, Sm and Em values, E/Em ratio, and MPI were similar in both groups (p>0.05).
Table 2.
Echocardiographic characteristics of the study population.
| Patients with DM | Controls | ||
| (n = 132) | (n = 80) | p | |
| LVEF (%) | 62.3(59.0-65.3) | 63.4(60.9-65.2) | 0.130 |
| IVST (mm) | 10.0(9.2-10.4) | 9.7(9.0-10.3) | 0.146 |
| LVPWT (mm) | 8.3(7.4-9.1) | 8.2(7.4-9.2) | 0.811 |
| LV mass index (g/m2) | 80.2±16.2 | 77.1±15.1 | 0.154 |
| Mitral E velocity (m/sn) | 0.92(0.70-0.93) | 0.82(0.72-1.0) | 0.637 |
| Mitral A velocity (m/sn) | 0.65(0.53-0.67) | 0.57(0.53-0.70) | 0.055 |
| E/A ratio | 1.33(0.76-1.65) | 1.44(0.99-1.78) | 0.028 |
| DT (ms) | 173.1±28.8 | 172.2±24.3 | 0.816 |
| Sm (cm/sn) | 7.9(7.1-9.2) | 8.1(7.9-8.5) | 0.051 |
| Em (cm/sn) | 9.6(8.2-11.5) | 9.9(8.5-11.7) | 0.299 |
| Am (cm/sn) | 7.3±0.8 | 7.0±0.9 | 0.014 |
| Em/Am ratio | 1.3±0.3 | 1.4±0.3 | 0.012 |
| E/Em ratio | 8.9±2.8 | 8.6±2.5 | 0.380 |
| MPI | 45.5±7.3 | 44.3±7.1 | 0.264 |
| LAVI (ml/m2) | 32.7±6.4 | 23.6±5.6 | <0.001 |
| PALS (%) | 24.5±6.6 | 33.4±8.2 | <0.001 |
| TACT (ms) | 131.7± 23.6 | 113.1±21.3 | <0.001 |
LVEF: left ventricular ejection fraction; IVST: interventricular septum thickness, LVPWT: left ventricular posterior wall thickness; LV: left ventricular; DT: deceleration time; Sm: tissue Doppler mitral annular systolic velocity; Em: tissue Doppler mitral annular early diastolic velocity; Am: tissue Doppler mitral annular late diastolic velocity; MPI: myocardial performance index; LAVI: left atrial volume index; PALS: peak atrial longitudinal strain; TACT: total atrial conduction time.
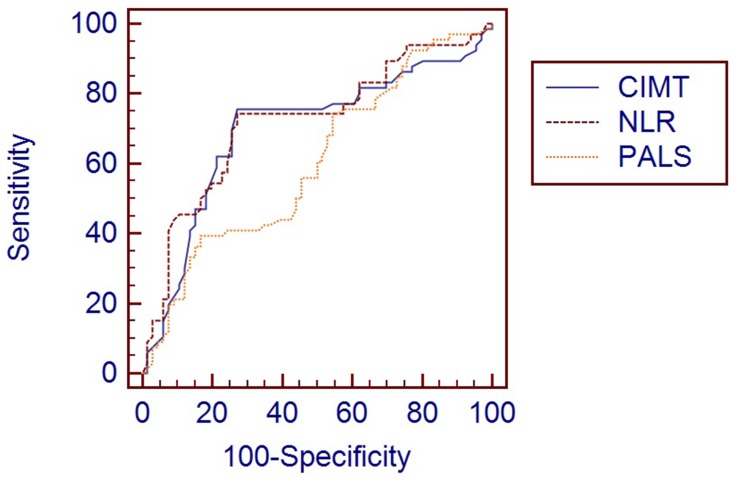
The TACT was positively correlated with hsCRP levels (r = 0.197, p = 0.024), the NLR (r = 0.311, p<0.001), the CIMT (r = 0.364, p<0.001) and the LAVI (r = 0.184, p = 0.035) and negatively correlated with the Em value (r = -0.296, p = 0.001), the Em/Am ratio (r = -0.195, p = 0.025) and global PALS (r = -0.188, p = 0.031) (Table 3). TACT was categorized into two groups, with the median as the cutpoint (<or ≥125.5). Variables showing significance values of p<0.05 in the univariate analysis (Table 4) between the inframedian and supramedian TACT groups were included in the multiple logistic regression model. There was multicollinearity between the Em value and Em/Am ratio; thus, Em was not included in the model. Accordingly, the NLR (OR: 1.78, 95% CI: 1.28-2.46; p<0.001), CIMT (OR: 7.99, 95% CI: 1.46-33.04; p = 0.016), and PALS (OR: 0.93, 95% CI: 0.87-0.99; p = 0.035) were found to be independent predictors of the TACT (Table 5). The cutoff value for supramedian TACT of the NLR was 4.0, with a sensitivity of 74.2% and a specificity of 72.7% (AUC, 0.708; 95% CI, 0.622-0.784; p<0.001), of CIMT was 0.81 mm, with a sensitivity of 75.8% and a specificity of 72.7% (AUC, 0.684; 95% CI, 0.597-0.762; p<0.001) and of PALS was 19.8%, with a sensitivity of 41% and a specificity of 83.3% (AUC, 0.602; 95% CI, 0.514-0.686; p = 0.038) in the ROC curve analysis (Figure 3). However, the AUC comparison of these parameters did not reach statistical significance (p>0.05). The results of the inter- and intraobserver agreement analyses for TACT, PALS and CIMT are shown in Table 6).
Table 3.
Bivariate correlation results between the total atrial conduction time and other parameters in diabetic patients.
| Variables | r | p |
| HsCRP | 0.197 | 0.024 |
| NLR | 0.311 | <0.001 |
| CIMT | 0.364 | <0.001 |
| LAVI | 0.184 | 0.035 |
| Em | -0.296 | 0.001 |
| Em/Am | -0.195 | 0.025 |
| PALS | -0.188 | 0.031 |
HsCRP: high-sensitivity C-reactive protein; NLR: neutrophil to lymphocyte ratio; CIMT: carotid intima-media thickness; LAVI: left atrial volume index; Em: tissue Doppler mitral annular early diastolic velocity; Am: tissue Doppler mitral annular late diastolic velocity; PALS: peak atrial longitudinal strain.
Table 4.
Comparison of clinical and echocardiographic variables between the inframedian and supramedian total atrial conduction times.
| TACT <125.5 | TACT ≥125.5 | ||
| n = 66 | n = 66 | p | |
| Age, years | 52.8±9.9 | 56.2±8.9 | 0.048 |
| HsCRP | 0.9±0.4 | 1.1±0.4 | 0.043 |
| NLR | 3.2±1.2 | 4.2±1.4 | <0.001 |
| CIMT | 0.72±0.22 | 0.88±0.26 | <0.001 |
| Em | 10.4(8.7-12.0) | 8.8(7.8-11.0) | 0.001 |
| Em/Am | 1.4±0.2 | 1.2±0.3 | 0.034 |
| LAVI | 31.5±5.8 | 33.9±6.8 | 0.035 |
| PALS | 25.7±6.6 | 23.2±6.4 | 0.031 |
HsCRP: high-sensitivity C-reactive protein; NLR: neutrophil to lymphocyte ratio; CIMT: carotid intima-media thickness; Em: tissue Doppler mitral annular early diastolic velocity; Am: tissue Doppler mitral annular late diastolic velocity; LAVI: left atrial volume index; PALS: peak atrial longitudinal strain.
Table 5.
Independent predictors of the total atrial conduction time in the multiple logistic regression analysis.
| Variables | Multiple OR (95% CI) | p |
| Age | 1.04(0.99-1.09) | 0.068 |
| HsCRP | 2.60(0.99-6.84) | 0.052 |
| NLR | 1.78(1.28-2.46) | <0.001 |
| CIMT | 7.99(1.46-33.58) | 0.016 |
| LAVI | 1.03(0.97-1.11) | 0.326 |
| Em/Am | 0.26(0.06-1.13) | 0.073 |
| PALS | 0.93(0.87-0.99) | 0.035 |
HsCRP: high-sensitivity C-reactive protein; NLR: neutrophil to lymphocyte ratio; CIMT: carotid intima-media thickness; LAVI: left atrial volume index; Em: tissue Doppler mitral annular early diastolic velocity; Am: tissue Doppler mitral annular late diastolic velocity; PALS: peak atrial longitudinal strain.
Figure 3.
Comparison ROC curves for the CIMT, NLR and PALS in the prediction of a longer TACT. ROC: receiver operating characteristic; CIMT: carotid intima-media thickness; NLR: neutrophil to lymphocyte ratio; PALS: peak atrial longitudinal strain; TACT: total atrial conduction time.
Table 6.
The Results of Inter- and Intraobserver Agreement Analyses.
| Variables 95% | Intraclass Correlation | Bland-Altman | |
| Coefficient (95% CI) | Mean Difference | Limits of Agreement | |
| TACT | 0.98 (0.97-0.99) | -0.15 | 0.57, -0.87 |
| PALS | 0.96(0.90-0.98) | -1.8 | 2.8, -6.4 |
| CIMT | 0.97(0.93-0.98) | - | - |
TACT: total atrial conduction time; PALS: peak atrial longitudinal strain; CIMT: carotid intima-media thickness.
DISCUSSION
The present study demonstrated that the TACT, measured with TDI, was increased and that LA myocardial deformation, assessed by two-dimensional strain imaging, was impaired in patients with T2DM. Furthermore, in this study, we also found that the NLR, CIMT and global PALS were independent predictors of the TACT in these patients.
Epidemiological studies have shown that the rate of AF development in diabetic subjects is higher than in normal subjects (25). A possible explanation for why diabetes mellitus causes predisposition to AF may involve LV hypertrophy, myocardial ischemia or fibrosis, left atrial remodeling, altered autonomic tone and inflammation (9,26,27). Additionally, the clinical hypoglycemic episodes in diabetic patients cause sympathetic activation, QT interval prolongation and cardiac repolarization. These changes may increase the risk of AF (28). However, the underlying mechanisms are still not clearly elucidated. The previous studies have demonstrated that the TACT, measured via the PA-TDI interval, could be used to predict the development of AF (29). Acar G et al. (30) reported that intra- and interatrial electromechanical coupling and atrial electromechanical delay, measured with TDI, were higher in patients with type 1 DM than in control subjects. In a recent experimental study, Fu H et al. (31) detected that the interatrial conduction time was prolonged in diabetic rabbits. In line with the results of these studies, in our study, we found that the TACT was significantly longer in patients with T2DM than in control subjects. In previous studies, chronic hyperglycemia was reported to cause prolongation of the interatrial conduction time by aggravating atrial fibrosis (32). However, the exact mechanism of TACT prolongation in diabetic patients remains unknown.
In a recent retrospective study, Chen LY et al. (33) reported that increased CIMT and arterial stiffness are associated with lone AF. In the population-based Rotterdam Study, Heeringa J et al. (7) reported that subclinical atherosclerosis, determined based on the CIMT, predicted new-onset AF in patients without overt coronary artery disease. In another population-based cohort study, Adamsson ES et al. (34) found that the CIMT is associated with the incidence of AF hospitalizations among middle-aged subjects. In contrast, the Cardiovascular Health Study (CHS) found no association between the CIMT and the AF incidence (35). Although these studies are population based, there are important differences in both the age distributions and the case report methods between the studies that might explain the different results. Subclinical atherosclerosis may lead to the development of fibrosis and microscopic scarring with consecutive remodeling of atrial tissue over time by decreasing the blood flow to the sinus node and atrial tissue (36). Atrial remodeling may account for the atrial conduction disturbances and the dispersion of the atrial refractory period, thereby facilitating reentry processes and the onset of atrial fibrillation (37). The TACT is a novel echocardiographic parameter used to assess the extent of atrial remodeling. In our study, we detected a weak but statistically significant positive correlation (r = 0.364, p<0.001) between the CIMT and the TACT, and the CIMT strongly and independently predicted the TACT in diabetic patients (OR: 7.99). Additionally, our study showed that a CIMT≥0.81 mm predicted the presence of a longer TACT, with a sensitivity of 75.8% and a specificity of 72.7%.
Generally, the relationship between AF and inflammation has been well established (38). Histological studies have demonstrated evidence of inflammatory infiltrates and oxidative damage within the atrial tissue in patients with AF compared with control subjects (5). Liu T et al. (9) suggested that inflammation was one of the mechanisms responsible for AF in diabetic patients. Inflammatory stimuli provoke fibroblast proliferation, migration and transformation into myofibroblasts and lead to atrial remodeling characterized by the shortening of the atrial refractory period (38). In studies investigating the AF-inflammation relationship, the most frequently studied inflammatory markers were CRP, hsCRP and interleukin (IL)-6 (5). In a few studies, the development of AF after cardiac surgery and the recurrence of AF after cryoballoon-based AF ablation were demonstrated to correlate with the NLR (39). Acar G et al. (40) have shown that atrial electromechanical delay is closely associated with the plasma level of CRP in patients with familial Mediterranean fever.
In our study, we detected a weak but statistically significant positive correlation (r = 0.311, p<0.001 and r = 0.197, p = 0.024, respectively) between the TACT, the NLR and hsCRP levels; in addition, the NLR independently predicted a longer TACT in diabetic patients (OR: 1.78). Furthermore, we showed that an NLR≥4.0 mm predicted the presence of a longer TACT, with a sensitivity of 74.2 and a specificity of 72.7.
In our study, the patients with T2DM had an increased LAVI and decreased E/A and Em/Am ratios compared with the normal volunteers. These results are consistent with prior studies in asymptomatic, normotensive type 1 and 2 diabetic patients (41). An increase in the LA volume might change the atrial fibrillar geometry, which in turn may contribute to TACT prolongation. We detected statistically significant but weak correlations between the TACT and the LAVI and the Em/Am ratio. However, it was demonstrated in our study that the LAVI and the Em/Am ratio were not strong parameters for predicting the longer TACT (OR: 1.03 and OR: 0.26, respectively). In previous studies, impaired LA deformation, assessed by the global PALS, was shown to correlate with atrial fibrosis and remodeling and was related to paroxysmal AF (22). In this study, we revealed that the global PALS decreased and was weakly but significantly correlated with the TACT in patients with T2DM. Among the echocardiographic parameters, only the global PALS independently predicted TACT (OR: 0.93). In addition, our study demonstrated that a PALS<19.8% predicted the presence of a longer TACT, with a sensitivity of 41% and a specificity of 83.3%.
In our study, the weak correlations detected between the TACT, the CIMT, the NLR, the hsCRP level and the echocardiographical parameters may have stemmed from the limited number of patients included in our study and relatively short disease duration. We only investigated the effects of subclinical atherosclerosis and inflammation on the TACT. However, other causes, such as cardiac autonomic neuropathy, renin-angiotensin aldosterone system activation, sympathetic overactivity, neural remodeling, the left atrial myocardial injury and fibrotic changes due to sustained hyperglycemia, all of which may cause an increased AF frequency and left atrial functional deterioration, could contribute to the prolongation of the TACT (42). The possible stronger relationships between the TACT and these factors may have led to the weak correlations observed between the TACT and the CIMT, NLR and hsCRP levels.
Limitations
The most important limitation is the cross-sectional design of the study; the patients were not prospectively followed-up in terms of arrhythmic episodes. Thus, we do not know whether TACT prolongation, subclinical atherosclerosis and inflammation, and impaired LA deformation predict AF in patients with T2DM. For this reason, the current findings need to be validated by long-term follow-up and in larger prospective studies. In our study, the TACT was not investigated by invasive electrophysiological techniques. Although we did not evaluate the patients who described a hypoglycemic episode within the past month, probable unreported hypoglycemic episodes occurring in the diabetic patients might have affected our study results. Another limitation was the use of non-invasive imaging techniques to exclude coronary artery disease in the study population. Coronary angiography was not performed in our study population on ethical grounds.
In the current study, we found that the TACT predicting AF development was prolonged and that LA myocardial deformation was impaired in patients with T2DM. Our study also indicated that subclinical atherosclerosis, inflammation and the global PALS were independently related to TACT. On the basis of these findings, we suggest that subclinical atherosclerosis and inflammation may be a mechanism related to TACT prolongation and prolonged TACT and impaired LA myocardial deformation may represent an early form of subclinical cardiac involvement in patients with T2DM and without clinical evidence of cardiovascular disease.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Ryden L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, et al. DESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34(39):3035–87. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Levy D, Vaziri SM, D′Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271(11):840–4. [PubMed] [Google Scholar]
- 3.Taniwaki H, Kawagishi T, Emoto M, Shoji T, Kanda H, Maekawa K, et al. Correlation between the intima-media thickness of the carotid artery and aortic pulse-wave velocity in patients with type diabetes. Vessel wall properties in type 2 diabetes. Diabetes Care. 1999;22(11):1851–57. doi: 10.2337/diacare.22.11.1851. [DOI] [PubMed] [Google Scholar]
- 4.Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011;11(2):98–107. doi: 10.1038/nri2925. [DOI] [PubMed] [Google Scholar]
- 5.Boos CJ, Anderson RA, Lip GY. Is atrial fibrillation an inflammatory disorder. Eur Heart J. 2006;27(2):136–49. doi: 10.1093/eurheartj/ehi645. [DOI] [PubMed] [Google Scholar]
- 6.Chen LY, Foo DC, Wong RC, Seow SC, Gong L, Benditt DG, et al. Increased carotid-intima media thickness and arterial stiffness are associated with lone atrial fibrillation. Int J Cardiol. 2013;168(3):3132–4. doi: 10.1016/j.ijcard.2013.04.034. [DOI] [PubMed] [Google Scholar]
- 7.Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Rooij FJ, Lip GY, et al. Subclinical atherosclerosis and risk of atrial fibrillation: the Rotterdam Study. Arch Intern Med. 2007;167(4):382–7. doi: 10.1001/archinte.167.4.382. [DOI] [PubMed] [Google Scholar]
- 8.Willeit K, Pechlaner R, Egger G, Weger S, Oberhollenzer M, Willeit J, et al. Carotid atherosclerosis and incident atrial fibrillation. Arterioscler Thromb Vasc Biol. 2013;33(11):2660–5. doi: 10.1161/ATVBAHA.113.302272. [DOI] [PubMed] [Google Scholar]
- 9.Liu T, Li G. Inflammation: Another potential mechanism between diabetes mellitus and atrial fibrillation. Am J Cardiol. 2008;101(11):1681–2. doi: 10.1016/j.amjcard.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Chao TF, Sung SH, Wang KL, Lin YJ, Chang SL, Lo LW, et al. Association between the atrial electromechanical interval, atrial remodeling and outcome of catheter ablation in paroxysmal atrial fibrillation. Heart. 2011;97(3):225–30. doi: 10.1136/hrt.2010.212373. [DOI] [PubMed] [Google Scholar]
- 11.Den Uijl DW, Gawrysiak M, Tops LF, Trines SA, Zeppenfeld K, Schalij MJ, et al. Prognostic value of total atrial conduction time estimated with tissue Doppler imaging to predict the recurrence of atrial fibrillation after radiofrequency catheter ablation. Europace. 2011;13(11):1533–40. doi: 10.1093/europace/eur186. [DOI] [PubMed] [Google Scholar]
- 12.de Vos CB, Weijs G, Crijns HJ, Cheriex EC, Palmans A, Habets J, et al. Atrial tissue Doppler imaging for prediction of new onset atrial fibrillation. Heart. 2009;95(10):835–40. doi: 10.1136/hrt.2008.148528. [DOI] [PubMed] [Google Scholar]
- 13.Libby P, Ridker PM, Maseri A. Inflammation and Atherosclerosis. Circulation. 2002;105(9):1135–43. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 14.Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102(6):653–7. doi: 10.1016/j.amjcard.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Papa A, Emdin M, Passino C, Michelassi C, Battaglia D, Cocci F. Predictive value of elevated neutrophil-lymphocyte ratio on cardiac mortality in patients with stable coronary artery disease. Clin Chim Acta. 2008;395(1-2):27–31. doi: 10.1016/j.cca.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 16.American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37(1):14–80. [Google Scholar]
- 17.Quinones MA, Otto CM, Stoddard M, Waggoner A, Zoghbi W. Recommendations for quantification of Doppler echocardiography: a report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. Jam Soc Echocardiogr. 2002;15(2):167–84. doi: 10.1067/mje.2002.120202. [DOI] [PubMed] [Google Scholar]
- 18.Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in men. Circulation. 1977;55(4):613–8. doi: 10.1161/01.cir.55.4.613. [DOI] [PubMed] [Google Scholar]
- 19.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22(2):107–33. doi: 10.1016/j.echo.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 20.Ulucay A, Tatlı E. Myocardial performance index. Anadolu Kardiyol Derg. 2008;8(2):143–8. [PubMed] [Google Scholar]
- 21.Merckx KL, De Vos CB, Palmans A, Habets J, Cheriex EC, Crijns HJ, et al. Atrial activation time determined by transthoracic Doppler tissue imaging can be used as an estimate of the total duration of atrial electrical activation. J Am Soc Echocardiogr. 2005;18(9):940–4. doi: 10.1016/j.echo.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 22.Cameli M, Lisi M, Reccia R, Bennati E, Malandrino A, Solari M, et al. Pre-operative left atrial strain predicts post-operative atrial fibrillation in patients undergoing aortic valve replacement for aortic stenosis. Int J Cardiovasc Imaging. 2014;30(2):279–86. doi: 10.1007/s10554-013-0323-6. [DOI] [PubMed] [Google Scholar]
- 23.Altekin RE, Yanikoglu A, Karakas MS, Ozel D, Yilmaz H, Demir I. Evaluation of left atrial function using two-dimensional speckle tracking echocardiography in end-stage renal disease patients with preserved left ventricular ejection fraction. Kardiol Pol. 2013;71(4):341–51. doi: 10.5603/KP.2013.0061. [DOI] [PubMed] [Google Scholar]
- 24.Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21(2):93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 25.Kannel WB, Abbott RD, Savage DD, McNamara PM. Epidemiologic features of chronic atrial fibrillation: The Framingham Study. N Engl J Med. 1982;306(17):1018–22. doi: 10.1056/NEJM198204293061703. [DOI] [PubMed] [Google Scholar]
- 26.Devereux RB, Roman MJ, Paranicas M, O′Grady MJ, Lee ET, Welty TK, et al. Impact of diabetes on cardiac structure and function: the strong heart study. Circulation. 2000;101(19):2271–6. doi: 10.1161/01.cir.101.19.2271. [DOI] [PubMed] [Google Scholar]
- 27.Crandall MA, Horne BD, Day JD, Anderson JL, Muhlestein JB, Crandall BG, et al. Atrial Fibrillation and CHADS2 Risk Factors are Associated with Highly Sensitive C-Reactive Protein Incrementally and Independently. Pacing Clin Electrophysiol. 2009;32(5):648–52. doi: 10.1111/j.1540-8159.2009.02339.x. [DOI] [PubMed] [Google Scholar]
- 28.Graveling AJ, Frier BM. Does hypoglycaemia cause cardiovascular events. Br J Diabetes Vasc Dis. 2010;10(1):5–13. [Google Scholar]
- 29.Özlü MF, Erdem K, Kırış G, Parlar Aİ, Demirhan A, Ayhan SS, et al. Predictive value of total atrial conduction time measured with tissue Doppler imaging for postoperative atrial fibrillation after coronary artery bypass surgery. J Interv Card Electrophysiol. 2013;37(1):27–33. doi: 10.1007/s10840-012-9756-4. [DOI] [PubMed] [Google Scholar]
- 30.Acar G, Akcay A, Sokmen A, Ozkaya M, Guler E, Sokmen G, et al. Assessment of Atrial Electromechanical Delay, Diastolic Functions, and Left Atrial Mechanical Functions in Patients with Type 1 Diabetes Mellitus. J Am Soc Echocardiogr. 2009;22(6):732–8. doi: 10.1016/j.echo.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 31.Fu H, Liu C, Li J, Zhou C, Cheng L, Liu T, et al. Impaired atrial electromechanical function and atrial fibrillation promotion in alloxan-induced diabetic rabbits. Cardiol J. 2013;20(1):59–67. doi: 10.5603/CJ.2013.0010. [DOI] [PubMed] [Google Scholar]
- 32.Liu C, Fu H, Li J, Yang W, Cheng L, Liu T, et al. Hyperglycemia aggravates atrial interstitial fibrosis, ionic remodeling and vulnerability to atrial fibrillation in diabetic rabbits. Anadolu Kardiyol Derg. 2012;12(7):543–50. doi: 10.5152/akd.2012.188. [DOI] [PubMed] [Google Scholar]
- 33.Chen LY, Foo DC, Wong RC, Seow SC, Gong L, Benditt DG, et al. Increased carotid intima-media thickness and arterial stiffness are associated with lone atrial fibrillation. Int J Cardiol. 2013;168(3):3132–4. doi: 10.1016/j.ijcard.2013.04.034. [DOI] [PubMed] [Google Scholar]
- 34.Adamsson Eryd S, Ostling G, Rosvall M, Persson M, Smith JG, Melander O, et al. Carotid intima-media thickness is associated with incidence of hospitalized atrial fibrillation. Atherosclerosis. 2014;233(2):673–8. doi: 10.1016/j.atherosclerosis.2014.01.050. [DOI] [PubMed] [Google Scholar]
- 35.Furberg CD, Psaty BM, Manolio TA, Gardin JM, Smith VE, Rautaharju PM. Prevalence of atrial fibrillation in elderly subjects (the Cardiovascular Health Study) Am J Cardiol. 1994;74(3):236–41. doi: 10.1016/0002-9149(94)90363-8. [DOI] [PubMed] [Google Scholar]
- 36.Anderson KR, Sutton MG, Lie JT. Histopathological types of cardiac fibrosis in myocardial disease. J Pathol. 1979;128(2):79–85. doi: 10.1002/path.1711280205. [DOI] [PubMed] [Google Scholar]
- 37.Tai CT, Chen SA, Tzeng JW, Kuo BI, Ding YA, Chang MS, et al. Prolonged fractionation of paced right atrial electrograms in patients with atrial flutter and fibrillation. J Am Coll Cardiol. 2001;37(6):1651–7. doi: 10.1016/s0735-1097(01)01215-3. [DOI] [PubMed] [Google Scholar]
- 38.Friedrichs K, Klinke A, Baldus S. Inflammatory pathways underlying atrial fibrillation. Trends Mol Med. 2011;17(10):556–63. doi: 10.1016/j.molmed.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 39.Canpolat U, Aytemir K, Yorgun H, Şahiner L, Kaya EB, Kabakçı G, et al. Role of Preablation Neutrophil/Lymphocyte Ratio on Outcomes of Cryoballoon-Based Atrial Fibrillation Ablation. Am J Cardiol. 2013;112(4):513–9. doi: 10.1016/j.amjcard.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 40.Acar G, Akcay A, Sayarlioglu M, Sokmen A, Sokmen G, Koroglu S, et al. Assessment of Atrial Conduction Time in Patients with Familial Mediterranean Fever. Pacing Clin Electrophysiol. 2009;32(3):308–13. doi: 10.1111/j.1540-8159.2008.02237.x. [DOI] [PubMed] [Google Scholar]
- 41.Poulsen MK, Henriksen JE, Dahl J, Johansen A, Gerke O, Vach W, et al. Left ventricular diastolic function in type 2 diabetes mellitus: prevalence and association with myocardial and vascular disease. Circ Cardiovasc Imaging. 2010;3(1):24–31. doi: 10.1161/CIRCIMAGING.109.855510. [DOI] [PubMed] [Google Scholar]
- 42.Asghar O, Alam U, Hayat SA, Aghamohammadzadeh R, Heagerty AM, Malik RA. Obesity, Diabetes and Atrial Fibrillation; Epidemiology, Mechanisms and Interventions. Curr Cardiol Rev. 2012;8(4):253–64. doi: 10.2174/157340312803760749. [DOI] [PMC free article] [PubMed] [Google Scholar]