Abstract
We sought to examine and describe neurocognitive function among middle-aged and older Hispanic/Latino Hispanic Community Health Study/Study of Latinos (HCHS/SOL) participants. We analyzed baseline cross-sectional data from the middle-aged and older (ages 45–74 years old) participants (n = 9,063) to calculate neurocognitive function scores and their correlates. Older age and higher depressive symptoms scores were associated with lower average neurocognitive performance, whereas greater educational attainment and household income were associated with higher neurocognitive performance. Hispanic/Latino heritage groups significantly varied in neurocognitive performances. Some neurocognitive differences between Hispanics/Latinos were maintained after controlling for language preference, education, household income, and depressive symptoms. We found notable differences in neurocognitive scores between Hispanic/Latino heritage groups that were not fully explained by the cultural and socioeconomic correlates examined in this study. Further investigations into plausible biological and environmental factors contributing to the Hispanic/Latino heritage group differences in neurocognitive found in the HCHS/SOL are warranted.
Keywords: Epidemiology, Neuroepidemiology, Cognitive function, Neurocognitive function, Neuropsychology, Hispanics, Latinos, Hispanic/Latinos
Introduction
Hispanic/Latinos currently comprise over 16% of the United States population and that proportion is projected to more than double by 2050 (Census, 2011). Hispanics/Latinos are culturally, demographically, ethnically, and socioeconomically diverse (Census, 2004), which has complicated and often obfuscated characterizations of this important population in research and policy (González et al., 2010; Miranda, Tarraf, González, Johnson-Jennings, & González, 2012). Specific to this report, Hispanic/Latino neurocognitive function characteristics come from a variety of studies with different age and ethnic samples, and neurocognitive tests. This has made it difficult to understand the epidemiology of neurocognitive health and disorders among Hispanics/Latinos.
In this study, we examine neurocognitive function among diverse Hispanics/Latinos. While we anticipate more commonalities than differences in neurocognitive function between Hispanic/Latino heritage groups, to our knowledge variations between these backgrounds in the same study have not been previously examined. To do so, we use data from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), which is a multisite, prospective cohort study of 16,415 community-dwelling Hispanic/Latino adults. In this study, we examine and describe cultural and socioeconomic correlates neurocognitive function among Hispanic/Latino adults (45- to 74-years) of Central American, Cuban, Dominican, Mexican, Puerto Rican, and South American heritage.
Methods
Study Sample
The HCHS/SOL is a multisite, prospective, population-based, cohort study. The sample design was formulated to estimate representative baseline disease risk factors for Hispanics/Latinos overall as well as for specific backgrounds, including Central Americans, Cubans, Dominicans, Mexicans, Puerto Ricans, and South Americans. Data were collected from four field centers located in major U.S. cities with substantial Hispanic/Latino population concentration. In brief, each field center (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA) recruited about 4,000 eligible, self-identified Hispanic/Latino adults (ages 18- to 74-years old; n = 16,415). Of the original sample, 87 individuals were excluded due to incomplete Latino heritage information. Middle-aged and older Hispanics/Latinos (ages 45–74 years) were oversampled (n = 9,652) and eligible for neurocognitive testing. Of that eligible sample, 59 participants were not tested with the neurocognitive battery. Neurocognitive data for this study (9,593) were collected in face-to-face interview during the baseline examination (2008–2011). Of that sample, 197 individuals were excluded from all analyses due to non-specific or mixed Hispanic/Latino background, and 333 (3.54% of eligible respondents) were excluded due to missing covariate values. Thus the analytic sample for this study includes 9,063 participants who were 45–74 years old, had a neurocognitive assessment, were of a specific background and had no missing covariate values. Means were compared to determine whether there were differences in neurocognitive performance between the analytic sample and the excluded subsample with neurocognitive testing but missing covariates. No statistically significant differences in neurocognitive function were observed across the considered tests. Detailed HCHS/SOL sampling methods have been published elsewhere (LaVange et al., 2010; Sorlie et al., 2010). The study was reviewed and approved by the Michigan State University institutional review board.
Neurocognitive Dependent Measures
The four neurocognitive tests administered in the HCHS/SOL were the: (i) Six-Item Screener (SIS) (Callahan, Unverzagt, Hui, Perkins, & Hendrie, 2002); (ii) Spanish English Verbal Learning Test (SEVLT; González, Mungas, & Haan, 2002; González, Mungas, Reed, Marshall, & Haan, 2001); (iii) Controlled Oral Word Association (COWAT or Word Fluency; WF) Test of the Multilingual Aphasia Examination (Benton & Hamsher, 1989; Lezak, Howieson, & Loring, 2004); and (iv) Digit Symbol Subtest (DSS) of the Wechsler Adult Intelligence Scale-Revised (Wechsler, 1981). To reduce participant burden, the original SEVLT and COWAT were abbreviated. For the SEVLT, three instead of five 15-word SEVLT learning trials were used. We will refer to the abbreviated SEVLT as the Brief-SEVLT (B-SEVLT) to distinguish it from the longer, original version. For the WF, two letters, F and A, served as the stimulus words, and the letter S was omitted. It should also be noted that the letters S and C are often pronounced similarly in Spanish, and using S could be a source of language bias. With the exception of the B-SEVLT, which was originally developed for English and Spanish use, the neurocognitive tests were translated from English to Spanish and backtranslated from Spanish to English. The neurocognitive tests were administered in the participants' preferred language during face-to-face interviews by study staff who were trained and supervised by doctorate-level, licensed, clinical neuropsychologists (TAM and HMG).
The SIS, like the Folstein Mini-Mental State exam, is a very brief “cognitive screener” that consists of a set of three orientation questions and a three-word list learning and memory trial (Callahan et al., 2002). The sum of correct SIS responses was the dependent measure. Following previous validation work with patients with dementia (Callahan et al., 2002), a dichotomous SIS indicator was generated to examine low mental status functioning with a score of 4 or less out of a total possible score of 6 as the cutpoint.
A detailed SEVLT description, including the translation and back-translation procedures, have been previously published (González et al., 2001). The order of B-SEVLT administration was fixed across the three learning trials using List A. After the third trial, a 15-item distractor list (List B) was introduced in which participants were asked to repeat aloud each word. Immediately following the interference trial, a delayed free-recall trial for List A occurred. The dependent measures examined were the summed total number of List A items correctly recalled across the three learning trials (Sum B-SEVLT) and the memory or delayed recall trial (B-SEVLT).
The WF test has been previously described in detail (Lezak et al., 2004). Briefly, study participants were instructed to orally generate as many unique words beginning with a specified letter (F and A) as possible within 60 s. Additionally, participants were instructed that conjugated words and proper nouns were unacceptable. The sum of correctly generated words with both letters served as the dependent measure.
Finally, the DSS test administration followed previously published instructions and procedures (Wechsler, 1981). Participants were asked to rapidly copy symbols encoded to numbers (i.e., 1–9) onto blank spaces below numbers printed on scoring sheets within 90 s.
Correlates
Consistent with neurocognitive assessment guidelines and building on previous clinical and epidemiological literature in the general and Hispanic/Latino-specific populations, we accounted for six covariates with evidenced statistical association with neurocognitive performance (APA, 2012). Sex was measured dichotomously (0 = man; 1 = woman). Age and education were measured using three-category indicators (0 = 45–54; 1 = 55–64; and 2 = 65 years+) and (0 = less than high school; 1 = high school or equivalent degree; 2 = more than high school), respectively. Age and years of education were also considered as continuous indicators and specified accordingly, and estimates from these analyses provided qualitatively similar conclusions compared with the categorical formulation. Household income was included as a four-category indicator ($20,000 or less; $20,001–50,000; 50,001 or more; and not reported). Given the sensitivity of the income question, and the relatively high number of respondents who declined to report their household income (9.6%), the “Not Reported” category was included to avoid unnecessary loss of respondent information due to missing data deletion. Language was assessed using respondents' indicated preference (0 = Spanish; 1 = English) for the language used to perform baseline examination on three core forms, including personal information, personal identifiers, and medical history. The determination of preference was based on the majority of language of choice across the three core forms. For instance, a respondent choosing English to respond to the “Personal Identifiers” and “Medical History” forms and Spanish for the “Personal Information” form would have English as their language of preference. Lastly, we accounted for depressive symptoms using respondents' scores on the 10-item Center for Epidemiological Studies Depression Scale (CES-D-10; Andresen, Malmgren, Carter, & Patrick, 1995).
To provide Hispanic/Latino-specific estimates of neurocognitive scores, we used a six-group indicator based on respondents' self-identification as one of the six major heritage groups: (i) Central American, (ii) Cuban, (iii) Dominican, (iv) Mexican, (v) Puerto Rican, and (vi) South American. Individuals specifying either “more than one” or “other” Hispanic/Latino background were excluded from the analyses to allow direct and substantive group comparisons.
Statistical Methods
Our analyses were conducted in four steps. First, we provided population-specific estimates of demographic characteristics, computed as unadjusted means and proportions, weighted to the target Hispanic/Latino population. Comparisons in demographic characteristics between Hispanic/Latino heritage groups were performed by fitting survey regression models (linear for CES-D-10; logistic for other categorical outcomes) with heritage as a categorical explanatory variable and using overall Wald tests. Second, we assessed bivariate relationships between the covariates and neurocognitive outcomes by fitting unadjusted linear regression models for complex survey data. To examine covariate relationships with the dichotomous SIS neurocognitive impairment outcome, we fit bivariate logistic regression for complex survey data to estimate weighted odds ratios and their 95% confidence intervals. Third, we used multivariate linear and logistic regression models for survey data to test the adjusted relationships between our outcomes and covariates (background, age, sex, education, income, language preference, CED-D-10 score). The final analysis step was an adjustment for study center. The fact that people with specific Hispanic/Latino backgrounds tend to concentrate in specific geographic areas meant that not all backgrounds were present in each study center, creating confounding between background and center. In particular, Cubans were predominantly in Miami, Dominicans were predominantly in the Bronx, and participants from San Diego were predominantly Mexican. We therefore examined possible center effects within background by fitting additional multivariate regression models adjusting for a background-by-center variable in place of the background variable, with levels corresponding to the 12 combinations of center and background that had 100 or more participants in the analysis sample, and one combined group for all cells with count <100 (Supplementary material online, Table S1). Results from this last step are provided as Supplementary material. All comparisons between the background-by-center groups were carried at significance levels obtained by using the Bonferroni correction for multiple comparisons.
A Taylor Series Linearization approach to variance estimation was used to obtain correct standard errors (Wolter, 2007). Regression coefficients from bivariate and multivariate models were assessed using two-tailed t-tests. Appropriate post-estimation techniques are used to assess deviations from the models' assumptions. To facilitate the interpretation of the multivariate results, we generated and plotted adjusted and unadjusted estimates of neurocognitive tests' means and probability estimates (logistic regression predicted marginals) for neurocognitive impairment, along with their confidence intervals, for each considered Hispanic/Latino background. Data analytic procedures designed for complex sample designs in the Stata software package (12.1) and SUDAAN 11.0.0 (RTI, Research Triangle Park, NC, USA) were used to perform all study analyses, and appropriate methods for subpopulations analyses of complex survey data were applied to generate our estimates. There were no adjustments for multiple comparisons, and no formal statistical hypotheses; all p-values are descriptive in nature.
Results
Demographic characteristic estimates for the target population of adults aged 45–74 living in the four study areas by Hispanic/Latino background are provided in Table 1. Cubans were, on average, older relative to the other considered groups (p < .001). Cubans and South Americans had higher levels of education (p < .001), compared with the other groups, with 46.0% and 49.7%, respectively, estimated as having more than a high school education. Mexicans were the least likely to have more than a high school education. Mexicans (16.1%) and Puerto Ricans (13.6%) were more likely to have an annual household income over U.S. $50,000. Cubans (14.2%) and Central Americans (11.5%) were more likely to decline reporting household income. The target population had a noticeable language skew with close to 6-in-7 respondents reporting Spanish as the language of preference. Puerto-Ricans (43.8%) and Mexicans (13.1%) presented the highest prevalence of respondents with English language preference (p < .001). The target population also had a slight female skew, especially present among Dominicans, Central Americans, and South Americans (p < .001). Finally, we found significant differences in depressive symptoms scores between the considered groups (p < .001). Puerto-Ricans had the highest mean CESD-10 score (M = 9.3) and Mexicans presented the lowest average score (M = 6.5).
Table 1.
Hispanic Community Health Study/Study of Latinos estimated baseline (2008–2011) characteristics of the target population (45–74 years old)
| Central American (n = 811) | Cuban (n = 919) | Dominican (n = 1,532) | Mexican (n = 3,466) | Puerto Rican (n = 1,716) | South American (n = 619) | Total (n = 9,063) | |
|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | % | |
| Age* | |||||||
| 45–54 | 50.3 | 39.4 | 51.2 | 52.2 | 45.0 | 49.3 | 46.9 |
| 45–64 | 33.6 | 30.3 | 31.8 | 32.8 | 33.6 | 31.0 | 32.1 |
| 65+ | 16.2 | 30.3 | 17.1 | 15.0 | 21.4 | 19.7 | 21.0 |
| Education* | |||||||
| Less than HS | 41.9 | 29.0 | 47.0 | 49.0 | 43.1 | 25.4 | 40.3 |
| HS or Equivalent | 19.6 | 25.0 | 18.7 | 17.9 | 23.2 | 24.9 | 21.5 |
| More than HS | 38.5 | 46.0 | 34.3 | 33.0 | 33.7 | 49.7 | 38.2 |
| Income* | |||||||
| ≤$20,00 | 48.2 | 51.7 | 51.9 | 39.0 | 47.6 | 45.1 | 46.4 |
| $20,001- | 34.5 | 28.7 | 32.4 | 38.7 | 30.8 | 37.7 | 33.5 |
| ≥$50,00 | 5.8 | 5.3 | 6.1 | 16.1 | 13.6 | 9.6 | 10.6 |
| Not Reported | 11.5 | 14.2 | 9.6 | 6.2 | 7.9 | 7.6 | 9.5 |
| Language* | |||||||
| Spanish | 95.9 | 97.7 | 95.9 | 86.9 | 56.2 | 95.0 | 86.1 |
| English | 4.1 | 2.3 | 4.1 | 13.1 | 43.8 | 5.0 | 13.9 |
| Sex* | |||||||
| Male | 39.3 | 51.4 | 39.2 | 44.0 | 46.3 | 39.8 | 45.5 |
| Female | 60.7 | 48.6 | 60.8 | 56.0 | 53.7 | 60.2 | 54.5 |
| Mean | Mean | Mean | Mean | Mean | Mean | Mean | |
| Depressive Symptoms* | |||||||
| CESD10 | 7.0 | 7.8 | 7.5 | 6.5 | 9.3 | 6.8 | 7.5 |
Note 1: All reported results are weighted to the target Hispanics/Latinos population, based on the sampling weights of the 9063 participants in the analysis set. Note 2: CES-D-10 is the 10-item Center for Epidemiological Studies Depression Scale (range 0–30).
*Differences between groups, as indicated by design adjusted overall Wald tests, were all significant at P < 0.001.
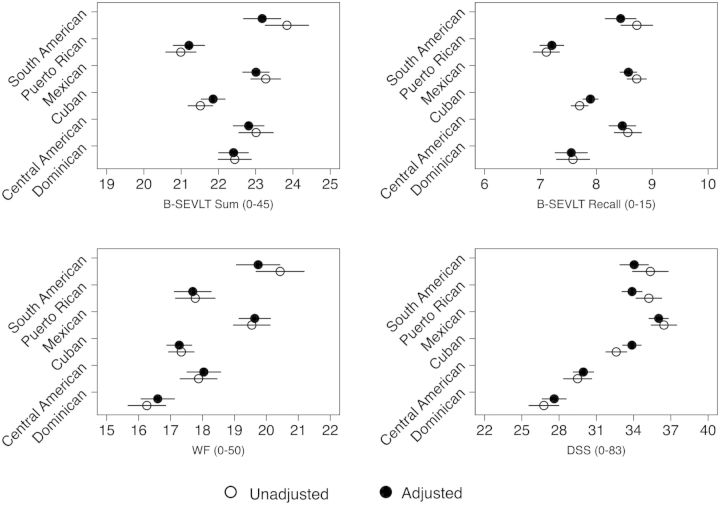
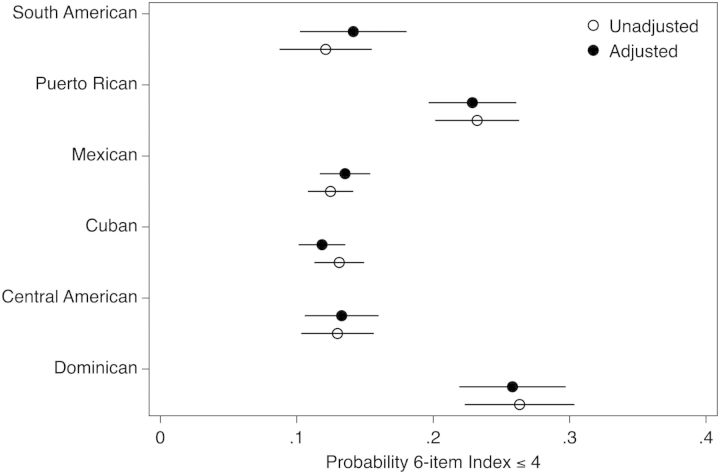
The unadjusted bivariate regressions included in Table 2 present the associations between sample demographic characteristics and neurocognitive measures. There were notable positive associations between neurocognitive performance and higher educational achievement, higher income, English language preference, and female sex. Higher scores on the CES-D-10 (i.e., higher depressive symptoms) were associated with lower levels of neurocognitive performance. We found notable Hispanic/Latino background variations in neurocognitive performance (Table 2, Fig. 1). Compared with the reference group (Mexicans), Cubans and Dominicans had significantly lower unadjusted scores on all tests. Puerto Ricans had significantly lower scores on all tests except the DSS compared with the reference group. Central Americans had significantly lower WF and DSS scores compared with the reference group. South Americans did not present any significant differences relative to Mexicans. The bivariate logistic results indicated that Dominicans and Puerto Ricans had significantly higher odds of low mental status scores (SIS ≤4) compared with the reference group (Table 2, Fig. 2). Finally, older age and higher CES-D-10 scores increased the odds of being classified as low mental status while higher educational achievement and income were associated with decreased odds of low mental status, which is in line with previous research (Callahan et al., 2002; Raji, Reyes-Ortiz, Kuo, Markides, & Ottenbacher, 2007).
Table 2.
Estimated bivariate associations between neurocognitive test scores and covariates among Hispanic/Latinos ages 45–74 years old in the target population
| B-SEVLT Sum | B-SEVLT Recall | WF | DSS | SIS ≤4 | |
|---|---|---|---|---|---|
| β (SE) | β (SE) | β (SE) | β (SE) | OR[95% CI] | |
| Background | |||||
| Central American | −0.26 (0.31) | −0.16 (0.15) | −1.67*** (0.43) | −6.95*** (0.80) | 1.05 (0.79,1.39) |
| Cuban | −1.76*** (0.27) | −1.02*** (0.12) | −2.21*** (0.37) | −3.84*** (0.70) | 1.06 (0.85,1.32) |
| Dominican | −0.83** (0.30) | −1.14*** (0.18) | −3.29*** (0.42) | −9.67*** (0.83) | 2.51*** (1.94,3.25) |
| Mexican (ref) | 23.27 (0.21) | 8.72 (0.09) | 19.54 (0.30) | 36.45 (0.54) | 1.00 (1.00,1.00) |
| Puerto Rican | −2.28*** (0.29) | −1.62*** (0.15) | −1.77*** (0.44) | −1.21 (0.76) | 2.12*** (1.68,2.68) |
| South American | 0.57 (0.37) | 0 (0.17) | 0.89 (0.49) | −1.09 (0.89) | 0.97 (0.68,1.38) |
| Age | |||||
| 45–54 (ref) | 23.57 (0.13) | 8.64 (0.07) | 18.87 (0.17) | 38.15 (0.35) | 1.00 (1.00,1.00) |
| 55–64 | −1.56*** (0.18) | −0.74*** (0.09) | −0.80** (0.27) | −6.00*** (0.40) | 1.49*** (1.25,1.79) |
| 65+ | −3.74*** (0.24) | −1.83*** (0.12) | −1.85*** (0.36) | −12.37*** (0.64) | 2.69*** (2.12,3.42) |
| Education | |||||
| Less than HS (ref) | 20.46 (0.15) | 7.26 (0.07) | 15.40 (0.23) | 26.41 (0.38) | 1.00 (1.00,1.00) |
| HS or Equivalent | 1.81*** (0.20) | 0.67*** (0.10) | 2.79*** (0.28) | 8.28*** (0.46) | 0.51*** (0.41,0.63) |
| More than HS | 3.76*** (0.21) | 1.62*** (0.10) | 5.74*** (0.29) | 14.21*** (0.47) | 0.32*** (0.26,0.40) |
| Income | |||||
| ≤$20,000 (ref) | 21.42 (0.24) | 7.62 (0.24) | 17.17 (0.24) | 30.91 (0.24) | 1.00 (1.00,1.00) |
| $20,001–$50,000 | 1.76*** (0.24) | 0.81*** (0.24) | 1.82*** (0.24) | 5.32*** (0.24) | 0.56*** (0.46,0.67) |
| ≥$50,001 | 3.35*** (0.24) | 1.60*** (0.24) | 5.21*** (0.24) | 12.97*** (0.24) | 0.33*** (0.21,0.52) |
| Not Reported | −0.84* (0.24) | −0.47* (0.24) | −1.32*** (0.24) | −4.44*** (0.24) | 1.57*** (1.24,2.00) |
| Language | |||||
| English | 0.66** (0.24) | 0.17 (0.24) | 2.17*** (0.24) | 11.04*** (0.24) | 0.84 (0.65,1.08) |
| Spanish (ref) | 22.20 (0.24) | 8.00 (0.24) | 17.93 (0.24) | 32.18 (0.24) | 1.00 (1.00,1.00) |
| Sex | |||||
| Female | 2.03*** (0.24) | 0.97*** (0.24) | 0.22 (0.24) | 1.47*** (0.24) | 0.83* (0.69,0.98) |
| Male (ref) | 21.18 (0.24) | 7.49 (0.24) | 18.11 (0.24) | 32.92 (0.24) | 1.00 (1.00,1.00) |
| Depressive Symptoms | |||||
| CESD10 (per unit increase) | −0.11*** (0.24) | −0.06*** (0.24) | −0.12*** (0.24) | −0.22*** (0.24) | 1.03*** (1.02,1.04) |
| Intercept | 23.15 (0.24) | 8.46 (0.24) | 19.12 (0.24) | 35.35 (0.24) | |
Notes: Results are from the Hispanic Community Health Study/Study of Latinos baseline (2008–2011).
Note 1: All reported results are weighted to represent the target Hispanics/Latinos population based on the sampling weights of the 9063 participants in the analysis set (actual sample size varied by outcome from N = 8,797 for the DSS outcome to N = 9,042 for Six-Item Screener due to sporadic missing data of neurocognitive tests). Note 2: The Spanish English Verbal Learning Test (SEVLT). Note 3: The Word Fluency (WF) test of the Controlled Oral Word Association Test. Note 4: The Digit Symbol Substitution (DSS) test of the Wechsler Adult Intelligence Scale-Revised. Note 5: The βs are the coefficients from unadjusted bivariate linear regression for survey data. Note 6: CES-D-10 is the 10-item Center for Epidemiological Studies Depression Scale.
***P < .001; **P < .01; *P < 005.
Fig. 1.
Unadjusted and adjusted neurocognitive test score means by Hispanic/Latino groups (ages 45–74 years old). Results are from multivariable analyses of the Hispanic Community Health Study/Study of Latinos baseline (2008–2011). Note 1: All reported results are weighted to represent the target Hispanics/Latinos population. Note 2: Unadjusted indicates unadjusted bivariate linear regression model for survey data. Note 3: Adjusted indicates fully adjusted linear regression model for survey data. Covariates include sex, age, education, household income, language and depressive symptoms (CES-D-10; 10-item Center for Epidemiological Studies Depression Scale) score. Note 4: The Spanish English Verbal Learning Test (SEVLT). Note 5: The Word Fluency (WF) test of the Controlled Oral Word Association Test. Note 6: The Digit Symbol Substitution (DSS) test of the Wechsler Adult Intelligence Scale-Revised. Note 7: Lines represent the 95% confidence intervals of the estimated means.
Fig. 2.
Unadjusted and adjusted probability estimates for low Six-Item Screener performance by Hispanic/Latino background (ages 45–74 years old). Results are from multivariable logistic analyses of the Hispanic Community Health Study/Study of Latinos baseline (2008–2011). Note 1: All reported results are weighted to represent the target Hispanics/Latinos population. Note 2: Unadjusted stands for unadjusted logistic survey regression model. Note 3: Adjusted indicates fully adjusted logistic survey regression model. Covariates include sex, age, education, household income, language and depressive symptoms (CES-D-10; 10-item Center for Epidemiological Studies Depression Scale) score. Note 4: The lines represent the 95% confidence intervals for the estimated probabilities.
Our multivariable results (Table 3) indicated that being female, with the exception of the WF test, remained consistently associated with higher neurocognitive performance relative to being male. The effects of age on WF performance were completely attenuated, but the negative association between age and neurocognitive performance remained consistent across the other considered tests. The effects of higher education and household income on all neurocognitive measures were resilient to controlling for the other covariates; small attenuations in the coefficients relative to the unadjusted results were uncovered. English language preference presented positive associations with the WF (p < .05) and DSS tests (p < .001), but not with the B-SEVLT. The CES-D-10 scale scores coefficients were also slightly diminished, but remained negatively significantly associated with all the considered neurocognitive measures; the statistical significance of the association between language and WF was relatively weaker (p < .05) in comparison to the other tests. Finally, controlling for the model covariates did not explain the bivariate differences between Hispanic/Latino backgrounds and the referent group (Table 3). The multivariable adjustments, generally, had slight attenuating effects on the estimated coefficients. The unadjusted and adjusted Hispanic/Latino background-specific neurocognitive scores are presented in Fig. 1.
Table 3.
Estimated covariate-adjusted neurocognitive test scores among Hispanic/Latino backgrounds ages 45–74 years old in the target population. Results are from multivariable analyses of the Hispanic Community Health study/Study of Latinos baseline (2008–2011)
| B-SEVLT Sum | B-SEVLT Recall | WF | DSS | SIS ≤4 | |
|---|---|---|---|---|---|
| β(SE) | β(SE) | β(SE) | β(SE) | OR(95%CI) | |
| Background | |||||
| Central American | −0.20 (0.26) | −0.11 (0.13) | −1.59*** (0.36) | −6.07*** (0.52) | 0.98 (0.73,1.31) |
| Cuban | −1.15*** (0.25) | −0.68*** (0.1) | −2.36*** (0.32) | −2.16*** (0.49) | 0.85 (0.66,1.09) |
| Dominican | −0.60* (0.25) | −1.02*** (0.16) | −3.04*** (0.35) | −8.41*** (0.58) | 2.37*** (1.81,3.11) |
| Mexican | ref (n/a) | ref (n/a) | ref (n/a) | ref (n/a) | 1.00 (1.00,1.00) |
| Puerto Rican | −1.80*** (0.27) | −1.37*** (0.13) | −1.94*** (0.39) | −2.15*** (0.53) | 1.99*** (1.52,2.61) |
| South American | 0.17 (0.31) | −0.14 (0.16) | 0.11 (0.42) | −1.97** (0.65) | 1.06 (0.72,1.55) |
| Age | |||||
| 45–54 | ref (n/a) | ref (n/a) | ref (n/a) | ref (n/a) | 1.00 (1.00,1.00) |
| 55–64 | −1.18*** (0.15) | −0.57*** (0.08) | −0.09 (0.25) | −4.36*** (0.31) | 1.34** (1.12,1.61) |
| 65+ | −3.00*** (0.21) | −1.51*** (0.11) | −0.46 (0.36) | −9.59*** (0.40) | 2.36*** (1.87,2.97) |
| Education | |||||
| Less than HS | ref (n/a) | ref (n/a) | ref (n/a) | ref (n/a) | 1.00 (1.00,1.00) |
| HS or Equivalent | 1.39*** (0.20) | 0.46*** (0.10) | 2.72*** (0.27) | 6.28*** (0.38) | 0.63*** (0.50,0.79) |
| More than HS | 3.02*** (0.20) | 1.25*** (0.09) | 5.25*** (0.27) | 11.31*** (0.37) | 0.44*** (0.35,0.55) |
| Income | |||||
| ≤$20,000 | ref (n/a) | ref (n/a) | ref (n/a) | ref (n/a) | 1.00 (1.00,1.00) |
| $20,001–$50,000 | 0.98*** (0.18) | 0.43*** (0.08) | 0.87*** (0.23) | 2.57*** (0.35) | 0.67*** (0.55,0.81) |
| ≥$50,001 | 1.85*** (0.30) | 0.89*** (0.14) | 2.59*** (0.49) | 5.83*** (0.55) | 0.48*** (0.31,0.73) |
| Not Reported | −0.59* (0.29) | −0.38* (0.17) | −0.87* (0.36) | −2.76*** (0.51) | 1.53** (1.18,1.99) |
| Language | |||||
| Spanish | ref (n/a) | ref (n/a) | ref (n/a) | ref (n/a) | 1.00 (1.00,1.00) |
| English | 0.20 (0.24) | 0.11 (0.12) | 0.88* (0.43) | 6.84*** (0.62) | 0.85 (0.62,1.18) |
| Sex | |||||
| Male | ref (n/a) | ref (n/a) | ref (n/a) | ref (n/a) | ref (n/a) |
| Female | 2.53*** (0.17) | 1.23*** (0.08) | 0.65** (0.22) | 3.31*** (0.31) | 0.65*** (0.54,0.77) |
| Depression Scale | |||||
| CESD10 | −0.09*** (0.01) | −0.05*** (0.01) | −0.05* (0.02) | −0.15*** (0.03) | 1.02** (1.01,1.03) |
| Intercept | 21.39 (0.26) | 7.96 (0.12) | 16.55 (0.41) | 30.70 (0.56) | |
Note 1: All reported results are weighted to represent the target Hispanics/Latinos population based on the sampling weights of the 9063 participants in the analysis set (actual sample size varied by outcome from N = 8,797 for the DSS outcome to N = 9,042 for Six-Item Screener due to sporadic missing data of neurocognitive tests). Note 2: The Spanish English Verbal Learning Test (SEVLT). Note 3: The Word Fluency (WF) test of the Controlled Oral Word Association Test. Note 4: The Digit Symbol Substitution (DSS) test of the Wechsler Adult Intelligence Scale-Revised. Note 5: The βs are the coefficients from multivariate linear regression for survey data and ORs are odds ratios from survey logistic regression model. Note 6: CES-D-10 is the 10-item Center for Epidemiological Studies Depression Scale) score.
***P< .001; **P < .01; *P < .05.
The results of the fully adjusted logistic regression model for low SIS performance (SIS score ≤4) also remained consistent with the bivariate findings. Older age and male sex were significantly associated with increased odds of low mental status scores, while higher education and household income presented lower odds ratios. CES-D-10 scores were not diminished and remained significantly associated with higher odds of low mental status. The effects of background were also congruent. The higher odds for Dominicans and Puerto Ricans were slightly attenuated, but remained statistically significantly higher (p < .001) relative to the Mexican reference (Table 3). The adjusted and unadjusted probability estimates of low mental status are presented in Fig. 2.
Evaluation of Field Center effects within Hispanic/Latino backgrounds identified some notable differences; however, no clear pattern of systematic Center by background differences was apparent. For the B-SEVLT-Recall, Puerto Ricans from Chicago had higher recall scores than those from the Bronx. For the Word Fluency and Digit Symbol Substitution tests, Mexicans from San Diego had higher scores than those from Chicago. For low mental status (SIS score ≤4), Central Americans from both Chicago and Miami had lower probabilities than those from the Bronx. Supplementary material online, Figs S1 and S2 depict adjusted estimates and 95% confidence intervals for each background-center combination. These results suggest that there may be some factors between regions that merit further investigation. However, overall there was no consistent pattern for the differences between the Field Center within Hispanic/Latino heritages (Supplementary material online, Table S2). Similarly, an assessment of notable differences of backgrounds within Field Center were generally consistent with overall background comparisons, with the exception that for WF and DSS, Mexicans from Chicago performed substantially lower than Mexicans from San Diego.
Discussion
In this large, community-dwelling, middle-aged, and older adult HCHS/SOL sample, we found Hispanic/Latino background and socioeconomic differences in neurocognitive performance. With the exception of mental status, Hispanics/Latinos of Caribbean (Cubans, Dominicans, and Puerto Ricans) descent had lower neurocognitive scores compared with other groups. The magnitude of background-specific differences in neurocognitive scores (DSS) in one test was sizable (i.e., −0.37 standard deviations). The adjusted average NC test scores relative to the SOL target population mean ranged from −0.16 SD among Dominicans to 0.13 SD among South Americans for the SEVLT sum, −0.23 SD among Puerto-Ricans to 0.16 among Mexicans for the SEVLT recall, −0.18 SD among Dominicans to 0.17 SD among South Americans for the WF test, and finally, −0.37 SD among Dominicans to 0.14 SD among Mexicans for the DSS. Our findings suggest that there may be more individuals with clinically significant neurocognitive test scores within some Hispanic/Latino heritage groups compared with others. However, it is not possible to ascertain clinically meaningful significance from group mean neurocognitive scores. Previous work suggests that cultural and socioeconomic factors, particularly education, could play a role in explaining some of the neurocognitive differences between Hispanic/Latino background groups. However, we found that these differences were largely maintained after statistical adjustment for sociodemographic covariates. Given that the neurocognitive scores differences we reported were not explained by the cultural and socioeconomic factors considered herein, the findings suggest that other plausible biological and non-biological explanations are needed to better understand the implications of our findings. Our HCHS/SOL findings represent the first report of neurocognitive function among previously unexamined Hispanic/Latino groups with adequately large sample sizes using sophisticated probability sampling procedures to reduce likelihood of sampling biases to confidently characterize groups based on background of origin (LaVange et al., 2010).
It is commonly believed that Hispanics/Latinos are at increased risk for dementia compared with non-Hispanic Whites. In previous work from the Sacramento Area Latinos Study on Aging (SALSA), which is mostly comprised of Mexican Americans from northern California, the prevalence of dementia was 4.8%; whereas in the Washington Heights-Inwood Columbia Aging Project (WHICAP), a largely Caribbean Hispanic/Latino cohort (i.e., Dominican, Puerto Rican, and Cuban, respectively) in New York, the prevalence of dementia was over four times higher (20.8%) (Gurland et al., 1999; Haan et al., 2003). These neuroepidemiologic differences among Hispanics/Latinos have been neglected in research for over a decade. Because SALSA and WHICAP used different methodologies (e.g., neurocognitive tests) and may have had other differences (e.g., age and SES), there remains some uncertainty that those large variations in dementia estimates could be attributable to procedural or other population differences. Since HCHS/SOL used the same methods with extensive Field Center coordination and quality control, this problem, to a large extent, was likely to have been controlled. While Mild Cognitive Impairment syndromes and dementias were not ascertained in HCHS/SOL, our findings suggest some similar patterns with previous neuroepidemiologic work that merits further investigations.
Verbal episodic learning and memory function were relatively and notably lower for participants of Puerto Rican and Cuban heritage than other groups in the HCHS/SOL cohort. DSS performance was lowest for Dominicans in the sample. The DSS is a test of psychomotor speed and working memory that has been associated with ischemic leukoaraiosis, which is strongly associated with hypertension, and has been shown to predict future stroke (Elkins, Knopman, Yaffe, & Johnston, 2005; O'Sullivan, Morris, & Markus, 2005). It is not clear from this study which, if any, biological processes may be driving these differences in neurocognitive performance. More generally, it remains to be seen, which, if any, biological factors explain the neurocognitive differences we found and if they are stable over time or accelerate. Ideally, modifiable risks for neurocognitive decline, such as diabetes and hypertension, would allow for low-cost interventions for improving public health. Our findings provide an opportunity for understanding behavioral, cultural, and biological (e.g., vascular health) factors associated with brain health in midlife and older Hispanics/Latinos, and we will be able to monitor important relationships between these factors as the cohort ages. The Global Vascular Risk Score (GVRS), which is a vascular risk prediction tool based on a racial and ethnically diverse cohort (Sacco et al., 2009), has been shown to possess better characteristics than other risk scores in predicting cognitive outcomes with older Hispanic/Latinos in the Northern Manhattan Aging Study (Warsch et al., 2013), and is a prime candidate for future consideration for predicting neurocognitive performance in HCHS/SOL. Genetic risk factors, which may vary by Hispanic/Latino backgrounds, are potential contributors to explaining neurocognitive function and disorders. A promising approach, currently underway in HCHS/SOL, is to characterize genetic variants for shared cardiovascular and neurocognitive risk factors for Hispanics/Latinos. It is expected that future studies would leverage the rich genetic data that are currently being generated to validate loci linked to CVD and neurocognitive function in the general population and establish new loci specific to Hispanics/Latinos and potentially those from diverse heritage groups.
It is possible that other cultural and socioeconomic factors not examined in this study could explain some of the between Hispanic/Latino neurocognitive performance differences we have reported. It has been argued that reading ability and vocabulary, two tests of educational achievement, may explain differences in neurocognitive performance previously observed in other studies of ethnic/racial groups (Manly, Byrd, Touradji, & Stern, 2004). However, in HCHS/SOL, Hispanic/Latino groups with the greater high school completion rates had the lowest neurocognitive performance on verbal (SEVLT and WF) and non-verbal (DSS) tests, which suggests any possible biases attributable to educational attainment differences between Hispanic/Latino backgrounds had limited impact on our results. Nevertheless, further work related to reading ability, a proxy of educational quality, might explain the neurocognitive performance differences we found in this study.
It should be noted that inferring “educational quality” based on proxy reading tests results (e.g., Wide Range Achievement Test) is more challenging in Spanish compared with English. In contrast to English, which has irregular consonant and vowel pronunciations, Spanish consonants and vowels are regular with unchanging pronunciations. Therefore, Spanish reading tests are considered less cognitively demanding compared with English tests and may be poor proxies of educational quality. As an alternative, word accentuation tests have been developed in Spain and the US on small convenience samples of older Spanish-speakers (Del Ser, González-Montalvo, Martínez-Espinosa, Delgado-Villapalos, & Bermejo, 1997; Schrauf, Weintraub, & Navarro, 2006). Picture naming vocabulary tests are widely accepted measures and have more similar cognitive demands and test characteristics to reading and traditional vocabulary tests and are available in English and Spanish in the NIH Toolbox. While proxy measurement of education quality has received considerable attention for English speakers, it is a fundamentally more complex measurement task for Spanish speakers and has not been researched to our knowledge. Additionally, conducting such studies with large samples of Hispanics/Latinos of diverse heritages in the United States has not been feasible until the advent of studies like HCHS/SOL. HCHS/SOL data are publically available data and investigators with interests in educational quality measurement among diverse English- and Spanish-speaking Hispanics/Latinos are encouraged to consider using this rich resource.
The HCHS/SOL cohort was selected through a stratified multi-stage area probability sample of four communities (LaVange et al., 2010). The probability-based sampling allows HCHS/SOL to estimate prevalence of diseases and baseline risk factors in the target population, which included all non-institutionalized Hispanic/Latino adults aged 18–74 years (45–74 for this study) residing in the four defined community areas. The selected communities were from different US regions with high concentrations of Hispanic/Latino heritages, allowing us to derive risk factors and disease prevalence estimates for each background. Although the target populations were limited to four communities rather than nationally, the HCHS/SOL hybrid design, which uses probability sampling within pre-selected diverse regions, is superior to the convenience samples that are typically used in neuropsychological and neuroepidemiologic cohort studies. Nevertheless, the HCHS/SOL study design (e.g., possible regional differences associated with Field Center locations) limits generalizations of our findings to Hispanics/Latinos at the national level. Neurocognitive measurement invariance between language and Hispanic/Latino heritage groups was not evaluated in this study. Therefore, it cannot be ruled-in or ruled-out that measurement bias contributed to the differences reported herein. Previous work for the SEVLT, language and sex bias were reportedly minimal for older Mexican-origin adults (Mungas, Reed, Haan, & Gonzalez, 2005). However, additional in-depth work is needed to examine possible sources of bias. Nevertheless, the relative magnitude of differences between the reference group and other Hispanic/Latino groups ranged from 2% to 23.3%. While the highest between group differences were seen in episodic memory and processing speed scores, pathological inferences based on our findings would be premature and additional information would be required before such any inferences could be made. As such, neurocognitive disorders, such as Mild Cognitive Impairment or dementia, were not ascertained and such clinical inferences cannot be made from this study.
In summary, this is the largest study of neurocognitive function among middle-aged and older Hispanics/Latinos of diverse backgrounds. The differences we found between Hispanic/Latino heritage groups raise several questions about the brain health, function and aging of this demographically important population that merit further investigation within the HCHS/SOL cohort.
Supplementary Material
Supplementary material online Material is available at Archives of Clinical Neuropsychology online.
Funding
This work was supported by the National Institutes of Health, National Heart Lung Blood Institute, and the National Institute of Mental Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Conflict of Interest
None declared.
Supplementary Material
Acknowledgements
The authors thank the staff and participants of HCHS/SOL for their important contributions. Investigators website—http://www.cscc.unc.edu/hchs/.
References
- Andresen E. M., Malmgren J. A., Carter W. B., Patrick D. L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1995;10(2):77–84. [PubMed] [Google Scholar]
- APA. Guidelines for the evaluation of dementia and age-related cognitive change. American Psychologist. 2012;67(1):1–9. doi: 10.1037/a0024643. [DOI] [PubMed] [Google Scholar]
- Benton A. L., Hamsher K. Multilingual aphasia examination. 2nd ed. Iowa City: AJA Associates; 1989. [Google Scholar]
- Callahan C. M., Unverzagt F. W., Hui S. L., Perkins A. J., Hendrie H. C. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40(9):771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- Census. We Are the Americans...hispanics. Washington, DC: U.S. Dept. of the Commerce Economics and Statistics Administration Bureau of the Census; 2004. [Google Scholar]
- Census. American Community Survey. 2011. http://census.gov/en.html. (Accessed on 6 January 2014)
- Del Ser T., González-Montalvo J.-I., Martínez-Espinosa S., Delgado-Villapalos C., Bermejo F. Estimation of Premorbid Intelligence in Spanish People with the Word Accentuation Test and Its Application to the Diagnosis of Dementia. Brain and Cognition. 1997;33(3):343–356. doi: 10.1006/brcg.1997.0877. [DOI] [PubMed] [Google Scholar]
- Elkins J. S., Knopman D. S., Yaffe K., Johnston S. C. Cognitive function predicts first-time stroke and heart disease. Neurology. 2005;64(10):1750–1755. doi: 10.1212/01.WNL.0000161850.01792.77. [DOI] [PubMed] [Google Scholar]
- González H. M., Mungas D., Haan M. N. A verbal learning and memory test for English- and Spanish-speaking older Mexican-American adults. The Clinical Neuropsychologist. 2002;16(4):439–451. doi: 10.1076/clin.16.4.439.13908. [DOI] [PubMed] [Google Scholar]
- González H. M., Mungas D. M., Reed B. R., Marshall S., Haan M. N. A new verbal learning and memory test for English- and Spanish-speaking older people. Journal of the International Neuropsychological Society. 2001;7(5):544–555. doi: 10.1017/s1355617701755026. [DOI] [PubMed] [Google Scholar]
- González H. M., Vega W. A., Williams D. R., Tarraf W., West B. T., Neighbors H. W. Depression Care in the United States: Too Little for Too Few. Archives of General Psychiatry. 2010;67(1):37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurland B. J., Wilder D. E., Lantigua R., Stern Y., Chen J., Killeffer E. H., et al. Rates of dementia in three ethnoracial groups. International Journal of Geriatric Psychiatry. 1999;14(6):481–493. [PubMed] [Google Scholar]
- Haan M. N., Mungas D. M., González H. M., Ortiz T. A., Acharya A., Jagust W. J. Prevalence of dementia in older Latinos: The influence of type 2 diabetes mellitus, stroke and genetic factors. Journal of the American Geriatrics Society. 2003;51(2):169–177. doi: 10.1046/j.1532-5415.2003.51054.x. [DOI] [PubMed] [Google Scholar]
- LaVange L. M., Kalsbeek W. D., Sorlie P. D., Avilés-Santa L. M., Kaplan R. C., Barnhart J., et al. Sample Design and Cohort Selection in the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology. 2010;20(8):642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezak M., Howieson D. B., Loring D. W. Neuropsychological assessment. New York: Oxford University Press; 2004. [Google Scholar]
- Manly J. J., Byrd D. A., Touradji P., Stern Y. Acculturation, reading level, and neuropsychological test performance among African American elders. Applied Neuropsychology. 2004;11(1):37–46. doi: 10.1207/s15324826an1101_5. [DOI] [PubMed] [Google Scholar]
- Miranda P. Y., Tarraf W., González P., Johnson-Jennings M., González H. M. Breast Cancer Screening Trends in the United States and Ethnicity. Cancer Epidemiology Biomarkers & Prevention. 2012;21(2):351–357. doi: 10.1158/1055-9965.EPI-11-0873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mungas D., Reed B. R., Haan M. N., Gonzalez H. Spanish and English neuropsychological assessment scales: Relationship to demographics, language, cognition, and independent function. Neuropsychology. 2005;19(4):466–475. doi: 10.1037/0894-4105.19.4.466. [DOI] [PubMed] [Google Scholar]
- O'Sullivan M., Morris R. G., Markus H. S. Brief cognitive assessment for patients with cerebral small vessel disease. Journal of Neurology, Neurosurgery & Psychiatry. 2005;76(8):1140–1145. doi: 10.1136/jnnp.2004.045963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raji M. A., Reyes-Ortiz C. A., Kuo Y.-F., Markides K. S., Ottenbacher K. J. Depressive Symptoms and Cognitive Change in Older Mexican Americans. Journal of Geriatric Psychiatry and Neurology. 2007;20(3):145–152. doi: 10.1177/0891988707303604. [DOI] [PubMed] [Google Scholar]
- Sacco R. L., Khatri M., Rundek T., Xu Q., Gardener H., Boden-Albala B., et al. Improving Global Vascular Risk Prediction With Behavioral and Anthropometric Factors: The Multiethnic NOMAS (Northern Manhattan Cohort Study) Journal of the American College of Cardiology. 2009;54(24):2303–2311. doi: 10.1016/j.jacc.2009.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrauf R. W., Weintraub S., Navarro E. Is adaptation of the Word Accentuation Test of Premorbid Intelligence necessary for use among older, Spanish-speaking immigrants in the United States? Journal of the International Neuropsychological Society. 2006;12(03):391–399. doi: 10.1017/s1355617706060462. [DOI] [PubMed] [Google Scholar]
- Sorlie P. D., Avilés-Santa L. M., Wassertheil-Smoller S., Kaplan R. C., Daviglus M. L., Giachello A. L., et al. Design and Implementation of the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology. 2010;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warsch J. R., Rundek T., Paik M. C., Elkind M. S., Sacco R. L., Wright C. B. Association between northern Manhattan study global vascular risk score and successful aging. Journal of the American Geriatrics Society. 2013;61(4):519–524. doi: 10.1111/jgs.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. WAIS-R Manual. San Antonio, TX: Psychological Corporation; 1981. [Google Scholar]
- Wolter K. M. Introduction to variance estimation. 2nd ed. New York: Springer; 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.