Abstract
Metabolic syndrome (MetS) is a cluster of cardiovascular risk factors that includes obesity, diabetes, and dyslipidemia. Accumulating evidence implies that MetS contributes to the development and progression of Alzheimer's disease (AD); however, the factors connecting this association have not been determined. Insulin resistance (IR) is at the core of MetS and likely represent the key link between MetS and AD. In the central nervous system, insulin plays key roles in learning and memory, and AD patients exhibit impaired insulin signaling that is similar to that observed in MetS. As we face an alarming increase in obesity and T2D in all age groups, understanding the relationship between MetS and AD is vital for the identification of potential therapeutic targets. Recently, several diabetes therapies that enhance insulin signaling are being tested for a potential therapeutic benefit in AD and dementia. In this review, we will discuss MetS as a risk factor for AD, focusing on IR and the recent progress and future directions of insulin-based therapies.
Metabolic syndrome (MetS) is a major contributor for the development of diabetes.1 A subject is diagnosed with MetS when he/she has central obesity plus any two of four additional factors, which include elevated triglycerides, reduced high density lipoprotein (HDL) cholesterol, hypertension, or abnormal fasting plasma glucose. The National Health and Nutrition Examination Survey study found that MetS affects 34% of adults in the US.2 The incidence increases with both higher body mass index (BMI) and advancing age. Insulin resistance (IR) is a state of decreased responsiveness of target tissues to normal circulating levels of insulin and is a major feature of type 2 diabetes (T2D), glucose intolerance, obesity, dyslipidemia and hypertension; that is, MetS.3 Both genetic and environmental factors such as a lack of exercise, obesity, smoking, stress, and aging affect the development of IR.4
Alzheimer's disease (AD) is a slow progressing terminal neurodegenerative disease that can that can remain asymptomatic for several decades.5 It is the most common form of dementia, accounting for over 70% of all cases. Aging is the most definitive risk factor for AD, with the incidence doubling every five years in the population over 65 years old; 50% of people over 85 years old are affected by various degrees of AD. Currently, 5.2 million Americans have AD, and this number is expected to rise to 16 million by 2050 without a breakthrough in the treatment and prevention of the disease (http://www.alz.org/downloads/Facts_Figures_2014.pdf). AD is estimated to cost American society $214 billion in direct medical expenses; a cost expected to rise to $1.2 trillion (in today's dollars) in 2050. At the cellular level, the most prominent neuropathological features of AD are the appearance of senile plaques composed of amyloid β (Aβ) peptides and neurofibrillary tangles (NFTs) derived from the aggregation of the microtubule-associated protein, tau.6 Clinically, AD is characterized by the loss of memory and other cognitive functions necessary to perform complex daily activities.5
Multiple studies demonstrate a strong connection between MetS and the increased risk of AD.7, 8, 9 Accumulating evidence also suggests that AD is closely related to dysfunction of bothinsulin signaling and glucose metabolism in the brain, prompting some investigators to refer AD as type 3 diabetes or an insulin-resistant brain state.10, 11 In this manuscript, we will review recent findings connecting MetS and AD, focusing on IR as the major link between the two diseases.
Metabolic syndrome and insulin signaling
Insulin plays a critical role in glucose homeostasis by regulating the balance between glucose production by the liver and glucose uptake by muscle and adipose tissues. In adipocytes and myocytes, insulin regulates glucose transport by controlling the translocation of the glucose transporter, (Glut)4.12 IR has a rather loose definition, but generally refers to the fact that tissues do not respond sufficiently to physiological insulin concentrations. T2D patients usually have hyperinsulinemia, and poor insulin sensitivity is a common characteristic of obesity and hyperlipidaemia.4, 13
Insulin initiates its effects by binding to the extracellular α-subunit of insulin receptor (InsR), resulting in autophosphorylation of the intracellular β-subunit.14 Once activated, the InsR recruits and phosphorylates intracellular substrates, including InsR substrate (IRS) family proteins and Shc. Phosphorylated tyrosine residues on IRS and Shc then recruit downstream signaling molecules containing Src homology 2 (SH2) domains, such as the p85 subunit of phosphatidylinositol 3 kinase (PI3K), which activates Akt-mediated signaling, and growth factor receptor-binding protein 2 (Grb2), which leads to the activation of mitogen-activated protein kinase (MAPK) signaling pathway.15
In addition to over 20 tyrosine residues, IRS proteins contain more than 50 potential serine/threonine phosphorylation sites. In general, IRS serine/threonine phosphorylation inhibits insulin signaling by antagonizing tyrosine phosphorylation.15 Increased serine/threonine phosphorylation of IRS-1 accelerates its dissociation from the InsR and downstream signaling molecules, induces mislocalization, and accelerates its degradation by the ubiquitin-proteasome pathway. Multiple IRS serine kinases are activated during IR, resulting in increased IRS serine phosphorylation and impaired insulin signaling.15 Increased IRS serine phosphorylation in IR states, including obesity and T2D, are reported in both animal and human studies.16, 17
Akt (Akt1, Akt2, and Akt3), also known as PKB (PKBα, PKBβ, and PKBγ), is a serine/threonine kinase activated by PI3K downstream of growth factors and various cellular stimuli.18 Many molecules involved in Akt signaling are the key therapeutic targets for the treatment of human diseases, including T2D and cancer. Akt mediates the bulk of insulin's action, including glycogen, lipid, and protein synthesis, cell survival, and the anti-inflammatory response. Alterations in Akt activity are one of the key characteristics of IR. Akt2 activation is closely correlated to Glut4 translocation via insulin-activated PI3K signals in adipocytes,19 and T2D patients have reduced Akt activation in adipocytes and skeletal muscle.18 Akt2 knockout mice have impaired insulin action in liver and skeletal muscle and develop diabetes with hyperglycemia, hyperinsulinemia, glucose intolerance, and impaired muscle glucose uptake.18
In contrast to the decrease in PI3K-Akt activity, the MAPK pathway is relatively unaffected by IR.20 MAPK pathway activation by insulin signaling is responsible for gene expression, cell growth, and mitogenesis.4 MAPK acts as an IRS serine kinase in certain conditions;15 therefore, inappropriate activation of MAPK may worsen IR by increasing serine phosphorylation of IRS and interfering with insulin signaling.
Insulin signaling in the brain
Insulin, a peptide secreted by pancreatic beta cells, enters the central nervous system by crossing the blood–brain barrier in a regulated and saturable fashion, although de novo synthesis of insulin in the brain is still under debate.21 InsRs are widely expressed in the brain, including in the olfactory bulb, cerebral cortex, hippocampus, hypothalamus, and amygdala.22 InsRs are more concentrated in neurons relative to glial cells and are especially high in post-synaptic densities.22
Brain insulin signaling plays critical roles in the regulation of food intake, body weight, reproduction, and learning and memory.23 Intranasal insulin administration improves working memory in both human and animal studies,24 and intrahippocampal delivery of insulin improves hippocampal-dependent spatial working memory.25 In addition, InsR mRNA and protein levels are increased in the hippocampus CA1 region in association with short-term memory formation after a spatial memory task,26 suggesting that neuronal insulin sensitivity could be enhanced during learning.
Disruption of insulin signaling, however, makes neurons more vulnerable to metabolic stress, thus accelerating neuronal dysfunction. Defective insulin signaling is associated with decreased cognitive ability and the development of dementia, including AD.27 Poor cognitive performance in diabetes and AD are associated with a decrease in InsR expression and cerebrospinal fluid (CSF) insulin levels.28, 29 A recent study demonstrated decreases in the phosphorylation of similar insulin signaling molecules in both AD and T2D patient brains, and this decrease was more severe in the brains of the patients with both AD and T2D.30 Decreased insulin signaling, including altered kinase activity and IRS expression, in AD gets worse with disease progression,31, 32 and increased basal IRS-1 phosphorylation, a key signature of IR, is evident in the AD brain.33 Interestingly, the brain regions with the highest densities of InsR, such as the hippocampus and temporal lobe, are also the major targets of neurodegeneration in AD.34, 35, 36 Therefore, impaired insulin signaling caused by IR can have a profound effect on cognitive decline and the development of AD.
MetS and AD
Multiple studies report that patients with MetS have an increased risk of developing AD compared to age- and gender-matched controls, and accumulating evidence suggests that AD is closely related to dysfunction of both insulin signaling and glucose metabolism in the brain, prompting some investigators to refer AD as type 3 diabetes, or an insulin resistant brain state.10, 11 The incidence of both T2D and dementia rise in later life, increasing the prevalence of the comorbidity of these age-related diseases. Indeed, T2D predicts cognitive decline in older adults37 and is related not only to vascular dementia (VD), but also to AD.32 One of the pioneering epidemiological studies about the connection between T2D and dementia is the Rotterdam study,38 which demonstrates that T2D almost doubles the risk of dementia AD; interestingly, people who were insulin-treated (therefore, with more severe diabetes) at baseline were at the highest risk. Another study on a Japanese-Hawaiian cohort further showed a 1.5-, 1.8-, and 2.3-fold increased risk of total dementia, AD, and VD, respectively, for people with diabetes.39 The Religious Order Study demonstrated a 65% increased risk of AD among T2D patients.40 Among the diabetes-related factors, higher levels of 2-hour post-load plasma glucose, fasting insulin, and homeostasis model assessment-estimated IR (HOMA-IR) were associated with increased risk for senile plaques after adjustment for age, sex, systolic blood pressure, total cholesterol, BMI, habitual smoking, regular exercise, and cerebrovascular disease.8 A detailed analysis of 14 high quality longitudinal studies from MEDLINE and EMBASE searches41 further demonstrates that individuals with T2D have a greater than two-fold increased risk of developing AD compared to individuals without T2D, adjusted for age, sex, education, and vascular risk factors (including a history of stroke, hypertension, and heart disease). The duration of diabetes is also a risk factor for increased cognitive decline, and this may be related to the length of exposure to high levels of insulin combined with the severity of disease.42 The converse is also true, as patients with AD are also more likely to develop diabetes. The Mayo Clinic AD Patient Registry reveals that 80% of AD patients have either T2D or an impaired fasting glucose level.43
Animal studies also demonstrate the connection between diabetes and AD. We have reported that db/db mice, a model of T2D, exhibit age-dependent increases in tau phosphorylation and cleavage.44, 45 Inducing type 1 diabetes (T1D) and IR by streptozotocin (STZ) treatment or by feeding with a high fat diet (HFD) in AD animal models exacerbates both amyloid and tau accumulation.46, 47 High-fat and high carbohydrate diet feeding of AD rats significantly increased hyperphosphorylated tau and total tau mRNA compared to rats with T2D or AD alone, and there was also a significant difference in spatial memory deficits between AD and AD+T2D groups.48
Obesity is a pathologic state defined by an excessive accumulation and maintenance of adipose tissue. BMI is a simple index of weight-for-height that is commonly used to classify overweight and obese adults (kg m−2). Worldwide, obesity has nearly doubled between 1980–2008, with ~35% and ~11% of adults currently overweight or obese, respectively (http://www.who.int/mediacentre/factsheets/fs311/en/). In the United States, the epidemic is even worse; 35% of adults and 15% of children were obese in 2010 and 80% of obese individuals are insulin resistant.49, 50 Obesity has been associated with several processes related to the acceleration of aging, including the excessive production of free radicals, oxidation, and inflammation.51 Visceral adipose tissue is a metabolically active endocrine organ, and dysfunction in this organ is responsible for increased plasma free fatty acids (FFAs).51 The inappropriate accumulation of lipids in muscle and liver due to abnormal fatty acid metabolism is one of the main features of IR. Visceral fat is also infiltrated with inflammatory cells and secretes proinflammatory cytokines, such as interleukin 6 and tumor necrosis factor-α,52 which are implicated in the development of IR. Furthermore, these proinflammatory cytokines produced by adipocytes can cross the blood-brain barrier (BBB) and induce neuroinflammation and subsequent neurodegeneration.53, 54 Increased inflammation induces accelerated Aβ deposition and/or decreased clearance53 and facilitates the polymerization of tau.55 FFAs also increase tau phosphorylation through astroglia-mediated oxidative stress.56
Midlife obesity (measured by BMI) consistently demonstrates a strong and independent association with late-onset dementia and AD.57 In a 30 year longitudinal study involving 6583 members of Kaiser Permanente of Northern California, central obesity (sagittal abdominal diameter) alone doubled the risk of dementia after adjusting for age, sex, race, education, marital status, diabetes, hypertension, hyperlipidemia, stroke, heart disease, and medical utilization.58 Studies examining later onset obesity, however, have generated mixed results. In the Cardiovascular Health Study, which involved people 65 years or older, underweight individuals (BMI<20) had an increased risk of dementia (hazard ratio [HR]=1.62), whereas obese individuals (BMI>30) exhibited a reduced risk (HR=0.63) relative to normal BMI controls.59 Another study found a decreased risk of dementia with higher BMI in subjects over 76 years old, and BMI and dementia further exhibited a U-shaped correlation in individuals younger than 76 years.60
Similar results have been observed in animal studies. Rats fed with diets high in saturated or unsaturated fat for 3 months display impairments in learning and memory tasks,61 and mice fed with a HFD have impaired spatial working memory, as assessed by a T-maze.62 Furthermore, brains of HFD-fed mice exhibit dysfunctional Akt signaling and increased IRS serine phosphorylation, a marker of IR, and mice fed with a high fat/high cholesterol diet display increased APP C-terminal fragment accumulation63 and increased tau phosphorylation.64 These results suggest that obesity-induced peripheral IR alters central insulin signaling and leads to AD-like cognitive impairment.
Dyslipidemia is an important component of IR. Because insulin plays a critical role in lipid metabolism by stimulating lipogenesis and suppressing lipolysis, perturbations in insulin signaling lead to accelerated lipolysis and increased production of FFAs.65 Approximately 30% of total body cholesterol is contained in the brain; therefore, slight changes in lipid metabolism may have profound effects on cognitive function. Cholesterol is the key component of the plasma membrane, and the processing of APP into Aβ occurs in the plasma membrane.66, 67 The interaction between cholesterol and APP in the plasma membrane is critical for Aβ production and clearance. In Tg2576 AD mice, a high-fat/high-cholesterol diet significantly increased the production of Aβ,68 and cholesterol lowering drugs reduced this brain amyloid load by more than two-fold.69 Lowering cholesterol levels in vitro also stimulates non-amyloidogenic processing of APP, thereby reducing Aβ production.70
A meta-analysis of 18 prospective studies ranging from 3–29 years revealed a consistent association between high midlife total cholesterol and an increased risk of AD and dementia.71 Interestingly, no evidence was found to support an association between total cholesterol later in life and AD. Cohorts of the Seven Countries Study by a Finnish group concluded that high serum total cholesterol is an independent risk factor for AD,72 while another Finnish study further demonstrated that high midlife cholesterol levels are positively connected with an increased risk of AD later in life.73 Further, a retrospective cohort study of members of the Kaiser Permanente Medical Care Program of Northern California showed that midlife cardiovascular risk factors including smoking, hypertension, high cholesterol, and diabetes are all positively connected with increased dementia in later life, with diabetes and high cholesterol being the strongest risk factors.74 Despite these findings, however, the connection between cholesterol and dementia is still complex and inconclusive, as some studies show no correlation, and others even demonstrate a protective role for cholesterol.75, 76
IR and tau
Abnormal phosphorylation of tau has been implicated as a mechanism of AD pathophysiology since the mid-1980s.77 Tau is commonly regulated by post-translational modifications, including phosphorylation, glycation, glycosylation, sumoylation, O-GlcNAcylation, and cleavage.78 In AD, tau is abnormally phosphorylated at its over 80 serine/threonine residues, which leads to the aggregation of tau filaments, appearing as NFTs, in cell bodies and proximal dendrites. Several kinases, including glycogen synthase kinase-3 beta (GSK3β), cyclin-dependent kinase 5, MAPK, and microtubule affinity-regulating kinases, and phosphatases, such as protein phosphatase 2A, are responsible for tau phosphorylation.78 These kinases and phosphatases are the targets of insulin regulation.78, 79, 80 As in peripheral tissues, IR mostly affects PI3K-Akt signaling in the brain, and chronic hyperinsulinemia prevents insulin-stimulated Akt phosphorylation in cortical neuron cultures.81 Increased basal Akt phosphorylation is also present in the cortex of T2D db/db mice, and ex vivo insulin stimulation could not increase cortical Akt phosphorylation as it did in non-diabetic control mouse (db+).81 GSK3β is one of the key signaling molecules downstream of Akt82 and is a major tau kinase. Impaired insulin signaling results in aberrant GSK3β activation and increased tau phosphorylation and accumulation.81 Therefore, the precise regulation of Akt signaling is critical for both amyloid and tau neuropathology in AD.
Impaired glucose metabolism due to IR can affect tau pathology via the dysregulation of O-GlcNAcylation. Similar to phosphorylation, O-GlcNAcylation is a dynamic post-translational modification involving the attachment of N-acetyl-D-glucosamine (GlcNAc) moieties to the hydroxyl group of serine and threonine residues.83 O-GlcNAcylation is affected by nutrients in circulation, especially glucose;84 therefore, the accumulation of excess energy associated with obesity and IR can result in the dysregulation of O-GlcNAcylation. Furthermore, in some cases, O-GlcNAcylation may occur at or near the residues that can also be phosphorylated.85 Tau has at least 12 O-GlcNAcylation sites which are mostly inversely correlated with phosphorylation status.83 Recent reports demonstrate that reduced brain glucose metabolism and O-GlcNAcylation leads to increased tau phosphorylation in both in vivo and in vitro models.86 Conversely, increased O-GlcNAcylation prevents pathological tau accumulation.87 Thus, the failure of proper insulin signaling can promote the accumulation of neurofibrillary tau, disrupt neuronal cytoskeletal networks and axonal transport, and lead to a loss of synaptic connections and progressive neurodegeneration.
Abnormal phosphorylation of IRS-1 is also a pathological feature of AD. A recent study examining 157 human brain autopsies demonstrated that IRS-1 serine phosphorylation is increased in multiple sites in AD, and in other tauopathies such as Pick's disease, corticobasal degeneration and progressive supranuclear palsy.88 Furthermore, increased IRS-1 serine phosphorylation was frequently co-expressed with pathologic tau in neurons and dystrophic neurites.88 Similar results were observed in transgenic PS19 tau mouse brains, where abnormally increased IRS-1 serine phosphorylation co-localized with tangle-bearing neurons.89 Conversely, inducing IR by feeding mice a HFD increased tau phosphorylation and impaired insulin signaling,62, 64, 90 and high fat-feeding of animal models of AD exacerbated the pathologies. After 23 wk on HFD, APPswe/PS1dE9 mice displayed severe hyperinsulinemia along with increased tau phosphorylation, Aβ levels, and amyloid burden.91 HFD-feeding from an early age in THY-Tau22 mice also potentiated spatial learning deficits and significantly increased tau phosphorylation,92 and direct disruption of insulin signaling by inducing T1D using STZ93 or IRS-2 knockout94 increased tau pathology. In addition, STZ injections in pR5 tau transgenic mice greatly increased insoluble hyperphosphorylated tau and the later deposition of NFTs, features not observed in control pR5 mice.47 Together, these results suggest that IR accelerates the onset and increases the severity of AD, especially in situations with a predisposition to developing tau pathology.
IR and Aβ
Brain insulin signaling plays a critical role in the regulation of food intake, body weight, reproduction, and learning and memory,23 and defective insulin signaling is associated with decreased cognitive ability and the development of dementia and AD.27 AD is characterized by improper expression and processing of APP and the accumulation of insoluble neurotoxic Aβ into subsequent senile plaques. Studies show that insulin signaling regulates multiple steps of the amyloid cascade and affects Aβ aggregation in the brain. Insulin increases the transcription of anti-amyloidogenic proteins, such as the insulin-degrading enzyme (IDE) and α-secretase, and stimulates Aβ clearance.95 While GSK3β is the major tau kinase, GSK3α increases Aβ production by stimulating γ-secretase activity.96 Constitutively active Akt inhibits APP trafficking and Aβ secretion through feedback inhibition of IRS and PI3-K.97 APP is modified by O-GlcNAc in a region that may affect its degradation, and a recent report demonstrated that O-GlcNAcylation of APP encourages non-amyloidogenic α-secretase processing, thus decreasing Aβ secretion.98
Conversely, Aβ can affect insulin signaling by competing with or reducing the affinity of insulin binding to its own receptor or by regulating intracellular signaling. Soluble Aβ binds to the InsR in hippocampal neurons to inhibit receptor autophosphorylation and subsequent activation of PI3K/Akt,99 and Aβ derived diffusible ligands (ADDLs) induce the abnormal expression of InsR and interrupt insulin signaling, thereby potentially contributing the development of central IR.100, 101 In addition, Aβ inhibits insulin signaling by c-Jun N-terminal kinase (JNK)-mediated increases in IRS serine phosphorylation.89 Intracellularly, Aβ prevents the interaction of pyruvate dehydrogenase lipoamide kinase isozyme 1 (PDK1) with Akt to inhibit Akt activation.102 Therefore, a feed-forward interaction between impaired insulin signaling and increased Aβ production exacerbates AD pathology in the presence of IR.
In a recent cross-sectional study of the Wisconsin Registry for Alzheimer's Prevention that included187 late middle-aged adults, higher IR levels were connected with increased amyloid deposition, as measured by Pittsburgh compound B uptake.103 Inducing IR in rats using fructose-containing water also enhanced Aβ production by increasing the expression of β-secretase, stimulating γ-secretase activity, and decreasing IDE levels.104 In cultured primary cortical neurons, insulin reduced Aβ buildup by enhancing the conversion of oligomers to monomers and also prevented Aβ oligomer-induced synaptic toxicity at the level of both synapse composition and structure.105 In contrast, inhibiting InsR activity by transfecting a kinase-dead mutant receptor or a tyrosine kinase inhibitor increased Aβ oligomer aggregation;105 similar results were obtained through either InsR knock-down or PI3K pathway inhibition.106 Thus, dysfunctional insulin signaling due to IR accelerates amyloid pathology, both in human and animal models.
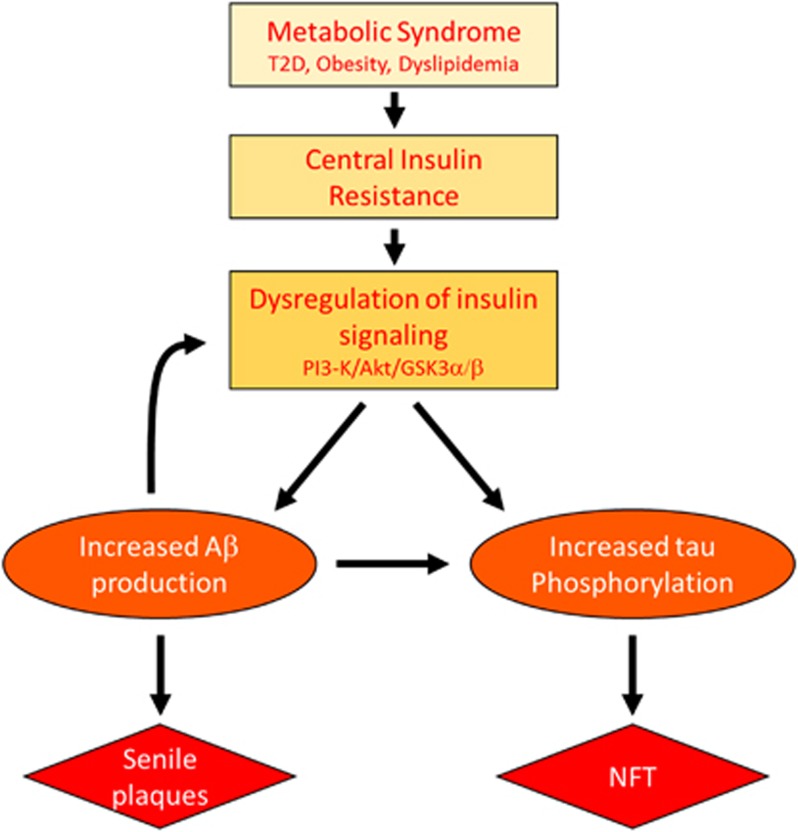
In summary, peripheral MetS induces central IR in the brain. The resulting impaired insulin signaling, which mainly impacts the PI3K/Akt pathway, then increases APP processing/Aβ levels and tau phosphorylation. Finally, increased Aβ further disrupts insulin signaling to exacerbate AD pathology and cognitive decline (Figure 1).
Figure 1.
MetS and AD Aβ/tau pathology may act in a feed-forward mechanism to accelerate AD pathology in the presence of IR.
Insulin signaling as a therapeutic target of AD
Given the close correlation between brain IR and cognitive impairment, therapeutic approaches using anti-diabetic drugs to improve insulin levels or signaling have been tested to treat AD. In rats, intracerebroventricular (icv) administration of insulin improved spatial learning and memory107 and reversed STZ-induced cognitive decline,108 and intranasal delivery of insulin reduced HFD-induced tau phosphorylation, whereas subcutaneous injection only had a minimal effect.109 Although systemic insulin infusion demonstrated beneficial effects on memory,110 it is not a viable long-term option for AD patients due to adverse hypoglycemic effects, including cognitive deficits and neuronal death.111 Intranasal delivery of insulin, however, is a safe and effective alternative to increase CSF insulin concentrations without affecting systemic insulin and glucose levels, and studies have demonstrated the beneficial effects of intranasal insulin on memory function.24 Intranasal insulin delivery for 8 wk improved delayed word recall test in cognitively normal young adults,24, 112 and a single-dose intranasal insulin administration improved verbal memory in subjects with AD and mild cognitive impairment (MCI).113 In a subsequent study, chronic intranasal insulin for 21 days resulted in enhanced declarative memory and selective attention performance in early AD patients.114 Intranasal insulin also increased plasma Aβ40/Aβ42 ratios, suggesting decreased amyloid pathology levels.114 Likewise, daily intranasal insulin treatment for 4 months in 104 adults with early AD or amnestic MCI also improved delayed memory and preserved caregiver-rated ability to carry out daily functions.115 These studies provide compelling evidence that intranasal insulin may be a promising novel therapeutic approach for early AD and MCI patients; however, it should also be noted that some studies suggest that intranasal insulin treatment is effective only in individuals with ApoE-ɛ4-negative genotypes.113, 116
Thiazolidinediones (TZDs), rosiglitazone, and pioglitazone are ligands for peroxisome proliferator-activated receptors (PPARs), a family of nuclear receptors that regulate the transcription of genes involved in lipid and glucose metabolism.117 TZDs have been used as an anti-diabetic drug since the 1990s due to their beneficial effects on glucose homeostasis, which include increasing insulin sensitivity, reducing blood glucose levels and improving lipid metabolism. A number of animal and clinical studies further suggest that TZDs improve cognitive function by enhancing insulin action. Early treatment with PPAR agonists effectively prevented icv-STZ-induced neurodegeneration and its associated learning and memory deficits,118 and rosiglitazone similarly improved learning and memory and reduced IDE mRNA levels in Tg2576 AD mice.119 Chronic treatment with rosiglitazone also facilitated Aβ clearance, reduced amyloid plaques, decreased tau phosphorylation, and improved cognitive function in AD mouse models,120, 121 and pioglitazone prevented IR and Aβ overproduction that are associated with fructose-drinking in rats.104 Some studies, however, show inconsistent results depending on gender and/or genotype of the selected animal models.122, 123
Likewise, there are mixed results from human clinical trials with TZDs. An early study demonstrated that mild AD or amnestic MCI patients who received rosiglitazone for 6 months exhibited better delayed recall and selective attention,124 and rosiglitazone protected cognitive decline in older individuals with both T2D and MCI.125 Similar to intranasal insulin treatment, the effect of rosiglitazone was effective only on the individuals with ApoE-ɛ4-negative genotypes.126 More recent follow-up studies show disappointing results with rosiglitazone. A multicenter trial proved no effect of rosiglitazone on brain atrophy or cognitive function in AD patients,127 and two large phase III clinical trials also demonstrated no evidence of clinically significant efficacy in cognition or global function, regardless of ApoE-ɛ4 genotype.128, 129 Pioglitazone has produced similarly mixed results. Two prospective randomized open-labelled studies demonstrated that pioglitazone induced cognitive and functional improvements and stabilization of the disease in the individuals with mild AD and MCI with T2D.130, 131 However, another study evaluating the safety of pioglitazone as the primary outcome exhibited no significant treatment effect on cognition after 6 months of treatment in non-diabetic AD patients.132
Incretins, glucose-dependent insulinotropic peptide (GIP) and glucagon-like peptide-1 (GLP-1), are a group of gastrointestinal hormones secreted by intestinal epithelial cells in response to food intake that can affect whole body glucose utilization.133 GLP-1 receptors are widely expressed throughout the body, including in the pancreas, intestines, heart, and lungs, and in both the central and the peripheral nervous system.134 The activation of GLP-1 receptors leads to the facilitation of glucose utilization and antiapoptotic effects in various organs,135, 136 and two long-lasting GLP-1 analogues, exenatide (Byetta) and liraglutide (Victoza), are approved for the treatment of T2D. More importantly, GLP-1 can readily cross the BBB and enhance insulin signaling in the brain.137, 138 Therefore, GLP-1 analogues are an attractive therapeutic approach to improve IR in AD and in T2D because they can activate pathways common to insulin signaling and facilitate brain synaptic plasticity, cognition, and cell survival.139, 140
Excendin-4 prevented glucose-induced tau hyperphosphorylation or Aβ-mediated toxicity in cultured neurons,141, 142 and subcutaneous injection of liraglutide for 30 days reduced icv-STZ-induced tau hyperphosphorylation and significantly improved learning and memory in mice.143 Two months of liraglutide injections in APP/PS1 mice reduced plaque load, APP and Aβ oligomer levels, and overall inflammation and increased IDE levels.144 Furthermore, long-term potentiation was significantly enhanced and liraglutide also improved cognitive function, as measured by novel object recognition and Morris water maze tests. Liraglutide not only has a protective effect at an early stage of AD (7 mo),145 but it is also able to reverse AD-related changes in older (14 mo) APP/PS1 mice.144 Moreover, liraglutide reduced tau phosphorylation and restored Akt and GSK3β phosphorylation in a HFD-induced model of T2D in rats.146 Other GLP-1 analogues demonstrated similar beneficial effects on AD pathologies and cognitive function in AD mouse models.147, 148, 149
Although the first small clinical trial of liraglutide in AD patients did not lead to any improvement in cognition or changes in Aβ deposition, as measured by Pittsburgh compound B PET,150 a recent clinical trial of exenatide in Parkinson's disease patients demonstrated clinically relevant improvements in motor and cognitive measures.151 Currently two additional clinical trials are in progress with exenatide (http://clinicaltrials.gov/ct2/show/NCT01255163?term) and liraglutide (http://clinicaltrials.gov/ct2/show/NCT01843075?term) in MCI and early AD patients, and completion is estimated in 2016 and 2017, respectively.
Conclusion
Recent evidence supports the contention that AD may be a slow-progressing brain metabolic disease, and numerous studies demonstrate an intricate connection between MetS and AD. Individuals with MetS features, such as T2D and obesity, have a higher risk of developing AD, while AD patients often develop hyperglycemia and IR. IR due to impaired insulin signaling is a common characteristic of both MetS and AD, and likely represents the key link between the two diseases. Insulin signaling regulates Aβ and tau, and Aβ has negative effects on insulin signaling; therefore, dysfunctional insulin signaling can enhance Aβ and tau pathology, and increased Aβ production can further exacerbate IR. Thus, several diabetes treatments that enhance insulin signaling are being tested for therapeutic potential in AD and dementia, and even though the results from the TZD clinical trials were disappointing, intranasal insulin and GLP-1 analogues are still being actively pursued as a potential treatments for AD and have exhibited some promising results. Intranasal insulin, however, is only effective in early AD and MCI patients, and individuals with the ApoE-ɛ4 allele do not respond well. In addition, exenatide and liraglutide are still in the early stages of therapeutic development, and large clinical trials are currently in progress.
Effective AD and MCI treatment demands the development of specific biomarkers to support the diagnosis of these conditions as early as possible. Currently, total tau, hyperphosphorylated tau, and Aβ40/Aβ42 ratios in the CSF exhibit over 80% specificity as biomarkers of AD.152, 153 Continued research to discover the precise mechanism of how IR contributes to the onset and progression of AD, is also imperative for the development of improved therapeutic interventions. Given the current obesity epidemic among all ages and increased life expectancy, there is a critical need to understand the underlying causes of cognitive impairment due to IR, which may be the key link for the increased incidence of AD in individuals with metabolic disorders.
Acknowledgments
Support during the preparation of this review was received from the Program for Neurology Research & Discovery, the A. Alfred Taubman Medical Research Institute, and the National Institutes of Health (1DP3DK094292 and R24 082841 to ELF). The authors would also like to thank Dr Stacey Sakowski for critical review of this manuscript.
References
- Duvnjak L, Duvnjak M. The metabolic syndrome—an ongoing story. J Physiol Pharmacol. 2009;60:19–24. [PubMed] [Google Scholar]
- Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Report. 2009;5:1–7. [PubMed] [Google Scholar]
- Bruce KD, Hanson MA. The developmental origins, mechanisms, and implications of metabolic syndrome. J Nutr. 2010;140:648–652. doi: 10.3945/jn.109.111179. [DOI] [PubMed] [Google Scholar]
- Sesti G. Pathophysiology of insulin resistance. Best Pract Res Clin Endocrinol Metab. 2006;20:665–679. doi: 10.1016/j.beem.2006.09.007. [DOI] [PubMed] [Google Scholar]
- Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E. Alzheimer's disease. Lancet. 2011;377:1019–1031. doi: 10.1016/S0140-6736(10)61349-9. [DOI] [PubMed] [Google Scholar]
- Selkoe D, Mandelkow E, Holtzman D. Deciphering Alzheimer disease. Cold Spring Harbor perspectives in medicine. 2012;2:a011460. doi: 10.1101/cshperspect.a011460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrijvers EM, Witteman JC, Sijbrands EJ, Hofman A, Koudstaal PJ, Breteler MM. Insulin metabolism and the risk of Alzheimer disease: the Rotterdam Study. Neurology. 2010;75:1982–1987. doi: 10.1212/WNL.0b013e3181ffe4f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuzaki T, Sasaki K, Tanizaki Y, Hata J, Fujimi K, Matsui Y, et al. Insulin resistance is associated with the pathology of Alzheimer disease: the Hisayama study. Neurology. 2010;75:764–770. doi: 10.1212/WNL.0b013e3181eee25f. [DOI] [PubMed] [Google Scholar]
- Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68:51–57. doi: 10.1001/archneurol.2010.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisardi V, Solfrizzi V, Capurso C, Imbimbo BP, Vendemiale G, Seripa D, et al. Is insulin resistant brain state a central feature of the metabolic-cognitive syndrome. J Alzheimers Dis. 2010;21:57–63. doi: 10.3233/JAD-2010-100015. [DOI] [PubMed] [Google Scholar]
- Lester-Coll N, Rivera EJ, Soscia SJ, Doiron K, Wands JR, de la Monte SM. Intracerebral streptozotocin model of type 3 diabetes: relevance to sporadic Alzheimer's disease. J Alzheimers Dis. 2006;9:13–33. doi: 10.3233/jad-2006-9102. [DOI] [PubMed] [Google Scholar]
- Huang S, Czech MP. The GLUT4 glucose transporter. Cell Metab. 2007;5:237–252. doi: 10.1016/j.cmet.2007.03.006. [DOI] [PubMed] [Google Scholar]
- Muntoni S, Muntoni S. Insulin resistance: pathophysiology and rationale for treatment. Ann Nutr Metab. 2011;58:25–36. doi: 10.1159/000323395. [DOI] [PubMed] [Google Scholar]
- Kim B, Feldman EL. Insulin resistance in the nervous system. Trends Endocrinol Metab. 2012;23:133–141. doi: 10.1016/j.tem.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boura-Halfon S, Zick Y. Phosphorylation of IRS proteins, insulin action, and insulin resistance. Am J Physiol Endocrinol Metab. 2009;296:E581–E591. doi: 10.1152/ajpendo.90437.2008. [DOI] [PubMed] [Google Scholar]
- Bouzakri K, Roques M, Gual P, Espinosa S, Guebre-Egziabher F, Riou JP, et al. Reduced activation of phosphatidylinositol-3 kinase and increased serine 636 phosphorylation of insulin receptor substrate-1 in primary culture of skeletal muscle cells from patients with type 2 diabetes. Diabetes. 2003;52:1319–1325. doi: 10.2337/diabetes.52.6.1319. [DOI] [PubMed] [Google Scholar]
- Langlais P, Yi Z, Finlayson J, Luo M, Mapes R, De Filippis E, et al. Global IRS-1 phosphorylation analysis in insulin resistance. Diabetologia. 2011;54:2878–2889. doi: 10.1007/s00125-011-2271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay N. Akt isoforms and glucose homeostasis—the leptin connection. Trends Endocrinol Metab. 2011;22:66–73. doi: 10.1016/j.tem.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez E, McGraw TE. Insulin-modulated Akt subcellular localization determines Akt isoform-specific signaling. Proc Natl Acad Sci USA. 2009;106:7004–7009. doi: 10.1073/pnas.0901933106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusi K, Maezono K, Osman A, Pendergrass M, Patti ME, Pratipanawatr T, et al. Insulin resistance differentially affects the PI 3-kinase- and MAP kinase-mediated signaling in human muscle. J Clin Invest. 2000;105:311–320. doi: 10.1172/JCI7535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskin DG, Figlewicz DP, Woods SC, Porte D, Jr, Dorsa DM. Insulin in the brain. Annu Rev Physiol. 1987;49:335–347. doi: 10.1146/annurev.ph.49.030187.002003. [DOI] [PubMed] [Google Scholar]
- Unger JW, Livingston JN, Moss AM. Insulin receptors in the central nervous system: localization, signalling mechanisms and functional aspects. Prog Neurobiol. 1991;36:343–362. doi: 10.1016/0301-0082(91)90015-s. [DOI] [PubMed] [Google Scholar]
- van der Heide LP, Ramakers GM, Smidt MP. Insulin signaling in the central nervous system: learning to survive. Prog Neurobiol. 2006;79:205–221. doi: 10.1016/j.pneurobio.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Benedict C, Frey WH, 2nd, Schioth HB, Schultes B, Born J, Hallschmid M. Intranasal insulin as a therapeutic option in the treatment of cognitive impairments. Exp Gerontol. 2011;46:112–115. doi: 10.1016/j.exger.2010.08.026. [DOI] [PubMed] [Google Scholar]
- McNay EC, Ong CT, McCrimmon RJ, Cresswell J, Bogan JS, Sherwin RS. Hippocampal memory processes are modulated by insulin and high-fat-induced insulin resistance. Neurobiol Learn Mem. 2010;93:546–553. doi: 10.1016/j.nlm.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao W, Chen H, Xu H, Moore E, Meiri N, Quon MJ, et al. Brain insulin receptors and spatial memory. Correlated changes in gene expression, tyrosine phosphorylation, and signaling molecules in the hippocampus of water maze trained rats. J Biol Chem. 1999;274:34893–34902. doi: 10.1074/jbc.274.49.34893. [DOI] [PubMed] [Google Scholar]
- de la Monte SM. Insulin resistance and Alzheimer's disease. BMB Rep. 2009;42:475–481. doi: 10.5483/bmbrep.2009.42.8.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte AI, Moreira PI, Oliveira CR. Insulin in central nervous system: more than just a peripheral hormone. Journal of aging research. 2012;2012:384017. doi: 10.1155/2012/384017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moloney AM, Griffin RJ, Timmons S, O'Connor R, Ravid R, O'Neill C. Defects in IGF-1 receptor, insulin receptor and IRS-1/2 in Alzheimer's disease indicate possible resistance to IGF-1 and insulin signalling. Neurobiol Aging. 2010;31:224–243. doi: 10.1016/j.neurobiolaging.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Liu Y, Liu F, Grundke-Iqbal I, Iqbal K, Gong CX. Deficient brain insulin signalling pathway in Alzheimer's disease and diabetes. J Pathol. 2011;225:54–62. doi: 10.1002/path.2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosco D, Fava A, Plastino M, Montalcini T, Pujia A. Possible implications of insulin resistance and glucose metabolism in Alzheimer's disease pathogenesis. J Cell Mol Med. 2011;15:1807–1821. doi: 10.1111/j.1582-4934.2011.01318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Holscher C. Common pathological processes in Alzheimer disease and type 2 diabetes: a review. Brain Res Rev. 2007;56:384–402. doi: 10.1016/j.brainresrev.2007.09.001. [DOI] [PubMed] [Google Scholar]
- Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky A, et al. Demonstrated brain insulin resistance in Alzheimer's disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest. 2012;122:1316–1338. doi: 10.1172/JCI59903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Monte SM, Wands JR. Review of insulin and insulin-like growth factor expression, signaling, and malfunction in the central nervous system: relevance to Alzheimer's disease. J Alzheimers Dis. 2005;7:45–61. doi: 10.3233/jad-2005-7106. [DOI] [PubMed] [Google Scholar]
- Freude S, Schilbach K, Schubert M. The role of IGF-1 receptor and insulin receptor signaling for the pathogenesis of Alzheimer's disease: from model organisms to human disease. Curr Alzheimer Res. 2009;6:213–223. doi: 10.2174/156720509788486527. [DOI] [PubMed] [Google Scholar]
- Gammeltoft S, Fehlmann M, Van Obberghen E. Insulin receptors in the mammalian central nervous system: binding characteristics and subunit structure. Biochimie. 1985;67:1147–1153. doi: 10.1016/s0300-9084(85)80113-9. [DOI] [PubMed] [Google Scholar]
- Tilvis RS, Kahonen-Vare MH, Jolkkonen J, Valvanne J, Pitkala KH, Strandberg TE. Predictors of cognitive decline and mortality of aged people over a 10-year period. J Gerontol A Biol Sci Med Sci. 2004;59:268–274. doi: 10.1093/gerona/59.3.m268. [DOI] [PubMed] [Google Scholar]
- Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology. 1999;53:1937–1942. doi: 10.1212/wnl.53.9.1937. [DOI] [PubMed] [Google Scholar]
- Peila R, Rodriguez BL, Launer LJ. Type 2 diabetes, APOE gene, and the risk for dementia and related pathologies: The Honolulu-Asia Aging Study. Diabetes. 2002;51:1256–1262. doi: 10.2337/diabetes.51.4.1256. [DOI] [PubMed] [Google Scholar]
- Leibson CL, Rocca WA, Hanson VA, Cha R, Kokmen E, O'Brien PC, et al. Risk of dementia among persons with diabetes mellitus: a population-based cohort study. Am J Epidemiol. 1997;145:301–308. doi: 10.1093/oxfordjournals.aje.a009106. [DOI] [PubMed] [Google Scholar]
- Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol. 2006;5:64–74. doi: 10.1016/S1474-4422(05)70284-2. [DOI] [PubMed] [Google Scholar]
- Cosway R, Strachan MW, Dougall A, Frier BM, Deary IJ. Cognitive function and information processing in type 2 diabetes. Diabet Med. 2001;18:803–810. doi: 10.1046/j.1464-5491.2001.00577.x. [DOI] [PubMed] [Google Scholar]
- Janson J, Laedtke T, Parisi JE, O'Brien P, Petersen RC, Butler PC. Increased risk of type 2 diabetes in Alzheimer disease. Diabetes. 2004;53:474–481. doi: 10.2337/diabetes.53.2.474. [DOI] [PubMed] [Google Scholar]
- Kim B, Backus C, Oh S, Hayes JM, Feldman EL. Increased tau phosphorylation and cleavage in mouse models of type 1 and type 2 diabetes. Endocrinology. 2009;150:5294–5301. doi: 10.1210/en.2009-0695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim B, Backus C, Oh S, Feldman EL. Hyperglycemia-induced Tau cleavage in vitro and in vivo: a possible link between diabetes and Alzheimer's disease. J Alzheimers Dis. 2013;34:727–739. doi: 10.3233/JAD-121669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohjima M, Sun Y, Chan L. Increased food intake leads to obesity and insulin resistance in the tg2576 Alzheimer's disease mouse model. Endocrinology. 2010;151:1532–1540. doi: 10.1210/en.2009-1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ke YD, Delerue F, Gladbach A, Gotz J, Ittner LM. Experimental diabetes mellitus exacerbates tau pathology in a transgenic mouse model of Alzheimer's disease. PLoS ONE. 2009;4:e7917. doi: 10.1371/journal.pone.0007917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma YQ, Wu DK, Liu JK. mTOR and tau phosphorylated proteins in the hippocampal tissue of rats with type 2 diabetes and Alzheimer's disease. Molecular medicine reports. 2013;7:623–627. doi: 10.3892/mmr.2012.1186. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS data brief. 2012;106:1–8. [PubMed] [Google Scholar]
- Pan L, Blanck HM, Sherry B, Dalenius K, Grummer-Strawn LM. Trends in the prevalence of extreme obesity among US preschool-aged children living in low-income families, 1998–2010. JAMA. 2012;308:2563–2565. doi: 10.1001/jama.2012.108099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf G. Role of fatty acids in the development of insulin resistance and type 2 diabetes mellitus. Nutr Rev. 2008;66:597–600. doi: 10.1111/j.1753-4887.2008.00110.x. [DOI] [PubMed] [Google Scholar]
- Espinola-Klein C, Gori T, Blankenberg S, Munzel T. Inflammatory markers and cardiovascular risk in the metabolic syndrome. Front Biosci. 2011;16:1663–1674. doi: 10.2741/3812. [DOI] [PubMed] [Google Scholar]
- Spielman LJ, Little JP, Klegeris A. Inflammation and insulin/IGF-1 resistance as the possible link between obesity and neurodegeneration. J Neuroimmunol. 2014;273:8–21. doi: 10.1016/j.jneuroim.2014.06.004. [DOI] [PubMed] [Google Scholar]
- Meraz-Rios MA, Toral-Rios D, Franco-Bocanegra D, Villeda-Hernandez J, Campos-Pena V. Inflammatory process in Alzheimer's Disease. Frontiers in integrative neuroscience. 2013;7:59. doi: 10.3389/fnint.2013.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamblin TC, King ME, Kuret J, Berry RW, Binder LI. Oxidative regulation of fatty acid-induced tau polymerization. Biochemistry. 2000;39:14203–14210. doi: 10.1021/bi001876l. [DOI] [PubMed] [Google Scholar]
- Patil S, Chan C. Palmitic and stearic fatty acids induce Alzheimer-like hyperphosphorylation of tau in primary rat cortical neurons. Neurosci Lett. 2005;384:288–293. doi: 10.1016/j.neulet.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Whitmer RA, Gunderson EP, Quesenberry CP, Jr, Zhou J, Yaffe K. Body mass index in midlife and risk of Alzheimer disease and vascular dementia. Curr Alzheimer Res. 2007;4:103–109. doi: 10.2174/156720507780362047. [DOI] [PubMed] [Google Scholar]
- Whitmer RA, Gustafson DR, Barrett-Connor E, Haan MN, Gunderson EP, Yaffe K. Central obesity and increased risk of dementia more than three decades later. Neurology. 2008;71:1057–1064. doi: 10.1212/01.wnl.0000306313.89165.ef. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick AL, Kuller LH, Lopez OL, Diehr P, O'Meara ES, Longstreth WT, Jr, et al. Midlife and late-life obesity and the risk of dementia: cardiovascular health study. Arch Neurol. 2009;66:336–342. doi: 10.1001/archneurol.2008.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchsinger JA, Patel B, Tang MX, Schupf N, Mayeux R. Measures of adiposity and dementia risk in elderly persons. Arch Neurol. 2007;64:392–398. doi: 10.1001/archneur.64.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winocur G, Greenwood CE. Studies of the effects of high fat diets on cognitive function in a rat model. Neurobiol Aging. 2005;26:46–49. doi: 10.1016/j.neurobiolaging.2005.09.003. [DOI] [PubMed] [Google Scholar]
- Arnold SE, Lucki I, Brookshire BR, Carlson GC, Browne CA, Kazi H, et al. High fat diet produces brain insulin resistance, synaptodendritic abnormalities and altered behavior in mice. Neurobiol Dis. 2014;67C:79–87. doi: 10.1016/j.nbd.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirumangalakudi L, Prakasam A, Zhang R, Bimonte-Nelson H, Sambamurti K, Kindy MS, et al. High cholesterol-induced neuroinflammation and amyloid precursor protein processing correlate with loss of working memory in mice. J Neurochem. 2008;106:475–485. doi: 10.1111/j.1471-4159.2008.05415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat NR, Thirumangalakudi L. Increased Tau phosphorylation and impaired brain insulin/IGF signaling in mice fed a high fat/high cholesterol diet. J Alzheimers Dis. 2013;36:781–789. doi: 10.3233/JAD-2012-121030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czech MP, Tencerova M, Pedersen DJ, Aouadi M. Insulin signalling mechanisms for triacylglycerol storage. Diabetologia. 2013;56:949–964. doi: 10.1007/s00125-013-2869-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Scala C, Chahinian H, Yahi N, Garmy N, Fantini J. Interaction of Alzheimer's beta-amyloid peptides with cholesterol: mechanistic insights into amyloid pore formation. Biochemistry. 2014;53:4489–4502. doi: 10.1021/bi500373k. [DOI] [PubMed] [Google Scholar]
- Wood WG, Li L, Muller WE, Eckert GP. Cholesterol as a causative factor in Alzheimer's disease: a debatable hypothesis. J Neurochem. 2014;129:559–572. doi: 10.1111/jnc.12637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Refolo LM, Malester B, LaFrancois J, Bryant-Thomas T, Wang R, Tint GS, et al. Hypercholesterolemia accelerates the Alzheimer's amyloid pathology in a transgenic mouse model. Neurobiol Dis. 2000;7:321–331. doi: 10.1006/nbdi.2000.0304. [DOI] [PubMed] [Google Scholar]
- Refolo LM, Pappolla MA, LaFrancois J, Malester B, Schmidt SD, Thomas-Bryant T, et al. A cholesterol-lowering drug reduces beta-amyloid pathology in a transgenic mouse model of Alzheimer's disease. Neurobiol Dis. 2001;8:890–899. doi: 10.1006/nbdi.2001.0422. [DOI] [PubMed] [Google Scholar]
- Kojro E, Gimpl G, Lammich S, Marz W, Fahrenholz F. Low cholesterol stimulates the nonamyloidogenic pathway by its effect on the alpha -secretase ADAM 10. Proc Natl Acad Sci USA. 2001;98:5815–5820. doi: 10.1073/pnas.081612998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anstey KJ, Lipnicki DM, Low LF. Cholesterol as a risk factor for dementia and cognitive decline: a systematic review of prospective studies with meta-analysis. Am J Geriatr Psychiatry. 2008;16:343–354. doi: 10.1097/JGP.0b013e31816b72d4. [DOI] [PubMed] [Google Scholar]
- Notkola IL, Sulkava R, Pekkanen J, Erkinjuntti T, Ehnholm C, Kivinen P, et al. Serum total cholesterol, apolipoprotein E epsilon 4 allele, and Alzheimer's disease. Neuroepidemiology. 1998;17:14–20. doi: 10.1159/000026149. [DOI] [PubMed] [Google Scholar]
- Kivipelto M, Helkala EL, Laakso MP, Hanninen T, Hallikainen M, Alhainen K, et al. Midlife vascular risk factors and Alzheimer's disease in later life: longitudinal, population based study. Bmj. 2001;322:1447–1451. doi: 10.1136/bmj.322.7300.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology. 2005;64:277–281. doi: 10.1212/01.WNL.0000149519.47454.F2. [DOI] [PubMed] [Google Scholar]
- Reitz C, Tang MX, Schupf N, Manly JJ, Mayeux R, Luchsinger JA. Association of higher levels of high-density lipoprotein cholesterol in elderly individuals and lower risk of late-onset Alzheimer disease. Arch Neurol. 2010;67:1491–1497. doi: 10.1001/archneurol.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielke MM, Zandi PP, Sjogren M, Gustafson D, Ostling S, Steen B, et al. High total cholesterol levels in late life associated with a reduced risk of dementia. Neurology. 2005;64:1689–1695. doi: 10.1212/01.WNL.0000161870.78572.A5. [DOI] [PubMed] [Google Scholar]
- Grundke-Iqbal I, Iqbal K, Tung YC, Quinlan M, Wisniewski HM, Binder LI. Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci USA. 1986;83:4913–4917. doi: 10.1073/pnas.83.13.4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal K, Liu F, Gong CX, Alonso Adel C, Grundke-Iqbal I. Mechanisms of tau-induced neurodegeneration. Acta Neuropathol. 2009;118:53–69. doi: 10.1007/s00401-009-0486-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M, Gautam D, Surjo D, Ueki K, Baudler S, Schubert D, et al. Role for neuronal insulin resistance in neurodegenerative diseases. Proc Natl Acad Sci USA. 2004;101:3100–3105. doi: 10.1073/pnas.0308724101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat RV, Budd Haeberlein SL, Avila J. Glycogen synthase kinase 3: a drug target for CNS therapies. J Neurochem. 2004;89:1313–1317. doi: 10.1111/j.1471-4159.2004.02422.x. [DOI] [PubMed] [Google Scholar]
- Kim B, Sullivan KA, Backus C, Feldman EL. Cortical neurons develop insulin resistance and blunted Akt signaling: a potential mechanism contributing to enhanced ischemic injury in diabetes. Antioxid Redox Signal. 2011;14:1829–1839. doi: 10.1089/ars.2010.3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takashima A. GSK-3 is essential in the pathogenesis of Alzheimer's disease. J Alzheimers Dis. 2006;9:309–317. doi: 10.3233/jad-2006-9s335. [DOI] [PubMed] [Google Scholar]
- Dias WB, Hart GW. O-GlcNAc modification in diabetes and Alzheimer's disease. Mol Biosyst. 2007;3:766–772. doi: 10.1039/b704905f. [DOI] [PubMed] [Google Scholar]
- Myslicki JP, Belke DD, Shearer J. Role of O-GlcNAcylation in nutritional sensing, insulin resistance and in mediating the benefits of exercise. Appl Physiol Nutr Metab. 2014;39:1205–1213. doi: 10.1139/apnm-2014-0122. [DOI] [PubMed] [Google Scholar]
- Whelan SA, Hart GW. Proteomic approaches to analyze the dynamic relationships between nucleocytoplasmic protein glycosylation and phosphorylation. Circ Res. 2003;93:1047–1058. doi: 10.1161/01.RES.0000103190.20260.37. [DOI] [PubMed] [Google Scholar]
- Deng Y, Li B, Liu Y, Iqbal K, Grundke-Iqbal I, Gong CX. Dysregulation of insulin signaling, glucose transporters, O-GlcNAcylation, and phosphorylation of tau and neurofilaments in the brain: Implication for Alzheimer's disease. Am J Pathol. 2009;175:2089–2098. doi: 10.2353/ajpath.2009.090157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuzwa SA, Cheung AH, Okon M, McIntosh LP, Vocadlo DJ. O-GlcNAc modification of tau directly inhibits its aggregation without perturbing the conformational properties of tau monomers. J Mol Biol. 2014;426:1736–1752. doi: 10.1016/j.jmb.2014.01.004. [DOI] [PubMed] [Google Scholar]
- Yarchoan M, Toledo JB, Lee EB, Arvanitakis Z, Kazi H, Han LY, et al. Abnormal serine phosphorylation of insulin receptor substrate 1 is associated with tau pathology in Alzheimer's disease and tauopathies. Acta Neuropathol. 2014;128:679–689. doi: 10.1007/s00401-014-1328-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma QL, Yang F, Rosario ER, Ubeda OJ, Beech W, Gant DJ, et al. Beta-amyloid oligomers induce phosphorylation of tau and inactivation of insulin receptor substrate via c-Jun N-terminal kinase signaling: suppression by omega-3 fatty acids and curcumin. J Neurosci. 2009;29:9078–9089. doi: 10.1523/JNEUROSCI.1071-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvo-Ochoa E, Hernandez-Ortega K, Ferrera P, Morimoto S, Arias C. Short-term high-fat-and-fructose feeding produces insulin signaling alterations accompanied by neurite and synaptic reduction and astroglial activation in the rat hippocampus. J Cereb Blood Flow Metab. 2014;34:1001–1008. doi: 10.1038/jcbfm.2014.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Rodriguez JJ, Ortiz-Barajas O, Gamero-Carrasco C, de la Rosa PR, Infante-Garcia C, Zopeque-Garcia N, et al. Prediabetes-induced vascular alterations exacerbate central pathology in APPswe/PS1dE9 mice. Psychoneuroendocrinology. 2014;48:123–135. doi: 10.1016/j.psyneuen.2014.06.005. [DOI] [PubMed] [Google Scholar]
- Leboucher A, Laurent C, Fernandez-Gomez FJ, Burnouf S, Troquier L, Eddarkaoui S, et al. Detrimental Effects of Diet-Induced Obesity on tau Pathology Are Independent of Insulin Resistance in tau Transgenic Mice. Diabetes. 2013;62:1681–1688. doi: 10.2337/db12-0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planel E, Tatebayashi Y, Miyasaka T, Liu L, Wang L, Herman M, et al. Insulin dysfunction induces in vivo tau hyperphosphorylation through distinct mechanisms. J Neurosci. 2007;27:13635–13648. doi: 10.1523/JNEUROSCI.3949-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M, Brazil DP, Burks DJ, Kushner JA, Ye J, Flint CL, et al. Insulin receptor substrate-2 deficiency impairs brain growth and promotes tau phosphorylation. J Neurosci. 2003;23:7084–7092. doi: 10.1523/JNEUROSCI.23-18-07084.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandini G, Pace V, Copani A, Squatrito S, Milardi D, Vigneri R. Insulin has multiple antiamyloidogenic effects on human neuronal cells. Endocrinology. 2013;154:375–387. doi: 10.1210/en.2012-1661. [DOI] [PubMed] [Google Scholar]
- Muyllaert D, Kremer A, Jaworski T, Borghgraef P, Devijver H, Croes S, et al. Glycogen synthase kinase-3beta, or a link between amyloid and tau pathology. Genes Brain Behav. 2008;7:57–66. doi: 10.1111/j.1601-183X.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- Shineman DW, Dain AS, Kim ML, Lee VM. Constitutively active Akt inhibits trafficking of amyloid precursor protein and amyloid precursor protein metabolites through feedback inhibition of phosphoinositide 3-kinase. Biochemistry. 2009;48:3787–3794. doi: 10.1021/bi802070j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun YS, Park Y, Oh HG, Kim TW, Yang HO, Park MK, et al. O-GlcNAcylation Promotes Non-Amyloidogenic Processing of Amyloid-beta Protein Precursor via Inhibition of Endocytosis from the Plasma Membrane. J Alzheimers Dis. 2014;44:261–275. doi: 10.3233/JAD-140096. [DOI] [PubMed] [Google Scholar]
- Townsend M, Mehta T, Selkoe DJ. Soluble Abeta inhibits specific signal transduction cascades common to the insulin receptor pathway. J Biol Chem. 2007;282:33305–33312. doi: 10.1074/jbc.M610390200. [DOI] [PubMed] [Google Scholar]
- De Felice FG, Vieira MN, Bomfim TR, Decker H, Velasco PT, Lambert MP, et al. Protection of synapses against Alzheimer's-linked toxins: insulin signaling prevents the pathogenic binding of Abeta oligomers. Proc Natl Acad Sci USA. 2009;106:1971–1976. doi: 10.1073/pnas.0809158106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Teng Z, Cui C, Wang R, Liu M, Zhang Y. Amyloid beta-derived diffusible ligands (ADDLs) induce abnormal expression of insulin receptors in rat hippocampal neurons. J Mol Neurosci. 2014;52:124–130. doi: 10.1007/s12031-013-0216-0. [DOI] [PubMed] [Google Scholar]
- Lee HK, Kumar P, Fu Q, Rosen KM, Querfurth HW. The insulin/Akt signaling pathway is targeted by intracellular beta-amyloid. Mol Biol Cell. 2009;20:1533–1544. doi: 10.1091/mbc.E08-07-0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willette AA, Johnson SC, Birdsill AC, Sager MA, Christian B, Baker LD, et al. Insulin resistance predicts brain amyloid deposition in late middle-aged adults Alzheimer's Dement(e-pub ahead of print 17 July 2014; doi: 10.1016/j.jalz.2014.03.011 [DOI] [PMC free article] [PubMed]
- Luo D, Hou X, Hou L, Wang M, Xu S, Dong C, et al. Effect of pioglitazone on altered expression of Abeta metabolism-associated molecules in the brain of fructose-drinking rats, a rodent model of insulin resistance. Eur J Pharmacol. 2011;664:14–19. doi: 10.1016/j.ejphar.2011.04.045. [DOI] [PubMed] [Google Scholar]
- Zhao WQ, Lacor PN, Chen H, Lambert MP, Quon MJ, Krafft GA, et al. Insulin receptor dysfunction impairs cellular clearance of neurotoxic oligomeric a{beta} J Biol Chem. 2009;284:18742–18753. doi: 10.1074/jbc.M109.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto N, Matsubara T, Sobue K, Tanida M, Kasahara R, Naruse K, et al. Brain insulin resistance accelerates Abeta fibrillogenesis by inducing GM1 ganglioside clustering in the presynaptic membranes. J Neurochem. 2012;121:619–628. doi: 10.1111/j.1471-4159.2012.07668.x. [DOI] [PubMed] [Google Scholar]
- Haj-ali V, Mohaddes G, Babri SH. Intracerebroventricular insulin improves spatial learning and memory in male Wistar rats. Behavioral neuroscience. 2009;123:1309–1314. doi: 10.1037/a0017722. [DOI] [PubMed] [Google Scholar]
- Shingo AS, Kanabayashi T, Kito S, Murase T. Intracerebroventricular administration of an insulin analogue recovers STZ-induced cognitive decline in rats. Behav Brain Res. 2013;241:105–111. doi: 10.1016/j.bbr.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Yang Y, Ma D, Wang Y, Jiang T, Hu S, Zhang M, et al. Intranasal insulin ameliorates tau hyperphosphorylation in a rat model of type 2 diabetes. J Alzheimers Dis. 2013;33:329–338. doi: 10.3233/JAD-2012-121294. [DOI] [PubMed] [Google Scholar]
- Kern W, Peters A, Fruehwald-Schultes B, Deininger E, Born J, Fehm HL. Improving influence of insulin on cognitive functions in humans. Neuroendocrinology. 2001;74:270–280. doi: 10.1159/000054694. [DOI] [PubMed] [Google Scholar]
- MacLeod KM, Hepburn DA, Frier BM. Frequency and morbidity of severe hypoglycaemia in insulin-treated diabetic patients. Diabet Med. 1993;10:238–245. doi: 10.1111/j.1464-5491.1993.tb00051.x. [DOI] [PubMed] [Google Scholar]
- Benedict C, Hallschmid M, Schmitz K, Schultes B, Ratter F, Fehm HL, et al. Intranasal insulin improves memory in humans: superiority of insulin aspart. Neuropsychopharmacology. 2007;32:239–243. doi: 10.1038/sj.npp.1301193. [DOI] [PubMed] [Google Scholar]
- Reger MA, Watson GS, Frey WH, 2nd, Baker LD, Cholerton B, Keeling ML, et al. Effects of intranasal insulin on cognition in memory-impaired older adults: modulation by APOE genotype. Neurobiol Aging. 2006;27:451–458. doi: 10.1016/j.neurobiolaging.2005.03.016. [DOI] [PubMed] [Google Scholar]
- Reger MA, Watson GS, Green PS, Wilkinson CW, Baker LD, Cholerton B, et al. Intranasal insulin improves cognition and modulates beta-amyloid in early AD. Neurology. 2008;70:440–448. doi: 10.1212/01.WNL.0000265401.62434.36. [DOI] [PubMed] [Google Scholar]
- Craft S, Baker LD, Montine TJ, Minoshima S, Watson GS, Claxton A, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: a pilot clinical trial. Arch Neurol. 2012;69:29–38. doi: 10.1001/archneurol.2011.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger MA, Watson GS, Green PS, Baker LD, Cholerton B, Fishel MA, et al. Intranasal insulin administration dose-dependently modulates verbal memory and plasma amyloid-beta in memory-impaired older adults. J Alzheimers Dis. 2008;13:323–331. doi: 10.3233/jad-2008-13309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verges B. Clinical interest of PPARs ligands. Diabetes Metab. 2004;30:7–12. doi: 10.1016/s1262-3636(07)70083-6. [DOI] [PubMed] [Google Scholar]
- de la Monte SM, Tong M, Lester-Coll N, Plater M, Jr, Wands JR. Therapeutic rescue of neurodegeneration in experimental type 3 diabetes: relevance to Alzheimer's disease. J Alzheimers Dis. 2006;10:89–109. doi: 10.3233/jad-2006-10113. [DOI] [PubMed] [Google Scholar]
- Pedersen WA, McMillan PJ, Kulstad JJ, Leverenz JB, Craft S, Haynatzki GR. Rosiglitazone attenuates learning and memory deficits in Tg2576 Alzheimer mice. Exp Neurol. 2006;199:265–273. doi: 10.1016/j.expneurol.2006.01.018. [DOI] [PubMed] [Google Scholar]
- Yu Y, Li X, Blanchard J, Li Y, Iqbal K, Liu F, et al. Insulin sensitizers improve learning and attenuate tau hyperphosphorylation and neuroinflammation in 3xTg-AD mice J Neural Transm(e-pub ahead of print 13 August 2014). [DOI] [PubMed]
- Escribano L, Simon AM, Gimeno E, Cuadrado-Tejedor M, Lopez de Maturana R, Garcia-Osta A, et al. Rosiglitazone rescues memory impairment in Alzheimer's transgenic mice: mechanisms involving a reduced amyloid and tau pathology. Neuropsychopharmacology. 2010;35:1593–1604. doi: 10.1038/npp.2010.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masciopinto F, Di Pietro N, Corona C, Bomba M, Pipino C, Curcio M, et al. Effects of long-term treatment with pioglitazone on cognition and glucose metabolism of PS1-KI, 3xTg-AD, and wild-type mice. Cell death & disease. 2012;3:e448. doi: 10.1038/cddis.2012.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulos P, Rosa-Neto P, Rochford J, Hamel E. Pioglitazone improves reversal learning and exerts mixed cerebrovascular effects in a mouse model of Alzheimer's disease with combined amyloid-beta and cerebrovascular pathology. PLoS ONE. 2013;8:e68612. doi: 10.1371/journal.pone.0068612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson GS, Cholerton BA, Reger MA, Baker LD, Plymate SR, Asthana S, et al. Preserved cognition in patients with early Alzheimer disease and amnestic mild cognitive impairment during treatment with rosiglitazone: a preliminary study. Am J Geriatr Psychiatry. 2005;13:950–958. doi: 10.1176/appi.ajgp.13.11.950. [DOI] [PubMed] [Google Scholar]
- Abbatecola AM, Lattanzio F, Molinari AM, Cioffi M, Mansi L, Rambaldi P, et al. Rosiglitazone and cognitive stability in older individuals with type 2 diabetes and mild cognitive impairment. Diabetes Care. 2010;33:1706–1711. doi: 10.2337/dc09-2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risner ME, Saunders AM, Altman JF, Ormandy GC, Craft S, Foley IM, et al. Efficacy of rosiglitazone in a genetically defined population with mild-to-moderate Alzheimer's disease. The pharmacogenomics journal. 2006;6:246–254. doi: 10.1038/sj.tpj.6500369. [DOI] [PubMed] [Google Scholar]
- Tzimopoulou S, Cunningham VJ, Nichols TE, Searle G, Bird NP, Mistry P, et al. A multi-center randomized proof-of-concept clinical trial applying [(1)(8)F]FDG-PET for evaluation of metabolic therapy with rosiglitazone XR in mild to moderate Alzheimer's disease. J Alzheimers Dis. 2010;22:1241–1256. doi: 10.3233/JAD-2010-100939. [DOI] [PubMed] [Google Scholar]
- Gold M, Alderton C, Zvartau-Hind M, Egginton S, Saunders AM, Irizarry M, et al. Rosiglitazone monotherapy in mild-to-moderate Alzheimer's disease: results from a randomized, double-blind, placebo-controlled phase III study. Dement Geriatr Cogn Disord. 2010;30:131–146. doi: 10.1159/000318845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C, Sawchak S, Chiang C, Davies J, Donovan C, Saunders AM, et al. Rosiglitazone does not improve cognition or global function when used as adjunctive therapy to AChE inhibitors in mild-to-moderate Alzheimer's disease: two phase 3 studies. Curr Alzheimer Res. 2011;8:592–606. doi: 10.2174/156720511796391935. [DOI] [PubMed] [Google Scholar]
- Hanyu H, Sato T, Kiuchi A, Sakurai H, Iwamoto T. Pioglitazone improved cognition in a pilot study on patients with Alzheimer's disease and mild cognitive impairment with diabetes mellitus. J Am Geriatr Soc. 2009;57:177–179. doi: 10.1111/j.1532-5415.2009.02067.x. [DOI] [PubMed] [Google Scholar]
- Sato T, Hanyu H, Hirao K, Kanetaka H, Sakurai H, Iwamoto T. Efficacy of PPAR-gamma agonist pioglitazone in mild Alzheimer disease. Neurobiol Aging. 2011;32:1626–1633. doi: 10.1016/j.neurobiolaging.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Geldmacher DS, Fritsch T, McClendon MJ, Landreth G. A randomized pilot clinical trial of the safety of pioglitazone in treatment of patients with Alzheimer disease. Arch Neurol. 2011;68:45–50. doi: 10.1001/archneurol.2010.229. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Powell AM, Kaidanovich-Beilin O, Soczynska JK, Alsuwaidan M, Woldeyohannes HO, et al. The neuroprotective effects of GLP-1: possible treatments for cognitive deficits in individuals with mood disorders. Behav Brain Res. 2013;237:164–171. doi: 10.1016/j.bbr.2012.09.021. [DOI] [PubMed] [Google Scholar]
- Goke R, Larsen PJ, Mikkelsen JD, Sheikh SP. Distribution of GLP-1 binding sites in the rat brain: evidence that exendin-4 is a ligand of brain GLP-1 binding sites. Eur J Neurosci. 1995;7:2294–2300. doi: 10.1111/j.1460-9568.1995.tb00650.x. [DOI] [PubMed] [Google Scholar]
- Drucker DJ. Enhancing incretin action for the treatment of type 2 diabetes. Diabetes Care. 2003;26:2929–2940. doi: 10.2337/diacare.26.10.2929. [DOI] [PubMed] [Google Scholar]
- McClean PL, Gault VA, Harriott P, Holscher C. Glucagon-like peptide-1 analogues enhance synaptic plasticity in the brain: a link between diabetes and Alzheimer's disease. Eur J Pharmacol. 2010;630:158–162. doi: 10.1016/j.ejphar.2009.12.023. [DOI] [PubMed] [Google Scholar]
- Talbot K. Brain insulin resistance in Alzheimer's disease and its potential treatment with GLP-1 analogs. Neurodegener Dis Manag. 2014;4:31–40. doi: 10.2217/nmt.13.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holscher C. Insulin, incretins and other growth factors as potential novel treatments for Alzheimer's and Parkinson's diseases. Biochem Soc Trans. 2014;42:593–599. doi: 10.1042/BST20140016. [DOI] [PubMed] [Google Scholar]
- During MJ, Cao L, Zuzga DS, Francis JS, Fitzsimons HL, Jiao X, et al. Glucagon-like peptide-1 receptor is involved in learning and neuroprotection. Nat Med. 2003;9:1173–1179. doi: 10.1038/nm919. [DOI] [PubMed] [Google Scholar]
- Abbas T, Faivre E, Holscher C. Impairment of synaptic plasticity and memory formation in GLP-1 receptor KO mice: Interaction between type 2 diabetes and Alzheimer's disease. Behav Brain Res. 2009;205:265–271. doi: 10.1016/j.bbr.2009.06.035. [DOI] [PubMed] [Google Scholar]
- Li Y, Duffy KB, Ottinger MA, Ray B, Bailey JA, Holloway HW, et al. GLP-1 receptor stimulation reduces amyloid-beta peptide accumulation and cytotoxicity in cellular and animal models of Alzheimer's disease. J Alzheimers Dis. 2010;19:1205–1219. doi: 10.3233/JAD-2010-1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, An FM, Yin L, Liu AR, Yin DK, Yao WB, et al. Glucagon-like peptide-1 protects hippocampal neurons against advanced glycation end product-induced tau hyperphosphorylation. Neuroscience. 2014;256:137–146. doi: 10.1016/j.neuroscience.2013.10.038. [DOI] [PubMed] [Google Scholar]
- Xiong H, Zheng C, Wang J, Song J, Zhao G, Shen H, et al. The neuroprotection of liraglutide on Alzheimer-like learning and memory impairment by modulating the hyperphosphorylation of tau and neurofilament proteins and insulin signaling pathways in mice. J Alzheimers Dis. 2013;37:623–635. doi: 10.3233/JAD-130584. [DOI] [PubMed] [Google Scholar]
- McClean PL, Holscher C. Liraglutide can reverse memory impairment, synaptic loss and reduce plaque load in aged APP/PS1 mice, a model of Alzheimer's disease. Neuropharmacology. 2014;76:57–67. doi: 10.1016/j.neuropharm.2013.08.005. [DOI] [PubMed] [Google Scholar]
- McClean PL, Parthsarathy V, Faivre E, Holscher C. The diabetes drug liraglutide prevents degenerative processes in a mouse model of Alzheimer's disease. J Neurosci. 2011;31:6587–6594. doi: 10.1523/JNEUROSCI.0529-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Zhang J, Ma D, Zhang M, Hu S, Shao S, et al. Subcutaneous administration of liraglutide ameliorates Alzheimer-associated tau hyperphosphorylation in rats with type 2 diabetes. J Alzheimers Dis. 2013;37:637–648. doi: 10.3233/JAD-130491. [DOI] [PubMed] [Google Scholar]
- Holscher C. The incretin hormones glucagonlike peptide 1 and glucose-dependent insulinotropic polypeptide are neuroprotective in mouse models of Alzheimer's disease. Alzheimer's Dement. 2014;10:S47–S54. doi: 10.1016/j.jalz.2013.12.009. [DOI] [PubMed] [Google Scholar]
- Ma T, Du X, Pick JE, Sui G, Brownlee M, Klann E. Glucagon-like peptide-1 cleavage product GLP-1(9-36) amide rescues synaptic plasticity and memory deficits in Alzheimer's disease model mice. J Neurosci. 2012;32:13701–13708. doi: 10.1523/JNEUROSCI.2107-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwai T, Sawabe T, Tanimitsu K, Suzuki M, Sasaki-Hamada S, Oka J. Glucagon-like peptide-1 protects synaptic and learning functions from neuroinflammation in rodents. J Neurosci Res. 2014;92:446–454. doi: 10.1002/jnr.23335. [DOI] [PubMed] [Google Scholar]
- Egefjord L, Gejl M, Moller A, Braendgaard H, Gottrup H, Antropova O, et al. Effects of liraglutide on neurodegeneration, blood flow and cognition in Alzheimer s disease—protocol for a controlled, randomized double-blinded trial. Danish Med J. 2012;59:A4519. [PubMed] [Google Scholar]
- Aviles-Olmos I, Dickson J, Kefalopoulou Z, Djamshidian A, Ell P, Soderlund T, et al. Exenatide and the treatment of patients with Parkinson's disease. J Clin Invest. 2013;123:2730–2736. doi: 10.1172/JCI68295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson O, Zetterberg H, Buchhave P, Londos E, Blennow K, Minthon L. Association between CSF biomarkers and incipient Alzheimer's disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol. 2006;5:228–234. doi: 10.1016/S1474-4422(06)70355-6. [DOI] [PubMed] [Google Scholar]
- Ewers M, Buerger K, Teipel SJ, Scheltens P, Schroder J, Zinkowski RP, et al. Multicenter assessment of CSF-phosphorylated tau for the prediction of conversion of MCI. Neurology. 2007;69:2205–2212. doi: 10.1212/01.wnl.0000286944.22262.ff. [DOI] [PubMed] [Google Scholar]