Abstract
Rationale: Although the number of intensive care unit (ICU) beds in the United States is increasing, it is unknown whether this trend is consistent across all regions.
Objectives: We sought to better characterize regional variation in ICU bed changes over time and identify regional characteristics associated with these changes.
Methods: We used data from the Centers for Medicare and Medicaid Services and the U.S. Census to summarize the numbers of hospitals, hospital beds, ICU beds, and ICU occupancy at the level of Dartmouth Atlas hospital referral region from 2000 to 2009. We categorized regions into quartiles of bed change over the study interval and examined the relationship between change categories, regional characteristics, and population characteristics over time.
Measurements and Main Results: From 2000 to 2009 the national number of ICU beds increased 15%, from 67,579 to 77,809, mirroring population. However, there was substantial regional variation in absolute changes (median, +16 ICU beds; interquartile range, −3 to +51) and population-adjusted changes (median, +0.9 ICU beds per 100,000; interquartile range, −3.8 to +5.9), with 25.0% of regions accounting for 74.8% of overall growth. At baseline, regions with increasing numbers of ICU beds had larger populations, lower ICU beds per 100,000 capita, higher average ICU occupancy, and greater market competition as measured by the Herfindahl-Hirschman Index (P < 0.001 for all comparisons).
Conclusions: National trends in ICU bed growth are not uniformly reflected at the regional level, with most growth occurring in a small number of highly populated regions.
Keywords: critical care, infrastructure, intensive care unit, bed supply
At a Glance Commentary
Scientific Knowledge on the Subject
Critical care bed supply is increasing over time in the United States. However, little is known about whether this growth is consistent across regions or the regional factors influencing growth.
What This Study Adds to the Field
Critical care bed supply increased substantially from 2000 to 2009, similar to growth in the adult population. However, the changes in critical care bed supply are not uniform at the regional level, with most growth occurring in a small number of regions and many regions decreasing in bed supply. Regions experiencing an increase in critical care beds tended to have large populations, fewer baseline intensive care unit beds per 100,000 capita, higher baseline intensive care unit occupancy, and increased market competition. Future efforts to constrain critical care growth should emphasize reducing population-based use in a small number of growing regions.
The United States spends more on health care as a proportion of its gross domestic product than any other industrialized nation (1). A large proportion of this spending relates to the intensive care unit (ICU), with recent estimates suggesting that critical care expenditures exceed $82 billion annually (2). One important determinant of ICU use and spending may be the availability of ICU beds (3). Epidemiologic evidence suggests that in the presence of available ICU beds physicians tend to admit lower-risk patients to the ICU and use the ICU more for care at the end of life (4–6). These findings suggest that overuse of ICU beds may be mediated, at least in part, by excess supply. Yet the number of ICU beds in the United States continues to increase, from 69,300 in 1985 to 93,955 in 2005 (2, 7).
The rise in total ICU beds in the United States is well documented, but this finding is based on aggregate bed counts at the national level. Such national trends may not accurately describe more granular regional changes (8). Understanding regional differences in ICU bed growth may provide insight into the factors underlying that growth, and may reveal targets for slowing future growth. Additionally, because population demographics are a major determinant of ICU demand (9), it is important to understand to what degree regional changes in ICU bed counts are associated with changing population demographics. To address these knowledge gaps, we sought to characterize regional variation in ICU bed supply changes; describe characteristics of regions with expanding, unchanged, and contracting ICU bed supply; and evaluate to what extent regional changes in ICU bed supply are tracking with changes in the adult population.
Methods
Study Design and Data Sources
We performed a longitudinal study of the U.S. ICU bed supply during the 10-year period between 2000 and 2009. Data on ICU beds were obtained from the Centers for Medicare and Medicaid Services Hospital Cost Report Information System (HCRIS), a publically available hospital-level data file containing structural, organizational, and cost data on all nonfederal U.S. hospitals. We excluded nongeneral acute care hospitals (i.e., skilled nursing facilities and long-term acute care hospitals), hospitals located in the U.S. territories, and hospitals with insufficient reporting in a study year (2, 7). We obtained population data from the U.S. Census (10). Regions were defined using Dartmouth Atlas hospital referral regions (11). We assigned hospitals and populations to hospital referral regions using publically available Dartmouth Atlas crosswalks.
Variables
We obtained counts of hospitals, hospital beds, and ICU beds directly from HCRIS. We defined ICU beds as the sum of HCRIS hospital counts of ICU beds, surgical ICU beds, cardiac ICU beds, and burn ICU beds (2, 7). Using U.S. Census data we examined two population denominators: all adults, defined as persons aged 20 years and older; and elderly adults, defined as adults aged 65 or older. We examined the elderly as a unique category because they are at high risk for critical illness compared with the younger population (12, 13) and therefore drive many projected estimates of future ICU demand (14).
Data Analysis
First, we examined temporal trends in ICU bed supply at the national and regional levels. At the national level, we summarized the annual number of hospitals, hospital beds, ICU beds, adult population, elderly adult population, ICU beds per adult population, and ICU beds per elderly adult population using standard summary statistics. At the regional level, we calculated the number of ICU beds, ICU beds per adult population, ICU beds per elderly adult population, and proportion of ICU beds, and plotted these values over time using violin plots. Violin plots demonstrate both the range of the data and the density at different values. We used the Brown-Forsythe F statistic to compare the magnitude of variation at the beginning and end of the study interval. We performed these analyses to show the extent of regional variation within and between study years, and evaluate whether regional variation in ICU bed supply was changing in magnitude over time.
Second, we determined baseline regional characteristics associated with changes in ICU bed supply. We categorized regions by quartile of ICU bed change between 2000 and 2009, and then combined the middle two quartiles, defining regions as undergoing negative growth (lowest quartile of change in ICU beds), unchanged or moderate growth (middle two quartiles of change in ICU beds), or high growth (highest quartile of change in ICU beds), according to the observed distribution. We then compared regional characteristics at baseline across categories of ICU bed changes using percentages, means and standard deviations, and medians and interquartile ranges as appropriate. Regional characteristics of interest included the number of hospitals, hospital beds, and ICU beds; population counts and population densities; the number of hospitals, hospital beds, and ICU beds per 100,000 capita; and ICU bed occupancy (defined as the number of ICU bed days divided by the number of ICU bed days available, obtained from HCRIS).
To evaluate the association between region level hospital competition and changes in infrastructure, we calculated the Herfindahl-Hirschman Index. This measure is calculated as the summed squares of market proportion (in this case, proportion of ICU beds) within a region. The index ranges from 0 to 10,000, with lower numbers indicating increased competition (beds are more evenly distributed between hospitals within a region) and higher numbers indicating less competition (beds are more centralized within fewer hospitals in a region). We used the Kruskal-Wallis test for statistical comparisons, applying a Bonferroni correction for multiple comparisons.
Third, we determined the relationship between regional ICU bed supply change and population growth. To accomplish this step we created scatterplots of 10-year change in the regional number of ICU beds and 10-year change in the regional population, highlighting regions that increased or decreased the number of ICU beds by more than 100, relative to what would be expected by their change in population. We estimated the relationship between change in ICU beds and change in population using Spearman rank correlation. We extrapolated a reference line showing the predicted number of ICU beds in 2009, conditional on ICU supply per 100,000 capita remaining at year 2000 levels. We compared the slopes of observed and predicted lines using seemingly unrelated regression (15). This technique compares the observed and predicted slopes of ICU bed changes across regions, while accounting for correlation in the model error terms. For example, finding no difference between the slope of the actual regression line and the predicted line would indicate that regional changes in population and ICU beds tracked with the population. We performed these analyses using adult and elderly adult denominators.
All analyses were performed in STATA 12.1 (Stata Corp., College Station, TX). This research involved analyses of publically available data at the hospital and population level, and therefore did not meet the University of Pittsburgh Institutional Review Board definition of human subject research.
Results
Temporal trends in bed supply and populations are shown in Table 1. From 2000 to 2009 the number of acute care hospitals in the United States decreased (from 3,468 to 3,155; −9.0% growth), the number of total hospital beds remained largely constant (from 621,578 to 627,112; 0.8% growth), but the number of ICU beds substantially increased (from 67,579 to 77,809; +15.1%). In 2000, the adult population living within Dartmouth Atlas regions was 200,914,864, resulting in overall 33.6 ICU beds per 100,000 persons. By 2009, the adult population had increased to 224,305,184, which, coupled with changes in ICU bed supply, resulted in a small net increase of 1.1 beds per 100,000 capita, to 34.7 ICU beds per 100,000 adults. In 2000, the elderly adult population was 34,987,216, resulting in overall 193.2 ICU beds per 100,000 elderly persons. In 2009, the elderly adult population increased to 41,080,936, resulting in a small net decrease of 3.8 per 100,000 capita, to 189.4 ICU beds per 100,000 elderly persons. The proportion of beds assigned to the ICU increased progressively over the study interval, from 0.109 in 2000 to 0.124 in 2009.
Table 1.
U.S. Hospitals, Hospital Beds, ICU Beds, and Population between 2000 and 2009
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Hospitals | 3,468 | 3,424 | 3,363 | 3,323 | 3,334 | 3,280 | 3,247 | 3,222 | 3,199 | 3,155 |
| Hospital beds | 621,578 | 616,679 | 616,454 | 615,468 | 619,395 | 618,743 | 619,894 | 623,775 | 627,378 | 627,112 |
| ICU beds | 67,579 | 67,710 | 68,920 | 70,258 | 71,468 | 72,678 | 74,533 | 75,863 | 76,803 | 77,809 |
| ICU bed proportion | 0.109 | 0.110 | 0.112 | 0.114 | 0.115 | 0.117 | 0.120 | 0.122 | 0.122 | 0.124 |
| Population 20+ | 200.9M | 203.8M | 206.9M | 209.5M | 212.2M | 214.9M | 217.6M | 219.9M | 222.3M | 224.3M |
| Population 65+ | 35.0M | 35.3M | 35.9M | 36.4M | 36.9M | 37.5M | 38.3M | 39.1M | 40.2M | 41.1M |
| Hospital beds per 100K | ||||||||||
| Population 20+ | 309.4 | 302.6 | 298.0 | 293.8 | 291.9 | 287.9 | 284.9 | 283.7 | 282.2 | 279.6 |
| Population 65+ | 1,776.6 | 1,745.9 | 1,718.0 | 1,692.7 | 1,678.4 | 1,649.9 | 1,620.3 | 1,594.1 | 1,561.8 | 1,526.5 |
| ICU beds per 100K | ||||||||||
| Population 20+ | 33.6 | 33.2 | 33.3 | 33.5 | 33.7 | 33.8 | 34.3 | 34.5 | 34.5 | 34.7 |
| Population 65+ | 193.2 | 191.7 | 192.1 | 193.2 | 193.7 | 193.8 | 194.8 | 193.9 | 191.2 | 189.4 |
Definition of abbreviations: ICU = intensive care unit; K = thousand; M = million.
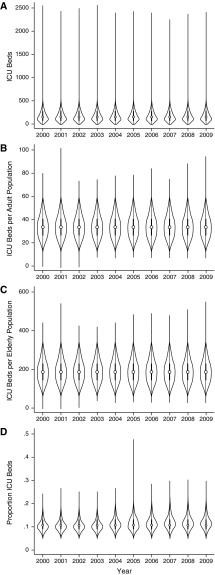
Region level ICU beds and ICU beds per 100,000 capita varied widely in all study years (157.5- to 419.7-fold for ICU beds; 6.6- to 32.0-fold range for ICU beds per 100,000 adults; and 6.5- to 18.4-fold range for ICU beds per 100,000 elderly adults) (Figures 1A–1C). The Brown-Forsythe F statistic for equivalence of variances between study years was 1.63 (P = 0.20) for regional number of ICU beds, 1.20 (P = 0.27) for ICU beds per adult capita, and 0.45 (P = 0.50) for ICU beds per elderly capita, all indicating similar regional variation in 2000 and 2009.
Figure 1.
Violin plots of ICU beds (A), ICU beds per 100,000 persons aged 20 years and older (B), ICU beds per 100,000 persons aged 65 and older (C), and ICU beds as a proportion of regional hospital beds (D) in 306 Dartmouth Atlas hospital referral regions over the years 2000–2009. Violin plots are similar to boxplots but also show the cohort’s distribution density. Wider areas in the violin plot correspond to increased observation frequency at that y-value. The open circle indicates the median and the thick vertical line indicates the first and third interquartile range. ICU = intensive care unit.
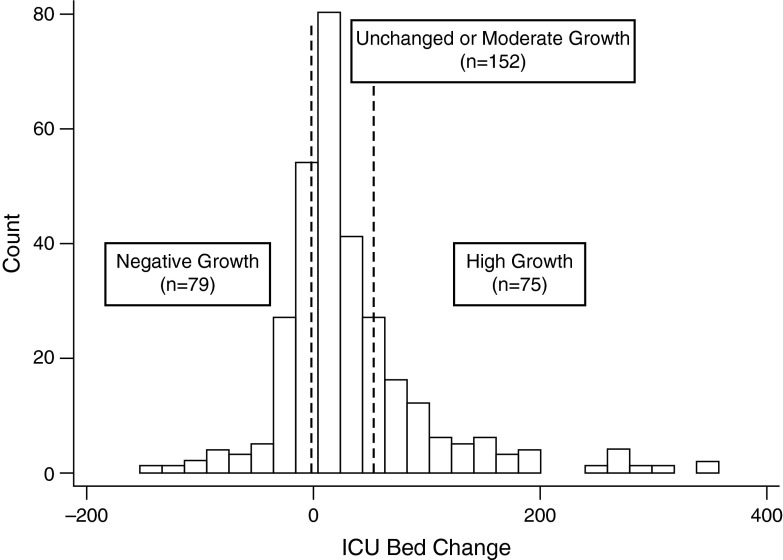
Overall, the unadjusted median regional change was +16 beds, with an interquartile range of −3 ICU beds to +51 ICU beds and a total range from −152 to +358. The median relative regional change was +12%, with an interquartile range of −4 to +31% and a total range of −64 to +354%. On a per 100,000 capita basis, the median regional change was +0.9 beds per 100,000, with an interquartile range of −3.8 to +5.9 beds per 100,000 and a total range of −44.9 to +33.6 beds per 100,000. We classified 26% of regions (n = 79) as having negative growth, 50% of regions (n = 152) as having no or moderate growth, and 25% of regions (n = 75) as having high growth during the study period (Figure 2). Despite making up only one-quarter of regions, high-growth regions accounted for 74.8% of all added ICU beds. At baseline, regions with high ICU bed growth tended to have more hospitals, hospital beds, and ICU beds (P < 0.001 for all comparisons). High-growth regions had the largest adult and elderly populations (P < 0.001 for both comparisons) and highest average ICU occupancy (P < 0.001). Compared with negative-growth regions, regions with high growth had fewer ICU beds per 100,000 capita at baseline for both adult and elderly adult populations (32.0 compared with 39.2 per 100,000 for adults, and 200.4 compared with 209.8 for elderly adults) (Table 2). High-growth regions had the greatest market competition for ICU beds, as measured by the Herfindahl-Hirschman Index (1,563 for high-growth, 2,451 for unchanged or moderate-growth, and 2,850 for negative-growth regions; P < 0.001) (Table 2).
Figure 2.
Histogram of change in number of intensive care unit beds in 306 Dartmouth Atlas hospital referral regions between the years 2000 and 2009. ICU = intensive care unit.
Table 2.
Baseline Regional Characteristics by Quartile of ICU Bed Growth between 2000 and 2009
| Negative Growth (n = 79) | Unchanged or Moderate Growth (n = 152) | High Growth (n = 75) | P Value | |
|---|---|---|---|---|
| Population (thousands) | ||||
| 20 yr+ | 279 (184–535) | 360 (201–550) | 802 (507–1,690) | <0.001 |
| 65 yr+ | 53 (36–112) | 65 (37–102) | 152 (87–264) | <0.001 |
| Population density (persons per square mile) | ||||
| 20 yr+ | 66 (31–192) | 77 (40–218) | 106 (51–246) | 0.18 |
| 65 yr+ | 13 (6–40) | 15 (8–36) | 18 (9–44) | 0.37 |
| Hospitals and beds, n | ||||
| Hospitals | 7 (4–11) | 7 (4–12) | 13 (9–22) | <0.001 |
| Hospital beds | 934 (578–2,118) | 1,024 (640–1,710) | 2,450 (1,460–4,677) | <0.001 |
| ICU beds | 114 (71–228) | 111 (60–189) | 257 (146–525) | <0.001 |
| Hospitals and beds per capita, n* | ||||
| 20 yr+ | ||||
| Hospitals per capita | 2.2 (1.6–2.9) | 2.0 (1.5–2.5) | 1.5 (1.2–2.0) | <0.001 |
| Hospital beds per capita | 340.1 (273.6–405.1) | 301.3 (243.7–362.1) | 301.4 (242.5–351.3) | 0.004 |
| ICU beds per capita | 39.2 (29.8–46.3) | 32.1 (25.0–37.6) | 32.0 (25.5–39.1) | <0.001 |
| 65 yr+ | ||||
| Hospitals per capita | 11.7 (8.8–14.9) | 10.9 (8.2–13.5) | 9.5 (7.3–12.1) | 0.002 |
| Hospital beds per capita | 1,730.1 (1,444.5–2194.6) | 1,622.6 (1,374.6–1,940.0) | 1,714.8 (1,382.4–2,033.5) | 0.30 |
| ICU beds per capita | 209.8 (158.5–255.3) | 170.6 (138.6–205.6) | 200.4 (141.1–226.5) | <0.001 |
| Average ICU occupancy | 59% (52–66) | 62% (57–69) | 65% (61–72) | 0.004 |
| Herfindahl-Hirschman Index† | 2,850 (1,735–3,923) | 2,451 (1,627–3,645) | 1,563 (827–2,599) | <0.001 |
Definition of abbreviation: ICU = intensive care unit.
Values are median (interquartile range).
Per 100,000 population.
Measure of market competition ranging from 0 to 10,000, where lower numbers indicate more competition between hospitals within regions and higher numbers indicate less competition.
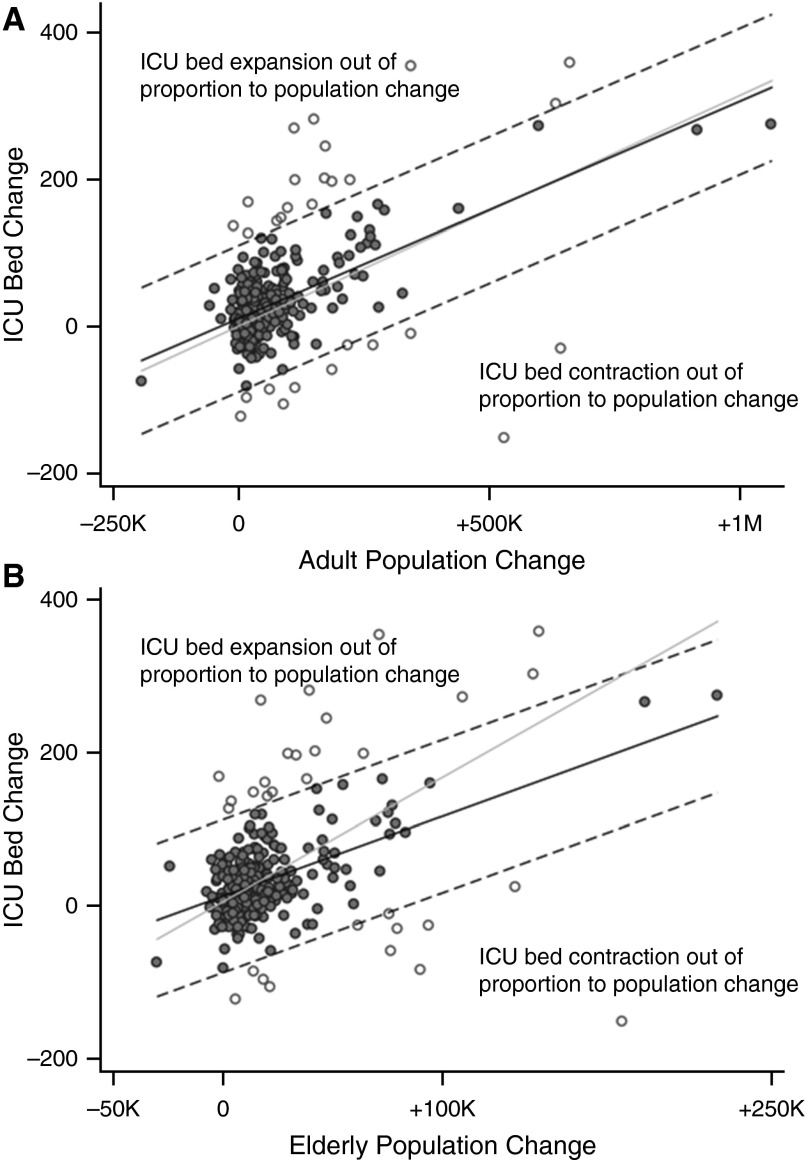
The regional change in the number of ICU beds was moderately positively correlated with population change, both for adult (r = 0.55; P < 0.001) and elderly (r = 0.46; P < 0.001) populations (Figures 3A and 3B). There was also substantial variation, with many regions increasing in bed number out of proportion to population change, and others decreasing in bed number out of proportion to population change.
Figure 3.
Comparison of regional change in the number of ICU beds and population change among adults aged 20 and older (A) and 65 and older (B). For both plots, the dark solid line represents the linear regression line and each dark circle represents a Dartmouth Atlas hospital referral region. The open circles outside the dashed lines represent outlier regions that increased or decreased the number of ICU beds by more than 100 beds, relative to the predicted change. The light solid line represents the predicted change in ICU beds for change in population, based on year 2000 ICU beds per 100,000 capita. ICU = intensive care unit; K = thousand; M = million.
Seventeen regions (5.6%) increased the number of ICU beds by more than 100 relative to the change predicted by the adult population. These high relative growth regions had a median 34.0 ICU beds per 100,000 capita and an interquartile range of 30.6 to 38.7 ICU beds per 100,000 capita at baseline. Eleven regions (3.6%) decreased the number of ICU beds by more than 100 relative to the change predicted by the adult population. These regions had a median 30.4 ICU beds per 100,000 capita and an interquartile range 28.9–38.8 ICU beds per 100,000 capita at baseline.
For the elderly adult population, 19 regions (6.2%) increased the number of ICU beds by more than 100, relative to the predicted change. These high relative growth regions had a median 200.7 ICU beds per elderly capita and an interquartile range of 141.1–219.4 ICU beds per 100,000 capita at baseline. Twelve regions (3.9%) decreased the number of ICU beds by more than 100, relative to the predicted change. These regions had a median 212.8 ICU beds per 100,000 capita and an interquartile range of 190.6–257.5 ICU beds per 100,000 capita at baseline.
The increase in the number of ICU beds over the 10 years tracked closely with regional changes in the adult population (χ2 = 0.85; P = 0.36), but was outstripped by growth of the elderly adult population (χ2 = 87.7; P < 0.0001).
Discussion
Overall, the decade from 2000 to 2009 saw little change in U.S. acute care hospital beds and a large increase in ICU beds. These trends were not consistent across regions, with most of the increase driven by a minority of regions and many regions decreasing in supply. National population-adjusted ICU bed supply remained relatively constant, although some regions increased in bed supply out of proportion with population growth, and other regions decreased in bed supply relative to population trends.
At the national level, our results confirm previous work demonstrating that an increasing proportion of hospital care is devoted to critical care (2). The causes of this trend are likely multifactorial. Advances in outpatient surgery (17) and efforts to keep patients with chronic disease out of the hospital (18, 19) seem to be decreasing demand for acute hospital care (20). Yet at the same time there has been little success in reducing demand for intensive care (21) or to shift the site of intensive care to other settings (22). Indeed, although long-term acute care hospitals are in part designed to reduce the need for ICU beds for patients with chronic critical illness, the rise in long-term acute care hospitals seems not to have impacted the national ICU bed supply (23).
At the regional level, our work shows that examination of national trends fails to reveal more nuanced regional changes. Despite overall bed growth, many regions actually decreased in supply over the study period. Although national bed supply tracked closely with population, many regional ICU bed changes occurred out of proportion to population changes, with both large per capita increases and decreases in ICU bed supply. This finding underscores the inherent complexity of the ICU supply in the United States. Indeed, little is known about the factors driving the ICU bed supply, either at the hospital or regional level (24). We found that regions increasing in supply had relatively low ICU bed supply and high ICU occupancy at baseline, suggesting that ICU bed supply is at least in part responsive to population demand. However, we also found that the overall level of variation persisted from year to year, indicating that U.S. regions are not triangulating an “ideal mean” based on population demand.
Furthermore, regions with the largest population-adjusted changes did not neatly align with baseline levels of ICU bed supply. For example, regions with disproportionate growth relative to population change did not have fewer ICU beds per 100,000 capita at baseline. These observations suggest that regions are instead increasing and decreasing in supply in response to other factors, such as financial and competitive pressures (25). Finally, at the hospital level, ICU bed growth may be a response to progressively heightened risk avoidance or lowering tolerance for managing sick patients on the floor.
Using an econometric measure of market competition, we observed the most critical care bed growth in regions with high competition, and bed contraction in regions with low competition. One interpretation of this finding is that regions with less competition (where most of the beds are centralized in few hospitals) tend to downsize critical care capacity at noncentral hospitals. Hospital specialization coupled to active triage and transport of critically ill patients, components of explicitly regionalized care, may allow these regions to function with fewer overall ICU beds. Another explanation is that in regions with high competition ICU beds are used to support services for which hospitals intensely compete, such as cardiac surgery or cancer care. In this way, competition may introduce inefficiencies through duplication of ICU services. Future work should examine the implications of competition and how competition impacts patient outcomes and total costs.
Our results have important policy implications for U.S. health care delivery. Given wide differences in ICU use across hospitals (26, 27) and the apparent influence of bed supply on use (5), some analysts have recommended constraining the number of ICU beds through certificate of need laws (3). Certificate of needs laws seem effective at reducing unnecessary bed proliferation in the neonatal ICU (28), and could be useful in adult ICUs. Our analysis shows that these efforts need not be national in scope, but could be directed to a small number of quickly growing regions. Our analysis also provides data on the range of ICU beds per 100,000 capita that could be used to develop population-based targets, perhaps allowing for reductions in the ICU bed supply in some areas. Most prior work in this area focused on planning at the hospital level (29, 30). However, given the increasing role that interhospital transfers play in critical care (31), more efficient use of ICU beds may be obtainable through regional planning, building off our regional estimates (32).
As part of this planning it is important to first better characterize the impact of regional variation in ICU bed supply on ICU use and outcomes. To the degree that ICU beds create their own demand, ICU bed reductions may be a safe and effective way to reduce ICU-related spending in the United States. However, to the degree that ICU bed increases are in response to increasing demand, ICU bed reductions may create admission delays leading to poor clinical outcomes (33). Future studies should more closely examine this issue at the population level to determine where and when constraining ICU resources may be safe.
Our study has several limitations. We obtained ICU bed data from HCRIS, which relies on self-reporting and therefore may be inaccurate in some circumstances. Additionally, HCRIS ICU bed counts do not reliably distinguish between adult and pediatric assignment. Therefore, although we excluded standalone pediatric hospitals, we expect some pediatric ICU beds were included in the numerator counts. Consequently, our estimates may be higher than estimates derived from other sources. However, HCRIS are validated by audit and are considered a reliable source of bed-count data in the United States (34). We defined our regions using the Dartmouth Atlas, which was not developed with critical illness in mind and does not necessarily respect political and legislative geographic boundaries (35). Nonetheless, the Dartmouth Atlas is the most widely used schema for examining regional variation in health care use and has extensive face validity (11).
Additionally, we were only able to examine a subset of potential factors potentially related to regional ICU bed growth. Direct hospital competition, health system integration, regional care coordination, and the use of ICU telemedicine all may affect the ICU bed supply but could not be measured in our data. Finally, it is possible that the duration of observation was not long enough to identify changes in intensive care infrastructure occurring in response to more protracted population trends.
Despite these limitations, our results provide new insights into the regional determinants of ICU infrastructure expansion in the United States and challenge national bed analyses as a method of understanding supply and use patterns. A further understanding of how regional supply impacts patient-level use and outcomes is an important next step. In the meantime, our results help inform and focus efforts to slow the growth of critical care spending by targeting the apparent oversupply of ICU beds in the United States.
Footnotes
Supported by National Institutes of Health grants T32 HL07820, K12 HL109068, and K23 GM104022.
Author Contributions: All authors provided substantial contributions to the conception and design, acquisition of data, and analysis and interpretation of findings. D.J.W. drafted the manuscript and all authors contributed substantially to revisions. All authors give approval for the final version submitted for publication.
Originally Published in Press as DOI: 10.1164/rccm.201409-1746OC on December 18, 2014
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.The World Bank. Data [accessed 2014 Sept 1]. Available fromhttp://data.worldbank.org
- 2.Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38:65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 3.Gooch RA, Kahn JM. ICU bed supply, utilization, and health care spending: an example of demand elasticity. JAMA. 2014;311:567–568. doi: 10.1001/jama.2013.283800. [DOI] [PubMed] [Google Scholar]
- 4.Singer DE, Carr PL, Mulley AG, Thibault GE. Rationing intensive care—physician responses to a resource shortage. N Engl J Med. 1983;309:1155–1160. doi: 10.1056/NEJM198311103091905. [DOI] [PubMed] [Google Scholar]
- 5.Stelfox HT, Hemmelgarn BR, Bagshaw SM, Gao S, Doig CJ, Nijssen-Jordan C, Manns B. Intensive care unit bed availability and outcomes for hospitalized patients with sudden clinical deterioration. Arch Intern Med. 2012;172:467–474. doi: 10.1001/archinternmed.2011.2315. [DOI] [PubMed] [Google Scholar]
- 6.Strauss MJ, LoGerfo JP, Yeltatzie JA, Temkin N, Hudson LD. Rationing of intensive care unit services. An everyday occurrence. JAMA. 1986;255:1143–1146. [PubMed] [Google Scholar]
- 7.Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985-2000: an analysis of bed numbers, use, and costs. Crit Care Med. 2004;32:1254–1259. doi: 10.1097/01.ccm.0000128577.31689.4c. [DOI] [PubMed] [Google Scholar]
- 8.Carr BG, Addyson DK, Kahn JM. Variation in critical care beds per capita in the United States: implications for pandemic and disaster planning. JAMA. 2010;303:1371–1372. doi: 10.1001/jama.2010.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seferian EG, Afessa B. Demographic and clinical variation of adult intensive care unit utilization from a geographically defined population. Crit Care Med. 2006;34:2113–2119. doi: 10.1097/01.CCM.0000227652.08185.A4. [DOI] [PubMed] [Google Scholar]
- 10.GeoLytics Inc. CensusCD 2000–2009. Somerville, NJ; GeoLytics Inc.
- 11.The Center for the Evaluative Clinical Sciences. Chicago: American Hospital Publishing; 1998. The Dartmouth atlas of health care. [PubMed] [Google Scholar]
- 12.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- 14.Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J, Jr Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS) Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284:2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 15.Zellner A. An efficient method of estimating seemingly unrelated regressions and tests for aggregation bias. J Am Stat Assoc. 1962;57:348–368. [Google Scholar]
- 16.Halpern NA, Pastores SM, Thaler HT, Greenstein RJ. Changes in critical care beds and occupancy in the United States 1985-2000: differences attributable to hospital size. Crit Care Med. 2006;34:2105–2112. doi: 10.1097/01.CCM.0000227174.30337.3E. [DOI] [PubMed] [Google Scholar]
- 17.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009;11:1–25. [PubMed] [Google Scholar]
- 18.Casas A, Troosters T, Garcia-Aymerich J, Roca J, Hernández C, Alonso A, del Pozo F, de Toledo P, Antó JM, Rodríguez-Roisín R, et al. members of the CHRONIC Project. Integrated care prevents hospitalisations for exacerbations in COPD patients. Eur Respir J. 2006;28:123–130. doi: 10.1183/09031936.06.00063205. [DOI] [PubMed] [Google Scholar]
- 19.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 20.MPA Commission. Washington, DC: MedPAC; 2013. A data book: health care spending and the Medicare program. [Google Scholar]
- 21.Luce JM, Rubenfeld GD. Can health care costs be reduced by limiting intensive care at the end of life? Am J Respir Crit Care Med. 2002;165:750–754. doi: 10.1164/ajrccm.165.6.2109045. [DOI] [PubMed] [Google Scholar]
- 22.Prin M, Wunsch H. The role of stepdown beds in hospital care. Am J Respir Crit Care Med. 2014;190:1210–1216. doi: 10.1164/rccm.201406-1117PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kahn JM, Benson NM, Appleby D, Carson SS, Iwashyna TJ. Long-term acute care hospital utilization after critical illness. JAMA. 2010;303:2253–2259. doi: 10.1001/jama.2010.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kahn JM. Matching supply and demand in critical care. Curr Opin Crit Care. 2011;17:618–619. doi: 10.1097/MCC.0b013e32834cdcf5. [DOI] [PubMed] [Google Scholar]
- 25.Cutler DM, Scott Morton F. Hospitals, market share, and consolidation. JAMA. 2013;310:1964–1970. doi: 10.1001/jama.2013.281675. [DOI] [PubMed] [Google Scholar]
- 26.Seymour CW, Iwashyna TJ, Ehlenbach WJ, Wunsch H, Cooke CR. Hospital-level variation in the use of intensive care. Health Serv Res. 2012;47:2060–2080. doi: 10.1111/j.1475-6773.2012.01402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen LM, Render M, Sales A, Kennedy EH, Wiitala W, Hofer TP. Intensive care unit admitting patterns in the Veterans Affairs health care system. Arch Intern Med. 2012;172:1220–1226. doi: 10.1001/archinternmed.2012.2606. [DOI] [PubMed] [Google Scholar]
- 28.Lorch SA, Maheshwari P, Even-Shoshan O. The impact of certificate of need programs on neonatal intensive care units. J Perinatol. 2012;32:39–44. doi: 10.1038/jp.2011.47. [DOI] [PubMed] [Google Scholar]
- 29.Green LV. How many hospital beds? Inquiry. 2002-2003;39:400–412. doi: 10.5034/inquiryjrnl_39.4.400. [DOI] [PubMed] [Google Scholar]
- 30.Williams SV. How many intensive care beds are enough? Crit Care Med. 1983;11:412–416. doi: 10.1097/00003246-198306000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Iwashyna TJT, Christie JDJ, Moody J, Kahn JMJ, Asch DAD. The structure of critical care transfer networks. Med Care. 2009;47:787–793. doi: 10.1097/MLR.0b013e318197b1f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olafson K, Ramsey C, Yogendran M, Fransoo R, Chrusch C, Forget E, Garland A. Surge capacity: analysis of census fluctuations to estimate the number of intensive care unit beds needed. Health Serv Res. [online ahead of print] Jul 15 2014; DOI: 10.1111/1475-6773.12209. [DOI] [PMC free article] [PubMed]
- 33.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP DELAY-ED study group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 34.Halpern NA, Pastores SM, Thaler HT, Greenstein RJ. Critical care medicine use and cost among Medicare beneficiaries 1995-2000: major discrepancies between two United States federal Medicare databases. Crit Care Med. 2007;35:692–699. doi: 10.1097/01.CCM.0000257255.57899.5D. [DOI] [PubMed] [Google Scholar]
- 35.National Quality Forum Regionalized emergency medical care services: emergency department crowding and boarding, healthcare system preparedness and surge capacity - performance measurement gap analysis and topic prioritization Washington, DC: National Quality Forum; 2013. [Google Scholar]