Abstract
BACKGROUND:
Acupuncture stimulates points on the body, influencing the perception of myofascial pain or altering physiologic functions.
OBJECTIVE:
The aim was to evaluate the effect of electroacupuncture (EAC) and acupuncture (AC) for myofascial pain of the upper trapezius and cervical range of motion, using SHAM acupuncture as control.
METHOD:
Sixty women presenting at least one trigger point at the upper trapezius and local or referred pain for more than six months were randomized into EAC, AC, and SHAM groups. Eight sessions were scheduled and a follow-up was conducted after 28 days. The Visual Analog Scale assessed the intensity of local and general pain. A fleximeter assessed cervical movements. Data were analyzed using paired t or Wilcoxon's tests, ANOVA or Friedman or Kruskal-Wallis tests and Pearson's correlation (α=0.05).
RESULTS:
There was reduction in general pain in the EAC and AC groups after eight sessions (P<0.001). A significant decrease in pain intensity occurred for the right trapezius in all groups and for the left trapezius in the EAC and AC groups. Intergroup comparisons showed improvement in general pain in the EAC and AC groups and in local pain intensity in the EAC group (P<0.05), which showed an increase in left rotation (P=0.049). The AC group showed increases in inclination (P=0.005) sustained until follow-up and rotation to the right (P=0.032).
CONCLUSION
: EAC and AC were effective in reducing the pain intensity compared with SHAM. EAC was better than AC for local pain relief. These treatments can assist in increasing cervical range of motion, albeit subtly.
Keywords: myofascial pain syndromes, acupuncture therapy, trapezius muscle, physical therapy
Introduction
Myofascial pain is characterized by the presence of tender, firm nodules called trigger points (MTrP). Within each trigger point is a hyperirritable spot, the "taut-band", which is composed of hyper-contracted muscle fibers1. Clinically, the muscle with MTrP presents with stiffness and is associated with diminished strength and restricted range of motion1 , 2. If latent, palpation of this spot within the trigger point provokes radiating, aching-type pain into localized referred zones consisting in an important musculoskeletal dysfunction3 and one of main causes of headache and neck pain4. If active, MTrP promotes spontaneous pain.
Myofascial pain affects up to 85% of the general population1. Fleckenstein et al.5 reported that physicians did not observe difference between genders. Nevertheless, women were more likely than men to develop neck pain and less likely to recover from such pain6. Moreover, women have a greater frequency of musculoskeletal pain than men7.
The treatment of myofascial pain requires that MTrP and muscles be identified as primary or ancillary pain generators3. Acupuncture (AC) has been used as an alternative to more traditional treatments for musculoskeletal pain, because it inactivates the neural loop of the trigger point (pain-contraction-pain), reducing pain, and reduces muscular over-contraction. Acupuncture stimulates points on the body via the insertion of needles to prevent or modify the perception of pain or to alter physiologic functions8. Electroacupuncture (EAC) includes the passage of an electrical current through the needle9.
AC8 , 10 and EAC9 , 11 , 12 have been shown to effectively decrease the intensity of chronic pain. Nevertheless, it is still unknown whether one of these treatments is more effective than the other for treating myofascial pain. Since EAC presents the electrical stimulation added to AC, better results are expected.
Myofascial pain treatment should increase muscle function2, promoting pain decrease and the unstringing of the contracted fibers. Consequently, a reduction in muscle stiffness and an increased range of motion would be expected.
Fiber contraction in the upper trapezius muscle, which presents a high prevalence of MTrP13 - 15, promotes the extension and inclination of the head to the same side and rotation to the opposite side16. Therefore, to evaluate muscle function, cervical range of motion is indicated. To achieve that, non-invasive methods are available such as the Cervical Range of Motion device (Roseville, MN, USA)17 and the fleximeter (Code Research Institute, Brazil)18, which have presented moderate to excellent reliability for both intra- and inter-examiner measurements. Although both methods are effective, the fleximeter offers lower costs and easier handling, and it can evaluate other body segments.
The aim of this study was to evaluate the effectiveness of EAC and AC on pain intensity and cervical range of motion in women with myofascial pain in the upper trapezius, using SHAM acupuncture as a control. The hypothesis was that EAC could determine better effectiveness than AC in pain relief and increase the cervical range of motion.
Method
This research was conducted at the Clinical Research Laboratory, Departamento de Odontologia Infantil, Faculdade de Odontologia de Piracicaba, Universidade Estadual de Campinas (FOP-UNICAMP), Piracicaba, SP, Brazil, from June 2012 to August 2013. The sample size was calculated considering previous data for pain intensity12. A two-sided test with α=0.05, null mean=0.5, alternate mean=0, standard deviation=2.5, and statistical power=0.80, determined a sample size of 24 subjects for each group. The project was approved by the Research Ethics Committee of FOP-UNICAMP (protocol 003/2011). The volunteers read and signed the consent form and were informed about the procedures, discomfort or risks, the benefits of the research, and the need to attend all sessions. They were blinded to group allocation, as was the examiner who did the assessments (C.E.E.M.). The Brazilian Clinical Trials Registry number is RBR-42kz9z (available at: http://www.ensaiosclinicos.gov.br/rg/RBR-42kz9z/).
Women suffering from head and neck pain were included in the study. The participants were interviewed to obtain information about general health pertaining to the inclusion and exclusion criteria, as follows: (1) Inclusion criteria: age range from 18 to 40 years; body mass index (BMI) ranging from 18 to 30 Kg/m2; regular menstrual cycle (regardless of oral contraception use); and at least one active MTrP in the upper trapezius muscle, with spontaneous local or referred persistent pain for at least six months. (2) Exclusion criteria: accentuated postural abnormalities (verified by physical therapist C.E.E.M.), fibromyalgia syndrome, cervical radiculopathy, systemic disease or physical therapy interventions for myofascial pain within one month before the study, pregnancy, chronic pacemaker or electronic implant use (reported by the subject). Latent MTrP was not an exclusion criterion. The continuous use of medications for headache and muscular pain was also an exclusion criterion. Moreover, subjects with evident cognitive impairment or communication difficulties during the first meeting were excluded.
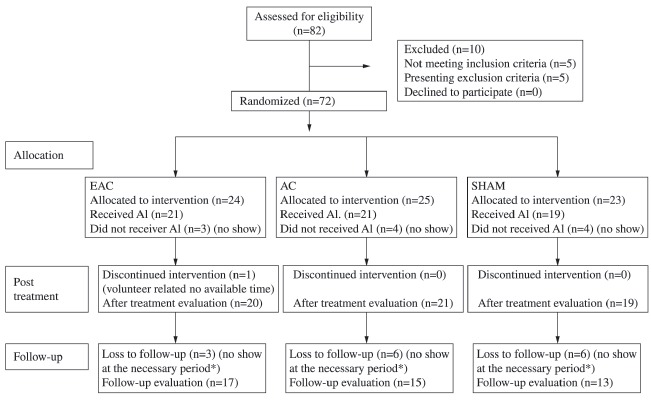
Initially, 82 volunteers were eligible. Ten were not included: two above BMI limit; one without active MTrPs; one with pain for less than six months, one without a regular menstrual cycle; one pregnant, one with a cervical hernia; one with trigeminal neuralgia; two with fibromyalgia. Seventy-two volunteers were included. Of these, seven dropped out before the first session and five started but did not complete the eight treatment sessions (Figure 1). Consequently, the statistical power was reconsidered as 0.70, according to the parameters cited above, determining a minimum of 20 subjects for each group. Nevertheless, in the SHAM group, 19 volunteers completed the treatment.
Figure 1. Enrollment of participants and study design. Al = Allocated intervention; *refers to menstrual cycle period.
Women should be evaluated in the same phase of their cycle because both absolute and relative hormone levels could influence pain19. Thus, measurements (pre-, post-treatment, and follow-up) were fixed between the second and the fifth day of menstruation period, with 28 days between each measurement. Between evaluation and reevaluation, eight sessions were scheduled, two per week. Reevaluation was scheduled three to six days after the last session, coinciding with the second to the fifth day of the volunteer's menstrual phase.
All volunteers were diagnosed as having active MTrPs bilaterally. Each side was analyzed separately. They were distributed among three groups: EAC, AC, and SHAM. First, the volunteers were coded by the blinded examiner according to their use of oral contraceptives: paused, continuous or without oral contraception. After that, they were randomly allocated to each group using Excel. Therefore, all volunteers had the same chance of being allocated to any group, avoiding the predominance of one oral contraceptive condition among groups. Right was the dominant side. One volunteer was left-handed (EAC group).
Instrumentation
The device used for the EAC was the EL608 NKL (ANVISA 80191680002). The needles were stainless steel, individually wrapped, sterile, and disposable, with a diameter of 0.25 mm and a length of 30 mm (Dong-Bang, Korea).
The Visual Analog Scale (VAS) assessed the intensity of general pain and pain in the right and left upper trapezius. The scale consists of an unanchored horizontal line 10 centimeters in length, with one end corresponding to zero ("no pain") and the other to 10 ("maximum pain").
The fleximeter, used for cervical motion measurements, consisted of a gravity-dependent inclinometer with a graduated scale attached to the head with Velcro tap (Code Research Institute, Brazil).
To monitor intercurrences between sessions, an additional data form, consisting of open-ended questions about trauma, headaches, neck and shoulder pain, medications (such as analgesics, non-steroidal anti-inflammatories, and spasmolytic drugs) and the respective doses, was applied at the beginning of the sessions. Additionally, emotional stress conditions that could occur between sessions were considered because muscle tension can be an expression of anxiety and emotional tension1. Such conditions were considered influencing factors, i.e. they could interfere with the treatment effects.
Procedures
The diagnosis of MTrP was based on five criteria1 , 3: (1) the presence of a palpable taut band in the muscle; (2) the presence of a hypersensitive tender spot in a taut band; (3) a local twitch response elicited by the snapping palpation of the taut band; (4) reproduction of the typical referred pain pattern of the MTrP in response to compression; (5) the spontaneous presence of the typical referred pain pattern and/or recognition of the referred pain as familiar. MTrP was considered active if the referred pain, whether spontaneous or evoked by compression, reproduced the subject's complaint; MTrP was considered latent if the referred pain did not reproduce a usual or familiar pain. The volunteer remained seated on a chair during the examination.
Both VAS and fleximetry were measured pre- and post-treatment and at the follow up. Volunteers were asked to mark their pain between "no pain" and "maximum pain" on the printed VAS. Afterwards, the marked location was measured with a ruler (in centimeters) by the blinded examiner.
The head and neck movements evaluated were: flexion, extension, inclination to the right and to the left, and rotation to the right and to the left. All movements except rotation were measured with the subjects seated on a chair with the back straight, eyes looking straight ahead and parallel to the floor, knees flexed at 90 degrees and feet flat on the floor. For the rotation movements, the volunteers had to stay in the supine position to keep the fleximeter favorably positioned relative to the effects of gravity.
During EAC application, the patient remained in the prone position. Needles were inserted bilaterally into points GB21 and GB20 (local analgesic acupoints) and unilaterally into LI4, LV320 (distal analgesic acupoints), and a maximum of two needles on each side directly in the region of the "Ashi Points" (painful points not predicted on meridians, not necessarily MTrP, detected before each session according to subject report at soft palpation of muscle). The equipment was programmed as follows: alternating frequency F1=2 Hz, T1=5 seconds, F2=100 Hz, T2=5 seconds; total time: 30 minutes; intensity: maximum supported by the patient without pain12 , 21. The acupuncture group received the same treatment but without the connection to the alternating frequency equipment. The SHAM acupuncture group had the needles inserted 1 cm distally from the correct acupoints.
Statistics
The assumptions of equality of variances and normal distribution were checked for all variables (Shapiro-Wilk test). Intragroup comparisons were analyzed using Student's paired t-test or Wilcoxon's signed rank test, one-way repeated measures ANOVA or the Friedman repeated measures with the Student-Newman-Keuls method for post-hoc analysis. To identify intergroup differences, one-way ANOVA or the Kruskal-Wallis test was used, with Dunn's Method as the post-hoc analysis. Moreover, analysis of variance was applied based on a generalized linear mixed model for two factors: group (fixed) and time of evaluation as repeated measures. This analysis used the t-test adjusted with the Tukey-Kramer test. Pearson's correlation was applied and SigmaPlot (Systat Software, San Jose, CA, USA) was used. A generalized linear mixed model was developed with SAS System (SAS Institute Inc, release 9.3. SAS Institute Inc., Cary, NC, USA; 2010).
Results
The final sample consisted of 60 females. Their mean age was 27.33±4.95 years, and their BMI ranged from 19.31 to 25.79 Kg/m2 (22.55±3.24 Kg/m2). All volunteers were diagnosed with active MTrPs bilaterally. Each side was analyzed separately. The sample distribution in accordance to oral contraceptive use was similar among treatment groups. For paused and continuous oral contraception, eight and four volunteers were allocated to the EAC, AC, SHAM groups, respectively. The corresponding values for those without oral contraception were eight, nine, and seven.
Forty-five females attended the follow-up session. Their mean age and BMI were 26.73±4.76 years and 22.58±3.30 Kg/m2, respectively.
Pain intensity
Pre-treatment (Figure 2A, B, C)
Figure 2. Means and standard deviations for general pain (A), pain at the right upper trapezius (B) and at the left upper trapezius (C) in pre- and post-treatment and including the follow-up evaluation (D, E, F). Uppercase letters above the standard deviation bars refer to intragroup comparisons: A?B (P<0.05); lowercase letters refer to intergroup comparisons: c: AC=EAC and AC=SHAM; d: SHAM=AC and AC?EAC; a?b*(P<0.05).
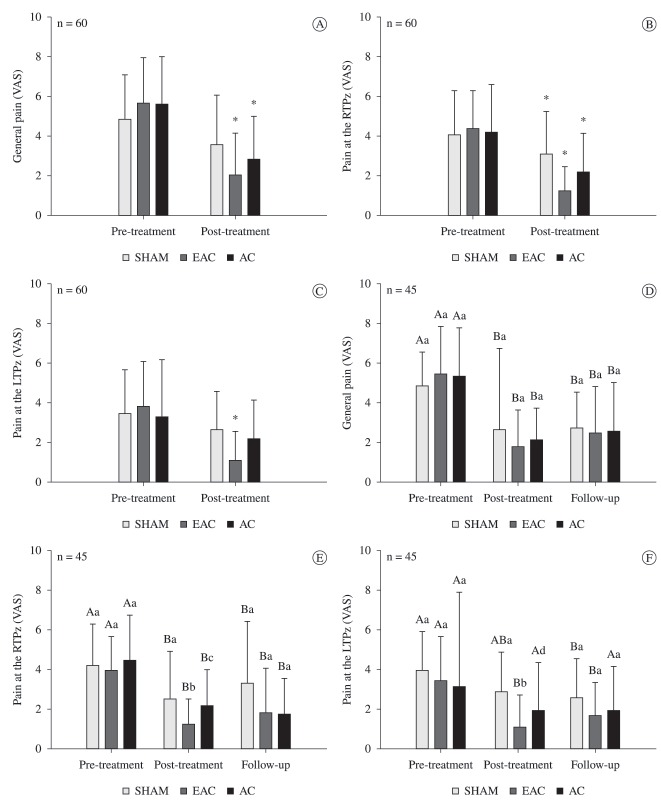
The comparisons among the three treatment groups in the same moment showed that in the pre-treatment evaluation, there were no differences among groups concerning general pain (P=0.493) or pain in the right upper trapezius (P=0.908) or the left upper trapezius (P=0.723), indicating the homogeneity of the groups.
The basal pain values showed no differences according to oral contraceptive conditions.
Post-treatment (Figure 2A, B, C)
As Figure 2 presents, only the EAC and AC groups showed significant decreases in general pain after treatment (EAC, P<0.001; AC, P<0.001; SHAM, P=0.078). The upper trapezius muscle presented a significant improvement in pain intensity in all groups for right upper trapezius (EAC, P<0.001; AC, P=0.025; SHAM, P=0.038) and in the EAC for left upper trapezius (P<0.001). Post-treatment comparisons indicated significantly lower pain on both sides of the upper trapezius in the EAC group compared to SHAM (right P=0.030; left P=0.015).
Follow-up (Figure 2D, E, F)
A comparison of the volunteers who attended the follow-up evaluation showed no pre-treatment difference between the groups (general pain: P=0.581, right upper trapezius: P=0.761, left upper trapezius: P=0.844). In the post-treatment evaluations, the EAC showed significantly lower pain intensity on both sides of the upper trapezius (P<0.05). There were no differences among groups at follow-up.
Multiple comparisons
A generalized linear mixed model analysis for two factors (group and time of evaluation) showed a decrease in general pain in the EAC and AC groups (P<0.05) and a decrease in pain intensity in the right and left upper trapezius for the EAC group (P<0.05), but not for the AC and SHAM groups. Despite this finding, no significant intragroup difference was noted in the follow-up data (Figure 2D, E, F).
Range of motion
There were no significant differences in basal values among the three groups for the movements. After treatment, a significant increase in rotation to the right (P=0.049) was observed in the EAC group, and significant increases in inclination to the right (P=0.005) and rotation to the right (P=0.032) were observed in the AC group. No changes occurred in the SHAM group (Table 1). Regarding the follow-up evaluation, only the increase in inclination to the right in the AC group was maintained (P>0.05; Table 2). An analysis of generalized linear mixed models failed to identify intragroup differences, either after treatment or at follow-up (P>0.05). Moreover, the correlations between VAS and fleximetry data were not significant (P>0.05). Some correlations among cervical range of motion that were not significant before treatment were significant on post-treatment evaluation: flexion vs rotation to the left (r=0.32); flexion vs rotation to the right (r=0.26); extension vs rotation to the right (r=0.30); and extension vs inclination to the right (r=0.53).
Table 1. Intra- and intergroup comparisons of range of motion pre-treatment and post-treatment (eight sessions; means±standard deviations).
| EAC (n=20) | AC (n=21) | SHAM (n=19) | |||||
|---|---|---|---|---|---|---|---|
| Flexion | PRE | 53.95±7.78 | P=0.218 | 54.00±18.00 | P=0.054 | 52.63±11.39 | P=0.213 |
| POST | 56.15±9.04 | 58.00±8.00 | 55.68±5.64 | ||||
| Extension | PRE | 64.85±10.06 | P=0.844 | 66.76±12.31 | P=0.356 | 70.00±14.00 | P=0.927 |
| POST | 64.40±10.63 | 69.05±13.59 | 67.00±13.00 | ||||
| Inclination to the right | PRE | 43.40±6.29 | P=0.587 | 41.81±6.20* | P =0.005 | 41.21±7.66 | P=0.152 |
| POST | 44.20±6.64 | 44.86±5.79* | 43.26±6.89 | ||||
| Inclination to the left | PRE | 41.65±7.11 | P=0.220 | 40.67±6.92 | P=0.060 | 42.79±9.67 | P=0.751 |
| POST | 43.95±7.78 | 42.95±7.58 | 43.37±8.01 | ||||
| Rotation to the right | PRE | 69.50±9.43 | P=0.051 | 70.67±7.92* | P=0.032 | 69.84±9.63 | P=0.117 |
| POST | 73.70±10.25 | 74.00±7.73* | 72.84±7.94 | ||||
| Rotation to the left | PRE | 69.05±11.36* | P=0.049 | 70.86±9.70 | P=0.095 | 70.05±10.89 | P=0.917 |
| POST | 73.30±8.29* | 73.19±10.18 | 70.26±12.43 | ||||
PRE= Pre-treatment, POST= Post-treatment; *in the same column means intragroup differences (bold fonts); Intergroup comparisons: no significant differences (P>0.05); Normal fonts: Paired t-test (means and standard deviations); Italic fonts: Wilcoxon's signed rank test (medians and interquartile deviations).
Table 2. Intra- and intergroup comparisons of range of motion in 45 volunteers who attended the follow-up evaluation (pre-treatment, post-treatment: eight sessions; follow-up: one month).
| EAC (n=17) | AC (n=15) | SHAM (n=13) | |||||
|---|---|---|---|---|---|---|---|
| Flexion | PRE | 53.41±7.49 | P=0.415 | 52.27±9.99 | P=0.079 | 52.39±12.06 | P=0.263 |
| POST | 55.77±9.34 | 56.20±8.28 | 55.79±5.02 | ||||
| FU | 55.06±7.66 | 55.60±10.75 | 57.15±7.67 | ||||
| Extension | PRE | 64.24±8.15 | P=0.997 | 68.00±12.04 | P=0.244 | 71.70±9.40 | P=0.853 |
| POST | 64.18±9.11 | 72.60±13.30 | 70.62±9.20 | ||||
| FU | 64.06±9.89 | 70.87±12.80 | 70.00±7.82 | ||||
| Inclination to the right | PRE | 43.53±6.62 | P=0.859 | 40.00±9.50A | P=0.002 | 43.20±7.71 | P=0.797 |
| POST | 44.00±7.12 | 45.00±8.00B | 44.30±7.30 | ||||
| FU | 44.35±4.99 | 45.00±9.50B | 44.31±6.42 | ||||
| Inclination to the left | PRE | 41.82±6.61 | P=0.166 | 41.60±6.05 | P=0.068 | 45.00±10.10 | P=0.981 |
| POST | 43.53±8.29 | 44.87±6.91 | 44.46±7.54 | ||||
| FU | 44.94±6.05 | 43.67±5.95 | 45.00±6.06 | ||||
| Rotation to the right | PRE | 69.00±10.00 | P=0.079 | 69.53±8.37 | P=0.100 | 70.84±10.39 | P=0.081 |
| POST | 76.00±13.00 | 73.47±7.93 | 75.46±9.63 | ||||
| FU | 71.00±14.00 | 73.73±7.18 | 76.308±6.90 | ||||
| Rotation to the left | PRE | 68.24±10.48 | P=0.135 | 69.80±10.44 | P=0.398 | 71.00±12.60 | P=0.399 |
| POST | 72.61±6.82 | 72.20±10.23 | 71.08±3.97 | ||||
| FU | 72.41±9.89 | 72.60±9.29 | 74.23±12.11 | ||||
PRE= pre-treatment; POST= post-treatment; FU=Follow-up; Different uppercase letters in the same column = intragroup differences (italic bold fonts); Intergroup comparisons: no significant differences; Normal fonts: one-way repeated measures analysis of variance (means and standard deviations); Italic fonts: Friedman's repeated measures analysis of variance (medians and interquartile deviations).
Considering the obtained data, the hypothesis was partially confirmed.
Additional Data Form
The monitored occurrences on previous days and between sessions were similar among groups (Table 3). Compared with the EAC and AC groups, the SHAM volunteers showed an increase in medication use and headache frequency in the last week of treatment and before the post-treatment evaluation. While the EAC and AC volunteers showed a decrease in headache frequency, the SHAM volunteers reported more headaches during the later sessions compared with the first sessions. Positive and negative life experiences remained almost unchanged for all groups. Neck and shoulder pain frequency decreased slightly in all groups, with an increase in shoulder pain between the last session and the post-treatment evaluation for the AC group.
Table 3. Percentage of volunteers who reported medication use, positive or negative life experiences, headache or neck and shoulder pain in the post-treatment evaluation (n=60).
| Sessions | 1 (n) % | 2 (n) % | 3 (n) % | 4 (n) % | 5 (n) % | 6 (n) % | 7 (n) % | 8 (n) % | 9* (n) % | |
|---|---|---|---|---|---|---|---|---|---|---|
| Medication use | SHAM | (9) 47 | (7) 37 | (5) 26 | (7) 37 | (2) 11 | (3) 16 | (2) 11 | (6) 32 | (9) 47 |
| EAC | (8) 40 | (5) 25 | (5) 25 | (8) 40 | (6) 30 | (1) 5 | (2) 10 | (3) 15 | (6) 30 | |
| AC | (13) 62 | (7) 33 | (3) 14 | (3) 14 | (5) 24 | (6) 29 | (2) 10 | (7) 33 | (6) 29 | |
| Positive life experiences | SHAM | (2) 11 | (0) 0 | (2) 11 | (1) 5 | (0) 0 | (1) 5 | (2) 11 | (1) 5 | (2) 11 |
| EAC | (3) 15 | (1) 5 | (0) 0 | (1) 5 | (0) 0 | (3) 15 | (2) 10 | (1) 5 | (2) 10 | |
| AC | (1) 5 | (0) 0 | (2) 10 | (2) 10 | (2) 10 | (0) 0 | (3) 14 | (1) 5 | (3) 14 | |
| Negative life experiences | SHAM | (8) 42 | (5) 26 | (3) 16 | (5) 26 | (3) 21 | (6) 32 | (3) 21 | (7) 37 | (6) 32 |
| EAC | (5) 25 | (3) 15 | (5) 25 | (5) 25 | (3) 15 | (3) 15 | (1) 5 | (2) 10 | (2) 10 | |
| AC | (6) 29 | (6) 29 | (4) 19 | (3) 14 | (5) 24 | (5) 24 | (3) 14 | (2) 10 | (7) 33 | |
| Headache | SHAM | (8) 42 | (11) 58 | (7) 37 | (5) 26 | (6) 32 | (7) 37 | (8) 42 | (12) 63 | (15) 79 |
| EAC | (12) 60 | (8) 40 | (8) 40 | (10) 50 | (10) 50 | (6) 30 | (9) 45 | (6) 30 | (8) 40 | |
| AC | (16) 76 | (15) 71 | (7) 33 | (8) 38 | (8) 38 | (11) 52 | (7) 33 | (8) 38 | (10) 48 | |
| Neck pain | SHAM | (13) 68 | (11) 58 | (9) 47 | (9) 47 | (8) 42 | (10) 53 | (10) 53 | (10) 53 | (9) 47 |
| EAC | (13) 65 | (11) 55 | (13) 65 | (11) 55 | (10) 50 | (6) 30 | (8) 40 | (11) 55 | (8) 40 | |
| AC | (16) 76 | (12) 57 | (10) 48 | (13) 62 | (11) 52 | (13) 62 | (10) 48 | (11) 52 | (13) 62 | |
| Shoulder pain | SHAM | (19) 100 | (16) 84 | (12) 63 | (13) 68 | (15) 79 | (11) 58 | (13) 68 | (14) 74 | (11) 58 |
| EAC | (16) 80 | (16) 80 | (16) 80 | (14) 70 | (12) 60 | (12) 60 | (9) 45 | (13) 65 | (12) 60 | |
| AC | (20) 95 | (15) 71 | (17) 81 | (16) 76 | (11) 52 | (11) 52 | (12) 57 | (13) 62 | (11) 52 | |
post-treatment evaluation.
Discussion
This study aimed to identify whether EAC and AC are effective for treating pain and increasing range of motion in women with myofascial pain in the upper trapezius, with SHAM acupuncture as a control. The treatment did not intend to inactivate a specific MTrP, but to reestablish balance, stop stagnant energy, decrease pain, and therefore improve muscle function. Only women were included as they are more likely to develop neck pain than men5 , 6. Both the paired data and the results of the intergroup comparisons indicated that EAC and AC contribute more to the decrease in myofascial pain than SHAM acupuncture does. The fact that the EAC group presented significantly lower pain on both sides than SHAM after the respective treatments, whereas no difference was found between AC and SHAM, suggests that EAC treatment had an advantage with respect to pain intensity. Intergroup analysis for two factors showed that EAC improved general and local pain in the right and left upper trapezius, whereas AC was effective only for general pain, indicating better analgesic effects of EAC. In this sense, the analgesic effect of transcutaneous electrical acupoint stimulation22, which differs from EAC by the presence of a transcutaneous electrode instead of a needle, has already been described. An increase in blood flow after the use of transcutaneous electrical nerve stimulation within the upper trapezius muscle has also been reported23. Therefore, it is possible that the use of EAC may increase blood flow and remove the chemical mediators from the MTrP area, thereby facilitating a mechanical relaxation of the MTrP taut band. Although AC has showed a superior analgesic effect compared with SHAM or placebo8, the data in the present study suggest that the EAC group had electrical analgesic effects in addition to the needle acupoint stimulation effect of AC, therefore presenting better results. Accordingly, it was demonstrated that EAC reduced the use of opioid-like medication by chronic pain patients11 and also decreased pain intensity and increased the pressure pain threshold in women with myofascial pain in the upper trapezius after eight sessions of EAC applied to the same acupoints12. Regarding the analgesic effect of needling, although multiple needle insertion has been found to be better than simple needling insertion as in AC and EAC, myofascial trigger point irritability was found to be suppressed after remote acupuncture treatment, as considered by Chou et al.24. Therefore, the decrease in pain intensity in these treated groups could have been partially related to this suppression.
The treated groups also showed better results than SHAM with respect to range of motion. Although the decrease in pain would lead to a decrease in muscular stiffness and an increase in range of motion, no correlation between VAS and fleximetry data was found, corroborating a recent cohort study evaluating 4,293 subjects, which found a significant difference in pain intensity but not in cervical range of motion25, and agreeing with Gemmell and Hilland26.
Bilateral contraction of the upper trapezius muscle extends the neck and unilateral contraction flexes the neck, inclining the head to the same side and rotating it to the opposite side16. Thus, the improvement in myofascial pain in the upper trapezius would be expected to improve function, increasing the range of motion as described above. However, the increase in inclination to the right that was observed after treatment with AC and maintained until the follow-up evaluation can be related to the shortening of right upper trapezius fibers and the stretching of left upper trapezius fibers27. Although one side's function depends on the other side's function, the expected significant improvement in the inclination to the left was not obtained, reflecting the complexity of interpreting each component of neck movements separately. Moreover, it should be noted that rotation to the right almost presented significant difference for EAC and flexion for AC (Table 1). In this sense, we found three moderate positive correlations between movements related to upper trapezius in post-treatment that were absent in pre-treatment. These results might suggest integrated improvement in muscle function despite the absence of significant changes in some cervical movements.
Currently, the number of studies comparing individuals with nonspecific neck pain to the normal population is insufficient to allow conclusions about any specific physical dimensions related to nonspecific neck pain28, which can be caused by a mechanical or myofascial problem. Furthermore, available research comparing range of motion assessment tools shows that despite the high reproducibility and reliability of some methods, average values vary greatly depending on the instrument used29. Often, data findings represent healthy individuals6 in other age groups or include both genders29.
Nevertheless, paired data showed some improvement in the cervical range of motion of the two treated groups indicating the efficacy of AC and EAC compared to SHAM, which presented no significant changes. Despite this, intergroup analyses have failed to detect differences between groups. It is possible that both EAC and AC have contributed, albeit slightly, to the relaxation of the contracted fibers, however it is important that further studies include stretching exercises to investigate the benefits of the combination of both treatments.
Differences in muscle activity between the dominant and non-dominant side have been shown30, probably influencing the effects of treatment for muscle function. The contraction of the right upper trapezius promoted a significant increase (P<0.05) in inclination to the right (AC) and rotation to the right (EAC and AC). The left-handed volunteer (EAC) was the only one presenting improvement in rotation to the left.
The homogeneous distribution according to oral contraception could minimize the effects of hormonal fluctuations. Also, the additional data form was helpful, among other things, for monitoring factors such as the frequency of medication use and for showing that pain relief was not caused by an increased use of analgesics. There was little variation in reported positive and negative life experiences, which do not seem to have influenced the results. The percentage of headache complaints, possibly the referred pain from myofascial pain in the upper trapezius, was lower for the EAC and AC groups and higher for the SHAM group, in accordance with the data obtained.
Limitations must be addressed, such as the needle insertion 1 cm away from acupoints in the SHAM group but still in the dysfunctional region, possibly having some effect on the pain. Conversely, the effect of needle insertion could be present in all treated groups, thus weakening the respective influence. Fifteen volunteers did not attend the follow-up session, however this fact is inherent to clinical research. On the other hand, the initial sample attended all sessions accordingly, supporting the findings.
Conclusion
Both AC and EAC were superiorly effective in reducing myofascial pain compared with SHAM acupuncture. Nonetheless, EAC was better than AC for pain relief in the studied sample. There are indications that those treatments can assist in increasing range of motion, albeit subtly.
Acknowledgements
To Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), São Paulo, SP, Brazil (Process 2010/11684-0 and Process 2011/12659-1). We also wish to thank the volunteers.
References
- 1.Simons DG, Travell JG, Simons LS. Myofascial pain and dysfunction: the trigger point manual. Baltimore: Williams & Wilkins; 1999. [Google Scholar]
- 2.Gerber LH, Sikdar S, Armstrong K, Diao G, Heimur J, Kopecky J, et al. A systematic comparison between subjects with no pain and pain associated with active myofascial trigger points. PM R. 2013;5(11):931–938. doi: 10.1016/j.pmrj.2013.06.006. http://dx.doi.org/10.1016/j.pmrj.2013.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerwin RD. Differential diagnosis of myofascial pain syndrome and fibromyalgia. J Musculoskeletal Pain. 1999;7(1):209–215. http://dx.doi.org/10.1300/J094v07n01_19 [Google Scholar]
- 4.Grosshandler SL, Stratas NE, Toomey TC, Gray WF. Chronic neck and shoulder pain. Focusing on myofascial origins. Postgrad Med. 1985;77(3):149-51, 154-8. doi: 10.1080/00325481.1985.11698897. [DOI] [PubMed] [Google Scholar]
- 5.Fleckenstein J, Zaps D, Rüger LJ, Lehmeyer L, Freiberg F, Lang PM, et al. Discrepancy between prevalence and perceived effectiveness of treatment methods in myofascial pain syndrome: results of a cross-sectional, nationwide survey. BMC Musculoskelet Disord. 2010;11(1):32–32. doi: 10.1186/1471-2474-11-32. http://dx.doi.org/10.1186/1471-2474-11-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skillgate E, Magnusson C, Lundberg M, Hallqvist J. The age- and sex-specific occurrence of bothersome neck pain in the general population-results from the Stockholm public health cohort. BMC Musculoskelet Disord. 2012;13(1):185–185. doi: 10.1186/1471-2474-13-185. http://dx.doi.org/10.1186/1471-2474-13-185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rollman GB, Lautenbacher S. Sex differences in musculoskeletal pain. Clin J Pain. 2001;17(1):20–24. doi: 10.1097/00002508-200103000-00004. http://dx.doi.org/10.1097/00002508-200103000-00004 [DOI] [PubMed] [Google Scholar]
- 8.Stux G, Pomeranz B. Basics of acupuncture. Berlin: Springer-Verlag; 1995. [Google Scholar]
- 9.Koski BL, Dunn KS, Shebuski MR. Daily activity patterns of an adult experiencing lower back pain undergoing electro-acupuncture: a case study. Pain Manag Nurs. 2009;10(4):188–196. doi: 10.1016/j.pmn.2008.06.001. http://dx.doi.org/10.1016/j.pmn.2008.06.001 [DOI] [PubMed] [Google Scholar]
- 10.Sun MY, Hsieh CL, Cheng YY, Hung HC, Li TC, Yen SM, et al. The therapeutic effects of acupuncture on patients with chronic neck myofascial pain syndrome: a single-blind randomized controlled trial. Am J Chin Med. 2010;38(5):849–859. doi: 10.1142/S0192415X10008299. http://dx.doi.org/10.1142/S0192415X10008299 [DOI] [PubMed] [Google Scholar]
- 11.Zheng Z, Guo RJ, Helme RD, Muir A, Costa C, Xue CCL. The effect of electroacupuncture on opioid-like medication consumption by chronic pain patients: a pilot randomized controlled clinical trial. Eur J Pain. 2008;12(5):671–676. doi: 10.1016/j.ejpain.2007.10.003. http://dx.doi.org/10.1016/j.ejpain.2007.10.003 [DOI] [PubMed] [Google Scholar]
- 12.Aranha MFM, Alves MC, Bérzin F, Gavião MBD. Efficacy of electroacupuncture for myofascial pain in the upper trapezius muscle: a case series. Rev Bras Fisioter. 2011;15(5):371–379. doi: 10.1590/s1413-35552011005000022. http://dx.doi.org/10.1590/S1413-35552011005000022 [DOI] [PubMed] [Google Scholar]
- 13.Fernández-de-las-Peñas C, Alonso-Blanco C, Miangolarra JC. Myofascial trigger points in subjects presenting with mechanical neck pain: a blinded, controlled study. Man Ther. 2007;12(1):29–33. doi: 10.1016/j.math.2006.02.002. http://dx.doi.org/10.1016/j.math.2006.02.002 [DOI] [PubMed] [Google Scholar]
- 14.Muñoz-Muñoz S, Muñoz-García MT, Alburquerque-Sendín F, Arroyo-Morales M, Fernández-de-las-Peñas C. Myofascial trigger points, pain, disability, and sleep quality in individuals with mechanical neck pain. J Manipulative Physiol Ther. 2012;35(8):608–613. doi: 10.1016/j.jmpt.2012.09.003. http://dx.doi.org/10.1016/j.jmpt.2012.09.003 [DOI] [PubMed] [Google Scholar]
- 15.Grieve R, Barnett S, Coghill N, Cramp F. The prevalence of latent myofascial trigger points and diagnostic criteria of the triceps surae and upper trapezius: a cross sectional study. Physiotherapy. 2013;99(4):278–284. doi: 10.1016/j.physio.2013.04.002. http://dx.doi.org/10.1016/j.physio.2013.04.002 [DOI] [PubMed] [Google Scholar]
- 16.Kendall FP, McCreary EK, Provance PG. Músculos provas e funções. Brasil: Editora Manole; 1995. [Google Scholar]
- 17.Tousignant M, Smeesters C, Breton AM, Breton E, Corriveau H. Criterion validity study of the cervical range of motion (CROM) device for rotational range of motion on healthy adults. J Orthop Sports Phys Ther. 2006;36(4):242–248. doi: 10.2519/jospt.2006.36.4.242. http://dx.doi.org/10.2519/jospt.2006.36.4.242 [DOI] [PubMed] [Google Scholar]
- 18.Florêncio LL, Pereira PA, Silva ER, Pegoretti KS, Gonçalves MC, Bevilaqua-Grossi D. Agreement and reliability of two non-invasive methods for assessing cervical range of motion among young adults. Rev Bras Fisioter. 2010;14(2):175–181. [PubMed] [Google Scholar]
- 19.Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, Fillingim RB, et al. Consensus Working Group of the Sex, Gender, and Pain SIG of the IASP Studying sex and gender differences in pain and analgesia: a consensus report. Pain. 2007;132(Suppl 1):S26–S45. doi: 10.1016/j.pain.2007.10.014. http://dx.doi.org/10.1016/j.pain.2007.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin YL, Chen CY, Hammes M, Kolster BC. Atlas gráfico de acupuntura. São Paulo: Konemann Port; 2005. [Google Scholar]
- 21.Zhu XM, Polus B. A controlled trial on acupuncture for chronic neck pain. Am J Chin Med. 2002;30(1):13–28. doi: 10.1142/S0192415X02000028. http://dx.doi.org/10.1142/S0192415X02000028 [DOI] [PubMed] [Google Scholar]
- 22.Yuan CS, Attele AS, Dey L, Lynch JP, Guan X. Transcutaneous electrical acupoint stimulation potentiates analgesic effect of morphine. J Clin Pharmacol. 2002;42(8):899–903. doi: 10.1177/009127002401102812. http://dx.doi.org/10.1177/009127002401102812 [DOI] [PubMed] [Google Scholar]
- 23.Sandberg ML, Sandberg MK, Dahl J. Blood flow changes in the trapezius muscle and overlying skin following transcutaneous electrical nerve stimulation. Phys Ther. 2007;87(8):1047–1055. doi: 10.2522/ptj.20060178. http://dx.doi.org/10.2522/ptj.20060178 [DOI] [PubMed] [Google Scholar]
- 24.Chou LW, Hsieh YL, Chen HS, Hong CZ, Kao MJ, Han TI. Remote therapeutic effectiveness of acupuncture in treating myofascial trigger point of the upper trapezius muscle. Am J Phys Med Rehabil. 2011;90(12):1036–1049. doi: 10.1097/PHM.0b013e3182328875. http://dx.doi.org/10.1097/PHM.0b013e3182328875 [DOI] [PubMed] [Google Scholar]
- 25.Kauther MD, Piotrowski M, Hussmann B, Lendemans S, Wedemeyer C. Cervical range of motion and strength in 4,293 young male adults with chronic neck pain. Eur Spine J. 2012;21(8):1522–1527. doi: 10.1007/s00586-012-2369-x. http://dx.doi.org/10.1007/s00586-012-2369-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gemmell H, Hilland A. Immediate effect of electric point stimulation (TENS) in treating latent upper trapezius trigger points: a double blind randomised placebo-controlled trial. J Bodyw Mov Ther. 2011;15(3):348–354. doi: 10.1016/j.jbmt.2010.04.003. http://dx.doi.org/10.1016/j.jbmt.2010.04.003 [DOI] [PubMed] [Google Scholar]
- 27.Rodríguez-Fernández AL, Garrido-Santofimia V, Güeita-Rodríguez J, Fernández-de-Las-Peñas C. Effects of burst-type transcutaneous electrical nerve stimulation on cervical range of motion and latent myofascial trigger point pain sensitivity. Arch Phys Med Rehabil. 2011;92(9):1353–1358. doi: 10.1016/j.apmr.2011.04.010. http://dx.doi.org/10.1016/j.apmr.2011.04.010 [DOI] [PubMed] [Google Scholar]
- 28.Lee H, Nicholson LL, Adams RD. Cervical range of motion associations with subclinical neck pain. Spine (Phila Pa 1976) 2004;29(1):33–40. doi: 10.1097/01.BRS.0000103944.10408.BA. http://dx.doi.org/10.1097/01.BRS.0000103944.10408.BA [DOI] [PubMed] [Google Scholar]
- 29.Chaves TC, Nagamine HM, Belli JFC, Hannai MCT, Bevilaqua-Grossi D, Oliveira AS. Reliability of fleximetry and goniometry for assessing neck range of motion among children. Rev Bras Fisioter. 2008;12(4):283–289. http://dx.doi.org/10.1590/S1413-35552008000400006 [Google Scholar]


