Abstract
Young female offenders represent a growing number of young offenders. Studies have shown that youth in the juvenile justice system, particularly young females, report higher rates of lifetime sexual abuse than their nonoffending peers. The aim of this study was to examine gender differences in risk factors for recidivism, including a history of sexual abuse, among a juvenile court clinic sample. Findings suggest that, even after accounting for previously identified risk factors for recidivism such as prior legal involvement and conduct problems, a history of sexual abuse is the most salient predictor of recidivism for young female offenders, but not for males. The development of gender-responsive interventions to reduce juvenile recidivism and continued legal involvement into adulthood may be warranted.
Keywords: juvenile justice, recidivism, gender differences, sexual abuse
Girls make up a growing percentage of the juvenile justice population. From 1985 to 2009, delinquent crimes among girls increased by 86% (from 222,900 in 1985 to 415, 600 in 2009). For boys, however, rates of delinquency increased only slightly (by 17%) over that same time period (i.e., from 932,300 to 1,088,600 total male delinquency crimes reported). (Puzzanchera, Adams, & Hockenberry, 2012). Unlike boys entering the legal system, girls are most often nonviolent offenders (Zavlek & Maniglia, 2007) who present with numerous psychosocial challenges including elevated rates of child abuse, violence exposure, mental health problems, family conflict, pregnancy, and school failure (Zahn, Hawkins, Chiancone, & Whiteworth, 2008). Although there is growing evidence that girls involved in the juvenile justice system have unique needs (Chandy, Blum, & Resnick, 1996; Gavazzi, Yarcheck, & Chesney–Lind, 2006; Odgers, Moretti, & Reppucci, 2010; Puzzanchera et al., 2012; Salekin, Rogers, Ustad, & Sewell, 1998) only a small number of studies have focused on gender-specific trajectories into the legal system and even fewer have focused on factors that pose risk for repeat legal involvement (i.e., recidivism).
Sexual Abuse
Childhood sexual abuse (CSA) is a potent risk factor for delinquency and subsequent juvenile justice involvement, especially for young women (Chesney–Lind, 1997; Gavazzi et al., 2006; Hubbard & Pratt, 2002). A person that experiences any type of maltreatment during childhood, including sexual abuse, is significantly more likely to be arrested, as a juvenile or adult, than a person who was not maltreated (Widom, 1995; Widom & Maxfield, 2001). In 2008 alone there were 690,869 children in the United States who were confirmed by Child Protective Services as being victims of maltreatment and 11% of those children were confirmed victims of sexual abuse (Nelson, 2008). Studies have shown that CSA victims are more susceptible to psychosocial and behavioral difficulties than other abuse and neglect victims (Widom & Ames, 1994) and are more likely to experience psychiatric symptoms (Chen et al., 2010; Paolucci, Genuis, & Violato, 2001; Tebbutt, Swanson, Oates, & O'Tool, 1997). A recent meta-analysis conducted by Chen et al. (2010) found that CSA was associated with multiple psychiatric disorders including anxiety, depression, eating disorders and posttraumatic stress disorder (PTSD). Additionally, research of sexually abused youth have shown that sexually victimized youth are more likely to report having committed crimes than nonabused youth, and show significantly higher rates of externalizing behavior, specifically aggression, relative to their nonabused counterparts (Chen et al., 2010; Paolucci et al., 2001; Swanston et al., 2003).
Research related to gender differences in the psychiatric sequelae of sexual abuse is mixed. While Chen et al. (2010) did not find gender differences in the associations between sexual abuse and psychiatric diagnosis, other studies have suggested that sexual abuse during childhood impacts girls differently than boys (Rind & Tromovitch, 1997). Rind and Tromovitch (1997) conducted a meta-analysis of the psychological correlates of sexual abuse and found that negative symptomatology (e.g., poor physical and mental health, general adjustment, low self-esteem, and sexual risk behavior) was more commonly associated with girls who had been sexually abused. Furthermore, the symptom expression linked with childhood abuse has been shown to be greater in girls than boys (Goodkind, Ng, & Sarri, 2006; Rind & Tromovitch, 1997) and include symptoms such as higher levels of depression, lower levels of self-esteem, intrusive thoughts, hyper-arousal, anxiety, and personal vulnerability (Feiring, Taska, & Lewis, 1999).
For females, sexual abuse has been associated with a variety of negative outcomes including involvement in both the juvenile justice system and the adult criminal justice system (Goodkind et al., 2006; Holsinger, Belknap, & Sutherland, 1999; Hubbard & Pratt, 2002). High rates of trauma, abuse victimization and neglect in offending girls (up to 84% of justice involved girls reporting some kind of trauma exposure) have been associated with girls' increased substance use and more severe psychopathology (Abram et al., 2004; Lopez et al., 2011; McCabe, Lansing, Garland, & Hough, 2002); these outcomes are also correlated with juvenile justice involvement (Abram et al., 2007; Teplin, Mericle, McClelland, & Abram, 2003). Furthermore, certain psychological constructs that appear to be impacted by the experience of sexual abuse, such as self-esteem, self-efficacy, gender, and ethnic identity development and empowerment, are related to girls' development of poor health and behavioral outcomes such as increased HIV risk behaviors and substance use (De La Rosa, Dillion, Rojas, Schwartz, & Duan, 2010; Guthrie & Flinchbaugh, 2001; Khoury, 1998).
Recidivism
Court-involved, nonincarcerated (CINI) juveniles comprise approximately two-thirds of the juvenile justice population (Puzzanchera, 2009). It has been estimated that between one-half and one-third of this population has a diagnosable psychiatric condition (Gavazzi et al., 2006). A majority of these youth present with symptoms of conduct disorder and substance use disorders (Vermeiren, Jespers, & Moffitt, 2006). Studies have found that CINI juveniles with substance use disorders and psychiatric problems are at increased risk for substance-related recidivism (Vermeiren et al., 2006), persistent reoffending and self-reported antisocial activity (Schubert, Mulvey, & Glasheen, 2011). Additionally, cooccurring substance use and psychiatric (“dual diagnosis”) disorders have been linked with higher risk for future detention in youth court-ordered for forensic mental health evaluation (Tolou-Shams, et al., in press). However, little is known about the impact of sexual abuse history on risk for recidivism among this sample of young offenders.
Chesney–Lind (1989, 1997) has suggested that there are gender differences in recidivism risk and that abuse experiences in childhood are often the precipitant for delinquent behavior in girls (Zahn et al., 2008). The difference in adult male and female pathways to recidivism has been highlighted in the adult literature (Reisig, Holtfreter, & Morash, 2006). Studies focused on recidivism among adult women have shown that sexual abuse in childhood, interpersonal relationships (e.g., association with negative males partners and limited sources of interpersonal support) and substance use are associated with increased recidivism risk for women (Daly, 1992; Hubbard & Pratt, 2002; Owen & Bloom, 1995). However, males appear to become involved in the juvenile justice through association with deviant peers, physical aggression (toward person or property), or oppositional attitudes and behaviors (Dembo, Williams, & Schmeidler, 1993; Reid, Patterson, & Dishion, 1997).
When evaluating the influence of CSA on recidivism, the role of externalizing disorders (one of the strongest predictors of recidivism among juvenile justice youth) must also be considered (Gavazzi et al., 2006). It has been estimated that over 40% of incarcerated juveniles meet criteria for a disruptive behavior disorder (Teplin, Abram, McClelland, Dulcan, & Mericle, 2002) and longitudinal studies suggest that these disorders are persistent across period of 2 years (Teplin, Welty, Abram, Dulcan, & Washburn, 2012). Among boys, a diagnosis of conduct disorder (CD) is one of the strongest predictors of adult antisocial behavior (Pardini & Fite, 2010). Oppositional defiant disorder (ODD) symptoms have also been shown to predict later criminal charges and conduct problems among boys (Pardini & Fite, 2010). Although externalizing disorders are more prevalent among boys they likely also contribute to recidivism among girls. Moreover, it is not known whether CSA confers risk above and beyond the most salient risk of having an externalizing disorder diagnosis.
Juvenile Court Clinics
Court mental health clinics provide a wide array of mental health services, including forensic assessment and linkage to care to help the courts determine ways to address the high prevalence of mental health problems in the juvenile justice system (Grisso & Quinlan, 2005). Court clinics serve as court-affiliated third party to assist the bench in making mental health related decisions about juveniles. Mental health evaluations are court-ordered by a presiding judge or magistrate and evaluations are conducted by neutral (i.e., not affiliated with the prosecution or the defense) licensed clinicians. Although most youth who commit crimes as juveniles do not reoffend into adulthood, court mental health clinics serve youth who may be among some of the most vulnerable to recidivate; this is because of the increased risk associated with mental health and juvenile justice system involvement. As there is a relationship between mental health disorders and CSA (Tebbutt et al., 1997), court mental health clinics may serve as an ideal setting to examine the link between CSA and recidivism.
The goal of the present study is to examine gender specific predictors of juvenile recidivism in a sample of CINI juveniles court-ordered for forensic mental health evaluation. We aimed to explore the effect of CSA on recidivism risk and how that association may vary by gender. Specifically, we hypothesized that lifetime incidence of CSA would contribute to increased risk for recidivism in adolescent girls, but not for boys. Exploring the moderating effect of gender on recidivism could assist in understanding gender-specific pathways to recidivism and identifying factors to consider when developing gender-responsive interventions for these underserved youth.
Method
Participants
This study was a retrospective chart review of 454 juvenile offenders, ages 11–17, who were court-ordered to receive a forensic mental health evaluation at a Juvenile Court Clinic (JCC) in the Northeast between 2006 and 2008. This court clinic serves status and criminal juvenile offenders who appear in front of judges and magistrates presiding over specialty court (e.g., truancy, juvenile drug court) and formal delinquency cases. Judges and magistrates provide a reason for referral that includes questions such as: is this juvenile suffering from depression; does this child need an Individual Education Plan (IEP); what level of mental health and/or substance use treatment is appropriate; is this juvenile a danger to self? Referral questions did not include questions of adjudicative competency or criminal responsibility.
Typical brief evaluation interviews lasted no more than 3–4 hr and included the following: (1) brief forensic interview of the juvenile (45–60 min), (2) forensic interview of the caregiver (45–60 min), and (3) completion of evidence-based self-report psychological assessment measures by both caregiver (regarding the juvenile's symptoms and behaviors) and the juvenile (self-report of symptoms and behaviors) (45–60 min). When English was not the juvenile or caregiver's primary language, a court-based interpreter assisted with forensic interviews, which typically extended the length of time required for the evaluation visit. In addition to the evaluation visit, time was also spent conducting relevant records review (legal and other relevant records, such as school, and outside treatment providers) and obtaining any other relevant collateral information (e.g., through interview of collateral informants). Time spent obtaining collateral information ranged from 1–3 hr, depending on the case. All forensic evaluations were conducted by licensed mental health professionals (i.e., psychologists, psychiatrists, and social workers) and the families incurred no costs for the evaluation.
Study Design and Procedures
Between 2006 and 2008, 454 juveniles were referred for a JCC mental health evaluation. Of those, 402 juveniles received a full mental health evaluation and were included in this chart review study. Fifty referred juveniles were not evaluated because of missed appointments and two juveniles received only educational testing. There were no differences between those evaluated (n = 402) and those not evaluated (n = 52) on any of the demographic or legal history variables under study (all ps > .05).
For this study, court mental health clinic records and court-maintained databases were reviewed by trained research assistants to obtain data on juveniles. This study was approved as a retrospective chart review study by the hospital Institutional Review Board. As such, a waiver was authorized for informed consent.
Mental health evaluations were coded by trained research assistants for objective variables that are included in this study, such as age, gender, race or ethnicity, psychiatric diagnosis, history of substance use, and history of CSA. Research assistants were trained to obtain κ scores of above .70 (indicating strong interrater reliability) for each variable coded. As part of this training process, each coder rated 20 mental health evaluations and then rated charts were compared with determine variables that required additional training. After coding the initial 20 charts, two research assistants independently coded the same randomly selected 100 charts. The ratings for these charts were reviewed for reliability and differences were reconciled using an independent third rater. An additional 20% (n = 70) of charts were randomly selected from the remaining 345 charts for double coding; reliability was computed to assure that coders continued to maintain high reliability. All κ coefficients remained above .70.
Measures
Predictors
Demographics
Demographic information including age, gender, and race or ethnicity were collected using a standard intake form. This form was completed by a caregiver(s) before the mental health evaluation. Age was dichotomized (based on median split) into categories of “15 years or older” and “younger than 15 years” to be consistent with other categorical demographic data.
Lifetime history of substance use
As part of the mental health evaluation, juveniles and their caregiver were asked to report the youth's history of substance use including alcohol, marijuana, and other drugs. This information was routinely included in the standard forensic mental health assessment. Raters coded yes or no for whether there was any endorsement of alcohol, marijuana, or other drug use. For this study, the aforementioned variables were collapsed into a single lifetime substance use variable. This “lifetime substance use” variable was coded yes or no based on report of any alcohol, marijuana or other drug use. Interrater reliability for this variable was acceptable (κ = .95).
Psychiatric diagnosis
A full Diagnostic and Statistical Manual for Mental Disorders–Fourth Edition (DSM–IV) axial diagnostic formulation was included in each forensic mental health evaluation. This information was used to code the presence or absence of externalizing disorders such as ODD, CD, and attention deficit hyperactivity disorder (ADHD) (κ = .94). This information was used to compute the yes or no variable related to the presence of at least one externalizing disorder for each juvenile. DSM–IV diagnoses were determined by clinicians' use of forensic interviews and standardized measures:
Forensic interviews
Separate forensic interviews were conducted by licensed mental health professionals (i.e., psychologists, psychiatrists, or social workers) with the caregiver(s) and juvenile. These interviews yielded information regarding number and type of past and current psychiatric diagnoses and substance use diagnosis comorbidity, as well as history of mental health treatment, and psychiatric hospitalization.
Standardized measures
Juveniles completed the Diagnostic Interview Schedule for Children: Present State Voice Version (VDISC; Wasserman, McReynolds, Fisher, & Lucas, 2005) and/or the Youth Inventory-4 (YI-4; Gadow & Sprafkin, 1994) and caregivers completed the Adolescent Symptom Inventory-4 (ASI-4; Gadow, Sprafkin, & Weiss, 2004). The VDISC is a self-administered computerized interview that assesses for the presence of 30 DSM–IV diagnoses. Based on their responses to questions about symptoms, each juvenile took a unique computer generated interview that provides computer scored provisional DSM–IV diagnoses. The VDISC has been validated for use with juvenile justice samples. The YI-4 (Gadow & Sprafkin, 1994) is a 128-item, self-report rating scale for children and adolescents, ages 12 to 18 years. It screens for symptoms of psychiatric disorders contained in the DSM–IV. The YI-4 has satisfactory internal consistency (α = 66 −.87), test–retest reliability (r = .54−0.92), and convergent and discriminant validity (Gadow & Sprafkin, 1994). The ASI-4 (Gadow et al., 2004) is the parallel caregiver completed questionnaire. It is a 120-item questionnaire of adolescent behaviors based on DSM–IV criteria. The ASI has demonstrated good evidence of internal consistency, test–retest reliability, and convergent validity (Gadow et al., 2004). The VDISC, YI-4, and ASI-4 are all measures that provide provisional diagnoses used to inform clinician-generated final diagnoses.
Legal history
The JCC maintains a database of legal information relevant to each juvenile referred for evaluation that is extracted from a larger court database of all juveniles processed through the Family Court. Data include: source of referral (e.g., truancy, drug, or delinquency petition), number and type of charges (criminal vs. status), history of social service involvement, and prior legal involvement or prior offense history.
Lifetime history of CSA
As part of the forensic interview, court clinic clinicians routinely asked juveniles, and their caregivers, about the juvenile's lifetime history of sexual, physical, and emotional abuse as well as other traumatic experiences (e.g., death of close family member, witness to domestic violence). History of CSA was coded “yes” if either the caregiver or the juvenile endorsed that the juvenile had any lifetime CSA experience. A code of “no” was entered if the evaluation included a statement indicating that lifetime CSA was assessed and denied by both juvenile and caregiver. Evaluations that did not include any mention of lifetime CSA were coded as missing this information. Interrater reliability for this variable was excellent (κ = .97).
Outcome
Recidivism rates were calculated using the family court database. Recidivism was defined as accruing any additional charge at 3, 6, 9, or 12 month postevaluation. For the purposes of these analyses, a recidivism outcome score (yes or no) was calculated for accruing at least one charge over the 12-month follow-up period.
Data Analysis
Before conducting group comparisons, descriptive statistics were calculated for all of the main study variables. For continuous demographic variables, such as age, median splits were used to create dichotomous variables to be consistent with other categorical or dichotomous demographic data. A series of independent logistic regression models were conducted to explore bivariate associations between study variables and to compute effect size in the form of an odds ratio (OR). Bivariate analyses compared (1) recidivists (accrued at least one new charge over 12 month follow-up; n = 114) to nonrecidivists (accrued no new charges over 12 month follow-up; n = 288) on (a) demographics (age, gender, race, and ethnicity), (b) self-reported lifetime substance use, (c) DSM–IV psychiatric diagnosis (internalizing and/or externalizing disorders) made at the time of evaluation, (d) legal history (e.g., prior status and criminal offenses), and (e) lifetime CSA. Bivariate analyses were also conducted to determine if group differences existed between evaluations that included a history of CSA (yes or no) and those that did not include this information. Results of the bivariate analyses and any additional variables known in the literature to contribute to risk of recidivism (e.g., substance use, externalizing disorders) were included in a multiple logistic regression model to determine prospective associations between juvenile demographics, legal and psychiatric factors, and 12-month recidivism. An interaction term comprised of gender and CSA was created and entered last into the logistic regression model step to test moderating hypotheses.
Results
Baseline Descriptive Data
Demographics
Of the 402 juveniles included in this study, the majority were male (240 males, 162 females) with an average age of 14.80 (SD 1.6) years. Most juveniles identified their race as White (60%) with the remainder identifying as African American (6%), Hispanic/Latino (18%), and Other (e.g., Asian Pacific Islander, Native American; 3%); 7% of juveniles were missing race and ethnicity data. Demographic data, split by gender, are presented in Table 1.
Table 1. Bivariate Relationships Between Study Variables and Gender.
| Total (n = 402) N (%) | Male (n = 240) N (%) | Female (n = 162) N (%)a | Unadjusted OR | 95% CI | p | |
|---|---|---|---|---|---|---|
| Baseline demographics | ||||||
| Age (15+) | 254 (60%) | 147 (61%) | 98 (60%) | .97 | .64–1.45 | .87 |
| Race (White) | 243 (60%) | 140 (58%) | 103 (62%) | .80 | .53–1.21 | .29 |
| Ethnicity (non-Latino) | 302 (75%) | 173 (72%) | 129 (79%) | .80 | .47–1.37 | .42 |
| Baseline psychiatric and substance use variables | ||||||
| Lifetime substance use | 244 (60%) | 146 (61%) | 98 (60%) | .98 | .65–1.48 | .94 |
| Prior offense | 118 (29%) | 74 (31%) | 44 (28%) | .83 | .53–1.30 | .42 |
| Externalizing disorder | 153 (38%) | 90 (38%) | 63 (39%) | .94 | .63–1.42 | .78 |
| Lifetime CSA | 37 (14%) | 12 (8%) | 25 (23%) | 3.52 | 1.68–7.37 | .01* |
| Primary outcome | ||||||
| 12-month recidivism | 114 (28%) | 77 (32%) | 37 (23%) | .67 | .39–.98 | .04* |
Note. OR = odds ratio; CI = confidence interval.
Females = referent group.
p ≤ .05.
Lifetime substance use
Sixty percent (n = 244) of juveniles reported some history of substance use (e.g., marijuana use, alcohol use, or other substance use). History of marijuana use was reported by 57% (n = 213) of juveniles; alcohol was reported by 52% (n = 182) and 15% (n = 42) of the sample reported history of other drug use (e.g., ecstasy, LSD, and cocaine). Males and females reported similar rates of marijuana use (60% of males and 54% of females), alcohol use (52% of males and 52% of females) and other drug use (15% of males and 17% of females), all ps > .05.
Legal history
Seventy-one percent (n = 288) were first-time offenders at the time of their court-ordered evaluation (see Table 1). Of the entire sample 18% (n = 71) of juveniles had a prior status offenses (range of 1–4 prior status offenses) and 11% (n = 43) of the sample had prior criminal offenses (range of 1–4 prior criminal offenses; offenders could have one petition filed with multiple charges or offenses). Girls had higher rates of status offenses (21% of females vs. 18% of males) but lower rates of past criminal offenses (12% of females vs. 17% of males). Bivariate analysis showed there were no differences between type of initial charge (i.e., status or criminal offense) on rates of recidivism.
Psychiatric disorders
Eighty-three percent (n = 337) of juveniles evaluated were given a primary Axis I diagnosis with the most common diagnoses being ODD (23%); mood disorders (15%); anxiety disorders (11%), and CD (10%). Approximately 68% (n = 249) of the total sample were diagnosed with externalizing disorders as their primary diagnosis resulting from the juvenile court clinic, which included a similar proportion of males and females. Additionally, 3% of the total samples were diagnosed with PTSD. Rates of PTSD diagnosis were higher in females; 4.3% (n = 8 of 162) of females were diagnosed with PTSD and 1.6% of males (n = 4 of 240). The majority of juveniles (61%) reported prior mental health treatment, 14% reported at least one prior psychiatric hospitalization and 37% reported a history of psychotropic medication.
History of CSA
Of the 404 evaluations, 66% (n = 263) included information about presence or absence of past CSA. Bivariate analyses comparing those evaluations that included history of sexual (n = 263) and those that did not (n = 141) revealed no between group differences on all study variable including gender, age, race, past offense history, history of substance use, and 12-month recidivism. In the evaluations that included this information, 14% (n = 37) of juveniles (or caregivers) reported that the juvenile had a CSA history. A higher proportion of girls and/or their caregivers reported a history of CSA (23% of girls vs. 8% of boys). Additionally, 75% (n = 263) reported experiencing any type of trauma (e.g., witness to violence, loss, and abuse). General trauma exposure was not found to be associated with recidivism in the full sample or separately for boys or girls. Of those juveniles diagnosed with PTSD (n = 11), 8 (6 out of 7 females; 2 out of 4 males) reported a history of CSA, 2 (1 female; 1 male) denied history of CSA. Additionally, 1 female evaluation (with PTSD diagnosis) was coded as missing lifetime history of CSA.
Longitudinal Outcome: Descriptive Data
Over the 12 month follow-up period, 28% of juveniles were classified as recidivists (n = 114). Males in the sample had higher rates of recidivism (32%) than girls (22%). The most common charges over time were larceny, breaking/entering, destruction of property (each representing on average approximately 25% of all crimes accrued) followed by vagrant or disorderly conduct (∼20% of all crimes accrued).
Longitudinal Outcome: Bivariate Analyses
Bivariate analyses were conducted between recidivists and non-recidivists on gender, age, race, lifetime substance use, externalizing disorder, prior offense, and history of CSA. Group comparisons are presented in Table 2. Recidivists did not differ from nonrecidivists on age and race/ethnicity or offense type (i.e., status vs. criminal offender). Recidivists were, however, more likely to have an externalizing disorder and prior status offense than non-recidivists. When examining separately within gender, male recidivists were more likely to report lifetime substance use and have a history of past offense than male nonrecidivists. Female recidivists reported higher rates of past CSA than female nonrecidivists.
Table 2. Differences Between Recidivist and Non-Recidivist, by Gender (N = 402).
| Males (n = 240) | Females (n = 162) | Tota1 sample (N = 402) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||
| Recidivist (n = 77)a N (%) |
Nonrecidivist (n = 163) N (%) |
Unadjusted OR |
95% CI | P | Recidivist (n = 37) N (%) |
Nonrecidivist (n = 125) N (%) |
Unadjusted OR |
95% CI | P | Recidivist (n = 114) N (%) |
Nonrecidivist (n = 288) N (%) |
Unadjusted OR |
95% CI | P | |
| Gender | — | — | — | — | — | — | 77 male (67%) | 163 male (57%) | .63 | .39–.98 | .04* | ||||
| Age (15+) | 59 (77%) | 88 (54%) | 2.11 | 1.2–4.65 | .01* | 16 (43%) | 82 (65%) | 1.3 | 8.4–2.10 | .21 | 75 (65%) | 39 (34%) | .97 | .57–1.18 | .08 |
| Race (White) | 48 (62%) | 92 (56%) | 1.27 | .73–2.22 | .38 | 23 (62%) | 48 (64%) | .61 | .43–1.97 | .83 | 71 (62%) | 172 (60%) | 1.11 | .71–1.74 | .63 |
| Lifetime Substance use | 39 (51%) | 107 (66%) | 1.86 | 1.07–3.23 | .03* | 25 (68%) | 73 (58%) | 1.48 | .64–3.22 | .31 | 64 (56%) | 180 (62%) | 1.30 | .83–2.02 | .24 |
| Externalizing disorder | 36 (47%) | 54 (33%) | 1.77 | 1.01–3.08 | .04* | 20 (54%) | 43 (34%) | 2.24 | 1.06–4.72 | .03* | 56 (50%) | 97 (33%) | 1.90 | 1.22–2.95 | .01* |
| Prior offense | 34 (44%) | 40 (24%) | 2.43 | 1.36–4.31 | .02* | 8 (22%) | 36 (29%) | 1.46 | .61–3.51 | .39 | 42 (37%) | 76 (27%) | 1.62 | 1.02–2.58 | .04* |
| Lifetime CSA | 3 (4%) | 9 (6%) | 1.48 | .38–5.74 | .56 | 10 (27%) | 15 (12%) | 2.62 | 1.01–6.86 | .05* | 13 (11%) | 24 (8%) | 1.37 | .65–2.85 | .40 |
Note. OR = odds ratio; CI = confidence interval.
Recidivist = referent group.
p ≤ .05.
Longitudinal Outcomes: Logistic Regression
The association between baseline variables and 12-month recidivism was tested through a multiple logistic regression model. We accounted for well-established predictors of recidivism including diagnosis of an externalizing disorder (Niarhos & Routh, 1992; Wierson & Forehand, 1995), race or ethnicity (Dembo et al., 1998; Wierson & Forehand, 1995), lifetime substance use (Dembo et al., 1991), and past offense history (Loeber & Dishion, 1983). Additionally, history of CSA was entered into the model to test the hypothesis that sexual abuse may impact future criminal behavior in young offenders, particularly owing to bivariate findings that differentiated female recidivists from nonrecidivists on this abuse variable. An interaction term between gender and CSA was included in the model to test gender-specific hypotheses about the role of CSA in predicting recidivism in offending girls, but not boys. Variables were entered into the model in two different steps as two distinct groups of variables: demographics (age, gender, race, and ethnicity); other associated variables (lifetime substance use, externalizing diagnosis, past offense, history of CSA, and gender by CSA interaction term). Table 3 reflects the unadjusted and adjusted odds ratios of these associations.
Table 3. Predictors of 12-Month Recidivism (N = 262).
| Variables | β | SE | Wald | Sig. | AORa | 95% CI |
|---|---|---|---|---|---|---|
| Age | .15 | .31 | .25 | .62 | 1.17 | .63–2.17 |
| Gender | 2.56 | 1.65 | 2.40 | .12 | .07 | .01–1.97 |
| Race | .01 | .30 | .01 | .98 | 1.01 | .54–1.82 |
| Lifetime substance use | .27 | .32 | .72 | .40 | .76 | .41–1.43 |
| Externalizing disorder | .72 | .28 | 6.46 | .01* | 2.06 | 1.18–3.54 |
| Past offense | .52 | .31 | 2.81 | .09 | .59 | .56–1.82 |
| Lifetime CSAb | 2.22 | 1.51 | 2.16 | .14 | .11 | .01–2.1 |
| Gender by CSA | 1.62 | 3.41 | 3.44 | .05* | 5.01 | 1.0–28.28 |
AOR = adjusted odds ratio.
CSA = childhood sexual abuse.
p ≤ .05.
The overall model fit the data well: Model χ2 = 16.81 (8), p = .03; 71% of the cases were correctly classified. Accounting for age, race, gender, past offense, and lifetime substance use, 12-month recidivism was significantly associated with being diagnosed with an externalizing disorder (AOR = 2.06; 95% CI = 1.18, 3.54; p < .01). Additionally, the interaction between gender and history of CSA was significantly associated with 12-month recidivism (AOR = 5.01; 95% CI = 1.0, 28.28; p = .05). There was not a statistically significant main effect of gender on recidivism; however, for males a history of sexual abuse did not differentiate rate of 12 month recidivism whereas for girls, those who had a history of sexual abuse had five times greater odds of recidivating than their nonabused female counterparts. No other variables in the model for were significant predictors of recidivism.
To further explore the significant interaction, post hoc probing was conducted as proposed by Holmbeck (2002). To examine the conditions of the moderator, the effects of gender (moderator) on the relationship between CSA (predictor) and recidivism (outcome) were tested. Results of the follow up analysis showed that CSA was a significant predictor for females (Wald = 3.88, p = .04) but not for males (Wald = .33, p = .57). Figure 1 illustrates regression lines for the association between CSA and recidivism moderated by gender.
Figure 1.
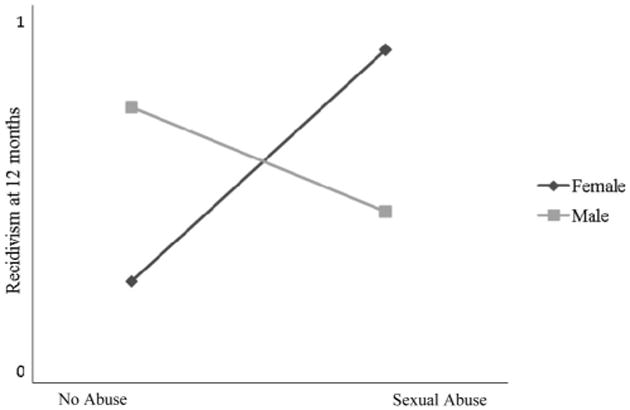
Interaction effect of gender by lifetime history of CSA on 12-month recidivism.
Discussion
This study is one of the first to measure self-reported rates of CSA and examine important gender differences in predictors of recidivism among a juvenile court clinic sample, of whom 91% were diagnosed with at least one DSM–IV psychiatric diagnosis. Published rates of sexual abuse among female juvenile offenders and delinquent youth vary greatly. Some published studies of justice system involved girls report high rates of abuse (e.g., 72%) (Zahn et al., 2010); however, others report lower rates, such as 25% of one detained sample of girls (Lederman, Dakof, Larrea, & Hua, 2004) and 56% of another adolescent female detained sample (Acoca, 1998). Thus, our study's CSA reporting rate of 23% was consistent with some other studies of adolescent female offenders. Additionally, our data demonstrate similar disparities in reporting of CSA by gender; girls reported almost four times the rate of lifetime CSA than boys in our sample (23% females vs. 8% males). Furthermore, even after accounting for known risk factors for recidivism (e.g., prior offense history), CSA remains a unique significant predictor of recidivism for young female, but not male, juvenile offenders with identified psychiatric concerns. Thus, our findings contribute to existing literature that suggests a history of CSA may uniquely contribute to girls' risk for legal involvement and that CSA may be a notable precedent for female criminal activity (Zahn et al., 2010).
While some meta-analyses have found no gender differences in symptoms related to abuse (Chen et al., 2010), other meta-analyses have found that gender differences in symptom expression do exist (Rind & Tromovitch, 1997). Thus, while previous findings are mixed, some earlier research supports that the notion that CSA history may impact girl's behaviors, thoughts and feelings in different ways than their male counterparts (Finkelhor, Hotaling, Lewis, & Smith, 1990; Tolin & Foa, 2008). For girls, CSA has been associated with a variety of negative outcomes, such as low self-esteem (Finkelhor & Browne, 1985; Grayston, 1992; Rhodes, Ebert, & Meyers, 1993), poor interpersonal functioning (Rhodes et al., 1993; Zahn et al., 2008), increased psychological distress (e.g., level of anger, anxiety, and depression) and externalizing behaviors (e.g., running away, promiscuous sexual behaviors) (Goodkind et al., 2006; Zahn et al., 2008). For boys, significant substance use, aggressive criminal behaviors and sexual risk taking (Chandy et al., 1996; Garnefski & Arends, 1998) are associated with a history of sexual (or other types) of abuse. Behaviors that are correlated with CSA history among girls (e.g., elopement, truancy, and aggressive or assaultive) are also those behaviors that typically result in their legal involvement (the majority being status offenses) (Zahn et al., 2008). Thus, relative to boys, there may be something distinct about girls' behavioral symptom expression of having a CSA history that increases their risk for legal involvement.
Girls may also have a different experience of CSA than boys that could impact their behavioral and psychiatric presentation. Girls are more likely to be chronically victimized, to be victim to more severe acts of sexual abuse and at an earlier age than boys (Ullman & Filipas, 2005); factors that are also associated with poorer psychiatric and behavioral (e.g., substance use) outcomes (Browne & Finkelhor, 1986). Traumatic experiences, and the subsequent symptom expression, could be contributing to an increase in behaviors that are associated with legal involvement for girls (e.g., aggression, truancy, and substance use) (Zahn et al., 2010). Thus, girls already involved in the justice system with CSA histories may be placed at greater risk for additional legal involvement by virtue of the behaviors associated with untreated trauma symptoms. In particular, delinquent girls with a trauma (including sexual abuse) history are at increased risk for developing depression relative to their male delinquent counterparts (Adams et al., 2012), which could perhaps be attributed to some of these aforementioned abuse characteristics that differ by gender. Because of the nature of the chart review approach in our study, data on these specific abuse factors were unavailable for study; however, future a priori studies should consider measuring these factors when exploring gender-specific pathways to juvenile recidivism.
Studies that measure general trauma exposure (that may include sexual abuse) have mixed findings with respect to gender differences in rates of PTSD development and differential psychiatric effects of trauma on delinquent or offending young females versus males. In our CINI sample, rates of any trauma exposure were similar to high rates found among juvenile detainees (e.g., Abram et al., 2004) and likewise, rates specifically of sexual abuse or trauma were significantly higher in females versus males (Abram et al., 2004). Despite that 75% of our sample reported any trauma exposure, rates of PTSD in our study were low and much lower than PTSD incidence (15% girls; 11% boys) reported in the Abram et al. (2004) juvenile detainee study. However, a more recent study with nondetained delinquent youth found, similar to our own study, that rates of PTSD (and sexual assault) are significantly greater among female versus male delinquent youth (Adams et al., 2012). Some data suggest that delinquent girls may be differentially affected by their trauma history (perhaps depending on type of trauma), which may lead to gender differences in pathways to the development of PTSD and/or pathways to other life consequences, such as repeat offending and chronic substance use (Abram et al., 2007). We did not examine PTSD as a predictor of recidivism because rates of diagnosis were low and studies have demonstrated that psychiatric diagnosis alone is not a significant predictor of juvenile recidivism; rather it's the cooccurrence of other disorders or risk behaviors, particularly substance use, that significantly increases the likelihood of recommitting an offense (Goodkind et al., 2006; Tolou-Shams, et al., in press). Further research is warranted to understand more about the specific impact of trauma history (including CSA) on young female offenders' psychiatric (e.g., development of PTSD, depression), behavioral (e.g., conduct problems) and health (e.g., substance use) outcomes and the impact of the complex interaction of these factors on juvenile recidivism.
Limitations
This study has several limitations that are worth noting. First these data were derived from forensic clinical evaluations and interviews with juveniles and their caregivers. While these can provide a rich source of data, coders are only able to rate information that is included in the written report. Thus, there may be omissions in information related to self-report variables including history of substance use and history of CSA. Court-involved families may have been hesitant to reveal sensitive information in court-ordered evaluations and thus the endorsement of abuse histories (for males and females), may have been underreported by juveniles and/or their caregivers. However, it is notable that even within the interview format, significant numbers of juveniles reported substance use and sexual abuse histories.
An additional limit to this study is the dichotomous nature of the CSA variable. Studies have shown that it is not just the experience of CSA but the frequency and intensity of the abuse that may impact behavior in adolescents. This study did not have continuous data available for analyses. Furthermore, many of the clinicians did not include information about the absence or presence of a CSA history in the report. Bivariate analyses indicated no group differences on variables of interest; however, having this information from all evaluations may have enhanced study findings.
Finally, this study represents a specific subset of young offenders. Only those referred for mental health evaluations were included in this study and thus findings may not be generalizable to the larger juvenile justice population. However, it might be expected that examining the impact of CSA in this mental health population may be of particular relevance because of the cooccurrence of psychiatric difficulties and CSA history.
Implications and Future Directions
This study provides preliminary data related to gender differences in recidivism risk for court-involved nonincarcerated youth with identified mental health concerns. Adolescents who continue to commit crimes once involved in the justice system are at increased risk for a variety of negative outcomes including repeat incarceration, involvement in the adult criminal justice system, substance use, high risk sexual behavior, and poor academic achievement. Thus, understanding the risk factors associated with recidivism is an important step in identifying youth who may be in need of additional support or specific intervention to reduce the risk of continued system involvement. While most Risk-Need-Responsivity (RNR) Assessments, aimed at reducing further delinquency, are for use with both genders and they do not include abuse history as a factor for possible intervention point for risk reduction. Future studies may wish to explore CSA as a risk factor for future recidivism and consider incorporating this variable into risk assessment tools; future research could also examine whether this should be a static or dynamic risk factor, which was beyond the scope of our study but could be of great relevance to the field.
Empirically supported and effective trauma interventions for children and adolescents (e.g., TF-CBT [Cohen & Mannarino, 2004]; EMDR [Adler–Tapia & Settle, 2009], PE-A [Gilboa–Schechtman et al., 2010]) do exist but few are specifically designed to meet the needs of adolescent girls. Furthermore, to our knowledge these interventions have not been tested with girls a juvenile justice setting. Despite that several recent calls for gender-specific programming within juvenile justice systems have been issued, there are few trauma-informed interventions specifically developed for juvenile justice girls (e.g., see VOICES [Covington, 2004] for one exception) and we are not aware of any empirically supported evidence-based interventions to reduce recidivism that specifically address trauma among juvenile justice girls. Thus, our data add to the growing body of literature that suggests that gender-responsive supports and interventions may be warranted.
This study represents an initial, but important, exploration of the association between recidivism and CSA. Future studies may wish to explore types of abuse (e.g., physical, emotional, and witness to violence) and frequency and intensity of abuse on risk for recidivism. Additionally, studies focused on larger and more general samples of court involved nonincarcerated youth could provide additional information, particularly with respect to the development of PTSD and it is association with recidivism. While male juvenile offenders may need additional intervention surrounding criminal attitudes and impulsive behavior, young female offenders with an identified history of CSA may need trauma-informed treatment and support to deter continued criminal behavior.
Acknowledgments
Research supported by NIDA K23 DA051232, NIMH K23 MH 086328, NIDA T32 DA013911, and by the Lifespan/Brown/Tufts Center for AIDS Research (P30 AI042853).
Contributor Information
Selby M. Conrad, The Miriam Hospital, Providence, Rhode Island and Bradley Hasbro Children's Research Center, Providence, Rhode Island
Nicole Placella, Rhode Island Hospital, Providence, Rhode Island.
Marina Tolou-Shams, Bradley Hasbro Children's Research Center, Providence, Rhode Island and The Warren Alpert Medical School of Brown University.
Christie J. Rizzo, Bradley Hasbro Children's Research Center, Providence, Rhode Island and The Warren Alpert Medical School of Brown University
Larry K. Brown, Bradley Hasbro Children's Research Center, Providence, Rhode Island and The Warren Alpert Medical School of Brown University
References
- Abram KM, Teplin LA, Charles DR, Longworth SL, McClelland GM, Dulcan MK. Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry. 2004;61:403–410. doi: 10.1001/archpsyc.61.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abram KM, Washburn JJ, Teplin LA, Emanuel KM, Romero EG, McClelland GM. Posttraumatic stress disorder and psychiatric comorbidity among detained youths. Psychiatric Services. 2007;58:1311–1316. doi: 10.1176/appi.ps.58.10.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acoca L. Outside/inside: The violation of American girls at home, on the streets and in the juvenile justice system. Crime & Delinquency. 1998;44:561–589. doi: 10.1177/0011128798044004006. [DOI] [Google Scholar]
- Adams Z, McCart M, Zajac K, Danielson K, Sawyer G, Saunders B, Kilpatrick D. Psychiatric problems and trauma exposure in nondetained delinquent and nondelinquent adolescents. Journal of Child & Adolescent Psychology. 2012;42:323–331. doi: 10.1080/15374416.2012.749786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler–Tapia R, Settle C. Evidence of the efficacy of EMDR with children and adolescents in individual psychotherapy: A review of the research published in peer-reviewed journals. Journal of EMDR Practice and Research. 2009;3:232–247. doi: 10.1891/1933-3196.3.4.232. [DOI] [Google Scholar]
- Browne A, Finkelhor D. Impact of child sexual abuse: A review of the research. Psychological Bulletin. 1986;99:66–77. doi: 10.1037/0033-2909.99.1.66. [DOI] [PubMed] [Google Scholar]
- Chandy JM, Blum R, Resnick M. Gender-specific outcomes for sexually abused adolescents. Child Abuse & Neglect. 1996;20:1219–1231. doi: 10.1016/S0145-2134(96)00117-2. [DOI] [PubMed] [Google Scholar]
- Chen LP, Hassan Mural M, Para's M, Colenso K, Sattler A, Grandson N, et al. Zirakzadeh A. Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clinic Proceedings. 2010;85:618–629. doi: 10.4065/mcp.2009.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesney–Lind M. The female offender: Girls, women and crime. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- Cohen JA, Mannarino A. Treatment of childhood traumatic grief. Journal of Clinical Child and Adolescent Psychology. 2004;33:819–831. doi: 10.1207/s15374424jccp3304_17. [DOI] [PubMed] [Google Scholar]
- Covington S. Voices: A program of self-discovery and empowerment for girls. Carson City, NV: The Change Companies; 2004. [Google Scholar]
- Daly K. Women's pathways to felony court: Feminist theories of lawbreaking and problems of representation. Review of Law and Women's Studies. 1992;2:11–52. [Google Scholar]
- De La Rosa M, Dillion F, Rojas P, Schwartz S, Duan R. Latina mother-daughter dyads: Relations between attachment and sexual behavior under the influence of alcohol or drugs. Archives of Sexual Behavior. 2010;39:1305–1319. doi: 10.1007/s10508-009-9498-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Schmeidler J, Nini–Gough B, Sue C, Borden B, Manning D. Predictors of recidivism to a juvenile assessment center: A three year study. Journal of Child & Adolescent Substance Abuse. 1998;7:57–77. doi: 10.1300/J029v07n03_03. [DOI] [Google Scholar]
- Dembo R, Williams L, Getreu A, Genung L, Schmeidler J, Berry E, et al. La Voie L. Recidivism among high-risk youths: Study of a cohort of juvenile detainees. Substance Use and Misuse. 1991;26:121–177. doi: 10.3109/10826089109053178. [DOI] [PubMed] [Google Scholar]
- Dembo R, Williams L, Schmeidler J. Gender difference in mental health service needs among youths entering a juvenile detention center. Journal of Prison and Jail Health. 1993;12:73–101. [Google Scholar]
- Feiring C, Taska L, Lewis M. Age and gender differences in children's and adolescents” adaptation to sexual abuse. Child Abuse & Neglect. 1999;23:115–128. doi: 10.1016/S0145-2134(98)00116-1. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Browne A. The traumatic impact of child sexual abuse: A conceptualization. American Journal of Orthopsychiatry. 1985;55:530–541. doi: 10.1111/j.1939-0025.1985.tb02703.x. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Hotaling G, Lewis I, Smith C. Sexual abuse in a national survey of adult men and women: Prevalence characteristics and risk factors. Child Abuse & Neglect. 1990;14:19–28. doi: 10.1016/0145-2134(90)90077-7. [DOI] [PubMed] [Google Scholar]
- Gadow K, Sprafkin J. Youth's inventory 4 manual. Stony Brook, NY: Checkmate Plus, Ltd; 1994. [Google Scholar]
- Gadow K, Sprafkin J, Weiss M. Adult self-report inventory-4 manual. Stony Brook, NY: Checkmate Plus Ltd; 2004. [Google Scholar]
- Garnefski N, Arends E. Sexual abuse and adolescent maladjustment: Differences between male and female. Journal of Adolescent. 1998;21:99–107. doi: 10.1006/jado.1997.0132. [DOI] [PubMed] [Google Scholar]
- Gavazzi S, Yarcheck C, Chesney–Lind M. Global risk indicators and the role of gender in juvenile detention samples. Criminal Justice and Behavior. 2006;33:597–612. doi: 10.1177/0093854806288184. [DOI] [Google Scholar]
- Gilboa–Schechtman E, Foa E, Shafran N, Aderka I, Powers M, Rachamin L, et al. Apter A. Prolonged exposure versus dynamic therapy for adolescent PTSD: A pilot randomized control trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:1034–1042. doi: 10.1016/j.jaac.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodkind S, Ng I, Sarri R. The impact of sexual abuse in the lives of young women involved or at risk of involvement with the juvenile justice system. Violence Against Women. 2006;12:456–477. doi: 10.1177/1077801206288142. [DOI] [PubMed] [Google Scholar]
- Grayston AD. Self-esteem, anxiety and loneliness in preadolescent girls who have experienced sexual abuse. Child Psychiatry and Human Development. 1992;22:277–286. doi: 10.1007/BF00707669. [DOI] [PubMed] [Google Scholar]
- Grisso T, Quinlan J. Juvenile court clinical services: A national description. Juvenile and Family Court Journal. 2005;56:9–20. doi: 10.1111/j.1755-6988.2005.tb00175.x. [DOI] [Google Scholar]
- Guthrie B, Flinchbaugh L. Gender-specific substance prevention programming: Going beyond just focusing on girls. The Journal of Early Adolescence. 2001;21:354–372. doi: 10.1177/0272431601021003005. [DOI] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Holsinger K, Belknap J, Sutherland J. Assessing the gender specific program and service needs for adolescent females in the juvenile justice system. Columbus, OH: Office of Criminal Justice Services; 1999. [Google Scholar]
- Hubbard D, Pratt T. A meta-analysis of the predictors of delinquency among girls. Journal of Offender Rehabilitation. 2002;34:1–13. doi: 10.1300/J076v34n03_01. [DOI] [Google Scholar]
- Khoury E. Are girls different? A development perspective on gender differences in risk factors for substance use among adolescents. In: Vega W, Gil A, editors. Drug use and ethnicity in early adolescence. New York, NY: Plenum Press; 1998. pp. 97–123. [Google Scholar]
- Lederman CS, Dakof G, Larrea M, Hua L. Characteristics of adolescent females in juvenile detention. International Journal of Law and Psychiatry. 2004;27:321–337. doi: 10.1016/j.ijlp.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Loeber R, Dishion T. Early predictors of male delinquency: A review. Psychological Bulletin. 1983;94:68–99. doi: 10.1037/0033-2909.94.1.68. [DOI] [PubMed] [Google Scholar]
- Lopez V, Kopak A, Robillard A, Gillmore M, Holliday R, Braithwaite R. Pathways to sexual risk taking among female adolescent detainees. Journal of Youth and Adolescence. 2011;40:945–957. doi: 10.1007/s10964-010-9623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe KM, Lansing A, Garland A, Hough R. Gender differences in psychopathology, functional impairment, and familial risk factors among adjudicated delinquents. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:860–867. doi: 10.1097/00004583-200207000-00020. [DOI] [PubMed] [Google Scholar]
- Nelson D. Road map to juvenile justice reform. Baltimore, MD: Annie E. Casey Foundation; 2008. [Google Scholar]
- Niarhos F, Routh D. The role of clinical assessment in the juvenile court: Predictors of juvenile dispositions and recidivism. Journal of Clinical Child Psychology. 1992;21:151–159. doi: 10.1207/s15374424jccp2102_7. [DOI] [Google Scholar]
- Odgers C, Moretti M, Reppucci N. A review of findings from the “gender and aggression project” informing juvenile justice policy and practice through gender-sensitive research. Court Review. 2010;46:5–8. [Google Scholar]
- Owen B, Bloom B. Profiling women prisoners: Findings from national survey and California sample. Prison Journal. 1995;75:165–185. doi: 10.1177/0032855595075002003. [DOI] [Google Scholar]
- Paolucci EO, Genuis M, Violato C. A meta-analysis of the published research on the effects of child sexual abuse. The Journal of Psychology: Interdisciplinary and Applied. 2001;135:17–36. doi: 10.1080/00223980109603677. [DOI] [PubMed] [Google Scholar]
- Pardini DA, Fite P. Symptoms of conduct disorder, oppositional defiant disorder, attention-deficit/hyperactivity disorder, and callous-unemotional traits as unique predictors of psychosocial maladjustment in boys: Advancing an evidence base for DSM-V. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:1134–1144. doi: 10.1016/j.jaac.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puzzanchera C. Juvenile Justice Bulletin. Juvenile Arrests 2008. 2009 Retrieved from https://http://www.ncjrs.gov/pdffiles1/ojjdp/228479.pdf.
- Puzzanchera C, Adams B, Hockenberry S. Juvenile Court Statistics 2009. Pittsburgh, PA: National Center for Juvenile Justice; 2012. [Google Scholar]
- Reid J, Patterson G, Dishion T. Antisocial boys. Portland, OR: Castalia; 1997. [Google Scholar]
- Reisig M, Holtfreter K, Morash M. Assessing recidivism risk across female pathways to crime. Justice Quarterly. 2006;23:384–405. doi: 10.1080/07418820600869152. [DOI] [Google Scholar]
- Rhodes JE, Ebert L, Meyers A. Sexual victimization in young, pregnant and parenting African-American women: Psychological and social outcomes. Violence and Victims. 1993;8:153–163. [PubMed] [Google Scholar]
- Rind B, Tromovitch P. A meta-analytic review of findings from national samples on psychological correlates of child sexual abuse. Journal of Sex Research. 1997;34:237–255. doi: 10.1080/00224499709551891. [DOI] [Google Scholar]
- Salekin RT, Rogers R, Ustad K, Sewell K. Psychopathy and recidivism among female inmates. Law and Human Behavior. 1998;22:109–128. doi: 10.1023/A:1025780806538. [DOI] [PubMed] [Google Scholar]
- Schubert CA, Mulvey EP, Glasheen C. Influence of mental health and substance use problems and criminogenic risk on outcomes in serious juvenile offenders. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:925–937. doi: 10.1016/j.jaac.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Swanston H, Parkinson P, O'Tool B, Plunkett A, Shrimpton S, Oates R. Juvenile crime, aggression and delinquency after sexual abuse: A longitudinal study. British Journal of Criminology. 2003;43:729–749. doi: 10.1093/bjc/43.4.729. [DOI] [Google Scholar]
- Tebbutt J, Swanson H, Oates R, O'Tool B. Five years after child sexual abuse: Persisting dysfunction and problems of prediction. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:330–339. doi: 10.1097/00004583-199703000-00011. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Abram K, McClelland G, Dulcan M, Mericle A. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2002;59:1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Mericle A, McClelland G, Abram K. HIV and AIDS risk behaviors in juvenile detainees: Implications for public health policy. American Journal of Public Health. 2003;93:906–912. doi: 10.2105/AJPH.93.6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin L, Welty D, Abram K, Dulcan M, Washburn J. Prevalence and persistence of psychiatric disorders in youth after detention: A prospective longitudinal study. Journal of the American Medical Association Psychiatry. 2012;69:1031–1043. doi: 10.1001/archgenpsychiatry.2011.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin D, Foa E. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Trauma: Theory, Research, Practice, and Policy, S. 2008:37–85. doi: 10.1037/1942-9681.S.1.37. [DOI] [PubMed] [Google Scholar]
- Tolou-Shams M, Rizzo CJ, Conrad SM, Johnson S, Oliveria C, Brown LK. Predictors of recidivism and detention among juveniles referred for a court clinic forensic evaluation. Journal of the American Academy of Psychiatry and Law. in press. [PMC free article] [PubMed] [Google Scholar]
- Ullman S, Filipas H. Gender differences in social reactions to abuse disclosure, post-abuse coping and PTSD of child sexual abuse survivors. Child Abuse & Neglect. 2005;29:767–782. doi: 10.1016/j.chiabu.2005.01.005. doi:10.1016/j.chiabu .2005.01.005. [DOI] [PubMed] [Google Scholar]
- Vermeiren R, Jespers I, Moffitt T. Mental health problems in juvenile justice populations. Child and Adolescent Psychiatric Clinics of North America. 2006;15:333–351. doi: 10.1016/j.chc.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Wasserman G, McReynolds L, Fisher P, Lucas C. Mental Health Screening and Assessment in Juvenile Justice. New York, NY: Guilford Press; 2005. Diagnostic interview schedule for children: Present state voice version; pp. 224–239. [Google Scholar]
- Widom C. Victims of childhood sexual abuse: Later criminal consequences. Washington, DC: National Institute of Justice; 1995. [DOI] [Google Scholar]
- Widom CP, Ames M. Criminal consequences of childhood sexual victimization. Child Abuse & Neglect. 1994;18:303–318. doi: 10.1016/0145-2134(94)90033-7. [DOI] [PubMed] [Google Scholar]
- Widom C, Maxfield M. An update on the “cycle of violence”. Washington, DC: Department of Justice, Office of Justice Programs; 2001. [Google Scholar]
- Wierson M, Forehand R. Predicting recidivism in juvenile delinquents: The role of mental health diagnosis and qualifications of conclusions by race. Behaviour Research and Therapy. 1995;33:63–67. doi: 10.1016/0005-7967(94)E0001-Y. [DOI] [PubMed] [Google Scholar]
- Zahn M, Agnew R, Fishbein D, Miller S, Winn D, Dakoff G, et al. Chesney–Lind M. Causes and correlates of girls' delinquency. In: Slowikowski J, editor. Girls study group: Understanding and responding to girls' delinquency. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 2010. pp. 1–20. [Google Scholar]
- Zahn M, Hawkins S, Chiancone J, Whiteworth A. The girls study group-Charting the way to delinquency prevention for girls. In: Robert Flores J, editor. Girls study group: Understanding and responding to girls' delinquency. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 2008. pp. 1–8. [Google Scholar]
- Zavlek S, Maniglia R. Developing correctional facilities for female juvenile offenders: Design and programmatic considerations. Corrections Today. 2007;69:58–63. [Google Scholar]


