Abstract
While a growing body of research suggests that religion offers mental health benefits for individuals with schizophrenia, few studies have examined the mechanisms underlying this effect. The present study investigated two potential mediators (seeking social support and meaning-making coping) that may elucidate the nature of this relationship. The sample included 112 individuals with schizophrenia or schizoaffective disorder. Structural equation modeling was used to test whether religion was related to symptom severity and quality of life (QoL), and whether seeking social support and meaning-making coping mediated these effects. As expected, meaning-making coping significantly mediated the effect of intrinsic religion (use of religion as a framework to understand life) on QoL. While extrinsic religion (use of religion as a social convention) was associated with seeking social support, it did not relate to either outcome variable. Findings offer insight into the ways in which religion may improve the mental health of patients with schizophrenia. Results suggest that the adaptive elements of intrinsic religion seen in prior research may be explained by the meaning that religion offers. Clinical interventions that encourage patients to find meaning amidst adversity may improve QoL in this population. Future research would benefit from further investigation of the meaning-making process in individuals with schizophrenia.
Keywords: Quality of Life, Symptom Severity, Meaning-Making, Social Support, Religion
Introduction
The increased availability of psychotropic medications and psychosocial interventions for schizophrenia has greatly facilitated symptom management for individuals with the illness. With these advances, researchers and clinicians are now thinking beyond mere symptom alleviation and aspiring toward more global improvements that target overall quality of life (QoL) (1). Religion is one variable that may improve QoL, as it has been linked to greater mental and physical health (2). In individual studies and comprehensive review papers, religion has been associated with delayed onset of physical conditions (e.g., coronary heart disease and hypertension), improved course and outcome of illness (e.g., reduced mortality after heart transplant and in breast cancer patients and higher quality of life in physically ill patients), and lower mortality rates (for review, see 2, 3). Relationships between religion and mental health are similarly robust and demonstrate reduced rates of anxiety, depression, and substance dependence among religious individuals (2-5). Longitudinal studies of patients with depression have shown that religious individuals are more likely to recover and do so more quickly than those who report little to no religious involvement (for review, see 2, 3). Among patients with schizophrenia, religious involvement has been related to greater symptomatic remission and psychological well-being (6-8).
The literature on religion in non-psychiatric populations differentiates between intrinsic and extrinsic religious orientations. Intrinsic religion has been described as “a meaning-endowing framework in which all of life is understood” (9). This orientation has been related to greater mental health (10) and has predicted faster remission from depression among medical patients (11). By contrast, early research on extrinsic religion (religion as a “social comfort and social convention”) (9) conceptualized this orientation as a self-serving defense or escape mechanism. Although some research indicates that people with an extrinsic religious orientation are closed-minded, prejudiced, and dogmatic (9), extrinsic religious orientations may also offer benefits for coping with adversity. In one study, extrinsic religion was associated with greater general and religious outcomes among people coping with adverse events. In addition, seeking social support through religion was associated with positive self-reports of how well participants handled the event and their emotions, how they felt about themselves after the event, and how much they learned from the event (12).
Interestingly, most studies of religion in serious mental illness (SMI) do not differentiate between intrinsic and extrinsic religion even though patients do distinguish between these orientations. In a qualitative study, patients with SMI defined “religion” by its extrinsic characteristics (e.g., church attendance, involvement with religious rituals), while they defined “spirituality” by its intrinsic qualities (i.e., as an internally driven experience) (13). In addition, much prior research on religion's role in SMI has focused on the adverse influences of religion in this population. Religious activity prior to hospitalization has predicted religious delusions during hospitalization (14), and religious delusions have been related to greater symptom severity and lower levels of functioning among hospitalized schizophrenia patients (15). In another study, patients with religious delusions displayed more psychotic symptoms, but there was no difference in religious affiliation or centrality between patients with and without positive symptoms with religious content (16). In a recent review of the literature on religion in SMI, the authors concluded that while religious delusions may be a poor prognostic indicator, the evidence to date generally suggests that there are adaptive components of religion that offer clinical benefits for patients (8).
Given the status of research on religion and mental health, researchers have begun identifying variables that may help explain the mechanisms underlying this relationship. Two proposed mechanisms include the social support and sense of meaning that religion cultivates (5, 17, 18). It is important to note that meaning-making and social support are not unique to religion. In fact, we chose to examine these potential mechanisms because they are common goals of both religion and more traditional psychotherapeutic approaches, including humanistic, existential and cognitive-behavioral approaches in which patients are encouraged to engage socially and examine the meaning ascribed to personal beliefs. Among schizophrenia patients, greater social support has been related to less severe positive symptoms and fewer psychiatric hospitalizations over the course of three years (19). Social support has also been associated with QoL among individuals with schizophrenia, even after controlling for symptom severity (1).
Research has also linked religion and meaning-making. Huguelet and colleagues found that two-thirds of their sample of patients with schizophrenia reported that religion provided meaning to their illness (20). Meaning-making is also associated with greater psychological well-being (21). Only one prior study has evaluated the relationships among religion, meaning, and mental health in schizophrenia (22). Results indicated that beliefs that mental illness can provide an opportunity for spiritual growth were associated with greater psychological growth and well-being. By contrast, beliefs that mental illness is a punishment from God were correlated with lower levels of psychological well-being and higher levels of personal loss and psychological distress (22).
The literature reviewed above suggests that religion, meaning-making and social support are positively associated with mental health. There also appears to be a positive association between intrinsic religion and meaning-making (10) and between extrinsic religion and social support (12). Therefore, meaning-making and social support coping may be mediating variables that account for some of the variance in well-being that is generally attributed to religion. In fact, life meaning has mediated the relationship between intrinsic religion and life satisfaction in an “at risk” community sample of unemployed mothers (23). Similarly, meaning-making coping mediated the association between intrinsic religion and subjective well-being among bereaved participants (18). In both studies, initial relationships between intrinsic religion and well-being were positive, but small (effect sizes were 0.18 and 0.17, respectively), which is consistent with prior research. A meta-analysis of 28 studies found that effect sizes for associations between religion and well-being ranged from -.01 to 0.58 (95% confidence interval=0.14 to 0.25) (24).
The present study examined relationships among religion, potential mediators, QoL and symptom severity in an outpatient sample of patients with schizophrenia. Based on prior research in non-psychiatric populations, we hypothesized that meaning-making coping would mediate the relationship between intrinsic religion and mental health (18, 23). We also hypothesized that seeking social support would mediate the relationship between extrinsic religion and outcome variables (QoL and symptom severity) (12). Finally, several exploratory analyses were conducted to examine associations among religion, mediators, and specific psychiatric symptom clusters.
Methods
Participants
This study was part of a larger project examining how psychosocial factors relate to coping with schizophrenia. Participants were recruited for our “Schizophrenia Study” through local hospitals and clinics and advertisements on public transportation and in free local magazines. No mention of religion was made in the ads. The following wording was used to recruit participants:
Have you or one of your relatives been diagnosed with schizophrenia or schizoaffective disorder? If so, you may be eligible to participate in a research study. During the study you will take part in an interview (regarding symptoms, how you cope with the illness and cultural information) and, if interested, you may also be eligible for a free family therapy for schizophrenia/schizoaffective disorder. Interviews/therapy are available in English and Spanish. You will be compensated $25 for your interview time.
Following the initial assessment, eligible and interested participants were invited to participate in a free family therapy study, which is why relatives were also recruited, but their data were not included in the present investigation.
Participants included 112 patients (81 male), mean age M (SD)=39.53 (12.51) years, 13.5% Caucasian, 36.9% African American, 45.9% Hispanic and 3.6% “Other.” To assess DSM-IV symptom criteria, the Psychotic Symptoms Module (B) of the Structured Clinical Interview for the DSM-IV (SCID) was used (25). Interviewers were first trained on SCID criteria using practice tapes. After training, all interviewers—including the study's Principal Investigator (PI)— watched six videotaped interviews from the current study and independently determined an overall diagnosis. Interviewers were in complete consensus regarding the presence or absence of diagnosis (κ=1.0). Only patients who met lifetime symptom criteria for schizophrenia or schizoaffective disorder were included. We did not use the Psychotic Differential Module (C) to distinguish between schizophrenia and schizoaffective disorder or between schizophrenia subtypes. Individuals who met criteria for Psychotic Mood Disorders were excluded from the present investigation.
Procedures
The study was approved by the University of Miami Internal Review Board. Prior to participation, participants were given a detailed description of study protocol and provided informed consent. To address variations in reading ability, all measures were administered in interview format by trained undergraduate and graduate research assistants. Participants chose to complete the interview in English or Spanish. Measures were translated to Spanish using the editorial board approach, which is considered to be more effective than the translation-back-translation approach because it takes into account within-group language variations that can pose problems with translation (26).
Measures
Symptom Severity
Current psychiatric symptom severity (based on the past three months) was assessed via the 24-item Brief Psychiatric Rating Scale (BPRS) (27). Symptom severity was rated on a scale from 1 (not present) to 7 (extremely severe). Total scores were obtained by averaging ratings across all items. The BPRS was also broken down into four symptom clusters that have demonstrated stability across schizophrenia patients with a wide range of chronicity and severity of psychiatric symptoms (positive symptoms=unusual thought content, suspiciousness, bizarre behavior, grandiosity, hallucinations, disorientation and conceptual disorganization; negative symptoms=blunted affect, motor retardation, and emotional withdrawal; agitation/mania=uncooperativeness, tension, excitement, distractibility, motor hyperactivity, and mannerisms and posturing; depression/anxiety=anxiety, depression, suicidality, and guilt) (28).
All interviewers were trained in BPRS coding by the PI. Interviewers coded practice tapes until they achieved high inter-rater reliability with the trainer. All interviewers then watched six videotaped BPRS training interviews developed by Joseph Ventura at UCLA. Inter-rater reliability between study interviewers and Dr. Ventura's consensus ratings was acceptable: κ=0.85–0.98 (total symptoms), κ=0.86–0.97 (positive symptoms), κ=0.47–0.88 (negative symptoms), κ=0.65–0.91 (agitation/mania) and κ=0.89–0.96 (depression/anxiety). The symptom clusters also demonstrated good internal reliability: α=0.73 (total symptoms), α=0.62 (positive symptoms), α=0.78 (negative symptoms), α=0.63 (agitation/mania) and α=0.76 (depression/anxiety).
Finally, the BPRS provided eligibility information for the present study. Patients who received a score of 5 (moderately severe) or higher on item 14, which assesses disorientation, were excluded due to inadequate cognitive capacity. In addition, if a patient received a score of 6 (severe) or higher on any of the four BPRS psychosis items (suspiciousness, hallucinations, conceptual disorganization and unusual thought content), the patient was considered too psychiatrically unstable to participate in the remainder of the interview. In other words, participants were excluded when symptoms were interfering with their ability to provide accurate responses on self-report measures. Including these participants would have diminished the reliability and validity of assessment tools, which have not been normed on floridly psychotic patients. In these cases, the interview was terminated prematurely and the patient was given appropriate referrals. The mean BPRS score in the current study was 2.34 (SD=0.55), indicating participants were experiencing very mild to mild symptoms at the time of evaluation.
Religion
Religion was measured by the Religious Orientation Scale-Revised (29). Items are measured on a 1 (I strongly disagree) to 5 (I strongly agree) scale. Examples of items from the intrinsic (eight items) and extrinsic subscale (six items) include: “My whole approach to life is based on my religion” and “I go to church because it helps me make friends.” Subscale scores were calculated by averaging responses across items in each scale. In the present study, Cronbach's alphas were 0.67 (intrinsic) and 0.80 (extrinsic).
Meaning-Making Coping
Following Park (18), meaning-making coping was assessed via the 4-item positive reinterpretation and growth subscale of the COPE (30). As suggested by the authors, COPE instructions were tailored to make them more relevant to the current sample. An example of an item from this scale is “I am trying to grow as a person as a result of the experience.” Items were scored on a 1 (I haven't been doing this at all) to 4 (I've been doing this a lot) scale. Total scores were calculated by averaging responses across items. Cronbach's alpha for the present study was 0.80.
Seeking Social Support
The extent to which individuals cope by seeking out social support was examined via two subscales of the COPE (30). Seeking social support for instrumental reasons involves seeking advice and assistance from others, and seeking social support for emotional reasons involves seeking moral support and sympathy from others. Each subscale is composed of four items on a 1 (I haven't been doing this at all) to 4 (I've been doing this a lot) scale. Examples of items from the instrumental and emotional subscales include: “I try to get advice from someone about what to do” and “I talk to someone about how I feel.” Total scores for each subscale were calculated by averaging responses across items. In the present study, Cronbach's alphas were 0.71 (instrumental) and 0.80 (emotional).
Quality of Life
QoL was measured by the 22-item Quality of Life Inventory, which asks respondents to rate their perceived importance and satisfaction with certain life domains (i.e., health, self-esteem, love) (31). An example of an item on this scale is “HEALTH is being physically fit, not sick, and without pain or disability. How important is HEALTH to your happiness? How satisfied are you with your HEALTH?” Importance items are rated from 0 (not important) to 2 (extremely important). Satisfaction items are rated from 0 (very dissatisfied) to 5 (very satisfied). Total scores were obtained by multiplying the importance and satisfaction rating for each domain and then averaging ratings across all eleven domains. In the current study, Cronbach's alpha was 0.88.
Medication Adherence
Adherence to psychiatric medications was measured using the Medication Adherence Rating Scale (MARS) (32). The full 10-item scale consists of three factors which assess medication adherence behavior (factor 1), attitudes toward taking medication (factor 2), and negative side effects/attitudes to psychotropic medication (factor 3). Only factor 1 scores were used in the present study because this factor has been shown to be a better indicator of adherence behavior than the total MARS scale (33), and we were interested in measuring medication adherence behavior rather than attitudes about medication or its side effects. An example of an item on factor 1 is “Do you ever forget to take your medication?” Total scores were calculated by averaging responses across items. Cronbach's alpha for factor 1 of the MARS was 0.71 in the present study.
Drug Abuse
The 20-item Drug Abuse Scale (34) was used to measure current drug abuse (over the past three months). Total scores were calculated by averaging responses across items. Cronbach's alpha for the current study was 0.94.
Education
Participants indicated how much formal education they have received on a scale from one to seven (1=advanced degree, 2=college degree, 3=some college, 4=high school graduate, 5=some high school beyond grade eight, 6=grade eight completed, 7=below grade eight). Responses were reverse-coded so that higher scores corresponded to a higher level of education.
Illness Duration
Participants were asked about the onset of symptoms and first diagnosis. Age of onset was subtracted from a patient's current age to determine illness duration.
Statistical Analyses
Analyses were conducted using SPSS version 18 and Mplus version 6.0 (35). In Mplus, full information maximum likelihood was used to estimate model parameters with missing data. This approach results in greater power and accuracy, as it has been shown to provide unbiased parameter estimates when data are missing (36). Model fit was evaluated using several indices recommended by Hu and Bentler (37): comparative fit index (CFI) ≥.95, root-mean-square error of approximation (RMSEA) ≤.06, Standardized Root Mean Squared Residual (SRMR) ≤.09 and a non-significant χ2 goodness-of-fit statistic. In addition to overall model fit, structural equation modeling allows effects to be divided into their components (indirect, direct, and total effects) and tested for statistical significance.
Preliminary Analyses
Prior to conducting primary analyses, relationships among variables known to impact symptom severity and QoL in schizophrenia patients were examined to identify and statistically control for potential confounds. For continuous variables (age, education, drug abuse, medication adherence and illness duration), Pearson correlation coefficients were calculated. Independent sample t-tests were used to test gender differences and one-way ANOVAs were used to examine differences between ethnic groups on variables of interest.
Mediation
We followed Shrout and Bolger's (38) procedure for mediation analysis with two path models. Step one of this approach statistically tests the effect of X (independent variable, IV) on Y (dependent variable, DV). Some researchers have argued that this relationship does not need to be statistically significant to identify mediation when there is an a priori belief that the effect size is small or suppression is possible (38, 39). Step two involves estimating the path from the IV (X) to the mediator (M). In step three, the path from the mediator (M) to the DV (Y) is estimated, while holding the X→Y path constant. The fourth step involves testing the indirect path from X to Y through M. We utilized nonparametric bootstrapping in step four of the mediation analyses, which has been shown to be a more sensitive approach, especially with small to moderate sample sizes (38). With this method, standard errors of direct and indirect effects were estimated from a pseudopopulation of 5,000 samples drawn with replacement from our data. These standard errors were then employed in significance testing. If the indirect effect is statistically significant, the 95% confidence interval of the indirect effect specified in each model will not include zero. We first tested the model including intrinsic religion (X), meaning-making coping (M), symptom severity (Y) and QoL (Y). We next tested the model including extrinsic religion (X), a latent social support variable (M), symptom severity (Y), and QoL (Y). In both models, we included covariates identified through preliminary analyses.
Results
Means and standard deviations for all study variables are presented in Table 1. Zero-order correlations among main study variables are presented in Table 2. Relationships among continuous covariates and outcome variables are depicted in Table 3.
Table 1. Means and Standard Deviations of Study Variables.
| Measure | Mean | Standard Deviation |
|---|---|---|
| Education | 4.33 | 1.21 |
| Illness duration | 16.67 | 11.60 |
| Medication adherence | 1.56 | 0.36 |
| Drug abuse | 0.14 | 0.24 |
| Intrinsic religion | 3.38 | 0.81 |
| Extrinsic religion | 3.14 | 1.10 |
| Meaning-making coping | 2.94 | 0.87 |
| Seeking social support, instrumental | 2.59 | 0.84 |
| Seeking social support, emotional | 2.59 | 0.91 |
| Quality of life | 4.89 | 2.36 |
| BPRS-Total | 2.34 | 0.55 |
| BPRS-Positive | 2.62 | 0.93 |
| BPRS-Negative | 1.65 | 0.82 |
| BPRS-Agitation/Mania | 1.40 | 0.50 |
| BPRS-Depression/Anxiety | 3.34 | 1.34 |
This table shows means and standard deviations for all study variables. Information regarding scores and scales are included in the Methods section. BPRS=Brief Psychiatric Rating Scale.
Table 2. Zero-Order Correlations among the Main Study Variables.
| BPRS Total | BPRS-P | BPRS-N | BPRS-D/A | BPRS-A/M | IR | ER | MMC | SSI | SSE | QoL | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| BPRS-T | 1.00 | .81† | .01 | .73† | .31† | -.10 | -.05 | .04 | .05 | .07 | -.18 |
| BPRS-P | 1.00 | -.19* | .40† | .16 | -.01 | .06 | .14 | .08 | .10 | -.12 | |
| BPRS-N | 1.00 | -.14 | .03 | .13 | -.09 | -.21* | -.10 | -.13 | -.00 | ||
| BPRS-D/A | 1.00 | -.08 | -.09 | .01 | -.02 | .08 | .06 | -.26† | |||
| BPRS-A/M | 1.00 | -.19 | -.19 | -.04 | -.21* | -.10 | .09 | ||||
| IR | 1.00 | .42† | .28† | .22† | .10 | .15 | |||||
| ER | 1.00 | .17 | .25* | .25* | .10 | ||||||
| MMC | 1.00 | .58† | .55† | .27† | |||||||
| SSI | 1.00 | .73† | .16 | ||||||||
| SSE | 1.00 | .11 | |||||||||
| QoL | 1.00 |
p<.05;
p<.01.
BPRS-T=BPRS Total; BPRS-P=BPRS Positive Symptoms; BPRS-N=BPRS Negative Symptoms; BPRS-D/A=BPRS Depression/Anxiety; BPRS-A/M=BPRS Agitation/Mania; IR=Intrinsic Religion; ER=Extrinsic Religion; MMC=Meaning-Making Coping; SSI=Social Support, Instrumental; SSE=Social Support, Emotional; QoL=Quality of Life.
Table 3. Zero-Order Correlations among Covariates and Main Study Variables.
| Age | Education | Drug Abuse | Medication Adherence | Illness Duration | |
|---|---|---|---|---|---|
| BPRS Total | .05 | -.28† | .37† | -.31† | .27† |
| BPRS-Pos. | -.03 | -.27† | .28† | -.24† | .08 |
| BPRS-Neg. | -.16 | .10 | -.07 | .01 | -.03 |
| BPRS-A/M | -.30† | -.04 | .19 | -.01 | -.20* |
| BPRS-D/A | .29† | -.19* | .25* | -.18 | .45† |
| QoL | .06 | .05 | -.12 | .27* | -.03 |
p<.05;
p<.01.
BPRS-Pos.=BPRS Positive Symptoms; BPRS-Neg.=BPRS Negative Symptoms; BPRS-A/M=BPRS Agitation/Mania; BPRS-D/A=BPRS Depression/Anxiety; QoL=Quality of Life.
Preliminary Analyses
Greater symptom severity was associated with less education (r=-0.28, p<.01), less medication adherence (r=-0.31, p<.01), greater drug abuse (r=0.37, p<.01), and greater illness duration (r=0.27, p<.01). QoL was associated with greater medication adherence (r=0.27, p<.05). As these variables were known to relate to dependent variables, they were included as covariates in path models. There were no gender or ethnic differences on QoL or total symptom severity. Gender differences were noted on the depression/anxiety factor of the BPRS, with women (M=3.73, SD=1.29) displaying higher depression/anxiety than men (M=3.16, SD=1.34), t (109)=-2.02, p<.05.
Mediation
To test whether meaning-making coping mediated the expected relationships between intrinsic/extrinsic religion and outcomes, we first examined relationships between intrinsic religion and dependent variables, while controlling for relevant covariates. While in the expected direction, the initial relationships between intrinsic religion and QoL (standardized coefficient=0.13, SE=0.09, p=.14) and symptom severity (standardized coefficient=-0.12, SE=0.09, p=.17) did not reach the level of significance. As noted above, this path is not considered necessary to determine mediation when there is an a priori belief that the effect size is small (38, 39). As indicated in the introduction, 95% of the time the true population parameter of the effect size linking religion with well-being will fall between 0.14 and 0.25, which are considered small effect sizes (24). Thus, we proceeded with step two.
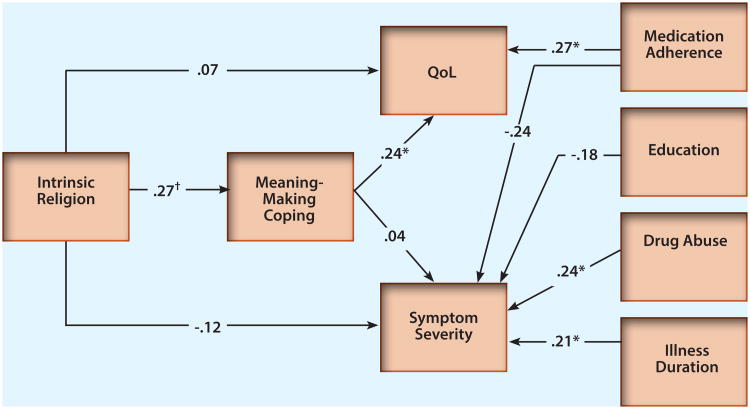
As hypothesized, the path estimating the effect from intrinsic religion to meaning-making coping was statistically significant (standardized coefficient=0.27, SE=0.09, p<.01), indicating that patients who reported higher intrinsic religion also reported higher meaning-making coping. Next, we found that the path between meaning-making coping and QoL was statistically significant (standardized coefficient=0.24, SE=0.09, p<.05), indicating a positive relationship between greater meaning-making coping and higher QoL. The path between meaning-making coping and symptom severity was not significant (standardized coefficient=0.04, SE=0.09, p>.05). Finally, the confidence interval associated with the specific indirect effect of intrinsic religion on QoL through meaning-making coping did not include zero (95% CI=0.05 to 0.44, p<.05), confirming that the data are consistent with mediation (35). In addition, the path estimating the direct effect of intrinsic religion on QoL was not significant (standardized coefficient=0.07, SE=0.09, p>.05), which is consistent with complete mediation. Complete mediation is confirmed by the finding that the bootstrapping estimate of the direct path between intrinsic religion and QoL was not statistically significant (95% CI=-0.29 to 0.67, p>.05). As hypothesized, meaning-making coping mediated the relationship between intrinsic religion and QoL. The final model was a good fit for the data, as evidenced by adequate fit indices: X2 (7)=5.37, p>.05, CFI=1.0, RMSEA=0.00, SRMR=0.03 (see Figure 1).
Figure 1. Path Model Depicting the Relationships between Intrinsic Religion, Meaning-Making Coping and Outcome Variables (QoL and Symptom Severity).
The four variables on the right of the model represent known covariates. *p<.05; †p<.01.
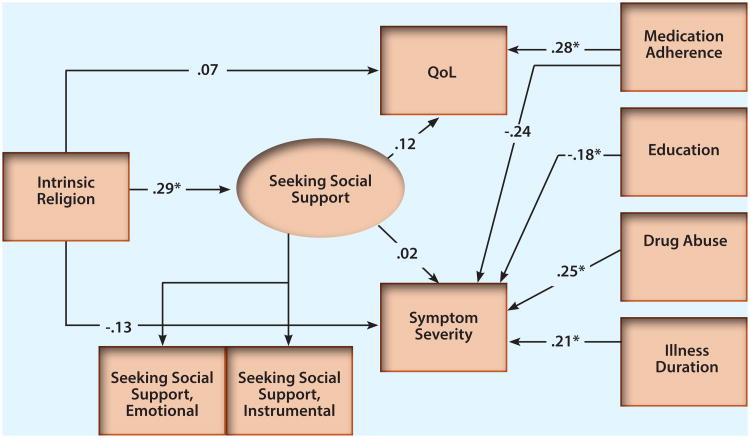
To test whether social support seeking mediated the relationship between extrinsic religion and outcomes, we created a hybrid model. This model included a latent seeking social support variable, which was estimated by two indicators: 1) seeking social support for instrumental reasons and 2) seeking social support for emotional reasons. Fit indices indicated that the overall model was a good fit for the data: X2 (13)=12.49, p>.05, CFI=1.0, RMSEA=0.00, SRMR=0.05 (see Figure 2). Initial relationships between extrinsic religion and QoL (standardized coefficient=0.10, SE=0.09, p=.28) and symptom severity (standardized coefficient=-0.13, SE=0.09, p=.13) were not significant. As the paths linking extrinsic religion and outcomes were in the expected direction, we proceeded with the analysis. The path estimating the effect of extrinsic religion on seeking social support was statistically significant (standardized coefficient=0.29, SE=0.10, p<.01). Patients who endorsed higher extrinsic religion also endorsed higher seeking social support. However, the paths linking seeking social support to QoL and symptom severity were not significant (standardized coefficient=0.12, SE=0.11, p>.05 and standardized coefficient=0.02, SE=0.10, p>.05, respectively). While extrinsic religion predicted greater seeking social support, results were not in line with the hypothesis that seeking social support mediates the relationship between extrinsic religion and outcomes.
Figure 2. Path Model Depicting the Relationships between Extrinsic Religion, Seeking Social Support and Outcome Variables (QoL and Symptom Severity).
The four variables on the right of the model represent known covariates. *p<.05.
Exploratory Analyses
Several exploratory regression analyses examining relationships among religion, meaning-making coping, seeking social support, and specific BPRS symptom clusters were conducted to follow-up some of the null findings regarding symptom severity. After controlling for relevant covariates, there was a significant inverse relationship between meaning-making coping and negative symptoms (B=-0.21, p<.05). There was also a significant inverse relationship between seeking social support for instrumental reasons and the agitation/mania symptom cluster of the BPRS (B=-0.25, p<.05). All other regression analyses were non-significant.
Discussion
This study is the first to test whether meaning-making coping and seeking social support mediate potential benefits of religion on the mental health of patients with schizophrenia. This was also one of the first studies to differentiate between intrinsic and extrinsic religious orientations in SMI. The direct effects of religion on mental health did not reach the level of significance, but were in the expected direction. As hypothesized, the effect of intrinsic religion on QoL was completely mediated by meaning-making coping. This finding was in line with previous studies in non-psychiatric populations (17, 18). Results suggest that the ability to learn, grow and make sense out of the experience of living with schizophrenia may be related to increased life satisfaction. QoL is an important variable in schizophrenia research because it reflects patients' subjective sense of psychological well-being. Addressing meaning-making efforts in therapeutic settings, perhaps through cognitive restructuring techniques, may be one way to target this important clinical variable.
Also in line with hypotheses, extrinsic religion was positively related to seeking social support. This coping style did not, however, mediate the relationship between extrinsic religion and mental health. Previous research has demonstrated the beneficial effects of social support in patients with schizophrenia (1). One potential reason for the lack of support for this meditational model may relate to the fact that our social support measure assessed the extent to which participants seek (not obtain) social support. Previous studies of social support in SMI have used detailed social support interviews in which participants describe their relationships with kin and non-kin supports and rate their satisfaction with social support. In the present study, we chose to examine seeking social support because we were interested in examining coping styles that might relate to beneficial outcomes rather than one's ability to obtain and/or maintain social support. Future research would benefit from using more detailed assessments of social support to measure the extent to which participants receive and benefit from their support networks and, in turn, how successful use of social support affects recovery variables.
Exploratory analyses revealed some interesting directions for future research. Meaning-making coping was related to less severe negative symptoms. Treatment of negative symptoms has provided a major challenge for clinicians as these symptoms tend to be persistent and are associated with poor functional outcome (40). Incorporating a recovery-oriented approach in which individuals are encouraged to make meaning from their difficult experiences with SMI may be one pathway toward improvement in this domain. As meaning-making is linked to important outcome variables such as negative symptoms and QoL, future research would greatly benefit from further investigation of this construct and the development of a reliable and psychometrically valid meaning-making scale specific to coping with SMI.
In addition, seeking social support for instrumental reasons was related to less agitation/mania. While this finding is not directly supported by prior research, empirical investigations have revealed that individuals who see their situation as more amenable to change are more likely to seek social support for instrumental reasons when compared to those who believe their situation is uncontrollable (30). Individuals with less agitation/mania may be more likely to view their situation as controllable and, thus, seek out advice from friends and family. While these results are encouraging, they were conducted on an exploratory basis and should be replicated before firm conclusions are drawn.
Finally, we found some interesting relationships with covariates that support prior research. For example, higher education was related to less symptom severity in our study and in prior research (41). Greater drug abuse was associated with more severe psychiatric symptoms among patients, which provides further support for the deleterious effects of drug abuse for people with schizophrenia (42). Medication adherence was related to less symptom severity and greater QoL, which, in conjunction with earlier studies (33), provides rationale for encouraging patients to maintain compliance with psychopharmacological interventions.
This study has several notable limitations. First, the data were cross-sectional, which precludes the ability to determine causal relationships. While prior research has supported our conclusion that religion may offer mental health benefits for individuals with schizophrenia, it is also possible that the lack of severe psychiatric symptoms allows patients to experience greater religious conviction. In this case, religion may be the result of decreased symptom severity rather than the determinant. Future research would benefit from examining changes in religion, coping variables, and outcomes over time. For example, we might ask participants to specifically discuss how they made sense of the experience upon first diagnosis. This information could be used to examine discrepancies between situational and global meaning in this context to help clarify how patients undergo the meaning-making process. In addition, the present study did not include a control group and, therefore, we were unable to examine whether the paths from religion to QoL differ for those with and without a schizophrenia diagnosis. Future research would benefit from this inclusion and from the use of more sensitive measures of the main study variables that may confirm that findings can be accurately attributed to religion and the associated mediator variables.
There are also limits to the generalizability of our results based on sample characteristics. The present sample was made up of relatively high-functioning outpatients with very mild to mild levels of psychiatric symptoms. While we believe our results would generalize to common outpatient clinics in which patients are in recovery versus acute phases of the illness, researchers should be cautious when applying these results to individuals with more severe symptoms. Nonetheless, we believe that the findings from the present study are important and suggest that this line of research deserves further empirical investigation.
Clinical Implications.
This study is the first to test whether meaning-making coping and seeking social support mediate potential benefits of religion on the mental health of patients with schizophrenia. This was also one of the first studies to differentiate between intrinsic and extrinsic religious orientations in serious mental illness (SMI). The direct effects of religion on mental health did not reach the level of significance, but were in the expected direction. As hypothesized, the effect of intrinsic religion on quality of life was completely mediated by meaning-making coping. This finding was in line with previous studies in non-psychiatric populations (17, 18). Results suggest that the ability to learn, grow and make sense out of the experience of living with schizophrenia may be related to increased life satisfaction. QoL is an important variable in schizophrenia research because it reflects patients' subjective sense of psychological well-being. Addressing meaning-making efforts in therapeutic settings, perhaps through cognitive restructuring techniques, may be one way to target this important clinical variable.
Also in line with hypotheses, extrinsic religion was positively related to seeking social support. This coping style did not, however, mediate the relationship between extrinsic religion and mental health. Previous research has demonstrated the beneficial effects of social support in patients with schizophrenia (1). One potential reason for the lack of support for this meditational model may relate to the fact that our social support measure assessed the extent to which participants seek (not obtain) social support. Previous studies of social support in SMI have used detailed social support interviews in which participants describe their relationships with kin and non-kin supports and rate their satisfaction with social support. In the present study, we chose to examine seeking social support because we were interested in examining coping styles that might relate to beneficial outcomes rather than one's ability to obtain and/or maintain social support. Future research would benefit from using more detailed assessments of social support to measure the extent to which participants receive and benefit from their support networks and, in turn, how successful use of social support affects recovery variables.
Acknowledgments
This work was supported by the National Institute of Mental Health at the National Institutes of Health (5R34MH7 to Amy Weisman de Mamani).
References
- 1.Eack SM, Newhill CE, Anderson CM, Rotondi AJ. Quality of life for persons living with schizophrenia: more than just symptoms. Psychiatr Rehabil J. 2007;30(3):219–222. doi: 10.2975/30.3.2007.219.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.George L, Larson D, Koenig H, McCullough M. Spirituality and health: what we know, what we need to know. J Soc Clin Psychol. 2000;19:102–116. [Google Scholar]
- 3.Koenig HG, Larson DB, Weaver AJ. Research on religion and serious mental illness. New Dir Ment Health Serv. 1998;(80):81–95. doi: 10.1002/yd.23319988010. [DOI] [PubMed] [Google Scholar]
- 4.Koenig HG, Hays JC, George LK, Blazer DG, Larson DB, Landerman LR. Modeling the cross-sectional relationships between religion, physical health, social support, and depressive symptoms. Am J Geriatr Psychiatry. 1997;5(2):131–143. [PubMed] [Google Scholar]
- 5.Kennedy GJ, Kelman HR, Thomas C, Chen J. The relation of religious preference and practice to depressive symptoms among 1,855 older adults. J Gerontol B Psychol Sci Soc Sci. 1996;51(6):301–308. doi: 10.1093/geronb/51b.6.p301. [DOI] [PubMed] [Google Scholar]
- 6.Borras L, Mohr S, Brandt PY, Gillieron C, Eytan A, Huguelet P. Religious beliefs in schizophrenia. Schizophr Bull. 2007;33(5):1238–1246. doi: 10.1093/schbul/sbl070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pieper JZT. Religious coping in highly religious psychiatric inpatients. Ment Health Relig Cult. 2004;7:349–363. [Google Scholar]
- 8.Weisman de Mamani AG, Tuchman N, Duarte E. Incorporating religion/spirituality into treatment for serious mental illness. Cogn Behav Pract. 2010;17:348–357. [Google Scholar]
- 9.Donahue MJ. Intrinsic and extrinsic religiousness: review and meta-analysis. J Pers Soc Psychol. 1985;48:400–419. [Google Scholar]
- 10.Ventis WL. The relationships between religion and mental health. J Soc Issues. 1995;51:33–48. [Google Scholar]
- 11.Koenig HG, George LK, Peterson BL. Religiosity and remission of depression in medically ill older patients. Am J Psychiatry. 1998;155(4):536–542. doi: 10.1176/ajp.155.4.536. [DOI] [PubMed] [Google Scholar]
- 12.Pargament KI, Ensing DS, Falgout K, Olsen H, Reilly B, van Haitsma K, et al. God help me: (I): Religious coping effects as predictors of outcomes to significant negative life events. Am J Community Psychol. 1990;18(6):793–824. [Google Scholar]
- 13.Russinova Z, Cash D. Personal perspectives about the meaning of religion and spirituality among persons with serious mental illnesses. Psychiatr Rehabil J. 2007;30(4):271–284. doi: 10.2975/30.4.2007.271.284. [DOI] [PubMed] [Google Scholar]
- 14.Getz GE, Fleck DE, Strakowski SM. Frequency and severity of religious delusions in Christian patients with psychosis. Psychiatry Res. 2001;103(1):87–91. doi: 10.1016/s0165-1781(01)00262-1. [DOI] [PubMed] [Google Scholar]
- 15.Siddle R, Haddock G, Tarrier N, Faragher EB. Religious delusions in patients admitted to hospital with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2002;37(3):130–138. doi: 10.1007/s001270200005. [DOI] [PubMed] [Google Scholar]
- 16.Mohr S, Gillieron C, Borras L, Brandt PY, Huguelet P. The assessment of spirituality and religiousness in schizophrenia. J Nerv Ment Dis. 2007;195(3):247–253. doi: 10.1097/01.nmd.0000258230.94304.6b. [DOI] [PubMed] [Google Scholar]
- 17.McIntosh DN, Silver RC, Wortman CB. Religion's role in adjustment to a negative life event: coping with the loss of a child. J Pers Soc Psychol. 1993;65(4):812–821. doi: 10.1037//0022-3514.65.4.812. [DOI] [PubMed] [Google Scholar]
- 18.Park CL. Religion as a meaning-making framework in coping with life stress. J Soc Issues. 2005;61:707–729. [Google Scholar]
- 19.Norman RM, Malla AK, Manchanda R, Harricharan R, Takhar J, Northcott S. Social support and three-year symptom and admission outcomes for first episode psychosis. Schizophr Res. 2005;80(2-3):227–234. doi: 10.1016/j.schres.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Huguelet P, Mohr S, Borras L. Recovery, spirituality, and religiousness in schizophrenia. Clin Schizophr Relat Psychoses. 2009;2(4):307–316. [Google Scholar]
- 21.Zika S, Chamberlain K. On the relation between meaning in life and psychological well-being. Br J Psychol. 1992;83(Pt 1):133–145. doi: 10.1111/j.2044-8295.1992.tb02429.x. [DOI] [PubMed] [Google Scholar]
- 22.Phillips RE, 3rd, Stein CH. God's will, God's punishment, or God's limitations? Religious coping strategies reported by young adults living with serious mental illness. J Clin Psychol. 2007;63(6):529–540. doi: 10.1002/jclp.20364. [DOI] [PubMed] [Google Scholar]
- 23.Chamberlain K, Zika S. Religiosity, life meaning and wellbeing: some relationships in a sample of women. J Sci Study Relig. 1988;27:411–420. [Google Scholar]
- 24.Witter RA, Stock WA, Okun MA, Haring MJ. Religion and subjective well-being in adulthood: a quantitative synthesis. Rev Relig Res. 1985;26:332–342. [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis-I Disorders–Patient edition (SCID-I/P, Version 2.0) New York (NY): Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 26.Geisinger KF. Cross-cultural normative assessment: translation and adaptation issues influencing the normative interpretation of assessment instruments. Psychol Assess. 1994;6:304–312. [Google Scholar]
- 27.Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: “The Drif Busters”. Int J Methods Psychiatr Res. 1993;3:221–224. [Google Scholar]
- 28.Kopelowicz A, Ventura J, Liberman RP, Mintz J. Consistency of Brief Psychiatric Rating Scale factor structure across a broad spectrum of schizophrenia patients. Psychopathology. 2008;41(2):77–84. doi: 10.1159/000111551. [DOI] [PubMed] [Google Scholar]
- 29.Gorsuch RL, McPherson SE. Intrinsic/extrinsic measurement: I/E-revised and single-item scales. J Sci Study Relig. 1989;28:348–354. [Google Scholar]
- 30.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 31.Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the Quality of Life Inventory: a measure of life satisfaction for use in treatment planning and outcome assessment. Psychol Assess. 1992;4:92–101. [Google Scholar]
- 32.Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–247. doi: 10.1016/s0920-9964(99)00130-9. [DOI] [PubMed] [Google Scholar]
- 33.Fialko L, Garety PA, Kuipers E, Dunn G, Bebbington PE, Fowler D, et al. A large-scale validation study of the Medication Adherence Rating Scale (MARS) Schizophr Res. 2008;100(1-3):53–59. doi: 10.1016/j.schres.2007.10.029. [DOI] [PubMed] [Google Scholar]
- 34.Panton J, Brisson R. Characteristics associated with drug abuse within a state prison population. Correct Psych J Soc Ther. 1971;17:3–33. [Google Scholar]
- 35.Muthén LK, Muthén BO. Mplus user's guide. Sixth. Los Angeles (CA): Muthén & Muthén; pp. 1998–2010. [Google Scholar]
- 36.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 37.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 38.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7(4):422–445. [PubMed] [Google Scholar]
- 39.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buchanan RW. Persistent negative symptoms in schizophrenia: an overview. Schizophr Bull. 2007;33(4):1013–1022. doi: 10.1093/schbul/sbl057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 42.Barry KL, Fleming MF, Greenley J, Widlak P, Kropp S, McKee D. Assessment of alcohol and other drug disorders in the seriously mentally ill. Schizophr Bull. 1995;21(2):313–321. doi: 10.1093/schbul/21.2.313. [DOI] [PubMed] [Google Scholar]