Abstract
Background/Objectives
We assessed the impact of an electronic health record-based transitional care intervention involving automated alerts to primary care providers and staff when older patients were discharged from the hospital.
Design
Randomized controlled trial.
Setting
A large multispecialty group practice.
Participants
Patients aged 65 or older discharged from hospital to home.
Intervention
In addition to notifying primary care providers about the patient's recent discharge, the system provided information about new drugs added during the inpatient stay, warnings about drug-drug interactions, and recommendations for dose changes and laboratory monitoring of high-risk medications, as well as alerts to the primary care provider's support staff to schedule a post-hospitalization office visit.
Measurements
An outpatient office visit with a primary care provider following discharge and rehospitalization within 30 days following discharge.
Results
Of the 1870 discharges in the intervention group, 27.7% had an office visit with a primary care provider within 7 days of discharge. Of the 1,791 discharges in the control group, 28.3% had an office visit with a primary care provider within 7 days of discharge. In the intervention group, 18.8% experienced a rehospitalization within the 30-day period post-discharge compared with 19.9% in the control group. The hazard ratio for an office visit with a primary care physician did not significantly differ between the intervention and control groups. The hazard ratio for rehospitalization in the 30-day period following hospital discharge in the intervention versus the control group was 0.94 (95% confidence interval: 0.81, 1.1).
Conclusion
We did not demonstrate a significant effect of this electronic health record-based intervention in increasing the timeliness of office visits to primary care providers following hospitalization, or reducing risk of rehospitalization.
Keywords: rehospitalization, care transitions, readmission, patient safety, randomized controlled trial
Introduction
It is well established that the transition between the inpatient and outpatient setting is a period of high risk for older patients.3,4 Nearly one fifth of older patients suffers an adverse event within 3 weeks of hospital discharge.5 Medication prescribing and monitoring errors are particularly common during the high-risk post-hospital discharge period.6,7 Hospital readmissions among older adults are also costly and an important opportunity to reduce Medicare spending. Under the Affordable Care Act, the Centers for Medicare and Medicaid Services has implemented financial penalties for hospitals with 30-day readmission rates that are considered excessive.1, 2
It has been suggested that optimal post-hospital transitions may hinge on scheduled follow-up with the primary care physician following hospital discharge.8,9 In a large study of patients in the Medicare fee-for-service program, of the nearly one in five rehospitalized within 30 days, over half had not been seen in follow-up in the outpatient setting prior to readmission.10 Starting in 2013, two new Current Procedural Terminology (CPT) codes became available to support “Transitional Care Management Services” and some health plans have begun to provide financial incentives to medical groups that achieve specified benchmarks relating to timely post-discharge follow-up office visits for older patients.
Several approaches for improving transitions of older adults from the hospital to the outpatient setting have been developed, but most require substantial and ongoing commitments of resources and personnel.11, 12 With the widespread adoption of electronic health records (EHR) by medical group practices, there may be new opportunities to automate processes that improve the quality and safety of care for patients discharged from hospitals. We conducted a randomized controlled trial of an EHR-based transitional care intervention for older adults discharged from hospital to home to assess the impact on having an outpatient visit with a primary care provider after discharge and being rehospitalized within 30 days of discharge.
Methods
Study Setting, Population, and Design
Our study was conducted in the setting of a large multispecialty group practice. The group practice employs 265 physicians, including 66 primary care providers who care for adult patients in the outpatient setting. Hospital care is delivered by hospitalists employed by the medical group. The group practice has used an electronic health record (EHR) since 2006 (Epic Systems Corporation). The primary inpatient facility to which the group practice admitted its patients used a different EHR; however, the EHR utilized by the group practice captured selected clinical data from the inpatient setting.
The group provides care to approximately 24,000 senior plan members of an associated health plan, with which the group shares financial risk. The study population was derived from this population of patients. We studied patients discharged from the primary hospital used by the group practice from August 26, 2010 to August 25, 2011. Eligibility criteria for inclusion in the study were: (1) patient age 65 years or older at the time of discharge; (2) discharged from the primary inpatient facility serving the medical group for a non-psychiatric condition; (3) no plans to enroll in hospice upon discharge; and (4) discharged to the community (not a skilled nursing facility, rehabilitation facility, or long-term care setting). Hospitalizations that included a surgical procedure were included, as were hospitalizations with observation status.13 Patients were randomized to having the EHR-based transitional care intervention (see below) or to the usual approach to follow-up care at the time of hospital discharge. The same individual could be included multiple times in the study if more than one hospital discharge was experienced by that person over the study period.
On a daily basis, a computer program identified each hospital discharge of a patient who was age 65 or older, enrolled in the health plan, and under the care of the medical group. The program used a random number generator to assign each discharge to the intervention or control group. The EHR-based transitional care intervention was applied to all hospital discharges in the intervention group. At the time of randomization, the automated system could not identify whether the patient had been discharged to home. Therefore, post-randomization, all discharges were manually reviewed by reviewers who were blinded to the intervention status assigned by the automated system to confirm eligibility for the study. The EHR-based transitional care intervention was not operational between September 25, 2010 and October 23, 2010 due to upgrades to the EHR.
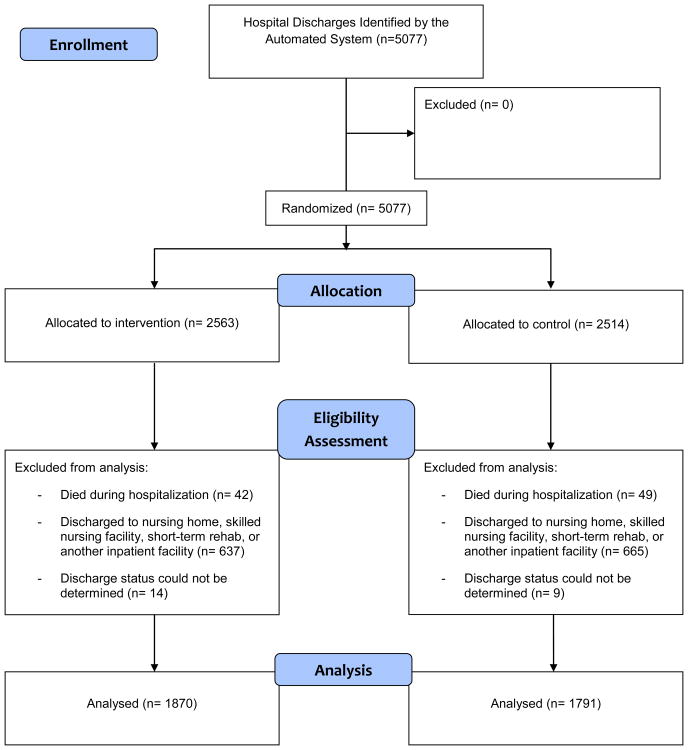
There were 5,077 hospital discharges randomized (Figure 1). It was subsequently determined that 91 had died during the hospitalization. In addition, it was determined that 1,302 were discharged to a nursing home, skilled nursing facility, an inpatient rehabilitation facility, or transferred to another acute care hospital. For 23 patients, discharge status could not be definitively determined. This left 3,661 study discharges: 1870 in the intervention group and 1791 in the control group.
Figure 1. Adapted CONSORT Flow Diagram.
The institutional review board of the University of Massachusetts Medical School and the institutional review board of the multispecialty medical group and the health plan approved this study. The approval did provide a waiver of consent. The study was registered with ClinicalTrials.gov (NCT00611091).
Characteristics of Study Subjects
We characterized discharged patients according to age at the time of discharge, gender, length of stay, whether a surgical procedure was performed during the hospitalization, home health services during the week following hospitalization, hospitalizations during the prior year, office visits during the prior year, number of different providers seen during the prior year in the outpatient setting, number of prescriptions filled during the prior year for different medications based on National Drug Codes (NDC), number of lab tests ordered during the prior year, Charlson comorbidity index,14 and selected medical conditions (diabetes mellitus, myocardial infarction, heart failure, chronic lung disease, cancer, stroke and cerebrovascular disease, and renal disease) on the basis of diagnoses, using relevant ICD-9 codes derived from health plan administrative data.
EHR-Based Transitional Care Intervention
The process of developing the EHR-based intervention has been described previously.15 We developed an automated system to facilitate the flow of information to the medical group's primary care providers about patients who were discharged to home from the hospital. The primary inpatient facility to which the medical group admitted its patients used a different EHR than the medical group; however, an interface engine was linked to the hospital's admission, discharge, transfer (ADT) registration system. The medical group provided the names of its providers to the hospital and the hospital transmitted information including admission and discharge dates for the medical group's patients. This information was automatically incorporated into the medical group's EHR.
In addition to notifying providers about the patient's discharge, the system provided information about new drugs at the time of hospital discharge, warnings about selected drug-drug interactions and recommendations for consideration of dose changes and laboratory monitoring of high-risk medications,16 as well as alerts to the provider's support staff to schedule a post-hospitalization office visit within one week of discharge if not already scheduled. Messages were delivered on day 3 following discharge from the hospital. The reason for the delay was to allow information on newly filled prescriptions to come through the system to develop alerts about the new medications. Information about medications prescribed prior to the hospitalization was derived from the EHR and health plan data, while information about new medications dispensed following hospital discharge was obtained just from health plan data.
Messages to schedule an office visit with the primary care provider within one week were sent to the primary care provider's support staff. These messages were not sent when scheduling information within the EHR indicated that such a visit had already been scheduled to avoid sending unnecessary alerts.
Outcome Measures
We determined whether discharged patients had an office visit with a primary care physician in the 7-day, 14-day, and 30-day periods following hospital discharge. We also determined whether a patient was rehospitalized within 30 days. We ascertained information related to office visits and hospitalizations from the medical group's EHR and from health plan data, which allowed for determination of whether a rehospitalization had occurred at any hospital, and not just the primary hospital that served patients cared for by the medical group. Analysts determined these outcomes at least 6 months after completion of the study and were blinded to intervention status.
Statistical Analysis
We originally estimated that 5000 hospital discharges would be enrolled which we achieved; however, ultimately 3,661 study discharges were analyzed following eligibility assessment (Figure 1): 1870 in the intervention group and 1791 in the control group. We estimate that a sample of 3600 hospital discharges approximately evenly split between the intervention and control groups provides 80% power to detect a hazard ratio of 0.81 for time to rehospitalization in the intervention group as compared with the control group. This estimate assumes a 30-day rehospitalization rate of 20%.10
For direct comparisons of baseline characteristics between those randomized to the intervention and control groups, we used Fischer exact tests for categorical variables and t-tests for continuous variables. Reported p-values are 2-sided. Analyses of outcomes included comparisons of the intervention and control discharges with regard to having an office visit with a primary care physician in the 7, 14, and 30-day post-discharge periods, and rehospitalization within 30 days. These analyses included data for hospital discharges of patients who were discharged to the community (not to a skilled nursing facility, rehabilitation facility, or long-term care setting), as depicted in Figure 1. For the office visit outcomes, estimates included the proportion of patients receiving office visits within the three time frames among the intervention and control groups. Time to occurrence of an office with a primary care physician was estimated with the use of Kaplan-Meier methods and survival curves. For comparisons between the two groups, we excluded days 0-2 post-discharge which preceded the delivery of the alerts, and we used Cox proportional hazards models to calculate hazard ratios to take into account varying amounts of “opportunity time” for office visits due to rehospitalization or death. To accommodate repeated measures for patients with multiple discharges during the study, we used a frailty model to estimate 95% confidence intervals. The proportional hazard assumptions were checked by inclusion of the cross-product of log (follow-up time) by exposure group.
Analyses relating to the rehospitalization outcome were similar to those for the office visit outcomes. We prepared estimates of the overall proportion of discharges followed by rehospitalization separately for the intervention and control groups. We prepared survival curves for rehospitalization in the 30-day follow-up period and used Cox proportional hazards models to calculate the hazard ratio comparing the intervention and control groups. As with the office visit outcomes, we used frailty models to estimate 95% confidence intervals and checked the proportional hazard assumption.
SAS software version 9.2 and Stata/IC version 12 for Unix were used for statistical analyses.
Results
There were 3,661 hospital discharges included in the intervention and control groups that were experienced by 2,645 unique patients (range 1-12). Of these 2,645 patients, 627 (23.7%) contributed >1 discharge.
Baseline demographic and clinical characteristics were similar across the intervention and control groups of hospital discharges (Table 1). There were no differences between the two groups in age at the time of hospital discharge, gender, length of stay, a surgical procedure having been performed during the hospitalization, or use of home health services in the week following discharge. In addition, the number of hospitalizations, office visits to any outpatient provider, different health care providers seen, number of prescriptions filled, number of outpatient lab tests performed, and Charlson comorbidity index scores were similar for discharged patients in the intervention and control groups. The percentages with a history of diabetes mellitus, heart failure, chronic lung disease, cancer, stroke/cerebrovascular disease, and renal disease were also similar between the two groups.
Table 1. Characteristics of discharges in the intervention and control groups.
| Characteristic | Intervention, N=1870 | Comparison, N=1791 | |||
|---|---|---|---|---|---|
|
| |||||
| Mean | STD | Mean | STD | ||
| Patient age at the time of discharge (years) | 79.0 | 7.16 | 79.1 | 7.23 | |
| # | % | # | % | p-value | |
| Categories of patient ages (years) | |||||
| 65-74 | 568 | 30.4 | 527 | 29.4 | 0.233 |
| 75-84 | 840 | 44.9 | 853 | 47.6 | |
| 85+ | 462 | 24.7 | 411 | 23.0 | |
| Patient gender – female | 990 | 52.9 | 931 | 52.0 | 0.561 |
| Length of stay | |||||
| 1 night | 515 | 27.5 | 475 | 26.5 | 0.122 |
| 2 nights | 496 | 26.5 | 432 | 24.1 | |
| 3-4 nights | 534 | 28.6 | 571 | 31.9 | |
| 5+ nights | 313 | 17.4 | 325 | 17.5 | |
| Surgery during hospitalization | 390 | 20.9 | 344 | 19.2 | 0.213 |
| Home health in week after discharge | 471 | 25.2 | 427 | 23.8 | 0.895 |
| Hospitalizations during past year | |||||
| 0 | 1043 | 55.8 | 989 | 55.2 | 0.204 |
| 1-2 | 491 | 26.3 | 510 | 28.5 | |
| 3+ | 336 | 17.9 | 292 | 16.3 | |
| Office visits during past year | |||||
| 0-3 | 528 | 28.2 | 507 | 28.3 | 0.971 |
| 4-6 | 412 | 22.0 | 400 | 22.3 | |
| 7-11 | 471 | 25.2 | 439 | 24.5 | |
| 12+ | 459 | 24.6 | 445 | 24.9 | |
| Number of different providers during past year | |||||
| 0-2 | 477 | 25.5 | 451 | 25.2 | 0.901 |
| 3-5 | 643 | 34.4 | 634 | 35.4 | |
| 6-7 | 333 | 17.8 | 306 | 17.1 | |
| 8+ | 417 | 22.3 | 400 | 22.3 | |
| Number of prescriptions filled in past year | |||||
| <8 | 455 | 24.3 | 464 | 25.9 | 0.540 |
| 8-12 | 480 | 25.7 | 428 | 23.9 | |
| 13-18 | 449 | 24.0 | 428 | 24.5 | |
| 19+ | 486 | 26.0 | 461 | 25.7 | |
| Number of lab tests performed in past year | |||||
| <28 | 475 | 25.4 | 490 | 27.3 | 0.079 |
| 28-42 | 475 | 25.4 | 397 | 22.2 | |
| 43-64 | 478 | 25.6 | 447 | 25.0 | |
| 65+ | 442 | 23.6 | 457 | 25.5 | |
| Charlson comorbidity score | |||||
| 0 | 266 | 14.2 | 254 | 14.2 | 0.164 |
| 1 | 404 | 21.6 | 342 | 19.1 | |
| 2 | 348 | 18.6 | 370 | 20.6 | |
| 3 | 328 | 17.5 | 284 | 15.9 | |
| 4 | 200 | 10.7 | 209 | 11.7 | |
| 5+ | 324 | 17.3 | 332 | 18.5 | |
| Diabetes | 690 | 36.9 | 708 | 39.5 | 0.101 |
| Myocardial infarction | 268 | 14.3 | 238 | 13.3 | 0.361 |
| Heart failure | 488 | 26.1 | 482 | 26.9 | 0.576 |
| Chronic obstructive pulmonary disease | 581 | 31.1 | 579 | 32.3 | 0.413 |
| Cancer | 482 | 25.8 | 472 | 26.4 | 0.690 |
| Stroke/cerebrovascular disease | 382 | 20.4 | 373 | 20.8 | 0.766 |
| Renal disease | 339 | 18.1 | 348 | 19.4 | 0.313 |
Of the 1,870 hospital discharges in the intervention group, 518 (27.7%) had an office visit with a primary care provider within 7 days of discharge, 990 (52.9%) had an office visit within 14 days of discharge, and 1,283 (68.6%) had an office visit within 30 days of discharge. Of the 1,791 hospital discharges in the control group, 507 (28.3%) had an office visit with a primary care provider within 7 days of discharge, 940 (52.5%) had an office visit within 14 days of discharge, and 1,233 (68.8%) had an office visit within 30 days of discharge. Figure 2 displays the Kaplan-Meier estimates of time to an office visit with a primary care physician. The hazard ratio for an office visit with a primary care physician in the 7-day period following hospital discharge (excluding the first 2 days post-discharge which preceded the intervention) was 0.95 (95% confidence interval: 0.83, 1.1) for the intervention group as compared with the control group. For the 14-day period following hospital discharge, the hazard ratio was 0.98 (95% confidence interval: 0.89, 1.1), and for the 30-day period, it was 0.99 (95% confidence interval: 0.91, 1.1).
Figure 2.
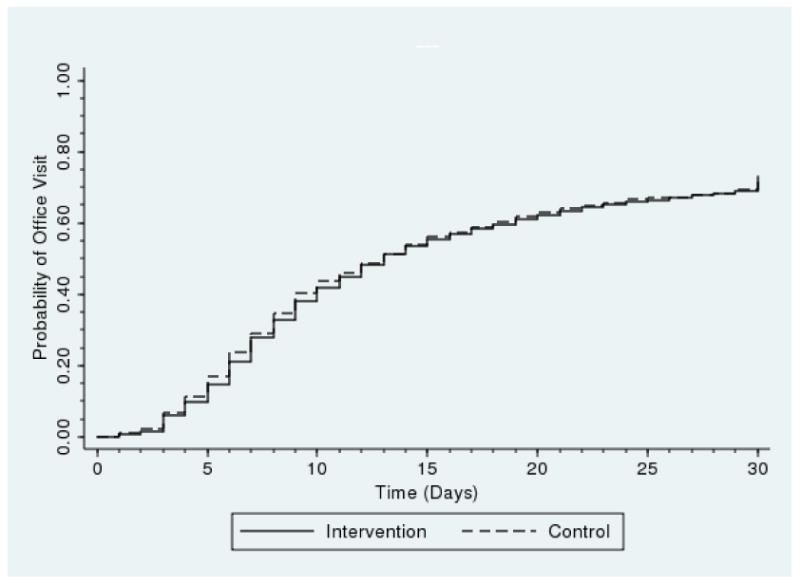
Kaplan-Meier estimates of time to an office visit with a primary care physician.
Of the 1,870 hospital discharges in the intervention group, 351 (18.8%) experienced a rehospitalization within the 30-day period post-discharge; of the 1,791 hospital discharges in the control group, 356 (19.9%) experienced a rehospitalization in that 30-day period. Figure 3 displays the Kaplan-Meier estimates of time to rehospitalization. The hazard ratio for rehospitalization in the 30-day period following hospital discharge (excluding the first 2 days post-discharge which preceded the intervention) was 0.94 (95% confidence interval: 0.81, 1.1) for the intervention versus the control group.
Figure 3.
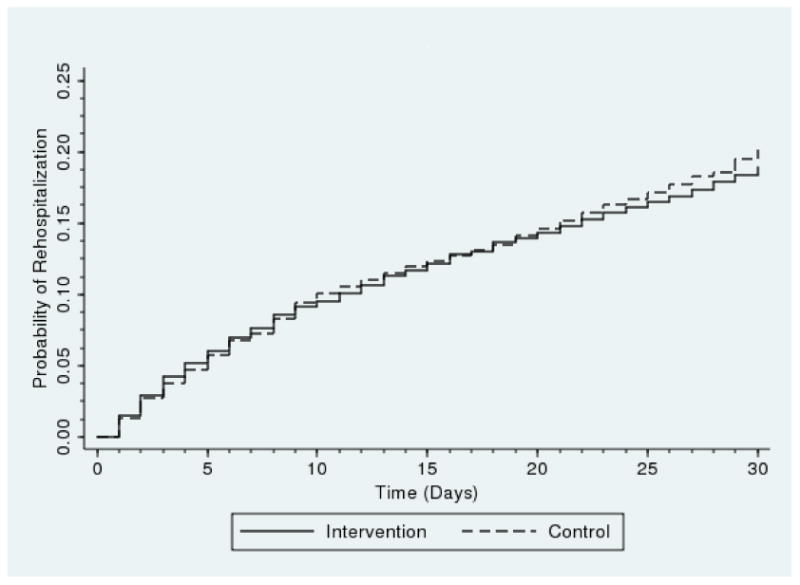
Kaplan-Meier estimates of time to rehospitalization.
Discussion
In our study of an EHR-based transitional care intervention in older patients discharged from hospital to home, we were not able to demonstrate either an increase in follow-up visits with a primary care physician or a reduction in the risk of rehospitalization. Despite a large number of randomized hospital discharges and high 30-day rehospitalization rates among both the intervention and the control groups, our study was not powered to detect a very modest reduction in the risk of rehospitalization relating to the intervention, as observed in our study. In addition, we did not find a difference in office visits with a primary care physician between the two groups, which had been hypothesized as the component of the intervention most essential to its success. There are several plausible explanations for why our intervention was not successful, but one possibility is that other competing efforts at reducing rehospitalizations were ongoing within the hospital and/or within various components of the multispecialty group practice. While nascent efforts focused on reducing rehospitalizations may have existed during the period of our study, to our knowledge, there were no systematic, hospital or practice-wide competing interventions. The high rates of rehospitalization observed in our study also serve to reduce the likelihood of this possibility.
The importance of hospital readmissions among older patients as a target for improving quality of care and reducing healthcare costs has been widely recognized, yet the optimal approach to addressing this challenge remains uncertain.12 Over a decade ago, Coleman proposed key elements of effective transitions between clinical settings.3 These include: communication between sending and receiving clinicians; reconciliation of the patient's medication regimen; a follow-up plan for how outstanding tests and follow-up appointments will be completed; preparation of the patient and caregiver for what to expect at the next site of care; and a discussion with the patient and caregiver regarding warning symptoms and signs to monitor. The intervention tested in the present study touched on some, but certainly not all of these elements. Of particular importance, the intervention did not engage the patient or caregiver. Family caregivers have been characterized as “de facto care coordinators” helping to ensure quality, safety, and adherence to patient preferences.9 Hansen and colleagues have written that “engaging the patient in the discharge process and transforming the process into an activity done with a patient rather than to a patient” may hold the greatest promise for reducing rehospitalization rates.12
The success of our EHR-based intervention required a very high level of responsibility and accountability on the part the primary care provider and staff. Providers and staff had to open alerts, then follow-up on information and recommendations provided. This might necessitate ascertaining additional information about the hospitalization that had not been incorporated into the alerts, reviewing discharge summaries, test results, and additional details about newly prescribed medications, scheduling visits with other providers, and determining whether home health services had been provided or were needed. It is commonly assumed that the primary care provider will automatically accept ultimate responsibility for care coordination relating to transitions from the hospital to the outpatient setting. Coleman and Williams have emphasized that “at the center of this problem lies a lack of understanding of where the responsibility of the hospital ends and the outpatient physician assuming care begins.”9
The alerts sent to providers and staff competed for their attention with other messages in their EHR in-boxes. It is well established that excessive numbers of alerts produced by clinical decision support systems may cause healthcare providers to suffer “alert fatigue” and pay less attention to or even ignore alerts, limiting the effectiveness of EHR-based interventions.17, 18 This effect may be further exacerbated when alerts display inappropriately, leading to reduced user response and inattention.19 Although the system tested in the present study avoided sending alerts when follow-up visits with the primary care physician had already been scheduled, alerts may have been sent when patients were not discharged to home (e.g., to skilled nursing facilities), and did not require a follow-up visit with the primary care physician. The system was unable to accurately identify these types of discharges prior to the alerts being sent. Similarly, some patients also had follow-up visits scheduled with specialists such as oncologists, cardiologists, or pulmonologists. Under this circumstance a follow-up visit with the primary care physician may be considered redundant and unnecessary.
Over half of Medicare patients readmitted to the hospital within 30 days have no outpatient contact with a physician.10 We developed our intervention hypothesizing that timely post-discharge follow-up with a primary care physician would have a powerful protective effect against rehospitalization. However, the value of a post-discharge follow-up visit remains uncertain. Targeting the highest risk patients for prompt follow-up with an outpatient provider may be the most important consideration to enhance the value of such visits. Some have argued for “a tiered approach whereby patients are assigned a hospital readmission [risk] score at the time of discharge that then determines the timing of their follow-up appointment.”9, 20 This approach might also limit the adverse impact of automatic and universal follow-up visits for all discharged patients resulting in overfilled schedules for primary care providers, thus limiting access for other patients.
The results of our efforts, while disappointing in many respects, provide some valuable insights that may inform the design and testing of future interventions. Our intervention, while technologically complex, was relatively simplistic in its execution, and targeted primary care providers and their staff exclusively. Most EHRs now incorporate patient portals providing the opportunity to directly engage patients and caregivers. Although evidence is limited as to the potential of patient portals to empower patients and improve quality of care,21 there is increasing enthusiasm relating to this approach for involving patients more fully in their care.22
We feel that the EHR with clinical decision support is an important tool that can be employed to deliver multifaceted interventions to improve care transitions and reduce risk of rehospitalization in older patients. However, improved identification of which patients are at greatest risk for rehospitalization, a more sophisticated understanding of the value of a follow-up visit and its timing with a primary care provider, and enhanced engagement of patients and caregivers will be essential to the design and testing of future EHR-based transitional care interventions.
Acknowledgments
We would like to give special thanks to Donna Curboy and Paul Lavallee for software development efforts relating to the EHR-transitional care intervention described in this paper.
Funding source: This study was funded by grant R18 HS017203 from the Agency for Healthcare Research and Quality (AHRQ). Dr. Cutrona is supported by Award Number KL2RR031981 from the National Center for Research Resources (NCRR) of the National Institutes of Health (NIH).
Sponsor's Role: The sponsor was not involved in the study design, methods, subject recruitment, data collections, analysis, or preparation of the paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Footnotes
Trial Registration: The study was registered with ClinicalTrials.gov (NCT00611091).
This work was presented in at the 2013 Annual Scientific Meeting of the American Geriatrics Society on May 3, 2013 in Grapevine, Texas.
Author Contributions: Jerry H. Gurwitz, Terry S. Field, Jessica Tjia, and Lawrence Garber contributed to conception and design, acquisition of data, analysis and interpretation of data, as well as drafting and revising the article critically for important intellectual content.
Jessica Ogarek, Jennifer L. Donovan, Abir O. Kanaan, George Reed, Sarah L. Cutrona, Shawn J. Gagne, Peggy Preusse, and Leslie R. Harrold contributed to acquisition of data, analysis and interpretation of data, and revising the article critically for important intellectual content.
References
- 1.Berenson RA, Paulus RA, Kalman NS. Medicare's readmissions-reduction program--a positive alternative. N Engl J Med. 2012;366:1364–1366. doi: 10.1056/NEJMp1201268. [DOI] [PubMed] [Google Scholar]
- 2.Joynt KE, Jha AK. Thirty-day readmissions--truth and consequences. N Engl J Med. 2012;366:1366–1369. doi: 10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 3.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 6.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanaan AO, Donovan JL, Duchin NP, et al. Adverse drug events after hospital discharge in older adults: Types, severity, and involvement of beers criteria medications. J Am Geriatr Soc. 2013;61:1894–1899. doi: 10.1111/jgs.12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5:392–397. doi: 10.1002/jhm.666. [DOI] [PubMed] [Google Scholar]
- 9.Coleman EA, Williams MV. Executing high-quality care transitions: A call to do it right. J Hosp Med. 2007;2:287–290. doi: 10.1002/jhm.276. [DOI] [PubMed] [Google Scholar]
- 10.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 11.Phillips CO, Wright SM, Kern DE, et al. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: A meta-analysis. JAMA. 2004;291:1358–1367. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 12.Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: A systematic review. Ann Intern Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 13.Sheehy AM, Graf B, Gangireddy S, et al. Hospitalized but not admitted: characteristics of patients with “observation status” at an academic medical center. JAMA Intern Med. 2013;173:1991–1998. doi: 10.1001/jamainternmed.2013.8185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 15.Field TS, Garber L, Gagne SJ, et al. Technological resources and personnel costs required to implement an automated alert system for ambulatory physicians when patients are discharged from hospitals to home. Inform Prim Care. 2012;20:87–93. doi: 10.14236/jhi.v20i2.29. [DOI] [PubMed] [Google Scholar]
- 16.Tjia J, Field TS, Garber LD, et al. Development and pilot testing of guidelines to monitor high-risk medications in the ambulatory setting. Am J Manag Care. 2010;16:489–496. [PubMed] [Google Scholar]
- 17.Schreiber R, Knapp J. Premature condemnation of clinical decision support as a useful tool for patient safety in computerized provider order entry. J Am Geriatr Soc. 2009;57:1941–1942. doi: 10.1111/j.1532-5415.2009.02465.x. [DOI] [PubMed] [Google Scholar]
- 18.Kesselheim AS, Cresswell K, Phansalkar S, et al. Clinical decision support systems could be modified to reduce ‘alert fatigue’ while still minimizing the risk of litigation. Health Aff (Millwood) 2011;30:2310–2317. doi: 10.1377/hlthaff.2010.1111. [DOI] [PubMed] [Google Scholar]
- 19.Eslami S, Abu-Hanna A, de Keizer NF. Evaluation of outpatient computerized physician medication order entry systems: A systematic review. J Am Med Inform Assoc. 2007;14:400–406. doi: 10.1197/jamia.M2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Donze J, Aujesky D, Williams D, et al. Potentially avoidable 30-day hospital readmissions in medical patients: Derivation and validation of a prediction model. JAMA Intern Med. 2013;173:632–638. doi: 10.1001/jamainternmed.2013.3023. [DOI] [PubMed] [Google Scholar]
- 21.Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: A systematic review of controlled trials. J Med Internet Res. 2012;14:e162. doi: 10.2196/jmir.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palen TE, Bayliss EA, Steiner JF. Are patient portals one key to unlocking the door for engaging patients in their healthcare? J Comp Eff Res. 2013;2:99–101. doi: 10.2217/cer.13.8. [DOI] [PubMed] [Google Scholar]