Abstract
Objectives:
The aim of this study was to compare the effect on self-rated pain, disability, and self-efficacy of 3 interventions for the management of chronic whiplash-associated disorders: physiotherapist-led neck-specific exercise (NSE), physiotherapist-led NSE with the addition of a behavioral approach, or Prescription of Physical Activity (PPA).
Materials and Methods:
A total of 216 volunteers with chronic whiplash-associated disorders participated in this randomized, assessor blinded, clinical trial of 3 exercise interventions. Self-rated pain/pain bothersomeness (Visual Analogue Scale), disability (Neck Disability Index), and self-efficacy (Self-Efficacy Scale) were evaluated at baseline and at 3 and 6 months.
Results:
The proportion of patients reaching substantial reduction in pain bothersomness (at least 50% reduction) was more evident (P<0.01) in the 2 NSE groups (29% to 48%) compared with the PPA group (5%) at 3 months. At 6 months 39% to 44% of the patients in the 2 neck-specific groups and 28% in the PPA group reported substantial pain reduction. Reduction of disability was also larger in the 2 neck-specific exercise groups at both 3 and 6 months (P<0.02). Self-efficacy was only improved in the NSE group without a behavioral approach (P=0.02). However, there were no significant differences in any outcomes between the 2 physiotherapist-led NSE groups.
Discussion:
NSE resulted in superior outcomes compared with PPA in this study, but the observed benefits of adding a behavioral approach to the implementation of exercise in this study were inconclusive.
Key Words: chronic, whiplash, exercise, disability, pain
One year after injury 50% of people with whiplash-associated disorders (WAD) still report neck pain,1 but effective treatment remains a scientific gap of knowledge.2 One factor attributed to the persistence of symptoms in individuals with WAD is deconditioned neck muscles that may affect the physical support of the cervical vertebral column.3 Studies have shown characteristic morphologic changes in the cervical muscles of patients with WAD,4,5 as well as altered muscle behavior6–10 and reductions in strength and endurance.11 On the basis of such findings there are some recommendations that patients with WAD undertake neck-specific exercise to condition their cervical muscles.12
Despite clinical recommendations, however, there is as yet no clear evidence of benefit from any conservative management of chronic WAD, including neck-specific exercise.2,13 As a consequence there is uncertainty as to the optimal exercise approach.14 One approach that is commonly used and recommended in Sweden is the concept of the Prescription of Physical Activity (PPA). Similar approaches are recommended in several countries for a variety of diagnoses, including chronic pain, and involve patients undertaking self-directed general physical activity outside the health care system.15 However, although physical activity in general is reported to result in positive pain reduction and improved function in some chronic pain states,15,16 there is no evidence for its benefit in the management of mechanical neck disorders.17 General physical activity approaches also do not specifically address the known cervical muscle impairments in WAD.4,5 In addition, there is some evidence that a supervised specific neck/shoulder exercise approach in patients with subacute WAD may result in better pain reduction than unsupervised exercise (as is the emphasis in the PPA approaches).18
Furthermore, there is clear evidence of the effectiveness of neck-specific exercise in the management of chronic nonspecific neck pain,19–22 and it has been reported to be effective in reducing neck pain in fighter pilots with repeated whiplash-like exposure.23
Considering that chronic neck disorders such as WAD may involve a variety of symptoms with overlap between both physical and psychosocial contributing factors,24 it is reasonable to assume that the incorporation of a behavioral approach to neck-specific exercise, such as implemented for chronic low back pain,25 may result in better outcomes in response to neck-specific exercise for patients with chronic WAD. For example, a behavioral approach may moderate the detrimental impact some psychological factors may have on the success of exercise, such as low self-efficacy (SE), which can be a predictor of total pain behavior26 as well as a predictor of persistent disability or reduced health-related quality of life in acute27 and subacute28 WAD. Although previous studies have combined neck exercise and behavioral approaches in the management of chronic WAD, the methodology utilized in these studies (multimodal exercise29 or incorporating neck-specific exercise in a multimodal treatment approach30) unfortunately make it difficult to determine the effect of neck-specific exercise alone, or if any additional benefits of the combined approach were evident.
The aim of this study was to compare the effect on self-rated pain, disability, and SE of 3 interventions in chronic WAD management, grade 2 or 3: physiotherapist-led neck-specific exercise (NSE), physiotherapist-led neck-specific exercise with a behavioral approach (NSEB), or PPA.
We hypothesized that NSE would have a better effect on pain and disability than PPA, and that the addition of the behavioral approach to exercise would result in superior improvements than NSE alone. We have included participants with both WAD classifications grade 2 and 3. We anticipate that this will improve the clinical meaningfulness of the findings as studies rarely include participants classified as WAD grade 3 (with neurological signs)31 despite concomitant upper limb symptoms reported as present in most individuals with chronic WAD,32,33 which could be an indication that neurological signs might be present in some of these individuals.
MATERIALS AND METHODS
Design
This was a multicenter prospective randomized clinical trial with assessor and group allocation blinding. Because of the nature of the interventions participants and physiotherapists were unable to be blinded to the interventions.
Participants and Settings
A total of 216 individuals with chronic WAD participated in the study, including 142 (65%) women and 74 (35%) men with a mean age of 40.5 years (range, 18 to 63 y, SD 11.4 y). Participants were included if they were aged between 18 and 63 years and had experienced a whiplash injury in the preceding 6 to 36 months that was nominated as the cause of current symptoms. To be included in the study participants’ condition had to be classified as WAD grade 2 or 3,31 they had to record a Neck Disability Index (NDI) score34 of at least 10/50 points, and record an average pain on a Visual Analogue Scale (VAS) of >20/100 mm (0=no pain, 100=worst imaginable pain)35 for the preceding week. Participants were excluded if they reported signs of traumatic brain injury (unconsciousness/loss of memory in connection to the whiplash injury), previous neck trauma with unresolved symptoms, neck pain causing >1 month’s work absence in the preceding year before the whiplash injury, myelopathy, spinal infection, or tumor or previous neck surgery. Exclusion was also made if participants reported a more dominant pain elsewhere in the body, or conditions potentially detrimental to completing the study interventions, such as ongoing malignant disease, severe psychiatric disorders, neurological diseases, drug abuse, or insufficient competence of the Swedish language. The interventions were conducted in a primary-care setting with physiotherapists who were experienced in managing neck pain disorders, and all physiotherapist visits were made within the ordinary publicly funded reimbursement system.
Procedure
Potential participants were identified from health care registers of 6 Swedish counties, including primary health care centers, specialist orthopedic clinics, and hospital outpatient services. Participants were screened for eligibility by a 4-step process (Fig. 1). This process included: (1) an initial screening letter (sent to 7950 potential participants) that contained study information, basic inclusion/exclusion criteria (Fig. 1), as well as a NDI34 and pain VAS measure, and a prepaid return envelope; (2) a telephone interview; (3) checking of medical records if uncertainty existed regarding medical history; (4) clinical physical examination by a blinded experienced physiotherapist (mean, 18 y experience) to classify the disorder as either a WAD grade 2 (neck pain and clinical findings) or WAD grade 3 (addition of neurological signs).31 In preparation for the study, test-leaders had practical sessions together to ensure standardized performances of the tests were employed before any participants were recruited. The criteria of neurological signs was met if patients reported arm pain or paresthesia without other known causes, together with at least 2 positive physical examination findings indicating neurological deficit in the same dermatome/myotome.36 In addition, when arm symptoms were present in the supine test position, alteration of symptoms by manual neck traction at the corresponding cervical vertebral levels was also a mandatory finding to further strengthen the assumption that the symptoms were neck induced.
FIGURE 1.
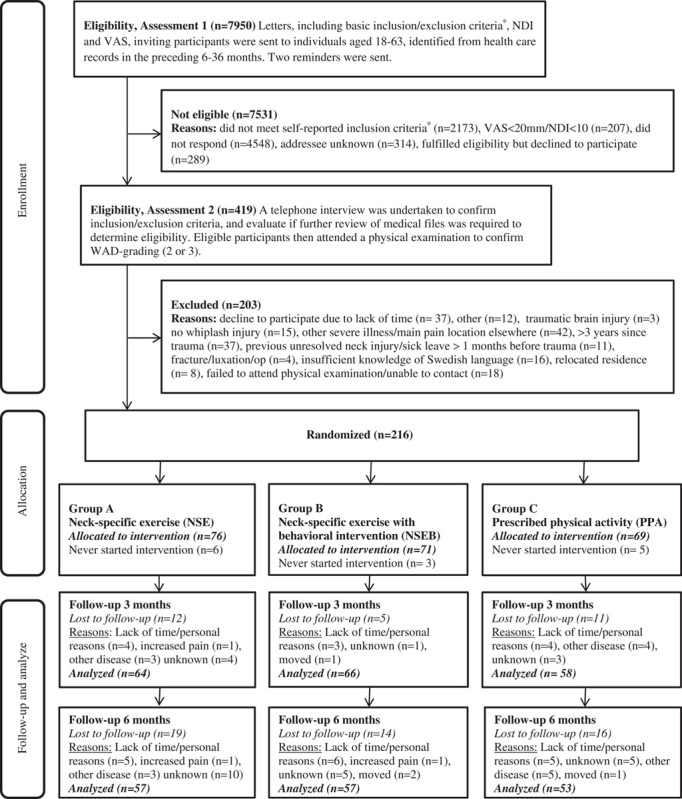
Participant flow through study. *Whiplash injury in the preceding 6 to 36 months, reported to be the onset of current symptoms, excluding unconsciousness/loss of memory in connection to the whiplash injury, previous neck trauma with unresolved symptoms, previous neck surgery, ongoing malignant disease, severe psychiatric disorders, drug abuse, difficulties understanding the Swedish language. NDI indicates Neck Disability Index; VAS, Visual Analogue Scale; WAD, whiplash-associated disorders.
Participants were recruited between February 2011 and May 2012 and all participants received verbal and written information about the study. Informed consent and baseline outcome measurements were collected before allocation. Allocation from a computerized randomization list was made by an independent researcher, who also put the individual results in sealed completely opaque envelopes for further distribution to the treating physiotherapists. The study was approved by the Regional Ethics Committee of Linköping University, Sweden.
Interventions
The physiotherapists conducting the interventions were provided with standardized oral and written information about their interventions, and those in charge of physiotherapist-led exercise interventions received a day of standardized theoretical and practical training from the project leaders. The behavioral approach was designed to be basic and manageable by experienced physiotherapists in primary care with some previous knowledge of behavioral approaches. All physiotherapists were encouraged to become familiar with any of the specific neck exercises that they previously were not implementing by incorporating them into their clinical practice during the 1 month (or more) period before receiving study patients. They were also encouraged to contact project leaders if in need of further guidance throughout the study. All patients were first examined by their treating physiotherapist, and all 3 interventions were undertaken over a 12-week period. Participants were urged to refrain from having any other physical treatments for their neck disorder during the 6 months of participating in this study.
Physiotherapist-led Neck-specific Exercise Group (NSE)
Participants undertook supervised exercise, and received basic information about the musculoskeletal system of the neck, relevant to the exercise. The exercise program consisted of 2 physiotherapy sessions weekly in addition to home exercise. Initially the program focused on daily gentle unresisted isometric cervical flexion, extension and rotation exercises (about 3 sets of 5 repetitions of each exercise daily at home), aimed at facilitating activity of the deep cervical muscle layers. Exercise was then progressed in each direction with low isometric resistance, increasing the exercise parameters toward 3 sets of 10 repetitions in supine and sitting positions in preparation of the forthcoming gym exercise. The importance of good posture was also emphasized to further facilitate deep cervical muscle function.37 Gradually exercise was introduced in the gym with progressive resistance training with a focus on low-load endurance training, using a weighted pulley for head resistance, or guild board. Progression was made to higher repetitions (up to 3 sets of 30 repetitions) within the symptom tolerance. Although a standardized framework of exercises was followed, progression was tailored to each individual according to their symptomatic response and capability. In this manner participants were encouraged to avoid the aggravation of pain as impaired endogenous pain mechanisms are thought to be present in some individuals with chronic WAD, underpinning recommendations to avoid pain provocation in this group.38 If considered appropriate for an individual, the exercise program could also include exercise for the lower back, abdomen, and scapulae, as well as stretching exercises. Toward the end of the 12-week exercise period participants were encouraged to continue exercise in the home by providing them with resistive exercise bands and a written individualized exercise program also including prescription of general physical activity (Fig. 2).
FIGURE 2.
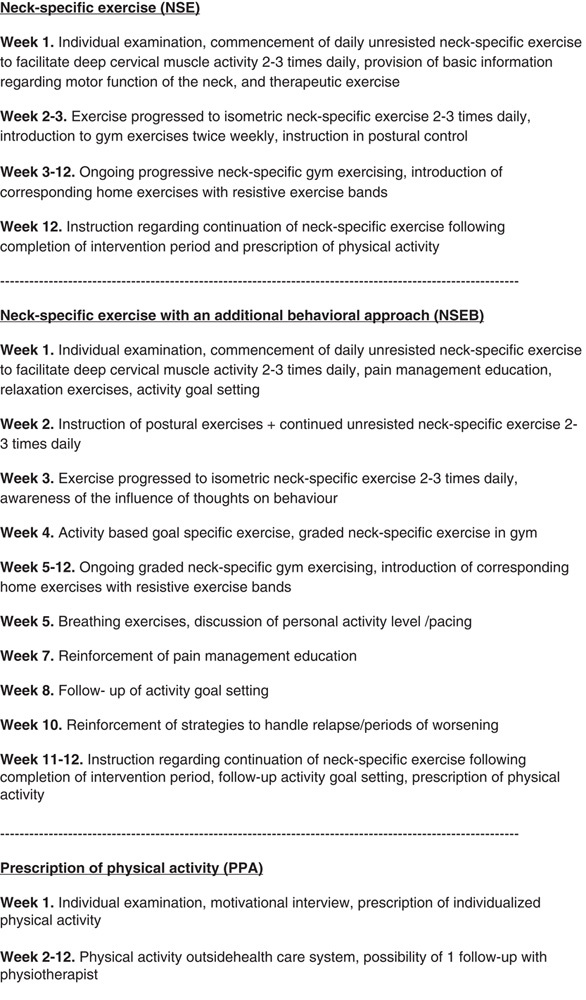
Timeframe of specific components of interventions.
Physiotherapist-guided Neck-specific Exercise Group With a Behavioral Approach (NSEB)
The protocol of exercises in the NSEB group was the same as that undertaken by the NSE group; however, it was initially progressed slower to accommodate the additional behavioral component. In accordance with the concept of graded exercise, patients were encouraged not to focus on temporary increases in neck pain. Furthermore, patients were encouraged to take responsibility for the exercise progression, with the physiotherapist acting as a coach, in an operant-conditioning behavioral approach, focusing on success in exercise progression.39
They also received basic behavioral intervention training, led by the physiotherapist. The behavioral intervention included oral education regarding physiological and psychological aspects of pain, as well as activities aimed at pain management and problem-solving, including the management of symptomatic relapses (Fig. 2). Patients were encouraged to consider what they learnt and practice relevant pain management skills, for instance relaxation exercises, at home between sessions.
Prescription of Physical Activity Group (PPA)
The concept of PPA is based on the patient receiving a written prescription of physical activity, just like a prescription of medication, to be performed outside the health care system.15 Participants in this group first had a short motivational interview conducted by the physiotherapist, and based on the discussions within the interview and the subsequent physical examination, were prescribed individualized physical activity. The purpose of this prescription was to increase overall physical activity, either with individualized home exercise or activities performed in public gyms, or elsewhere, outside the health care system. Individualized exercise is suggested to enhance exercise adherence.40 Neck-specific exercises including any form of head resistance were not prescribed. One follow-up visit or phone call was encouraged. And consistent with the approach taken with the NSE and NSEB groups, participants were encouraged to continue exercising after the 12-week intervention was over.
Outcome Measures
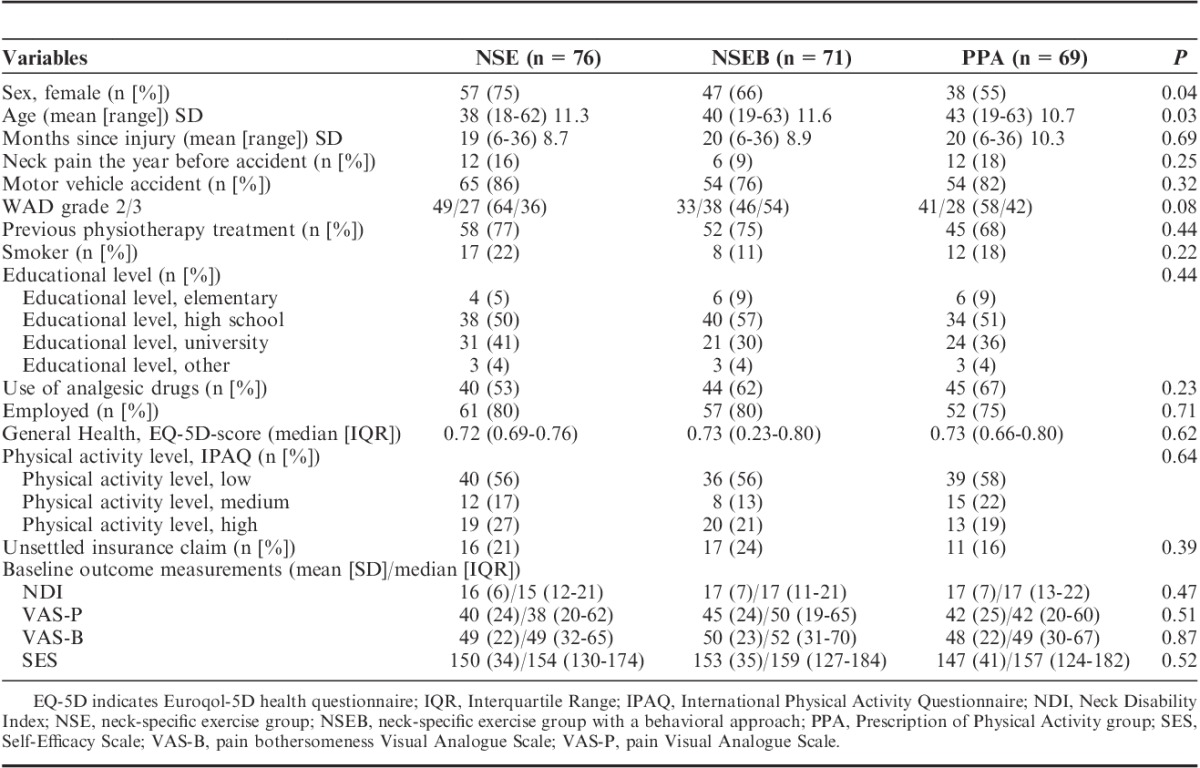
Background variables including generic data, self-reported general health measured with the Euroqol 5-D instrument,41 and activity level, measured with the International Physical Activity Questionnaire,42 are presented in Table 1. All outcome measures were collected at baseline and after 3 and 6 months following commencement of the intervention. All outcome measures were collected and registered by research staff blinded to intervention group allocation. Patients completed questionnaires at home.
TABLE 1.
Background Variables of Participants
Disability
The primary outcome measurement (in accordance with previously published protocol on Clinical Trials.gov, no NCT01528579) was the NDI.34,43 The NDI consists of 10 items grading neck disability from 0 (no activity limitations) to 5 (major activity limitations) with a total maximum score of 50 points34 with a higher score representing a higher level of disability. The NDI is widely used, is reported to be reliable (intraclass correlation coefficient up to 0.98) and valid measurement of disability in neck pain disorders.43 The Minimal Clinical Important Difference of the NDI score is suggested to be 3.5 to 5/50 points,34 with a reduction of 5 set as the cutoff score defining a positive responder (clinically relevant improvement in disability) in this study. To make sure the cutoff value exceeded the measurement error in this study population, Minimum Detectable Change was calculated as previously done in other neck pain populations,44 using the NDI scores from both the inquiry letters, and baseline questionnaire from 5 counties (n=150), rendering a Minimal Detectable Change of 3.3/50 points.
Pain
Pain was recorded in terms of current neck pain intensity, measured with a Pain VAS (anchored by 0=no pain, 100=worst imaginable pain)35 and pain bothersomeness, recorded for the preceding 24 hours (anchored by 0=not bothersome at all, 100=extremely bothersome). Pain bothersomeness has been shown to be more responsive than pain intensity in individuals with WAD.45 The Initiative on Methods, Measurement and Pain Assessment in Clinical Trials (IMMPACT) also recommend reporting the proportion of patients achieving a certain degree of pain relief. A reduction in pain intensity of ≥50% is suggested to indicate substantial improvements, or treatment success,46 and was used in this study to define a positive responder regarding pain. Patients also recorded if they used analgesics to manage their neck pain (yes/no).
Self-Efficacy
The participants’ confidence in their ability to perform activities despite their pain was evaluated using the Self-Efficacy Scale (SES).47,48 SES is a reliable instrument in WAD populations24,49 consisting of 20 different physical and psychosocial activity items (from 0=not confident at all, to 10=very confident), thus generating a total score from 0 to 200.
Intervention Compliance and Other Interventions
Completion rate of recommended exercise (at least 50% attendance to the intervention sessions) was collected from the physiotherapists and from participant exercise diaries (PPA group). Patients were also asked about any neck-related treatments outside the study protocol.
Statistics and Data Management
The required sample size was determined on the basis of the expected difference between groups for main outcome, NDI (3.5/50, SD 7), for the 3 groups with an α-level of 5% and a power goal of 80%, allowing for 10% drop-outs, rendering a sample size of 216. If only 1 item of data for the NDI (or 2 data items for the SES) were missing, these missing data points were substituted by the average item score of the questionnaire for that participant. If more data were missing, that particular score was omitted from the analysis. The primary analysis was made on an intention-to-treat basis, but including all patients completing each measurement. Descriptive statistics were calculated, and a repeated-measures analysis of variance was used to evaluate within-group comparisons, with Mauchly or Greenhouse-Geisser correction depending on sphericity. Between-group comparisons were evaluated with a 1-way analysis of variance with Tukeys correction for post hoc tests. All outcomes were normally distributed. In binary outcomes χ2 tests were used.
To determine the proportion of responders to treatment in each group, a subanalysis of patients with at least 50% exercise compliance was conducted. Cutoff values were used for primary disability and pain outcomes as previously described. Significance level was set at P<0.05. SPSS version 20 (SPSS Inc., Chicago, IL) was used for all statistical analysis.
RESULTS
Of the total 216 participants included in the study, 122 (57%) were classified as WAD grade 2 and 94 (43%) as grade 3. Apart from a slight difference in age and sex there were no differences between the 3 intervention groups at baseline (Table 1). There was no correlation between age (all rs<0.11, P>0.19), sex (all rs<0.12, P>0.09), and any of the outcomes. Patients with WAD grade 3 reported more baseline disability (NDI +2.5, P<0.01) and current pain (VAS +8, P=0.02) than those with grade 2. The drop-out rate at the 3-month-follow-up was 12%, and 20% at 6 months.
Disability
Disability levels in both the NSE and NSEB groups significantly improved (NDI, P<0.01/<0.001) over time with no improvement observed for the PPA group. When separating WAD grades, the results did not change (P<0.05). There were significant changes between groups in disability at the 3-month follow-up (NDI, P=0.02) where the PPA group had less improvements than the NSE/NSEB groups. At 6 months the difference remained significant. There was no significant difference between the NSE and NSEB groups (Table 2).
TABLE 2.
Change Scores From Baseline to 3 and 6 Months
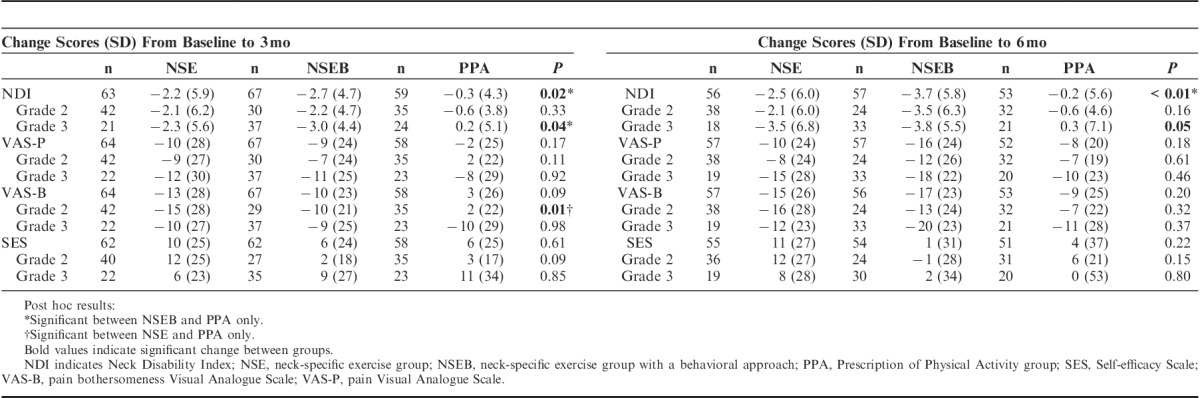
With regard to the proportion of responders as indicated by change in NDI score, there was no significant difference between groups (P=0.23) in the proportion of responders at 3 months (40% NSE, 43% NSEB, 21% PPA), however, at 6 months the difference was significant (P=0.02) between groups (28% NSE, 54% NSEB, and 21% PPA) (Fig. 3).
FIGURE 3.
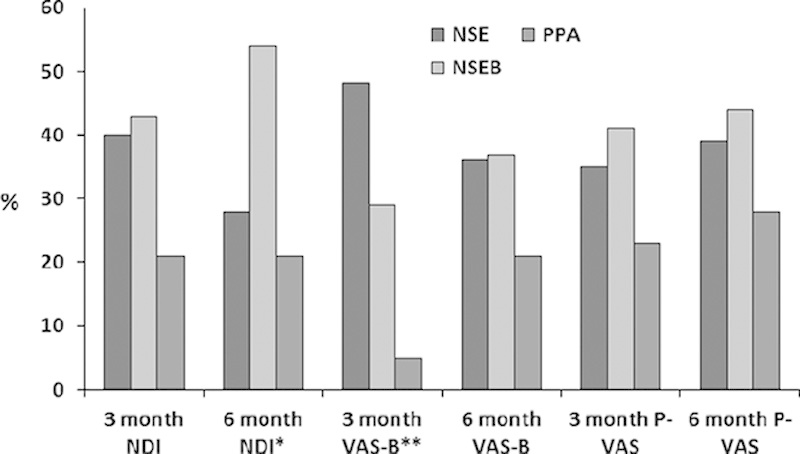
Proportion of responders to treatment in the 3 intervention groups. The proportion of responders reaching clinical important difference in the Neck Disability Index (NDI, cutoff change of ≥5/50), Visual Analogue Scale Bothersomeness (VAS-B, ≥50% reduction), Current Pain Visual Analogue Scale (P-VAS, ≥50% reduction) at the 3- and 6-month follow-up periods is presented. Significant difference between groups at *P=0.02, **P=0.004. NSE indicates neck-specific exercise group; NSEB, neck-specific exercise group with a behavioral approach; PPA, Prescription of Physical Activity group.
Pain
Pain bothersomeness was significantly reduced over time in all the 3 groups (NSE and NSEB, P<0.001; PPA, P=0.04) and between-group differences were only observed between the NSE/NSEB groups and the PPA group for participants with WAD grade 2 (P=0.01) at 3 months but not 6 months. Current pain was also reduced in all 3 groups (NSE, P=0.001; NSEB, P≤0.001; PPA, P=0.04), but between-group differences were not evident at either 3 or 6 months (Table 2).
With regard to substantial reduction in pain bothersomeness, there were significantly more responders in the NSE groups, NSE/NSEB, compared with the PPA group (P<0.01, NSE 48%, NSEB 29%, PPA 5%), but not current pain (P=0.39, NSE 35%, NSEB 41%, PPA 22%) at 3 months. The differences were not significant at 6 months for either the pain bothersomeness (P=0.44, NSE 36%, NSEB 37%, PPA 17%) or current pain (P=0.51, NSE 39%, NSEB 44%, PPA 28%) measures (Fig. 3).
There was a difference in the proportion of participants reporting use of analgesic drugs due to neck pain (P=0.05) where the PPA group had the highest proportion of users (NSE 40% [n=26], NSEB 55% [n=37], and PPA 62% [n=37]) at 3 months. At 6 months significantly fewer patients (P=0.03) in both the NSE (42% [n=24)] and NSEB groups [41% n=23]) still reported using analgesic drugs than those in the PPA group (64% [n=33]).
Self-Efficacy
SE improved only in the NSE group (P=0.02) but only for those with WAD grade 2 (P<0.01). There were no between-group differences.
Intervention Compliance and Other Treatments
At the 3-month follow-up, compliance (at least 50% attendance to the intervention sessions) was 70% and 71% in the NSE and NSEB group, respectively. In the PPA group 50% of patients reported compliance to their prescribed physical activity (P=0.07). Compliance at 6 months was rated at 52%, 55%, and 50% in the NSE, NSEB, and PPA groups, respectively (P=0.90). At 6 months 3 patients in the NSE, 4 in the NSEB, and 7 in the PPA groups reported having received additional care from physiotherapists/chiropractors elsewhere (P=0.20).
DISCUSSION
Taking all measurements into consideration this study indicates that supervised neck-specific exercise with, or without a behavioral approach, may have greater clinical benefits than the PPA for patients with chronic WAD. Both neck-specific exercise interventions (NSE and NSEB) resulted in significantly greater changes in disability compared with the PPA group. These improvements were particularly evident after the first 3 months of intervention. Although group differences in pain measurements were less robust, the use of analgesic drugs was significantly lower in the 2 NSE groups at 6 months compared with the PPA group. In addition, the proportion of patients achieving substantial reduction in pain bothersomeness was also greater in the 2 NSE groups at 3 months, albeit not significantly so at 6 months. The findings of this study therefore support our hypothesis and clinical proposition that neck-specific exercise may be more beneficial than PPA for the management of patients with chronic WAD.
However, the results do not support our hypothesis that the addition of a behavioral approach would result in greater benefits than NSE alone, even though there was a trend toward better results for the NSEB group, especially regarding disability at 6 months. It was surprising, however, to find that only patients in the NSE group demonstrated a significant improvement in SE. A subgroup analysis excluding those with <50% compliance did not alter this relationship, even though mean improvements were somewhat higher in all groups in this subanalysis. A possible explanation could be that in contrast to the NSEB group, exercise in the NSE group was supposed to be pain-free and they had fewer tasks to focus on, which may have been successful factors in boosting their mastery experience during the study period. Mastery experience is reported to be the strongest influence on SE belief, enabling a person to succeed in increasingly challenging performances of a behavior that is attainable and desired.50 Although this is an interesting finding it should also be acknowledged that the difference between groups in SE was insignificant, and behavioral approaches vary. Although all physiotherapists had some knowledge of behavioral approaches before involvement in the study, we do acknowledge that results may have been different with physiotherapists specialized in incorporating more advanced behavioral approaches, or if a different behavioral approach was utilized.
This study, to our knowledge, is also the first study to report the effects of exercise on participants with WAD grade 2 and 3 separately. The findings suggest that there is a tendency for those with grade 3 to benefit more than those with grade 2 from NSE with or without a behavioral approach. On the basis that participants classified as WAD grade 3 had more baseline pain and disability our findings are in accordance with previous findings that show supervised exercise to be more effective for those with higher baseline neck pain and disability.29 There were no significant improvements for those with grade 3 in the PPA group.
From a clinical perspective although the changes observed in this study were statistically significant, the mean reductions in pain and disability are relatively modest. However, in heterogeneous population like chronic WAD, variable responses to an intervention may be expected and central tendency analysis may not give enough information to be clinically meaningful.51 In addition, criteria for clinically important changes in individuals cannot be extrapolated to the evaluation of group differences.52 We addressed this by analyzing the proportion of patients achieving a clinically meaningful positive response with main outcomes to provide information beyond group mean differences alone.52 Examining the data in this manner may thus give a stronger indication of treatment success and may be more informative to clinical practice than mean group differences that have potential wash-out effects. The results of this study clearly demonstrate that even though mean group reductions were fairly modest, well over a third of the patients in the NSE/NSEB groups and over 21% of those in the PPA group had reached substantial reduction in pain/pain bothersomeness at 6 months. Pain reduction is one of the most important outcomes to people with chronic pain53 and taking into account that little change can be expected after 3 months’ duration in chronic WAD,31,54 the results of this study are promising. They indicate that all 3 interventions can be effective to a fair proportion of individuals, even though the NSE interventions (NSE/NSEB) seem more likely to be of benefit. Different cutoff values for clinical important changes in NDI have been presented in the literature, and the result may have been different with another cutoff value. However, the cutoff value of 5 used in this study has previously been used and recommended34 and exceeded measurement error in this study.
There were more women than men in this study, which is consistent with the general WAD population.55 Analysis of individuals that fulfilled the criteria, but declined to participate in this study showed that the study sample was well representative in age, sex, and level of pain (declined to participate, mean age 39 [SD 17], sex female 62%, VAS 45 [SD 24]), but those who declined reported somewhat more disability (NDI 22 [SD 17]) than the study sample. As those with more disability previously have been reported to benefit more29 it is not unlikely that the results would be at least equally promising in the whole population.
Limitations
A multicenter study such as this involving multiple intervening therapists offers less control and may potentially compromise performance of the intended interventions. We attempted to minimize this by ensuring that the physiotherapists were trained and practiced the standardized interventions in preparation for the study. Also, results from such a multicenter study may be more generalizable to physiotherapy practice in a range of primary-care settings and may also enhance implementation.
The study sample size was not calculated for subgrouping, and differences between subgroups (ie, WAD grade 2 and 3) may therefore be underpowered to detect other possible differences than those presented between intervention groups. Despite this, the power was stronger and the significant improvement in disability was larger in patients with WAD grade 3 compared with grade 2. However, possible differences between grades regarding response to different exercise treatments needs to be further investigated in future studies.
Regarding statistics, imputation of data may produce an overconservative estimate of treatment effect, but the choice not to impute data, as in this study, may cause selection bias instead. However, there was no difference in the baseline outcomes (NDI, P=0.12; pain VAS, P=0.50; and VAS bothersomeness, P=0.64) between participants who dropped out and those who completed. There was a small, but significant difference in age and sex between groups, but no significant correlation between age or sex and any of the outcomes, and when incorporated into the analysis these variables did not alter the results. Being female has been associated with worse prognosis,1,55 yet the group with the highest proportion of women (NSE) still did better than the group with the lowest proportion (PPA).
Consistent with the concept, participants in the PPA group only had 1 to 2 physiotherapist visits, which may have influenced the results, as the other 2 groups had regular physiotherapist contact. All patients, however, also visited blinded experienced physiotherapists (project leaders) 3 times for other tests, and were all encouraged to keep exercising in accordance with the guidelines given by their treating physiotherapist. Compliance was somewhat lower at 3 months in the PPA group which may have been partly due to a greater amount of missing exercise data for this group. Some patients may have felt that the PPA intervention was less direct and specific to their problem and may have been less motivated. However, others may have preferred unspecific approaches in fear of overloading their neck. Expectations of the 3 interventions were similar at baseline and there was no difference between groups regarding fulfillment of expectations at 6 months (76 to 85 on a 100 mm VAS scale, P=0.64). In the analysis of responders, only those with at least 50% compliance were included, and the outcomes were still better in the 2 neck-specific groups.
Clinician treatment preferences has previously failed to show any moderation of treatment effect in chronic WAD56 and the physiotherapists were selected and matched to work within their field of interest and knowledge as much as possible. Our aim was to use a protocol that would be manageable by experienced physiotherapists in primary care, and thus also possible to implement in clinical care without major changes. However, 1 session of education in neck-specific exercise may have been inadequate for some physiotherapists to manage this skill optimally, even though they were used to handling neck pain patients. We did attempt to minimize this by allowing at least a month to practice before commencing the study and permitting advice to be sought from project leaders throughout the study period.
Considering the heterogeneity of chronic WAD populations even within the Quebec Task Force classification,31 both in physical and psychosocial manifestations, it is unlikely that any 1 treatment will suit all, but in this study there are clear indications that NSE with, or without a behavioral approach, may be appropriate for a number of these individuals. Future studies will need to be undertaken to predict which patients will benefit more from which kind of exercise approach. These studies will also have to consider the cost-effectiveness of these interventions as PPA in itself is a much cheaper intervention. There is also a need to explore whether individuals with chronic WAD grades 2 and 3 may need different rehabilitation approaches, including exercise.
CONCLUSIONS
Physiotherapist-led NSE resulted in superior outcomes compared with PPA in this chronic WAD population. The observed benefits of adding a behavioral approach to the implementation of exercise in this study were inconclusive.
ACKNOWLEDGMENTS
The authors thank all the participants in this study, including WAD participants, physiotherapists, and staff involved at any stage of the study.
Footnotes
Supported by funding from the Swedish government through the Swedish Research Council in cooperation with the Swedish Social Insurance Agency through the REHSAM foundation Stockholm, Sweden, and the regional Centers for Clinical Research of Östergötland, Linköping, Sweden and Sörmland, Uppsala, Sweden County Councils. A.P. is supported by the Swedish Research Council, Stockholm, Sweden. S.O.L. is supported by a Health Practitioner Research Fellowship (Queensland Health and the University of Queensland, Brisbane, Australia [NHMRC CCRE Spinal Pain, Injury and Health]). The authors declare no conflict of interest.
REFERENCES
- 1.Carroll LJ, Holm LW, Hogg-Johnson S, et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 2008;33supplS83–S92. [DOI] [PubMed] [Google Scholar]
- 2.Verhagen AP, Scholten-Peeters GG, van Wijngaarden S, et al. Conservative treatments for whiplash. Cochrane Database Syst Rev. 2007;2:CD003338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayoux-Benhamou MA, Revel M, Vallee C, et al. Longus colli has a postural function on cervical curvature. Surg Radiol Anat. 1994;16:367–371. [DOI] [PubMed] [Google Scholar]
- 4.Elliott JM. Are there implications for morphological changes in neck muscles after whiplash injury? Spine (Phila Pa 1976). 2011;36supplS205–S210. [DOI] [PubMed] [Google Scholar]
- 5.Elliott JM, Pedler AR, Jull GA, et al. Differential changes in muscle composition exist in traumatic and nontraumatic neck pain. Spine (Phila Pa 1976). 2014;39:39–47. [DOI] [PubMed] [Google Scholar]
- 6.Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther. 2004;9:89–94. [DOI] [PubMed] [Google Scholar]
- 7.Nederhand MJ, Hermens HJ, IJzerman MJ, et al. Cervical muscle dysfunction in chronic whiplash-associated disorder grade 2: the relevance of the trauma. Spine (Phila Pa 1976). 2002;27:1056–1061. [DOI] [PubMed] [Google Scholar]
- 8.Woodhouse A, Vasseljen O. Altered motor control patterns in whiplash and chronic neck pain. BMC Musculoskelet Disord. 2008;9:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sterling M, Jull G, Vicenzino B, et al. Development of motor system dysfunction following whiplash injury. Pain. 2003;103:65–73. [DOI] [PubMed] [Google Scholar]
- 10.Falla D, Bilenkij G, Jull G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine (Phila Pa 1976). 2004;29:1436–1440. [DOI] [PubMed] [Google Scholar]
- 11.O’Leary S, Jull G, Kim M, et al. Cranio-cervical flexor muscle impairment at maximal, moderate, and low loads is a feature of neck pain. Man Ther. 2007;12:34–39. [DOI] [PubMed] [Google Scholar]
- 12.Seferiadis A, Rosenfeld M, Gunnarsson R. A review of treatment interventions in whiplash-associated disorders. Eur Spine J. 2004;13:387–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 2008;33supplS123–S152. [DOI] [PubMed] [Google Scholar]
- 14.Teasell RW, McClure JA, Walton D, et al. A research synthesis of therapeutic interventions for whiplash-associated disorder (WAD): part 4 - noninvasive interventions for chronic WAD. Pain Res Manag. 2010;15:313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Professional Associations for Physical Activity Sweden, Physical Activity in the Prevention and Treatment of Disease. 2010Stockholm: Swedish National Institute of Public Health; Available at: http://www.fyss.se/fyss-in-english/. [Google Scholar]
- 16.Sullivan AB, Scheman J, Venesy D, et al. The role of exercise and types of exercise in the rehabilitation of chronic pain: specific or nonspecific benefits. Curr Pain Headache Rep. 2012;16:153–161. [DOI] [PubMed] [Google Scholar]
- 17.Kay TM, Gross A, Goldsmith CH, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2012;8:CD004250. [DOI] [PubMed] [Google Scholar]
- 18.Bunketorp L, Lindh M, Carlsson J, et al. The effectiveness of a supervised physical training model tailored to the individual needs of patients with whiplash-associated disorders—a randomized controlled trial. Clin Rehabil. 2006;20:201–217. [DOI] [PubMed] [Google Scholar]
- 19.Ylinen J, Nikander R, Nykanen M, et al. Effect of neck exercises on cervicogenic headache: a randomized controlled trial. J Rehabil Med. 2010;42:344–349. [DOI] [PubMed] [Google Scholar]
- 20.Chiu TT, Lam TH, Hedley AJ. A randomized controlled trial on the efficacy of exercise for patients with chronic neck pain. Spine (Phila Pa 1976). 2005;30:E1–E7. [PubMed] [Google Scholar]
- 21.Ylinen J, Takala EP, Nykanen M, et al. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA. 2003;289:2509–2516. [DOI] [PubMed] [Google Scholar]
- 22.Falla D, Jull G, Hodges P, et al. An endurance-strength training regime is effective in reducing myoelectric manifestations of cervical flexor muscle fatigue in females with chronic neck pain. Clin Neurophysiol. 2006;117:828–837. [DOI] [PubMed] [Google Scholar]
- 23.Lange B, Toft P, Myburgh C, et al. Effect of targeted strength, endurance, and coordination exercise on neck and shoulder pain among fighter pilots: a randomized-controlled trial. Clin J Pain. 2013;29:50–59. [DOI] [PubMed] [Google Scholar]
- 24.Soderlund A, Denison E. Classification of patients with whiplash associated disorders (WAD): reliable and valid subgroups based on the Multidimensional Pain Inventory (MPI-S). Eur J Pain. 2006;10:113–119. [DOI] [PubMed] [Google Scholar]
- 25.Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147:492–504. [DOI] [PubMed] [Google Scholar]
- 26.Asghari A, Nicholas MK. Pain self-efficacy beliefs and pain behaviour. A prospective study. Pain. 2001;94:85–100. [DOI] [PubMed] [Google Scholar]
- 27.Kyhlback M, Thierfelder T, Soderlund A. Prognostic factors in whiplash-associated disorders. Int J Rehabil Res. 2002;25:181–187. [DOI] [PubMed] [Google Scholar]
- 28.Bunketorp L, Lindh M, Carlsson J, et al. The perception of pain and pain-related cognitions in subacute whiplash-associated disorders: its influence on prolonged disability. Disabil Rehabil. 2006;28:271–279. [DOI] [PubMed] [Google Scholar]
- 29.Stewart MJ, Maher CG, Refshauge KM, et al. Randomized controlled trial of exercise for chronic whiplash-associated disorders. Pain. 2007;128:59–68. [DOI] [PubMed] [Google Scholar]
- 30.Soderlund A, Lindberg P. Cognitive behavioural components in physiotherapy management of chronic whiplash associated disorders (WAD)—a randomised group study. G Ital Med Lav Ergon. 2007;29suppl AA5–A11. [PubMed] [Google Scholar]
- 31.Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on whiplash-associated disorders: redefining “whiplash” and its management. Spine (Phila Pa 1976). 1995;20suppl1S–73S. [PubMed] [Google Scholar]
- 32.Bunketorp L, Nordholm L, Carlsson J. A descriptive analysis of disorders in patients 17 years following motor vehicle accidents. Eur Spine J. 2002;11:227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hincapie CA, Cassidy JD, Cote P, et al. Whiplash injury is more than neck pain: a population-based study of pain localization after traffic injury. J Occup Environ Med. 2010;52:434–440. [DOI] [PubMed] [Google Scholar]
- 34.Vernon H. The Neck Disability Index: state-of-the-art, 1991-2008. J Manipulative Physiol Ther. 2008;31:491–502. [DOI] [PubMed] [Google Scholar]
- 35.Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. [DOI] [PubMed] [Google Scholar]
- 36.Bertilson B, Grunnesjo M, Johansson SE, et al. Pain drawing in the assessment of neurogenic pain and dysfunction in the neck/shoulder region: inter-examiner reliability and concordance with clinical examination. Pain Med. 2007;8:134–146. [DOI] [PubMed] [Google Scholar]
- 37.Falla D, Jull G, Russell T, et al. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87:408–417. [DOI] [PubMed] [Google Scholar]
- 38.Van Oosterwijck J, Nijs J, Meeus M, et al. Lack of endogenous pain inhibition during exercise in people with chronic whiplash associated disorders: an experimental study. J Pain. 2012;13:242–254. [DOI] [PubMed] [Google Scholar]
- 39.Pool JJ, Ostelo RW, Knol DL, et al. Is a behavioral graded activity program more effective than manual therapy in patients with subacute neck pain? Results of a randomized clinical trial. Spine (Phila Pa 1976). 2010;35:1017–1024. [DOI] [PubMed] [Google Scholar]
- 40.Jordan JL, Holden MA, Mason EE, et al. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010;1:CD005956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. [DOI] [PubMed] [Google Scholar]
- 42.Ekelund U, Sepp H, Brage S, et al. Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutr. 2006;9:258–265. [DOI] [PubMed] [Google Scholar]
- 43.Macdermid JC, Walton DM, Avery S, et al. Measurement properties of the Neck Disability Index: a systematic review. J Orthop Sports Phys Ther. 2009;39:400–417. [DOI] [PubMed] [Google Scholar]
- 44.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74. [DOI] [PubMed] [Google Scholar]
- 45.Stewart M, Maher CG, Refshauge KM, et al. Responsiveness of pain and disability measures for chronic whiplash. Spine (Phila Pa 1976). 2007;32:580–585. [DOI] [PubMed] [Google Scholar]
- 46.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9:105–121. [DOI] [PubMed] [Google Scholar]
- 47.Altmaier EM, Russell DW, Kao CF, et al. Role of self-efficacy in rehabilitation outcome among chronic low back pain patients. Journal of Counseling Psychology. 1993;40:335–339. [Google Scholar]
- 48.Denison E, Asenlof P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain. 2004;111:245–252. [DOI] [PubMed] [Google Scholar]
- 49.Bunketorp L, Carlsson J, Kowalski J, et al. Evaluating the reliability of multi-item scales: a non-parametric approach to the ordered categorical structure of data collected with the Swedish version of the Tampa Scale for Kinesiophobia and the Self-Efficacy Scale. J Rehabil Med. 2005;37:330–334. [DOI] [PubMed] [Google Scholar]
- 50.McAlister AL, Perry CL, Parcel GS.Glanz K, Rimer B, Viswanath K. How individuals, environments and health behaviours interact: social cognitive theory. Health Behavior and Health Education: Theory, Research, and Practice. 2008San Fransisco: Jossey-Bass;169–185. [Google Scholar]
- 51.Farrar JT. What is clinically meaningful: outcome measures in pain clinical trials. Clin J Pain. 2000;16supplS106–S112. [DOI] [PubMed] [Google Scholar]
- 52.Dworkin RH, Turk DC, McDermott MP, et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–244. [DOI] [PubMed] [Google Scholar]
- 53.Turk DC, Dworkin RH, Revicki D, et al. Identifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with pain. Pain. 2008;137:276–285. [DOI] [PubMed] [Google Scholar]
- 54.Rebbeck T, Sindhusake D, Cameron ID, et al. A prospective cohort study of health outcomes following whiplash associated disorders in an Australian population. Inj Prev. 2006;12:93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Poorbaugh K, Brismee JM, Phelps V, et al. Late whiplash syndrome: a clinical science approach to evidence-based diagnosis and management. Pain Pract. 2008;8:65–87quiz 8-9. [DOI] [PubMed] [Google Scholar]
- 56.Stewart MJ, Maher CG, Refshauge KM, et al. Patient and clinician treatment preferences do not moderate the effect of exercise treatment in chronic whiplash-associated disorders. Eur J Pain. 2008;12:879–885. [DOI] [PubMed] [Google Scholar]


