Abstract
Objectives:
Nucleoplasty is a minimally invasive procedure that is developed to treat patients with symptomatic, but contained disc herniations or bulging discs. The purpose of this study was to evaluate a decade follow-up of coblation nucleoplasty treatment for protruded lumbar intervertebral disc.
Methods:
In this retrospective study there a total 50 patients who underwent intradiscal coblation therapy for symptomatic, but contained lumbar degenerative disc disease were included. Relief of low back pain, leg pain and numbness after the operation were assessed by visual analog pain scale (VAS). Function of lower limb and daily living of patients were evaluated by the Oswestry disability index (ODI) and subjective global rating of overall satisfaction were recorded and analyzed.
Results:
There were 27 male and 23 female with followup mean follow up of 115 months (range 105–130 months) with a mean age was 52 years (range 26–74 years). Analgesic consumption was reduced or stopped in 90% of these cases after 1 year. At 24 months follow up VAS was four points and ODI was 7.2. In three patients, we repeated the cool ablation after 36 months, at L3–4 level in two cases. Ten patients continue to be asymptomatic after 114 months of intervention. There were no complications with the procedure including nerve root injury, discitis or allergic reactions.
Conclusions:
Nucleoplasty may provide intermittent relief in contained disc herniation without significant complications and minimal morbidity. In accordance with the literature the evidence for intradiscal coablation therapy is moderate in managing chronic discogenic low back pain; nucleoplasty appears to be safe and effective.
Keywords: Degenerative disc disease, low back pain, minimally invasive surgery, sciatica
Introduction
Contained disc herniation is one of the most difficult pathology to manage by conservative procedures, physiotherapy and drugs. However it has been suggested that open surgery should be avoided.[1] Based on the recent information it has been recommend that we should “abandon the instrumented pathway” in a great number of present indications for degenerative disc disease spine surgery, and look for new strategies in the field of rehabilitation and conservative treatments.[2] Recently, there is development of many minimally invasive techniques those are gaining popularity for the treatment of discogenic low-back pain with good outcome.[3,4] The primary rationale for any form of surgery for disc prolapse is to relieve nerve root irritation or compression due to herniated disc material. Coblation or “controlled ablation” is a tissue removal via plasma molecular dissociation. In the present article, we report our experience with cool ablation therapy with a mean follow up of 114 months.
Materials and Methods
The present retrospective study included 50 patients who underwent intradiscal cool ablation therapy for symptomatic but contained lumbar degenerative disc disease. The inclusion criteria in this group were patient with one symptomatic contained, focal herniated lumbar disc, with age between 18 years and 75 years old with a visual analogue pain scale (VAS) for radicular pain of seven or greater on a scale of 0–10. The radicular pain concordant with image findings (magnetic resonance imaging (MRI) or computed tomography) and the disc herniation must be no >1/3 the sagittal diameter of the spinal canal. In every case the conservative management including medications, physical therapy and epidural steroid injections documented as ineffective. The exclusion criteria were previous spinal surgery at the level to be treated, patient is morbidly obese (body mass index >40) or have spinal fracture, tumor or infection, the back pain greater than radicular (leg) pain or radicular pain originating from more than one disc level or radiological evidence of severe stenosis at the level to be treated, radiological evidence of spondylolisthesis at the level to be treated, severe disc degeneration (with >50% loss of disc height), evidence of extruded or sequestered disc herniation on MRI, patients who had clinical evidence of cauda equina syndrome or progressive neurological deficit and allergy to the contrast media or drugs to be used in the procedure. The data were collected, and response to the cool ablation both immediate and at follow up was analyzed. Relief of low back pain, leg pain and numbness after the operation were assessed using VAS, function of lower limb and daily living of patients were evaluated by the Oswestry disability index (ODI) and subjective global rating of overall satisfaction were recorded and analyzed every year. Reduction in analgesic treatment was also recorded. The procedure was performed under local anesthesia. In all cases, the percutaneous approach to the ipsilateral side was used [Figures-1,2 and 3].
Figure 1.
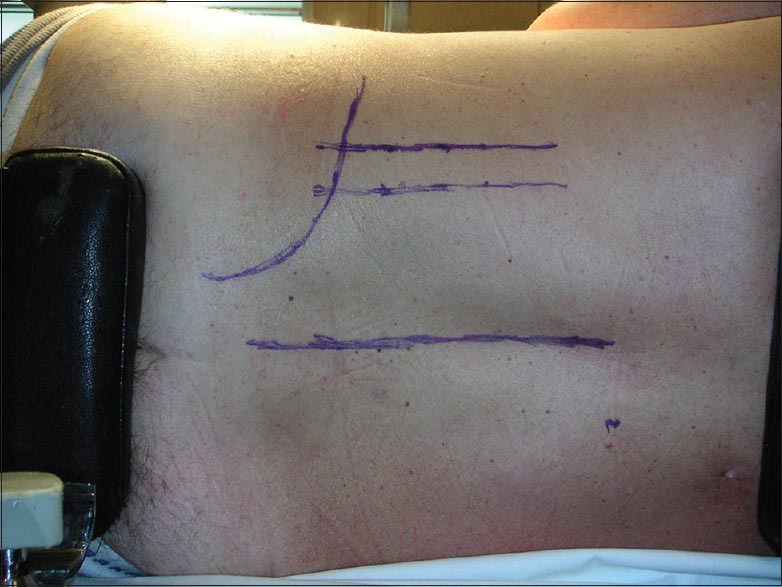
Procedure was performed in the lateral position in all the patients, please note the markings over the patient
Figure 2.
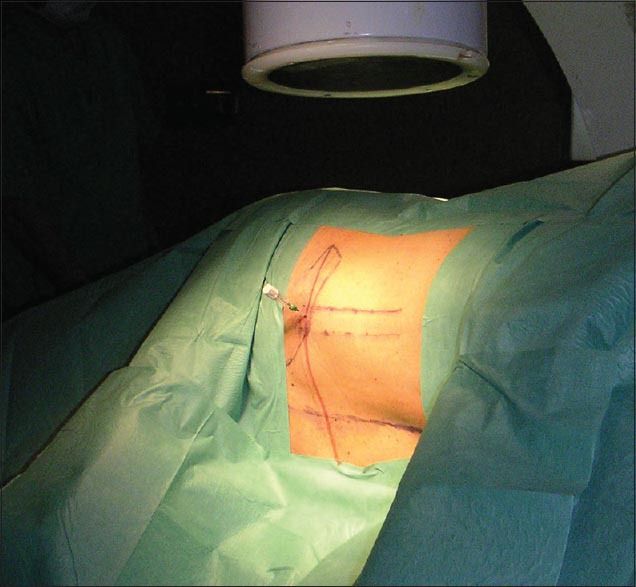
Needle was inserted and the position was confirmed by C-arm
Figure 3.

Fluoroscopic view of the position of the needle in disc space
Statistical analysis
All data were analyzed using the PSPP. Analysis of variance parametric test used to evaluate the improvements in VAS and ODI scores. Also, the correlation and regression analysis used to analyze the correlation between changes in VAS scores and duration of pain and between changes in VAS scores and age.
Result
There were 27 male and 23 female with follow up mean follow up of 114 months (range 103–130 months) with a mean age was 52 years (range 26–74 years) [Table-1]. In 36 cases were the radiculopathy was not clearly identifiable with the dermatome and MR objective degeneration in consecutive levels a provocative discography was performed previous to the surgery to confirm that the disc is the cause of low back, pseudoradicular and radicular pain. Twenty-four patients presented with acute and continuous pain symptomatology of <12 weeks duration, the rest of patients have more than 12 weeks. From these 24 patients who have more than 12 weeks of pain, four patients presented with only intermittent radicular pain, 10 patients presented with intermittent low back and radicular pain and 12 patients presented with continuous low back and radicular pain partially responding to conservative management. In all patients, intervention was performed at L4-L5 level. Nine patients had previous L5-S1 surgery discectomy or arthrodesis. Forty-five patients showed clinical improvement within 72 hours. Fifteen patients presented with recurrence in pain within 30 days and were needed another type of treatment. 12 months post-intervention 27 patients had improvement in VAS of pain five points and 24 patients ODI 9.2 [Table 2]. Analgesic consumption was reduced or stopped in 90% of these cases after 1 year. At 24 months follow up VAS was four points, and ODI was 7.2. In three patients, we repeated the cool ablation after 36 months, at L3–4 level in two cases. At 48 months the VAS was 4.2 and OS was 7. At 72 months the VAS was 4.8 and OS was 7 and we repeat the proceeding in two cases at the same level and two patients how has L5-S1 surgery previously to the proceeding go to surgery for rigid fixation from L4 to S1 level one in our hospital and one in another center. At 84 months follow up three patients more was operated for L4-L5, one case from previously L5-S1 and he receive a L4-S1 rigid fixation, and another two cases from L4 to L5 nucleoplasty in one case we do a simple discectomy and in another one a L4-L5 discectomy and L4-L5 and insertion of interespinous Coflex device. One and half year later this last patient underwent rigid arthrodesis of L4-L5. Analgesic consumption was reintroduced in 80% of the cases after 7 years follow up. Ten patients continue to be asymptomatic after 114 months of intervention [Figure 4]. There were no complications with the procedure including nerve root injury, discitis or allergic reactions.
Table 1.
Demographic characteristics of patients
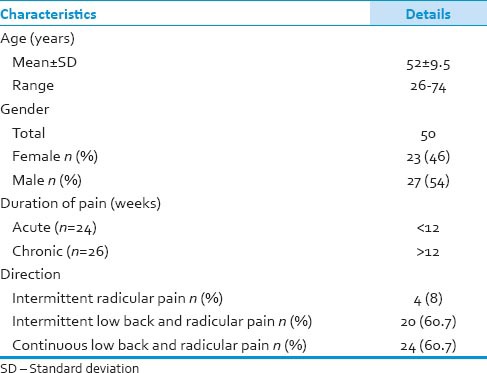
Table 2.
Pair wise comparisons of VAS and ODI scores
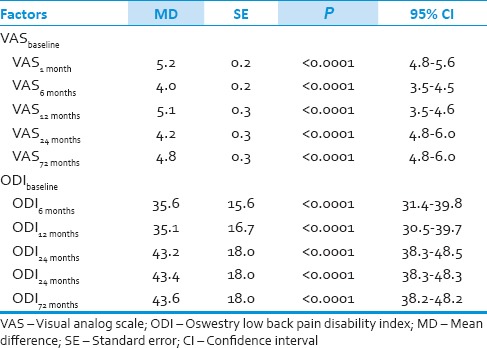
Figure 4.
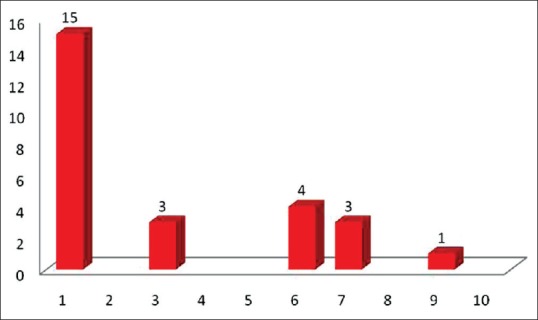
Pain recurrence in the follow up period (number of cases)
Discussion
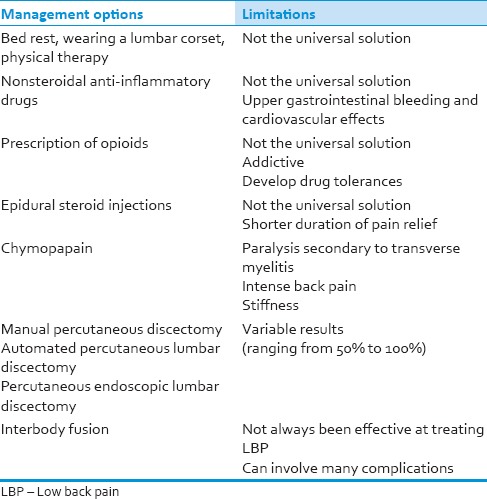
Classically discogenic low back pain is described as “band-like” distribution without radiculopathy that is worse in the morning, worse with Valsalva, and aggravated by standing in flexion.[4] Diagnosing discogenic low back pain is the key to successful treatment and provocative discography with manometric monitoring are recommended for the diagnosis of for this type of pain[4] with moderate sensitivity.[5] Many treatment options both conservative[6,7,8,9,10,11] and operative[12,13,14,15,16,17] have been used to treat low back pain with their limitations [Table 3]. Recently, minimally invasive techniques are gaining popularity as an alternative treatment for degenerative lumbar disc disease in order to reduce the morbidity caused by open surgery.[18,19] In recent years, there has been a gradual shift toward less invasive treatments for disc herniation, including chymopapain, automated percutaneous disc decompression, laser disc decompression, and more recently, minimally invasive nuclear decompression. These techniques include percutaneous thermo-coagulation intradiscal techniques [percutaneous intradiscal radiofrequency thermo-coagulation and intradiscal electrothermal therapy],[3,20] ultrasound.[21] etc., Nucleoplasty and other minimally invasive nuclear decompression devices are trying to bridge the gap between non-invasive treatment modalities and surgical fusion. Disc Nucleoplasty and Dekompressor are the two leading percutaneous discectomy technologies currently.[22] Percutaneous disc decompression using a bipolar radiofrequency device – also known as nucleoplasty, place the electrode in the center of the nucleus pulposus and has emerged as one of the minimally invasive techniques for treatment of low back pain and lower extremity pain due to contained herniated discs.[23,24] The targeted removal of herniated nucleus behind a protrusion is a more logical strategy for achieving the desired effect of removing the source of inflammation and relieving tension on the adjacent irritated annulus than open discectomy, fusion or disc arthroplasty. Complications reported from percutaneous disc decompression include discitis, anaphylaxis (with chemonucleolysis), instability, increased back pain, and reherniation.[25] There were no intra-and postoperative complications, and significant improvements in patient functional capacity, and pain scores were noted.[26] Our data indicate that nucleoplasty coblation is a promising treatment option for patients with symptomatic disk protrusion and herniation who present with lumbalgic and/or sciatalgic pain, have failed conservative therapies, and are not considered candidates for open surgery.[27] Nucleoplasty is appealing because it is simple, relatively safe, and destroys minimal tissue. Disc height should therefore be maintained or collapse more slowly and allow the body time to adapt. In addition, the 17-gauge introducer needle should cause significantly less collateral damage to the normal annulus compared with surgical arthroscopic decompression techniques that remove herniations from inside the disc. Nucleoplasty has certain advantages in the group of over these minimally invasive techniques as the temperature is kept low during ablation, charring or burning of surrounding tissues is minimized and the procedure is under the physician's complete control, unlike chemonucleolysis, which is dosage dependent.[28,29] Minimally invasive techniques can be used as repeat procedures with excellent in the selected group of patients.[30] However, the prospective studies are needed to identify the best candidates for repeat intradiscal therapy.[30] Although, nucleoplasty appeared to be a safe minimally invasive procedure, the value of this new technique for the treatment of discogenic low-back pain remains as yet unproven.[3] Many factors can explain the ineffectiveness of nucleoplasty for degenerative discs. First, aging of the lumbar spine causes the elastic nucleus pulposus to become dehydrated and fibrotic.[31] Second, healthier discs contain a soft and hydrated central region that distributes stress, whereas degenerated discs have only a small hydrostatic region that exhibits high stress.[32]
Table 3.
Some management options for the management of LBP and radicular pain and their limitations
Conclusions
In our study, only 20% of patients were completely asymptomatic at 114 months follow up. 54% patients had mild pain but could be managed with lesser dosage of medication. Nucleoplasty may provide intermittent pain relief in properly selected patients with contained disc herniation without significant complications and minimal morbidity. In accordance with the literature, the evidence for intradiscal coablation therapy is moderate in managing chronic discogenic low back pain; nucleoplasty appears to be safe and effective.[33]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Alexandre A, Corò L, Azuelos A, Pellone M. Percutaneous nucleoplasty for discoradicular conflict. Acta Neurochir Suppl. 2005;92:83–6. doi: 10.1007/3-211-27458-8_18. [DOI] [PubMed] [Google Scholar]
- 2.Robaina-Padrón FJ. Controversies about instrumented surgery and pain relief in degenerative lumbar spine pain. Results of scientific evidence. Neurocirugia (Astur) 2007;18:406–13. [PubMed] [Google Scholar]
- 3.Calisaneller T, Ozdemir O, Karadeli E, Altinors N. Six months post-operative clinical and 24 hour post-operative MRI examinations after nucleoplasty with radiofrequency energy. Acta Neurochir (Wien) 2007;149:495–500. doi: 10.1007/s00701-007-1146-9. [DOI] [PubMed] [Google Scholar]
- 4.Kosharskyy B, Rozen D. Lumbar discogenic pain. Disk degeneration and minimally invasive interventional therapies. Anasthesiol Intensivmed Notfallmed Schmerzther. 2007;42:262–7. doi: 10.1055/s-2007-980027. [DOI] [PubMed] [Google Scholar]
- 5.Hao DJ, Liu TJ, Wu QN, He BR. The application of lumbar discography in the diagnosis and treatment of the discogenic low back pain. Zhonghua Wai Ke Za Zhi. 2006;44:1675–7. [PubMed] [Google Scholar]
- 6.Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine (Phila Pa 1976) 1990;15:683–6. doi: 10.1097/00007632-199007000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976) 1983;8:131–40. [PubMed] [Google Scholar]
- 8.Wheeler M, Oderda GM, Ashburn MA, Lipman AG. Adverse events associated with postoperative opioid analgesia: A systematic review. J Pain. 2002;3:159–80. doi: 10.1054/jpai.2002.123652. [DOI] [PubMed] [Google Scholar]
- 9.Singh G, Triadafilopoulos G. Epidemiology of NSAID induced gastrointestinal complications. J Rheumatol Suppl. 1999;56:18–24. [PubMed] [Google Scholar]
- 10.Singh G, Lanes S, Triadafilopoulos G. Risk of serious upper gastrointestinal and cardiovascular thromboembolic complications with meloxicam. Am J Med. 2004;117:100–6. doi: 10.1016/j.amjmed.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 11.Javid MJ, Nordby EJ. Current status of chymopapain for herniated nucleus pulposus. Neurosurg Q. 1994;4:92–101. [Google Scholar]
- 12.Coppes MH, Marani E, Thomeer RT, Groen GJ. Innervation of “painful” lumbar discs. Spine (Phila Pa 1976) 1997;22:2342–9. doi: 10.1097/00007632-199710150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Lee CK, Vessa P, Lee JK. Chronic disabling low back pain syndrome caused by internal disc derangements. The results of disc excision and posterior lumbar interbody fusion. Spine (Phila Pa 1976) 1995;20:356–61. doi: 10.1097/00007632-199502000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Vamvanij V, Fredrickson BE, Thorpe JM, Stadnick ME, Yuan HA. Surgical treatment of internal disc disruption: An outcome study of four fusion techniques. J Spinal Disord. 1998;11:375–82. [PubMed] [Google Scholar]
- 15.Mochida J, Toh E, Nomura T, Nishimura K. The risks and benefits of percutaneous nucleotomy for lumbar disc herniation. A 10-year longitudinal study. J Bone Joint Surg Br. 2001;83:501–5. doi: 10.1302/0301-620x.83b4.11508. [DOI] [PubMed] [Google Scholar]
- 16.Schreiber A, Suezawa Y, Leu H. Does percutaneous nucleotomy with discoscopy replace conventional discectomy? Eight years of experience and results in treatment of herniated lumbar disc. Clin Orthop Relat Res. 1989:35–42. [PubMed] [Google Scholar]
- 17.Kambin P. Arthroscopic microdiscectomy of the lumbar spine. Clin Sports Med. 1993;12:143–50. [PubMed] [Google Scholar]
- 18.Nordby EJ, Wright PH, Schofield SR. Safety of chemonucleolysis. Adverse effects reported in the United States, 1982-1991. Clin Orthop Relat Res. 1993:122–34. [PubMed] [Google Scholar]
- 19.Tonami H, Kuginuki M, Kuginuki Y, Matoba M, Yokota H, Higashi K, et al. MR imaging of subchondral osteonecrosis of the vertebral body after percutaneous laser diskectomy. AJR Am J Roentgenol. 1999;173:1383–6. doi: 10.2214/ajr.173.5.10541125. [DOI] [PubMed] [Google Scholar]
- 20.Urrútia G, Kovacs F, Nishishinya MB, Olabe J. Percutaneous thermocoagulation intradiscal techniques for discogenic low back pain. Spine (Phila Pa 1976) 2007;32:1146–54. doi: 10.1097/01.brs.0000261492.55121.93. [DOI] [PubMed] [Google Scholar]
- 21.Nau WH, Diederich CJ, Shu R, Kinsey A, Bass E, Lotz J, et al. Intradiscal thermal therapy using interstitial ultrasound: An in vivo investigation in ovine cervical spine. Spine (Phila Pa 1976) 2007;32:503–11. doi: 10.1097/01.brs.0000256905.39488.c7. [DOI] [PubMed] [Google Scholar]
- 22.Pomerantz SR, Hirsch JA. Intradiscal therapies for discogenic pain. Semin Musculoskelet Radiol. 2006;10:125–35. doi: 10.1055/s-2006-939030. [DOI] [PubMed] [Google Scholar]
- 23.Yakovlev A, Tamimi MA, Liang H, Eristavi M. Outcomes of percutaneous disc decompression utilizing nucleoplasty for the treatment of chronic discogenic pain. Pain Physician. 2007;10:319–28. [PubMed] [Google Scholar]
- 24.Teixeira A, Sluijter ME. Intradiscal high-voltage, long-duration pulsed radiofrequency for discogenic pain: A preliminary report. Pain Med. 2006;7:424–8. doi: 10.1111/j.1526-4637.2006.00138.x. [DOI] [PubMed] [Google Scholar]
- 25.Smuck M, Benny B, Han A, Levin J. Epidural fibrosis following percutaneous disc decompression with coblation technology. Pain Physician. 2007;10:691–6. [PubMed] [Google Scholar]
- 26.Kapural L, Mekhail N. Novel intradiscal biacuplasty (IDB) for the treatment of lumbar discogenic pain. Pain Pract. 2007;7:130–4. doi: 10.1111/j.1533-2500.2007.00120.x. [DOI] [PubMed] [Google Scholar]
- 27.Masala S, Massari F, Fabiano S, Ursone A, Fiori R, Pastore F, et al. Nucleoplasty in the treatment of lumbar diskogenic back pain: One year follow-up. Cardiovasc Intervent Radiol. 2007;30:426–32. doi: 10.1007/s00270-006-0223-4. [DOI] [PubMed] [Google Scholar]
- 28.Sasaki M, Takahashi T, Miyahara K, Hirose AT. Effects of chondroitinase ABC on intradiscal pressure in sheep: An in vivo study. Spine (Phila Pa 1976) 2001;26:463–8. doi: 10.1097/00007632-200103010-00008. [DOI] [PubMed] [Google Scholar]
- 29.Takahashi T, Nakayama M, Chimura S, Nakahara K, Morozumi M, Horie K, et al. Treatment of canine intervertebral disc displacement with chondroitinase ABC. Spine (Phila Pa 1976) 1997;22:1435–9. doi: 10.1097/00007632-199707010-00002. [DOI] [PubMed] [Google Scholar]
- 30.Cohen SP, Shockey SM, Carragee EJ. The efficacy of repeat intradiscal electrothermal therapy. Anesth Analg. 2007;105:495–8. doi: 10.1213/01.ane.0000268499.62456.67. [DOI] [PubMed] [Google Scholar]
- 31.Southern EP, Fye MA, Panjabi MM, Patel TC, Cholewicki J. Disc degeneration: A human cadaveric study correlating magnetic resonance imaging and quantitative discomanometry. Spine (Phila Pa 1976) 2000;25:2171–5. doi: 10.1097/00007632-200009010-00005. [DOI] [PubMed] [Google Scholar]
- 32.Adams MA, Freeman BJ, Morrison HP, Nelson IW, Dolan P. Mechanical initiation of intervertebral disc degeneration. Spine (Phila Pa 1976) 2000;25:1625–36. doi: 10.1097/00007632-200007010-00005. [DOI] [PubMed] [Google Scholar]
- 33.Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, et al. Interventional techniques: Evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10:7–111. [PubMed] [Google Scholar]


