Abstract
Spontaneous spinal epidural hematoma (SSEH) is an uncommon neurological emergency which can present with the features ranging from simple back pain with radiculopathy to complete paraplegia or quadriplegia depending on the site and severity of the compression. Spinal hemorrhage associated with anti-platelet drugs is rarely seen. We report a case of SSEH in a 68-year-old hypertensive male who was on a low dose clopidogrel for secondary stroke prophylaxis and presented with bilateral lower limb paralysis, preceeded by severe back bain. A spinal magnetic resonance imaging scan was performed which revealed a posterior epidural hematoma of the thoraco-lumbar spine. To the best of our knowledge, not more than four cases of clopidogrel related spinal epidural hematoma have been reported. Emergent decompressive laminectomy was done within 4 hours of the presentation with excellent clinical outcome. Clinicians should, therefore, consider the remote risk of SSEH in hypertensive patients who are on anti-platelet drugs as early decompressive laminectomy and evacuation of the hematoma minimizes the permanent neurological damage.
Keywords: Clopidogrel, decompressive laminectomy, hypertension, spontaneous spinal epidural hematoma
Introduction
The incidence of spontaneous spinal epidural hematoma (SSEH) is estimated to be 0.1/100, 000 patients per year and accounts for <1% of spinal epidural space-occupying lesions.[1] SSEH has been reported in association with coagulopathies, anticoagulant therapy, blood dyscrasias, pregnancy and vascular malformation.[2] SSEH associated with anti-platelet agents is very rare, and only a few cases have been documented in the literature. The classic clinical presentation is acute onset of severe, often radiating, back pain followed by features of nerve root and/or spinal cord compression, which develop minutes to hours later. We report a rare case of clopidogrel associated SSEH in a 68-year-old hypertensive male who presented with acute paraparesis with back pain and underwent successful decompressive laminectomy with complete recovery. A brief review of the literature is discussed.
Case Report
A 68-year-old male presented with complaints of bilateral lower limb weakness and back pain for 6 h. The pain had started suddenly in the middle of the night and was radiating to the upper trunk and chest. He had noticed subjective anterior thigh numbness initially and was unable to move his lower limbs in the morning when the pain had subsided. He also developed urinary retention. The patient had no history of trauma, headache, fever, nausea, vomiting, and breathlessness. He was hypertensive and had a history of right-sided hemiparesis 6 years back which had recovered without any residual deficit. Previous computed tomography scan of the brain showed multiple left-sided lacunar infarcts, and he was on 5 mg amlodipine, 75 mg clopidogrel, and 10 mg atorvastatin, once daily dose.
On examination, the patient was alert, orientated and afebrile with a blood pressure of 160/86 mmHg, pulse rate of 84 beats/min. Neurologic examination revealed paraplegia with Medical Research Council (MRC) Grade I muscle power of hip and knee flexors with flaccid lower extremities. The knee and ankle reflexes were absent bilaterally while the plantar reflexes were flexor at the time of examination. The urinary bladder was palpable, and the anal tone was not traced with impaired perianal sensation. There was a loss of all sensory modalities from D10 downwards. He had an unremarkable chest, cardiovascular and abdominal examination. Laboratory findings included a hemoglobin value of 11.0 g/dL, white blood cell count of 10,000/mm3 (normal differential count) and a platelet count of 214,000/mm3. Serum electrolytes and coagulation profile was within normal limits. Magnetic resonance (MR) imaging of the thoraco-lumbar spine was ordered urgently which showed a mild hyperintense mass on T2-weighted images occupying the posterior epidural space from T12 to L2 [Figure 1]. The spinal cord was compressed and displaced anteriorly [Figure 2a and b]. Based on the clinical presentation and imaging findings, an epidural hematoma was suspected and steroid therapy (methylprednisolone 1000 mg IV) was started and neurosurgical consultation was done. l Antihypertensive medication was continued. At approximately 4 hours after initial onset of spinal cord compression symptoms, the patient underwent emergency decompressive laminectomy of D10–L2 level and evacuation of extradural hematoma, which histologically proved out to be a hematoma. Just after the surgery there was a significant sensory recovery, his weakness also improved and at the time of discharge after 1-week, muscle power of hip and knee flexors was 3/5 (MRC). Followed-up MR angiography of spine revealed no evidence of the vascular malformation and adequate cord decompression. One month postoperatively, his could walk without any assistance.
Figure 1.
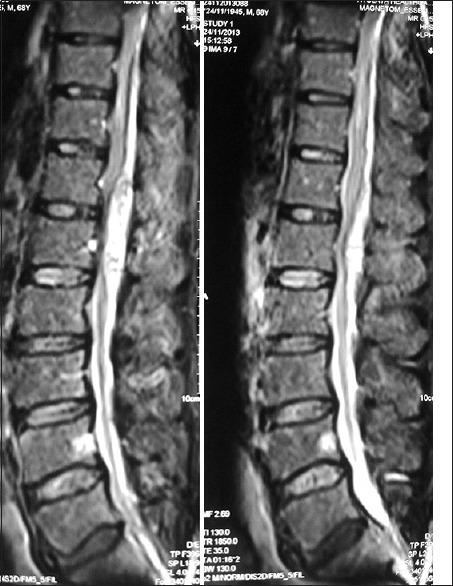
Sagittal T2-weighted images of the spine showing hyper intense signal from T12 to L2 in the posterior spinal epidural space
Figure 2.
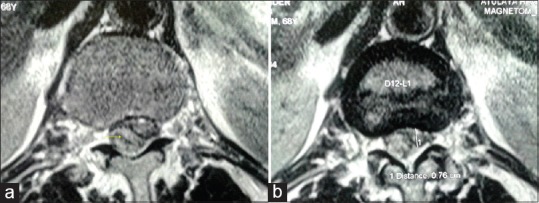
Axial T2-weighted images showing a posterior spinal epidural hematoma with compression worst at (a) T12 and conus medullaris (b) L1
Discussion
SSEH is defined as an accumulation of blood in the vertebral epidural space that has no obvious cause. It can present with features ranging from simple back pain with radiculopathy to complete paraplegia or quadriplegia depending on the site and severity of spinal cord compression.[3] In SSEH, the “spontaneous” refers to atraumatic etiology, and the multifactorial factors, that might contribute, include hemophilia, neoplasm, arteriovenous malformation, hypertension, anticoagulants, straining, sneezing, lifting or postoperative complications.[3] Idiopathic cases accounts for approximate 40–60% of cases.[4]
Unlike anticoagulants, anti-platelet agents have a lower risk of major bleeding and constitute a rare possible etiology of SSEH. Skin or gastrointestinal system are the common sites of their hemorrhagic complications, if any.[5] Clopidogrel, an anti-platelet drug irreversibly blocks adenosine diphosphate receptors (P2Y12), which are associated with amplification of platelet aggregation and secretion.[2] We cannot completely rule out the possibility of a coincidence of clopidogrel intake and SSEH. However, there was no history of trauma, anticoagulant use, straining, sneezing, lifting or any bleeding disorder. In addition, MR angiography of the spine showed no arterio-venous abnormalities. One risk factor, which might have augmented the pathogenesis of bleed, was uncontrolled hypertension in this patient. However, considering the mechanism of action of clopidogrel, the probability of a causal association seems to be much higher. A thorough literature search revealed only four cases of clopidogrel induced SSEH,[2,4,6,7] although several cases with asprin and clopidrogel combination have been reported.[8]
The most common site of a SSEH is the cervicothoracic region or thoracolumbar region and is usually located posterior to the thecal sac.[9] Some controversies exist about the origin of SSEH. Most authors believe that it originates from the epidural venous system, the raised intra-thoracic or intra-abdominal pressure may predispose to epidural vein rupture. However, clinically in the context of rapidly deteriorating neurological deficit an arterial source has been proposed.[10] SSEH occurs mostly after the fourth decade of life and the symptoms may include ascending numbness, progressive paraplegia and/or isolated loss of sensory function, and cauda-equina syndrome.[1] However, owing to its rarity, it may lead to an undue delay if neuro-surgical intervention is warranted.
Urgent surgical decompression and evacuation of the hematoma is the mainstay of treatment, but there has been much speculation on the cause of spontaneous resolution of neurological signs and symptoms in coagulopathy-induced spinal bleed. It is assumed that the hematoma remains liquid for a longer time, therefore enabling the spread of the hematoma into the spinal epidural space and hence alleviating compressive symptoms.[9] Prior neurological state and the timing of surgery are very critical to the final outcome and results are satisfactory if surgery is carried within 12 hours of the onset.[10] In our case, the patient underwent surgery at slightly more than 4 hours after the onset of the classical symptoms of spinal cord compression. The differential diagnosis of SSEH are acute herniated intervertebral disc, transverse myelitis, acute ischemia of the spinal cord and epidural tumor or abscess, and MR imaging should be performed to confirm the diagnosis if suspicion arises.[8]
In conclusion, SSEH is a rare neurosurgical emergency and with the growing trend of anti-platelet prescriptions for prophylactic use, clinicians should be aware of this serious complication especially when other risk factors like uncontrolled hypertension are present. Correct diagnosis and urgent decompressive surgery with evacuation of the hematoma is imperative for successful recovery if severe neurological deterioration is present.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Taniguchi LU, Pahl FH, Lúcio JE, Brock RS, Gomes MQ, Adoni T, et al. Complete motor recovery after acute paraparesis caused by spontaneous spinal epidural hematoma: Case report. BMC Emergency Medicine. 2011;11:10. doi: 10.1186/1471-227X-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung JH, Hong JT, Son BC, Lee SW. Clopidogrel-induced spontaneous spinal epidural hematoma. J Korean Med Sci. 2007;22:577–9. doi: 10.3346/jkms.2007.22.3.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim KT, Cho DC, Ahn SW, Kang SH. Epidural hematoma related with low-dose aspirin: Complete recovery without surgical treatment. J Korean Neurosurg Soc. 2012;51:308–11. doi: 10.3340/jkns.2012.51.5.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karabatsou K, Sinha A, Das K, Rainov NG. Nontraumatic spinal epidural hematoma associated with clopidogrel. Zentralbl Neurochir. 2006;67:210–2. doi: 10.1055/s-2006-933536. [DOI] [PubMed] [Google Scholar]
- 5.Moon HJ, Kim JH, Kim JH, Kwon TH, Chung HS, Park YK. Spontaneous spinal epidural hematoma: An urgent complication of adding clopidogrel to aspirin therapy. J Neurol Sci. 2009;285:254–6. doi: 10.1016/j.jns.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 6.Seet RC, Lim EC, Wilder-Smith EP, Ong BK. Spontaneous epidural haematoma presenting as cord compression in a patient receiving clopidogrel. Eur J Neurol. 2005;12:811–2. doi: 10.1111/j.1468-1331.2005.01057.x. [DOI] [PubMed] [Google Scholar]
- 7.Morales Ciancio RA, Drain O, Rillardon L, Guigui P. Acute spontaneous spinal epidural hematoma: an important differential diagnosis in patients under clopidogrel therapy. Spine J. 2008;8:544–7. doi: 10.1016/j.spinee.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Kim T, Lee CH, Hyun SJ, Yoon SH, Kim KJ, Kim HJ. Clinical outcomes of spontaneous spinal epidural hematoma: A comparative study between conservative and surgical treatment. J Korean Neurosurg Soc. 2012;52:523–7. doi: 10.3340/jkns.2012.52.6.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Groen RJ. Non-operative treatment of spontaneous spinal epidural hematomas: A review of the literature and a comparison with operative cases. Acta Neurochir (Wien) 2004;146:103–10. doi: 10.1007/s00701-003-0160-9. [DOI] [PubMed] [Google Scholar]
- 10.Shin JJ, Kuh SU, Cho YE. Surgical management of spontaneous spinal epidural hematoma. Eur Spine J. 2006;15:998–1004. doi: 10.1007/s00586-005-0965-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


