Abstract
Background
Unequal HIV/AIDS distribution is influenced by certain social and structural contexts that facilitate HIV transmission and concentrate HIV in disease epicenters. Thus, one of the first steps in designing effective community-level HIV/AIDS initiatives is to disentangle the influence of individual, social, and structural factors on HIV risk. Combining ethnographic methodology with geographic information systems (GIS) mapping can allow for a complex exploration of multilevel factors within communities that facilitate HIV transmission in highly affected areas.
Objectives
We present the formative comparative community-based case study findings of an investigation of individual-, social- , and structural-level factors that contribute to the HIV/AIDS epidemic among Black Philadelphians.
Methods
Communities were defined using census tracts. The methodology included ethnographic and GIS mapping, observation, informal conversations with residents and business owners, and secondary analyses of census tract-level data in four Philadelphia neighborhoods.
Results
Factors such as overcrowding, disadvantage, permeability in community boundaries, and availability and accessibility of health-related resources varied significantly. Further, HIV/AIDS trended with social and structural inequities above and beyond the community’s racial composition.
Discussion
This study was a first step to disentangle relationships between community-level factors and potential risk for HIV in an HIV epicenter. The findings also highlight stark sociodemographic differences within and across racial groups, and further substantiate the need for comprehensive, community-level HIV prevention interventions. These findings from targeted United States urban communities have potential applicability for examining the distribution of HIV/AIDS in broader national and international geosocial contexts.
Keywords: ethnography, geographic mapping, HIV, public health
The HIV/AIDS epidemic is an enduring quagmire. Researchers have documented individual, social, and structural factors that drive local epidemics (Brawner, Gomes, Jemmott, Deatrick, & Coleman, 2012; Kerr, Valois, Siddiqi, Vanable, & Carey, 2014; Nunn et al., 2011). More specifically, disproportionate HIV/AIDS infection rates among Blacks may be attributable to the hyper-incarceration of Black men, poverty, racism, and a paucity of harm reduction (e.g., syringe exchange) and comprehensive sexual health education programs (Adimora & Auerbach, 2010; Blankenship, West, Kershaw, & Biradavolu, 2008; Bowleg & Raj, 2012). These multilevel factors may help explain differences in HIV disease burden across neighboring geographic areas. For example, while HIV incidence rates in Philadelphia are five times the national average (Philadelphia Department of Public Health AIDS Activities Coordinating Office [AACO], 2008), GIS mapping of the local epidemic indicates drastic differences in HIV concentration across neighboring census tracts—with higher HIV concentrations mostly in predominantly Black tracts (AACO, 2010). Moreover, Eberhart et al. (2013) analyzed geographical patterns of the HIV care continuum and discovered that spatial patterns independently predicted linkage to care, retention in care, and viral suppression.
Community/neighborhood-level effects on health, including HIV/AIDS risk and outcomes, are well documented within the literature (Lindberg & Orr, 2011; Sampson, 2003). Studies have also demonstrated that rates of sex in exchange for money and sex with high-risk sexual partners are higher in communities which have high levels of poverty, and associated vandalism, litter, vacant housing, burglary, and drug sales (Généreux, Bruneau, & Daniel, 2010; Rudolph, Linton, Dyer, & Latkin, 2012; Schensul, Levy, & Disch, 2003). These community-level influences on HIV risk are particularly important to consider when individuals are socially/structurally restricted by income or race to geographic areas that foster disadvantage (e.g., racial residential segregation; Smedley, 2012). In situations of geographic and social isolation and marginalization, people tend to select sexual partners from within their networks (Friedman & Aral, 2001; Youm & Laumann, 2002). Hence, if someone lives in a community with high HIV prevalence and frequents the same geographic areas and/or engages with the same social networks, then HIV transmission is more likely to occur among and between these community members (Millett, Peterson, Wolitski, & Stall, 2006; Youm & Laumann, 2002). Targeting individual behavior alone may not be powerful enough to overcome the mediating effect of the environment on HIV risk (Sumartojo, Doll, Holtgrave, Gayle, & Merson, 2000).
Given Philadelphia’s epidemiologic profile, it’s an appropriate setting to analyze the influence of multilevel factors on subsequent HIV risk among Blacks. Philadelphia is a 135-square mile city of neighborhoods, with approximately 1,526,006 residents and 10,000 persons per square mile (U.S. Census Bureau, 2010b). The land area is divided into 12 planning analysis sections, comprising 63 named neighborhood areas and nearly 400 census tracts (Philadelphia City Planning Commission, 2005). Each community has its own distinct character and pulse.
In this paper, we present the findings of a formative, comparative community-based case study analysis of four Philadelphia communities addressing the individual-, social-, and structural-level factors that contribute to the HIV/AIDS epidemic among Black Philadelphians. The ultimate goal of this line of inquiry is to inform the development of community-level HIV/AIDS initiatives that have implications across multilevel intervention strategies (e.g., group-level behavioral interventions, social media campaigns, and recommendations for laws and policies). Although the findings are from a small sample of targeted U.S. urban communities, the methodology can be replicated to better understand the distribution of HIV/AIDS in broader national and international geosocial contexts.
Guiding Conceptual Model
An ecological conceptual model (Bronfenbrenner, 1986) guided the study (see Brawner, 2014 for an illustration of the model and additional details). Four major pathways are posited:
It is presumed that multilevel factors, such as mental health, social capital, and poverty, interact to influence community-level indicators of HIV transmission (e.g., HIV incidence rates).
These same multilevel interactions are purported to also influence behaviors that transmit HIV (e.g., multiple sexual partners).
The association between behaviors that transmit HIV and subsequent HIV risk is thought to be mediated by community-level indicators of HIV transmission in different geographical locations (e.g., community viral load).
The end result of HIV risk, referred to as “geobehavioral vulnerability to HIV”—the probability of HIV acquisition based on what you do, where you do it, and who you do it with—is the manifestation of multilevel interactions that create and sustain the risk context in certain populations and geosocial spaces (Brawner, 2014).
Inequitable social and structural factors, such as high unemployment rates (Tan, Earnshaw, Pratto, Rosenthal, & Kalichman, 2015), are believed to heighten geobehavioral vulnerability by modifying both individual behavior (e.g., survival sex; Raiford et al., 2014) and the concentration of HIV (e.g., limited viral suppression). This conceptual model may explain why higher concentrations of HIV are found within specific sociospatial communities (Das et al., 2010), and why the epidemic becomes localized in certain regions and social/sexual networks (Hammett & Drachman-Jones, 2006).
Methods
This study was approved by the University of Pennsylvania and Yale University Institutional Review Boards. Communities were defined as census tracts, and we acknowledge that defining communities in this manner may not have social meaning for residents. However, the data required for this endeavor were only available at the census tract-level. Based on the work of Schensul and LeCompte (2012), we conducted ethnographic and geographic information systems (GIS) mapping, observation, informal conversations with residents and business owners, and secondary analyses of census tract-level data. Secondary data were obtained for 2008 and 2010. Primary data were collected from October 2011 through April 2012.
Sample Description and Inclusion Criteria
Four Philadelphia communities were selected based on the following criteria: (a) high (10 or more cases) or low (less than five cases) HIV incidence, and high (35 or more cases) or low (less than five cases) AIDS prevalence; (b) predominantly (more than 85%) Black or White area; (c) total population greater than 1,000; and (d) percent male population comparable to Philadelphia’s male population. HIV incidence and AIDS prevalence rates per community were determined from publicly available census tract maps through the local health department (AACO, 2009). The remaining criteria were determined from the 2009 American Community Survey (ACS) five-year estimates (U.S. Census Bureau, 2010a). First, the HIV/AIDS maps were reviewed and then overlaid with maps of the percentage of Black and White populations (City of Philadelphia, 2010a, 2010b). Communities A and B immediately stood out as predominantly Black communities with low and high HIV incidence/prevalence, respectively; very few predominantly Black communities had low HIV incidence/prevalence rates. Community D stood out as a predominantly White community with high HIV incidence/prevalence and, upon further investigation, met the study criteria. Numerous predominantly White communities had low HIV incidence/prevalence. Community C was selected based on its total population and percent male population, as well as comparability to Community D. Similar age, educational attainment, and socioeconomic status within the racial groups were also ensured in the selection process using the census data (U.S. Census Bureau, 2010a).
Census tracts are small, relatively permanent statistical subdivisions of a county. They are delineated for most metropolitan areas and other densely populated counties by local census statistical areas committees following Census Bureau guidelines (U.S. Census Bureau, 1994). All census tracts included were within the City of Philadelphia. Prior knowledge of the study community boundaries enabled the research team to find historical information on each area, and identify key locations within the community where potential stakeholders could be reached (e.g., churches and community centers).
Census Tract-Level Data and Procedures
The Cartographic Modeling Lab (CML) at the University of Pennsylvania assembled a census tract-level spatial database for the four study communities for 2006, 2008, and 2010. The CML received data transfers from Geolytics 2001–2008 premium estimates, the Philadelphia Neighborhood Information System, and the Public Health Management Corporation’s (PHMC) Southeastern Pennsylvania Household Health Survey through data license agreements. These data were merged with sociodemographic data from the ACS (U.S. Census Bureau, 2010a). With the exception of calculating the racial residential segregation data, the CML received data that were analyzed by the providing source (e.g., community perception averages provided by PHMC). This paper focuses solely on the 2010 data as those data were closest to the community ethnography timeframe; some information, however, was only available in the 2008 datasets.
Based on the work of Massey and Denton (1987), racial residential segregation was measured by an index of dissimilarity (the distribution of minority and majority groups across census tracts) and an exposure index (the likelihood of contact between minority and majority members within a census tract). Index of dissimilarity values range from 0 (complete integration) to 100 (complete segregation). Exposure index values range from 0% to 100%. Lower percentages indicate that Blacks are less likely to be exposed to or have the potential to interact with Whites in the census tract. The values were calculated using data from the U.S. Census Bureau (2000b).
The PHMC used small area estimation of their citywide survey (N = 10,006; Jiang & Lahiri, 2006) to calculate community perceptions and HIV testing history for the census tracts. Values presented in Table 1 are the mean and standard error for dichotomized variables created from the following survey questions: How many local groups or organizations in your neighborhood do you currently participate in, such as social, political, religious, school-related, or athletic organizations? One or more groups were defined as actively engaged in the community. “Most people in my neighborhood can be trusted” and “I feel that I belong and am a part of my neighborhood” were assessed on a 4-point Likert scale. Agree or strongly agree were collapsed and defined as “trust people in the neighborhood” and “feel a sense of belonging in the neighborhood,” respectively. For “Would you say that most people in your neighborhood are always, often, sometimes, rarely, or never willing to help their neighbors?” and “Have people in your neighborhood ever worked together to improve the neighborhood?” “Yes” was defined as “neighbors willing to help” and “work together for improvement,” respectively. Lastly, “Have you ever been tested for HIV/AIDS?” “Yes” was defined as “ever tested for HIV” in their lifetime.
TABLE 1.
Census Tract-Level Data
| Characteristic | Community |
|||
|---|---|---|---|---|
| A | B | C | D | |
| Tract size (in square miles) | 0.3 | 0.8 | 0.6 | 0.8 |
| Total population | 4,481 | 6,983 | 3,200 | 2,276 |
| Population density | 16,014 | 46,261 | 36,519 | 55,870 |
| Housing unit density | 7,873 | 12,766 | 17,883 | 46,075 |
| Predominant racial | 88.7% | 97.2% | 96.8% | 88% |
| compositiona | Black | Black | White | White |
| Sex ratio (males per 100 females)a | 72 | 90.3 | 91.4 | 96.7 |
| Median agea | 49 | 35.9 | 42.5 | 33.5 |
| At least a high school diploma or GEDa | 69.2% | 65.5% | 83.5% | 96.9% |
| % receive public assistance incomea | 4.4% | 11.9% | 0% | 0% |
| % unemployeda | 33.2% | 18.8% | 6.2% | 4.3% |
| % below federal poverty levela | 32.5% | 36.5% | 10.3% | 8.6% |
| % female-headed householdsa | 24.1% | 28.4% | 12% | 4.9% |
| # of vacant parcelsb | 15 | 121 | 21 | 58 |
| # of vacant parcels structurally maintainedc | 0 | 9 | 0 | 0 |
| Criminal homicide incidents | 0 | 2 | 0 | 0 |
| Aggravated assault incidents | 15 | 96 | 6 | 4 |
| All thefts (including motor vehicles) | 40 | 183 | 166 | 204 |
| Vandalism and criminal mischief incidents | 15 | 91 | 50 | 57 |
| Disorderly conduct incidences | 3 | 37 | 11 | 6 |
| Prostitution | 0 | 1 | 0 | 0 |
| Sex offenses (including rape) | 2 | 3 | 0 | 2 |
| Narcotic violationsd | 14 | 197 | 18 | 12 |
| Exposure Indexe | 0.8% | 0.4% | 0.9% | 9% |
| Actively engaged in the | 0.53 | 0.48 | 0.40 | 0.44 |
| communityf | (0.09) | (0.10) | (0.08) | (0.08) |
| Trust people in neighborhoodf | 0.60 | 0.68 | 0.78 | 0.65 |
| (0.12) | (0.13) | (0.10) | (0.11) | |
| Neighbors willing to helpf | 0.86 | 0.91 | 0.92 | 0.87 |
| (0.06) | (0.06) | (0.05) | (0.06) | |
| Neighbors work together for | 0.85 | 0.84 | 0.72 | 0.82 |
| improvementf | (0.07) | (0.10) | (0.10) | (0.08) |
| Feel a sense of belonging in | 0.90 | 0.94 | 0.94 | 0.90 |
| neighborhoodf | (0.05) | (0.04) | (0.04) | (0.05) |
| Ever tested for HIVf | 0.56 | 0.53 | 0.50 | 0.53 |
| (0.11) | (0.13) | (0.11) | (0.10) | |
| HIV incidence (cases)g | < 5 | ≥ 15 | < 5 | 10–14 |
| Persons living with AIDS (cases)g | < 5 | ≥ 35 | < 5 | ≥ 35 |
Note. Data are from the University of Pennsylvania Cartographic Modeling Lab database unless otherwise noted)
Data from the 2009 American Community Survey five-year estimates;
Includes commercial, residential and industrial parcels;
Parcels cleaned, greened, and tended in the Pennsylvania Horticultural Society Vacant Land Stabilization program;
Includes narcotic sales, possession, manufacture, and delivery;
Exposure Index values range from 0% to 100% (lower percentage values indicate that Blacks are less likely to be exposed to or have the potential to interact with Whites in the census tract), calculated from 2008 data;
Values are from 2008 data, reported as Mean (Standard Error) calculated as small area estimates from dichotomized responses to the PHMC questions (N = 10,006);
Data from 2008 from the Philadelphia AIDS Activities Coordinating Office report.
For the acronyms, GED is general education development test certification, HIV is human immunodeficiency virus, and AIDS is acquired immune deficiency syndrome.
Ethnographic Data and Procedures
Staff training
In ethnographic research, how the members of the community view the researchers shapes the community-researcher interaction and, thereby, influences the nature of the data collected (Blommaert & Jie, 2010). An experienced ethnographer conducted two, six-hour trainings on Community-Based Participatory Research (CBPR) combined with ethnographic methods (McQuiston, Parrado, Olmos-Muñiz, & Bustillo Martinez, 2005). Team members were asked to consider their own positionality in the study—in particular, the social categories which may be ascribed to them by the community (LeCompte & Schensul, 2014), how those ascriptions shape the information participants provide (Blommaert & Jie, 2010), and how the researchers’ views of the community impact the interpretation of the data. Additional key concepts and practices introduced in the training included: attending to “cultural meanings, insider understandings, and the sign/symbols used to understand them” (Singer, 2006, p. 233); identifying public areas where people congregate (Schensul, LeCompte, Trotter II, Cromley, & Singer, 1999); identifying community assets and strengths, as well as needs and concerns (Wallerstein, Duran, Minkler, & Foley, 2005); and viewing community residents as equal partners throughout the research process (Israel, Eng, Schultz, & Parker, 2012). Role-playing was incorporated into the training to build skills around potential obstacles researchers might face in gaining access to community sites and engaging with residents during fieldwork.
Field visits
The research team spent two consecutive weeks (approximately 40 hours) in each community. Field visits or observations were conducted at minimum three days during the week, and occasional Saturdays with a rotation of morning, afternoon, and evening hours to discover peak hours of activity. Community observations were guided by a neighborhood observational checklist and field notes guide (Israel et al., 2012). Approximately 15 businesses and community-based organizations were targeted in each area. The team observed and notated the flow and patterns of customer traffic at each location, and collected artifacts (e.g., flyers, brochures, newspapers, and photos) for further analyses.
In addition to passive observation, team members engaged residents (0 to 5 residents per visit) as they walked down the street, waited at public transportation stops, and patronized local businesses. There was no script for these conversations, but the team was trained to probe for information related to the guiding conceptual framework , such as community health, HIV/AIDS awareness, and neighborhood social order and safety. The variability of resident engagement per day can be attributed to the number of people on the street (a factor often influenced by the time of day and inclement weather), and the team members’ perception of how busy an individual or group was.
Multiple measures were taken to ensure appropriate engagement. The research team traveled in pairs (typically one Black and one Caucasian female) when recruiting residents rather than in larger groups due to the sensitivity of the topic and the attention drawn to the researchers in the prospective communities. Depending on the team’s perception of the receptiveness of the resident or business owner in question, a direct or indirect approach was chosen for engagement. When approaching residents or business owners with a direct approach, team members briefly described the project and proceeded to probe for information about community safety, education, and drug use—leading up to community health in the area, including HIV. In the indirect approach, the team engaged residents in typical conversations without revealing that they were outsiders. This indirect approach, at times, provoked suspicion amongst residents and questions of whether team members were FBI agents or social workers. In these instances, the team disclosed the purpose of the project and residents either continued the conversation or walked away.
Field notes
Field notes were first recorded individually on small notebooks or less conspicuous smartphones, and then typed up in Microsoft Word. Electronic field notes were stored on a worksite hard drive and distributed to team members by email. Team members were given the opportunity to read the field notes by email to prepare for subsequent visits, as well as in recognition of the role field notes play in the interpretive process. Weekly team debriefings also contributed to the writing and synthesis of ethnographic field notes by allowing team members to reflect on community visits, discuss their positionality in the visits, and identify aspects of the community to focus on in future visits. Residents’ names were omitted from field notes to maintain anonymity.
Ethnographic mapping
After stakeholders were identified and observations and informal interviews were completed in all four Philadelphia communities, the team revisited each of the areas over the course of one week to complete the mapping task. Five residents were randomly selected per community (N = 20), presented with paper copies of satellite maps of their census tract, and asked to draw the geographic boundaries that they perceived to define their community. They were also asked to mark the locations of meaningful and important places/structures in their area.
Data Analysis
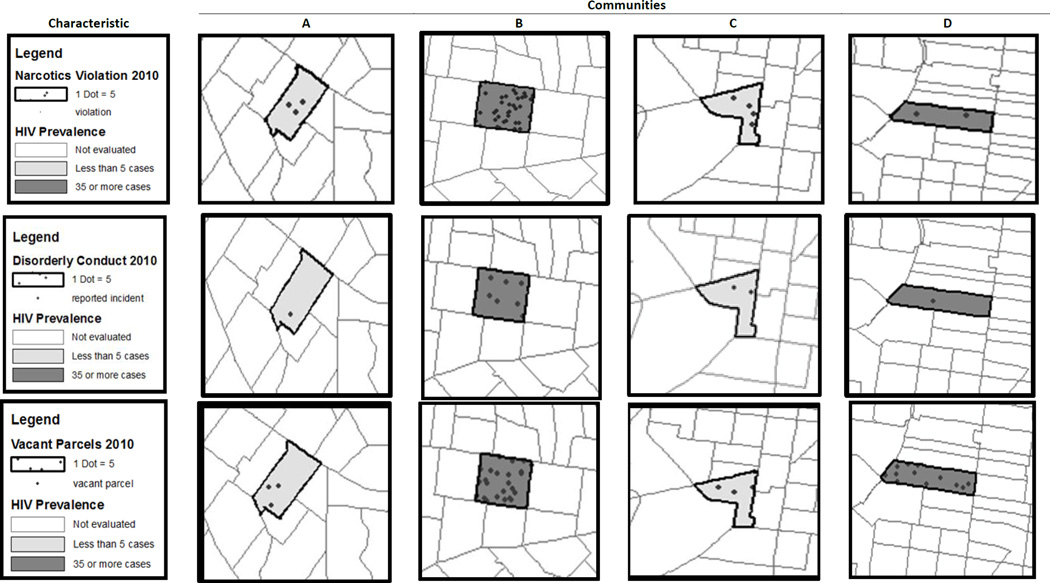
The communities were stratified by race and HIV/AIDS incidence/prevalence to conduct within and across community and population examinations. ArcGIS 10.1 (2012) was used to create dot density and chloropleth maps to depict narcotics violations, disorderly conduct incidents, and vacant parcels in each community. The variables were overlapped in the maps to explore social and structural factors related to HIV/AIDS rates. The field notes, conversations with residents, and ethnographic mapping were integrated to provide context and meaning for the quantitative data.
Results
The four study communities are hereafter referred to as Communities A, B, C, and D. Overall, the highest number of residents were engaged in informal conversations in Communities A (n = 14) and C (n = 13). Fewer residents were engaged in Communities B (n = 6) and D (n = 5). It should be noted, however, that these numbers do not reflect the quality of interaction and the willingness of residents to talk about issues connected with HIV/AIDS. Although team members engaged similarly high numbers of residents in Community A and Community C, it was observed that residents seemed more reluctant to talk about or acknowledge HIV/AIDS and its risk behaviors in Community C than in Community A. Despite the relatively low numbers in Community B, highly relevant information was gleaned from the residents in this community.
Philadelphia has named neighborhood areas demarcated by streets, waterways, etc., that typically represent multiple census tracts. None of the maps the residents drew (N = 20) coincided with the census demarcations or any other boundaries identified by the city. Most residents considered their block—or a very narrow radius surrounding their block—to be their community. Some who identified with the city’s neighborhood naming system (e.g., Millcreek) drew markers that more closely aligned to those neighborhood areas.
As seen in Table 1, the four communities vary dramatically across sociodemographic criteria, as well as HIV/AIDS rates. In each community, however, the majority of residents felt a sense of belonging (A: M = 0.90, SE = 0.05; B: M = 0.94, SE = 0.04; C: M = 0.94, SE =0.04; D: M = 0.90, SE = 0.05), and that their neighbors were willing to help each other (A: M = 0.86, SE = 0.06; B: M = 0.91, SE = 0.06; C: M = 0.92, SE = 0.05; D: M = 0.87, SE = 0.06). The index of dissimilarity was 78, which indicates that Philadelphia is highly segregated. Stratification of the communities by race and HIV/AIDS statistics maximized the degree of difference for comparisons. Findings from each community are described in more detail below.
Community A
Community A is predominantly Black (89%) with low HIV incidence and prevalence. As seen in Table 1, the exposure index is low (0.8%), indicating that Blacks in this community are unlikely to be exposed to or have the potential to interact with Whites. This census tract has the second largest total population of the four communities, but has the smallest square mileage; population and housing density are still relatively low compared to the other areas. The community has the fewest vacant parcels, and the lowest number of thefts, vandalism, and disorderly conduct incidents. There are also relatively few narcotic violations (see Figure 1). The sex ratio is the lowest in the sample (72 males per 100 females), and the tract has the highest percentage of unemployed residents (33.2%). Nearly one third of residents live below the federal poverty level and almost one quarter of households are female-headed households—all of which highlight a degree of concentrated disadvantage in the community. Residents reported the highest average of active community engagement (M = 0.53, SE = 0.09), but the lowest average of trust of their neighbors (M = 0.60, SE = 0.12). More than half had ever been tested for HIV (M = 0.56, SE = 0.11).
FIGURE 1.
Social and structural characteristics, and HIV prevalence, in the four study communities.
The tract is taken up mostly by an arboretum, which appeared to be the focal point of the community from the ethnographic maps. Along the streets that border the arboretum are homes, a public high school, fast food restaurants, and other businesses. The residences closer to and within the arboretum are more “opulent” when compared with the row homes lining the smaller streets. Upon observation, it was discovered that the side streets vary block by block in curb appeal and safety similar to most Philadelphia communities. The research team gathered that the community is relatively safe after speaking with community members and surveying the area. According to the residents, the arboretum has had incidents of prostitution on the park grounds after dusk. The evidence of this practice, as reported by arboretum staff, was the discovery of used condoms and wrappers, as well as drug paraphernalia, on the grounds.
One resident described the community as “middle/working class folks.” She shared that the people are just trying to work, raise their families, and live in peace. The presence of the arboretum appeared to be the glue that holds the community together. The site has many community projects in which community members and families can get involved; however, none of these focus on HIV/AIDS education, awareness, or prevention.
Based on the participants’ maps and the teams’ observations, there are limited healthcare resources available in Community A. There are no HIV/AIDS or sexually transmitted infections (STI)-related agencies in the area. When asked about HIV perceptions, residents avoided answering the question, made no comment, or referenced that it was not a problem in their community. Some people were more open and shared that they knew people living with HIV/AIDS. They identified interventions with younger populations as a strategy to curb HIV infection rates. Concern was also expressed about educating “high-risk individuals” (e.g., prostitutes) about safer sexual practices.
Community B
Community B is predominantly Black (97%) with high HIV incidence and prevalence; the community also has the lowest exposure index (0.4%). This community is the second most populous of the four areas. The community is primarily made up of residences; however, lining one of the main streets are a plethora of businesses and street vendors selling clothing/accessories. Most of the businesses in the community are restaurants, barber/beauty salons, clubs, bars, retail stores, and day cares. There are also very few medical resources. Based on findings from the ethnographic maps, the focal points of Community B appear to be the YMCA, a free library, a park, and numerous churches. As shown in Table 1, this census tract has the greatest number of vacant parcels, and the greatest incidents of criminal homicides, aggravated assaults, vandalism and criminal mischief, disorderly conduct, prostitution, sex offenses, and narcotic violations. Figure 1 shows the prevalence of disorderly conduct in Community B relative to the other communities.
Many residences at the time of the observations were condemned, abandoned, or in deplorable condition. There were very few streets where the properties and blocks were maintained. Overall, the community did not feel very safe to the research team who were easily distinguished by residents as “outsiders.” There were several instances in which the team felt threatened, especially when they frequented the smaller side streets with more vacant properties. Yet, census-level community cohesion indexes are relatively high. Community B has the second-highest level of trust in the neighborhood (M = 0.68, SE =0.13), neighbors willing to help (M = 0.91, SE = 0.06), and neighbors working for improvement (M = 0.84, SE = 0.10); it ties with Community C for feeling a sense of belonging in the neighborhood (M = 0.94, SE = 0.04). These data suggest that the community is supportive of insiders, but closed to outsiders.
When asked about the safety of the community, one resident stated that he believed his neighborhood is relatively safe. He mentioned that the biggest crime-related issue is drug use and distribution. Another community member commented that sex acts occur in any discrete “alley, nook, or cranny”; public sex acts were broadly mentioned as an issue in this community. One door entryway of a residence was ridden with condom wrappers. The tenant of this home shared the phenomenon and dilemma of “corner houses.” As she described, the position of a home at the intersection of two cross streets makes the property a prime location for drug and sex trade activity (even if the homeowner was not involved in the activities). She recounted numerous occurrences of hearing individuals having sex outside of her window, and discovering used condoms on the steps and in the doorway that led down to the basement of her property.
Although the unemployment rate in Community B is nearly half that of Community A (18.8% vs. 33.2%, respectively), Community B has the largest percentage of individuals receiving public assistance (11.9%) and living below the federal poverty level (36.5%). Several homeless individuals were also identified. The appearance of homes could lead to the assumption that residents do not have the means to upkeep their properties. However, the overall dilapidation of public property and streets allude to a broader sociopolitical concern. A 30-year community resident stressed that the major issues in the area are unemployment and low literacy; he did not believe HIV/AIDS was an issue in the community. The YMCA and free library offer residents a variety of resources, such as initiatives to increase literacy and gainful employment.
Other community resources are the numerous churches located in the vicinity. One local church congregant shared his mixed feelings on the HIV epidemic. He also did not believe HIV was an issue in his community; however, he believed the “growing homosexual population” will cause HIV to become an issue. In contrast with data reporting the second-highest rate of HIV testing among the four communities (M = 0.53, SE = 0.13), the presence of HIV in Community B seems to be under-addressed. No HIV/AIDS or STI related agencies were present in this community.
Community C
Community C is predominantly White (97%) with low HIV incidence and prevalence. The census tract has the second smallest total population compared to the other communities, but the second highest housing unit density. Incidents of theft and vandalism were high; yet, crime rates were reported by residents to be low. A local business owner and community resident stressed that although her immediate area is safe, there are some neighborhoods within a five-block radius of her community that she “would not step foot in.” The exposure index is 0.9, but the sex ratio is relatively high (91.4). With respect to Communities A and B, Community C has a higher high school graduation percentage (83.5%) and lower percentages of public assistance (0%), unemployment (6.2%), poverty (10.3%), and female-headed households (12%).
There are many commercial and small businesses lining the streets. According to the participants’ maps, community residents have a variety of resources at their disposal, including supermarkets and health clinics. Compared to the other communities, Community C contains many medical resources for residents; however, there are no HIV/AIDS or STI agencies in the community. Residents noted that the one HIV awareness program the community had recently lost its funding and closed. Similar to Community B, the research team sensed a hostile attitude toward their presence; there may be a strict sense of boundaries between insiders and outsiders.
Surrounded by busy roads, the middle of Community C contains residences. At the center are estates which surround a large park. The estates are made up of large, twin homes that appear to be very well maintained. The team noted a strong sense of community unity among the residents; this particular community is historically known for its strong Irish and Italian presence. A local library employee believed that nine out of 10 residents in the community own their homes and that there are very few renters. These findings are consistent with statistics that Community C has the lowest number of vacant parcels (n = 21; see Figure 1).
Community C has the lowest rates of active engagement in the community (M = 0.40, SE = 0.08) and neighbors working together for improvement (M = 0.72, SE = 0.10), but high rates of neighbors’ willingness to help (M = 0.92, SE = 0.05). The census tract-level and ethnographic data combined suggest that the “quiet” feeling may come from individuals living separately, observing behavior of others to know who is part of their neighborhood, and being willing to help individual neighbors without getting involved collectively at the community level. As one resident described it, pockets of communities such as the estates around the park “take care of one another,” but everyone outside of those communities keeps to themselves.
Community D
Community D is predominantly White (86%) with high HIV incidence and prevalence. The community has the smallest total population of the four study areas, but has the highest population and housing density. The Exposure Index was also greatest in this tract (9%), indicating that Blacks are more likely to be exposed to Whites in this area. There were a high number of reported thefts; however, the other crimes were relatively low. It is also by far the most affluent community as judged by the rent prices, upkeep of the homes and apartment buildings, luxury vehicles pulling into garages, and the availability of spa services. The sex ratio was also highest in this community (96.7). Community D had the highest rates of education, with 96.9% of residents holding a high school diploma or GED. The community was tied with Community C for the lowest percentage of public assistance (0%), and had the lowest percentages of unemployment (4.3%), poverty (8.6%), and female-headed households (4.9%).
The community is mostly made up of homes and a few small businesses. There are also many expensive restaurants, bars, and clubs. A branch of a local university’s medical center is located in the community and appears to be one of the few medical resources in the area. Additional resources include a health clinic, a shelter for homeless populations, and a local labor federation. One health-related resource in the area provides confidential HIV testing and shows an educational film/drama about making choices to avoid contracting HIV.
The community overall is very quiet. Most people who were outside seemed to be involved in purposeful, directional activities (i.e., pushing a stroller, walking a dog, or riding a bike). Compared to the other four communities, all community and neighborhood indices for Community D were in the moderate range. This suggests individual residents maintain a mix of attachment to the community and focus on personal goals or personal space. The most interaction the researchers received was from local business owners who were very interested and curious about the project. However, residents did not seem to want to talk about the issue of HIV in their community.
During the mapping activity, individuals on the street and in restaurants who were willing to talk to the team described important sites of engagement around community behavior outside of the community boundaries. For example, business employees described a park outside of the Community D boundaries as an important place for residents. Although there are several shelters and related resources in Community D, a homeless man selling newspapers on the street said most homeless individuals do not go to shelters but instead congregate in a park near city hall.
Discussion
This study was a first step to disentangle relationships between community-level factors and potential risk for HIV in an HIV epicenter. The innovation of combining ethnography with GIS mapping and census tract-level data helped to provide a more contextualized understanding of HIV/AIDS in the targeted communities (Chirowodza et al., 2009). For example, ethnographic findings uncovered interesting phenomena, such as “corner houses” as prime locations for drug and sex trade. This has implications for HIV services and prevention efforts and can inform resource allocation for activities, including late night street outreach with safer sex kits, and/or increased police presence at certain cross streets. Moreover, the ethnographic mapping exercise demonstrated that the subjective and varied nature with which residents defined their neighborhoods could make it difficult to standardize interventions at a “neighborhood level.” The findings, however, provide support for block-level HIV prevention work—or at minimum efforts that engage geographical spaces smaller than census tracts. This will be particularly important in highly affected communities. Given that HIV risk increases with an individual’s probability of being exposed to an HIV-positive sexual partner (Friedman, Cooper, & Osborne, 2009); individuals in higher prevalence communities will have greater geobehavioral vulnerability to HIV and, thus, require concerted prevention efforts (Brawner, 2014). GIS mapping of census tract-level data can be used to identify areas in need of intervention (e.g., high HIV incidence and concentrated disadvantage), while ethnographic methodologies can be used to engage community residents and design sustainable strategies.
The findings also highlight stark sociodemographic differences within and across racial groups, and further substantiate the need for comprehensive, community-level HIV prevention interventions. Similar to other researchers (Adimora, Ramirez, Schoenbach, & Cohen, 2014; Bowleg et al., 2014; Raymond et al., 2014), we found that decreased economic opportunities, population density, residential segregation, high incidence of drug-related crimes, low educational attainment, and lack of access to a community-based HIV testing and treatment are complex drivers of the disproportionate HIV rates in Black communities. This provides insight for areas to target in the development of “culturally tailored and geographically circumscribed” strategies to curb the epidemic in high HIV prevalence areas (Nunn et al., 2014, p. 777).
There is significant variability in Philadelphia’s population descriptors, with higher concentrations of HIV/AIDS, crime, poverty, and poorer health outcomes in the city’s predominantly Black census tracts. These community-level factors may undergird both the decisions that individuals make about sexual behaviors, as well as the concentration of HIV in geographical and socially meaningful spaces (Johns, Bauermeister, & Zimmerman, 2010). Above and beyond race, and similar to previous findings (Cubbin, Santelli, Brindis, & Braveman, 2005; Vaughan, Rosenberg, Shouse, & Sullivan, 2014), community context had a substantial influence on the HIV epidemic. Specifically, this study demonstrates that HIV incidence and prevalence rates trend with social and structural factors, such as overcrowding, disadvantage, limited permeability of neighborhood boundaries, and hampered availability and accessibility of health-related resources.
From an assets-based perspective, the results reveal that there may be protective factors in certain communities that buffer risk. For example, Community A had similar sociodemographic characteristics as Community B (e.g., percent living in poverty), yet, Community A had fewer criminal incidents, as well as lower HIV incidence and prevalence rates. The same was true for Communities C and D. What factors in communities A and C helped to mediate the well-documented link between poverty and crime in these areas? Philadelphia’s history of discriminatory housing policies, economic disinvestment, and gentrification may partially explain these disparities; neighborhoods most vulnerable for historical or geographic reasons are subject to these dynamics. Further exploration of social, economic, political, and environmental factors that either protect against or increase risk for HIV is warranted. Our comparison of neighborhoods by racial composition, HIV status, and structural and social characteristics, demonstrates that there are complex interactions which warrant additional investigation in a citywide endeavor.
Limitations
The use of census tracts as the unit of analysis made it difficult to ascertain socially meaningful geographic spaces for community members. Asking residents to map their own community, and then intervening in those ascribed communities, may be more effective in intervention planning. The analysis of data from multiple time points further complicated the shortcomings of cross-sectional analyses. A longitudinal analysis would have greatly strengthened the approach. Additionally, because PHMC used small area estimation for their data, we did not know the sample size for respondents in each census tract. Lastly, given the small number of communities, the study was not powered to conduct advanced statistical analyses. Future studies could examine a citywide approach and incorporate multilevel modeling.
Conclusion
Novel strategies are needed to decrease HIV transmission in highly affected/high prevalence areas, and to prevent the spread of HIV to unaffected/low prevalence areas. Combined prevention strategies—inclusive of individual, social and structural approaches—are feasible, and quite frankly, necessary, to curb the HIV pandemic. For example, a three pronged approach, targeted to a small, circumscribed geographic area, could focus on: (a) individual education and skills training; (b) increased social capital among community residents to promote health and improve neighborhood social order and safety; and (c) implementing microfinance interventions to reverse the effects of historically inequitable economic and political practices. Actively engaged community health research, in concert with GIS technology, can continue to develop this area of science.
Acknowledgments
The authors acknowledge this study was funded by pilot funding awarded to Dr. Brawner through the National Institute of Mental Health R25MH087217 (Guthrie, Schensul and Singer, PIs).
The authors thank the Cartographic Modeling Lab (CML) at the University of Pennsylvania, especially the efforts of the CML Executive Director, Tara Jackson, PhD, in preparing the spatial database for the analyses. The authors are also grateful to the study participants, and thank research assistants Ashley DeShazo, BS, Jazz Robinson, and Danielle Stevenson, BS, for their assistance with data collection.
Footnotes
The authors have no conflicts of interest to report.
Contributor Information
Bridgette M. Brawner, Center for Health Equity Research, Center for Global Women's Health, University of Pennsylvania School of Nursing, Philadelphia, Pennsylvania..
Janaiya L. Reason, Center for Health Equity Research, Center for Global Women's Health, University of Pennsylvania School of Nursing, Philadelphia, Pennsylvania..
Bridget A. Goodman, Graduate School of Education, Nazarbayev University, Astana, Republic of Kazakhstan ..
Jean J. Schensul, Institute for Community Research, Hartford, Connecticut..
Barbara Guthrie, Director of the Nursing PhD Program, Northeastern University, Boston, Massachusetts..
References
- Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2010;55(Suppl 2):S132–S135. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adimora AA, Ramirez C, Schoenbach VJ, Cohen MS. Policies and politics that promote HIV infection in the Southern United States. AIDS. 2014;28:1393–1397. doi: 10.1097/QAD.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ArcGIS. ArcGIS for Desktop (Version 10.1): Esri. 2012 [Google Scholar]
- Blankenship KM, West BS, Kershaw TS, Biradavolu MR. Power, community mobilization, and condom use practices among female sex workers in Andhra Pradesh, India. AIDS. 2008;22:S109–S116. doi: 10.1097/01.aids.0000343769.92949.dd. [DOI] [PubMed] [Google Scholar]
- Blommaert J, Jie D. Ethnographic fieldwork: A beginner’s guide. Bristol, UK: Multilingual Matters; 2010. [Google Scholar]
- Bowleg L, Neilands TB, Tabb LP, Burkholder GJ, Malebranche DJ, Tschann JM. Neighborhood context and Black heterosexual men’s sexual HIV risk behaviors. AIDS and Behavior. 2014;18(11):2207–2218. doi: 10.1007/s10461-014-0803-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, Raj A. Shared communities, structural contexts, and HIV risk: Prioritizing the HIV risk and prevention needs of Black heterosexual men. American Journal of Public Health. 2012;102:S173–S177. doi: 10.2105/AJPH.2011.300342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brawner BM. A multilevel understanding of HIV/AIDS disease burden among African American women. J Obstet Gynecol Neonatal Nurs. 2014;43(5):633–643. doi: 10.1111/1552-6909.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brawner BM, Gomes MM, Jemmott LS, Deatrick JA, Coleman CL. Clinical depression and HIV risk-related sexual behaviors among African-American adolescent females: Unmasking the numbers. AIDS Care. 2012;24:618–625. doi: 10.1080/09540121.2011.630344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–746. [Google Scholar]
- Chirowodza A, van Rooyen H, Joseph P, Sikotoyi S, Richter L, Coates T. Using participatory methods and geographic information systems (GIS) to prepare for an HIV community-based trial in Vulindlela, South Africa (Project Accept-HPTN 043) Journal of Community Psychology. 2009;37:41–57. doi: 10.1002/jcop.20294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- City of Philadelphia. Percentage Black population, 2010. 2010a Retrieved from http://www.phila.gov/CityPlanning/resources/Maps/Black_Percentage_Population_2010.pdf.
- City of Philadelphia. Percentage White population, 2010. 2010b Retrieved from http://www.phila.gov/CityPlanning/resources/Maps/White_Percentage_Population_2010.pdf.
- Cubbin C, Santelli J, Brindis CD, Braveman P. Neighborhood context and sexual behaviors among adolescents: Findings from the National Longitudinal Study of Adolescent Health. Perspectives on Sexual and Reproductive Health. 2005;37:125–134. doi: 10.1363/psrh.37.125.05. [DOI] [PubMed] [Google Scholar]
- Das M, Chu PL, Santos G-M, Scheer S, Vittinghoff E, McFarland W, Colfax GN. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5:e11068. doi: 10.1371/journal.pone.0011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhart MG, Yehia BR, Hillier A, Voytek CD, Blank MB, Frank I, …Brady KA. Behind the cascade: Analyzing spatial patterns along the HIV care continuum. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2013;64:S42–S51. doi: 10.1097/QAI.0b013e3182a90112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Aral S. Social networks, risk-potential networks, health, and disease. Journal of Urban Health. 2001;78:411–418. doi: 10.1093/jurban/78.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Cooper HLF, Osborne AH. Structural and social contexts of HIV risk among African Americans. American Journal of Public Health. 2009;99:1002–1008. doi: 10.2105/AJPH.2008.140327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Généreux M, Bruneau J, Daniel M. Association between neighbourhood socioeconomic characteristics and high-risk injection behaviour amongst injection drug users living in inner and other city areas in Montréal, Canada. International Journal of Drug Policy. 2010;21:49–55. doi: 10.1016/j.drugpo.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Hammett TM, Drachman-Jones A. HIV/AIDS, sexually transmitted diseases, and incarceration among women: National and southern perspectives. Sexually Transmitted Diseases. 2006;33:S17–S22. doi: 10.1097/01.olq.0000218852.83584.7f. [DOI] [PubMed] [Google Scholar]
- Israel BA, Eng E, Schultz AJ, Parker EA. Methods for community-based participatory research for health. 2nd ed. San Francisco, CA: Jossey-Bass; 2012. [Google Scholar]
- Jiang J, Lahiri P. Mixed model prediction and small area estimation. TEST. 2006;15:1–96. [Google Scholar]
- Johns MM, Bauermeister JA, Zimmerman MA. Individual and neighborhood correlates of HIV testing among African American youth transitioning from adolescence into young adulthood. AIDS Education and Prevention. 2010;22:509–522. doi: 10.1521/aeap.2010.22.6.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr JC, Valois RF, Siddiqi A, Vanable P, Carey MP. Neighborhood condition and geographic locale in assessing HIV/STI risk among African American adolescents. AIDS and Behavior. 2014 doi: 10.1007/s10461-014-0868-y. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeCompte MD, Schensul JJ. Ethics in ethnography: A mixed methods approach. 2nd ed. Lanham, MD: AltaMira Press; 2014. [Google Scholar]
- Lindberg LD, Orr M. Neighborhood-level influences on young men’s sexual and reproductive health behaviors. American Journal of Public Health. 2011;101:271–274. doi: 10.2105/AJPH.2009.185769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey DS, Denton NA. Trends in the residential segregation of Blacks, Hispanics, and Asians: 1970–1980. American Sociological Review. 1987;52:802–825. [Google Scholar]
- McQuiston C, Parrado EA, Olmos-Muñiz JC, Bustillo Martinez AM. Community-based participatory research and ethnography: The perfect union. In: Israel BA, Eng E, Schultz AJ, Parker EA, editors. Methods in community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2005. pp. 210–229. [Google Scholar]
- Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of Black men who have sex with men: A critical literature review. American Journal of Public Health. 2006;96:1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunn A, Dickman S, Cornwall A, Rosengard C, Kwakwa H, Kim D, …Mayer KH. Social, structural and behavioral drivers of concurrent partnerships among African American men in Philadelphia. AIDS Care. 2011;23:1392–1399. doi: 10.1080/09540121.2011.565030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunn A, Yolken A, Cutler B, Trooskin S, Wilson P, Little S, Mayer K. Geography should not be destiny: Focusing HIV/AIDS implementation research and programs on microepidemics in US neighborhoods. American Journal of Public Health. 2014;104:775–780. doi: 10.2105/AJPH.2013.301864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philadelphia City Planning Commission. City stats: General demographic and economic data. 2005 Retrieved from http://www.phila.gov/CityPlanning/resources/Data/citystats05.pdf.
- Philadelphia Department of Public Health AIDS Activities Coordinating Office (AACO) Annual surveillance report 2008: HIV/AIDS in Philadelphia: Cases reported through June 2009. Philadelphia, PA: Philadelphia Department of Public Health; 2008. http://www.phila.gov/health/pdfs/Epi_Update_2008.pdf. [Google Scholar]
- Philadelphia Department of Public Health AIDS Activities Coordinating Office (AACO) Annual surveillance report 2009: HIV/AIDS in Philadelphia: Cases reported through June 2010. Philadelphia, PA: Philadelphia Department of Public Health; 2009. http://www.phila.gov/health/pdfs/2009%20Surveillance%20Annual%20Report.pdf. [Google Scholar]
- Philadelphia Department of Public Health AIDS Activities Coordinating Office (AACO) Survelliance report 2010: HIV/AIDS in Philadelphia: Cases reported through June 2011. Philadelphia, PA: Philadelphia Department of Public Health; 2010. http://www.phila.gov/health/pdfs/2010SurveillanceReportFinal.pdf. [Google Scholar]
- Raiford JL, Herbst JH, Carry M, Browne FA, Doherty I, Wechsberg WM. Low prospects and high risk: Structural determinants of health associated with sexual risk among young African American women residing in resource-poor communities in the South. American Journal of Community Psychology. 2014;54(3-4):243–250. doi: 10.1007/s10464-014-9668-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond HF, Chen Y-H, Syme SL, Catalano R, Hutson MA, McFarland W. The role of individual and neighborhood factors: HIV acquisition risk among high-risk populations in San Francisco. AIDS and Behavior. 2014;18:346–356. doi: 10.1007/s10461-013-0508-y. [DOI] [PubMed] [Google Scholar]
- Rudolph AE, Linton S, Dyer TP, Latkin C. Individual, network, and neighborhood correlates of exchange sex among female non-injection drug users in Baltimore, MD (2005–2007) AIDS and Behavior. 2012;17:598–611. doi: 10.1007/s10461-012-0305-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ. The neighborhood context of well-being. Perspectives in Biology and Medicine. 2003;46:S53–S64. [PubMed] [Google Scholar]
- Schensul JJ, LeCompte MD. Specialized ethnographic methods: A mixed methods approach. 2nd ed. Vol. 4. Lanham, MD: Altamira Press; 2012. [Google Scholar]
- Schensul JJ, LeCompte MD, Trotter RT, II, Cromley EK, Singer M. Mapping social networks, spatial data, and hidden populations. Lanham, MD: AltaMira Press; 1999. [Google Scholar]
- Schensul JJ, Levy JA, Disch WB. Individual, contextual, and social network factors affecting exposure to HIV/AIDS risk among older residents living in low-income senior housing complexes. Journal of Acquired Immune Deficiency Syndromes. 2003;33(Suppl 2):S138–S152. doi: 10.1097/00126334-200306012-00011. [DOI] [PubMed] [Google Scholar]
- Singer M. Something dangerous: Emergent and changing illicit drug use and community health. Long Grove, IL: Waveland Press; 2006. [Google Scholar]
- Smedley BD. The lived experience of race and its health consequences. American Journal of Public Health. 2012;102:933–935. doi: 10.2105/AJPH.2011.300643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumartojo E, Doll L, Holtgrave D, Gayle H, Merson M. Enriching the mix: Incorporating structural factors into HIV prevention. AIDS. 2000;14(Suppl 1):S1–S2. doi: 10.1097/00002030-200006001-00001. [DOI] [PubMed] [Google Scholar]
- Tan JY, Earnshaw VA, Pratto F, Rosenthal L, Kalichman S. Social-structural indices and between-nation differences in HIV prevalence. Int J STD AIDS. 2015;26(1):48–54. doi: 10.1177/0956462414529264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. Census Tracts and Block Numbering Areas. In: Geography Division, editor. Geographic Areas Reference Manual (pp. 10.11-10.17) Washington, DC: U.S. Census Bureau; 1994. Retrieved from http://www.census.gov/geo/reference/pdfs/GARM/Ch10GARM.pdf. [Google Scholar]
- U.S. Census Bureau. Profile of general demographic characteristics: Philadelphia County, PA. 2000b Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF.
- U.S. Census Bureau. 2005–2009 American community survey 5-year estimates. 2010a Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_09_5YR_DP5YR3&prodType=table.
- U.S. Census Bureau. 2010 census interactive population search. 2010b Retrieved from http://www.census.gov/2010census/popmap/ipmtext.php.
- Vaughan AS, Rosenberg E, Shouse RL, Sullivan PS. Connecting race and place: A county-level analysis of White, Black, and Hispanic HIV prevalence, poverty, and level of urbanization. American Journal of Public Health. 2014;104:e77–e84. doi: 10.2105/AJPH.2014.301997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein N, Duran B, Minkler M, Foley K. Developing and maintaining partnerships with communities. In: Israel BA, Eng E, Schultz AJ, Parker EA, editors. Methods in community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2005. pp. 31–51. [Google Scholar]
- Youm Y, Laumann EO. Social network effects on the transmission of sexually transmitted diseases. Sexually Transmitted Diseases. 2002;29:689–697. doi: 10.1097/00007435-200211000-00012. [DOI] [PubMed] [Google Scholar]