Abstract
Background and Aims:
Clinician-family communication must be effective for medical decision making in any Intensive Care Unit (ICU) setting. We performed a prospective study to assess the effectiveness of communication to families of critically ill neurosurgical patients based on the two criteria of comprehension and satisfaction.
Materials and Methods:
The study was conducted on 75 patients in a 15 bedded neurosurgical ICU. An independent investigator assessed the comprehension and satisfaction of families between the 3rd and the 5th day of admission in ICU. Comprehension was tested using three components, that is, comprehension of diagnosis, prognosis and treatment. The satisfaction was measured using a modified version of the Critical Care Family Needs Inventory (CCFNI) (score of 56-extreme dissatisfaction and 14-extreme satisfaction).
Results:
Poor comprehension was noted in 52 representatives (71.2%). The mean satisfaction score as measured by the CCFNI score was 28. Factors associated with poor comprehension included increasing age of patient representative (P = 0.024), higher simplified acute physiology score (P = 0.26), nonoperated patients (P = 0.0087) and clinician estimation of poor prognosis (P = 0.01). Operated patients had significantly better satisfaction score (P = 0.04).
Conclusion:
Families of patients were reasonably satisfied, but had poor comprehension levels of the patient's illness. The severity of the patient's illness, poor prognosis as estimated by the physician and nonoperated patients were independent predictors of poor comprehension. Extra effort to communicate with patient representatives at risk of poor comprehension and provision of a family information leaflet could possibly remedy this situation.
Keywords: Clinician, communication, comprehension, critical care, family representatives, Intensive Care Unit, satisfaction
Introduction
In an intensive care setting, clinical decision making hinges on clinician — family communication. Intensive Care Unit (ICU) clinicians face an uphill task of providing family members with appropriate, clear and compassionate information they need, to participate in making decisions about patients who are unable to speak for themselves as well as coping with their own emotional distress. The receipt of honest, intelligible and timely information is among the primary concerns of family members of patients in the ICU.[1] Poor communication can adversely affect clinical decision making, family satisfaction and the psychological outcomes of family members. Studies have shown that half the families of ICU patients experience inadequate communication with their physicians[2] and health care providers often do not recognize poor family comprehension.[3]
Effectiveness of communication to family members of ICU patients can be assessed on two basic criteria of comprehension, and satisfaction with information provided by ICU clinician to family members. Family members must understand the diagnosis, prognosis and treatment if they are to participate in making management decisions and to speak for the patient. A good comprehension plays an important role in helping the family cope up with the psychological stress associated with the ICU admission.
In spite of rapid advances in critical care made in India, no study has yet reported on the effectiveness of communication between clinician and families of patients admitted in ICU. As this key component of ICU care needed better elucidation, we set out to study the effectiveness of communication between treating clinicians and the families of patients admitted in our neurosurgical ICU. Along with this, we measured the level of family satisfaction with care in the ICU as defined by the Critical Care Family Needs Inventory Scale (CCFNI).[4]
Materials and Methods
Our study was conducted in a 15-bed neurosurgical ICU in a teaching hospital in North India. One junior clinician was present round the clock in the ICU and a senior clinician was on-call, though not present in the ICU all the time.
Inclusion criteria
All patients admitted in neurosurgical ICU with expected length of stay at least 48 h. This included patients with moderate and severe head injury, spinal injury and patients recovering from elective cranial surgery.
Exclusion criteria
Patients who died or were discharged within 48 h of admission were excluded from the study.
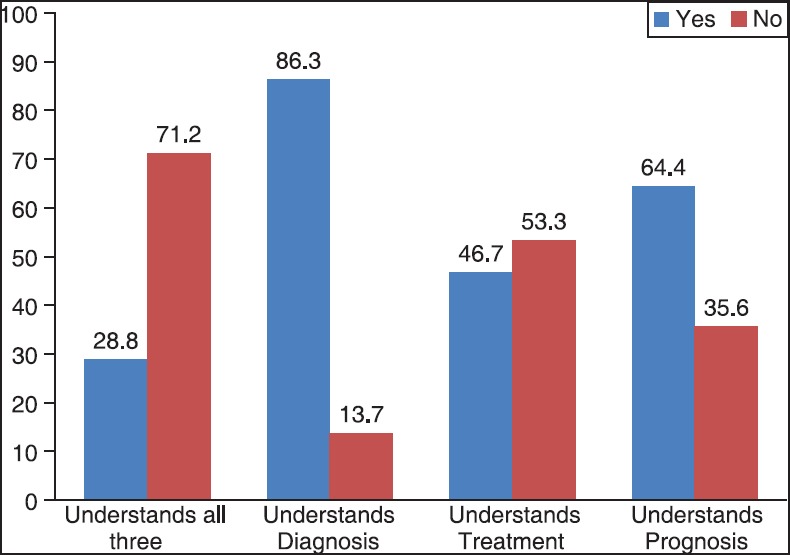
Sample size
Assuming 25% satisfaction, sample size was calculated as n = 4pq/d2 (where P = 25%, q = 1−p, d = 10%)
Therefore, 75 subjects were recruited into the study.
Patient's representatives
The representative was defined as a spouse or close relative who was present at the regular physician-family meeting held at a designated time in the morning and was specifically designated by the family to speak for and represent the family. Those who consented for the study were asked to complete a questionnaire, the modified CCFNI.
Caregivers (clinicians)
The clinician who met with the family on the day of admission and provided the information on the condition of the patient was interviewed by the investigator. All the possible disease processes of the patient, the different treatments being carried out and the prognosis was recorded on the prescribed format by the investigator based on this interview with the clinician.
Method of assessment
An independent investigator assessed the comprehension and satisfaction of the families of patients between the 3rd and the 5th day of the patient admission in ICU. For each patient, the following information was recorded: Age, sex, geographic origin, marital status, occupation, reasons for ICU admission and clinical status at admission including the simplified acute physiology score (SAPS II) score[5] and Glasgow coma scale score. Higher the SAPS II score, greater was the severity of illness. The investigator also entered the expected prognosis of the patient as per the treating clinician. Only one family member was interviewed, preferably the spouse or the closest relative of the patient.
All patient representatives were told that a study of their needs was on going and that they could participate in the study by completing a questionnaire. Family representatives entered the following data on a standardized questionnaire: Age, sex, relationship to the patient, occupation and distance from the house to the hospital, accommodation in hospital and how satisfied they were with the information provided by senior and junior clinicians.
Instruments to measure the effectiveness of information provided to family representatives
This interview used three prospectively defined components, as previously described in the paper by Azoulay et al.[2] Comprehension of the diagnosis defined as knowledge of which organ was primarily involved in the disease process, comprehension of the prognosis, defined as knowledge of the patient's condition: Whether he/she was expected to improve, not expected to improve, not expected to survive and comprehension of the treatment, defined as knowledge of at least one of the major treatments used among the list given by the clinicians. Poor comprehension was defined as failure to understand any one of the three components, and good comprehension as understanding all three components.
“I don’t know” answers were taken as indicating absence of comprehension.
We measured the satisfaction with care received using a modified version of the CCFNI.[4,6,7,8] CCFNI results were determined as follows: Each item received a score between 1 (indicating extreme satisfaction) and 4 (indicating extreme dissatisfaction). The satisfaction score was calculated as the sum of the scores on all 14 items; thus, the smallest possible score was 14 (extreme satisfaction) and the highest possible score was 56 (extreme dissatisfaction).
Statistical analysis
Data was entered into Epidata version 3.0 (Odense, Denmark), a public domain data entry program, and then exported to the Statistical Package for Social Sciences (SPSS) version 8.0 (Statistical Analysis, The Statistical Package for Social Sciences Inc, Chicago, IL) for analysis. Percentages were calculated for baseline characteristics and other discrete data. For continuous data, mean or median was calculated depending on whether the data were normally distributed or not. Factors affecting comprehension were analyzed using multiple logistic regression and adjusted odds ratios and statistically significant variables at an alpha level of 5% identified. Factors affecting satisfaction (CCFNI score) were identified using multiple linear regression.
Results
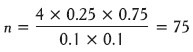
Results size was 75 patients and we recruited 75 patients. Two patients were rejected because of inadequate data to compile the SAPS II score. Sixty-six patients (90.4%) were admitted as emergency whereas 7 patients (9.6%) were elective admissions. Fifty patients (68.5%) were admitted secondary to trauma and 23 (31.5%) patients did not have trauma. Forty-one patients (56.2%) had a surgical operation while 32 were nonoperative [Figure 1]. The severity of the illness was measured by the SAPS II score. In our patients SAPS II score ranged from 4 to 55 with a mean of 27.3.
Figure 1.
Baseline patient characteristics
The average age of patient representative or relative was 38.2 (range: 10-72 years). Fifty-eight patient representatives were literate (79.5%) while 15 were illiterate (20.5%). Literacy was defined as ability to read and write and sign their names.
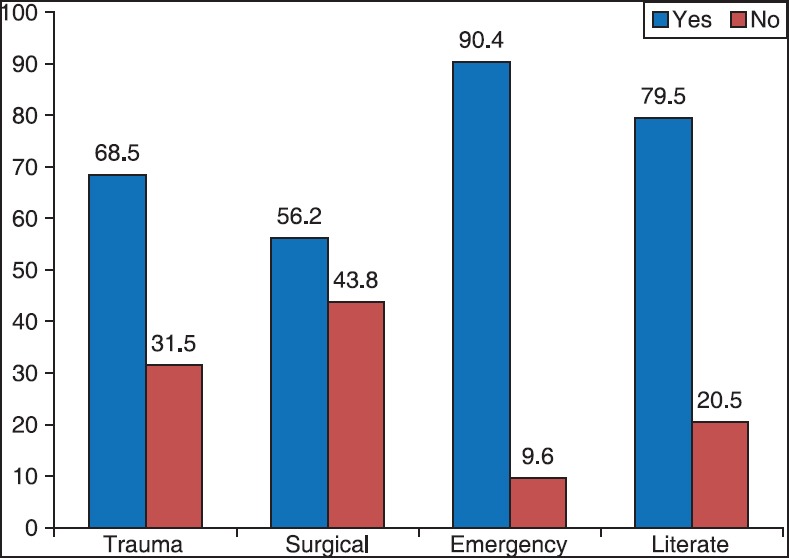
Comprehension by the representatives
Failure to comprehend the diagnosis, prognosis and treatment were noted in 52 representatives (71.2%). Ten representatives (13.7%) did not comprehend the diagnosis, 39 representatives (53.4%) did not comprehend the treatment and 26 representatives (35.6%) did not comprehend the prognosis. All the representatives were assessed by a single investigator. Only 21 out of 73 patients (28.8%) understood all three components of comprehension [Figure 2].
Figure 2.
Comprehension of information by patient representatives
Patient representative satisfaction as measured by critical care family needs inventory score
The mean satisfaction score was 28.4 (standard deviation = 5.89) with a range between 15 and 41. The median score was 30 (a score of 14 denotes extreme satisfaction and a 56 denotes extreme dissatisfaction).
Factors associated with poor comprehension
We compared age and literacy level of representative, whether patient was admitted as elective/emergency, operative/nonoperative, SAPS II score, and prognosis for survival as estimated by physician as independent predictors for comprehension. A multivariate analysis was done using the SPSS version 8.0. As shown in Table 1, the likelihood of poor comprehension was greater for increasing age of patient representative (P = 0.024), higher SAPS II scores (P = 0.026) nonoperated patients (P = 0.0087), and physician estimation of poor prognosis (P = 0.01). The latter two factors were highly significant as the adjusted odds ratio for nonoperated patients was 15.05 and for poor prognosis it was 40.13.
Table 1.
Multivariate analysis of comprehension upon various predictor variables
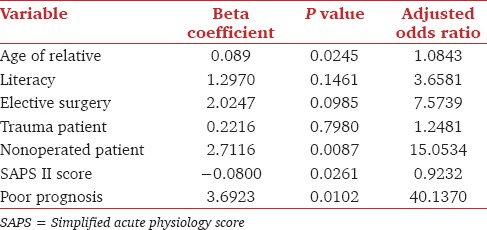
The literacy level, whether elective/emergency, trauma versus nontrauma did not show any significant statistical association with comprehension.
Factors associated with poor satisfaction score
We compared the above factors and comprehension as predictors of poor satisfaction (CCFNI score). Comprehension or the lack of it did not significantly affect the satisfaction. The operated patients had significantly better satisfaction score (P = 0.04). Satisfaction was not affected by severity of illness (SAPS II score), prognosis as estimated by the physician, or whether elective versus emergency admission.
Discussion
Clinician-family communication has to be adequate and effective for medical decision making. We attempted to evaluate the quality of communication by looking at comprehension and satisfaction levels in family members of patients.
We tried to assess how well the families understood medical information provided at ICU admission. Poor comprehension levels probably reflect failure to understand information conveyed by the clinicians, failure to recall information that was received and understood at some point, or failure to receive information. We found that only 28.6% understood all three components of the comprehension- namely diagnosis, prognosis, and treatment. Treatment was the facet most likely to be poorly comprehended (53.42%) followed by prognosis (35.6%) and diagnosis (13.7%). Comparable studies done by Azoulay et al.[2] showed a poor comprehension of 54% which dropped to 26.3% 2 years later[9] because of new interventions and lessons learnt. Although comprehension of representatives was poor, they were reasonably satisfied with the treatment the patient was receiving. The median satisfaction score (CCFNI score) in our study was 30 as compared to 22 in a previous study.[9] Surprisingly, comprehension (which has been shown in other studies to be a predictor of satisfaction) was not correlated with satisfaction in our study.
Our study found that younger representatives comprehended better (P = 0.024). It could be because the younger generation is more inclined to access medical information via media and internet, so has better awareness about medical conditions and treatment options in the ICU. The representatives of patients who had higher SAPS II score had poorer comprehension (P = 0.026). Also higher the estimation of grave prognosis as per the treating clinician, poorer was the comprehension (P = 0.01). This was highly significant as the adjusted odds ratio showed a value over 40. A possible explanation is that greater the severity of illness, information is not conveyed adequately to the representatives. This could be due to the demanding and difficult nature of this task and ICU clinicians consider breaking bad news to be the most stressful part of their job. Another reason could be initial stages of grief in relatives leading to a denial of the gravity of the illness. A suggestion to improve comprehension would be to identify patients with increased severity of illness and poorer prognosis and spend extra time and effort to interact and educate the representatives of these patients, so that they can participate better in decision making in the ICU.
Representatives of operated patients comprehended better (P = 0.0087) and satisfaction scores (P = 0.04) were also better. This was probably due to the fact that the clinician takes more time and effort to explain the nature of the illness and the prognosis before taking up a patient for surgery. Other similar studies have identified other factors related to poor comprehension by family member such as age, unemployment, admission for acute respiratory failure and unfavorable prognosis.[2]
Communication between clinician and families is the most important, but least accomplished factor in the quality of care in ICU.[10] If caregivers and family members are to work together to determine what is best for the patient, then the family members must have a reasonable level of comprehension of the patient's problems and be reasonably satisfied with the ICU. The manner in which health care workers communicate and the way in which family members are included in medical care and decision making can affect long term outcomes. Adverse psychological outcomes like posttraumatic stress, anxiety, depression etc., in family members of ICU patients is termed post intensive care syndrome-family.[11] Over the last decade, the concept of family centered care has been developed in which attention is given to meeting the emotional and informational needs of family members. The information provided helps family members to cope with their distress and to build reasonable expectations about the patient's outcome.
Written leaflets can be an effective way to provide information. Families given an informational brochure during their first visit to the ICU were more likely to understand patient prognosis than those who had not received such information. Azoulay et al.[9] improved both comprehension and communication in family representatives by giving a family information leaflet which explained the care given within the ICU, a simple description of the commonly used devices used within the ICU, the contact information of the care givers, the visiting hours and why the visiting hours are restricted.
Written resources provide an opportunity to revisit the information at a later time as caregivers may not be able to retain verbal information provided.[12] A similar intervention adapted to the Indian environment can be tried to improve communication. One important limitation of this study is that all factors affecting comprehension were not studied. Experienced clinicians can convey information more clearly to the families. This factor (senior or junior clinician conveying information) could have affected comprehension. Our comprehension criteria were much stricter than comparable studies done in the western world where good comprehension was defined as knowledge of any one of the three aspects of comprehension whereas our criteria defined good comprehension as knowledge of all three aspects of comprehension.
Conclusion
We evaluated the effectiveness of communication with families of critically ill-patients. Although the patient representatives in our study had reasonably good satisfaction with the care of their patient in the ICU, their comprehension level of the patient's illness was poor (71.2%). The severity of the patient's illness, poor prognosis as estimated by the clinician and nonoperated patients were independent predictors of poor comprehension.
This study reinforces the suspected notion that clinicians in the ICU often do not recognize poor family comprehension. Care givers should spend extra time and effort in communicating with families of patients with increased severity of illness and those patients perceived to have poorer prognosis. It is recommended that a family information leaflet be made available to families to further improve communication.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: Family rounds in the intensive care unit. Am J Crit Care. 2010;19:421–30. doi: 10.4037/ajcc2010656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Azoulay E, Chevret S, Leleu G, Pochard F, Barboteu M, Adrie C, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044–9. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez RM, Navarrete E, Schwaber J, McKleroy W, Clouse A, Kerrigan SF, et al. A prospective study of primary surrogate decision makers’ knowledge of intensive care. Crit Care Med. 2008;36:1633–6. doi: 10.1097/CCM.0b013e31816a0784. [DOI] [PubMed] [Google Scholar]
- 4.Harvey MA, Ninos NP, Adler DC, Goodnough-Hanneman SK, Kaye WE, Nikas DL. Results of the consensus conference on fostering more humane critical care: Creating a healing environment. Society of Critical Care Medicine. AACN Clin Issues Crit Care Nurs. 1993;4:484–549. [PubMed] [Google Scholar]
- 5.Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63. doi: 10.1001/jama.270.24.2957. [DOI] [PubMed] [Google Scholar]
- 6.Azoulay E, Pochard F, Chevret S, Lemaire F, Mokhtari M, Le Gall JR, et al. Meeting the needs of intensive care unit patient families: A multicenter study. Am J Respir Crit Care Med. 2001;163:135–9. doi: 10.1164/ajrccm.163.1.2005117. [DOI] [PubMed] [Google Scholar]
- 7.Molter NC. Needs of relatives of critically ill patients: A descriptive study. Heart Lung. 1979;8:332–9. [PubMed] [Google Scholar]
- 8.Lilly CM, De Meo DL, Sonna LA, Haley KJ, Massaro AF, Wallace RF, et al. An intensive communication intervention for the critically ill. Am J Med. 2000;109:469–75. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]
- 9.Azoulay E, Pochard F, Chevret S, Jourdain M, Bornstain C, Wernet A, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: A multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med. 2002;165:438–42. doi: 10.1164/ajrccm.165.4.200108-006oc. [DOI] [PubMed] [Google Scholar]
- 10.Arnold JN, Prendergast T, Emlet L, Weinstein E, Barnato A, Back A. Educational Modules for the Critical Care Communication (C3) Course — A Communication Skills Training Program for Intensive Care Fellows. 2010 [Google Scholar]
- 11.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: Postintensive care syndrome-family. Crit Care Med. 2012;40:618–24. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 12.MacIsaac L, Harrison MB, Godfrey C. Supportive care needs of caregivers of individuals following stroke: A synopsis of research. Can J Neurosci Nurs. 2010;32:39–46. [PubMed] [Google Scholar]


