Abstract
Objective To examine the association of hospital volume (a marker of quality of care) with hospital readmission rates.
Design Retrospective cross-sectional study.
Setting 4651US acute care hospitals.
Study data 6 916 644 adult discharges, excluding patients receiving psychiatric or medical cancer treatment.
Main outcome measures We used Medicare fee-for-service data from 1 July 2011 to 30 June 2012 to calculate observed-to-expected, unplanned, 30 day, standardized readmission rates for hospitals and for specialty cohorts medicine, surgery/gynecology, cardiorespiratory, cardiovascular, and neurology. We assessed the association of hospital volume by quintiles with 30 day, standardized readmission rates, with and without adjustment for hospital characteristics (safety net status, teaching status, geographic region, urban/rural status, nurse to bed ratio, ownership, and cardiac procedure capability. We also examined associations with the composite outcome of 30 day, standardized readmission or mortality rates.
Results Mean 30 day, standardized readmission rate among the fifth of hospitals with the lowest volume was 14.7 (standard deviation 5.3) compared with 15.9 (1.7) among the fifth of hospitals with the highest volume (P<0.001). We observed the same pattern of lower readmission rates in the lowest versus highest volume hospitals in the specialty cohorts for medicine (16.6 v 17.4, P<0.001), cardiorespiratory (18.5 v 20.5, P<0.001), and neurology (13.2 v 14.0, p=0.01) cohorts; the cardiovascular cohort, however, had an inverse association (14.6 v 13.7, P<0.001). These associations remained after adjustment for hospital characteristics except in the cardiovascular cohort, which became non-significant, and the surgery/gynecology cohort, in which the lowest volume fifth of hospitals had significantly higher standardized readmission rates than the highest volume fifth (difference 0.63 percentage points (95% confidence interval 0.10 to 1.17), P=0.02). Mean 30 day, standardized mortality or readmission rate was not significantly different between highest and lowest volume fifths (20.4 v 20.2, P=0.19) and was highest in the middle fifth of hospitals (range 20.6–20.8).
Conclusions Standardized readmission rates are lowest in the lowest volume hospitals—opposite from the typical association of greater hospital volume with better outcomes. This association was independent of hospital characteristics and was only partially attenuated by examining mortality and readmission together. Our findings suggest that readmissions are associated with different aspects of care than mortality or complications.
Introduction
There is a well established relationship between volume of work and outcomes in healthcare, particularly for surgery. High patient volume for practitioners or hospitals has been associated with reduced complications or mortality after numerous surgical procedures1 2 3 4 5 6 7 8 9 10 11 as well as some non-surgical conditions.12 13 14 As a result, the Leapfrog Group has advocated that patients be steered towards institutions with higher volume for certain procedures,15 and the Agency for Healthcare Research and Quality has created seven metrics of facility volume for major surgical procedures.16 17 The Centers for Medicare and Medicaid Services publicly reports these volume measures for US acute care hospitals to inform consumer choice.18
To date, only a few studies have examined the association of surgical volume with a different outcome: readmission. Of these, some have found that increased volume is associated with reduced readmission rates,19 20 21 but several have not.22 23 24 25 One study of patients with heart failure found that low volume hospitals had slightly higher readmission rates.26 To our knowledge, there are no other studies of volume and readmission in medical patients.
Given the intense national focus on improving transitions in care coupled with continued uncertainty as to the best means of doing so, it is important to understand whether increased patient volume is associated with better performance on readmission rates. Higher hospital volume may be associated with lower readmission rates, as is the case for other outcomes. However, readmission represents a different (but overlapping) quality domain than mortality and complications, reflecting not only the technical quality and safety of inpatient care but attention to care transitions,27 patient care strategies that address increased patient frailty after hospitalization,28 and post-acute care coordination and follow-up.29 30 A high patient volume and turnover might impede the provision of high quality transitional care instead of facilitating better outcomes. Furthermore, since clinicians are often unaware of readmissions,31 institutions may not be able to improve practice in response to readmissions in the same way they are able to respond to visible complications or inpatient mortality.32 It is also possible that the lower mortality rate of high volume hospitals produces more opportunity for surviving patients to be readmitted. Finally, effects might differ according to patient population. Increased patient volume might reduce readmission rates for surgical patients by increasing technical skill, because readmissions in these patients are often related to postoperative complications. Higher volume might not, however, promote better performance on transitional care for non-surgical patients. There are, therefore, several reasons to hypothesize that readmissions may not have the same relationship with volume as other outcomes such as complications and mortality.
Consequently, we examined the association between risk-standardized readmission rates and hospital volume for Medicare patients in order to determine whether there is a volume-outcome relationship for readmissions overall and for cohorts of patients by specialty.
Methods
Study data
We used 2010-12 Medicare inpatient claims data combined with the Medicare enrollment file to obtain data on discharges, risk adjustment variables, and outcomes.
Study cohort
For this analysis, we adopted the cohort definition of the publicly reported, hospital-wide, 30 day readmission measure.33 34 Briefly, we included all discharges between 1 July 2011 and 30 June 2012 from US short term acute care or critical access hospitals of patients who had Medicare fee-for-service insurance, were aged ≥65 years, and who were discharged alive, not against medical advice, and not transferred to another acute care hospital. We excluded patients admitted for medical treatment of cancer or primary psychiatric disease. In addition, we excluded patients without one year of prior enrollment in Medicare fee-for-service or without one month of post-discharge enrollment. Patients discharged from cancer hospitals exempt from fee-for-service were excluded from the measure. Multiple index admissions by the same patient could be included if each met eligibility criteria.
Outcome measure
Our primary outcome was based on the publicly reported, hospital-wide readmission measure. This measure assigns inpatients to one of five cohorts: medicine, surgery/gynecology, cardiorespiratory, cardiovascular, and neurology. Each cohort is modeled separately using hierarchical logistic regression to construct five standardized predicted-to-expected risk ratios, which are then pooled to create a single hospital metric.35
The hierarchical models used by the publicly reported measure use shrinkage estimators which have the known property of weighting the predictions for smaller volume hospitals towards the mean. While that approach is appropriate for public reporting of individual hospitals to avoid misclassifying small hospitals as outliers, this analysis examines small volume hospitals collectively and is specifically interested in determining performance of small volume hospitals. Consequently, to avoid shrinkage, we modified the publicly reported measure approach and calculated observed-to-expected risk ratios for each cohort instead of predicted-to-expected ratios.
The expected number of readmissions is calculated using a standard logistic regression model, accounting for clustering through generalized estimating equations, and adjusting for age, principal diagnosis, and 30 comorbidity indicators based on Part A claims—which include claims for hospital care, skilled nursing facility care, and hospice and home health services—during the year before admission. Comorbidities coded during the index hospitalization are also included if they were not likely to be in-hospital complications of care. Readmissions to any hospital are counted in the outcome. However, planned readmissions are excluded according to an algorithm that takes into account major procedures occurring during readmission and the principal diagnosis of the readmission.36 We calculated the hospital-wide standardized readmission rate by obtaining the weighted mean of the cohort ratios, multiplied by the mean national readmission rate for ease of interpretation. Our secondary outcomes were the five specialty cohort ratios at each hospital, each multiplied by the mean national readmission rate for that cohort.
As another secondary analysis, we constructed predicted-to-expected ratios in accordance with the approach used in public reporting. The predicted and expected numbers of readmissions are calculated using hierarchical logistic regression models and the same risk variables as above; the calculation for the predicted number of readmissions includes a hospital-specific effect. We expected to see smaller differences between the lowest volume hospitals and the highest volume hospitals using this approach, given the known shrinkage towards the mean for small volume hospitals.
Finally, since mortality is often higher is low volume centers, potentially putting fewer patients at risk for readmission, we repeated the main analysis using a combined outcome of readmission or mortality to determine whether competing mortality risk explained any findings.
Independent variables
Our primary independent variable of interest was hospital volume, which we defined as the number of index admissions included in the measure. In this way we prevented a high readmission rate from biasing the volume categorization. For analysis, we excluded hospitals with fewer than 25 qualifying cases and then divided the remaining hospitals by quintiles into five groups based on each hospital’s number of index discharges in 2010. In analyses of specialty cohorts, we categorized hospitals into volume fifths based on their number of discharges in each cohort. Thus a hospital might be in a high volume group for one specialty cohort but a low volume group for a different specialty cohort.
We included eight hospital characteristics as covariates, identified from the 2010 American Hospital Association annual survey, that have been associated with readmission37: safety net status (a public hospital or a private hospital with a Medicaid caseload more than one standard deviation above the state average for private hospitals38), hospital ownership (not for profit, private, or public), teaching status (member of Council of Teaching Hospitals, minor teaching hospital, non-teaching), nurse-to-bed ratio (divided by quartiles), availability of cardiac procedures (capable of cardiac bypass surgery, capable only of cardiac catheterization, not capable of either), urban status (defined according to the National Center for Health Statistics classification39), and geographic region (US Census Bureau division).
Statistical analysis
We calculated mean (standard deviation) and median (interquartile range) by volume fifth for the hospital-wide standardized readmission rate. We used linear regression to assess the volume effect on the overall standardized readmission rate, testing if other volume groups were significantly different from the highest volume group. We first assessed the volume effect without adjusting for any other hospital characteristics. We then repeated the linear regression analysis with the eight aforementioned hospital characteristics included to examine if the volume effect would be different after adjusting for hospital characteristics. To determine if any potential volume effect differed by specialty, we repeated the same analyses for each of the five specialty cohorts.
All analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC). P values less than 0.05 are considered statistically significant, and all reported P values are two sided. The Yale University Investigational Review Board approved this study.
Results
Study cohort
The final sample included 6 916 644 admissions to 4651 hospitals. The number of unplanned readmissions and admissions overall and in each specialty cohort, categorized by volume group, is shown in table 1. Among the specialty cohorts, the largest was medicine, with over 2.8 million admissions from 4407 hospitals. The smallest was the neurology cohort, with 411 375 admissions from 2594 hospitals. The observed patient-level, 30 day readmission rate was 16.0%. Specialty cohort readmission rates ranged from a low of 11.7% in the surgery/gynecology cohort to a high of 20.4% in the cardiorespiratory group.
Table 1.
Hospital volume (hospitals divided by quintiles based on hospital’s number of index discharges in 2010) and associated 30 day readmission rate (observed and standardized), by specialty cohort
| Volume group (No of index discharges) | No of hospitals | No of index discharges | No of readmissions | Mean (SD) readmission rate (%) | |
|---|---|---|---|---|---|
| Observed | Standardized | ||||
| Hospital-wide | |||||
| Excluded (<25 per hospital) | 158 | 1 823 | 205 | N/A | N/A |
| A (25 to 173) | 932 | 91 298 | 12 517 | 13.4 (5.5) | 14.7 (5.3) |
| B (173 to 423) | 930 | 266 303 | 39 465 | 14.8 (4.5) | 15.6 (3.5) |
| C (423 to 1108) | 929 | 649 751 | 102 357 | 15.7 (4.0) | 15.8 (2.8) |
| D (1108 to 2595) | 930 | 1 643 144 | 267 695 | 16.3 (3.1) | 16.0 (2.1) |
| E (2595 to 25 002) | 930 | 4 266 148 | 683 139 | 16.0 (2.4) | 15.9 (1.7) |
| Total included | 4 651 | 6 916 644 | 1 105 173 | 15.3 (4.2) | 15.6 (3.4) |
| Medicine cohort | |||||
| Excluded (<25 per hospital) | 347 | 3 673 | 456 | N/A | N/A |
| A (25 to 99) | 886 | 53 715 | 7 819 | 14.3 (5.9) | 16.6 (6.3) |
| B (99 to 218) | 883 | 134 386 | 20 708 | 15.3 (4.0) | 17.1 (4.2) |
| C (218 to 534) | 876 | 306 460 | 51 315 | 16.6 (3.6) | 17.3 (3.2) |
| D (534 to 1124) | 881 | 703 463 | 122 578 | 17.4 (2.9) | 17.3 (2.4) |
| E (1124 to 11 380) | 881 | 1 683 550 | 300 256 | 17.7 (2.4) | 17.4 (1.9) |
| Total included | 4 407 | 2 881 574 | 502 676 | 16.3 (4.1) | 17.2 (3.9) |
| Surgery/gynecology cohort | |||||
| Excluded (<25 per hospital) | 840 | 7 499 | 836 | N/A | N/A |
| A (25 to 79) | 666 | 32 088 | 3 408 | 10.5 (6.0) | 11.3 (5.7) |
| B (79 to 186) | 648 | 83 694 | 9 380 | 11.2 (4.9) | 11.5 (3.7) |
| C (186 to 389) | 660 | 184 435 | 21 043 | 11.4 (3.9) | 11.5 (2.7) |
| D (389 to 792) | 654 | 370 011 | 43 590 | 11.8 (3.2) | 11.6 (2.1) |
| E (792 to 6389) | 655 | 933 971 | 110 885 | 11.8 (2.5) | 11.5 (1.7) |
| Total included | 3 283 | 1 604 199 | 188 306 | 11.3 (4.3) | 11.5 (3.5) |
| Cardiorespiratory cohort | |||||
| Excluded (<25 per hospital) | 466 | 5 956 | 841 | N/A | N/A |
| A (25 to 68) | 844 | 37 723 | 6 064 | 15.9 (6.8) | 18.5 (7.6) |
| B (68 to 133) | 827 | 80 934 | 14 579 | 18.0 (5.3) | 19.7 (5.3) |
| C (133 to 252) | 832 | 155 497 | 30 919 | 19.8 (4.5) | 20.5 (4.1) |
| D (252 to 458) | 836 | 290 356 | 60 357 | 20.7 (3.9) | 20.7 (3.4) |
| E (458 to 3068) | 831 | 608 747 | 127 763 | 21.0 (3.1) | 20.5 (2.5) |
| Total included | 4 170 | 1 173 257 | 239 682 | 19.1 (5.2) | 20.0 (5.0) |
| Cardiovascular cohort | |||||
| Excluded (<25 per hospital) | 1 579 | 15 990 | 2 310 | N/A | N/A |
| A (25 to 50) | 593 | 20 962 | 3 117 | 14.9 (6.8) | 14.6 (6.4) |
| B (50 to 120) | 588 | 47 098 | 7 048 | 15.0 (5.0) | 14.5 (4.5) |
| C (120 to 237) | 587 | 102 434 | 14 835 | 14.6 (3.7) | 14.1 (3.1) |
| D (237 to 441) | 589 | 193 358 | 26 970 | 14.0 (2.9) | 13.7 (2.4) |
| E (441 to 3361) | 588 | 432 445 | 59 255 | 13.8 (2.3) | 13.7 (1.9) |
| Total included | 2 945 | 796 297 | 111 225 | 14.5 (4.5) | 14.1 (4.0) |
| Neurology cohort | |||||
| Excluded (<25 per hospital) | 1 917 | 18 647 | 2 239 | N/A | N/A |
| A (25 to 44) | 532 | 17 724 | 2 241 | 12.6 (6.7) | 13.2 (6.9) |
| B (44 to 84) | 508 | 31 903 | 4 251 | 13.3 (4.8) | 13.6 (4.8) |
| C (84 to 141) | 520 | 57 627 | 7 734 | 13.5 (4.0) | 13.6 (3.8) |
| D (141 to 249) | 518 | 98 675 | 13 431 | 13.6 (3.2) | 13.6 (3.0) |
| E (249 to 1429) | 516 | 205 446 | 29 150 | 14.1 (2.6) | 14.0 (2.3) |
| Total included | 2 594 | 411 375 | 56 807 | 13.4 (4.5) | 13.6 (4.5) |
Observed results
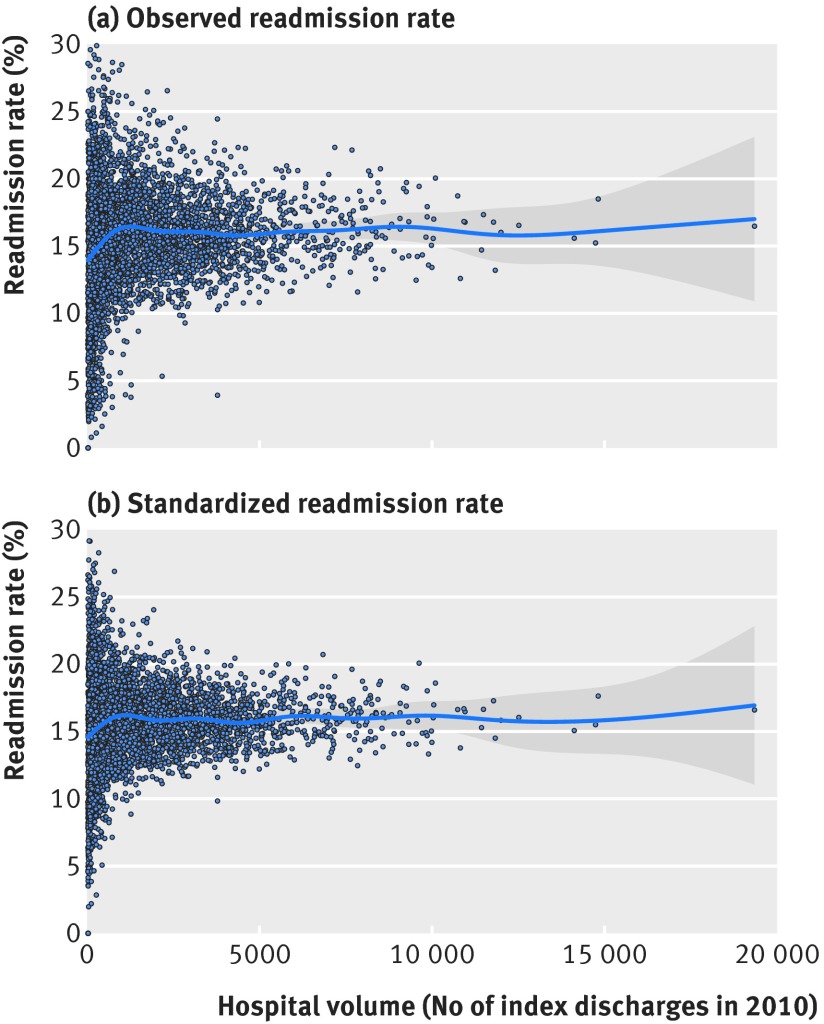
A scatter plot of the hospital-level, observed, unplanned, 30 day readmission rate is shown in figure 1, panel (a). Means and standard deviations are shown in table 1.The hospital-level observed readmission rate increased as hospital volume increased, ranging from a low of 13.4% in the smallest volume group to a high of 16.3% in the second largest volume group. Specialty cohorts exhibited a similar positive association of volume with observed readmission rates, with the exception of the cardiovascular cohort, in which observed readmission rates declined as hospital volume increased.
Fig 1 Scatter plots of hospital-wide unplanned, 30 day readmission rate by hospital volume: (a) observed rate, (b) standardized rate
Standardized results
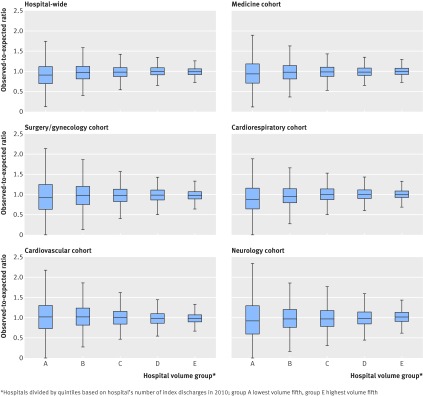
A scatter plot of the hospital-wide standardized, unplanned, 30 day readmission rate is shown in figure 1, panel (b). The mean and standard deviation of hospital-wide and specialty cohort standardized, unplanned, 30 day readmission rates are shown in box and whisker form in figure 2 and in table 1. The hospital-wide mean standardized readmission rate was 14.7% (standard deviation 5.3) in the smallest volume group and 15.9% (1.7) in the highest volume group, an absolute difference of 1.2 percentage points (95% confidence interval 0.9 to 1.5) (table 2). Among the specialty cohorts, we observed the same pattern of significantly lower standardized readmission rate in the lowest versus the highest volume hospitals in the medicine, cardiorespiratory, and neurology cohorts. The cardiorespiratory cohort showed the largest association, with hospitals in the lowest volume group having standardized readmission rates that were on average 2.0 percentage points lower than those in the highest volume group (95% CI 1.5 to 2.5). In the cardiovascular cohort, however, the lowest volume hospitals had significantly higher standardized readmission rates (0.9 percentage points (95% CI 0.4 to 1.3)). There was no significant association in the surgery/gynecology cohort. Using predicted-to-expected readmission ratios instead of observed-to-expected ratios yielded similar although much smaller differences (appendix A).
Fig 2 Distribution of standardized readmission rate, by hospital volume group and specialty cohort
Table 2.
Bivariate and multivariate associations of hospital volume* with standardized readmission rate: absolute differences in readmission rates compared with highest volume fifth of hospitals by specialty cohort
| Volume group* | Unadjusted difference in readmission rates | Adjusted difference in readmission rates† | |||
|---|---|---|---|---|---|
| Difference (95% CI) | P value | Difference (95% CI)* | P value | ||
| Hospital-wide | |||||
| A | −1.16 (−1.46 to −0.85) | <0.0001 | −1.56 (−2.03 to −1.08) | <0.0001 | |
| B | −0.29 (−0.59 to 0.02) | 0.07 | −0.72 (−1.16 to −0.28) | 0.001 | |
| C | −0.08 (−0.39 to 0.23) | 0.61 | −0.53 (−0.93 to −0.13) | 0.01 | |
| D | 0.14 (−0.17 to 0.44) | 0.38 | 0.06 (−0.27 to 0.39) | 0.73 | |
| E | Reference | — | Reference | — | |
| Medicine cohort | |||||
| A | −0.76 (−1.13 to −0.39) | <0.0001 | −1.41 (−1.96 to −0.85) | <0.0001 | |
| B | −0.28 (−0.65 to 0.08) | 0.13 | −0.99 (−1.51 to −0.47) | 0.0002 | |
| C | −0.06 (−0.43 to 0.30) | 0.73 | −0.67 (−1.13 to −0.21) | 0.004 | |
| D | −0.06 (−0.43 to 0.30) | 0.74 | −0.25 (−0.64 to 0.14) | 0.22 | |
| E | Reference | — | Reference | — | |
| Surgery/gynecology cohort | |||||
| A | −0.20 (−0.58 to 0.17) | 0.29 | 0.63 (0.10 to 1.17) | 0.02 | |
| B | −0.04 (−0.41 to 0.34) | 0.86 | 0.66 (0.16 to 1.16) | 0.01 | |
| C | −0.02 (−0.39 to 0.36) | 0.93 | 0.49 (0.04 to 0.94) | 0.03 | |
| D | 0.03 (−0.35 to 0.41) | 0.88 | 0.36 (−0.04 to 0.76) | 0.08 | |
| E | Reference | — | Reference | — | |
| Cardiorespiratory cohort | |||||
| A | −2.01 (−2.48 to −1.54) | <0.0001 | −3.01 (−3.68 to −2.34) | <0.0001 | |
| B | −0.78 (−1.25 to −0.31) | 0.001 | −1.81 (−2.42 to −1.20) | <0.0001 | |
| C | 0.01 (−0.46 to 0.49) | 0.96 | −0.84 (−1.39 to −0.29) | 0.003 | |
| D | 0.12 (−0.35 to 0.60) | 0.61 | −0.21 (−0.69 to 0.28) | 0.40 | |
| E | Reference | — | Reference | — | |
| Cardiovascular cohort | |||||
| A | 0.86 (0.40 to 1.32) | 0.0002 | −0.57 (−1.21 to 0.07) | 0.08 | |
| B | 0.73 (0.27 to 1.18) | 0.002 | −0.13 (−0.70 to 0.44) | 0.66 | |
| C | 0.36 (−0.10 to 0.81) | 0.13 | 0.03 (−0.49 to 0.54) | 0.92 | |
| D | 0.01 (−0.45 to 0.47) | 0.97 | −0.05 (−0.51 to 0.41) | 0.82 | |
| E | Reference | — | Reference | — | |
| Neurology cohort | |||||
| A | −0.73 (−1.27 to −0.19) | 0.01 | −0.87 (−1.59 to −0.16) | 0.02 | |
| B | −0.33 (−0.88 to 0.21) | 0.23 | −0.35 (−0.99 to 0.29) | 0.29 | |
| C | −0.41 (−0.96 to 0.13) | 0.14 | −0.23 (−0.82 to 0.35) | 0.44 | |
| D | −0.34 (−0.88 to 0.21) | 0.22 | −0.15 (−0.70 to 0.39) | 0.58 | |
| E | Reference | — | Reference | — | |
*Hospitals divided by quintiles based on hospital’s number of index discharges in 2010; group A is lowest volume fifth, group E is highest volume fifth.
†Adjusted for hospital safety net status, ownership, teaching status, cardiac procedure capability, urban/rural status, geographic region, and nurse-to-bed ratio (see text for details).
Adjustment for hospital characteristics
After adjustment for hospital safety net status, ownership, teaching status, cardiac procedure capability, nurse-to-bed ratio, urban/rural status, and geographic region, the differences between high and low volume hospitals were larger overall and in the medicine, cardiorespiratory, and neurology cohorts (table 2). Hospitals in the lowest volume group had a hospital-wide mean, adjusted, standardized readmission rate 1.6 percentage points lower than hospitals in the highest volume group (95% CI 1.1 to 2.0). The largest difference was still in the cardiorespiratory cohort, in which the lowest volume fifth of hospitals had an adjusted standardized readmission rate 3.0 points lower than the highest volume group (95% CI 2.3 to 3.7). After adjustment for hospital characteristics, there was no longer an association between hospital volume and outcome in the cardiovascular cohort, but the smallest volume hospitals in the surgery/gynecology cohort had a significantly higher standardized readmission rate than the largest hospitals (difference 0.6 percentage points (95% CI 0.1 to 1.2)). Full model coefficients for all cohorts are shown in appendix B.
Combined readmission and mortality outcome
The lowest volume and highest volume groups of hospitals were not significantly different in hospital-wide readmission or mortality (20.4% v 20.2%, P=0.19), whereas the middle volume fifth of hospitals had significantly higher standardized mortality or readmission rates (range 20.6% to 20.8%) (see table 3). Among the specialty cohorts, hospitals in the lowest volume group had significantly higher combined outcome rates in the medicine and cardiovascular cohorts, but significantly lower combined outcome rates in the cardiorespiratory cohort. There was no significant difference between highest and lowest volume hospitals in the surgery/gynecology or neurology cohorts.
Table 3.
Mean and median standardized mortality or readmission rate, hospital-wide and by specialty cohort, by hospital volume*
| Volume group* | No of hospitals | Standardized mortality or readmission rate (%) | Absolute difference in readmission rates† | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Parameter estimate (95% CI) | P value | |||
| Hospital-wide | ||||||
| A | 932 | 20.4 (6.1) | 20.5 (16.7 to 24.1) | 0.22 (−0.11 to 0.56) | 0.19 | |
| B | 930 | 20.8 (3.8) | 20.7 (18.4 to 23.4) | 0.61 (0.27 to 0.95) | 0.0004 | |
| C | 929 | 20.6 (2.9) | 20.5 (18.7 to 22.3) | 0.36 (0.02 to 0.70) | 0.037 | |
| D | 930 | 20.6 (2.2) | 20.5 (19.2 to 22.0) | 0.34 (0.00 to 0.68) | 0.047 | |
| E | 930 | 20.2 (1.7) | 20.2 (19.1 to 21.3) | Reference | — | |
| Overall | 4651 | 20.5 (3.7) | 20.4 (18.7 to 22.4) | |||
| Medicine cohort | ||||||
| A | 886 | 23.6 (7.2) | 23.5 (18.8 to 27.9) | 0.88 (0.47 to 1.28) | <0.0001 | |
| B | 883 | 23.6 (4.6) | 23.4 (20.5 to 26.6) | 0.83 (0.42 to 1.23) | <0.0001 | |
| C | 876 | 23.2 (3.4) | 23.0 (20.8 to 25.3) | 0.40 (−0.01 to 0.80) | 0.057 | |
| D | 881 | 23.0 (2.5) | 22.9 (21.3 to 24.6) | 0.20 (−0.21 to 0.61) | 0.33 | |
| E | 881 | 22.8 (1.9) | 22.7 (21.5 to 24.0) | Reference | — | |
| Overall | 4407 | 23.2 (4.4) | 23.0 (20.9 to 25.3) | |||
| Surgery/gynecology cohort | ||||||
| A | 666 | 13.5 (6.1) | 13.1 (9.1 to 16.7) | 0.11 (−0.29 to 0.51) | 0.59 | |
| B | 648 | 13.6 (3.9) | 13.5 (10.8 to 16.2) | 0.29 (−0.11 to 0.70) | 0.15 | |
| C | 660 | 13.5 (2.8) | 13.4 (11.7 to 15.4) | 0.18 (−0.22 to 0.58) | 0.39 | |
| D | 654 | 13.6 (2.3) | 13.6 (12.1 to 15.1) | 0.21 (−0.19 to 0.61) | 0.31 | |
| E | 655 | 13.3 (1.7) | 13.3 (12.3 to 14.4) | Reference | — | |
| Overall | 3283 | 13.5 (3.7) | 13.4 (11.5 to 15.4) | |||
| Cardiorespiratory cohort | ||||||
| A | 844 | 25.6 (8.4) | 25.0 (19.8 to 30.9) | −0.54 (−1.04 to −0.03) | 0.037 | |
| B | 827 | 26.3 (5.5) | 25.9 (22.6 to 29.8) | 0.19 (−0.31 to 0.70) | 0.45 | |
| C | 832 | 26.6 (4.2) | 26.4 (23.8 to 29.1) | 0.46 (−0.05 to 0.97) | 0.076 | |
| D | 836 | 26.4 (3.5) | 26.1 (24.0 to 28.8) | 0.23 (−0.28 to 0.74) | 0.38 | |
| E | 831 | 26.1 (2.6) | 26.0 (24.3 to 27.8) | Reference | — | |
| Overall | 4170 | 26.2 (5.3) | 26.0 (23.4 to 28.9) | |||
| Cardiovascular cohort | ||||||
| A | 593 | 18.6 (6.9) | 18.3 (14.0 to 22.7) | 2.55 (2.07 to 3.02) | <0.0001 | |
| B | 588 | 17.5 (4.6) | 17.6 (14.4 to 20.6) | 1.46 (0.98 to 1.94) | <0.0001 | |
| C | 587 | 16.9 (3.1) | 16.7 (14.6 to 19.0) | 0.82 (0.34 to 1.30) | 0.0008 | |
| D | 589 | 16.2 (2.5) | 16.1 (14.6 to 17.8) | 0.12 (−0.36 to 0.60) | 0.62 | |
| E | 588 | 16.1 (2.0) | 16.0 (14.7 to 17.4) | Reference | — | |
| Overall | 2945 | 17.1 (4.3) | 16.6 (14.6 to 19.1) | |||
| Neurology cohort | ||||||
| A | 532 | 21.4 (7.5) | 21.0 (16.2 to 25.9) | 0.27 (−0.33 to 0.87) | 0.38 | |
| B | 508 | 21.3 (5.6) | 21.3 (17.8 to 24.9) | 0.16 (−0.45 to 0.77) | 0.61 | |
| C | 520 | 20.9 (4.0) | 20.6 (18.3 to 23.8) | −0.25 (−0.86 to 0.35) | 0.42 | |
| D | 518 | 21.0 (3.5) | 20.7 (18.3 to 23.4) | −0.17 (−0.78 to 0.43) | 0.58 | |
| E | 516 | 21.1 (2.7) | 21.0 (19.2 to 22.8) | Reference | — | |
| Overall | 2594 | 21.1 (5.0) | 20.9 (18.2 to 23.9) | |||
*Hospitals divided by quintiles based on hospital’s number of index discharges in 2010; group A is lowest volume fifth, group E is highest volume fifth.
†Difference in readmission rates (in percentage points) compared with highest volume fifth of hospitals.
Discussion
Principal findings
We examined the association of hospital volume with standardized readmission rate and found that, overall, hospitals with the lowest volume had lower standardized readmission rates than those with the highest volume. Within individual specialty cohorts, the only exception was the cardiovascular cohort, in which hospitals with the lowest volume had the highest standardized readmission rates. After accounting for hospital characteristics, hospitals with the lowest volume still had the lowest readmission rates and the inverse association in the cardiovascular cohort no longer existed, though a small inverse association developed in the surgery/gynecology cohort.
Our findings suggest that readmission does not perform in the same way as mortality or complications in its association with hospital volume. Readmissions are often precipitated by acute exacerbations of chronic disease, persistence of the initial problem, or increased frailty.28 It is possible that the risk of these events may be reduced by more time and effort spent in educating patients, conducting high quality medication reconciliation, following up after discharge, and other activities that do not necessarily improve with greater patient volume and may even worsen if higher patient volume is associated with more turnover, more complicated team structure, or less time spent with each patient.
The competing risk of mortality also seems to play some role. Though the smallest hospitals still performed as well overall as the largest hospitals in a combined outcome of mortality or readmission, the smallest hospitals did have the highest combined outcome rate in two specialty cohorts. Of note, the difference was not explained by hospital characteristics—such as teaching status, urban location, public ownership, or safety net status—that might be associated with hospital volume and with readmission rates. In fact, adjustment increased the size of the effect.
The findings that only the procedure-heavy cohorts demonstrated the typical association of higher volume with better outcomes may be a consequence of the causes of readmissions in these cohorts. Readmissions after major procedures are often related to procedural complications,40 and higher volume centers produce fewer complications. Higher volume centers may also be more experienced at encouraging appropriate post-discharge care such as rehabilitation or home care services. It is notable that adjustment for hospital characteristics such as presence of advanced cardiac capability eliminated the association in the cardiovascular cohort, suggesting there may be a causal relationship between structural hospital characteristics and readmission risk in the cardiovascular group.
Comparison with other studies
Our findings are similar to those from some studies of surgery volume and readmissions, which found no association of surgical volume and readmissions.22 23 24 25 Our results are also consistent with a recent study by Tsai et al of six surgical procedures, in which high volume centers had lower readmission rates after adjustment for hospital characteristics.21 Like Tsai et al, we found that high volume centers in our surgery/gynecology cohort had significantly lower readmission rates than lower volume centers after adjustment for hospital characteristics—though we did not find this association without adjusting for hospital characteristics. Our study differs, however, in that it includes non-surgical patients. Indeed, we noted quite different associations of hospital volume and outcomes in other patient populations.
Strengths and limitations of study
A strength of this study is that we included only unplanned readmissions; this is particularly important given that larger centers are likely to conduct more planned readmissions for surgical procedures or chemotherapy. Moreover, this is the first study to examine all patients, rather than single diseases or specialties. None the less, our study has several limitations. We looked only at patients aged 65 years and over; results may differ in younger populations. We used administrative data for risk adjustment, which might not fully capture acuity of illness at high volume centers. Moreover, although we accounted for safety net status, there may have been unmeasured non-clinical risk factors that are associated both with readmission risk and with hospital volume. It is notable, however, that the relationship between high volume and better outcome for mortality and complications has been repeatedly demonstrated in studies that use similar claims-based risk adjustment as in this study, suggesting our results are unlikely to be driven by unmeasured confounding. We include all admissions per patient, potentially creating a bias against hospitals with disproportionate numbers of frequently admitted patients. Finally, we did not analyze the data on the level of individual procedures or diagnoses; results may differ for individual conditions.
Conclusions
Overall, we found that high volume centers have higher standardized unplanned readmission rates, except in procedure-heavy cohorts of patients. These effects were not explained by hospital characteristics and were only partially attenuated by considering both mortality and readmission as outcomes. As hospitals work to reduce readmissions, it may be helpful to explore reasons smaller hospitals have had more success at avoiding readmissions for non-procedural specialties than larger hospitals.
An earlier version of this work was presented at the Academy Health 2012 Annual Research Meeting in Orlando, FL, on 25 June 2012.
Contributors: Study concept and design: all authors. Acquisition of data: HMK. Analysis and interpretation of data: all authors. Drafting of the manuscript: LIH. Critical revision of the manuscript for important intellectual content: all authors. Approval of final manuscript for submission: all authors. Statistical analysis: ZL, JH. Obtained funding: HMK. Study supervision: LIH, EED.
Financial support: This work was performed under contract HHSM-500-2013-13018I, Task Order HHSM-500-T0001, funded by the Center for Medicare & Medicaid Services, an agency of the US Department of Health and Human Services. This work was also supported by the Agency for Healthcare Research and Quality (R01 HS022882). LIH and JSR are supported by the National Institute on Aging (K08 AG038336 and K08 AG032886, respectively) and by the American Federation for Aging Research through the Paul B Beeson Career Development Award Program. HMK is supported by grant U01 HL105270-03 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. No funding source had any role in the study design; in the collection, analysis, and interpretation of data; or in the writing of the report. The Center for Medicare & Medicaid Services reviewed and approved the use of its data for this work and approved submission of the manuscript.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that all authors have support from the Centers for Medicare & Medicaid Services for the submitted work. In addition, JSR is a member of a scientific advisory board for FAIR Health, and HMK chairs a cardiac scientific advisory board for UnitedHealth and is the recipient of research grants from Medtronic and Johnson & Johnson through Yale University.
Transparency: The lead author (LIH) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. ZL had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Cite this as: BMJ 2015;350:h447
Web Extra. Extra material supplied by the author
Appendix A: Bivariate and multivariate associations of hospital volume with standardized readmission rate
Appendix B: Parameter estimates
References
- 1.Holt PJ, Poloniecki JD, Gerrard D, Loftus IM, Thompson MM. Meta-analysis and systematic review of the relationship between volume and outcome in abdominal aortic aneurysm surgery. Br J Surg 2007;94:395-403. [DOI] [PubMed] [Google Scholar]
- 2.Post PN, Kuijpers M, Ebels T, Zijlstra F. The relation between volume and outcome of coronary interventions: a systematic review and meta-analysis. Eur Heart J 2010;31:1985-92. [DOI] [PubMed] [Google Scholar]
- 3.Magid DJ, Calonge BN, Rumsfeld JS, Canto JG, Frederick PD, Every NR, et al. Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy. JAMA 2000;284:3131-8. [DOI] [PubMed] [Google Scholar]
- 4.Zevin B, Aggarwal R, Grantcharov TP. Volume-outcome association in bariatric surgery: a systematic review. Ann Surg 2012;256:60-71. [DOI] [PubMed] [Google Scholar]
- 5.Wouters MW, Gooiker GA, van Sandick JW, Tollenaar RA. The volume-outcome relation in the surgical treatment of esophageal cancer: a systematic review and meta-analysis. Cancer 2012;118:1754-63. [DOI] [PubMed] [Google Scholar]
- 6.Gooiker GA, van Gijn W, Wouters MW, Post PN, van de Velde CJ, Tollenaar RA. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg 2011;98:485-94. [DOI] [PubMed] [Google Scholar]
- 7.Gooiker GA, van Gijn W, Post PN, van de Velde CJ, Tollenaar RA, Wouters MW. A systematic review and meta-analysis of the volume-outcome relationship in the surgical treatment of breast cancer. Are breast cancer patients better of with a high volume provider? Eur J Surg Oncol 2010;36(suppl 1):S27-35. [DOI] [PubMed] [Google Scholar]
- 8.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128-37. [DOI] [PubMed] [Google Scholar]
- 9.Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg 2005;242:512-7; discussion 517-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Urbach DR, Baxter NN. Does it matter what a hospital is “high volume” for? Specificity of hospital volume-outcome associations for surgical procedures: analysis of administrative data. BMJ 2004;328:737-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reames BN, Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and operative mortality in the modern era. Ann Surg 2014;260:244-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA 2000;283:1159-66. [DOI] [PubMed] [Google Scholar]
- 13.Phibbs CS, Bronstein JM, Buxton E, Phibbs RH. The effects of patient volume and level of care at the hospital of birth on neonatal mortality. JAMA 1996;276:1054-9. [PubMed] [Google Scholar]
- 14.Ross JS, Normand SL, Wang Y, Ko DT, Chen J, Drye EE, et al. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med 2010;362:1110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The Leapfrog Group. Evidence-based hospital referral factsheet. 2008. www.leapfroggroup.org/media/file/Leapfrog-Evidence-Based_Hospital_Referral_Fact_Sheet.pdf.
- 16.Agency for Healthcare Research and Quality. Inpatient quality indicators technical specifications—version 4.5. 2013. www.qualityindicators.ahrq.gov/Modules/IQI_TechSpec.aspx.
- 17.Agency for Healthcare Research and Quality. Pediatric quality indicators technical specifications—version 4.5. 2013. www.qualityindicators.ahrq.gov/Modules/PDI_TechSpec.aspx.
- 18.Medicare.gov. Hospital Compare. 2013. www.medicare.gov/hospitalcompare/search.html?AspxAutoDetectCookieSupport=1.
- 19.Nguyen NT, Paya M, Stevens CM, Mavandadi S, Zainabadi K, Wilson SE. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg 2004;240:586-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg 2007;204:383-91. [DOI] [PubMed] [Google Scholar]
- 21.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med 2013;369:1134-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goodney PP, Stukel TA, Lucas FL, Finlayson EV, Birkmeyer JD. Hospital volume, length of stay, and readmission rates in high-risk surgery. Ann Surg 2003;238:161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mayer EK, Bottle A, Aylin P, Darzi AW, Athanasiou T, Vale JA. The volume-outcome relationship for radical cystectomy in England: an analysis of outcomes other than mortality. BJU Int 2011;108:E258-65. [DOI] [PubMed] [Google Scholar]
- 24.Burns EM, Bottle A, Aylin P, Clark SK, Tekkis PP, Darzi A, et al. Volume analysis of outcome following restorative proctocolectomy. Br J Surg 2011;98:408-17. [DOI] [PubMed] [Google Scholar]
- 25.Borenstein SH, To T, Wajja A, Langer JC. Effect of subspecialty training and volume on outcome after pediatric inguinal hernia repair. J Pediatr Surg 2005;40:75-80. [DOI] [PubMed] [Google Scholar]
- 26.Joynt KE, Orav EJ, Jha AK. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Ann Intern Med 2011;154:94-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med 2009;150:178-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krumholz HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med 2013;368:100-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 2006;166:1822-8. [DOI] [PubMed] [Google Scholar]
- 30.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA 2010;303:1716-22. [DOI] [PubMed] [Google Scholar]
- 31.Roy CL, Kachalia A, Woolf S, Burdick E, Karson A, Gandhi TK. Hospital readmissions: physician awareness and communication practices. J Gen Intern Med 2009;24:374-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med 2009;361:1368-75. [DOI] [PubMed] [Google Scholar]
- 33.Horwitz LI, Partovian C, Lin Z, Grady JN, Herrin J, Conover M, et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Int Med 2014;161(10 suppl):S66-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Horwitz L, Partovian C, Lin Z, et al. Hospital-wide all-cause unplanned readmission measure: final technical report. 2012. https://www.qualitynet.org/dcs/ContentServer?cid=1219069855273&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page.
- 35.Normand SLT, Shahian DM. Statistical and clinical aspects of hospital outcomes profilling. Stat Sci 2007;22:206-26. [Google Scholar]
- 36.Horwitz LI, Partovian C, Lin Z, Herrin J, Grady JN, Keenan M, et al. Centers for Medicare & Medicaid Services planned readmission algorithm—version 2.1. 2013. http://hscrc.maryland.gov/documents/HSCRC_Initiatives/readmissions/Version-2-1-Readmission-Planned-CMS-Readmission-Algorithm-Report-03-14-2013.pdf.
- 37.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes 2011;4:53-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ross JS, Cha SS, Epstein AJ, Wang Y, Bradley EH, Herrin J, et al. Quality of care for acute myocardial infarction at urban safety-net hospitals. Health Aff (Millwood) 2007;26:238-48. [DOI] [PubMed] [Google Scholar]
- 39.National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties. 2006. www.cdc.gov/nchs/data_access/urban_rural.htm.
- 40.Fischer JP, Wes A, Nelson JA, Serletti JM, Kovach SJ. Factors associated with readmission following plastic surgery—a review of 10,669 procedures from 2011 American College of Surgeons Nation Surgery Quality Improvement Project (ACS-NSQIP) dataset. Plast Reconstr Surg 2013;132:666-74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix A: Bivariate and multivariate associations of hospital volume with standardized readmission rate
Appendix B: Parameter estimates