Abstract
Background
Severe femoral head deformities in the frontal plane such as hips with Legg-Calvé-Perthes disease (LCPD) are not contained by the acetabulum and result in hinged abduction and impingement. These rare deformities cannot be addressed by resection, which would endanger head vascularity. Femoral head reduction osteotomy allows for reshaping of the femoral head with the goal of improving head sphericity, containment, and hip function.
Questions/purposes
Among hips with severe asphericity of the femoral head, does femoral head reduction osteotomy result in (1) improved head sphericity and containment; (2) pain relief and improved hip function; and (3) subsequent reoperations or complications?
Methods
Over a 10-year period, we performed femoral head reduction osteotomies in 11 patients (11 hips) with severe head asphericities resulting from LCPD (10 hips) or disturbance of epiphyseal perfusion after conservative treatment of developmental dysplasia (one hip). Five of 11 hips had concomitant acetabular containment surgery including two triple osteotomies, two periacetabular osteotomies (PAOs), and one Colonna procedure. Patients were reviewed at a mean of 5 years (range, 1–10 years), and none was lost to followup. Mean patient age at the time of head reduction osteotomy was 13 years (range, 7–23 years). We obtained the sphericity index (defined as the ratio of the minor to the major axis of the ellipse drawn to best fit the femoral head articular surface on conventional anteroposterior pelvic radiographs) to assess head sphericity. Containment was assessed evaluating the proportion of patients with an intact Shenton’s line, the extrusion index, and the lateral center-edge (LCE) angle. Merle d’Aubigné-Postel score and range of motion (flexion, internal/external rotation in 90° of flexion) were assessed to measure pain and function. Complications and reoperations were identified by chart review.
Results
At latest followup, femoral head sphericity (72%; range, 64%–81% preoperatively versus 85%; range, 73%–96% postoperatively; p = 0.004), extrusion index (47%; range, 25%–60% versus 20%; range, 3%–58%; p = 0.006), and LCE angle (1°; range, −10° to 16° versus 26°; range, 4°–40°; p = 0.0064) were improved compared with preoperatively. With the limited number of hips available, the proportion of an intact Shenton’s line (64% versus 100%; p = 0.087) and the overall Merle d’Aubigné-Postel score (14.5; range, 12–16 versus 15.7; range, 12–18; p = 0.072) remained unchanged at latest followup. The Merle d’Aubigné-Postel pain subscore improved (3.5; range, 1–5 versus 5.0; range, 3–6; p = 0.026). Range of motion was not observed to have improved with the numbers available (p ranging from 0.513 to 0.778). In addition to hardware removal in two hips, subsequent surgery was performed in five of 11 hips to improve containment after a mean interval of 2.3 years (range, 0.2–7.5 years). Of those, two hips had triple osteotomy, one hip a combined triple and valgus intertrochanteric osteotomy, one hip an intertrochanteric varus osteotomy, and one hip a PAO with a separate valgus intertrochanteric osteotomy. No avascular necrosis of the femoral head occurred.
Conclusions
Femoral head reduction osteotomy can improve femoral head sphericity. Improved head containment in these hips with an often dysplastic acetabulum requires additional acetabular containment surgery, ideally performed concomitantly. This can result in reduced pain and avascular necrosis seems to be rare. With the number of patients available, function did not improve. Therefore, future studies should use more precise instruments to evaluate clinical outcome and include longer followup to confirm joint preservation.
Level of Evidence
Level IV, therapeutic study.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-4048-1) contains supplementary material, which is available to authorized users.
Introduction
Severe femoral head deformities typically occur in the growing skeleton but can also be present in mature hips. Most often, femoral head deformities result from Legg-Calvé-Perthes disease (LCPD) and are diagnosed either in the acute phase in childhood or as the sequelae of LCPD in adults. The femoral head typically has an aspherical shape and is enlarged. In the literature, the terms “coxa plana” [9] or “coxa magna” [18, 23] have been used to describe this entity. The deformed and enlarged femoral head is not contained by the acetabulum, resulting in impingement between the aspherical head and the acetabulum. In abduction, this has been referred to as “hinged abduction” [17, 18]. The altered joint biomechanics in patients with femoral head asphericities ultimately result in impaired function, hip pain, and early joint degeneration.
Osteotomies of the proximal femur at the sub- or intertrochanteric level can address intracapsular femoral head deformities only partially because the correction is not performed at the site of deformity. Surgical hip dislocation [2] gives access to the hip without the risk of avascular necrosis of the femoral head, and so can be used to facilitate femoral head osteotomy. Asphericities of the femoral head in the AP direction can usually be addressed with surgical hip dislocation and resection alone. However, asphericities in the frontal plane cannot be addressed by resection because of the risk of damage to nutrient retinacular vessels of the femoral head. Improved understanding of the vascular supply of the femoral head led to the development of head reduction osteotomy [3, 4], a procedure that allows for downsizing and reshaping the femoral head to improve head sphericity, containment, and potentially improve function and decrease hip pain [11].
We therefore asked whether femoral head reduction osteotomy in hips with severe asphericity of the femoral head results in (1) improved head sphericity and containment; (2) pain relief and improved hip function; and (3) subsequent reoperations or complications including avascular necrosis.
Patients and Methods
We reviewed results of all 11 patients (11 hips) with a severe deformity of the femoral head who underwent femoral head reduction osteotomy between December 2003 and November 2012 (Table 1) at our institution. The current study includes five of 11 hips with a minimum followup of 3 years from the original description of the surgical technique of femoral head reduction osteotomy [11]. Indication for surgery was a painful hip with an aspherical and oversized femoral head in the frontal plane, resulting in hinged abduction with insufficient femoral head containment. The goals of surgery were to decrease symptoms by improving femoral head sphericity so the head would fit into the acetabulum with improved containment. The underlying hip pathologies included LCPD in 10 hips and disturbance of epiphyseal perfusion after conservative treatment of developmental dysplasia of the hip in one hip. Seven of the 11 hips had open femoral head epiphyses at the time of operation. One patient (one hip) had a previous varus intertrochanteric osteotomy (Table 1). Concomitant surgical procedures included relative femoral neck lengthening in all 11 hips, anterior head-neck (offset) trimming in four hips, and acetabular rim trimming in one hip (Table 1). In addition, five of 11 hips had concomitant acetabular containment surgery including two triple osteotomies, two periacetabular osteotomies (PAOs) [5], and one Colonna procedure [1].
Table 1.
Study patient demographics
| Parameter | Value |
|---|---|
| Total hips (patients) | 11 (11) |
| Age at operation (years)* | 13 (7–23) |
| Sex (% men of all hips) | 64 |
| Side (% left of all hips) | 100 |
| Height (cm)* | 139 (119–178) |
| Weight (kg)* | 39 (24–64) |
| Body mass index (kg/m2)* | 20 (15–25) |
| Pathologies (hips) | |
| LCPD | 10 |
| Disturbance of epiphyseal perfusion after conservative treatment of hip dysplasia | 1 |
| Previous surgery (hips) | |
| Varus IO | 1 |
| Concomitant surgery (hips) | |
| Relative neck lengthening | 11 |
| Anterior head-neck (offset) trimming | 4 |
| Triple | 2 |
| PAO | 2 |
| Rim trimming | 1 |
| Colonna procedure | 1 |
* Continuous parameters expressed as mean with range in parentheses; LCPD = Legg-Calvé-Perthes disease; IO = intertrochanteric osteotomy; PAO = periacetabular osteotomy.
Mean patient age at the time of head reduction osteotomy was 13 ± 6 years (range, 7–23 years). We were able to follow all patients for a mean of 5 ± 4 years (range, 1–10 years); no patients were lost to followup. The mean time period between the last followup and the date of submission of this article was 0.8 years (range, 0.3–1.4 years). The study was approved by the local institutional review board.
Clinical evaluation preoperatively and at latest followup was performed by different observers not involved in the surgical care of the patients and included ROM and the Merle d’Aubigné-Postel score [14]. Substantial inter- and intraobserver agreement has been reported for ROM [6, 13] and the Merle d’Aubigné-Postel scoring system [10].
Routine radiographic evaluation consisted of an AP pelvic radiograph and crosstable lateral view of the hip acquired in a standardized manner [24]. One of us not involved in the surgical care of the patients (HA) assessed seven radiographic parameters on plain radiographs to describe femoral head sphericity and containment (Table 2). Preoperative three-dimensional imaging of the hip was not performed consistently and included MRI arthrography in three hips, pelvic CT in two hips, and both modalities in one hip.
Table 2.
Radiographic data of the patient series
| Parameter | Preoperative | Postoperative† | Latest followup‡ | p value, overall | p value, pre- versus postoperative | p value, preoperative versus followup | p value, postoperative versus followup |
|---|---|---|---|---|---|---|---|
| Head sphericity (%) | 72 (64–81) | 86 (74–95)* | 85 (73–96)* | < 0.001 | 0.003 | 0.004 | 0.286 |
| Extrusion index (%) | 47 (25–60) | 21 (12–36)* | 20 (3–58)* | 0.001 | 0.003 | 0.006 | 0.328 |
| Lateral center-edge angle (°) | 1 (–10 to 16) | 20 (–2 to 35)* | 26 (4–40)* | 0.002 | 0.004 | 0.004 | 0.091 |
| Shenton’s line (% intact) | 64 | 82 | 100 | 0.087 | |||
| Acetabular index (°) | 17 (6–37) | 12 (1–39) | 7 (–7 to 19) | 0.078 | |||
| Centrum-collum-diaphyseal angle (°) | 133 (127–144) | 132 (117–145) | 139 (112–169) | 0.081 | |||
| Axial alpha angle (°) | 40 (28–48) | 42 (29–52) | 42 (31–54) | 0.482 |
Continuous parameters are expressed as mean with range in parentheses; *significant difference compared with preoperative; †after femoral head reduction osteotomy in all cases and concomitant acetabular containment surgery in five of 11 hips; ‡after subsequent containment surgery (acetabular and/or intertrochanteric osteotomies) in five of 11 hips.
The operative technique of the femoral head reduction osteotomy has been previously described in detail [4, 11, 25]. Briefly, it includes the surgical dislocation of the hip [2], the development of an extended retinacular soft tissue flap [4], and the osteotomies of the femoral head. The hip was dislocated with use of a flat trochanteric osteotomy (Fig. 1). The greater trochanter was trimmed down to the level of the superior aspect of the femoral neck, referred to as relative femoral neck lengthening (Fig. 2). The extended retinacular soft tissue flap [4] is a periosteal flap of the posterior aspect of the proximal femur. It contains the relevant branches of the medial circumflex femoral artery (MCFA), which ensures the vascularity of the femoral head (Fig. 1). The femoral head osteotomies have to be performed in the sagittal direction to protect the vascularity of the femoral head. The central necrotic segment of the femoral head (Fig. 2) can have a rectangular, trapezoidal, or triangular shape in the frontal plane. The lateral segment of the femoral head was mobilized with an osteotomy at its lateral base (Fig. 1). Blood supply of this pedicled and mobile fragment was ensured by the extended retinacular soft tissue flap and the retinacular branches of the MCFA (Fig. 1). Perfusion of the mobile fragment can be assessed by observing the osteotomized cancellous bone for bleeding. The mobile fragment was then fixed to the stable part of the femoral head with two 2.7- or 3.5-mm cortical screws. The stable part of the femoral head is perfused by the metaphyseal blood flow and the inferior retinacular artery running on top of Weitbrecht’s ligament [8]. The goal of the procedure was to achieve a spherical femoral head with improved containment, which would fit in the acetabulum (Fig. 3); however, care was needed to ensure that the resected central segment was not oversized, resulting in a too small femoral head and possible joint instability.
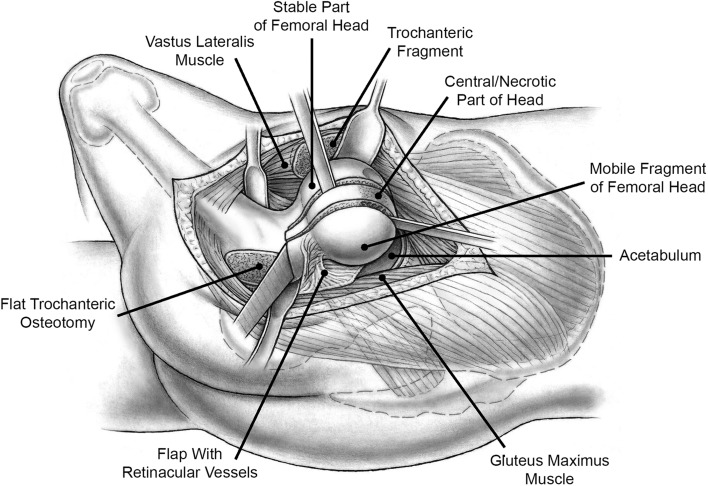
Fig. 1.
To perform the femoral head reduction osteotomy, the patient was placed in the lateral decubitus position. The hip was surgically dislocated through the interval between the gluteus maximums and medius muscle (Gibson interval) with use of a trigastric trochanteric osteotomy. The extended retinacular soft tissue flap ensured the vascularity of the mobile fragment of the femoral head. The flap was developed by subperiosteal dissection of the posterior aspect of the greater trochanter, including the medial circumflex femoral artery and insertion of the short external rotators. The central necrotic part of the femoral head was removed by osteotomies of the femoral head performed in the sagittal direction. Eventually, the mobile part of the femoral head was fixed to the stable part with the goals of improved head sphericity and decreased size of the head.
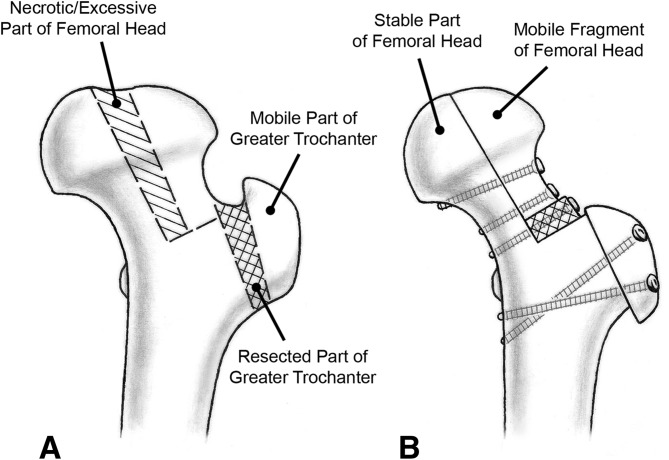
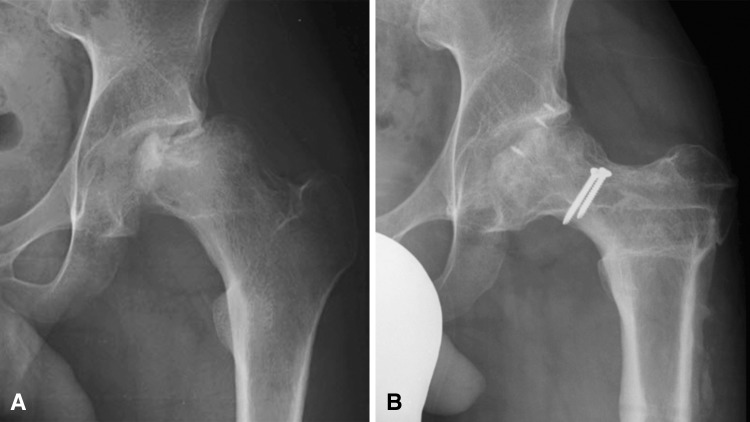
Fig. 2A–B.
(A) Severe femoral head asphericities in the frontal plane can be treated by femoral head reduction osteotomy. First, a trochanteric osteotomy was performed and the stable part of the typically high-riding trochanter was reduced (relative femoral neck lengthening). The necrotic central part of the femoral head was resected by osteotomies performed in the sagittal direction. Perfusion of the mobile fragment is ensured by the extended retinacular soft tissue flap including the medial circumflex femoral artery. The stable part of the femoral head is perfused by the metaphyseal blood flow and the inferior retinacular artery running on top of Weitbrecht’s ligament. (B) The mobile fragment of the femoral head was then fixed to the stable part of the head with the goals of restoring sphericity to the femoral head and having it fit in the acetabulum. Resulting bone deficiency of the femoral neck was filled with bone from the stable part of the greater trochanter. The trochanteric fragment was refixated in an advanced position. Republished with permission of Wichtig Editore SRL, from Tannast M, Macintyre N, Steppacher SD, Hosalkar HS, Ganz R, Siebenrock KA. A systematic approach to analyse the sequelae of LCPD. Hip Int. 2013;23(Suppl 9):S61–S70; permission conveyed through Copyright Clearance Center, Inc.
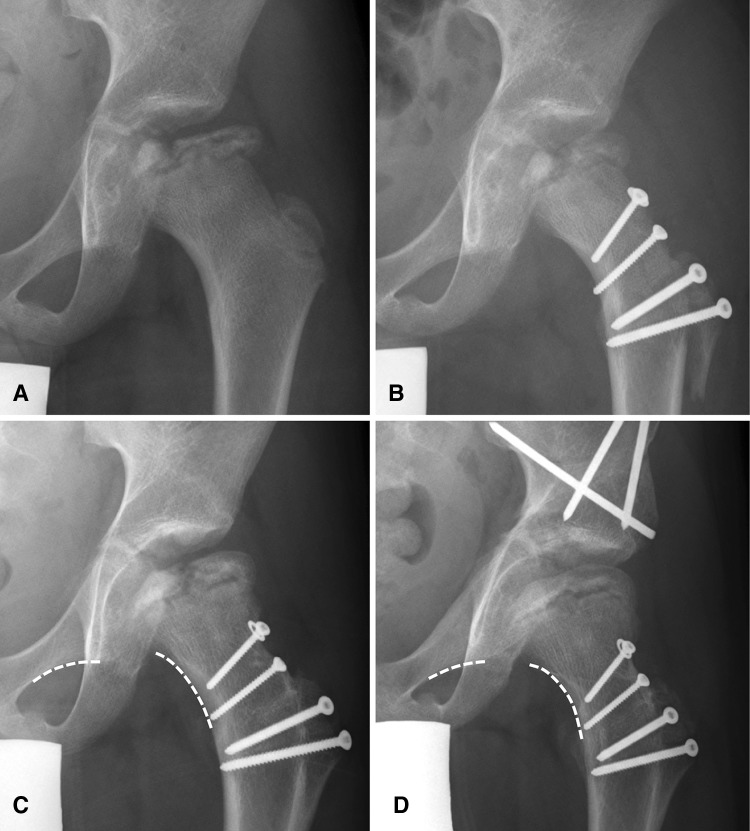
Fig. 3A–D.
A 9-year-old male patient had (A) collapse of the lateral pillar of the femoral head resulting from LCPD. (B) The patient underwent head reduction osteotomy with resection of the central necrotic area to improve head sphericity. In addition, advancement of the greater trochanter with resection of the stable part and improvement of the head-neck offset was performed (relative femoral neck lengthening). (C) Head containment was not sufficient and the femoral head remained subluxated (interrupted Shenton’s line; dashed line). (D) After a triple osteotomy, a well-contained femoral head with a good sphericity was achieved at a followup of 2 years.
Femoral head sphericity was evaluated with the head sphericity index [22], which was defined as the ratio of the minor to the major axis of the ellipse drawn to best fit the femoral head articular surface on the conventional AP pelvic radiograph. A femoral head was considered spherical if the head sphericity exceeded 80%. Femoral head containment was assessed using Shenton’s line, the extrusion index (percentage of femoral head width not covered by the acetabulum), and the lateral center-edge (LCE) angle. These radiographic parameters were compared between pre- and postoperative status. In addition, the final head morphology was classified on AP pelvic radiographs using the Stulberg classification [23]: Class I with a normal hip; Class II with a spherical but enlarged femoral head, a short femoral neck or steep acetabulum; Class III with a nonspherical femoral head; Class IV with a flat femoral head with abnormalities of the acetabulum and neck; and Class V with a flat femoral head and normal acetabulum and neck. To evaluate for improvement of hip pain and function, the Merle d’Aubigné-Postel scoring system [14] and ROM (flexion, internal and external rotation in 90° of flexion) were evaluated preoperatively and at most recent followup. Subsequent surgeries and complications were summarized based on a chart review and complications were graded according to the adapted Dindo-Clavien complication classification system for orthopaedic surgery by one of the authors (HA) not involved in the surgical care of the patients [19, 20]. Because the nature of our study was retrospective, only complications higher than Grade 1 were included. At most recent followup, radiographs were evaluated for healing of femoral head osteotomies or radiographic signs of avascular necrosis including osteopenia, variable density, subchondral lucency (crescent sign), microfractures, and finally the collapse of the femoral head.
Normal distribution was assessed using the Kolmogorov-Smirnov test. Not all parameters showed a normal distribution; therefore, nonparametric statistical tests were used. To compare radiographic parameters between pre- and postoperative status and most recent followup, the Friedman test was used for continuous data and the chi square test for binominal data. If significant differences existed for continuous radiographic parameters, we used the Wilcoxon test for pairwise comparison. The Wilcoxon test was also used for comparison of clinical data between patient preoperative status and latest followup.
Results
The femoral head sphericity improved from 72% (range, 64%–81%) preoperatively to 86% (range, 74%–99%) postoperatively (p = 0.003; Table 2). The mean extrusion index decreased from 47% (range, 25%–60%) preoperatively to 21% (range, 12%–36%) postoperatively (p = 0.003; Table 2). The mean LCE angle increased from 1° (range, –10° to 16°) preoperatively to 20° (range, –2° to 35°) postoperatively (p = 0.004; Table 2). Of the 10 hips with a closed femoral head epiphysis at most recent followup, one hip showed Class IV, four hips were Class III, and five hips Class II according to Stulberg et al. [23].
With the numbers available, the mean Merle d’Aubignè-Postel score did not improve from 14.5 (range, 12–16) preoperatively to 15.7 ± 1.8 (range, 12–16) at latest followup (p = 0.072; Table 3). The pain subscore improved from 3.5 (range, 1–5) preoperatively to 5.0 (range, 3–6) at latest followup (p = 0.026; Table 3). Flexion, internal rotation, and external rotation were not observed to have improved for all patients from preoperative status to the latest followup with the numbers available (Table 3).
Table 3.
Clinical results preoperatively and at followup
| Parameter (best–worst score possible) | Preoperative* | Followup* | p value |
|---|---|---|---|
| Merle d’Aubigné-Postel score [14] (18–0) | 14.5 (12–16) | 15.7 (12–18) | 0.072 |
| Pain (6–0) | 3.5 (1–5) | 5.0 (3–6)† | 0.026 |
| Mobility (6–0) | 5.3 (2–6) | 5.1 (4–6) | 0.608 |
| Walking ability (6–0) | 5.7 (5–6) | 5.6 (5–6) | 0.564 |
| ROM (°) | |||
| Flexion | 94 (35–130) | 91 (70–125) | 0.778 |
| Internal rotation in 90° of flexion | 13 (0–50) | 15 (5–35) | 0.465 |
| External rotation in 90° of flexion | 28 (0–45) | 23 (5–45) | 0.513 |
* Continuous parameters are expressed as mean with range in parentheses; †significant difference compared with preoperative.
Subsequent surgical procedures were performed in seven of 11 hips (Table 4). In addition to two hips with hardware removal only, subsequent surgery was performed in five of 11 hips for improvement of containment after a mean interval of 2.3 years (range, 0.2–7.5 years; Table 4). Of those, two hips had a triple osteotomy (Fig. 3), one hip a combined triple and valgus intertrochanteric osteotomy, one hip an intertrochanteric varus osteotomy, and one hip a PAO with a separate valgus intertrochanteric osteotomy. Resection of heterotopic ossification (Brooker Grade II) with hardware removal was performed in one hip with a subsequent triple osteotomy (Table 4). This hip was graded as a Grade III complication according to the Dindo-Clavien complication classification [19, 20] as a result of the heterotopic ossification. All femoral head and trochanteric osteotomies healed within 8 to 12 weeks after surgery. No hip developed avascular necrosis of the femoral head.
Table 4.
Detailed demographic and surgery-related data of the patient series
| Patient number | Disorder | Age (years) | Open femoral head physis | Sex | Previous surgery | Type and maximum width of resection | Concomitant surgery* | Subsequent surgery | Stulberg classification [23] at most recent followup | Final head morphology |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | LCPD | 7 | Yes | Woman | None | Rectangular (8 mm) | None | PAO†; valgus-derotational IO†; hardware removal | III | Not spherical; contained |
| 2 | LCPD | 7 | Yes | Man | None | Trapezoidal (14 mm) | None | Triple† resection of heterotopic ossification with hardware removal | IV | Flat; contained |
| 3 | LCPD | 8 | Yes | Man | None | Triangular (10 mm) | Triple†; anterior offset | Hardware removal | III | Not spherical; contained |
| 4 | LCPD | 9 | Yes | Man | None | Rectangular (8 mm) | Anterior offset | Triple† | II | Spherical; contained |
| 5 | LCPD | 9 | Yes | Woman | None | Rectangular (10 mm) | Triple† | Hardware removal | II | Spherical; contained |
| 6 | LCPD | 10 | Yes | Man | None | Rectangular (12 mm) | None | Triple with valgus IO† | NA‡ | Spherical; contained |
| 7 | LCPD | 11 | Yes | Man | None | Rectangular (8 mm) | None | None | III | Not Spherical; contained |
| 8 | LCPD | 14 | No | Man | Varus IO | Rectangular (15 mm) | PAO†; anterior offset | None | III | Not Spherical; contained |
| 9 | LCPD | 18 | No | Man | None | Rectangular (10 mm) | Acetabular rim trimming | Varus IO†; hardware removal | II | Spherical; contained |
| 10 | LCPD | 22 | No | Woman | None | Rectangular (20 mm) | PAO†; anterior offset | None | II | Spherical; contained |
| 11 | DDH | 23 | No | Woman | None | Rectangular (10 mm) | Colonna procedure† | None | II | Spherical; contained |
* Other than femoral head reduction osteotomy and relative femoral neck lengthening, which was performed in all 11 hips; †surgery to improve femoral head containment; ‡open physis at most recent followup; LCPD = Legg-Calvé-Perthes disease; DDH = developmental dysplasia of the hip; PAO = periacetabular osteotomy; IO = intertrochanteric osteotomy; NA = not applicable.
Discussion
An aspherical and enlarged femoral head, as exists in hips with LCPD, is not contained in the acetabulum and can result in hinged abduction, hip pain, and impaired function (Fig. 4). Hips with an asphericity in the frontal plane often present with central necrosis of the head and are difficult to treat. They cannot be treated by resection as a result of risk of damaging the nutrient vessels. Surgical hip dislocation with development of an extended retinacular soft tissue flap gives safe access to the femoral head and enables intracapital osteotomies. However, only limited information of clinical and radiographic outcome after femoral head reduction osteotomy has been reported [3, 11, 16]. We therefore asked whether femoral head reduction osteotomy in hips with severe asphericity of the femoral head results in (1) improved head sphericity and containment; (2) pain relief and improved hip function; and (3) subsequent reoperations or complications including avascular necrosis.
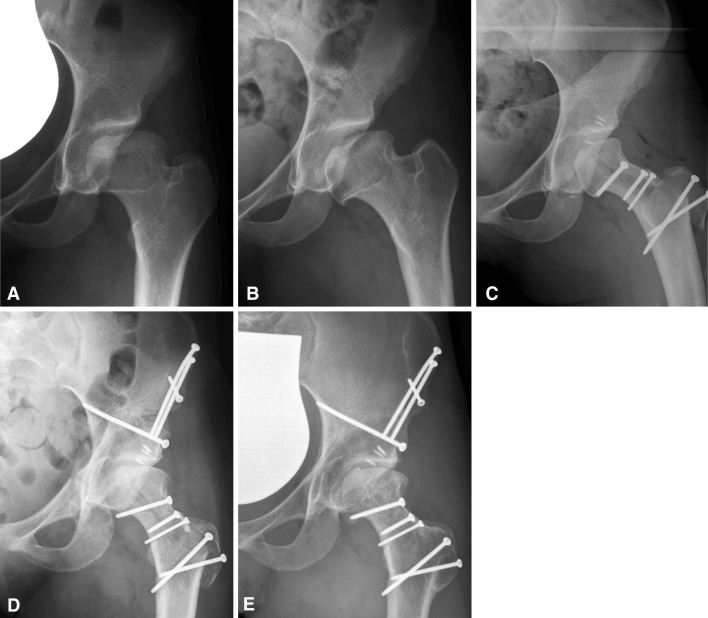
Fig. 4A–E.
(A) A 22-year-old female patient had sequelae of LCPD. (B) In abduction, the femoral head cannot enter the acetabulum as a result of the large asphericity of the head resulting in hinged abduction of the joint. (C) After head reduction osteotomy, the femoral head was able to enter the acetabulum as a result of decreased size and improved sphericity, which resulted in improved abduction. (D) Containment was improved by a concomitant PAO. (E) At 5-year followup, the head and trochanter osteotomies were healed and the joint space was maintained.
Our study has several limitations. First, femoral head sphericity and containment were only assessed with the use of plain AP pelvic radiographs, which are two-dimensional projections of three-dimensional reality; however, the main deformity in the hips we reviewed was found in the frontal plane, which is best seen in the AP view. Therefore, we believe we could quantify head sphericity adequately. Second, as a result of the retrospective design of the study, the only clinical scoring system available with preoperative values was the Merle d’Aubigné-Postel score and other preoperative clinical data, eg, complete assessment of ROM, were missing. Despite the relatively insensitive Merle d’Aubigné-Postel score, a small improvement in the pain subscore was found. Further studies should use more precise instruments to evaluate clinical outcome. Third, the total number of patients with femoral head reduction osteotomy was low as a result of the relatively rare hip pathology with a severe femoral head asphericity and the novel surgical technique. In the current series all patients who underwent femoral head reduction osteotomy at the authors’ institution were included. However, this limited number does not allow evaluating subgroups with and without an open femoral head physis and the limited followup does not allow drawing a definitive conclusion on joint preservation.
Both head sphericity and containment improved after femoral head reduction osteotomy and concomitant acetabular containment surgery in five of 20 hips (Table 2). Of the 10 hips with a closed femoral head epiphysis at most recent followup, five had a contained and spherical head (Class II according to Stulberg et al. [23]; Fig. 5), four had an ovoid but contained head (Class III), and one hip had a flat but contained head (Class IV). The hip with Class IV according to Stulberg et al. [23] and no improvement of head sphericity occurred in a 7-year-old boy, who required a subsequent triple osteotomy 10 months after index surgery to improve containment of the head (Table 4). Paley [16] reported a series of 20 patients (20 hips) undergoing femoral head reduction osteotomy and assessed femoral head sphericity using a ratio of femoral head diameter of the affected side divided by the diameter of the contralateral side [16]. An improvement in head sphericity from a mean ratio of 133% (range, 115%–160%) preoperatively to 96% (range, 91%–100%) postoperatively was reported [16].
Fig. 5A–B.
(A) An 18-year-old male patient presented with central necrosis of the femoral head and subluxation. (B) After head reduction osteotomy and subsequent varus intertrochanteric osteotomy, a spherical and contained femoral head was achieved with a good clinical result at 10-year followup.
No improvement of the total Merle d’Aubigné score or ROM was found at most recent followup (Table 3). The mean pain subscore improved from preoperatively 3.5 to 5.0 (p = 0.026; Table 3). This is comparable to the improvement found in hips with idiopathic FAI with an increase of the mean pain subscore from preoperatively 4 to 5 at followup [21]. Paley [16] reported the clinical results of 20 patients (20 hips) after femoral head reduction osteotomy. Both surgical technique and hip disorders (LCPD and hip dysplasia) were comparable to the current study. At a mean followup of 2.7 years (range, 1–5 years), he reported improvement in gait in all 20 hips, improvement in pain in 17 of 20 hips, and improvement of ROM in 15 of 20 hips [16]. However, no clinical scores or detailed information of ROM were reported for this study [16]. Therefore, direct comparison of the results is difficult. The lack of improvement of the total Merle d’Aubigné score or ROM in the current study could be the result of the limited number of 11 hips, which is associated with a decreased likelihood to detect differences.
In five of the 11 hips, subsequent surgery to improve femoral head containment was performed (Table 4). At the index operation, another five hips had concomitant surgery to improve containment (Table 4). In total, 10 of 11 hips had either concomitant or subsequent containment surgery including acetabular osteotomies, intertrochanteric osteotomies (Fig. 5), or a combination of them (Table 4). In only one of 11 hips did an isolated femoral head reduction osteotomy result in a spherical and contained femoral head (Table 4). This reflects the high proportion of dysplastic acetabula in hips with LCPD [7], especially in hips with a severe femoral head deformity [12, 15]. Leunig and Ganz [11] reported additional containment surgery in 13 of 14 hips, including nine concomitant (one Colonna procedure and eight PAOs) and four subsequent procedures (one varus intertrochanteric osteotomy [IO] and three PAOs). In contrast, Paley [16] reported a considerably lower proportion of five of 20 hips with additional containment surgery, including three concomitant Wagner pelvic osteotomies and two subsequent PAOs. In the current series, containment was overestimated in five hips at the time of index surgery and the femoral head subluxed over time requiring subsequent surgery (Fig. 3). As a consequence of these results, additional containment surgery is presently performed more frequently at the time of femoral head reduction osteotomy instead of a subsequent procedure. In the last six femoral head reduction osteotomies performed, five had a concomitant containment procedure. We believe that adequate femoral head containment allows the head to remodel in a more ideal way in hips with an open femoral head physis. The benefit of an additional containment surgery with a femoral head reduction osteotomy has also been emphasized by other authors [4, 11]. In the current series, there was only one complication according to the Dindo-Clavien [19, 20] classification, which was one hip with heterotopic ossification requiring resection. Paley [16] reported one of 20 hips with avascular necrosis of the head, which occurred in an 11-year-old boy. Reportedly, this was the only case of a patient with an open physis at the time of surgery and the only one who had undergone previous surgery (adduction IO) in his series. Our data show that femoral head reduction osteotomy can also be performed in hips with an open epiphysis or those having undergone previous surgery without the occurrence of avascular necrosis. Based on the current series and the results from Paley [16], avascular necrosis seems to be rare after femoral head reduction osteotomy. In the series by Paley [16], three of 21 hips converted to a THA [15]—one hip at the time of surgery as a result of a femoral neck fracture and two hips because of pain and advanced joint degeneration during followup. Despite the longer followup in our series, no hip underwent conversion to THA.
Severe asphericities of the femoral head in the frontal plane are rare but can result in subluxation, hinged abduction, pain, and impaired function. The femoral head reduction osteotomy respects the blood supply of the femoral head and allows improving femoral head sphericity. Avascular necrosis seems to be rare after this procedure. However, sufficient containment in these hips with an often dysplastic acetabulum requires additional surgery such as acetabular reorientation, which is ideally performed at the time of the head reduction osteotomy. Combined treatment of femoral head and acetabular pathomorphologies can result in reduced pain. With the limited numbers of hips available in the current study, function did not improve. Therefore, future studies should use more precise instruments to evaluate clinical outcome and include longer followup to prove joint preservation.
Electronic supplementary material
Footnotes
One of the authors (Moritz Tannast) has received funding from the Swiss National Science Foundation (SNSF). Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Colonna PC. Arthroplasty of the hip for congenital dislocation in children. J Bone Joint Surg Am. 1947;29:711–722. [PubMed] [Google Scholar]
- 2.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular osteotomies in complex hip deformities. Clin Orthop Relat Res. 2010;468:3168–3180. doi: 10.1007/s11999-010-1489-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganz R, Huff TW, Leunig M. Extended retinacular soft-tissue flap for intra-articular hip surgery: surgical technique, indications, and results of application. Instr Course Lect. 2009;58:241–255. [PubMed] [Google Scholar]
- 5.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. 1988. Clin Orthop Relat Res. 2004;418:3–8. doi: 10.1097/00003086-200401000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Holm I, Bolstad B, Lutken T, Ervik A, Rokkum M, Steen H. Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–248. doi: 10.1002/pri.204. [DOI] [PubMed] [Google Scholar]
- 7.Joseph B. Morphological changes in the acetabulum in Perthes’ disease. J Bone Joint Surg Br. 1989;71:756–763. doi: 10.1302/0301-620X.71B5.2584244. [DOI] [PubMed] [Google Scholar]
- 8.Kalhor M, Horowitz K, Gharehdaghi J, Beck M, Ganz R. Anatomic variations in femoral head circulation. Hip Int. 2012;22:307–312. doi: 10.5301/HIP.2012.9242. [DOI] [PubMed] [Google Scholar]
- 9.Keret D, Harrison MH, Clarke NM, Hall DJ. Coxa plana—the fate of the physis. J Bone Joint Surg Am. 1984;66:870–877. doi: 10.2106/00004623-198466060-00007. [DOI] [PubMed] [Google Scholar]
- 10.Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil. 2005;19:659–661. doi: 10.1191/0269215505cr869oa. [DOI] [PubMed] [Google Scholar]
- 11.Leunig M, Ganz R. Relative neck lengthening and intracapital osteotomy for severe Perthes and Perthes-like deformities. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S62–S67. [PubMed] [Google Scholar]
- 12.Madan S, Fernandes J, Taylor JF. Radiological remodeling of the acetabulum in Perthes’ disease. Acta Orthop Belg. 2003;69:412–420. [PubMed] [Google Scholar]
- 13.McWhirk LB, Glanzman AM. Within-session inter-rater realiability of goniometric measures in patients with spastic cerebral palsy. Pediatr Phys Ther. 2006;18:262–265. doi: 10.1097/01.pep.0000234960.88761.97. [DOI] [PubMed] [Google Scholar]
- 14.Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed]
- 15.Meurer A, Bohm B, Decking J, Heine J. [Analysis of acetabular changes in Morbus Perthes disease with radiomorphometry] [in German] Z Orthop Ihre Grenzgeb. 2005;143:100–105. doi: 10.1055/s-2004-832408. [DOI] [PubMed] [Google Scholar]
- 16.Paley D. The treatment of femoral head deformity and coxa magna by the Ganz femoral head reduction osteotomy. Orthop Clin North Am. 2011;42:389–399. doi: 10.1016/j.ocl.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 17.Quain S, Catterall A. Hinge abduction of the hip. Diagnosis and treatment. J Bone Joint Surg Br. 1986;68:61–64. doi: 10.1302/0301-620X.68B1.3941142. [DOI] [PubMed] [Google Scholar]
- 18.Rowe SM, Jung ST, Cheon SY, Choi J, Kang KD, Kim KH. Outcome of cheilectomy in Legg-Calve-Perthes disease: minimum 25-year follow-up of five patients. J Pediatr Orthop. 2006;26:204–210. doi: 10.1097/01.bpo.0000194696.83526.6d. [DOI] [PubMed] [Google Scholar]
- 19.Sink EL, Beaule PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011;93:1132–1136. doi: 10.2106/JBJS.J.00794. [DOI] [PubMed] [Google Scholar]
- 20.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470:2220–2226. doi: 10.1007/s11999-012-2343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steppacher SD, Huemmer C, Schwab JM, Tannast M, Siebenrock KA. Surgical hip dislocation for treatment of femoroacetabular impingement: factors predicting 5-year survivorship. Clin Orthop Relat Res. 2014;472:337–348. doi: 10.1007/s11999-013-3268-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 24.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 25.Ziebarth K, Slongo T, Siebenrock KA. Residual Perthes deformity and surgical reduction of the size of the femoral head. Oper Tech Orthop. 2013;23:134–139. doi: 10.1053/j.oto.2013.08.001. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.