Abstract
Background
Many patients who undergo periacetabular osteotomy (PAO) for symptomatic acetabular dysplasia experience decreased pain and improved function, yet some experience inadequate clinical improvement. The etiologies of treatment failure have not been completely defined, and sex-dependent disease characteristics that may be associated with less pain relief are not understood.
Question/purposes
We sought to determine whether there were clinically important sex-specific differences between male and female patients undergoing PAO for acetabular dysplasia in terms of (1) clinical parameters (anthropomorphic traits and hip scores), (2) radiographic findings, and (3) intraoperative findings at the time of PAO, in particular findings potentially associated with femoroacetabular impingement (FAI) such as chondromalacia at the head-neck junction, impingement trough, or reduced head-neck offset.
Methods
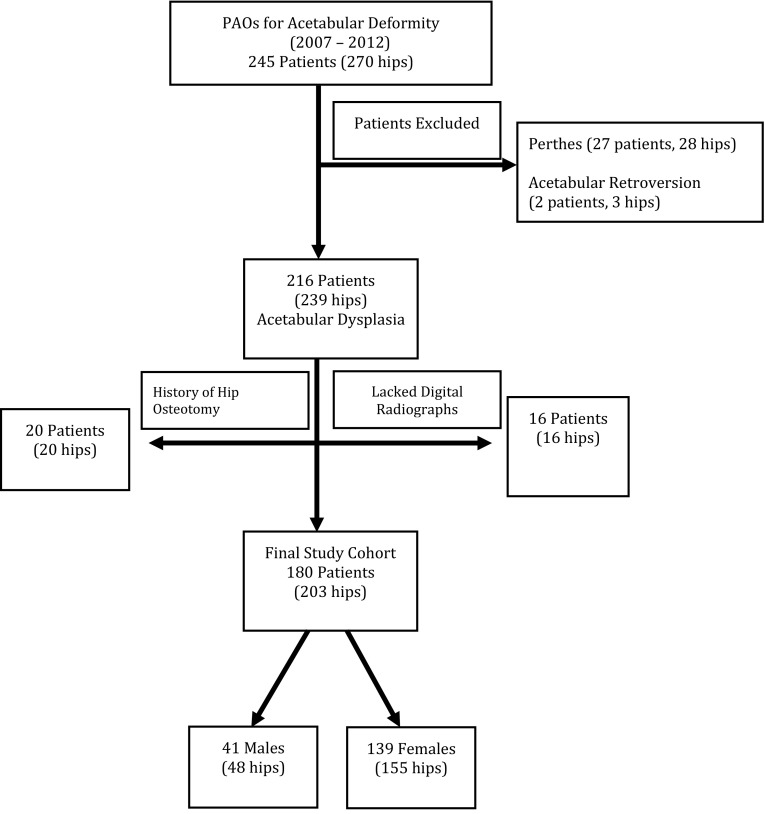
Between 2007 and 2012 we treated 245 patients (270 hips) with a PAO for symptomatic acetabular dysplasia. Of those, 16 patients (16 hips; 6%) had insufficient documentation for review in the medical record and another 49 patients (51 hips; 19%) met prespecified exclusion criteria, leaving 180 patients (203 hips; 75%) for analysis in this retrospective study. One hundred thirty-nine patients were females and 41 were males. Clinical data including patient demographics, physical examination, patient self-reported outcome scores, radiographic morphologic features, and intraoperative findings were collected prospectively as part of an institutional registry. Statistical analysis was performed with univariate and multivariate analyses.
Results
Mean age was similar among sexes; however, BMI was greater in males compared with females (26 versus 24 kg/m2; p = 0.002). Males had less hip ROM including internal rotation at 90° flexion (14° ± 13.8° versus 25° ± 16.2°; p = 0.001). Males had higher preoperative UCLA (7 ± 2, versus 6 ± 2; p = 0.02) and Harris hip scores (63 ± 15 versus 58 ± 16; p = 0.04). Radiographically, a crossover sign (88% versus 39%; p < 0.001) and posterior wall sign (92% versus 63%; p < 0.001) were more common in males. Males had greater alpha angles on the frog lateral (63° ± 15.3° versus 58° ± 16°; p = 0.04) and Dunn radiograph views (64° ± 15.5° versus 56° ± 14.8°; p = 0.02). The incidence of femoral head-neck chondromalacia (62% versus 82%; p = 0.03) and an impingement trough observed at surgery was greater in males (35% versus 17%; p = 0.01). Multivariate analysis showed differences between the sexes for reduced internal rotation in flexion, a higher Dunn alpha angle, increased incidence of a crossover sign, and a lower anterior center-edge angle.
Conclusions
There are sex-dependent, disease characteristic differences in patients with symptomatic acetabular dysplasia. Most notably, male patients have a greater prevalence of clinical, radiographic, and intraarticular findings consistent with concurrent FAI and instability and potentially a heightened risk of secondary FAI after PAO, however postoperative and long-term followup are needed to confirm these findings and it remains unclear which patients need surgical correction of the impingement and instability. Preoperative evaluation of acetabular dysplasia in males should at least include careful attention to factors associated with symptomatic FAI; however, further studies are needed to determine when surgical correction is needed.
Level of Evidence
Level III, therapeutic study.
Introduction
Acetabular dysplasia is characterized by a constellation of anatomic features, including relative deficiency in anterolateral acetabular coverage of the femoral head [13]. This results in increased joint reactive forces, acetabular rim overload, and eventual articular cartilage degeneration. The osteoarthritic biologic cascade associated with acetabular dysplasia is considered one of the most common causes of secondary hip degeneration [3, 15, 24, 29]. To correct acetabular dysplasia deformities, Ganz et al. [12] popularized the Bernese periacetabular osteotomy (PAO). The underlying principles of this procedure include reorientation of the acetabulum, reduction of superolateral inclination, improvement of femoral head coverage, medial translation of the joint center, and normalization of anterolateral acetabular rim loading [10, 12, 36].
Despite good surgical results in terms of improved pain and function for many patients treated with PAO [16, 21, 26, 37, 41], there are patients who do not experience optimal clinical results [1, 25, 37, 43]. Nevertheless, the reasons for suboptimal clinical results are not fully understood. Various factors affect the results of PAO including the details of acetabular reduction, associated intraarticular abnormalities, secondary femoroacetabular impingement (FAI), previous surgeries, and occurrence of perioperative complications [1, 10, 23, 31]. It is our clinical impression that sex-dependent disease characteristics are important, and improved understanding of these variable disease characteristics may clarify some of the differences in clinical results. More importantly, such information may assist in refining patient selection criteria and PAO surgical technique. For example, secondary FAI is a known cause of clinical failure and has been reported in males and females [25, 43]. The effect that patient sex may have on residual impingement or signs and symptoms of preoperative impingement has not been reported to our knowledge. With an increased concern that secondary FAI may compromise the clinical outcomes and survivorship of PAO, there is heightened interest in identifying patients at risk preoperatively and performing the surgical procedure such that secondary FAI is avoided [1, 26]. However, to our knowledge, the effect of patient sex on the clinical presentation and baseline clinical scores, radiographic findings, and intraoperative disease characteristics has not been fully investigated for patients with symptomatic acetabular dysplasia. The purpose of this study was to determine whether there were clinically important sex-specific differences between male and female patients undergoing PAO for acetabular dysplasia in terms of (1) clinical parameters (anthropomorphic traits and hip scores), (2) radiographic findings, and (3) intraoperative findings at the time of PAO, in particular findings potentially associated with FAI such as chondromalacia at the head-neck junction, impingement trough, or reduced head-neck offset.
Patients and Methods
We performed a review of our institution’s prospectively maintained database for patients treated at Barnes-Jewish Hospital (Washington University School of Medicine, St Louis, MO, USA) for symptomatic acetabular deformity with a PAO. The STROBE initiative guidelines were followed for this study. Institutional review board approval was obtained for this study. Between April 1, 2007, and January 1, 2012, 245 patients (270 hips) were treated with a PAO by the two senior authors (JCC, PLS) for acetabular dysplasia (Fig. 1). After excluding 31 hips (12%) that had acetabular dysplasia secondary to Perthes-like deformities or acetabular retroversion, there were 216 patients (239 hips). We excluded an additional 16 patients (16 hips, 6%) because digital radiographs were not archived in the electronic medical record and were unavailable for review and 20 patients (20 hips, 7%) who had a previous ipsilateral osteotomy to the affected hip. This left 180 patients (203 hips, 75%) for this study. Of the 180 patients (203 hips), 139 (155 hips, 76%) were females with an average age of 26 years (range, 9–49 years) and 41 (48 hips, 24%) were males with an average age of 27 years (range, 12–44 years) (p > 0.5).
Fig. 1.
The flow diagram shows the reasons for inclusion and exclusion for the study group.
We considered PAO in patients with symptomatic acetabular dysplasia for whom nonoperative treatment had failed, whose hips had a lateral center-edge angle less than 20°, and a congruent femoral head and acetabulum. All 180 patients who participated in the study had demographic data including sex, height, weight, BMI, and age at the time of surgery. All of the patients had a standard evaluation of bilateral hips, while in the supine position, for the endpoints to ROM, performed by one examiner (JCC) [32]. The patients were tested for ROM in flexion and flexion (90°) with internal rotation. The maximal amount of motion for flexion and internal rotation of each hip without causing motion of the pelvis was recorded [32]. The anterior impingement test was performed and recorded for all patients. The test was considered positive if groin pain was reproduced with the hip flexed (90°), adducted (10°), and internally rotated (10°–15°) [25].
Patients were given a self-reported, validated patient outcomes packet at their preoperative clinic visit that included the modified Harris hip score (HHS), Hip Disability and Osteoarthritis Score (HOOS), WOMAC, SF-12v2, and the UCLA activity score.
The patients were evaluated with standardized supine AP pelvic, false profile, frog leg lateral, cross-table lateral, and 45° Dunn view radiographs. Morphologic features of the acetabulum as seen on radiographs were defined with the lateral center-edge angle of Wiberg [42] (AP), the anterior center-edge angle of Lequesne and de Seze [18] (false profile), and acetabular inclination [11, 24] (AP). Parameters for evaluation of possible femoral head-neck junction abnormalities included the alpha angle [9, 22, 28] (frog leg lateral, Dunn, and cross-table lateral views). Additional parameters to evaluate acetabular version included the crossover sign (AP) [40] and posterior wall sign (AP) [40]. These measurements were performed only if appropriate pelvic tilt was present (sacrococcygeal distance for males 15–50 mm, females 30–65 mm) [34]. Appropriate pelvic tilt as measured on the AP radiographs was present in 52% of male and 57% of female patients. These measurements were made using computer-assisted radiographic measurement software (Emageon, Birmingham, AL, USA). Radiographic analysis was performed by one author (GP) experienced in radiographic measurements of the prearthritic hip. The intraclass correlation coefficients (ICCs) for intraobserver variability ranged from 0.91 to 0.99. Interobserver reliability between two of the authors (SD and GP) for ICCs for the lateral center-edge angle was 0.89, acetabular inclination was 0.95, and anterior center-edge angle was 0.91. Previous studies for ICCs for the lateral center-edge angle have ranged from 0.42 to 0.92, the acetabular inclination from 0.45 to 0.85, and anterior center-edge angle from 0.55 to 0.88 [2, 4, 5, 7, 20, 27, 39].
The acetabular osteotomy was performed using the technique popularized by Ganz et al. through an abductor-sparing, modified Smith-Petersen approach [6, 12, 19, 35]. Prospectively, data collection was performed for the intraoperative details that included the condition of the acetabular labrum, presence or absence of chondromalacia involving the femoral and/or acetabular chondral surfaces, the amount of femoral head-neck offset, and presence of an “impingement trough,” defined as a local indentation of the osteochondral tissue at the head-neck junction [33]. Agreement was reached by the two senior surgeons (JCC, PLS) on these details at the time surgery was performed during this prospective data collection. Eighty-eight percent of patients had an open arthrotomy at the time of the PAO (44 males, 178 females). Indications to perform an arthrotomy included reduced femoral head-neck offset requiring a femoral osteochondroplasty, suspected acetabular labral tear, and/or restricted interoperative rotation in flexion (45°) after the PAO. An arthrotomy was not performed if there were adequate head-neck offset, low suspicion for labral detachment, and adequate internal rotation in flexion (≥ 15°) after the PAO. Because not all patients underwent an open arthrotomy and, even in patients with an arthrotomy, intraarticular observation varied. Thus, reporting of the intraarticular data was not available for all patients and varied for each parameter depending on whether an arthrotomy was performed and adequate observation was achieved.
Statistical comparisons of the disease characteristics for female and male patients were performed using univariate and multivariate analyses with Bonferroni correction. Post hoc power analyses were performed for the radiographic parameters, patient-reported outcome scores, and the physical examination findings. These were 80%, 65%, and 99% powered respectively. The intraoperative data were not included in the multivariate analysis owing to the lack of complete data available.
Results
Anthropometric Differences and Hip Scores
Male patients had a higher BMI, and, in general, less flexible hips. The average BMI for males was 26 kg/m2 (range, 19–37 kg/m2) versus 24 kg/m2 (range, 16–34 kg/m2) for females (p = 0.002). Physical examination (Table 1) revealed that the male patients had decreased ROM compared with the female patients for internal rotation in flexion (14° ± 13.8° versus 25° ± 16.2°; p = 0.001). There was no clinical difference between males and females regarding hip flexion (96° ± 6.6 versus 99° ± 9.6; p = 0.08) or for the incidence of an anterior impingement sign (76% versus 82%; p = 0.62).
Table 1.
Comparison of clinical examination findings
| Finding | Females | Males | p value* univariate analysis | p value* multivariate analysis | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Mean | SD | 95% CI | |||
| Anterior impingement test positive (%)† | 82% | 3.3 | 76–88 | 76% | 6.3 | 64–88 | 0.62 | 0.73 |
| End flexion (degrees) | 99 | 9.6 | 97–101 | 96 | 6.6 | 93–99 | 0.08 | 0.26 |
| Internal rotation in flexion (degrees) | 25 | 16.2 | 22–27 | 14 | 13.8 | 9–18 | 0.001 | 0.002 |
* t-test; †Fisher’s exact test.
The baseline modified HHS was higher in males compared with females preoperatively (63 ± 15 versus 58 ± 16; p = 0.04) (Table 2). The UCLA activity score also was higher in males compared with females (7 ± 2 versus 6 ± 2; p = 0.02). The WOMAC, HOOS, and SF-12 scores were not different between the two sexes (Table 2).
Table 2.
Baseline clinical function scores
| Outcome score | Female | Male | p value* univariate analysis | p value* multivariate analysis | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Mean | SD | 95% CI | |||
| Modified HHS | 58 | 16 | 55–60 | 63 | 15 | 59–68 | 0.04 | 0.85 |
| UCLA Activity Score | 6 | 2 | 5–7 | 7 | 2 | 6–8 | 0.02 | 0.19 |
| WOMAC | 35 | 21 | 30–39 | 29 | 16 | 22–36 | 0.14 | 0.67 |
| HOOS | 248 | 90 | 233–262 | 275 | 84 | 248–302 | 0.07 | 0.90 |
| SF-12 | ||||||||
| Physical | 37 | 11 | 36–40 | 38 | 10 | 34–41 | 0.87 | 0.29 |
| Emotional | 53 | 11 | 50–54 | 55 | 8 | 51–58 | 0.24 | 0.25 |
* t-test; HHS = Harris hip score; HOOS = Hip Disability and Osteoarthritis.
Radiographic Differences Between Male and Female Patients
Radiographic features (Table 3) of cam-type FAI were more common in the male patients compared with the female patients with elevated alpha angles measured on the frog lateral view (63° ± 15.3°, versus 58° ± 16°; p = 0.04), and Dunn view (64° ± 15.5° versus 56° ± 14.8°; p = 0.02). A positive crossover sign was more common in males than females (88% versus 39%; p < 0.001). A positive posterior wall sign (posterior wall deficiency) was present in 92% of males and 63% of females (p < 0.006). Male patients were found to have a lower anterior center-edge angle compared with female patients (12° ± 16.5°, versus 14° ± 12.2°; p = 0.02), whereas no difference was seen in the lateral center-edge angle and acetabular inclination between males and females (p > 0.05).
Table 3.
Comparison of radiographic measures of morphologic features of the hips
| Radiographic finding | Females | Males | p value univariate analysis | p value multivariate analysis | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Mean | SD | 95% CI | |||
| Lateral center-edge angle (degrees) | 11 | 10.2 | 9–13 | 7 | 13.2 | 4–11 | 0.76 | 0.94 |
| Anterior center-edge angle (degrees) | 14 | 12.2 | 11–16 | 12 | 16.5 | 8–16 | 0.02 | 0.02 |
| Acetabular inclination (degrees) | 17 | 7 | 15–18 | 22 | 9.6 | 20–25 | 0.49 | 0.75 |
| Crossover sign (%)† | 39 | 4.2 | 31–47 | 88 | 4.8 | 79–97 | 0.001 | 0.01 |
| Posterior wall sign (%)† | 63 | 4.2 | 55–71 | 92 | 4.0 | 84–99 | 0.006 | 0.18 |
| α angle (degrees) | ||||||||
| Frog leg view | 58 | 16.0 | 55–61 | 63 | 15.3 | 58–67 | 0.04 | 0.14 |
| Dunn view | 56 | 14.8 | 53–59 | 64 | 15.5 | 58–69 | 0.02 | 0.03 |
†Fisher’s exact test.
Intraoperative Differences Between the Sexes
Intraoperative findings for intra- and extraarticular differences between the sexes were recorded (Table 4). At the time of surgery, several morphologic features consistent with FAI were more frequent in males than females, and included the presence of chondromalacia at the femoral head-neck junction (82%, n = 32/39 hips versus 62%, n = 77/144; p = 0.03) and an impingement trough (35%, n = 16/46 hips versus 17%, n = 23/137 hips; p = 0.01). Labral tears were relatively common in female and male patients (82%, n = 87/106 hips versus 66%, n = 19/29 hips, respectively; p = 0.07), as was reduced head-neck offset (females, 96%, n = 132/137 versus 100%, n = 46/46; p = 0.33).
Table 4.
Intraarticular disease characteristics
| Intraoperative finding | Female | Male | p value* |
|---|---|---|---|
| Percentage (number of hips/hips with data) | |||
| Labral tear | |||
| Yes | 82% (87/106) | 66% (19/29) | 0.07 |
| Chondromalacia head-neck junction | |||
| Yes | 62% (77/144) | 82% (32/39) | 0.03 |
| Reduced head-neck offset | |||
| Yes | 96% (132/137) | 100% (46/46) | 0.33 |
| Impingement trough | |||
| Yes | 17% (23/137) | 35% (16/46) | 0.01 |
* Fisher’s exact test; these data were obtained at the time of surgery. Not all patients had an arthrotomy, and in some the presence of disease was not able to be determined.
Multivariate analysis also revealed that male sex is associated with decreased internal rotation in flexion (p = 0.002), crossover sign (p = 0.01), Dunn view alpha angle (p = 0.03), and anterior center edge angle (p = 0.02).
Discussion
Periacetabular osteotomy for the treatment of symptomatic acetabular dysplasia is well established and provides good outcomes for most patients at intermediate to long-term followup [21, 37]. Nevertheless, with a survivorship rate of 76% at 9 years and 60% at 20 years, some patients do not achieve full pain relief and function, sometimes requiring conversion to THA earlier than expected. The reasons for this are not fully understood, and there is a need to refine and optimize patient selection for surgery, surgical technique, and postoperative rehabilitation protocols. We therefore sought to determine whether there were clinically important sex-specific differences between male and female patients undergoing PAO for acetabular dysplasia in terms of (1) clinical parameters (anthropomorphic traits and hip scores), (2) radiographic findings, and (3) intraoperative findings at the time of PAO, in particular findings potentially associated with FAI. We found that males presented with slightly higher preoperative hip scores and activity levels, and had radiographic and intraoperative features that might put them at increased risk for concurrent and/or secondary FAI after PAO.
Our study has some limitations. First, the intraarticular disease characterization data set is not complete for all patients because only 75% (135/180) of patients had adequate observation of the intraarticular structures and thus there was a decrease in the study size for those parameter comparisons. However, the majority of patients did have intraarticular examination and, despite this, statistically significant, sex-dependent differences were identified. Radiographic evaluation showed variation in the pelvic tilt and rotation that resulted in 52% (26/50) of the males and 58% (89/156) of the females with adequate radiographs. This affects the interpretation of the crossover and posterior wall signs. Radiographs were eliminated if they were not adequate for tilt and rotation. Despite this reduction in number of hips for analysis, post hoc power analysis for the crossover and posterior wall signs was 99%, which further adds support to the preoperative signs of impingement in males. We also identified differences in the baseline Harris hip (5 points) and UCLA Activity (1.0 point) scores between male and female patients in the univariate analysis, but the multivariate analysis failed to find a difference in sexes for the clinical outcome scores. In addition, our study probably was inadequately powered to detect differences in patient-reported outcomes. For this reason, we have not overemphasized the importance of the HHS and UCLA score findings. Finally, we do not present long-term data showing sex-dependent differences in surgical outcome attributable to secondary FAI. Such data are beyond the scope of this study, however, we have identified substantial sex-dependent differences in hip ROM, morphologic features, and objective signs of impingement (head-neck offset chondromalacia and impingement troughs). Ziebarth et al. [43] reported a higher incidence of clinical signs indicating the presence of secondary hip impingement in males after PAO.
Secondary impingement has been described as a potential source for failure of PAO [21, 25, 26, 36, 37]. Siebenrock et al. [36] found that 29% (17/58) of patients had symptomatic impingement after PAO. In a 20-year followup study, Steppacher et al. [38] examined demographic, clinical, radiographic, and surgery-related factors associated with survivorship and identified a postoperative impingement sign as one of six predictors of a poor outcome after PAO, and of these, it had the highest hazard ratio. However, no correlation between the impingement sign and sex was investigated. The other factors associated with poor outcome were advanced age, advanced osteoarthritis at the time of surgery, low Merle d’Aubigne and Postel score, preoperative limp, and postoperative extrusion index. Ziebarth et al. [43] reported on a cohort of male patients undergoing PAO, and found that 48% of them had a positive impingement sign postoperatively, but they did not compare this result with that of a female cohort. With secondary FAI, abnormal contact of the femoral head-neck junction and the anterior rim of the acetabular labrum occurs resulting in residual pain and decreased ROM [25]. The acetabulum and the proximal femur are the two involved structures in residual impingement. On the acetabular side, radiographs showing persistent anterior overcoverage or retroversion of the acetabulum can result in continued abnormal contact [14, 25, 30]. The morphologic features of the proximal femur are another potential source for residual impingement, with previous studies showing that 75% of patients with a dysplastic acetabulum have an aspheric femoral head and/or decreased head-neck offset [8, 38]. Recognizing that secondary impingement after PAO may contribute to early and late failures has prompted surgeons to avoid overcorrection of the acetabulum and/or perform femoral osteochondroplasty if needed after acetabular reorientation [1, 26]. Nevertheless, additional investigation is needed to define patient and deformity-specific factors that heighten the risk of secondary FAI after PAO. Such information will facilitate preoperative planning and surgical procedures to avoid secondary FAI.
Although there is consensus regarding the need to prevent secondary FAI after PAO, the necessity of treating potential FAI deformities is controversial. We currently use a standard set of intraoperative steps to minimize the risk of FAI. First, to ensure adequacy of the reduction of the acetabular correction and show that iatrogenic retroversion or anterior overcoverage has not occurred, intraoperative fluoroscopic imaging is obtained. Lehmann et al. [17] detailed the steps taken to obtain standardized fluoroscopic imaging of the acetabulum to ensure that proper tilt and rotation of the pelvis exist. Subjective evaluation of the lateral center-edge angle, anterior center-edge angle, acetabular inclination, extrusion index, and medial offset is performed for adequacy of the acetabular correction. We found good correlation between the values obtained for the lateral center-edge angle, anterior center-edge angle, and acetabular inclination when comparing the intraoperative fluoroscopic imaging with the postoperative radiographic imaging [17]. In addition to these radiographic measurements, acetabular version is checked to ensure the lack of a crossover sign indicating that overcorrection or anterior overcoverage does not exist. Second, we assess hip ROM after acetabular reorientation to evaluate for overcorrection and potential pincer-type impingement. Third, open arthrotomy is performed on patients at risk for FAI to dynamically assess for cam-type impingement after the acetabular reorientation [6]. The morphologic features of the femoral head and head-neck junction also are inspected. If evidence of insufficient head-neck offset exists, a femoral osteochondroplasty is performed. Nassif et al. [26] reported on this strategy and their results indicate that patients undergoing combined PAO and femoral osteochondroplasty had good results at 2 years followup without evidence of an increased complication rate [26]. Albers et al. [1] also found a higher survivorship at 10 years after PAO in patients with a spherical femoral head either preoperatively or after a concomitant femoral osteochondroplasty through an arthrotomy. Consistent with these observations, use of this combined fluoroscopic and arthrotomy technique may help reduce the chance for secondary impingement after PAO. However, whether the femoral head-neck osteoplasty is performed arthroscopically or through an open approach, the benefits must be tempered with the potential morbidity of added surgical time, femoral neck fracture with over-section, or avascular necrosis from disruption of the lateral retinacular blood vessels. Thus, understanding that males have clinical, radiographic, and intraoperative evidence of cam impingement can help guide the surgeon in the preoperative and intraoperative evaluations regarding assessment for possible impingement preoperatively and postoperatively. The data in the current study suggest that using these strategies to help treat and prevent further impingement are particularly important in male patients.
Male patients with acetabular dysplasia have a higher prevalence of clinical and radiographic signs consistent with concomitant and/or the potential for secondary FAI. At the time of PAO, preoperative evaluation of acetabular dysplasia in males should include careful attention to the preoperative ROM in flexion and internal rotation and the Dunn view α angle for the presence of potential cam impingement. Intraoperative assessment for the presence of femoral head-neck junction chondromalacia and an impingement trough will help guide the surgeon in determining the need for adjunctive femoral head-neck junction osteoplasty in light of the potential for the added morbidity associated with its performance [1, 26].
Acknowledgments
We thank Debbie Long, Associate degree and Angela Keith MS, from the Department of Orthopaedic Surgery, Washington University for assistance with preparation of the manuscript.
Footnotes
Funding was received from the Curing Hip Disease Fund (Washington University School of Medicine, St Louis, MO, USA) for research personnel salary support.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with the ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Washington University School of Medicine, St Louis, MO, USA.
References
- 1.Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614. doi: 10.1007/s11999-013-2799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson LA, Gililland J, Pelt C, Linford S, Stoddard GJ, Peters CL. Center edge angle measurement for hip preservation surgery: technique and caveats. Orthopedics. 2011;34:86. doi: 10.3928/01477447-20101221-17. [DOI] [PubMed] [Google Scholar]
- 3.Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect. 1986;35:119–128. [PubMed] [Google Scholar]
- 4.Carlisle JC, Zebala LP, Shia DS, Hunt D, Morgan PM, Prather H, Wright RW, Steger-May K, Clohisy JC. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–58. [PMC free article] [PubMed] [Google Scholar]
- 5.Carroll KL, Murray KA, MacLeod LM, Hennessey TA, Woiczik MR, Roach JW. Measurement of the center edge angle and determination of the Severin classification using digital radiography, computer-assisted measurement tools, and a Severin algorithm: intraobserver and interobserver reliability revisited. J Pediatr Orthop. 2011;31:e30–e35. doi: 10.1097/BPO.0b013e31821adde9. [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy in the treatment of severe acetabular dysplasia: surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1):65–83. doi: 10.2106/JBJS.E.00887. [DOI] [PubMed] [Google Scholar]
- 7.Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, Steger-May K, Schoenecker PL, Millis M. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467:666–675. doi: 10.1007/s11999-008-0626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009;467:128–134. doi: 10.1007/s11999-008-0481-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 10.Clohisy JC, Schutz AL. St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052. doi: 10.1007/s11999-009-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delaunay S, Dussault RG, Kaplan PA, Alford BA. Radiographic measurements of dysplastic adult hips. Skeletal Radiol. 1997;26:75–81. doi: 10.1007/s002560050197. [DOI] [PubMed] [Google Scholar]
- 12.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 13.Ganz R, Leunig M. Morphological variations of residual hip dysplasia in the adult. Hip Int. 2007;17(suppl 5):S22–S28. [PubMed] [Google Scholar]
- 14.Garras DN, Crowder TT, Olson SA. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br. 2007;89:721–724. doi: 10.1302/0301-620X.89B6.18805. [DOI] [PubMed] [Google Scholar]
- 15.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 16.Hartig-Andreasen C, Troelsen A, Thillemann TM, Soballe K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res. 2012;470:2978–2987. doi: 10.1007/s11999-012-2386-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lehmann CL, Nepple JJ, Baca G, Schoenecker PL, Clohisy JC. Do fluoroscopy and postoperative radiographs correlate for periacetabular osteotomy corrections? Clin Orthop Relat Res. 2012;470:3508–3514. doi: 10.1007/s11999-012-2483-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lequesne M, de Seze [False profile of the pelvis: a new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies][in French] Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed] [Google Scholar]
- 19.Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect. 2001;50:229–238. [PubMed] [Google Scholar]
- 20.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. doi: 10.1007/s11999-010-1447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 22.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 23.Millis MB, Kain M, Sierra R, Trousdale R, Taunton MJ, Kim YJ, Rosenfeld SB, Kamath G, Schoenecker P, Clohisy JC. Periacetabular osteotomy for acetabular dysplasia in patients older than 40 years: a preliminary study. Clin Orthop Relat Res. 2009;467:2228–2234. doi: 10.1007/s11999-009-0824-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip: a study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Nassif NA, Schoenecker PL, Thorsness R, Clohisy JC. Periacetabular osteotomy and combined femoral head-neck junction osteochondroplasty: a minimum two-year follow-up cohort study. J Bone Joint Surg Am. 2012;94:1959–1966. doi: 10.2106/JBJS.K.01038. [DOI] [PubMed] [Google Scholar]
- 27.Nelitz M, Guenther KP, Gunkel S, Puhl W. Reliability of radiological measurements in the assessment of hip dysplasia in adults. Br J Radiol. 1999;72:331–334. doi: 10.1259/bjr.72.856.10474491. [DOI] [PubMed] [Google Scholar]
- 28.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 29.Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011;93(suppl 2):17–21. doi: 10.2106/JBJS.J.01735. [DOI] [PubMed] [Google Scholar]
- 30.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. doi: 10.2106/JBJS.E.00515. [DOI] [PubMed] [Google Scholar]
- 31.Polkowski GG, Novais EN, Kim YJ, Millis MB, Schoenecker PL, Clohisy JC. Does previous reconstructive surgery influence functional improvement and deformity correction after periacetabular osteotomy? Clin Orthop Relat Res. 2012;470:516–524. doi: 10.1007/s11999-011-2158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prather H, Harris-Hayes M, Hunt DM, Steger-May K, Mathew V, Clohisy JC. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM R. 2010;2:888–895. doi: 10.1016/j.pmrj.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ross JR, Zaltz I, Nepple JJ, Schoenecker PL, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011;39(suppl):72S–78S. doi: 10.1177/0363546511412320. [DOI] [PubMed] [Google Scholar]
- 34.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 35.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed] [Google Scholar]
- 36.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. doi: 10.1097/00003086-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 40.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 41.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 42.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Act Chir Scand. 1939;83:7–38. [Google Scholar]
- 43.Ziebarth K, Balakumar J, Domayer S, Kim YJ, Millis MB. Bernese periacetabular osteotomy in males: is there an increased risk of femoroacetabular impingement (FAI) after Bernese periacetabular osteotomy? Clin Orthop Relat Res. 2011;469:447–453. doi: 10.1007/s11999-010-1544-9. [DOI] [PMC free article] [PubMed] [Google Scholar]