Abstract
Background
Complex proximal femoral deformities, including an elevated greater trochanter, short femoral neck, and aspherical head-neck junction, often result in pain and impaired hip function resulting from intra-/extraarticular impingement. Relative femoral neck lengthening may address these deformities, but mid-term results of this approach have not been widely reported.
Questions/purposes
Do patients who have undergone relative femoral neck lengthening show (1) less hip pain and greater function; (2) improved radiographic parameters; (3) significant complications requiring subsequent surgery; and (4) progression of osteoarthrosis (OA) or conversion to total hip arthroplasty (THA) at mid-term followup?
Methods
We retrospectively reviewed 40 patients (41 hips) with isolated relative femoral neck lengthening between 1998 and 2006 with sequelae of Legg-Calvé-Perthes disease (38 hips [93%]), slipped capital femoral epiphysis (two hips [5%]), and postseptic arthritis (one hip [2%]). During this time, the general indications for this procedure included a high-riding greater trochanter with a short femoral neck with abductor weakness and symptomatic intra-/extraarticular impingement. Mean patient followup was 8 years (range, 5–13 years), and complete followup was available in 38 patients (39 hips [95%]). We evaluated pain and function with the impingement test, limp, abductor force, Merle d’Aubigné-Postel score, and range of motion. Radiographic parameters included trochanteric height, alpha angle, and progression of OA. Subsequent surgeries, complications, and conversion to THA were summarized.
Results
The proportion of positive anterior impingement tests decreased from 93% (38 of 41 hips) preoperatively to 49% (17 of 35 hips) at latest followup (p = 0.002); the proportion of limp decreased from 76% (31 of 41 hips) to 9% (three of 35 hips; p < 0.001); the proportion of normal abductor strength increased from 17% (seven of 41 hips) to 91% (32 of 35 hips; p < 0.001); mean Merle d’Aubigné-Postel score increased from 14 ± 1.7 (range, 9–17) to 17 ± 1.5 (range, 13–18; p < 0.001); mean internal rotation increased to 25° ± 15° (range, 0°–60°; p = 0.045), external rotation to 32° ± 14° (range, 5°–70°; p = 0.013), and abduction to 37° ± 13° (range, 10°–50°; p = 0.004). Eighty percent of hips (33 of 41 hips) showed normal trochanteric height; alpha angle improved to 42° ± 10° (range, 27°–90°). Two hips (5%) had subsequent surgeries as a result of lack of containment; four of 41 hips (10%) had complications resulting in reoperation. Fourteen of 35 hips (40%) showed progression of OA; four of 40 hips (10%) converted to THA.
Conclusions
Relative femoral neck lengthening in hips with combined intra- and extraarticular impingement results in reduced pain, improved function, and improved radiographic parameters of the proximal femur. Although lack of long-term complications is gratifying, progression of OA was not prevented and remains an area for future research.
Level of Evidence
Level IV, therapeutic study.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-4032-9) contains supplementary material, which is available to authorized users.
Introduction
Extraarticular femoroacetabular impingement (FAI) is defined as a pathological, extracapsular abutment of the proximal femur and the pelvis. The impingement conflict occurs between the greater or lesser trochanter on the femoral side and the ischium or supraacetabular ilium on the pelvic side [42]. Extraarticular impingement is rarely reported but can occur with complex deformities of the proximal femur [1, 18, 38]. The deformities are often the sequelae of Legg-Calvé-Perthes disease (LCPD) or “Perthes-like” deformities such as sequelae of slipped capital femoral epiphysis (SCFE), postseptic arthritis, and trauma [1, 2, 23, 37]. Typically, the deformities include a high-riding greater trochanter, a short femoral neck, and an aspherical femoral head-neck junction [1, 2, 23, 37]. Complex deformities of the proximal femur can cause both intra- and extraarticular FAI, which can lead to degenerative hip pain, restricted ROM, and impaired abductor function [1].
Complex femoral deformities are difficult to address with conventional surgical techniques such as isolated proximal femoral osteotomy. Relative femoral neck lengthening addresses both extraarticular impingement by advancing the greater trochanter and intraarticular impingement by simultaneous head–neck osteochondroplasty [15, 16]. The hip is safely accessed by surgical hip dislocation [14], and femoral head perfusion is assured by developing an extended retinacular soft tissue flap [16]. Additional sources of intra- or extraarticular impingement can be treated by concomitant advancement of the lesser trochanter or femoral head reduction osteotomy [16]. Early results of relative neck lengthening in hips with complex deformities have been promising [2, 37], but to our knowledge, no mid-term results of the technique have been reported.
We therefore asked if patients with a complex deformity of the proximal femur undergoing relative neck lengthening for combined intra- and extraarticular impingement showed (1) less hip pain and greater function; (2) improved radiographic parameters; (3) significant complications requiring additional surgery; and (4) progression of osteoarthrosis (OA) or conversion to a THA at a minimum 5-year followup.
Patients and Methods
We retrospectively reviewed all 43 hips (42 patients) with a complex deformity of the proximal femur who underwent isolated relative neck lengthening for the treatment of combined intra- and extraarticular impingement between December 1998 and September 2006 (Table 1). Two hips (two patients) with skeletal immaturity Risser < Grade 3 [35] were excluded leaving 41 hips (40 patients) for analyses. The deformities were the result of sequelae of LCPD in 38 hips (93%), SCFE in two hips (5%), and septic arthritis in childhood in one hip (2%). The deformity in the 38 hips with sequelae of LCPD was graded according to Stulberg et al. [41] with Grade II (enlarged but spherical femoral head with a short neck or steep acetabulum) in two hips, Grade III (non-spherical femoral head) in 29 hips, and Grade IV (flat femoral head) in seven hips. Indication for surgery was pain in hips with a high-riding greater trochanter (Stulberg > quadrant 2 [41]), abductor weakness (< M4 [27]), intraarticular impingement of the femoral head/neck and acetabulum (positive anterior or posterior impingement test), and extraarticular impingement between the lesser/greater trochanter and the pelvis (positive impingement test; decreased abduction or external rotation with the hip extended). Contraindications for surgery were advanced OA (≥ Tönnis Grade 2 [44]). Relative femoral neck lengthening in combination with head-neck osteochondroplasty is the standard surgical procedure in our institution to address patients with complex proximal femoral deformities meeting these indications. Alternative techniques (such as true neck lengthening or other osteotomies) were not used during the study period. Goals of surgery were reduced hip pain, improved hip function, and prevention of progression of OA by eliminating intra- and extraarticular FAI. During the study period, four additional patients (four hips) underwent the procedure in addition to an acetabular osteotomy. These four patients and the two patients (two hips) with skeletal immaturity (Risser Grade < 3) were excluded from this report.
Table 1.
Demography of patient series (N = 41 hips)
| Parameter | Value |
|---|---|
| Number of patients (hips) | 40 (41) |
| Age at surgery (years ± SD) | 24 ± 11 (range, 12–48) |
| Sex (percentage men of all hips) | 54 |
| Side (percentage right of all hips) | 6 |
| Weight (kg ± SD) | 65 ± 18 (range, 31–107) |
| Height (cm ± SD) | 166 ± 13 (range, 130–184) |
| Body mass index (kg/m2 ± SD) | 23 ± 4 (17–33) |
| Previous surgery (number, hips) | |
| Isolated intertrochanteric osteotomy | 7 |
| Isolated triple osteotomy | 7 |
| Combined triple and intertrochanteric osteotomy | 2 |
| Periacetabular osteotomy | 1 |
| Femoral offset correction | 1 |
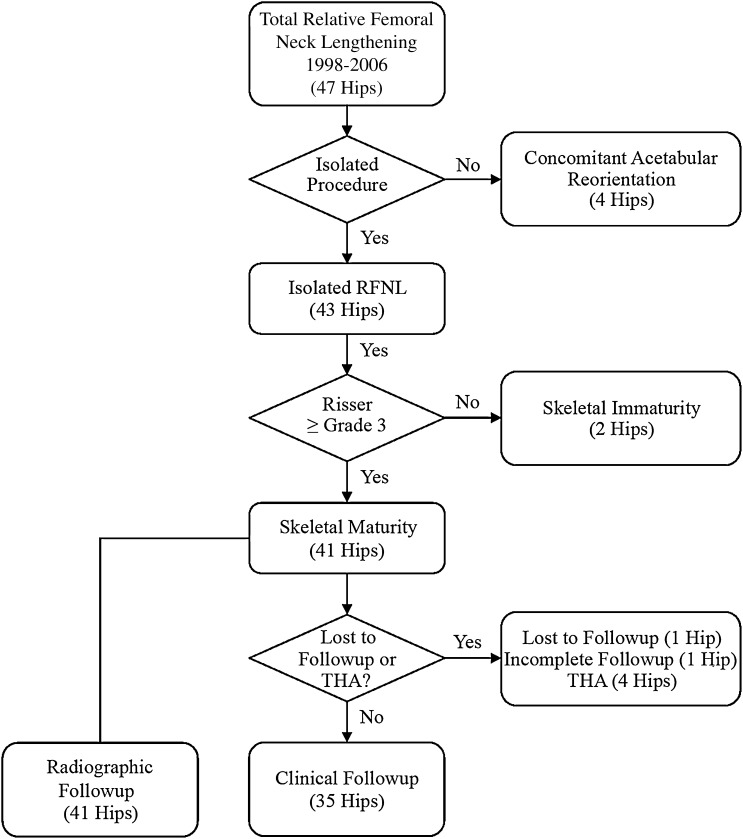
Of the initial 40 patients (41 hips) included in the study, one patient (one hip [2%]) was lost to followup before 5 years; at 3 years, the patient had an excellent clinical result (Merle d’Aubigné-Postel score of 18 points) and no radiographic signs of OA progression. Another patient refused both clinical and radiographic followup and was evaluated by means of a telephone interview and questionnaires. Since the last followup examination 2 years postoperatively, this patient has been asymptomatic and did not have further surgery of the hip. The remaining 38 patients (39 hips) were followed for a minimum of 5 years (mean, 8 years; range, 5–13 years). All patients with hips that converted to THA had complete evaluation of the postoperative radiographic parameters. Clinical followup and progression of OA were not obtained in these patients (Fig. 1). Previous surgeries included isolated acetabular osteotomy in eight hips (20%), isolated intertrochanteric osteotomy in seven hips (17%), combined acetabular and femoral osteotomy in two hips (5%), and femoral offset correction in one hip (2%; Table 1). Mean patient age at surgery was 24 years (range, 12–48 years). In all hips with relative femoral neck lengthening, concomitant osteochondroplasty of the head-neck area was performed. Additional surgical procedures were indicated in four hips (10%) to eliminate all sources of extra- or intraarticular impingement. Two hips (5%) with an aspherical femoral head in the frontal plane, which cannot be addressed by osteochondroplasty, were addressed with a femoral head reduction osteotomy [16] to obtain a spherical and well-contained femoral head. An extraarticular impingement resulting from a lesser trochanter impinging with the ischial tuberosity required distalization of the lesser trochanter in two hips (5%).
Fig. 1.
Patient selection and followup information are shown. Radiographic evaluation except progression of OA was obtained in all included 40 patients (41 hips) on the immediate postoperative radiographs.
Clinical evaluation was performed by different observers. Preoperative data were obtained based on chart review. At most recent follow up, patients were examined according to a standardized study protocol. Hip pain and function were assessed preoperatively and at most recent followup using the following parameters: anterior and posterior impingement tests (positive/negative) [43], limp (positive/negative), abductor strength (proportion of hips with abduction force M5 according to the British Medical Research Council [27]), full ROM (degrees of flexion/extension; adduction/abduction; internal/external rotation), and the Merle d’Aubigné-Postel scoring system (worst-best score of 3–18 points; Table 2) [28]. Substantial inter- and intraobserver agreement has been reported for anterior and posterior impingement tests [24, 34], abductor strength [12], full ROM [7, 33], and the Merle d’Aubigné-Postel scoring system [22]. At latest followup, additional hip scores were assessed including the WOMAC [4], Harris hip score [20], SF-12 physical and mental component scales [13, 45], and the UCLA activity scores [47].
Table 2.
Clinical results preoperatively and at minimum 5-year followup
| Parameter (best-worst score possible) | Preoperative value (n = 41) | Followup value (n = 35) | p value |
|---|---|---|---|
| Anterior impingement test (% positive) [43] | 93 | 49 | 0.002 |
| Posterior impingement test (% positive) [43] | 66 | 20 | 0.157 |
| Limp (% positive) | 76 | 9 | < 0.001 |
| Abductor strength (% with M5 of all hips) [27] | 17 | 91 | < 0.001 |
| ROM (° ± SD; range) | |||
| Flexion | 94 ± 14 (50–130) | 93 ± 16 (35–130) | 0.466 |
| Extension | 4 ± 6 (0–20) | 7 ± 7 (0–20) | 0.121 |
| Internal rotation | 18 ± 15 (0–85) | 25 ± 15 (0–60) | 0.045 |
| External rotation | 25 ± 12 (0–50) | 32 ± 14 (5–70) | 0.013 |
| Abduction | 24 ± 10 (0–45) | 37 ± 13 (10–50) | 0.004 |
| Adduction | 18 ± 11 (5–45) | 13 ± 5 (5–20) | 0.176 |
| Merle d’Aubigné scores (18–0) ± SD (range) [28] | 14 ± 1.7 (9–17) | 17 ± 1.5 (13–18) | < 0.001 |
| Pain (6–0) | 4 ± 1.1 (1–5) | 5 ± 0.8 (3–6) | < 0.001 |
| Mobility (6–0) | 5 ± 0.7 (3–6) | 6 ± 0.5 (5–6) | 0.115 |
| Walking ability (6–0) | 5 ± 0.9 (2–6) | 6 ± 0.6 (3–6) | < 0.001 |
| WOMAC (0–100) ± SD (range) [4] | 6 ± 23 (0–100) | ||
| Pain (0–100) | – | 7 ± 24 (0–100) | – |
| Stiffness (0–100) | 8 ± 25 (0–100) | ||
| Function (0–100) | 5 ± 24 (0–100) | ||
| Harris hip score (100–0) ± SD (range) [20] | – | 83 ± 10 (59–100) | – |
| SF-12 scores ± SD (range) [13, 45] | |||
| Physical component (100–0) | – | 47 ± 7 (23–59) | – |
| Mental component (100–0) | 55 ± 9 (29–64) | ||
| UCLA activity score (10–0) ± SD (range) [47] | – | 6 ± 2 (2–10) | – |
Continuous parameters are expressed as mean ± SD and range in parentheses.
Routine radiographic evaluation included AP pelvic and lateral crosstable images of the proximal femur. All radiographs were acquired in a standardized manner [43] with the patient in the supine position and the legs 15° internally rotated to compensate for femoral antetorsion. Supine films were used to allow comparison with intraoperative and early postoperative (nonweightbearing) films. The film-focus distance was 120 cm with the central beam directed to the midpoint between a line connecting both anterosuperior iliac spines and the superior border of the symphysis. The crosstable view was performed with the patient supine, the xray beam angled in a 45° angle, and centered to the inguinal fold. Improvement in morphology of the proximal femur was assessed by one of us not involved in the surgical care of the patients (CEA) and the following parameters evaluated pre- and postoperatively: trochanteric height [41], alpha angle in the AP and axial views [30], and neck-shaft angle (centrum-collum-diaphyseal [CCD] angle; Table 3). For the assessment of trochanteric height according to Stulberg et al. [41], the femoral head was divided into four horizontal quadrants on the AP pelvis radiograph. Trochanteric height was defined by the projection of the tip of the greater trochanter to the corresponding quadrant. Quadrant 1 represented the most inferior quarter of the femoral head and quadrant 4 the most superior quarter. An imaginary fifth quadrant was added if the tip of the greater trochanter was located superiorly to the femoral head. Normal trochanteric height was defined as the tip of the greater trochanter projected caudally to the center of the femoral head center (trochanteric height less than or equal to quadrant 2, according to Stulberg et al. [41]).
Table 3.
Preoperative and postoperative radiographic results of all hips (N = 41)
| Parameter | Preoperative | Postoperative | p value |
|---|---|---|---|
| Normal trochanteric height (% of hips ≤ quadrant 2) [41] | 5 | 80 | < 0.001 |
| Trochanteric height (%) [41] | |||
| Quadrant 1 | 5 | 12 | < 0.001 |
| Quadrant 2 | 0 | 68 | |
| Quadrant 3 | 15 | 17 | |
| Quadrant 4 | 51 | 3 | |
| Quadrant 5 | 29 | 0 | |
| Alpha angle on AP radiograph (° ± SD; range) [30] | 75 ± 18 (38–114) | 50 ± 12 (39–90) | < 0.001 |
| Alpha angle on axial radiograph (° ± SD; range) [30] | 77 ± 18 (45–109) | 42 ± 10 (27–90) | < 0.001 |
| CCD angle (° ± SD; range) | 127 ± 7 (106–137) | 129 ± 6 (116–140) | 0.179 |
| LCEA (° ± SD; range) [46] | 27 ± 6 (14–37) | 27 ± 7 (15–47) | 0.537 |
| OA grade according to Tönnis (%) [45]* | |||
| Grade 0 | 59 | 43 | 0.013 |
| Grade 1 | 41 | 40 | |
| Grade 2 | – | 14 | |
| Grade 3 | – | 3 | |
* OA evaluated at most recent followup (n = 35); CCD angle = centrum-collum-diaphyseal angle; LCEA = lateral center-edge angle; OA = osteoarthrosis.
Complications were classified according to the adapted Clavien-Dindo classification proposed by Sink et al. [8, 9, 39, 40]. It has been validated specifically for hip-preserving surgery [39]. The grading ranges from Grade I to V depending on the treatment required to manage complications and the associated long-term morbidity. Grade I complications require no treatment and there is no deviation from the routine postoperative followup (eg, asymptomatic heterotopic ossification). Grade II complications require no surgical treatment but there is deviation of the postoperative followup (eg, nerve palsy that requires bracing). Grade III complications require treatment but no long-term morbidity exists (eg, trochanteric nonunion requiring refixation). Grade IV complications require treatment and have long-term morbidity (eg, permanent nerve injury or pulmonary embolism). Grade V comprises death. As a result of the retrospective nature of the study, only complications greater than Grade 1 were included. Subsequent surgeries (eg, additional surgery to improve acetabular coverage) were summarized and distinguished from complications.
To assess progression of OA, the AP pelvic radiographs were reviewed by one of us not involved in the surgical care of the patients (CEA) preoperatively and at most recent followup and the affected hip was graded according to Tönnis for OA [44]. AP pelvic radiographs for evaluation of OA were available in 34 patients (35 hips) at the most recent followup (minimum 5-year followup; Fig. 1). Hips that converted to a THA were summarized and the date of conversion noted.
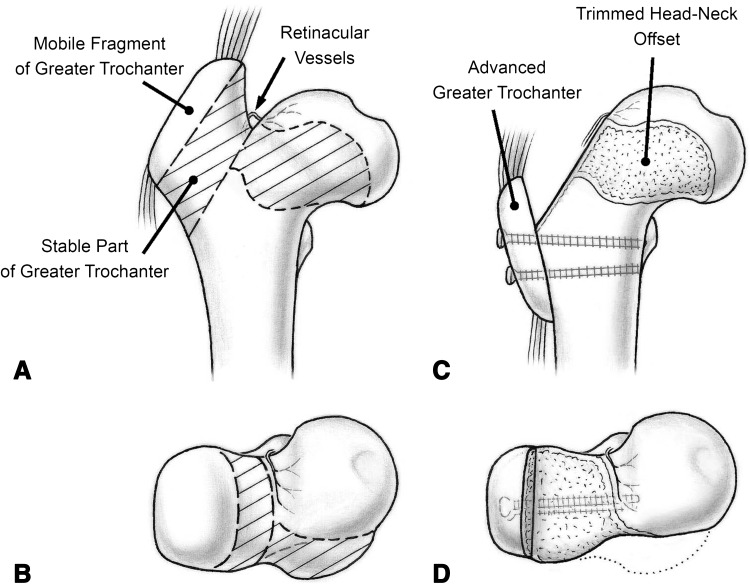
Relative femoral neck lengthening was performed according to the technique described by Ganz et al. [14]. The procedure included surgical dislocation of the hip [17], development of the extended retinacular soft tissue flap [16], and correction of intra- and extraarticular impingement (see Appendix 1 for a detailed description of the surgical procedure [Supplemental materials are available with the online version of CORR®.]). In brief, a flat trigastric osteotomy of the greater trochanter was performed to surgically dislocate the hip [17]. An extended retinacular soft tissue flap was developed by subperiosteal resection of the stable part of the greater trochanter (Fig. 2) [16]. Care was taken not to penetrate the periosteum and violate the nutrient vessels of the femoral head (medial circumflex femoral artery). The stable part of the greater trochanter was reduced to the level of the femoral neck (Fig. 2). To improve offset of the anterior aspect of the femoral neck, an osteochondroplasty was performed (Fig. 2). The mobile fragment of the greater trochanter was reattached to the proximal femur in a distalized position to optimize abductor muscle function (Fig. 2). Relative femoral neck lengthening with femoral neck osteochondroplasty and distalization of the greater trochanter was performed in all patients included in this study.
Fig. 2A–D.
(A) Complex proximal femoral deformities typically have a high-riding trochanter, a short neck with varus configuration, and (B) an asphericity in the AP direction, resulting in decreased offset. Relative femoral neck lengthening (C) comprised the following steps: a flat trochanteric osteotomy, reduction of the stable part of the greater trochanter, (D) osteochondroplasty of the femoral head-neck area to improve offset, and advancement of the trochanteric fragment. Reprinted with kind permission from Wichtig Publishing: Tannast M, Macintyre N, Steppacher SD, Hosalkar HS, Ganz R, Siebenrock KA. A systematic approach to analyse the sequelae of LCPD. Hip Int. 2013;23(Suppl 9):61–70; Fig. 11.
During the hospital stay (median, 9 days; range, 6–13 days), patients were kept on continuous passive motion for 30 minutes three times per day to prevent capsular adhesions. Patients were mobilized using crutches with partial weightbearing of 15 kg and restricted forced abduction and adduction to protect the trochanteric osteotomy. Full weightbearing and abductor training were initiated after 8 weeks and confirmed radiographic healing of the trochanteric osteotomy. Patients undergoing additional distalization of the lesser trochanter also had restricted active flexion. Patients were asked to return to our clinic for clinical and radiographic evaluation at 8 weeks, 3 months, 1 year, 2 years, and 5 years.
Normal distribution of continuous data was tested using the Kolmogorov-Smirnov test. The t-test was used to compare continuous clinical and radiographic data pre- and postoperatively. The Wilcoxcon rank sum test was used to compare ordinal data (Merle d’Aubigné-Postel score, trochanteric height, Tönnis score) pre- and postoperatively. Binominal data were compared using the McNemar test. Statistical analysis was performed using WinStat® (R. Fitch Software, Bad Krozingen, Germany).
Results
The proportion of a positive anterior impingement test decreased from preoperative to most recent followup from 93% (38 of 41 hips) to 49% (17 of 35 hips) and for limp from 76% (31 of 41 hips) to 9% (three of 35 hips) (p = 0.002 and p < 0.001, respectively; Table 2). The proportion of hips with a maximum abduction force M5 improved from 17% (seven of 41 hips) preoperatively to 91% (32 of 35 hips) at most recent followup (p < 0.001; Table 2). We found an increase in mean internal rotation (18° ± 15°; 95% confidence interval [CI], 13°–23° to 25° ± 15°; 20°–31°; p = 0.045), external rotation (25° ± 12° [21°–29°] to 32° ± 14° [27°–37°]; p = 0.013), and abduction (24° ± 10° [21°–28°] to 37° ± 13° [32°–43°]; p = 0.004; Table 2). No differences existed for flexion (94° ± 14°; 95% CI, 90°–98° to 93° ± 16°; 87°–98°; p = 0.466), extension (4° ± 6° [2°–5°] to 7° ± 7° [4°–9°]; p = 0.121), and adduction (18° ± 11° [14°–22°] to 13° ± 5° [11°–16°]; p = 0.176; Table 2). The mean Merle d’Aubigné-Postel score improved from 14 ± 1.7 (range, 9–17) to 17 ± 1.5 (13–18) at most recent followup (p < 0.001). This was the result of an improvement in the pain subscore from 4 ± 1.1 (range, 1–5) preoperatively to 5 ± 0.8 (range, 3–6) at followup (p < 0.001) and an improvement of the walking ability subscore from 5 ± 0.9 (2–6) preoperatively to 6 ± 0.6 (3–6) at followup (p < 0.001; Table 2).
The proportion of patients with normal trochanteric height increased from preoperatively 5% (two of 41 hips) to 80% (33 of 41 hips) postoperatively (p < 0.001; Table 3). The alpha angle on the AP radiograph improved from 75° ± 18° (95% CI, 70°–81°) to 50° ± 12° (47°–54°) postoperatively (p < 0.001) and the alpha angle on the axial view improved from 77° ± 18° (70°–84°0 to 42° ± 10° (39°–46°) (p < 0.001; Table 3).
Four hips (10%) had postoperative complications (Table 4). All complications were classified as Grade III complications [39, 40] and included two revisions of the greater trochanter for loss of fixation or nonunion and two hips with intraarticular adhesions (Table 4). Two hips underwent subsequent surgeries as a result of lack of sufficient femoral head containment (Table 4). These included one varus intertrochanteric osteotomy (IO) and one combined triple osteotomy with valgus IO (Table 4).
Table 4.
Repeat surgeries and complications of the patient series
| Patient | Description | Interval since surgery (years) | Grade | Treatment |
|---|---|---|---|---|
| Subsequent surgeries | ||||
| 1 | Lack of containment | 0.2 | NA | Varus-extension intertrochanteric osteotomy |
| 2 | Lack of containment | 0.5 | NA | Triple osteotomy with valgus intertrochanteric osteotomy |
| Complications | ||||
| 1 | Loss of trochanteric fixation | 0.2 | III | Revision fixation |
| 2 | Trochanteric nonunion | 1.2 | III | Revision fixation |
| 3 | Intraarticular adhesions | 0.4 | III | Closed manipulation |
| 4 | Intraarticular adhesions | 0.5 | III | Open capsulectomy |
Of the 35 hips with a preserved hip at most recent followup, 14 hips (40%) showed progression of OA by at least one grade according to Tönnis. Four of 40 hips (10%) were converted to a THA at a median of 5 years (range, 4–6 years) after relative femoral neck lengthening. All hips with conversion to THA had Grade 1 OA preoperatively (according to Tönnis), and THA was performed as a result of OA progression in all four cases.
Discussion
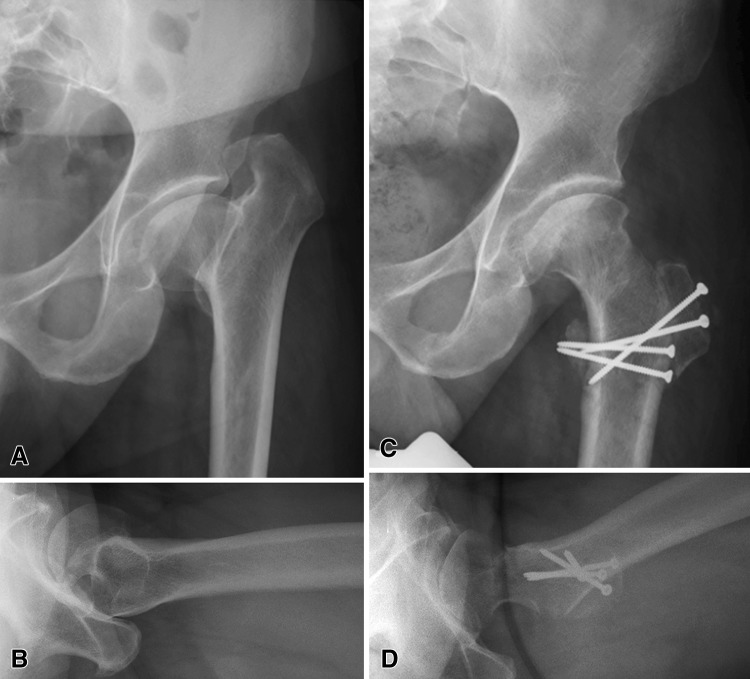
Complex proximal femoral deformities after LCPD may present with combined intra- and extraarticular FAI and resultant hip pain and limited function. Surgical dislocation of the hip [14] combined with the extended retinacular soft tissue flap [16] has expanded treatment options for patients with proximal femoral deformities (Fig. 3). Relative neck lengthening allows simultaneous correction of intra- and extraarticular impingement but little information on mid-term results of the procedure exists. Therefore, we asked if patients with a complex deformity of the proximal femur undergoing relative neck lengthening showed (1) improved hip pain and function; (2) improved radiographic parameters of the proximal femur; (3) significant complications requiring subsequent surgeries; and (4) progression of OA or conversion to THA at a minimum 5-year followup.
Fig. 3A–D.
(A) A 35-year-old male patient with sequelae of LCPD of the left hip is shown. His hip typically showed a high-riding trochanter, a short neck with varus configuration, and (B) a mushroom-shaped head with an asphericity in the AP direction. After relative femoral neck lengthening (C), the superior and (D) anterior offset was corrected and the greater trochanter refixated in an advanced position to improve the lever arm of the abductor muscles.
Our study has several limitations. First, we did not have a control group of patients with complex deformities of the proximal femur who did not undergo surgical treatment. We cannot, therefore, state whether one of the most significant clinical outcomes (progression of OA) was altered with surgery compared with no surgical intervention. Although 40% of study patients showed an increase in OA grade, all patients showed equivalent or improved clinical outcome scores at most recent followup compared with their preoperative status. Second, as a result of the retrospective design of our study, the only clinical scoring system available preoperatively was the Merle d’Aubigné-Postel score [28]. Despite the limited applicability of this relatively insensitive score, improvements in the mean Merle d’Aubigné-Postel score and the two subscores (pain, walking ability) were found. Next, inter- and intraobserver variability could have biased the results. Different observers assessed the clinical outcomes throughout the preoperative and followup visits, resulting in potential assessment bias. However, substantial interobserver agreement has been found for these clinical parameters [7, 12, 22, 24, 33, 34]. In contrast, a single observer evaluated the radiographic outcome. Nonetheless, intraobserver variability could also have biased outcome. No results for intraobserver agreement of the trochanteric height have been reported in the literature. However, substantial intraobserver agreement has been reported for the alpha and CCD angle [5, 19, 25, 29]. Therefore, we believe this did not jeopardize our conclusions. Finally, our patient population was very heterogeneous, including pediatric and adult patients, patients with prior surgery of the pelvis and/or the femur, and patients with a variety of etiologies.
We believe that the improvement in pain and function may be related to the correction of intra- and extraarticular impingement in these hips with complex femoral deformity, but future controlled studies will need to confirm these findings. The mean Merle d’Aubigné Postel score improved from 14 to 17 (Table 2), which is comparable to an increase from 14 to 16 found in hips with intra-/extraarticular impingement resulting from LCPD after surgical hip dislocation and/or pelvic osteotomy [1]. The mean Harris hip score of 83 and WOMAC score of 6 at most recent followup (Table 2) were comparable to the reported results in the literature for hips with complex femoral deformities and relative femoral neck lengthening (mean Harris hip score of 87 [2] and WOMAC score 3.5 [35]). In contrast, hips with LCPD after isolated intertrochanteric osteotomy without correction of intraarticular impingement or advancement of the greater trochanter showed a lower mean Harris hip score of 78.5 [31]. Abductor strength in hips with a proximal femoral deformity is often impaired as a result of the shortened femoral neck, high-riding greater trochanter, and varus hip morphology, which result in a decreased lever arm for the abductor muscles [32]. In the current study, the proportion of hips with normal abductor strength (M5) increased from 17% to 91% after relative neck lengthening and distalization of the greater trochanter (Table 2). In contrast, no hip after LCPD and isolated intertrochanteric osteotomy showed normal abductor strength (M5) at a mean followup of 11 years [21]. The proportion of patients with limp decreased from 76% to 9% in the current study, which is comparable to the reported proportion of 4% [2] or 18% [1] at last followup after relative neck lengthening. The proportion of hips with a positive anterior impingement test decreased from 93% to 49% in the current study (Table 2). Results in the literature for the anterior impingement test at last followup after surgical treatment of LCPD differ remarkably with a proportion ranging from 0% [10] to 59% [1]. Improvement for ROM was found for internal and external rotation and abduction (Table 2). Although abduction showed a mean improvement of 13°, both internal and external rotation only improved by 7°. In hips with intra-/extraarticular impingement resulting from LCPD after surgical hip dislocation [1], all amplitudes of ROM improved except flexion. However, the mean improvements were minor and ranged from 2° to 7°, which likely could be caused by different observers evaluating ROM [1].
Radiographic parameters of the proximal femur assessed in our study improved in the majority of hips after relative femoral neck lengthening (Table 3). The improvement of abduction force (Table 2) is likely the result of improved trochanteric height resulting in improvement of the abductor lever arm (Table 3). The proportion of hips with a normal trochanteric height (≤ quadrant 2 according to Stulberg et al. [41]) improved from 5% preoperatively to 80% postoperatively. Improvement of trochanteric height has been reported for both relative femoral neck lengthening [2, 37] and isolated advancement of the greater trochanter [21]. For relative neck lengthening, the mean trochanteric height improved from preoperatively a mean of 4.1 to postoperatively 2.9 in the trochanteric quadrant [37] according to Stulberg et al. [41] or the proportion of a normal trochanteric height (≤ quadrant 2 according to Stulberg et al. [41]) increased from 0% to 29% [2]. The offset angle improved on both the AP and axial views (Table 3). In the literature about relative femoral neck lengthening, the alpha angle has not been quantified [2, 10, 37]. In hips with isolated advancement of the greater trochanter, the offset is not affected. As expected, there were no changes for the CCD angle (Table 3) because the relative femoral neck lengthening includes no true cervical or intertrochanteric osteotomies.
Four patients (four hips) underwent revision surgery for complications (all Grade III according to the adapted Clavien-Dindo classification system [39, 40]; Table 4). The procedures ranged from manipulation under anesthesia to revision fixation of the greater trochanter. There were no complications with long-term morbidity. Specifically, there was no avascular necrosis of the femoral head. The two patients (two hips [5%]) with revision surgery resulting from intraarticular adhesions had no risk factors such as additional surgical procedures compared with hips without adhesions. Two patient (two hips [5%]) required revision fixation of the greater trochanter for loss of fixation or nonunion. The rates for trochanteric nonunion after surgical hip dislocation in the literature range from 4% to 23% [11, 36]. The lowest rate for trochanteric nonunions was found in hips with a stepped trochanteric osteotomy [3]. A stepped osteotomy is technically not possible in relative femoral neck lengthening as a result of the advancement of the greater trochanter. Despite this disadvantage and the decreased contact area between the reduced stable part of the greater trochanter and the trochanteric fragment, the rate of trochanteric nonunions in our study was comparable to that reported in the literature [11, 36]. Two patients (two hips) had subsequent surgery for unexpected lack of containment of the femoral head (Table 4). One patient with relative neck lengthening and concomitant head reduction osteotomy had a varus IO 6 weeks after the index procedure. The second patient with isolated relative neck lengthening underwent a triple osteotomy and valgus IO 6 months after surgery. Progression of OA could not be prevented; 14 of 35 (40%) showed progression at most recent followup and four of 40 hips (10%) converted to a THA. Comparison of our results with the literature on the natural course of OA is difficult because of the heterogeneity in patient series. Stulberg et al. [41] described the natural history of OA in hips with LCPD and found that the progression of OA depended on femoral head sphericity and joint congruency (Stulberg classification). Hips with Grade V (flat femoral head with normal acetabulum) showed rapid development of OA and hips with Class III and IV (non-spherical to flat femoral head with abnormalities of the acetabulum) developed mild to moderate OA. Although there were no hips with Grade V in our study, 95% of all hips presented with Grade III or IV preoperatively. Additionally, all patients included in our investigation were symptomatic with impaired function, which has been shown to be associated with a worse prognosis for progression of OA [6, 26]. The current results of OA progression and conversion to THA is comparable to reports in the literature for femoral neck lengthening with OA progression in 36% of the hips after a mean followup of 3.75 years [2] or a rate of conversion to THA of 7% [2] and 10% [37] at 3.75- and 3-year followup, respectively.
In summary, we show that relative femoral neck lengthening in hips with complex proximal femoral deformities results in reduced pain, improved function, and greater abductor strength for a majority of patients. We believe that the improvement in abduction force may be related to the improvement of the trochanteric height and the resulting abductor lever arm. In addition, we believe that the reduction of pain is the result of simultaneous correction of intra- and extraarticular impingement. All subsequent surgeries were performed as a result of unexpected lack of femoral containment. Complications in our study subjects were the result of loss of trochanteric fixation and intraarticular adhesions. The frequency of trochanteric nonunion was comparable or less than the reported frequency in hips after surgical hip dislocation [11, 36]. Most importantly, there were no long-term complications (> Grade 3 according to the Clavien-Dindo classification system [39, 40]) and no occurrences of avascular necrosis of the femoral head; however, progression of OA could not be prevented and and four hips (10%) that underwent conversion to THA in this series. Future research topics should therefore include the determination of factors predicting a poor outcome, in particular progression of OA.
Electronic supplementary material
Footnotes
One of the authors (SDS) has received funding from the Deutsche Arthrose-Hilfe e.V. One author (MT) has received funding from the Swiss National Science Foundation (SNSF).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Albers CE, Steppacher SD, Ganz R, Siebenrock KA, Tannast M. Joint-preserving surgery improves pain, range of motion, and abductor strength after Legg-Calve-Perthes disease. Clin Orthop Relat Res. 2012;470:2450–2461. doi: 10.1007/s11999-012-2345-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson LA, Erickson JA, Severson EP, Peters CL. Sequelae of Perthes disease: treatment with surgical hip dislocation and relative femoral neck lengthening. J Pediatr Orthop. 2010;30:758–766. doi: 10.1097/BPO.0b013e3181fcbaaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bastian JD, Wolf AT, Wyss TF, Notzli HP. Stepped osteotomy of the trochanter for stable, anatomic refixation. Clin Orthop Relat Res. 2009;467:732–738. doi: 10.1007/s11999-008-0649-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Carlisle JC, Zebala LP, Shia DS, Hunt D, Morgan PM, Prather H, Wright RW, Steger-May K, Clohisy JC. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–58. [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng JC, Lam TP, Ng BK. Prognosis and prognostic factors of Legg-Calve-Perthes disease. J Pediatr Orthop. 2011;31:147–151. doi: 10.1097/BPO.0b013e318223b470. [DOI] [PubMed] [Google Scholar]
- 7.Cibere J, Thorne A, Bellamy N, Greidanus N, Chalmers A, Mahomed N, Shojania K, Kopec J, Esdaile JM. Reliability of the hip examination in osteoarthritis: effect of standardization. Arthritis Rheum. 2008;59:373–381. doi: 10.1002/art.23310. [DOI] [PubMed] [Google Scholar]
- 8.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 9.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eijer H, Podeszwa DA, Ganz R, Leunig M. Evaluation and treatment of young adults with femoro-acetabular impingement secondary to Perthes’ disease. Hip Int. 2006;16:273–280. doi: 10.1177/112070000601600406. [DOI] [PubMed] [Google Scholar]
- 11.English TA. The trochanteric approach to the hip for prosthetic replacement. J Bone Joint Surg Am. 1975;57:1128–1133. [PubMed] [Google Scholar]
- 12.Florence JM, Pandya S, King WM, Robison JD, Baty J, Miller JP, Schierbecker J, Signore LC. Intrarater reliability of manual muscle test (Medical Research Council scale) grades in Duchenne’s muscular dystrophy. Phys Ther. 1992;72:115–122. doi: 10.1093/ptj/72.2.115. [DOI] [PubMed] [Google Scholar]
- 13.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 14.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 15.Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular osteotomies in complex hip deformities. Clin Orthop Relat Res. 2010;468:3168–3180. doi: 10.1007/s11999-010-1489-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ganz R, Huff TW, Leunig M. Extended retinacular soft-tissue flap for intra-articular hip surgery: surgical technique, indications, and results of application. Instr Course Lect. 2009;58:241–255. [PubMed] [Google Scholar]
- 17.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 18.Ganz R, Slongo T, Turchetto L, Masse A, Whitehead D, Leunig M. The lesser trochanter as a cause of hip impingement: pathophysiology and treatment options. Hip Int. 2013;23:35–41. doi: 10.5301/hipint.5000063. [DOI] [PubMed] [Google Scholar]
- 19.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49:436–441. doi: 10.1080/02841850801935567. [DOI] [PubMed] [Google Scholar]
- 20.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 21.Joo SY, Lee KS, Koh IH, Park HW, Kim HW. Trochanteric advancement in patients with Legg-Calve-Perthes disease does not improve pain or limp. Clin Orthop Relat Res. 2008;466:927–934. doi: 10.1007/s11999-008-0128-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil. 2005;19:659–661. doi: 10.1191/0269215505cr869oa. [DOI] [PubMed] [Google Scholar]
- 23.Mamisch TC, Kim YJ, Richolt JA, Millis MB, Kordelle J. Femoral morphology due to impingement influences the range of motion in slipped capital femoral epiphysis. Clin Orthop Relat Res. 2009;467:692–698. doi: 10.1007/s11999-008-0477-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin RL, Sekiya JK. The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J Orthop Sports Phys Ther. 2008;38:71–77. doi: 10.2519/jospt.2008.2677. [DOI] [PubMed] [Google Scholar]
- 25.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. doi: 10.1007/s11999-010-1447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McAndrew MP, Weinstein SL. A long-term follow-up of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1984;66:860–869. doi: 10.2106/00004623-198466060-00006. [DOI] [PubMed] [Google Scholar]
- 27.Medical Resarch Council. Aids to the Investigation of Peripheral Nerve Injuries. London, UK: HMSO: War Memorandum No. 7 (revised 2nd edition); 1943.
- 28.Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prostesis. J Bone Joint Surg. 1954;36:451–475. [PubMed]
- 29.Nelitz M, Guenther KP, Gunkel S, Puhl W. Reliability of radiological measurements in the assessment of hip dysplasia in adults. Br J Radiol. 1999;72:331–334. doi: 10.1259/bjr.72.856.10474491. [DOI] [PubMed] [Google Scholar]
- 30.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 31.Pecasse GA, Eijer H, Haverkamp D, Marti RK. Intertrochanteric osteotomy in young adults for sequelae of Legg-Calve-Perthes’ disease—a long term follow-up. Int Orthop. 2004;28:44–47. doi: 10.1007/s00264-003-0513-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Plasschaert VF, Horemans HL, de Boer LM, Harlaar J, Diepstraten AF, Roebroeck ME. Hip abductor function in adults treated for Perthes disease. J Pediatr Orthop B. 2006;15:183–189. doi: 10.1097/01.bpb.0000186645.76697.7a. [DOI] [PubMed] [Google Scholar]
- 33.Prather H, Harris-Hayes M, Hunt DM, Steger-May K, Mathew V, Clohisy JC. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM & R. 2010;2:888–895. doi: 10.1016/j.pmrj.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ratzlaff C, Simatovic J, Wong H, Li L, Ezzat A, Langford D, Esdaile JM, Kennedy C, Embley P, Caves D, Hopkins T, Cibere J. Reliability of hip examination tests for femoroacetabular impingement (FAI) Arthritis Care Res. 2013;65:1690–1696. doi: 10.1002/acr.22036. [DOI] [PubMed] [Google Scholar]
- 35.Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop Relat Res. 1958;11:111–119. [PubMed] [Google Scholar]
- 36.Schneeberger AG, Murphy SB, Ganz R. [The trochanteric flip osteotomy] [in German] Oper Orthop Traumatol. 1997;9:1–15. doi: 10.1007/s00064-006-0001-0. [DOI] [PubMed] [Google Scholar]
- 37.Shore BJ, Novais EN, Millis MB, Kim YJ. Low early failure rates using a surgical dislocation approach in healed Legg-Calve-Perthes disease. Clin Orthop Relat Res. 2011;470:2441–2449. doi: 10.1007/s11999-011-2187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Siebenrock KA, Steppacher SD, Haefeli PC, Schwab JM, Tannast M. Valgus hip with high antetorsion causes pain through posterior extraarticular FAI. Clin Orthop Relat Res. 2013;471:3774–3780. doi: 10.1007/s11999-013-2895-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sink EL, Beaule PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011;93:1132–1136. doi: 10.2106/JBJS.J.00794. [DOI] [PubMed] [Google Scholar]
- 40.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470:2220–2226. doi: 10.1007/s11999-012-2343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 42.Tannast M, Hanke M, Ecker TM, Murphy SB, Albers CE, Puls M. LCPD: reduced range of motion resulting from extra- and intraarticular impingement. Clin Orthop Relat Res. 2012;470:2431–2440. doi: 10.1007/s11999-012-2344-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 44.Tönnis D. Gerneral radiography of the hip joint. In: Tönnis D, editor. Congenital Dysplasia, Dislocation of the Hip. New York, NY, USA: Springer; 1987. pp. 100–142. [Google Scholar]
- 45.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83:7–38. [Google Scholar]
- 47.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.