Abstract
Background
We previously reported the 5-year followup of hips with femoroacetabular impingement (FAI) that underwent surgical hip dislocation with trimming of the head-neck junction and/or acetabulum including reattachment of the labrum. The goal of this study was to report a concise followup of these patients at a minimum 10 years.
Questions/purposes
We asked if these patients had (1) improved hip pain and function; we then determined (2) the 10-year survival rate and (3) calculated factors predicting failure.
Methods
Between July 2001 and March 2003, we performed surgical hip dislocation and femoral neck osteoplasty and/or acetabular rim trimming with labral reattachment in 75 patients (97 hips). Of those, 72 patients (93 hips [96%]) were available for followup at a minimum of 10 years (mean, 11 years; range, 10–13 years). We used the anterior impingement test to assess pain and the Merle d’Aubigné-Postel score to assess function. Survivorship calculation was performed using the method of Kaplan and Meier and any of the following factors as a definition of failure: conversion to total hip arthroplasty (THA), radiographic evidence of worsening osteoarthritis (OA), or a Merle d’Aubigné-Postel score less than 15. Predictive factors for any of these failures were calculated using the Cox regression analysis.
Results
At 10-year followup, the prevalence of a positive impingement test decreased from preoperative 95% to 38% (p < 0.001) and the Merle d’Aubigné-Postel score increased from preoperative 15.3 ± 1.4 (range, 9–17) to 16.9 ± 1.3 (12–18; p < 0.001). Survivorship of these procedures for any of the defined failures was 80% (95% confidence interval, 72%–88%). The strongest predictors of failure were age > 40 years (hazard ratio with 95% confidence interval, 5.9 [4.8–7.1], p = 0.002), body mass index > 30 kg/m2 (5.5 [3.9–7.2], p = 0.041), a lateral center-edge angle < 22° or > 32° (5.4 [4.2–6.6], p = 0.006), and a posterior acetabular coverage < 34% (4.8 [3.7–5.6], p = 0.006).
Conclusions
At 10-year followup, 80% of patients with FAI treated with surgical hip dislocation, osteoplasty, and labral reattachment had not progressed to THA, developed worsening OA, or had a Merle d’Aubigné-Postel score of less than 15. Radiographic predictors for failure were related to over- and undertreatment of acetabular rim trimming.
Level of Evidence
Level IV, therapeutic study.
Introduction
Surgical hip dislocation with trimming of the head-neck junction and/or acetabulum including reattachment of the labrum is an attractive option for the surgical treatment of patients with femoroacetabular impingement (FAI). We previously reported a good to excellent clinical result, no progression of osteoarthritis (OA), and no need for conversion to a THA in over 90% of patients so treated at a minimum 5-year followup (mean, 6 years; range, 5–7 years) [35]. These procedures were performed between July 2001 and March 2003 in 75 patients (97 hips) without prior surgery or Legg-Calvé-Perthes disease. Excessive acetabular rim trimming, OA, and increased age or weight were associated with conversion to THA, progression of OA, or a Merle d’Aubigné-Postel score less than 15 at 5-year followup. To our knowledge, no minimum 10-year followup exists for hips after surgical hip dislocation for the surgical treatment of FAI.
The goal of this study was to report a concise followup at 10 years of the same patient series to evaluate clinical results and the survival rate of surgery and to test for new factors predicting failure. We therefore asked if patients undergoing surgical hip dislocation with trimming of the head-neck junction and/or acetabulum including reattachment of the labrum had (1) improved hip pain and function at 10-year followup. We then (2) determined the 10-year survival rate using the endpoints defined as the need for conversion to THA, progression of OA, and a Merle d’Aubigné-Postel score less than 15 and (3) calculated factors predicting these endpoints at a minimum of 10 years of followup.
Patients and Methods
We retrospectively reviewed the same subset of 75 patients (97 hips) on whom we previously reported with a minimum 5-year followup after surgical hip dislocation for the treatment of idiopathic FAI [35]. Surgeries were performed between July 2001, when routine reattachment of the labrum was introduced, and March 2003. Of the total of 146 procedures (121 patients) for this period of time, we excluded 35 patients (37 hips) with FAI after previous surgery including femoral and/or pelvic osteotomies (26 hips), open reduction and internal fixation of the femur and/or acetabulum (six hips), and in situ pinning after slipped capital femoral epiphysis (five hips). In addition, we excluded 11 patients (12 hips) with Legg-Calvé-Perthes disease eventually resulting in the subset of 75 patients (97 hips) with idiopathic FAI (Table 1). These patients underwent surgical hip dislocation performed according to the technique described by Ganz et al. [11] with resection of a cam lesion and/or acetabular rim trimming including labral reattachment. Three patients (four hips [4%]) were lost to followup between 5 and 10 years. One patient (one hip) died 8 years postoperatively from a cause unrelated to surgery. The other two patients (three hips) were lost to followup between 5 and 6 years after surgery without undergoing conversion to THA or progression of OA. These patients presented with a good clinical result (Merle d’Aubigné-Postel score of 17 for all hips) at the most recent followup. The average followup of the remaining 72 patients (93 hips) was 11 years (range, 10–13 years). Of these, we had complete clinical and radiographic followup at a minimum of 10 years in 67 patients (88 hips). Five patients (five hips) refused radiographic followup as a result of radiation exposure. Of these, we had clinical followup including the clinical scores at a minimum of 10 years with latest radiographic followup between 5 and 7 years postoperatively.
Table 1.
Demographic and intraoperative data of the patient series
| Parameters | Value |
|---|---|
| Number of patients (hips) | 75 (97) |
| Age (years)* | 32 ± 8 (15–52) |
| Sex (percentage male of all hips) | 57 |
| Side (percentage right of all hips) | 58 |
| Height (cm)* | 175 ± 11 (152–204) |
| Weight (kg)* | 79 ± 17 (50–145) |
| Body mass index (kg/cm2)* | 25 ± 5 (18–43) |
| Type of femoroacetabular impingement | |
| Cam (percentage) | 4 |
| Pincer (percentage) | 11 |
| Mixed (percentage) | 85 |
* Mean ± SD (range).
The study was approved by the local institutional review board.
For the clinical and radiographic evaluation of the patients, the same assessment scheme from the previous report was used [35]. Clinical evaluation included the patient history, anterior impingement test (pain in combined flexion and internal rotation), and full goniometric ROM. Subsequent surgeries and complications were summarized and the complications were graded according to the adapted Dindo-Clavien complication classification system for orthopaedic surgery [9, 34]. Grade 1 complications were not included as a result of the retrospective nature of the study (Table 2). As a clinical scoring system, the Merle d’Aubigné-Postel score [25] was assessed preoperatively and at the 5- and 10-year followup. In addition, the WOMAC [4], Harris hip score (HHS) [12], the SF-12 physical and mental component scales [10, 41], and the UCLA activity score [43] were assessed at the 5- and 10-year followup. Radiographic evaluation consisted of an AP pelvic radiograph and a cross-table lateral view of the hip acquired in a standardized fashion [39]. Osteoarthritis was graded according to the classification of Tönnis [40].
Table 2.
Subsequent surgeries and complications graded according to the adapted Dindo-Clavien complication classification system for orthopaedic surgery [9, 34]
| Subsequent surgeries and complications | Value | Sink classification [9, 34] |
|---|---|---|
| Trochanteric screw removal (percentage) | 31 | – |
| THA (percentage) | 11 | – |
| Arthroscopic adhesiolysis (percentage) | 6 | 3 |
| Evacuation of wound hematoma (percentage) | 2 | 3 |
| Irrigation and débridement for subcutaneous wound infection (percentage) | 1 | 3 |
| Refixation of greater trochanter (percentage) | 2 | 3 |
| Arthroscopic acetabular rim trimming (percentage) | 1 | – |
| Revision of iliotibial band dehiscence (percentage) | 1 | 3 |
Different observers performed the clinical evaluation preoperatively, at 5-, and 10-year followup. To evaluate hip pain, the prevalence of a positive anterior impingement test was assessed. The anterior impingement test was considered positive if in 90° of hip flexion and combined internal rotation and adduction reproducible hip pain was triggered. Hip function was assessed including the full goniometric ROM and the Merle d’Aubigné-Postel score. Substantial inter- and intraobserver agreement has been reported for the anterior impingement test [22], ROM [13, 24, 42], and the Merle d’Aubigné-Postel score [18]. In addition for evaluation of hip function, the WOMAC, HHS, SF-12, and UCLA score were assessed at 5- and 10-year followup. We calculated survival rate at the 10-year followup and defined failure if any of the following occurred: conversion to THA, progression of OA by at least one grade according to the Tönnis classification [40], or a Merle d’Aubigné-Postel score [25] of less than 15 at most recent followup. The five patients (five hips) without a minimum 10-year radiographic followup were considered survivors because they did not show progression of OA on the latest radiographic followup (ranging from 5.2 to 7.2 years) and they presented with a good to excellent clinical result (HHS > 90) and high activity level (UCLA > 7) at a minimum 10-year followup. We calculated predictive factors for any of the previously defined endpoints by evaluating demographic data (Table 1), clinical data (Table 3), or OA. In addition, we evaluated the pre- and postoperative radiographic parameters from the AP pelvic radiograph or axial view for predictive factors including: the lateral center-edge angle (LCEA), acetabular index, extrusion index, ACM angle, crossover sign, retroversion index [32], posterior wall sign [32], ischial spine sign [16], alpha angle, and craniocaudal, anterior, and posterior acetabular coverage (calculated using computerized methods [38]). These radiographic parameters were evaluated by one of us not involved in the surgical care of the patients (SDS) and with previously defined ranges for normal, deficient, and excessive acetabular coverage [37].
Table 3.
Clinical results preoperatively and at 5- and 10-year followup
| Parameter (best-worst score possible) | Preoperative (n = 97) | 5-year followup (n = 90) | 10-year followup (n = 86) | p value global | p value preoperative versus 5-year* | p value preoperative versus 10-year* | p value 5- versus 10-year* |
|---|---|---|---|---|---|---|---|
| Merle d’Aubigné-Postel | |||||||
| Score [17] (18–0) | 15.3 ± 1.4 (9–17) | 17.2 ± 1.2 (12–18) | 16.9 ± 1.3 (12–18) | < 0.001 | < 0.001 | < 0.001 | 0.001 |
| Pain (6–0) | 3.8 ± 0.7 (2–5) | 5.3 ± 0.9 (2–6) | 5.2 ± 0.9 (3–6) | < 0.001 | < 0.001 | < 0.001 | 0.031 |
| Mobility (6–0) | 5.8 ± 0.5 (4–6) | 5.9 ± 0.2 (5–6) | 5.9 ± 0.4 (5–6) | 0.472 | – | – | – |
| Walking ability (6–0) | 5.7 ± 0.7 (2–6) | 5.9 ± 0.2 (5–6) | 5.9 ± 0.4 (4–6) | 0.264 | – | – | – |
| WOMAC [4] (0–100) | – | 8 ± 12 (0–52) | 6 ± 11 (0–59) | – | – | – | 0.053 |
| Pain (0–100) | 10 ± 14 (0–56) | 6 ± 11 (0–50) | 0.014 | ||||
| Stiffness (0–100) | 11 ± 14 (0–56) | 8 ± 13 (0–55) | 0.165 | ||||
| Function (0–100) | 7 ± 12 (0–58) | 6 ± 12 (0–63) | 0.110 | ||||
| Harris hip score [11] (100–0) | – | 92 ± 12 (48–100) | 92 ± 10 (44–100) | – | – | – | 0.842 |
| SF-12 [9, 33] | |||||||
| Physical component | 50 ± 8 (20–65) | 52 ± 7 (24–61) | < 0.001 | ||||
| Scale (100–0) | – | – | |||||
| Mental component | 54 ± 8 (21–67) | 52 ± 10 (20–63) | 0.375 | ||||
| Scale (100–0) | |||||||
| UCLA score [34] (10–0) | – | 7 ± 2 (2–10) | 8 ± 2 (2–10) | – | – | – | 0.166 |
| Anterior impingement test (percent positive) | 95 | 17 | 38 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| ROM | |||||||
| Flexion | 102 ± 11 (85–130) | 102 ± 9 (80–130) | 100 ± 10 (80–130) | 0.398 | – | – | – |
| Extension | 1 ± 4 (0–20) | 0 ± 2 (0–10) | 4 ± 3 (−10–10) | < 0.001 | 0.149 | 0.006 | < 0.001 |
| Internal rotation | 14 ± 10 (0–45) | 19 ± 8 (0–40) | 19 ± 11 (0–45) | < 0.001 | 0.003 | < 0.001 | 0.765 |
| External rotation | 29 ± 11 (5–60) | 30 ± 8 (10–45) | 31 ± 13 (5–60) | 0.697 | – | – | – |
| Abduction | 31 ± 10 (0–60) | 39 ± 6 (20–50) | 44 ± 11 (5–60) | < 0.001 | < 0.001 | < 0.001 | 0.004 |
| Adduction | 21 ± 8 (0–35) | 24 ± 7 (10–40) | 21 ± 7 (0–45) | 0.190 | – | – | – |
Values of continuous parameters are expressed as mean ± SD with range in parentheses; * the level of significance for pairwise comparison of the Merle d’Aubigné-Postel, prevalence of a positive anterior impingement, and ROM after Bonferroni correction was p = 0.05/3 = 0.017.
We tested normal distribution using the Kolmogorov-Smirnov test. We determined differences in hip pain and function among the preoperative and 5- and 10-year followup using repeated-measures analysis of variance for ROM and the Friedman test for the Merle d’Aubigné-Postel score. If differences existed, pairwise comparison was performed with the paired Student’ t-test for ROM and the Wilcoxon test for the Merle d’Aubigné-Postel score with Bonferroni correction. The frequency of positive anterior impingement tests was compared among preoperative and 5- and 10-year followup using the chi-square test. Clinical scores were compared between the 5- and 10-year followup using the paired Student’s t-test. Survival of surgery was calculated using the previously defined three endpoints and the method of Kaplan and Meier [17]. Predictive factors for failure were calculated using the univariate and multivariate Cox proportional model with corresponding hazard ratios and adjusted hazard ratios [8]. Hazard ratios were calculated with 95% confidence intervals (CIs).
Results
At the 10-year followup, hip pain was decreased and function remained improved in the majority of patients compared with the preoperative status (Table 3). The prevalence of a positive impingement test decreased from 95% preoperatively to 38% at 10-year followup (p < 0.001). The mean Merle d’Aubigné-Postel score increased from preoperatively 15.3 ± 1.4 (range, 9–17) to 16.9 ± 1.3 (range, 12–18; p < 0.001) at 10-year followup as a result of the Merle d’Aubigné-Postel pain subscore increasing from 3.8 ± 0.7 (range, 2–5) to 5.2 ± 0.9 (range, 3–6; p < 0.001). ROM increased (Table 3) for extension (mean at 10-year followup of 4° ± 3° [range, −10° to 10°]; p = 0.006), internal rotation (19° ± 11° [range, 0°–45°]; p < 0.001), and abduction (44° ± 11° [range, 5° to −60°]; p < 0.001) (Table 3). Compared with the 5-year evaluation, the following were decreased at 10 years: mean Merle d’Aubigné-Postel score (16.9 ± 1.3 [range, 12–18] versus 17.2 ± 1.2 [range, 12–18]; p = 0.001), and WOMAC pain subscore (6 ± 11 [range, 0–50] versus 10 ± 14 [range, 0–56]; p = 0.014) (Table 3). In contrast, an increased prevalence of a positive anterior impingement test (38% versus 17%; p < 0.001), physical component scale of the SF-12 (52 ± 7 [range, 24–61] versus 50 ± 8 [range, 20–65]; p < 0.001), extension (4 ± 3 [range, −10° to 10°] versus 0° ± 2° [range, 0°–10°]; p < 0.001), and abduction (44° ± 11° [range, 5°–60°] versus 39 ± 6 [range, 20°–50°]; p = 0.004) were found at 10- compared with 5-year followup (Table 3).
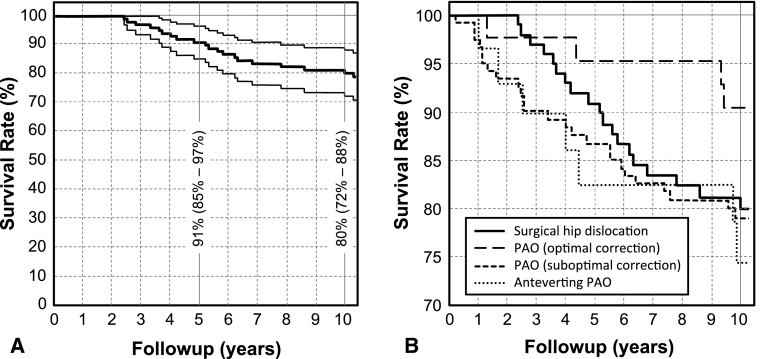
Twenty-two of 97 hips reached an endpoint of failure. Eleven hips were converted to a THA after a mean of 5 ± 2 years (range, 2–9 years). Eight hips showed progression of OA during the followup period. Three hips had a Merle d’Aubigné-Postel score of less than 15 at most recent followup. This resulted in a cumulative survivorship of 80% (95% CI, 72%–88%) at the 10-year followup (Fig. 1).
Fig. 1A–B.
(A) The Kaplan-Meier survivorship for hips after surgical hip dislocation with labral reattachment for the treatment of FAI is shown. Endpoints were defined as conversion to THA, progression of OA, and a Merle d’Aubigné-Postel score of less than 15. The cumulative survivorship at 10 years was 80% (95% CI, 72%–88%). (B) A comparable mean 10-year survivorship with the same endpoints was found for other hip-preserving surgeries including periacetabular osteotomy (PAO) (79% and 91% survival rate for PAO with optimal and suboptimal correction, respectively) [1] and anteverting PAO (74% survival rate) [33].
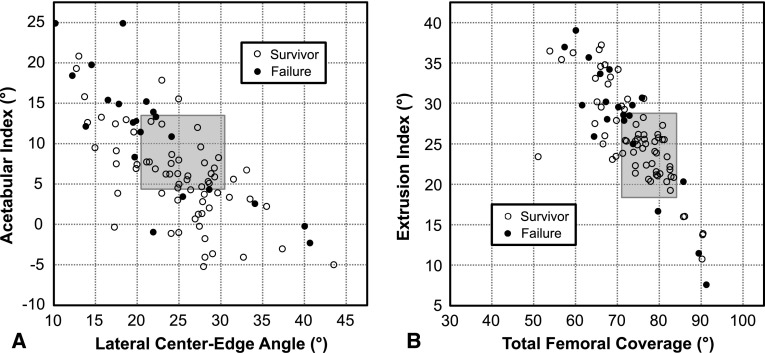
After controlling for potential confounding variables, our multivariate analysis identified age > 40 years (hazard ratio with 95% CI, 5.9 [4.8–7.1]; p = 0.002), a body mass index (BMI) > 30 kg/m2 (5.5 [3.9–7.1]; p = 0.041), a postoperative LCEA < 22° or > 32° (5.4 [4.2–6.6; p = 0.006]), or a postoperative posterior femoral coverage of < 34% (4.8 [3.7–5.9]) to be associated with a higher likelihood of failure (Table 4). In comparison to the predictors found at the 5–year followup, age > 40 years was repeatedly found to be a negative predictive factor. In contrast, an acetabular index > 14° or a total acetabular coverage < 72% were not identified as predictive factors at 10-year followup. The BMI, LCEA, and posterior femoral coverage were new predictive factors for failure not found at the 5-year followup in the multivariate analysis [35]. The LCEA was not only related to deficient acetabular coverage like the other predictive factors describing acetabular coverage (posterior femoral coverage or acetabular index and total femoral coverage from the 5-year followup), but also to excessive acetabular coverage (Fig. 2).
Table 4.
Predictive factors for failure with corresponding hazard ratios
| Category | Parameter | Hazard ratio† (95% confidence interval) | p value | Adjusted hazard ratioǂ (95% confidence interval) | p value |
|---|---|---|---|---|---|
| Demographic factors | Age > 40 years | 4.9 (4.0–5.8) | < 0.001 | 5.9 (4.8–7.1) | 0.002 |
| Weight > 100 kg | 4.6 (3.3–5.9) | 0.019 | |||
| Body mass index > 30 kg/m2 | 5.1 (3.6–6.6) | 0.033 | 5.5 (3.9–7.2) | 0.041 | |
| Preoperative radiographic factors | Anterior femoral coverage < 15%* | 4.3 (3.2–5.4) | < 0.001 | ||
| Osteoarthritis ≥ Tönnis Grade 1 | 6.2 (5.2–7.2) | < 0.001 | |||
| Postoperative factors related to surgical accuracy | LCEA < 22° or > 32°* | 5.4 (4.3–6.5) | 0.003 | 5.4 (4.2–6.6) | 0.006 |
| AI < 3° or > 13°* | 5.3 (3.7–6.9) | 0.037 | |||
| Extrusion index < 18% or > 28%* | 5.6 (4.5–6.7) | 0.002 | |||
| Total femoral coverage < 72% or > 83%* | 3.1 (2.1–4.1) | 0.029 | |||
| Anterior femoral coverage < 15%* | 3.7 (2.4–4.9) | 0.038 | |||
| Posterior femoral coverage < 34%* | 3.4 (2.4–4.3) | 0.011 | 4.8 (3.7–5.9) | 0.006 |
* Under- or overcoverage defined by Tannast et al. [37]; †univariate analysis; ǂmultivariate analysis; LCEA = lateral center-edge angle; AI = acetabular index.
Fig. 2A–B.
Scatterplots showing postoperative radiographic parameters describing acetabular morphology. The gray area represents the normal values for the radiographic parameters [37] and the white and black dots represent the surviving hips and failures at 10-year followup, respectively. Most failures had a dysplastic acetabular morphology with an (A) excessive acetabular index or (B) extrusion index and a deficient (A) LCEA or (B) total femoral coverage. At 10-year followup some hips failed with an acetabular morphology of persisting pincer type.
Discussion
Since the introduction of surgical hip dislocation [10], there has been increasing interest in the surgical treatment of FAI. Both open and arthroscopy treatment options have become widely accepted with generally promising short- and mid-term results [35]. To the best of our knowledge, no 10-year results for surgical treatment of FAI exist. The aim of the current study was to report the 10-year followup with clinical results, survival rate, and predictive factors for failure in patients undergoing surgical hip dislocation for symptomatic FAI with trimming of the head-neck junction and/or acetabulum including reattachment of the labrum. At the 10-year followup, we found decreased pain and improved function in a vast majority of these patients. There was a survival rate of surgery of 80% at 10-year followup using the endpoints defined as the need for conversion to THA, progression of OA, and a Merle d’Aubigné-Postel score less than 15. Predictive factors for these endpoints included an age > 40 years, a BMI > 30 kg/m2, a LCEA < 22° or > 32°, or a posterior femoral coverage of < 34%.
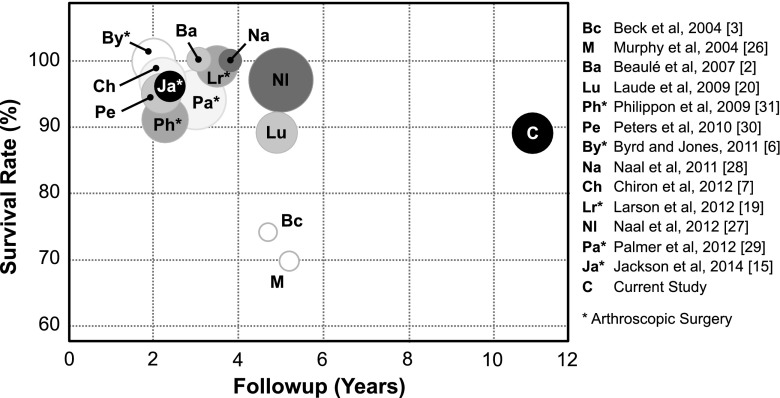
The limitations of the current study are similar to those from our previous report [35]. First, there is a lack of a control group with labral resection or untreated FAI. Therefore, the current results are compared with the literature on arthroscopic or open surgical treatment of FAI (Fig. 3). Second, the clinical data were assessed by different observers as a result of the retrospective design of the study and potentially biasing the results. However, substantial inter- and intraobserver agreement has been reported for those clinical parameters evaluated by different observers. Third, some clinical scores including the WOMAC, HHS, SF-12, and UCLA scores were only available at the 5- and 10-year followup. In addition, not all patients could be followed up for a minimum of 10 years. There were three patients with four hips, which were lost to followup and could have reached an endpoint because their last followup was between 5 and 6 years. An additional five patients (five hips) did not have radiographic followup at a minimum 10-year followup. These five patients (five hips) were not considered failures because they presented with good to excellent clinical results (HHS > 90) and a high activity level (UCLA > 7) making progression of OA unlikely.
Fig. 3.
Bubble chart shows followup, size of patient series (size of bubble), treatment (open or arthroscopic treatment [asterisk]), and survival rate with conversion to THA as the endpoint. In addition, the color represents the percentage of labral reattachment ranging from white for no reattachment to black for 100% of reattachment.
In a vast majority of patients hip pain and function were improved at the 10-year followup compared with the preoperative status (Table 3). A decreased prevalence of a positive anterior impingement test [6], improved hip pain [19, 29], or improved Merle d’Aubigné-Postel score [3, 26] at latest followup is consistent with the results in the literature regardless of the treatment of labral disease or open versus arthroscopic surgery. We found an improvement of internal rotation, abduction, and extension at the 10-year followup (Table 3). The internal rotation is typically decreased in patients with FAI and improvement after corrective surgery has been uniformly reported [5, 7, 21, 27]. However, improvements in abduction and extension after surgical correction in hips with FAI have not previously been reported in the literature (Table 3). Between the 5- and 10-year followup, some minor improvement in the WOMAC pain subscore and the physical component scale of the SF-12 were detected (Table 3). At latest followup, the results for the WOMAC [2, 14, 27], HHS [6, 15, 19, 21, 30, 31], SF-12 [2, 27, 28], and UCLA [2] scores were comparable to those found in the literature.
The survival rate of clinically good-functioning, nonarthritic hips decreased from 91% at 5-year to 80% at 10-year followup (Fig. 1). To our knowledge, no other long-term study for surgical treatment of FAI exists. Earlier results without or only partial labral reattachment [3, 20, 26] showed comparable survival rates at a considerably lower followup of 5 years (Fig. 3). Comparing our results with those of acetabular osteotomies for the treatment of hip dysplasia [1, 36] or acetabular retroversion [33], a comparable survival rate at 10-year followup ranging from 74% to 91% (Fig. 1) was found. However, one has to take into account the different natural course of OA among these hip pathologies and the younger mean age at the time of surgery [33].
Negative predictive factors found at both the 5- and 10-year followup included age > 40 years and deficient postoperative acetabular coverage (acetabular index > 14° or total acetabular coverage < 72% from the 5-year followup [35]; LCEA < 22°, and posterior femoral coverage < 34% from the current study). Additional predictive factors found at the 10-year followup were persistent overcoverage of the acetabulum (LCEA > 32°) and a BMI exceeding 30 kg/m2. Although deficient acetabular coverage, as might be seen from excessive trimming (Fig. 4) or trimming in borderline dysplastic hips, resulted in early failure after 5 years, hips with undercorrection and persisting pincer impingement failed later at the 10-year followup (Fig. 2). Thus, optimal acetabular coverage is critical for a good long-term result in hips after surgical correction of FAI (Table 4). Both deficient and excessive acetabular coverage can result in failure, whereas deficient coverage results in more rapid deterioration of the joint than persistent pincer-type impingement. In the literature, reported negative predictive factors include increased OA [20, 23, 26, 29, 31], increased age [15, 20], a decreased BMI [27], and labral resection [19, 23, 31]. Preoperative OA according to Tönnis [40] was not a predictive factor in our multivariate analysis (Table 4). This might be the result of the low percentage of hips with advanced OA (two hips [2%] with OA > Grade 1) in the current patient series. OA tends to progress with age and increased age has been reported as a negative predictive factor in the literature [15, 20] and the current study (Table 4). We found a worse outcome in patients aged > 40 years, which is comparable to the results of arthroscopic treatment with patients requiring THA aged > 48 years [15]. In contrast to our results, Naal et al. [27] found a lower BMI (21 versus 24 kg/m2) in patients with conversion of the hip to THA or major revision following open surgical treatment for FAI. We found a worse outcome in patients with an increased BMI, which shows that excessive weight could be a reason for OA also in the hip. Labral resection has repeatedly found to be a negative predictive factor [19, 23, 31]. In the current study, no labral resection had been performed.
Fig. 4A–F.
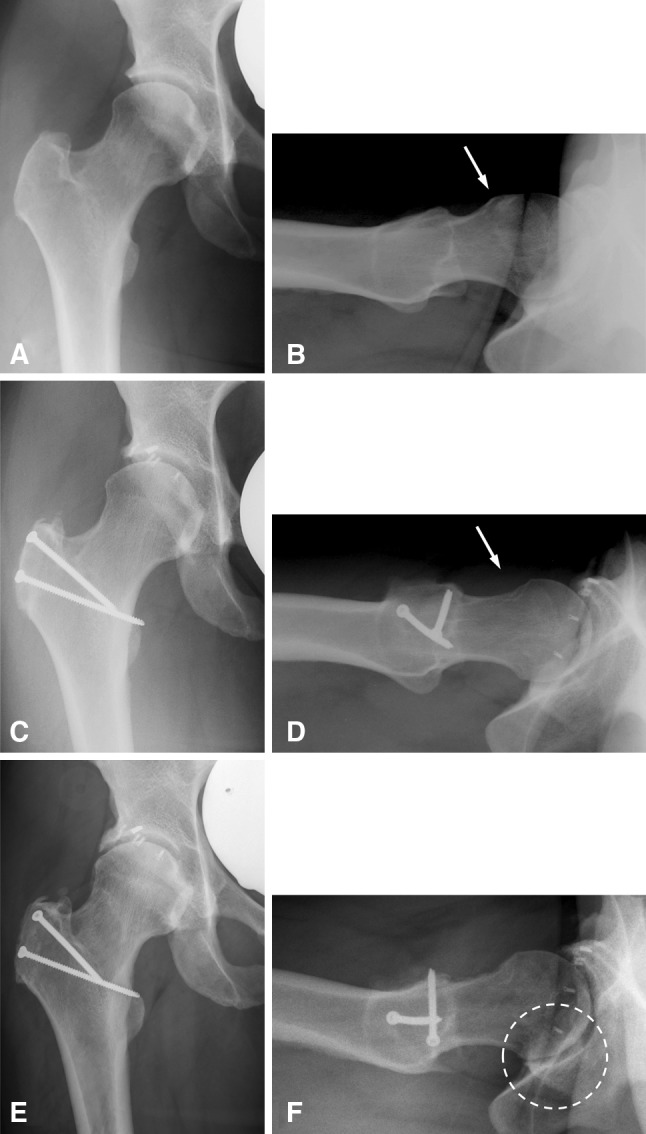
Forty-two-year-old female patient with (A) a normal acetabulum and (B) a decreased anterosuperior offset (arrow), referred to as cam-type FAI. (C) She underwent surgical hip dislocation and trimming of the acetabular rim with labral reattachment resulting in deficient acetabular coverage. (D) On the femoral side, trimming of the head-neck area normalized offset (arrow). (E) At 10-year followup, the hip presented with osteoarthritic changes with osteophyte formation and (F) posteroinferior joint space narrowing.
Based on the 5-year followup [35] and the current results, we have refined the indication for surgical hip dislocation with femoral neck osteoplasty and/or acetabular rim trimming. In addition, we place more emphasis on the ideal amount of acetabular correction. Today patients typically are at a younger age; however, patients aged > 40 years are not necessarily excluded if they present without joint degeneration graded ≥ Tönnis Grade 2. A BMI > 30 kg/m2 has not discouraged us from surgically treating patients with FAI. We believe these patients could benefit from improved joint kinematics with impingement-free motion despite the worse outcome at 5- and 10-year followup. Trimming should be performed according to the preoperative planning and should avoid both excessive and insufficient trimming. Normative data for acetabular coverage [37] can help the surgeon to plan the minimal required and maximal possible resection not to result in dysplastic acetabular coverage. Intraoperatively, care has to be taken not to trim all the damaged acetabular cartilage per se but only the maximal amount possible according to the planning. After correction, the hip should be dynamically assessed to check whether impingement-free ROM was achieved.
In summary, we found that 80% of patients after surgical hip dislocation with trimming of the head-neck junction and/or acetabulum including reattachment of the labrum had not progressed to THA, developed worsening OA, or had a Merle d’Aubigné-Postel score of less than 15. Negative predictors for failure were age > 40 years, a BMI exceeding 30 kg/m2, and both deficient or excessive acetabular coverage. Optimal acetabular coverage is critical for a good long-term result in hips after surgical correction of FAI, but deficient acetabular coverage results in more rapid deterioration of the joint than persistent overcoverage or pincer-type impingement.
Footnotes
One of the authors (MT) has received funding from the Swiss National Science Foundation (SNSF).
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614. doi: 10.1007/s11999-013-2799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beaule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Brunner A, Horisberger M, Herzog RF. Sports and recreation activity of patients with femoroacetabular impingement before and after arthroscopic osteoplasty. Am J Sports Med. 2009;37:917–922. doi: 10.1177/0363546508330144. [DOI] [PubMed] [Google Scholar]
- 6.Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27:1379–1388. doi: 10.1016/j.arthro.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 7.Chiron P, Espie A, Reina N, Cavaignac E, Molinier F, Laffosse JM. Surgery for femoroacetabular impingement using a minimally invasive anterolateral approach: analysis of 118 cases at 2.2-year follow-up. Orthop Traumatol Surg Res. 2012;98:30–38. [DOI] [PubMed]
- 8.Cox DR. Regression models and life tables. J R Stat Soc B. 1972;34:187–220. [Google Scholar]
- 9.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 11.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 13.Holm I, Bolstad B, Lutken T, Ervik A, Rokkum M, Steen H. Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–248. doi: 10.1002/pri.204. [DOI] [PubMed] [Google Scholar]
- 14.Ilizaliturri VM, Jr, Orozco-Rodriguez L, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23:226–234. doi: 10.1016/j.arth.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 15.Jackson TJ, Hanypsiak B, Stake CE, Lindner D, El Bitar YF, Domb BG. Arthroscopic labral base repair in the hip: clinical results of a described technique. Arthroscopy. 2014;30:208–213. doi: 10.1016/j.arthro.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 16.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 18.Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil. 2005;19:659–661. doi: 10.1191/0269215505cr869oa. [DOI] [PubMed] [Google Scholar]
- 19.Larson CM, Giveans MR, Stone RM. Arthroscopic débridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 20.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467:747–752. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lincoln M, Johnston K, Muldoon M, Santore R. Combined arthroscopic and modified open approach for cam femoroacetabular impingement: a preliminary experience. Arthroscopy. 2009;25:392–399. doi: 10.1016/j.arthro.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Martin RL, Sekiya JK. The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J Orthop Sports Phys Ther. 2008;38:71–77. doi: 10.2519/jospt.2008.2677. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy J, Mc Millan S. Arthrocopy of the hip: factors affecting outcome. Orthop Clin North Am. 2013;44:489–498. doi: 10.1016/j.ocl.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 24.McWhirk LB, Glanzman AM. Within-session inter-rater realiability of goniometric measures in patients with spastic cerebral palsy. Pediatr Phys Ther. 2006;18:262–265. doi: 10.1097/01.pep.0000234960.88761.97. [DOI] [PubMed] [Google Scholar]
- 25.Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prostesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed]
- 26.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 27.Naal FD, Miozzari HH, Schar M, Hesper T, Nötzli HP. Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med. 2012;40:1501–1510. doi: 10.1177/0363546512445884. [DOI] [PubMed] [Google Scholar]
- 28.Naal FD, Miozzari HH, Wyss TF, Notzli HP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011;39:544–550. doi: 10.1177/0363546510387263. [DOI] [PubMed] [Google Scholar]
- 29.Palmer DH, Ganesh V, Comfort T, Tatman P. Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy. 2012;28:1671–1681. doi: 10.1016/j.arthro.2012.04.154. [DOI] [PubMed] [Google Scholar]
- 30.Peters CL, Schabel K, Anderson L, Erickson J. Open treatment of femoroacetabular impingement is associated with clinical improvement and low complication rate at short-term followup. Clin Orthop Relat Res. 2010;468:504–510. doi: 10.1007/s11999-009-1152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 32.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 33.Siebenrock KA, Schaller C, Tannast M, Keel M, Büchler L. Anteverting periacetabular osteotomy for symptomatic acetabular retroversion: results at ten years. J Bone Joint Surg. Epub ahead of print. DOI: 10.2106/JBJS.M.00842. [DOI] [PubMed]
- 34.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470:2220–2226. doi: 10.1007/s11999-012-2343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steppacher SD, Huemmer C, Schwab JM, Tannast M, Siebenroc KA. Surgical hip dislocation for treatment of femoroacetabular impingement: factors predicting 5-year survivorship. Clin Orthop Relat Res. 2014;472:337–348. doi: 10.1007/s11999-013-3268-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tannast M, Kakaty DK, Zheng G, Siebenrock K. What is a normal acetabulum? A computer-assisted radiographic study. In: Davies BL, Joskowicz L, Murphy SB, editors. Computer Assisted Orthopaedic Surgery. Berlin, Germany: Pro Business; 2009. pp. 254–257. [Google Scholar]
- 38.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 39.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 40.Tönnis D. General radiography of the hip joint. In: Tönnis D, editor. Congenital Dysplasia and Dislocation of the Hip. Heidelberg, Germany: Springer-Verlag; 1987. pp. 100–142. [Google Scholar]
- 41.Ware JJ, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Wyss TF, Clark JM, Weishaupt D, Notzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158. doi: 10.1097/BLO.0b013e3180399430. [DOI] [PubMed] [Google Scholar]
- 43.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]