Abstract
Background
Normal changes in acetabular version over the course of skeletal development have not been well characterized. Knowledge of normal version development is important because acetabular retroversion has been implicated in several pathologic hip processes.
Questions/purposes
The purpose of this study was to characterize the orientation of the acetabulum by measuring (1) acetabular version and (2) acetabular sector angles in pediatric patients during development. We also sought to determine whether these parameters vary by sex in the developing child.
Methods
We evaluated CT images of 200 hips in 100 asymptomatic pediatric patients (45 boys, 55 girls; mean age, 13.5 years; range, 9–18 years) stratified by the status of the triradiate physis and sex. We determined the acetabular anteversion angle at various levels in the axial plane as well as acetabular sector angles at five radial planes around the acetabulum.
Results
For both genders, anteversion angle was greater for the closed physis group throughout all levels (p < 0.001) and both open and closed physis groups were more anteverted as the cut moved caudally away from the acetabular roof (p < 0.001). At the center of the femoral head, the mean anteversion angle (± SD) in girls was 15° ± 3° in the open group and 19° ± 5° in the closed group (p < 0.001). In boys, the mean anteversion angle increased from 14° ± 4° in the open group to 19° ± 4° in the closed group (p = 0.003). In the superior, posterosuperior, and posterior planes, the acetabular sector angles were greater in the closed compared with the open physis group for both boys and girls with the largest increase occurring in the male posterosuperior plane (approximately 20°) (all p < 0.05).
Conclusions
This study demonstrates that acetabular anteversion and acetabular sector angles in both male and female subjects increase with skeletal maturity as a result of growth of the posterior wall. This suggests that radiographic appearance of acetabular retroversion may not be attributable to overgrowth of the anterior wall but rather insufficient growth of the posterior wall, which has clinical treatment implications for pincer-type impingement.
Level of Evidence
Level IV diagnostic study.
Introduction
The pediatric acetabulum is formed by the confluence of the ilium, ischium, and pubis with the triradiate cartilage complex, a Y-shaped synchondrosis, at the center of these bones [24]. The depth of the acetabulum is governed by interstitial growth within the triradiate and formation of bone at the acetabular margin, causing the hip socket to expand [18, 24]. The concavity of the acetabulum is directly related to the sphericity of the femoral head [18].
During skeletal maturation, three secondary centers of ossification appear in the hyaline cartilage surrounding the acetabular cavity: the epiphysis of the pubis (os acetabuli), the epiphysis of the ilium (acetabular epiphysis), and the smaller epiphysis of the ischium [18, 28]. Recently, an MRI-based study demonstrated that the posterior wall of the acetabulum ossifies more slowly than the anterior wall and fuses just before closure of the triradiate cartilage [5].
Subtle variations in acetabular morphology, particularly acetabular retroversion, which may result from posterior wall deficiency, anterior wall overcoverage, or both, have been demonstrated to cause pincer-type femoroacetabular impingement (FAI) [7, 20]. Whether the acetabular retroversion is the result of a posterior deficiency or anterior overcoverage has potential treatment implications. For example, if retroversion is the result of a posterior deficiency, then anterior rim trimming makes less sense than an acetabular reorientation. Acetabular version is typically determined on a plain radiograph, which can be subject to the quality and position of the radiograph and the age of the patient [10, 27, 30]. Multidetector CT (MDCT) is a more accurate method of measure version [3]. Although there have been studies using CT scans to analyze acetabular version in children [4, 19, 29], our study looks in detail at the growth of the acetabulum-specific locations with skeletal maturation.
Therefore, we asked whether the orientation of the acetabulum and its morphological features, measured by the acetabular version angles and acetabular sector angles, are sex-specific and whether they change with skeletal maturity in asymptomatic pediatric patients.
Materials and Methods
Patient Selection
This was a retrospective review approved by institutional review board with HIPAA compliance and waiver of consent. A Picture Archiving and Communications System (PACS) database was queried to identify patients aged 9 to 18 years who underwent a MDCT of the pelvis with contrast between January 2008 and October 2010 for a history of right lower quadrant or abdominal pain. Electronic medical records for each patient were reviewed with documentation of age in years at the time of MDCT scan, sex, and indication for imaging as well as to ensure the patients had no history of hip pain or surgery. Three hundred thirty-two subjects were stratified by age in 1-year increments. Ten subjects from each age group from 9 years to 18 years (100 patients, 45 boys, 55 girls; mean age, 13.5 years) were sampled from this list to comprise the study population.
Demographics
Two hundred hips in 100 patients were stratified based on the status of the triradiate physis. Fifty hips (11 ± 2 years; range, 9–16 years) were classified into the “open” group and 50 hips (15 ± 2 years; range, 11–18 years) into the “closed” group. The status of the triradiate physis was the same in both hips for all patients.
Imaging Technique
The scanning protocol varied slightly over the study period. Eighty-eight patients were scanned on a GE Lightspeed Pro 32 scanner (GE Medical Systems, Milwaukee, WI, USA), 10 were scanned on a GE Lightspeed Pro 16, and two were scanned on a Siemens Sensation 64 scanner (Siemens Corporation, Erlangen, Germany). Ten studies were acquired helically at 1.25-mm collimation, two studies were acquired helically at 1.50-mm collimation, and 88 studies were acquired at 0.625-mm collimation using soft tissue algorithm. Patients were scanned according to standard departmental protocols at 120 kVp and 50 to 180 mAs depending on patient weight and/or girth with a standard gantry rotation of 0.6 seconds and a pitch of 1.375. Patients were imaged supine with hips extended and the pelvis in neutral position from the level of L3 through the proximal femurs.
Thin-section axial data sets from each scan were reformatted into coronal, sagittal, and axial planes with 0.6-mm thickness and 1.0-mm spacing through bilateral hips on a Leonardo 3D workstation (Siemens AG Medical Solutions, Erlangen, Germany) using bone algorithm. The coronal plane was defined as a plane passing through the center of each femoral head and the most superior aspect of the acetabulum. The axial and sagittal reformatted planes were directly orthogonal to this plane (Fig. 1). Oblique coronal reformatted images through the anterosuperior and posterosuperior acetabulum were performed by defining a plane passing through the center of each femoral head directed 45° in the anterosuperior and posterosuperior directions from the superior acetabulum (as described previously by Fujii et al. [6]) with 0.6-mm thickness. Reformatted images were saved as DICOM images and sent to a PACS workstation for review.
Fig. 1.
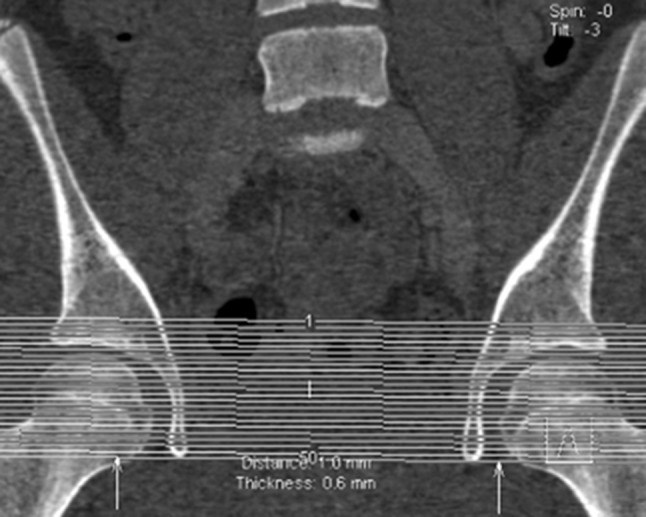
Coronal reformatted image from a MDCT scan demonstrates reformatting technique for axial plane images through the acetabulum. Contiguous axial images at 1.0-mm spacing and 0.6-mm thickness through both acetabula were performed.
Measurement Technique
All images were reviewed by a board-certified pediatric musculoskeletal radiologist, who also performed all subsequent imaging measurements (SB). Images were reviewed to determine the status of the triradiate, anterior, and posterior acetabular physes (open versus closed). The triradiate cartilage was considered “open” if it corresponded to level 1 (open) or level 2 (partially ossified) and “closed” if it corresponded to level 3 of the modified Oxford system (closed) [22] (Fig. 2). The anterior and posterior rim secondary ossification center was considered “open” if it corresponded to Stages I to III of development as described by Fabricant et al. [5] and “closed” if it corresponded to Stage IV (Fig. 3).
Fig. 2.

Coronal reformatted images through the center of the femoral demonstrate open and closed triradiate cartilage physes bilaterally (white arrows) are shown.
Fig. 3.
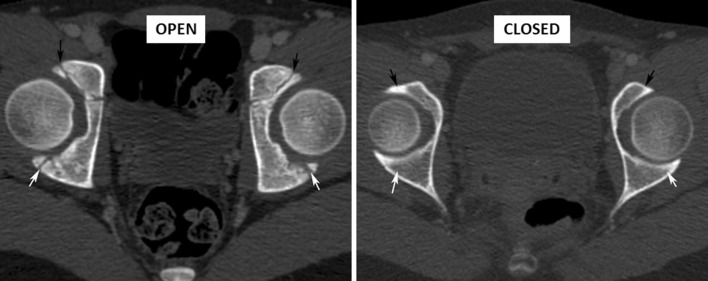
Axial reformatted images demonstrate open and closed anterior (black arrows) as well as posterior rim secondary ossification center (white arrows) bilaterally.
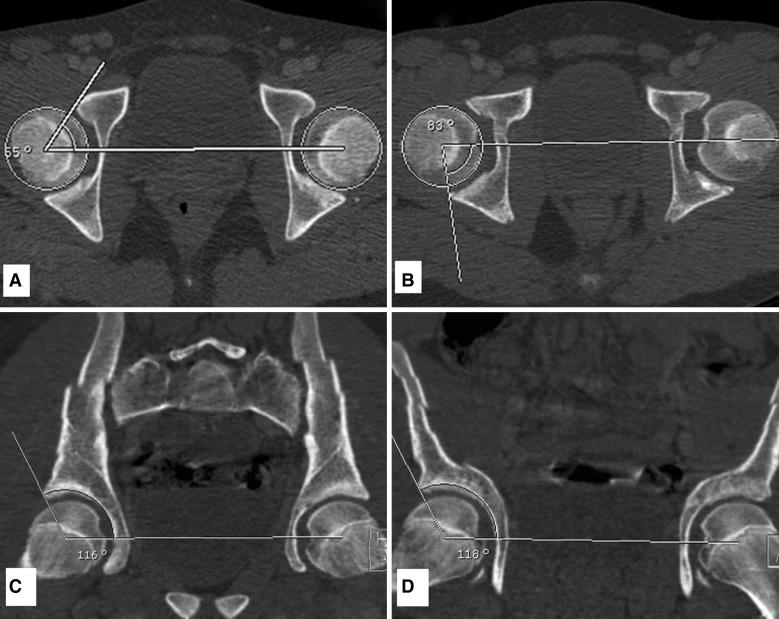
Axial reformatted images through the acetabula were used to measure acetabular version angles at four locations with respect to the acetabular roof on each side: 5 mm, 10 mm, 15 mm, and 20 mm below the roof. An additional measurement of acetabular version was acquired at the center of the femoral head on each side. Acetabular version angles were determined by a line connecting the anterior and posterior margins of the acetabulum and a line perpendicular to a centerline connecting the femoral heads (Fig. 4). The anterior acetabular sector angle [1] was determined by the angle between a centerline connecting the center of each femoral head and a line from the center of each femoral head to the anterior margin of the acetabulum, as previously described by Fujii et al. [6] (Fig. 5). The posterior acetabular sector angle was determined by the angle between the centerline and a line from the center of the femoral head to the posterior margin of the acetabulum. The superior sector angle was measured on a coronal reformatted image through the center of the femoral heads and was determined by the angle between a centerline connecting the femoral heads and a line from the center of each femoral head to the superior margin of the acetabulum. The anterosuperior acetabular sector angle was measured on an oblique coronal plane through the center of the femoral head and directed 45° in an anterior direction determined by the angle between the centerline and a line from the center of each femoral head and the anterosuperior margin of the bony acetabulum. Likewise, the posterosuperior sector angle was measured on an oblique coronal reformatted image through the femoral heads directed 45° in a posterior direction, determined by the angle between a centerline and a line from the center of each femoral head to the posterosuperior margin of the acetabulum.
Fig. 4.
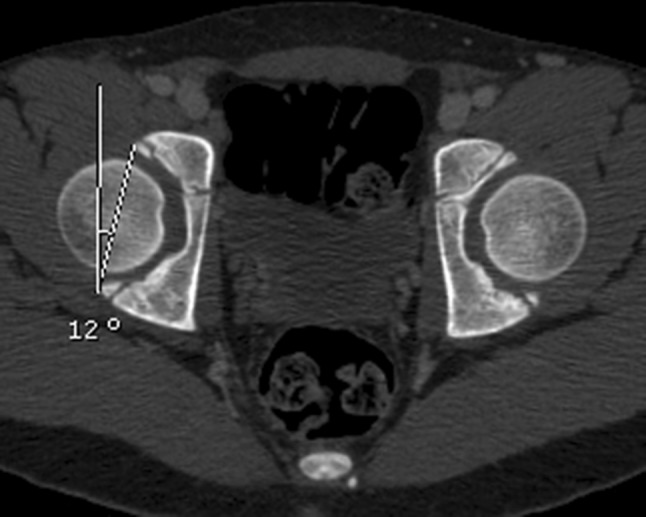
Axial reformatted CT image through the pelvis demonstrates the measurement technique for determining the anteversion angle. The anteversion angle is the angle between a line connecting the anterior and posterior acetabular rim and a line perpendicular to a centerline through both femoral heads.
Fig. 5A–D.
Axial reformatted CT images through the center of both femoral heads demonstrate the technique for measuring anterior acetabular sector angle (AASA) (A), posterior acetabular sector angle (PASA) (B), posterior superior sector angle (PSSA) (C), and superior sector angle (SSA) (D).
These measurements were repeated on a randomly selected 25 patients by the same reader (SB) for assessment of intraobserver variability. A second trained reader (AMH) also performed measurements on 25 patients for assessment of interobserver variability.
Reliability
The difference in acetabular version measurements between the two independent observers was not statistically significant based on paired t-tests (all p > 0.10), averaging less than 1° between them (SD < 2°). The correlation between observers in version exceeded Pearson r = 0.92 for each distance (levels 1–4) from the acetabular roof, indicating excellent interobserver reliability (all p < 0.001). For the five sector angles, the observers differed on average by less than 1° (SD < 3°) with no significant differences (all p > 0.10); correlation in sector angle measurements between the two observers was moderate to high, reflecting good interobserver reliability (anterior r = 0.78, anterosuperior r = 0.96, superior r = 0.72, posterosuperior r = 0.88, posterior r = 0.85; all p < 0.001).
Status of the Physes
Open versus closed status of the anterior acetabular physis, posterior acetabular physis, and the physis of the triradiate cartilage was highly concordant (κ = 0.84, κ = 0.86, and κ = 0.94; all p < 0.001). Given this high concordance, the status of the triradiate cartilage was used in all subsequent statistical analysis. Male gender was associated with an older age of closure of the triradiate physis compared with female gender by a factor of approximately 2 years. Specifically, all girls aged 13 years and older had closed triradiate physis, whereas only two of 10 boys aged 13 to 14 years had closed triradiate physis and six of 10 had closed triradiate physis at the age of 15 years (Table 1).
Table 1.
Closure of the triradiate and posterior acetabular physes stratified by age (years) and gender
| Age group (years) | Number | Triradiate physis | ||||
|---|---|---|---|---|---|---|
| All patients | Girls | Boys | ||||
| Closed | Number | Closed | Number | Closed | ||
| 9–10 | 20 | 0 (0%) | 10 | 0 | 10 | 0 |
| 11–12 | 20 | 2 (10%) | 12 | 2 | 8 | 0 |
| 13–14 | 20 | 12 (60%) | 10 | 10 | 10 | 2 |
| 15–16 | 20 | 16 (80%) | 10 | 10 | 10 | 6 |
| 17–18 | 20 | 20 (100%) | 13 | 13 | 7 | 7 |
| Total | 100 | 50 (50%) | 55 | 35 | 45 | 15 |
| Age group (years) | Number | Posterior acetabular physis | ||||
|---|---|---|---|---|---|---|
| All patients | Girls | Boys | ||||
| Closed | Number | Closed | Number | Closed | ||
| 9–10 | 20 | 0 (0%) | 10 | 0 | 10 | 0 |
| 11–12 | 20 | 5 (25%) | 12 | 4 | 8 | 1 |
| 13–14 | 20 | 13 (65%) | 10 | 10 | 10 | 3 |
| 15–16 | 20 | 18 (90%) | 10 | 9 | 10 | 9 |
| 17–18 | 20 | 20 (100%) | 13 | 13 | 7 | 7 |
| Total | 100 | 56 (56%) | 55 | 36 | 45 | 20 |
| Age group (years) | Number | Anterior acetabular physis | ||||
|---|---|---|---|---|---|---|
| All patients | Girls | Boys | ||||
| Closed | Number | Closed | Number | Closed | ||
| 9–10 | 20 | 0 (0%) | 10 | 0 | 10 | 0 |
| 11–12 | 20 | 3 (15%) | 12 | 3 | 8 | 0 |
| 13–14 | 20 | 14 (20%) | 10 | 10 | 10 | 4 |
| 15–16 | 20 | 18 (90%) | 10 | 9 | 10 | 9 |
| 17–18 | 20 | 20 (100%) | 13 | 13 | 7 | 7 |
| Total | 100 | 55 (55%) | 55 | 35 | 45 | 20 |
Statistical Analysis
Age and sex were compared with respect to acetabular version using repeated measures analysis of variance (ANOVA) to account for measurements at each distance from the acetabular roof as well as both left and right sides pooled with the F-test used to assess significance. This modeling approach also allowed assessment of differences in version based on distances from the acetabular roof. Reference ranges for all patents and each gender were determined by 95% confidence intervals stratified according to open or closed status of the physis. Interobserver agreement for measuring version was evaluated by paired t-tests and Pearson correlations (r), whereas concordance regarding open or closed physis status for anterior, posterior, and triradiate physis was determined by the kappa coefficient (κ). In girls and boys, acetabular sector angles were compared between open and closed triradiate physis using two-way ANOVA. Power analysis indicated that the sample sizes of each gender provided 80% power to detect significant differences of 10° in version across the range of distances from the acetabular roof using the F-test in repeated-measures ANOVA (Version 7.0; nQuery Advisor, Statistical Solutions, Saugus, MA, USA). Two-tailed Bonferroni-adjusted values of p < 0.05 were considered statistically significant. Data analysis and multivariate modeling were performed using SPSS software (Version 19.0; SPSS Inc/IBM, Chicago, IL, USA).
Results
Acetabular Anteversion Angle
Anteversion angle for both girls and boys increased as the hip matured.
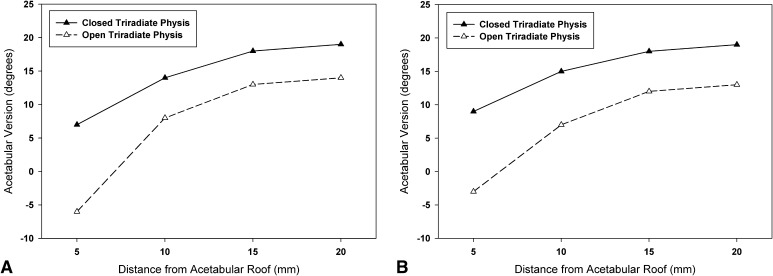
With normal anteversion of the acetabulum defined as 15° to 20° in previous studies [25], all hips demonstrated increasing anteversion with increasing distance from the acetabular roof (Table 2). In girls with closed physis, the mean anteversion angle increased from 7° at level 1 (most proximal) to 19° at level 4 (most distal) and from −6° to 14° in the open group (Fig. 6A). Overall, anteversion was greater for the “closed” physis group throughout all levels (F = 17.13, p < 0.001) and both groups showed more anteversion with further distance from the acetabular roof (F = 242.0, p < 0.001). In boys the mean anteversion angle increased from 9° at level 1 to 19° at level 4 in the closed group and from −3° to 13°, respectively, in the open group (Fig. 6B). Overall, anteversion was greater for the “closed” physis group throughout all levels (F = 11.60, p = 0.001) and both groups showed more anteversion with further distance from the acetabular roof (F = 115.66, p < 0.001).
Table 2.
Reference ranges for acetabular version stratified by gender and status of the triradiate physes*
| Distance (mm) | Level | All patients | Girls | Boys | |||
|---|---|---|---|---|---|---|---|
| Open | Closed | Open | Closed | Open | Closed | ||
| 5 | 1 | −4 (−27 to 21) | 8 (−10 to 28) | −6 (−26 to 8) | 7 (−12 to 29) | −3 (−25 to 25) | 9 (−8 to 26) |
| 10 | 2 | 7 (−16 to 25) | 14 (−6 to 30) | 8 (−23 to 21) | 14 (−7 to 30) | 7 (−15 to 25) | 15 (−1 to 30) |
| 15 | 3 | 12 (0–25) | 18 (4–30) | 13 (−10 to 21) | 18 (2–30) | 12 (0–25) | 18 (8–30) |
| 20 | 4 | 14 (4–25) | 19 (10–30) | 14 (–3 to 21) | 19 (10–30) | 13 (4–25) | 19 (9–30) |
| Center femoral head | 14 (6–22) | 19 (11–27) | 15 (9–21) | 19 (9–29) | 14 (6–22) | 19 (11–27) | |
* Data are mean version (degrees) with reference range defined by 95% confidence intervals shown in parentheses. Relatively greater anteversion is found for closed physis and for measurements farther from the acetabular roof for each gender.
Fig. 6A–B.
(A) Acetabular version is based on the distance from the acetabular roof for females. (B) Acetabular version is based on the distance from the acetabular roof for males.
At the center of the femoral head the mean anteversion angle (± SD) was 14° ± 4° in the open and 19° ± 4° in the closed group (p < 0.001). Further stratified by gender, in girls the mean anteversion angle was 15° ± 3° in the open group and 19° ± 5° in the closed group (p < 0.001). In boys the mean anteversion angle increased from 14° ± 4° in the open group to 19° ± 4° in the closed group (p = 0.003; Table 2).
Characterization of Femoral Head Coverage by the Acetabulum
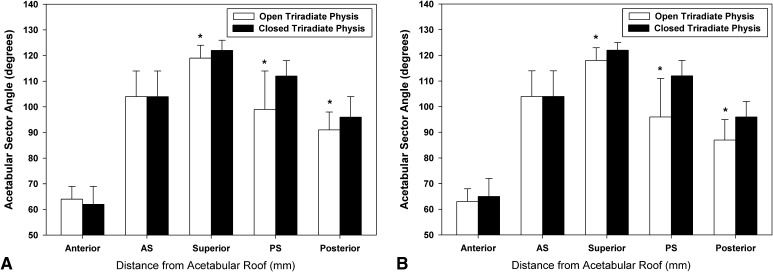
The acetabular sector angles, indices of the acetabular coverage of the femoral head, were greater in the superior, posterosuperior, and posterior directions in the closed physis group compared with the open physis group for both males and females with the largest increase (approximately 20°) occurring in the posterosuperior plane of male subjects (all p < 0.05). There was no difference in the anterior and anterosuperior direction in either gender (all p > 0.05) (Fig. 7A–B).
Fig. 7A–B.
(A) Acetabular sector angles are shown at five different directions in females. Asterisks denote significant difference between open and closed triradiate physes (p < 0.05). (B) Acetabular sector angles are shown at five different directions in males. Asterisks denote significant difference between open and closed triradiate physes (p < 0.05). AS = anterosuperior; PS = posterosuperior.
Discussion
Radiographic evaluation of the developing skeletal system plays a key role in the diagnosis of many pathologic conditions of the hips and pelvis in children and adolescents. Accurate diagnosis of pathology, however, requires an understanding of the normal and expected patterns of growth and development. The anterior and posterior walls of the acetabulum determine the anteversion of the acetabulum in the transverse plane. Abnormalities of anteversion, in particular retroversion, can be a predisposing factor for pain and degenerative disease of the hip [9, 25]. In this study, we sought to characterize the changes in acetabular version and femoral head coverage with skeletal maturity in asymptomatic subjects using MDCT data. Previous examinations with two-dimensional axial CT studies were susceptible to measurement errors as a result of differences in pelvic positioning in the scanner [19, 29]. Using reformatted data from MDCT studies, we were able to control for pelvic tilt and rotation in the gantry by establishing a standard coronal plane, which were the same for all patients, thereby eliminating the variability in positioning. In adults, normal values for this angle through the center of the femoral head range between 15° and 20° [17, 20, 25]. We found that in the developing adolescent the anteversion increased from 14° to 19° with the onset of physeal closure in the hip. Most of the increase in anteversion was the result of growth of the posterior aspect of the acetabulum with skeletal maturity.
This study has several limitations. Patients were not questioned about hip symptoms or activity level nor were patients evaluated with a dedicated hip examination. We attempted to overcome this limitation by excluding patients with mention of hip pain or hip-related conditions in the electronic medical records. It is unknown how many of the patients in this study went on to develop hip-related symptoms or developed osteoarthritis of the hip. Additionally, CT is not as sensitive as MRI for evaluating acetabular morphology before closure of the triradiate cartilage, because the cartilaginous portions of the acetabulum are not well visualized on CT [5, 21]. Therefore, it is possible that the acetabular version may not change as much with skeletal maturity if an MR measure was performed. However, it is the bony acetabulum that is most important in providing hip stability as well as being a potential source of impingement. We found the status of the anterior acetabular physis, posterior acetabular physis, and the physis of the triradiate cartilage was highly concordant. This is in contrast to the recent study of Fabricant et al. [5] reporting that the closure of the posterior acetabular physis precedes the closure of the triradiate cartilage on MRI scans of the hips. However, this may be related to differences in the imaging appearance of cartilage and bone on MRI versus CT [5, 12, 21]. Finally, we focused our attention on the development of the acetabulum and not the entire hemipelvis. Therefore, we were not able to assess whether the hips with acetabular retroversion were the result of malrotation of the entire hemipelvis versus the acetabulum alone.
In contrast to Weiner et al. [29], we found less anteversion in subjects with open physes compared with subjects with closed physes at the slice through the center of the femoral head. However, their study was limited in that only one slice of the axial CT scan was measured and the effect of pelvic tilt was not controlled.
Reikeras et al. [19] indicated that calculated values of the anteversion in children depended on the selected section of the acetabular socket, whereas studies of the adult hip reported that the adult anteversion seems to be quite constant, regardless of the level of the axial CT image [2, 26]. In our study of 200 hips, the mean anteversion angle at level 1 (most proximal) was −4° in the open and 8° in the closed group, which was significantly less than the measurement at level 2 (7° and 14°, respectively). Anteversion became increasingly anteverted with the anteversion most anteverted at level 4 (most distal) in the open and closed groups (14° and 19°). Overall, in mature hips, the anteversion angle was higher throughout all levels in both genders compared with immature hips. These results reveal a similar trend that was recently reported by Fujii et al. [6] using a similar measurement method as this study. Their values for the control group are comparable to ours with a reduced anteversion angle in the more proximal section of the acetabulum compared with the more distal levels. Furthermore, Monazzam et al. [15] recently corroborated our findings by measuring anteversion on standardized CT scans of 225 asymptomatic pediatric and adolescent patients. They reported an increase in anteversion with age and lower values in the superior compared with the center of the femoral head.
In terms of sex, we did not find a difference in acetabular anteversion between boys and girls in contrast to adult studies of normal hip morphology [11, 16]. This may be related to the younger age of our patients.
To determine acetabular coverage of the femoral head, we measured the acetabular sector angle using a method first described by Anda et al. [1] and recently modified by Fujii et al. [6]. As shown previously, a shallow acetabulum may have a normal anteversion indicating that the sector angles give a better quantitative description of the acetabulum in the unstable hip [1]. Our measurement of the acetabular sector angle correlates well with the change in acetabular orientation based on anteversion measurement. Compared with the open group, the closed group had higher acetabular sector angles in the superior, posterosuperior, and posterior directions in both genders. These measurement trends indicate a change in the shape and orientation of the posterior aspect of the acetabulum in the closed group.
The findings in our study may help explain the mechanism behind several different disease processes that affect the developing hip. Hip dislocations tend to be posterior and are usually seen in children in the preadolescent age group between 7 and 10 years of age [14]. A more retroverted, soft, pliable acetabulum in immature hips may predispose the hip to a posterior dislocation after minimal trauma [14, 23]. It has been further reported by several studies that premature closure of the triradiate cartilage leads to a shallow and more retroverted acetabulum [13]. Our data lend support to this statement, because we found that a more retroverted acetabulum is a physiological finding in immature hips before closure of the triradiate cartilage. A high prevalence of retroverted acetabula has been reported in patients with pincer-type and mixed-type (cam and pincer) FAI [8, 15]. Often in these cases the acetabulum is thought to be retroverted based on the presence of a crossover sign, which could be present if the anterior wall is overextended. However, a crossover sign could develop because a posterior wall is deficient as well. We saw an increase in acetabular anteversion in asymptomatic patients with increasing age, likely as a result of growth of the posterior wall. It might be hypothesized that a crossover sign may result from a disruption of posterior wall development; therefore, careful cross-sectional analysis of hip coverage should be performed before assuming there is an anterior overcoverage in hips with a crossover sign.
In conclusion, this study used MDCT in asymptomatic pediatric and adolescent patients and demonstrated an increase of acetabular anteversion in both male and female patients with closed triradiate physes compared with those with open physes. The additional growth of the acetabular wall with maturation is most pronounced in the posterior aspect of the hip. These findings may explain the ease of an adolescent hip to dislocate posteriorly with moderate trauma. Additionally, the presence of a crossover sign on radiographs may not necessarily be the result of an anterior overgrowth but may be a mark of posterosuperior deficiency. We suggest careful analysis of the hip coverage before performing an acetabular rim resection in hips with impingement. Further longitudinal studies will be critical in determining the role of these growth patterns in the development of various pathologic pediatric hip conditions.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that the institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Children’s Hospital Boston, Boston, MA, USA.
References
- 1.Anda S, Svenningsen S, Dale LG, Benum P. The acetabular sector angle of the adult hip determined by computed tomography. Acta Radiol. 1986;27:443–447. doi: 10.1177/028418518602700415. [DOI] [PubMed] [Google Scholar]
- 2.Anda S, Terjesen T, Kvistad KA. Computed tomography measurements of the acetabulum in adult dysplastic hips: which level is appropriate? Skeletal Radiol. 1991;20:267–271. doi: 10.1007/BF02341662. [DOI] [PubMed] [Google Scholar]
- 3.Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91:1031–1036. doi: 10.1302/0301-620X.91B8.22389. [DOI] [PubMed] [Google Scholar]
- 4.Dwek JR, Monazzam S, Chung CB. Radiologic analysis of femoral acetabular impingement: from radiography to MRI. Pediatr Radiol. 2013;43(Suppl 1):S61–S70. doi: 10.1007/s00247-012-2588-7. [DOI] [PubMed] [Google Scholar]
- 5.Fabricant PD, Hirsch BP, Holmes I, Kelly BT, Lorich DG, Helfet DL, Bogner EA, Green DW. A radiographic study of the ossification of the posterior wall of the acetabulum: implications for the diagnosis of pediatric and adolescent hip disorders. J Bone Joint Surg Am. 2013;95:230–236. doi: 10.2106/JBJS.L.00592. [DOI] [PubMed] [Google Scholar]
- 6.Fujii M, Nakashima Y, Yamamoto T, Mawatari T, Motomura G, Matsushita A, Matsuda S, Jingushi S, Iwamoto Y. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895–903. doi: 10.2106/JBJS.I.00046. [DOI] [PubMed] [Google Scholar]
- 7.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 8.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 9.Ito K. Minka MA 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 10.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the ‘cross-over-sign’. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 11.Kang AC, Gooding AJ, Coates MH, Goh TD, Armour P, Rietveld J. Computed tomography assessment of hip joints in asymptomatic individuals in relation to femoroacetabular impingement. Am J Sports Med. 2010;38:1160–1165. doi: 10.1177/0363546509358320. [DOI] [PubMed] [Google Scholar]
- 12.Lang P, Genant HK, Jergesen HE, Murray WR. Imaging of the hip joint. Computed tomography versus magnetic resonance imaging. Clin Orthop Relat Res. 1992;274:135–153. [PubMed] [Google Scholar]
- 13.Liporace FA, Ong B, Mohaideen A, Ong A, Koval KJ. Development and injury of the triradiate cartilage with its effects on acetabular development: review of the literature. J Trauma. 2003;54:1245–1249. doi: 10.1097/01.TA.0000029212.19179.4A. [DOI] [PubMed] [Google Scholar]
- 14.Meena S, Kishanpuria T, Gangari SK, Sharma P. Traumatic posterior hip dislocation in a 16-month-old child: a case report and review of literature. Chinese J Traumatol. 2012;15:382–384. [PubMed] [Google Scholar]
- 15.Monazzam S, Bomar JD, Dwek JR, Hosalkar HS, Pennock AT. Development and prevalence of femoroacetabular impingement-associated morphology in a paediatric and adolescent population: a CT study of 225 patients. Bone Joint J. 2013;95:598–604. doi: 10.1302/0301-620X.95B5.30118. [DOI] [PubMed] [Google Scholar]
- 16.Murtha PE, Hafez MA, Jaramaz B, DiGioia AM., 3rd Variations in acetabular anatomy with reference to total hip replacement. J Bone Joint Surg Br. 2008;90:308–313. doi: 10.1302/0301-620X.90B3.19548. [DOI] [PubMed] [Google Scholar]
- 17.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 18.Ponseti IV. Growth and development of the acetabulum in the normal child. Anatomical, histological, and roentgenographic studies. J Bone Joint Surg Am. 1978;60:575–585. [PubMed] [Google Scholar]
- 19.Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum in patients with idiopathic increased anteversion of the femoral neck. Acta Orthop Scand. 1982;53:847–852. doi: 10.3109/17453678208992837. [DOI] [PubMed] [Google Scholar]
- 20.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 21.Rubel IF, Kloen P, Potter HG, Helfet DL. MRI assessment of the posterior acetabular wall fracture in traumatic dislocation of the hip in children. Pediatr Radiol. 2002;32:435–439. doi: 10.1007/s00247-001-0634-y. [DOI] [PubMed] [Google Scholar]
- 22.Stasikelis PJ, Sullivan CM, Phillips WA, Polard JA. Slipped capital femoral epiphysis. Prediction of contralateral involvement. J Bone Joint Surg Am. 1996;78:1149–1155. doi: 10.2106/00004623-199608000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Steppacher SD, Albers CE, Siebenrock KA, Tannast M, Ganz R. Femoroacetabular impingement predisposes to traumatic posterior hip dislocation. Clin Orthop Relat Res. 2013;471:1937–1943. doi: 10.1007/s11999-013-2863-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strayer LM., Jr Embryology of the human hip joint. Clin Orthop Relat Res. 1971;74:221–240. doi: 10.1097/00003086-197101000-00029. [DOI] [PubMed] [Google Scholar]
- 25.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Visser JD, Jonkers A, Hillen B. Hip joint measurements with computerized tomography. J Pediatr Orthop. 1982;2:143–146. doi: 10.1097/01241398-198202020-00005. [DOI] [PubMed] [Google Scholar]
- 27.Wassilew GI, Heller MO, Diederichs G, Janz V, Wenzl M, Perka C. Standardized AP radiographs do not provide reliable diagnostic measures for the assessment of acetabular retroversion. J Orthop Res. 2012;30:1369–1376. doi: 10.1002/jor.22086. [DOI] [PubMed] [Google Scholar]
- 28.Watts HG. Fractures of the pelvis in children. Orthop Clin North Am. 1976;7:615–624. [PubMed] [Google Scholar]
- 29.Weiner LS, Kelley MA, Ulin RI, Wallach D. Development of the acetabulum and hip: computed tomography analysis of the axial plane. J Pediatr Orthop. 1993;13:421–425. doi: 10.1097/01241398-199307000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471:2463–2470. doi: 10.1007/s11999-012-2689-5. [DOI] [PMC free article] [PubMed] [Google Scholar]