Abstract
There is increasing concern that the media present conflicting health information on topics including cancer screening and nutrition. Although scholars have speculated that exposure to this information leads to increased public confusion, less trust in health recommendations, and less engagement in health behaviors, there is a lack of empirical research that directly addresses the role of media exposure to conflicting information. Using data from the Annenberg National Health Communication Survey, this study finds that exposure to conflicting information on the health benefits and risks of, for example, wine, fish, and coffee consumption is associated with confusion about what foods are best to eat and the belief that nutrition scientists keep changing their minds. There is evidence that these beliefs, in turn, may lead people to doubt nutrition and health recommendations more generally—including those that are not rife with contradictory information (e.g., fruit and vegetable consumption, exercise). The implications of these findings for healthy eating campaigns and interventions are discussed.
Keywords: Contradictory information, Nutrition, Media exposure
Nutrition researchers and clinicians have assumed that contradictory health and nutrition messages exist in the news media (e.g., Angell & Kassirer, 1994; Boyle, Boffetta, & Autier, 2008; Fineberg & Rowe, 1998), and that exposure to these messages negatively influences public understanding and health behavior (e.g., American Dietetic Association, 2007; Drummond, 2006; Goldberg & Hellwig, 1997). Although there is some evidence that this information exists (e.g., Greiner, Smith, & Guallar, 2010; Smith, Kromm, & Klassen, 2010; Squiers et al., 2011; Vardeman & Aldoory, 2008), there have been few efforts to capture exposure to contradictory health and nutrition messages (Nagler & Hornik, 2012) and assess its potential effects. In addition, the studies that exist lack a theoretical rationale for why these messages might lead to effects.
The present study therefore has two goals. First, it addresses the extent to which people notice contradictory nutrition messages in the media. Second, it evaluates whether such exposure is linked to potentially deleterious outcomes—specifically, nutrition confusion (defined as perceived ambiguity about nutrition recommendations and research), nutrition backlash (defined as negative beliefs about nutrition recommendations and research), and, ultimately, lower intentions to engage in recommended health behaviors (e.g., fruit and vegetable consumption, exercise). Following a brief review of the existing research on contradictory health and nutrition messages, this article provides a theoretical foundation for studying these messages and their effects. Then, using cross-sectional data from a population-based survey of U.S. adults, the analyses explore hypothesized relationships between contradictory information exposure, cognitions, and behavioral intentions. If there is evidence of associations, then efforts to demonstrate the effects of contradictory message exposure will be undertaken in future research, whether through experimental or longitudinal observational work.
Evidence for contradictory health and nutrition messages
Although there are several ways in which we might conceptualize contradictory health messages, this study focuses on a specific definition: messages that offer information about a single behavior producing two distinct outcomes. For example, one day someone might see a news article summarizing recent research that found an association between red wine consumption (a single behavior) and improved heart health (outcome #1), but a few weeks later, he or she might see another article reporting that new research linked increased consumption of red wine and other alcohol to an increased risk of breast cancer (outcome #2). Someone who notices both messages might wonder if he or she should consume red wine and, if so, how much.
From a nutritional epidemiological standpoint, these messages might not be contradictory per se. For example, in the case of red wine and other alcohol, consumption legitimately could contribute to cardiovascular health, on the one hand, and increased risk of breast cancer on the other. Contradictory findings also might arise because distinct study designs can produce seemingly conflicting findings: a randomized controlled trial of beta carotene might reach different conclusions than earlier observational work. Alternatively, studies may vary in how they measure nutritional intake, and some may be more prone to measurement error. Because researchers and clinicians understand these plausible explanations and know that nutrition science is evolutionary (Goldberg & Sliwa, 2011), they are well-equipped to negotiate seemingly conflicting results (Kushi, 1999; Taubes, 2007). In contrast, the public may be less able to reconcile such findings, as many Americans lack a thorough understanding of scientific research (Miller, 2004). In addition, news coverage of science and health often omits methodological and contextual information (e.g., Evans, Krippendorf, Yoon, Posluszny, & Thomas, 1990; Nelkin, 1995; Pellechia, 1997; Tankard & Ryan, 1974). Such omissions may influence people’s health cognitions (Jensen et al., 2011), as well as their ability to make sense of conflicting study results. Ultimately, then, it is important to understand whether the public notices contradictory health information in the media and, if so, how it responds to such content.
There is some evidence that these contradictory messages exist in the public information environment. For example, content analyses have identified contradictory information about cancer screening (Smith et al., 2010) and nutrition in the media (Greiner et al., 2010; Houn et al., 1995). Survey studies have found that women perceive conflict and controversy surrounding mammography guidelines (Meissner et al., 2003; Rimer, Halabi, Strigo, Crawford, & Lipkus, 1999; Squiers et al., 2011; Taplin, Urban, Taylor, & Savarino, 1997), while others have qualitatively explored public perceptions of contradictory nutrition messages (Basu & Hogard, 2008; Boyington, Schoster, Martin, Shreffler, & Callahan, 2009; Diekman & Malcolm, 2009; Dorey & McCool, 2009; Dye & Cason, 2005; Vardeman & Aldoory, 2008). Importantly, however, none specifically assessed media exposure to such content. Only one recent study did so, in an effort to evaluate four potential measures of media exposure to contradictory nutrition information (Nagler & Hornik, 2012). Another study considered potential outcomes of contradictory exposure—such as nutrition backlash, or “negative feelings about dietary recommendations”—without assessing exposure itself (Patterson, Satia, Kristal, Neuhouser, & Drewnowski, 2001, p. 38). Given this dearth of research on contradictory exposure, the following research question is posed:
RQ1: To what extent do people notice contradictory information about nutrition topics in the media (including television, radio, newspapers, magazines, and the Internet)?
Decision theory’s concept of ambiguity
As previously noted, confusion is often assumed to be an outcome of exposure to contradictory information (American Dietetic Association, 2007; Drummond, 2006; Goldberg, 1992; Goldberg & Hellwig, 1997; Johnson-Taylor, Yaroch, Krebs-Smith, & Rodgers, 2007). Yet what theoretical support is there for this relationship? The concept of “ambiguity,” as described by decision theorist Daniel Ellsberg (1961), provides a foundation for the link between contradictory information exposure and confusion. Importantly, Ellsberg made a distinction between uncertainty about decisional outcomes (which characterizes all decisions involving risk) and “ambiguity,” which refers to the quality of one’s information regarding the likelihood of those outcomes. In other words, “[ambiguity] may be high…even where there is ample quantity of information, when there are questions of reliability and relevance of information, and particularly where there is conflicting opinion and evidence [emphasis in original]” (Ellsberg, 1961, p. 659). The latter condition of conflicting opinion and evidence is particularly relevant to this study, and informs the following hypothesis:
H1: Exposure to contradictory nutrition messages will be positively associated with nutrition confusion, or perceived ambiguity about nutrition recommendations and research.
The decision theory concept of ambiguity has been applied in the health domain. In a set of studies, Han and colleagues explored the influence of perceived ambiguity about cancer prevention recommendations on other cancer-related perceptions and behaviors (Han, Kobrin, et al., 2007; Han, Moser, & Klein, 2006; Han, Moser, & Klein, 2007). Consistent with decision theory research, Han et al. suggested that most people will be averse to ambiguity about cancer prevention recommendations and, importantly, “may manifest this ambiguity aversion through pessimistic interpretations about the preventability of cancer—that is, lower preventability beliefs” (Han, Moser, & Klein, 2006, p. 54). As hypothesized, they found that people who reported greater perceived ambiguity about prevention recommendations reported lower preventability beliefs. By extension, the present study hypothesizes that people will be averse to ambiguity about nutrition recommendations, and thus may have lower or more negative beliefs regarding nutrition recommendations and research (defined as nutrition backlash). In other words, those who report greater confusion will be more likely to experience backlash:
H2: Nutrition confusion will be positively associated with nutrition backlash.
As evident in H1 and H2, nutrition confusion may play a central role in linking exposure with backlash. If there is evidence that exposure is associated with confusion, and that confusion is associated with backlash (controlling for exposure), then the following research question will be considered:
RQ2: Is there evidence of an indirect path from contradictory message exposure to nutrition backlash through nutrition confusion?
Whereas Ellsberg’s theorizing about ambiguity guides the hypothesized relationships between exposure and confusion (H1) and confusion and backlash (H2), it does not address whether exposure may be directly associated with backlash. That said, because a direct relationship may exist, a third research question is asked:
RQ3: Is there evidence of a direct path from contradictory message exposure to nutrition backlash?
Carryover effects on behavioral intentions
Researchers and clinicians have been concerned not only about cognitive outcomes of exposure to conflicting health information, but also downstream effects on recommended health behaviors (e.g., Department of Health and Human Services, 2008; Goldberg & Hellwig, 1997). The fundamental concern is that those who report greater contradictory exposure to topics such as fish, wine, and coffee consumption will experience greater feelings of confusion and backlash—and that these beliefs, in turn, may lead people to doubt public health recommendations more generally, including those about which there is little contradictory information (e.g., fruit and vegetable consumption, exercise). What theoretical rationale is there to expect such carryover effects? There has not been much theorizing or research in this area, but the work that exists provides some support for this concern.
First, there has been attention to carryover effects in the marketing domain. One study considered whether an “irritation transfer” effect occurs in advertising (Fennis & Bakker, 2001). The authors hypothesized that irritation elicited by disliked ads or a large number of ads would carry over to a subsequent unrelated neutral ad, and that this transfer would be particularly evident among high “need to evaluate” individuals (i.e., those who tend to engage in evaluative responding to products, future behaviors, etc.; Jarvis & Petty, 1996). Fennis and Bakker’s hypothesis was supported, and they suggested that such carryover effects may occur through excitation transfer. Excitation transfer theory predicts an enhanced emotional reaction to an emotion-arousing situation due to excitation that remains from a prior related or unrelated emotion-arousing situation (Zillman, 1983). Thus the excitation—here, irritation—resulting from exposure to the first series of ads might transfer to the unrelated ad because, as Zillman has argued, such residual sympathetic excitation is presumed to be largely nonspecific.
Perhaps excitation transfer could underlie a carryover effect of exposure to contradictory information and its associated cognitions. Suppose the current study finds that contradictory exposure is associated with confusion and, indirectly, with backlash. If backlash reflects negative affect, then it is plausible that such negativity could extend to nutrition-related recommendations about which there is little conflict or controversy (e.g., fruit and vegetable consumption) and even health-related recommendations in general (e.g., exercise). Since the underlying argument in this study is that any effects that may exist would result from cumulative exposure to contradictory messages, there would be many opportunities for negative affect or backlash to occur and, perhaps, to build over time via priming (Roskos-Ewoldsen, Roskos-Ewoldsen, & Dillman Carpentier, 2009).
In addition, there is empirical data to suggest that cognitive outcomes of exposure could have carryover effects. Han and colleagues demonstrated that perceived ambiguity about cancer prevention recommendations was inversely associated with colon cancer screening and sunscreen use (Han, Moser, et al., 2007), as well as decreased uptake of mammography over time (Han, Kobrin, et al., 2007). Similarly, it is possible that people who exhibit greater nutrition confusion may be less likely to engage in recommended nutrition-related behaviors (e.g., fruit and vegetable consumption). Again this prediction is based on the notion that people are ambiguity averse: confusion may lower perceptions of the usefulness of recommended behaviors, and thus reduce interest in engaging in them. Moreover, Niederdeppe & Levy (2007) found that fatalistic beliefs about cancer prevention were negatively associated with prevention behaviors, including fruit and vegetable consumption and exercise. Conceptually speaking, cancer fatalism and nutrition backlash are similar: both capture negative feelings toward recommendations and research, the former regarding cancer prevention and the latter regarding nutrition-related behavior. Thus it might be expected that backlash will be negatively associated with intention to engage in recommended health behaviors. Ultimately, then, this set of empirical findings, coupled with a theoretical rationale for why we might expect carryover effects, leads to the following hypotheses:
H3: Nutrition confusion will be negatively associated with intentions to adhere to healthy lifestyle recommendations (e.g., fruit and vegetable consumption, exercise).
H4: Nutrition backlash will be negatively associated with intentions to adhere to healthy lifestyle recommendations (e.g., fruit and vegetable consumption, exercise).
If analyses show that confusion is associated with backlash, and that backlash is associated with intentions to adhere to healthy lifestyle recommendations (controlling for confusion), then it will be important to assess whether part of confusion’s association with intentions is carried indirectly through backlash:
RQ4: Is there evidence of an indirect path from nutrition confusion to behavioral intentions through nutrition backlash?
All hypothesized relationships are summarized in the conceptual model of effects, which is shown in Figure 1.
Figure 1.
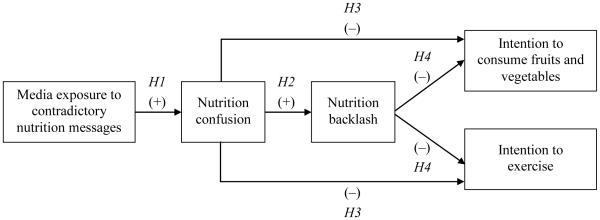
Predicted relationships between media exposure to conflicting nutrition information, nutrition confusion, nutrition backlash, and intentions to adhere to healthy lifestyle recommendations (e.g., fruit and vegetable consumption, exercise)
Method
This study used data from the February and March 2010 Annenberg National Health Communication Survey (ANHCS). ANHCS collects cross-sectional data monthly from a nationally representative sample of U.S. adults over age 18 (ANHCS, 2007). The online survey is administered by Knowledge Networks, a survey research firm that uses a list-assisted random-digit dialing procedure to recruit a panel from all U.S. landline telephone households. Every month respondents are recruited from the panel; those without Internet are provided with access. The February and March panel recruitment response rate was 20% and the survey completion rate was 59%.
Sample
A total of 631 adults participated in the survey. The sample was 56% female, with a mean age of 51 (SD = 16.5). Nine percent had less than a high school degree, 29% earned a high school degree or the equivalent, 29% had some college education, and 33% earned at least a Bachelor’s degree. Just over 80% of respondents were Non-Hispanic White and 5% were Non-Hispanic Black; 7% were Hispanic. Sixty-one percent were married.
Measures
Media exposure to contradictory nutrition information
In a previous study, we developed a measure of media exposure to contradictory nutrition information; validity evidence has been presented elsewhere (Nagler & Hornik, 2012). Participants were asked how much conflicting or contradictory information they heard from the media (including television, radio, newspapers, magazines, and the Internet) in the past year about the following nutrition topics: red wine or other alcohol, fish, coffee, and vitamins/supplements. These were selected because content analysis results have shown that there is substantial contradictory information about these topics in the media (Nagler, 2010). The four topics were randomly ordered. Response options included “Not at all” (1), “A little” (2), “Some” (3), and “A lot” (4). The four individual measures were summed to create a combined exposure index (range = 4–16; M = 9.6; SD = 3.3). A value of 4 reflected no reported exposure to contradictory information across topics. Values of 5 through 7 reflected “lower exposure” to contradictory information across topics, 8 through 11 reflected “medium exposure,” and 12 through 16 reflected “higher exposure.”
Nutrition confusion
Han and colleagues used a single item to capture perceived ambiguity about cancer prevention recommendations, but recognized that “the refinement of measures of perceived ambiguity is a critical task for future research” (Han, Kobrin, et al., 2007, p. 465). Thus in an effort to move away from single-item measurement, respondents were asked to give their opinion about six statements: “It is not always clear to me what foods are best for me to eat,” “I find nutrition recommendations to be confusing,” “Nutrition research findings make sense to me,” “I know what I should be eating to stay healthy,” “I find nutrition research studies hard to follow,” and “I understand scientists’ recommendations about what foods I should eat.” Response options ranged from “Strongly agree” (1) to “Strongly disagree” (5). The first, second, and fifth items were reverse-coded so that a higher score signified greater confusion. Items were summed to create a confusion scale (range = 6–28; M = 16.4; SD = 3.8), which demonstrated good internal consistency (α = .77). A principal components factor analysis provided evidence of unidimensionality: although two components were extracted, the second had an Eigenvalue barely higher than 1.0, and it accounted for only 17.8% of the variance. As often occurs, the three reverse-coded items loaded on a separate factor.
Nutrition backlash
To assess feelings of backlash towards nutrition recommendations and research, respondents were asked to give their opinion about six statements: “I am tired of hearing about what foods I should or should not eat,” “Scientific research provides good guidance about the best foods to eat,” “The evidence about healthy food choices is growing,” “Dietary recommendations should be taken with a grain of salt,” “Scientists really don’t know what foods are good for you,” and “I pay attention to new research on food and nutrition.” Response options ranged from “Strongly agree” (1) to “Strongly disagree” (5). The first, fourth, and fifth items were reverse-coded so that a higher score signified greater nutrition backlash. Items were summed to create a backlash scale (range = 6–30; M = 16.0; SD = 3.3), which demonstrated acceptable internal consistency (α = .71). There was also evidence of unidimensionality: again two components were extracted, but the second had an Eigenvalue barely higher than 1.0 and accounted for only 17.1% of the variance; the three reverse-coded items loaded on a separate factor. Items were adapted from an 11-item scale developed by Patterson and colleagues (2001; α = .72).
To assess whether confusion and backlash are distinct constructs, zero-order correlations were averaged across the confusion items and across the backlash items; the mean correlation for each set of items was compared to the average correlation across both sets of items. The mean correlation across the set of confusion and backlash items was positive (mean r = 0.23; 95% CI = 0.17–0.30) and significant (all correlations p < .05). However, the mean correlation within the set of confusion items was higher (mean r = 0.34; 95% CI = 0.25–0.42; all correlations p < .05), as was the mean correlation within the set of backlash items (mean r = 0.30; 95% CI = 0.22–0.38; all correlations p < .05). Thus there was some evidence for discriminant validity, but observed differences in correlations could have been chance differences, given overlap between the two within-items confidence intervals and the across-items confidence interval.
Intention to adhere to healthy lifestyle recommendations
Using a response scale from “Very unlikely” (1) to “Very likely” (5), respondents were asked to report their intentions to adhere to two healthy lifestyle recommendations, fruit and vegetable consumption and exercise. Standard intentions measures were used as proxies for the specific recommendations: “How likely is it that you will have five or more servings of fruits and vegetables most days in the next year?” and “How likely is it that you will exercise at least three times in most weeks over the next year?” (M = 3.3; SD = 1.2 and M = 3.6; SD = 1.2, respectively).
Potential confounders
Multivariable models adjusted for several sociodemographic characteristics, including age, education, gender, and race/ethnicity. Another likely potential confounder was generalized mistrust. We could imagine that those who tend to be more mistrustful might tend to notice more contradictory information and also might experience greater backlash. Importantly, backlash—which is conceptualized as a psychological state (brought on by contradictory exposure and confusion)—should be distinguished from more generalized mistrust, which is conceptualized as an individual difference characteristic. A proxy measure of mistrust was developed using five institutional trust items from the General Social Survey (Davis, Smith, & Marsden, 2009). Respondents were asked, “How much confidence do you have in each of the following institutions [Business and industry; U.S. Congress; Courts and the legal system; Executive branch of the federal government; Schools and the educational system]?” Response options ranged from “Complete confidence” (1) to “No confidence at all” (5). The five items were summed to create a mistrust scale (range = 5–25; M = 17.2; SD = 3.2), with higher scores reflecting greater mistrust. There was good evidence of internal consistency (α = 0.78) and unidimensionality (one component extracted with an Eigenvalue greater than 1.0).
Analytic approach
Basic frequency analyses were used to calculate the percentage of respondents who reported exposure to contradictory nutrition information (RQ1). Zero-order correlations were used to estimate bivariate associations between central hypothesized constructs. Multivariable linear regression was used to estimate the associations between constructs, adjusting for sociodemographic characteristics and generalized mistrust (H1–H4 and RQ3). Since fewer than 15% of cases were missing across analyses, listwise deletion was used to deal with missing data. Missing data were due to the number of refused on any given question.
To address the research questions on indirect effects (RQ2 and RQ4), the joint significance test was used. Compared with other methods for testing intervening variable effects (e.g., the causal steps approach popularized by Baron and Kenny (1986)), the joint significance test provides the best balance of statistical power and Type I error (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). It stipulates that if X is associated with M, and if M is associated with Y controlling for X, then there is evidence of an indirect effect. In other words, paths a and b, which comprise the intervening variable effect, are jointly significant. In contrast to the causal steps approach, the joint significance test does not require a significant total effect of X on Y—and thus is consistent with the more recent recommendation that researchers not require a significant total effect to proceed with tests of indirect effects (see Hayes, 2009 for a detailed discussion; MacKinnon, Krull, & Lockwood, 2000; Shrout & Bolger, 2002). In addition, the significance of indirect effects was tested using Preacher and Hayes’ bootstrapping methodology (2008). This approach, which allows researchers to obtain bootstrapped standard error estimates and confidence intervals, is preferable to the Sobel test because it does not require a normal sampling distribution for the indirect effect (Preacher & Hayes, 2008; Shrout & Bolger, 2002). All analyses were performed using PASW Statistics 18 (IBM SPSS Statistics, 2010).
Results
Reported exposure to contradictory nutrition information in the media
Respondents reported substantial media exposure to conflicting information about red wine or other alcohol, fish, coffee, and vitamins/supplements (Table 1). Across nutrition topics, nearly three-quarters (71.8%) of respondents reported medium or higher levels of contradictory information exposure; only 10.4% reported no contradictory exposure.
Table 1.
Percentage reporting exposure to contradictory information about nutrition topics
| Level of exposure |
Red wine or other alcohol (N = 627) |
Fish (N = 628) |
Coffee (N = 628) |
Vitamins/ supplements (N = 625) |
|---|---|---|---|---|
|
|
||||
| % | % | % | % | |
| Not at all | 21.4 | 22.5 | 28.5 | 24.5 |
| A little | 25.7 | 24.7 | 23.1 | 19.8 |
| Some | 41.1 | 42.2 | 36.1 | 39.2 |
| A lot | 11.8 | 10.7 | 12.3 | 16.5 |
Associations between exposure and cognitive outcomes
As predicted in H1, exposure to contradictory nutrition information was positively associated with nutrition confusion (r = .10, p < .05). Table 2 shows that, even after adjusting for potential confounders, those who reported greater exposure also reported greater confusion. Additionally, H2 was supported: those who reported greater confusion reported higher levels of backlash (r = .51, p < .001). Again, this association remained significant after adjusting for potential confounders. Importantly, generalized mistrust was positively and significantly associated with both confusion and backlash, but adjusting for mistrust did not eliminate the hypothesized relationships.
Table 2.
Multivariable linear regression models of the relationship between media exposure to contradictory nutrition information, nutrition confusion, and nutrition backlash
| Nutrition confusion | Nutrition backlash | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Variable | B | SE | β | B | SE | β |
| Exposure to contradictory nutrition information |
0.13** | 0.05 | 0.11 | −0.004 | 0.04 | −0.004 |
| Nutrition confusion | -- | -- | -- | 0.40*** | 0.03 | 0.48 |
| Age | 0.01 | 0.01 | 0.04 | −0.03*** | 0.01 | −0.16 |
| Education | −0.50*** | 0.08 | −0.25 | −0.03 | 0.06 | −0.02 |
| Gender (female) | −0.28 | 0.30 | −0.04 | −0.58* | 0.23 | −0.09 |
| Race/ethnicity (non-Hispanic White) |
0.27 | 0.41 | 0.03 | 0.05 | 0.31 | 0.01 |
| Mistrust | 0.21*** | 0.05 | 0.18 | 0.18*** | 0.04 | 0.18 |
| Constant | 16.05*** | 1.27 | -- | 8.58*** | 1.07 | -- |
| R 2 | 0.11 | 0.32 | ||||
| N | 587 | 577 | ||||
|
| ||||||
p < .05;
p < .01;
p < .001
As evident in Table 2, exposure was not directly associated with backlash. Despite the absence of a direct association—which is not required to test for indirect effects (Hayes, 2009)—there was evidence of a significant indirect path from exposure to backlash through confusion (Table 2). As specified by the joint significance test, exposure (X) was significantly associated with confusion (M), and confusion (M) was significantly associated with backlash (Y), controlling for exposure (X) and covariates. Based on 5,000 bootstrap samples, the indirect effect of X on Y through M was not zero (95% bias-corrected bootstrap confidence interval = 0.0075–0.0871; point estimate = 0.0467). This analysis controlled for age, education, gender, race/ethnicity, and generalized mistrust.
Associations between cognitive outcomes and behavioral intentions
The two cognitive outcomes of interest, confusion and backlash, were negatively associated with intentions to engage in prevention behaviors, thus providing support for H3 and H4. Specifically, confusion was associated with lower intentions to consume fruits and vegetables (r = −.22, p < .001) and to exercise (r = −.22, p < .001), as was backlash (r = −.21, p < .001 and r = −.28, p < .001, respectively). These associations remained significant in controlled analyses, although their magnitude was relatively small (Table 3).
Table 3.
Multivariable linear regression models of the relationship between nutrition confusion, nutrition backlash, and intentions to adhere to healthy lifestyle recommendations (e.g., fruit and vegetable consumption, exercise)
| Intention to consume fruits and vegetables |
Intention to exercise | Intention to consume fruits and vegetables |
Intention to exercise | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Variable | B | SE | β | B | SE | β | B | SE | β | B | SE | β |
| Nutrition confusion | −0.07*** | 0.01 | −0.22 | −0.06*** | 0.01 | −0.19 | −0.05** | 0.01 | −0.16 | −0.03^ | 0.02 | −0.09 |
| Nutrition backlash | -- | -- | -- | -- | -- | -- | −0.05** | 0.02 | −0.14 | −0.09*** | 0.02 | −0.24 |
| Age | 0.01 | 0.003 | 0.07 | 0.001 | 0.003 | 0.01 | 0.004 | 0.003 | 0.05 | −0.001 | 0.003 | −0.02 |
| Education | −0.004 | 0.03 | −0.01 | 0.06* | 0.03 | 0.09 | −0.01 | 0.03 | −0.02 | 0.05^ | 0.03 | 0.07 |
| Gender (female) | 0.39*** | 0.09 | 0.17 | 0.15 | 0.10 | 0.06 | 0.37*** | 0.09 | 0.16 | 0.10 | 0.10 | 0.04 |
| Race/ethnicity (non-Hispanic White) |
−0.46*** | 0.12 | −0.15 | −0.09 | 0.13 | −0.03 | −0.43** | 0.12 | −0.14 | −0.05 | 0.13 | −0.02 |
| Mistrust | 0.01 | 0.02 | 0.03 | −0.01 | 0.02 | −0.03 | 0.02 | 0.02 | 0.06 | 0.01 | 0.02 | 0.02 |
| Constant | 4.24*** | 0.43 | -- | 4.16*** | 0.46 | -- | 4.69*** | 0.45 | -- | 4.95*** | 0.48 | -- |
| R2 | 0.10 | 0.06 | 0.11 | 0.10 | ||||||||
| N | 599 | 598 | 589 | 588 | ||||||||
|
| ||||||||||||
p <. 10;
p < .05;
p < .01;
p < .001
There also was evidence of significant paths from confusion to behavioral intentions through backlash. We have seen that confusion (X) was significantly associated with backlash (M; H2), and Table 3 shows that backlash (M) was associated with lower intentions to consume fruits and vegetables and to exercise (Y), controlling for confusion and covariates. Based on 5,000 bootstrap samples, the indirect effect on intention to consume fruits and vegetables was not zero (95% bias-corrected bootstrap confidence interval = −0.0335– −0.0062; point estimate = −0.0196), nor was the indirect effect on intention to exercise (95% bias-corrected bootstrap confidence interval = −0.0516– −0.0210; point estimate = −0.0358).
Discussion
The goal of this study was to move beyond assumptions of media effects—which have been common among nutrition researchers and clinicians—and instead empirically assess whether exposure to contradictory nutrition messages in the public information environment may have important negative effects. This article makes a theoretical case for the hypothesized set of relationships by turning to the decision theory concept of ambiguity (Ellsberg, 1961). Overall, results show that a majority of U.S. adults in this sample reported coming across conflicting information about nutrition topics in the media. Those who reported greater exposure to contradictory information also reported greater levels of nutrition confusion. In addition, greater confusion was associated with greater backlash, and there was evidence of a significant indirect path linking exposure to backlash through confusion. Lastly, confusion and backlash were negatively associated with intentions to engage in healthy lifestyle behaviors.
Taken together, this set of findings suggests that there may be important carryover effects of contradictory message exposure and its associated cognitions. Exposure to conflicting information on the health benefits and risks of, for example, wine, fish, and coffee consumption was associated with confusion about what foods are best to eat and the belief that nutrition scientists keep changing their minds. We found evidence that confusion and backlash beliefs, in turn, may lead people to doubt nutrition and health recommendations more generally—including those that are not surrounded by conflict and controversy (e.g., fruit and vegetable consumption, exercise). Crucially, then, natural media exposure to contradictory nutrition information has the potential to undermine the success of healthy eating campaigns and interventions. If people notice contradictory information about wine, fish, and other topics and, ultimately, begin to doubt nutrition research and recommendations, then they might be less receptive to subsequent nutrition and non-nutrition-related health campaign messages—perhaps even rejecting them altogether. That said, this study provides only initial support for this idea. While carryover effects could be explained by excitation transfer and priming of negative affect, greater theoretical and empirical attention to such effects is advised.
Several study limitations should be noted. The use of cross-sectional data prevents us from speaking to the causal direction of any associations found. Reverse causation is a possibility: those who have poor health behaviors (or poor behavioral intentions) could be rationalizing their behavior by blaming the media for containing contradictory information. Although this pathway cannot be ruled out using the current data, this explanation is less likely than the pathways laid out here. A separate validity study (Nagler & Hornik, 2012) found evidence that people can distinguish between contradictory nutrition topics (e.g., red wine or other alcohol, fish) and those about which there is no conflicting information (e.g., mushrooms, poppy seeds). In other words, there was no evidence of a general tendency to report contradictions. If people were rationalizing their behavior, then it is unlikely that they would demonstrate such accuracy and discrimination in topic recall; rather, we would expect an overall tendency to report contradictions. Ultimately, establishing cross-sectional associations was an important first step, given the paucity of empirical work on contradictory health messages. This study’s findings offer a foundation for future research focused on strengthening causal inference, whether through an experimental or longitudinal survey design.
In addition, analyses adjusted for several sociodemographic characteristics and generalized mistrust, but there may be other important unmeasured confounders. Although survey space constraints limited the number of potential covariates that could be assessed, one potential threat to inference was addressed: that greater exposure to health media accounts for the observed association between contradictory information exposure and confusion. In a post-hoc analysis (Appendix), the latter association remained significant even after adjusting for health media exposure, suggesting that the association is specific to contradictory information exposure. Thus, although several recent studies found that general and/or health media exposure was linked to perceived ambiguity about cancer prevention recommendations (Han et al., 2009) and cancer fatalism (Lee & Niederdeppe, 2010; Niederdeppe, Fowler, Goldstein, & Pribble, 2010), the current study suggests that contradictory exposure in particular may be a stronger predictor of such outcomes—a prediction that is consistent with Ellsberg’s argument that ambiguity is likely when “available information is… highly conflicting” (1961, pp. 660-661).
Appendix.
Bivariate and multivariable linear regression models of the relationship between media exposure to contradictory nutrition information, health media exposure, and nutrition confusion
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | β | B | SE | β | B | SE | β |
| Constant | 15.22*** | 0.49 | - | 15.63*** | 0.60 | - | 15.94*** | 1.33 | - |
| Exposure to contradictory nutrition information |
0.12* | 0.05 | 0.10 | 0.14** | 0.05 | 0.12 | 0.13** | 0.05 | 0.12 |
| Health media exposure | −0.06 | 0.05 | −0.05 | −0.02 | 0.05 | −0.02 | |||
| Age | 0.01 | 0.01 | 0.04 | ||||||
| Education | −0.48*** | 0.08 | −0.24 | ||||||
| Gender (female) | −0.19 | 0.31 | −0.02 | ||||||
| Race/ethnicity (non-Hispanic White) |
0.25 | 0.42 | 0.02 | ||||||
| Mistrust | 0.22*** | 0.05 | 0.18 | ||||||
| R2 | 0.01 | 0.01 | 0.11 | ||||||
| N | 598 | 578 | 570 | ||||||
|
| |||||||||
p < .05;
p < .01;
p < .001
Note. To assess health media exposure, respondents were asked, “About how often have you... [read health sections of newspapers or general magazines]; [read special health or medical magazines or newsletters]; [watched health segments of local or national television news programs]; [watched television shows that address health issues (e.g., shows that focus on doctors or hospitals)]; [read health information on the Internet when you were not trying to find out about a specific health concern] in the past 30 days?” Response options were “Not at all,” “Less than once per week,” “Once per week,” and “A few times a week” (range = 1–4). An index of health media exposure was created by summing the five items (range = 5–20; M = 10.4; SD = 3.5). Model 1 = bivariate association of contradictory information exposure and confusion. Model 2 = association of contradictory information exposure and confusion, adjusting for health media exposure. Model 3 = association of contradictory information exposure and confusion, adjusting for health media exposure, age, education, gender, race/ethnicity, and generalized mistrust.
In sum, this study provides initial empirical support for the concern that exposure to contradictory health information may have adverse effects on cognitions and behaviors. In this way, it lays a foundation for the future study of contradictory messages in the health domain—an underexplored, but increasingly important, research arena. There are several key directions for future research. For example, the exposure measure did not distinguish among media sources. These could be separated out in future studies, allowing researchers to identify specific sources that might be important vehicles of contradictory information (e.g., women’s or health magazines, national news magazines such as Newsweek and Time, blogs, local television news, talk shows such as Oprah). In addition, the exposure measure could be adapted to study contradictory message exposure from medical (e.g., physicians, allied health professionals) and interpersonal sources (e.g., friends, family, co-workers). The relative contribution of media, medical, and interpersonal exposure to confusion, backlash, and behavioral intentions could be explored in future research. Exposure also could be tested in other health contexts—perhaps most notably, cancer screening, given the recent debates and subsequent media coverage surrounding mammography and prostate-specific antigen (PSA) testing (e.g., Harris, 2011; Hobson, 2009; Kolata, 2009; U.S. Preventive Services Task Force (USPSTF), 2009; USPSTF, 2011). Lastly, carryover effects and their implications for public health communication campaigns deserve additional attention.
Acknowledgments
This study was supported by a grant from the National Cancer Institute (NCI) (P20-CA095856-08). This publication’s contents are solely the responsibility of the author and do not necessarily represent the official views of NCI. Funding support for R.H.N. was also provided through NCI by the Harvard Education Program in Cancer Prevention and Control (5 R25-CA057711-18). The data were provided by the Annenberg National Health Communication Survey supported, in part, by the Annenberg Trust at Sunnylands. Thanks to Robert Hornik, Joseph Cappella, Michael Delli Carpini, the late Martin Fishbein, and Cabral Bigman for their helpful feedback during earlier stages of this research.
References
- American Dietetic Association Position of the American Dietetic Association: Total diet approach to communicating food and nutrition information. Journal of the American Dietetic Association. 2007;107:1224–1232. doi: 10.1016/j.jada.2007.05.025. [DOI] [PubMed] [Google Scholar]
- Angell M, Kassirer JP. Clinical research: What should the public believe? New England Journal of Medicine. 1994;331:189–190. doi: 10.1056/NEJM199407213310309. [DOI] [PubMed] [Google Scholar]
- Annenberg National Health Communication Survey (ANHCS) ANHCS overview. 2007 doi: 10.1080/10410236.2016.1214220. Retrieved October 18, 2011, from http://anhcs.asc.upenn.edu/ [DOI] [PubMed]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Basu AJ, Hogard E. Fit for public consumption? An exploratory study of the reporting of nutrition research in UK tabloids with regard to its accuracy, and a preliminary investigation of public attitudes towards it. Public Health Nutrition. 2008;11:1124–1131. doi: 10.1017/S1368980007001565. [DOI] [PubMed] [Google Scholar]
- Boyington JEA, Schoster B, Martin KR, Shreffler J, Callahan LF. Perceptions of individual and community environmental influences on fruit and vegetable intake, North Carolina, 2004. Preventing Chronic Disease. 2009;6 Retrieved October 1, 2011, from http://www.cdc.gov/pcd/issues/2009/jan/07_0168.htm. [PMC free article] [PubMed] [Google Scholar]
- Boyle P, Boffetta P, Autier P. Diet, nutrition and cancer: Public, media and scientific confusion. Annals of Oncology. 2008;19:1665–1667. doi: 10.1093/annonc/mdn561. [DOI] [PubMed] [Google Scholar]
- Davis JA, Smith TW, Marsden PV. General social surveys, 1972-2008: cumulative codebook. National Opinion Research Center; Chicago: 2009. Retrieved September 14, 2011, from http://www3.norc.org/GSS+Website/Documentation/ [Google Scholar]
- Department of Health and Human Services Funding Opportunity Announcement: Impact of health communication strategies on dietary behaviors (R21) 2008 Retrieved September 15, 2011, from http://grants.nih.gov/grants/guide/pa-files/PA-08-240.html.
- Diekman C, Malcolm K. Consumer perceptions and insights on fats and fatty acids: Knowledge on the quality of diet fat. Annals of Nutrition & Metabolism. 2009;54(Suppl. 1):25–32. doi: 10.1159/000220824. [DOI] [PubMed] [Google Scholar]
- Dorey E, McCool J. The role of the media in influencing children’s nutritional perceptions. Qualitative Health Research. 2009;19:645–654. doi: 10.1177/1049732309334104. [DOI] [PubMed] [Google Scholar]
- Drummond S. Bringing the sense back into healthy eating advice. Journal of Family Health Care. 2006;16:143–145. [PubMed] [Google Scholar]
- Dye CJ, Cason KL. Perceptions of older, low-income women about increasing intake of fruits and vegetables. Journal of Nutrition for the Elderly. 2005;25:21–41. doi: 10.1300/J052v25n01_04. [DOI] [PubMed] [Google Scholar]
- Ellsberg D. Risk, ambiguity, and the Savage axioms. Quarterly Journal of Economics. 1961;75:643–669. [Google Scholar]
- Evans WA, Krippendorf M, Yoon JH, Posluszny P, Thomas S. Science in the prestige and national tabloid presses. Social Science Quarterly. 1990;71:105–117. [Google Scholar]
- Fennis BM, Bakker AB. “Stay tuned—we will be back right after these messages”: Need to evaluate moderates the transfer of irritation in advertising. Journal of Advertising. 2001;30:15–25. [Google Scholar]
- Fineberg HV, Rowe S. Improving public understanding: Guidelines for communicating emerging science on nutrition, food safety, and health. Journal of the National Cancer Institute. 1998;90:194–199. doi: 10.1093/jnci/90.3.194. [DOI] [PubMed] [Google Scholar]
- Goldberg JP. Nutrition and health communication: the message and the media over half a century. Nutrition Reviews. 1992;50:71–77. doi: 10.1111/j.1753-4887.1992.tb01272.x. [DOI] [PubMed] [Google Scholar]
- Goldberg JP, Hellwig JP. Nutrition research in the media: The challenge facing scientists. Journal of the American College of Nutrition. 1997;16:544–550. [PubMed] [Google Scholar]
- Goldberg JP, Sliwa SA. Communicating actionable nutrition messages: Challenges and opportunities. Proceedings of the Nutrition Society. 2011;70:26–37. doi: 10.1017/S0029665110004714. [DOI] [PubMed] [Google Scholar]
- Greiner A, Smith KC, Guallar E. Something fishy? News media presentation of complex health issues related to fish consumption guidelines. Public Health Nutrition. 2010;13:1786–1794. doi: 10.1017/S1368980010000923. [DOI] [PubMed] [Google Scholar]
- Han PKJ, Kobrin SC, Klein WMP, Davis WW, Stefanek M, Taplin SH. Perceived ambiguity about screening mammography recommendations: Association with future mammography uptake and perceptions. Cancer Epidemiology, Biomarkers & Prevention. 2007;16:458–466. doi: 10.1158/1055-9965.EPI-06-0533. [DOI] [PubMed] [Google Scholar]
- Han PKJ, Moser RP, Klein WMP. Perceived ambiguity about cancer prevention recommendations: Relationship to cancer preventability, risk, and worry. Journal of Health Communication. 2006;11:51–69. doi: 10.1080/10810730600637541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Moser RP, Klein WMP. Perceived ambiguity about cancer prevention recommendations: Associations with cancer-related perceptions and behaviors in a U.S. population survey. Health Expectations. 2007;10:321–336. doi: 10.1111/j.1369-7625.2007.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Moser RP, Klein WMP, Beckjord EB, Dunlavy AC, Hesse BW. Predictors of perceived ambiguity about cancer prevention recommendations: Sociodemographic factors and mass media exposures. Health Communication. 2009;24:764–772. doi: 10.1080/10410230903242242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris G. U.S. panel says no to prostate screening for healthy men. New York Times. 2011 Oct 6; Retrieved October 7, 2011, from http://www.nytimes.com.
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. [Google Scholar]
- Hobson K. Prostate, ovarian cancer screening: When to test? Not so clear. U.S. News & World Report. 2009 Mar 18; Retrieved October 8, 2011, from http://health.usnews.com.
- Houn F, Bober MA, Huerta EE, Hursting SD, Lemon S, Weed DL. The association between alcohol and breast cancer: Popular press coverage of research. American Journal of Public Health. 1995;85:1082–1086. doi: 10.2105/ajph.85.8_pt_1.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM SPSS Statistics . PASW Statistics GradPack. Vol. 18. SPSS Inc; Chicago: 2010. [Google Scholar]
- Jarvis WBG, Petty RE. The need to evaluate. Journal of Personality and Social Psychology. 1996;70:172–194. [Google Scholar]
- Jensen JD, Carcioppolo N, King AJ, Bernat JK, Davis L, Yale R, Smith J. Including limitations in news coverage of cancer research: Effects of news hedging on fatalism, medical skepticism, patient trust, and backlash. Journal of Health Communication. 2011;16:486–503. doi: 10.1080/10810730.2010.546491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson-Taylor WL, Yaroch AL, Krebs-Smith SM, Rodgers AB. What can communication science tell us about promoting optimal dietary behavior? Journal of Nutrition Education and Behavior. 2007;39(Suppl. 1):S1–S4. doi: 10.1016/j.jneb.2006.05.011. [DOI] [PubMed] [Google Scholar]
- Kolata G. Panel urges mammograms at 50, not 40. New York Times. 2009 Nov 16; Retrieved September 18, 2011, from http://www.nytimes.com.
- Kushi LH. Vitamin E and heart disease: A case study. American Journal of Clinical Nutrition. 1999;69:1322S–1329S. doi: 10.1093/ajcn/69.6.1322S. Suppl. [DOI] [PubMed] [Google Scholar]
- Lee CJ, Niederdeppe J. Genre-specific cultivation effects: lagged associations between overall TV viewing, local TV news viewing, and fatalistic beliefs about cancer prevention. Communication Research. 2010 doi: 10.1177/0093650210384990. DOI: 10.1177/0093650210384990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding, and suppression effect. Prevention Science. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meissner HI, Rimer BK, Davis WW, Eisner EJ, Siegler IC. Another round in the mammography controversy. Journal of Women’s Health. 2003;12:261–276. doi: 10.1089/154099903321667609. [DOI] [PubMed] [Google Scholar]
- Miller JD. Public understanding of, and attitudes toward, scientific research: What we know and what we need to know. Public Understanding of Science. 2004;13:273–294. [Google Scholar]
- Nagler RH. Steady diet of confusion: Contradictory nutrition messages in the public information environment. 2010 Unpublished doctoral dissertation, Annenberg School for Communication, University of Pennsylvania, Philadelphia, PA. [Google Scholar]
- Nagler RH, Hornik RC. Measuring media exposure to contradictory health information: A comparative analysis of four potential measures. Communication Methods and Measures. 2012;6:56–75. doi: 10.1080/19312458.2011.651348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelkin D. Selling science: How the press covers science and technology. W.H. Freeman; New York, NY: 1995. [Google Scholar]
- Niederdeppe JD, Fowler EF, Goldstein K, Pribble J. Does local television news coverage cultivate fatalistic beliefs about cancer prevention? Journal of Communication. 2010;60:230–253. doi: 10.1111/j.1460-2466.2009.01474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiology, Biomarkers & Prevention. 2007;16:998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- Patterson RE, Satia JA, Kristal AR, Neuhouser ML, Drewnowski A. Is there a consumer backlash against the diet and health message? Journal of the American Dietetic Association. 2001;101:37–41. doi: 10.1016/S0002-8223(01)00010-4. [DOI] [PubMed] [Google Scholar]
- Pellechia MG. Trends in science coverage: A content analysis of three U.S. newspapers. Public Understanding of Science. 1997;6:49–68. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rimer BK, Halabi S, Strigo TS, Crawford Y, Lipkus IM. Confusion about mammography: Prevalence and consequences. Journal of Women’s Health & Gender-Based Medicine. 1999;8:509–520. doi: 10.1089/jwh.1.1999.8.509. [DOI] [PubMed] [Google Scholar]
- Roskos-Ewoldsen DR, Roskos-Ewoldsen B, Dillman Carpentier F. Media priming: an updated synthesis. In: Bryant J, Oliver MB, editors. Media effects: advances in theory and research. 3rd Taylor & Francis; New York: 2009. pp. 74–93. [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Smith KC, Kromm EE, Klassen AC. Print news coverage of cancer: What prevention messages are conveyed when screening is newsworthy? Cancer Epidemiology. 2010;34:434–441. doi: 10.1016/j.canep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- Squiers LB, Holden DJ, Dolina SE, Kim AE, Bann CM, Renaud JM. The public’s response to the U.S. Preventive Services Task Force’s 2009 recommendations on mammography screening. American Journal of Preventive Medicine. 2011;40:497–504. doi: 10.1016/j.amepre.2010.12.027. [DOI] [PubMed] [Google Scholar]
- Tankard JW, Ryan M. News source perceptions of accuracy of science coverage. Journalism Quarterly. 1974;51:219–225. [Google Scholar]
- Taplin SH, Urban N, Taylor VM, Savarino J. Conflicting national recommendations and the use of screening mammography: Does the physician’s recommendation matter? Journal of the American Board of Family Medicine. 1997;10:88–95. [PubMed] [Google Scholar]
- Taubes G. Do we really know what makes us healthy? New York Times Magazine. 2007 Sep 16; Retrieved September 16, 2011, from http://www.nytimes.com.
- U.S. Preventive Services Task Force Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force Screening for prostate cancer: U.S. Preventive Services Task Force Recommendation Statement Draft. 2011 Retrieved December 6, 2011, from http://www.uspreventiveservicestaskforce.org/uspstf12/prostate/draftrecprostate.htm.
- Vardeman JE, Aldoory L. A qualitative study of how women make meaning of contradictory media messages about the risks of eating fish. Health Communication. 2008;23:282–291. doi: 10.1080/10410230802056396. [DOI] [PubMed] [Google Scholar]
- Zillman D. Transfer of excitation in emotional behavior. In: Petty RE, Cacioppo JT, editors. Social psychophysiology: A sourcebook. Guilford Press; New York: 1983. pp. 215–240. [Google Scholar]


