Abstract
Dental caries is a common disease in children of all ages. It is desirable to know whether children with primary, mixed and permanent dentitions share risk factors for cavitated and non-cavitated caries.
Objective
To assess the longitudinal associations between caries outcomes and modifiable risk factors.
Methods
One hundred and fifty-six children in the Iowa Fluoride Study met inclusion criteria of three dental examinations and caries-related risk factor assessments preceding each examination. Surface-specific counts of new non-cavitated caries and cavitated caries at the primary (Exam 1: age 5), mixed (Exam 2: age 9) and permanent (Exam 3: age 13) dentition examinations were outcome variables. Explanatory variables were caries-related factors, including averaged beverage exposure frequencies, toothbrushing frequencies, and composite water fluoride levels collected from 3–5, 6–8, and 11–13 years, dentition category, socioeconomic status and gender. Generalized linear mixed models (GLMMs) were used to explore the relationships between new non-cavitated or cavitated caries and caries-related variables.
Results
Greater frequency of 100% juice exposure was significantly associated with fewer non-cavitated and cavitated caries surfaces. Greater toothbrushing frequency and high SES were significantly associated with fewer new non-cavitated caries. Children had significantly more new cavitated caries surfaces at the mixed dentition examination than at the primary and permanent dentition examinations.
Conclusions
There were common caries-related factors for more new non-cavitated caries across the three exams, including less frequent 100% juice exposure, lower toothbrushing frequency and lower socioeconomic status. Less frequent 100% juice exposures might be associated with higher exposures to several other cariogenic beverages.
Keywords: dental caries, cavitated caries, non-cavitated caries, beverage, child, longitudinal study
Introduction
Dental caries is a multifactorial disease that occurs in the complex environment of the oral cavity. Fermentable carbohydrates are known substrates for acidogenesis by cariogenic bacteria. The associations between dental caries and dietary risk factors have been examined for several decades. Non-dietary caries-related factors including fluoride, plaque/cariogenic bacteria, oral hygiene care/toothbrushing, demographic characteristics and previous caries experience also have been studied. Studies assessing caries risk factors have reported different results, due in part to different designs, analytical methods, subjects’ ages and definitions of risk factors and caries.
Among studies assessing the associations between dental caries and dietary exposures in children, most studies investigated associations between cavitated caries experience and specific types of foods and beverages at one specific age or in one specific age group (1–7). From a public health perspective, finding consistent caries-associated factors would be important for developing and implementing caries preventive strategies. Preventive measures that can be used not only for people of one specific age range would be more universal, and could thereby reduce screenings and reach a broad range of populations.
Longitudinal study designs with multiple dental exams allow us to assess caries-associated factors across age groups. Moreover, longitudinal studies provide data that can be analyzed using a repeated measures (correlated data) framework, which reduces unobserved (“not able to be assessed or not in the study”) individual differences in the study. This analytical approach usually allows statistical inference to be made with fewer subjects, which increases the statistical power of studies with similar numbers of subjects in long-term follow-up longitudinal designs compared with cross-sectional designs.
We used longitudinal data from the Iowa Fluoride Study to assess caries risk factors separately for non-cavitated caries and cavitated caries in children across the primary (Exam 1), mixed (Exam 2) and permanent (Exam 3) dentitions. These analyses assessed the associations between dental caries outcomes and modifiable risk factors, including beverage exposure frequencies, toothbrushing, and fluoride exposures.
Methods
The Iowa Fluoride Study recruited mothers and newborns from 8 Iowa hospital postpartum units from 1992–1995 and has been collecting fluoride, dietary and other related information associated with dental fluorosis and caries since children were 1.5 months old. This study was approved by the Human Subjects Review Committee of the University of Iowa initially and at least annually thereafter. Parental informed consent and subjects’ assent were obtained separately for each dental exam. Dietary diaries were sent every 1.5 to 6 months until age 8.5 years, and separate questionnaires assessing dietary, toothbrushing and fluoride were sent until age 13 years. Dental examinations were conducted at approximately ages 5, 9 and 13. Cohort children (n=156) who had all 3 dental examinations of the primary (Exam 1), mixed (Exam 2) and permanent (Exam 3) dentition and had at least 2 abstracted dietary diaries during the age 3–5 and 6–8 years periods and at least 2 questionnaires during the age 11–13 years period were included in this analysis.
Dietary Information
Diaries
Three-day dietary diaries were sent to parents every 1.5 to 6 months from age 1.5 months to 8.5 years to assess the food and beverage consumptions for two weekdays and one weekend day. Specific information regarding types of items consumed by children and details of consumption were collected. The yearly dietary diaries at ages 3, 4 and 5 years (for the age 3 to 5 period) and 6, 7 and 8 years (for the age 6 to 8 period) were abstracted by a trained registered dietitian or diet technician to provide dietary exposure frequency (occasions per day) of specific food and beverage categories. If the particular yearly diary was missing, then substitution was made using the diary either 4 or 6 months preceding (or succeeding, if necessary) the yearly diary. More detailed information concerning the dietary diary data collection has been published previously (8). Since response rates to the dietary diaries decreased over time, the protocol was changed after age 8.5 years, at which time the dietary diaries were discontinued and replaced with a detailed beverage consumption questionnaire.
Questionnaires
The new detailed questionnaires have been sent to parents every 6 months since age 9 years to assess the exposure frequencies (occasions per day) of specific beverage categories, as well as other information. The questionnaires returned at ages 11, 11.5, 12, 12.5 and 13 years were used for the age 11- to 13-year period.
Beverage Exposure Variables
For these analyses, the beverage exposure data were compiled for the following six categories: milk, water by itself, reconstituted sugared beverage from powder (i.e. powdered beverages), regular (sugared) soda pop, 100% juice, and juice drinks (fruit juice with added sugars) by type of beverage and fermentable carbohydrate type. Uncommon beverage categories (i.e., those for which less than 25% of children had any exposure during each period) were excluded from the analysis, including sport drinks and diet soda pop. Within each exposure period (3–5, 6–8 and 11–13 years), the frequencies of beverage consumption were averaged for each child. Each subject had 3 sets of explanatory data, one for each exposure period. The 3 sets of explanatory variables were not averaged, but were used as concurrent variables for each of the dental outcomes (3–5 year exposures for Exam 1 outcome, 6–8 year for Exam 2 outcome and 11–13 year for Exam 3 outcome). These period-specific exposure frequencies then were categorized into low, middle and high frequency categories using the approximate 25th and 75th percentiles of exposure frequency for each beverage category and exposure period. However, due to the prevalence of tied values, children were not always divided exactly into 25%, 50% and 25% for low, middle and high categories of exposure, respectively, as targeted.
Fluoride and SES
Toothbrushing frequency data were collected using the same questions on both the detailed questionnaires from age 6 weeks to 8.5 years and the questionnaires used since age 9 years (9). Composite water fluoride levels were determined at all time points as weighted averages of the main sources of water (i.e., home/school, bottled/filtered/tap water) at each time point (10). For those using public water without filtration, water fluoride information was obtained from the Iowa State Health Department. For individual water sources or public water with filtration, water samples were collected and fluoride levels determined by individual fluoride assay with a fluoride-ion specific electrode (10). All available toothbrushing frequency and composite water fluoride level data for each period (3–5, 6–8 and 11–13 years) were averaged separately for each child. Questionnaire reliability was assessed on a sample by telephone about 7–10 days after receipt of the questionnaires for selected questions, including toothbrushing frequency. Reliability results (weighted kappa) for toothbrushing frequency were 0.75, 0.81 and 0.73 for ages 3–5, 6–8 and 11–13 years, respectively. Socioeconomic status (SES) was classified into low, middle and high based on family income and mother’s education level information that was collected at recruitment (11).
Dental Caries Information
Dental caries examinations were conducted by trained examiners at about age 5 (Exam 1: primary dentition), age 9 (Exam 2: mixed dentition) and age 13 (Exam 3: permanent dentition) using non-cavitated/cavitated criteria (12) modified from Pitt’s criteria (13). The inter-examiner reliability results at the surface-level using weighted kappas to assess consistency of classification (sound, d1/D1 (non-cavitated caries), or d2+f/D2+F (cavitated/filled caries)) for the primary, mixed and permanent dentitions were 0.81, 0.82 and 0.58, respectively. The outcome variables were calculated using surface specific transitions based on the changes of caries status of specific tooth surfaces for each individual child between two consecutive examinations (person-level counts of caries increments).
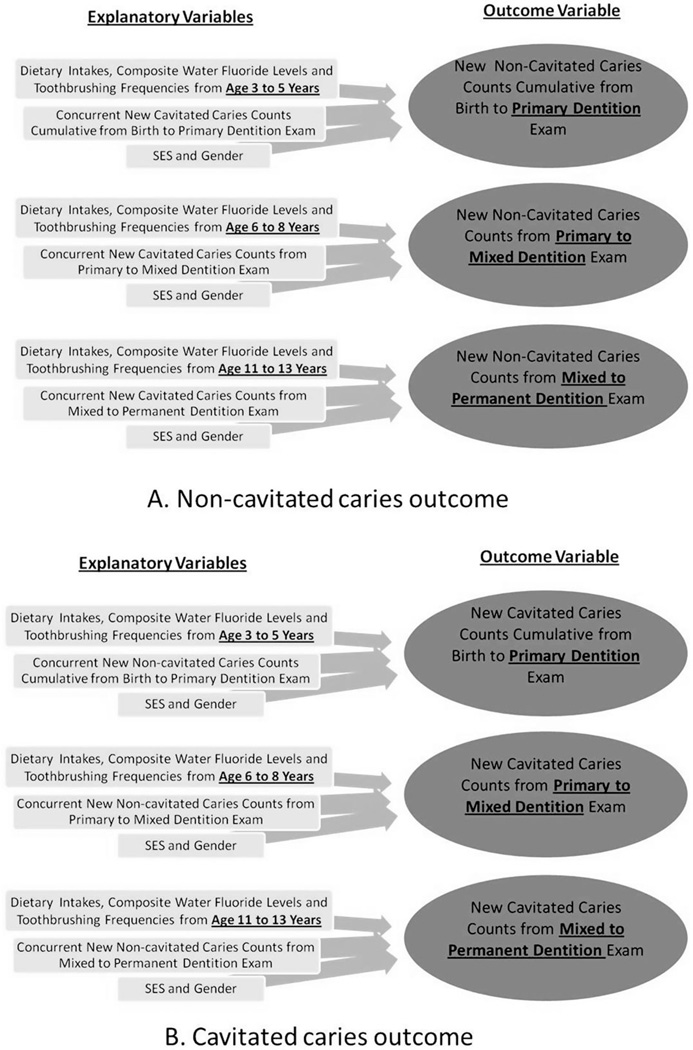
For Exam 1, counts of lesions of non-cavitated and cavitated caries/filled at the age 5 examination were used as new non-cavitated and new cavitated caries, respectively. For Exams 2 and 3, transitions of diagnosis from sound to non-cavitated lesions were counted as new non-cavitated caries, and from sound/non-cavitated caries lesions to cavitated caries or filled lesions were counted as new cavitated caries. Surface-specific transitions of caries status (sound, d1/D1, or d2+f/D2+F) from Exam 1 to Exam 2 were counted as new caries for the Exam 2 outcomes (Figure 1). Transitions of caries status on specific surfaces from Exam 2 to Exam 3 were counted as new caries for the Exam 3 outcomes.
Figure 1.
Diagram showing the associations between explanatory variables and outcome variables for each individual period (a. for non-cavitated caries outcome and b. for cavitated caries outcome).
The counts of new non-cavitated and cavitated caries served as the dependent variables. All surfaces present at Exam 1 were counted as surfaces at risk for both non-cavitated and cavitated caries for the Exam 1 outcomes. For later exams, surfaces that were sound at the previous exam plus newly-erupted surfaces were counted as surfaces at risk for non-cavitated caries. Surfaces that were sound or d1/D1 at the previous exam and newly-erupted surfaces were counted as surfaces at risk for cavitated caries. The counts of surfaces at risk served as offset variables. The offset variables, representing the number of surfaces at risk for non-cavitated or cavitated caries, were featured in all models. Moreover, the proportion of concurrent non-cavitated caries surfaces to surfaces at risk was a control variable in the multivariable regression models for the cavitated caries outcome, while the proportion of concurrent cavitated caries surfaces to surfaces at risk was a control variable for the non-cavitated caries outcome.
Analytical Methods
The nature of longitudinal data results in correlated data. This analysis used a repeated measures modeling framework that accounts for correlated outcomes from the same individual. The explanatory variables from ages 3 to 5 years, 6 to 8 years and 11 to 13 years were considered for associations with new cavitated and non-cavitated caries recorded at Exam 1 (primary dentition), Exam 2 (mixed dentition) and Exam 3 (permanent dentition), respectively (Figure 1).
Descriptive statistics of dental caries outcomes, beverage exposure variables and other caries-related factors for each individual period were assessed. Generalized linear mixed models (GLMMs) based on the negative binomial distribution were used to explore separately the relationships between new non-cavitated or cavitated caries and caries-related variables: frequency of beverage exposures, tooth brushing frequency, composite water fluoride level, SES, gender, and types of dentition. The log link function was used, and accordingly, the offset variable (representing counts of surfaces at risk) was log transformed. With this formulation, one can view the GLMMs as modeling the proportion of new non-cavitated or cavitated caries surfaces to surfaces at risk.
Random effects were included in each GLMM to account for the correlation among the longitudinal outcomes for each subject. The random effects were assumed to be independent between subjects and to have a constant variance. The resulting subject-specific GLMM was fit using the GLIMMIX (Generalized LInear Models MIXed) procedure in SAS 9.2, which employs a pseudo-likelihood fitting technique.
First, univariable regression models were developed separately for each beverage and other caries-related variable. Only variables with p-values <0.15 from the univariable regressions were considered further for inclusion in the multivariable model. The pairwise correlations between pairs of continuous variables comprised of selected beverage variables and other related factors were examined. For the moderate- to high-correlation pairs (Pearson-coefficients >0.3), the plan was to retain only the variable exhibiting the stronger association with caries in the multivariable regression analysis. However, there were no occurrences of such correlations of pairs of variables. All two-way interactions among these considered beverage variables and other caries-related factors were then assessed, except for those based on a product of two continuous variables. The considered variables and interaction terms with p-values <0.15 were included in the formulation of the initial multivariable model (along with the main effects corresponding to any interaction terms). A backward elimination procedure was performed to determine the final model, where each step in the procedure was specified only after evaluating the fitted model resulting from the previous step. The exam (time/age/dentition type) variable was a control (covariate), and was retained in the model regardless of the p-value to account for different ages and dental and oral environments at each examination. For other variables, the variable that had the largest p-value was removed from the model sequentially (except for main effects corresponding to interactions that were retained in the model). This step was repeated until all the variables remaining in the model were significant at the 0.05 level. The offset variable, representing the number of surfaces at risk for non-cavitated and cavitated caries, was featured in all models. All analyses were conducted using SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
One hundred and fifty-six children (45% female) were included in these analyses. Most children were of high or middle SES (37.8% and 34.4%, respectively). Mean ages at the primary, mixed and permanent dentition examinations were 5.15 ±0.38, 9.17 ±0.76 and 13.20 ±0.35 years, respectively.
Table 1 shows the descriptive analysis of the dental caries at each of the three exams. For the Exam 1, fewer children had non-cavitated caries (21.15%) when compared with the Exam 2 (39.10%) and Exam 3 (35.90%). The mean number of new non-cavitated caries surfaces among all children for Exam 1 (0.56) was lower than those for the Exam 2 (0.99) and Exam 3 (0.87). However, the mean number of new non-cavitated caries surfaces among only those children with new non-cavitated lesions for Exam 1 (2.67) was slightly greater than those for Exam 2 (2.54) and Exam 3 (2.41). For Exam 2, about 54% of the children had new cavitated caries vs. 26–28% for Exams 1 and 3. However, among those with new cavitated caries, the mean numbers of newly affected surfaces were 5.0 (Exam 1), 5.5 (Exam 2) and 2.4 (Exam 3). Table 1 also presents means of surfaces at risk for both non-cavitated and cavitated caries by examinations. More details of the descriptive information of counts of surfaces with new caries by specific tooth types and surface types are presented in Table 2.
Table 1.
Means (±SD) of caries counts and surfaces at risk at each of the three examinations (156 subjects)
| Parameter | Primary Dentition (Exam 1) |
Mixed Dentition (Exam 2) |
Permanent Dentition (Exam 3) |
|---|---|---|---|
| % with New Non-cavitated Caries | 21.15% | 39.10% | 35.90% |
| New Non-cavitated Caries (Surfaces)* | |||
| • All children | 0.56 ±1.65 | 0.99 ±1.94 | 0.87 ±1.77 |
| • Among children with new cavitated caries | 2.67 ±2.73 | 2.54 ±2.40 | 2.41 ±2.25 |
| % with New Cavitated Caries | 26.28% | 53.85% | 27.56% |
| New Cavitated Caries (Surfaces)* | |||
| • All children | 1.30 ±3.42 | 2.97 ±4.45 | 0.67 ±1.42 |
| • Among children with new cavitated caries | 4.95 ±5.17 | 5.52 ±4.77 | 2.42 ±1.76 |
| Surfaces at Risk for Non-cavitated Caries** | 86.81 ±3.78 | 110.73 ±5.26 | 123.01 ±11.83 |
| Surfaces at Risk for Cavitated Caries*** | 86.81 ±3.78 | 111.22 ±5.27 | 123.53 ±11.70 |
New counts determined though age 5 for primary dentition exam outcomes, from primary to mixed dentition for mixed dentition exam outcomes and from mixed to permanent dentition for permanent dental exam outcomes.
Sound at previous exam.
Sound or non-cavitated caries at previous exam.
Note: new cavitated caries included both untreated and treated cavitated lesions.
Table 2.
Total counts of surfaces with new non-cavitated and new cavitated caries by specific tooth types and surface types (156 subjects)
| Tooth (Surface Types) | Counts of Surfaces | |||||
|---|---|---|---|---|---|---|
| Primary Dentition Phase |
Mixed Dentition Phase |
Permanent Dentition Phase |
||||
| New Non- Cavitated Caries |
New Cavitated Caries |
New Non- Cavitated Caries |
New Cavitated Caries |
New Non- Cavitated Caries |
New Cavitated Caries |
|
| Primary Incisor (All) | 7 | 14 | 0 | 2 | ||
| Primary Canine (All) | 15 | 10 | 4 | 5 | ||
| 1st Primary Molar (B/L/M/D) | 10 | 57 | 2 | 111 | ||
| 1st Primary Molar (Occlusal) | 5 | 39 | 6 | 82 | ||
| 2nd Primary Molar (B/L/M/D) | 24 | 25 | 8 | 59 | ||
| 2nd Primary Molar (Occlusal) | 16 | 33 | 22 | 46 | ||
| Permanent Incisor (All) | 6 | 1 | 27 | 7 | ||
| Permanent Canine (All) | 1 | 0 | 14 | 1 | ||
| Premolar (B/L/M/D) | 0 | 0 | 15 | 1 | ||
| Premolar (Occlusal) | 0 | 0 | 1 | 5 | ||
| 1st Permanent Molar (B/L/M/D) | 55 | 0 | 17 | 20 | ||
| 1st Permanent Molar (Occlusal) | 26 | 47 | 27 | 44 | ||
| 2nd Permanent Molar (B/L/M/D) | 19 | 5 | ||||
| 2nd Permanent Molar (Occlusal) | 15 | 21 | ||||
Table 3 presents ranges of mean exposure frequency of each specific beverage category for low, middle and high levels at each of the three individual periods. The table also provides mean (SD) d1s/D1s and d2fs /D2Fs increments by beverage categories for each exposure level at each of the three periods. These summary statistics illustrate crude period-specific associations between the beverage variables and the caries outcomes.
Table 3.
Mean (SD) d1s/D1s and d2fs /D2Fs increments by categories of daily beverage exposure frequency at each of the three periods.
| Beverage Category |
Primary Dentition Phase | Mixed Dentition Phase | Permanent Dentition Phase | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beverage Exposures Age 3 to 5 |
Mean (SD) Caries (Exam 1) |
Beverage Exposures Age 6 to 8 |
Mean (SD) Caries Increment (Exam 2) |
Beverage Exposures Age 11 to 13 |
Mean (SD) Caries Increment (Exam 3) |
|||||||
| % | Occasions per Day* |
d1s | d2fs | % | Occasions per Day* |
d1s+D1s | d2fs+D2Fs | % | Occasions per Day* |
D1s | D2Fs | |
| Powdered Beverages | ||||||||||||
| • Low | 48.1 | 0 | 0.7 (2.1) | 1.0 (2.7) | 47.4 | 0 | 0.9 (1.9) | 3.1 (4.7) | 26.3 | 0 | 0.9 (1.8) | 0.7 (1.6) |
| • Middle | 25.6 | 0.01–0.33 | 0.5 (1.2) | 0.9 (2.2) | 21.8 | 0.01–0.22 | 0.9 (1.1) | 2.7 (4.7) | 47.4 | 0.01–0.29 | 0.8 (1.9) | 0.5 (1.3) |
| • High | 26.3 | >0.33 | 0.5 (1.1) | 2.3 (5.1) | 30.8 | >0.22 | 1.1 (2.4) | 3.0 (3.8) | 26.3 | >0.29 | 1.0 (1.5) | 0.9 (1.4) |
| Regular Soda Pop | ||||||||||||
| • Low | 17.3 | <0.11 | 0.4 (1.3) | 0.3 (0.8) | 25.6 | <0.14 | 1.2 (2.5) | 2.5 (4.8) | 18.0 | <0.14 | 0.9 (1.7) | 0.2 (0.4) |
| • Middle | 60.9 | 0.11–0.56 | 0.6 (1.8) | 1.5 (4.0) | 58.3 | 0.14–0.67 | 1.0 (1.8) | 3.3 (4.3) | 56.4 | 0.14–0.50 | 0.7 (1.6) | 0.7 (1.5) |
| • High | 21.8 | >0.56 | 0.7 (1.5) | 1.4 (2.8) | 16.0 | >0.67 | 0.8 (1.3) | 2.7 (4.4) | 25.6 | >0.50 | 1.1 (2.1) | 0.8 (1.6) |
| Juice Drinks | ||||||||||||
| • Low | 29.5 | 0 | 0.5 (1.3) | 1.7 (4.6) | 21.2 | <0.11 | 0.8 (1.5) | 1.9 (3.5) | 19.2 | 0 | 1.4 (2.3) | 0.7 (1.6) |
| • Middle | 38.5 | 0.01–0.44 | 0.7 (2.3) | 1.1 (2.7) | 55.8 | 0.11–0.50 | 1.1 (2.2) | 3.1 (4.6) | 59.6 | 0.01–0.36 | 0.7 (1.4) | 0.7 (1.4) |
| • High | 32.1 | >0.44 | 0.5 (1.0) | 1.2 (2.9) | 23.1 | >0.50 | 0.8 (1.4) | 3.7 (4.8) | 21.2 | >0.36 | 0.9 (2.0) | 0.7 (1.3) |
| 100% Juice | ||||||||||||
| • Low | 25.0 | <0.44 | 1.1 (2.6) | 2.0 (5.0) | 20.5 | <0.11 | 1.2 (2.1) | 2.6 (3.6) | 22.4 | <0.03 | 1.2 (1.9) | 0.8 (1.5) |
| • Middle | 50.6 | 0.44–1.33 | 0.5 (1.2) | 1.3 (3.0) | 58.3 | 0.11–0.78 | 1.0 (2.1) | 3.8 (5.1) | 50.0 | 0.03–0.57 | 0.9 (1.9) | 0.8 (1.6) |
| • High | 24.4 | >1.33 | 0.2 (1.0) | 0.7 (1.9) | 21.2 | >0.78 | 0.8 (1.1) | 1.2 (2.3) | 27.6 | >0.57 | 0.5 (1.3) | 0.3 (0.9) |
| Milk | ||||||||||||
| • Low | 27.6 | <1.67 | 0.6 (1.2) | 1.7 (3.9) | 18.6 | <1.33 | 0.8 (1.0) | 2.9 (4.1) | 26.3 | <1.03 | 1.0 (2.2) | 0.8 (1.4) |
| • Middle | 48.7 | 1.67–2.78 | 0.8 (2.1) | 0.9 (3.2) | 53.2 | 1.33–2.33 | 1.1 (2.1) | 3.1 (4.9) | 59.6 | 1.03–2.43 | 0.8 (1.6) | 0.6 (1.5) |
| • High | 23.7 | >2.78 | 0.1 (0.4) | 1.6 (3.3) | 28.2 | >2.33 | 1.0 (2.1) | 2.7 (3.8) | 14.1 | >2.43 | 1.0 (1.6) | 0.6 (1.2) |
| Water by Itself | ||||||||||||
| • Low | 20.5 | <0.44 | 0.5 (1.2) | 1.2 (2.8) | 23.7 | <0.50 | 1.2 (2.7) | 2.7 (4.9) | 17.3 | <1.03 | 1.3 (2.7) | 0.6 (0.9) |
| • Middle | 55.8 | 0.44–1.56 | 0.7 (2.0) | 1.2 (3.5) | 52.6 | 0.50–1.89 | 1.0 (1.8) | 2.8 (4.5) | 57.1 | 1.03–2.43 | 0.8 (1.5) | 0.8 (1.7) |
| • High | 23.7 | >1.56 | 0.4 (0.9) | 1.6 (3.8) | 23.7 | >1.89 | 0.7 (1.2) | 3.6 (3.9) | 25.6 | >2.43 | 0.7 (1.4) | 0.4 (1.0) |
Averages of exposure frequencies for 2–5 timepoints during age period.
Results from the separate GLMM regression analyses (Table 4) assessing the associations between the number of surfaces with new non-cavitated caries and cavitated caries and the levels of the beverage exposure frequencies were used to screen the dietary variables for inclusion in the multivariable regression. The only statistical significant dietary variable (p-value < 0.15) for non-cavitated caries was frequency level of 100% juice exposure, while two variables were significant for cavitated caries: frequency level of 100% juice and powdered beverages exposures.
Table 4.
Negative binomial GLMM regression results* for assessing the associations between new non-cavitated and cavitated caries and dietary variables (156 subjects)
| Variable | New Non-cavitated Caries** | New Cavitated Caries*** | ||||
|---|---|---|---|---|---|---|
| Est.§ | exp (Est.)£ | p-value | Est.§ | exp (Est.)£ | p-value | |
| Powdered Beverages (Overall p-value) | (0.72) | (0.003) | ||||
| • Low | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Middle | −0.11 | 0.90 | 0.61 | −0.64 | 0.53 | 0.005 |
| • High | 0.07 | 1.07 | 0.74 | 0.15 | 1.16 | 0.52 |
| Regular Soda Pop (Overall p-value) | (0.55) | (0.25) | ||||
| • Low | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Middle | −0.25 | 0.78 | 0.28 | 0.40 | 1.49 | 0.12 |
| • High | −0.14 | 0.87 | 0.62 | 0.19 | 1.21 | 0.54 |
| Juice Drinks (Overall p-value) | (0.72) | (0.72) | ||||
| • Low | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Middle | −0.17 | 0.84 | 0.46 | 0.15 | 1.16 | 0.54 |
| • High | −0.18 | 0.83 | 0.48 | 0.22 | 1.25 | 0.42 |
| 100% Juice (Overall p-value) | (0.003) | (<0.0001) | ||||
| • Low | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Middle | −0.31 | 0.73 | 0.15 | 0.21 | 1.23 | 0.35 |
| • High | −1.03 | 0.36 | 0.0007 | −1.12 | 0.33 | 0.0005 |
| Milk (Overall p-value) | (0.72) | (0.33) | ||||
| • Low | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Middle | −0.06 | 0.94 | 0.79 | 0.05 | 1.05 | 0.84 |
| • High | −0.22 | 0.80 | 0.44 | 0.36 | 1.43 | 0.21 |
| Water by Itself (Overall p-value) | (0.65) | (0.53) | ||||
| • Low | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Middle | 0.08 | 1.08 | 0.72 | −0.03 | 0.97 | 0.91 |
| • High | −0.12 | 0.89 | 0.66 | 0.23 | 1.26 | 0.43 |
Each row for the non-cavitated (second column) and for cavitated caries (fourth column) was from a separate regression model, with each beverage intake frequency treated as a categorical (3-level) variable.
Transitions are from sound to non-cavitated lesions.
Transitions are from sound/non-cavitated caries lesions to cavitated caries or filled lesions.
β estimates
Exponentiation of the estimates
Table 5 summarizes the separate GLMM regression analyses assessing the associations between new non-cavitated and new cavitated caries and factors other than dietary variables. Lower SES level and a higher proportion of new cavitated caries surfaces to surfaces at risk were significantly associated with more new non-cavitated caries. Greater toothbrushing frequency was significantly associated with fewer new non-cavitated caries, while gender, exam variable and composite water fluoride level were not significantly associated with new non-cavitated caries. Greater proportion of new non-cavitated caries surfaces to surfaces at risk was significantly associated with more new cavitated caries surfaces. Significantly more new cavitated caries were found in the Exam 1 and Exam 2 dentition than in the Exam 3. Gender, SES, toothbrushing frequency and composite water fluoride level were not significantly associated with new cavitated caries.
Table 5.
Negative binomial GLMM regression results* for assessing the associations between new non-cavitated and cavitated caries and other related variables (156 subjects)
| Variable | New Non-cavitated Caries** | New Cavitated Caries*** | ||||
|---|---|---|---|---|---|---|
| Est.§ | exp (Est.)£ |
p-value | Est.§ | exp (Est.)£ |
p-value | |
| Daily Toothbrushing Frequency (Occasions) | −0.40 | 0.67 | 0.03 | −0.36 | 0.70 | 0.08 |
| Composite Water Fluoride (ppm) | −0.28 | 0.76 | 0.34 | −0.18 | 0.84 | 0.57 |
| Proportion of New Non-cavitated Caries Lesions to Surfaces at Risk (10% change) | - | - | - | 0.48 | 1.62 | 0.0002 |
| Proportion of New Cavitated Caries Lesions to Surfaces at Risk (10% change) | 0.23 | 1.26 | 0.0004 | - | - | - |
| SES (overall p-value) | (0.02) | (0.48) | ||||
| • Low | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Middle | 0.07 | 1.07 | 0.80 | 0.03 | 1.03 | 0.92 |
| • High | −0.61 | 0.54 | 0.03 | −0.29 | 0.75 | 0.35 |
| Gender | ||||||
| • Males | 0.11 | 1.12 | 0.60 | −0.18 | 0.84 | 0.49 |
| Dentition (overall p-value) | (0.19) | (<0.0001) | ||||
| • Primary (Exam 1) | 0 | 1 | Ref. | 0 | 1 | Ref. |
| • Mixed (Exam 2) | 0.37 | 1.45 | 0.08 | 0.83 | 2.29 | <0.0001 |
| • Permanent (Exam 3) | 0.16 | 1.17 | 0.43 | −0.69 | 0.50 | 0.002 |
Each row for non-cavitated caries (columns 2–4) and for cavitated caries (columns 5–7) features results from a separate regression model.
Transitions are from sound to non-cavitated lesions.
Transitions are from sound/non-cavitated caries lesions to cavitated caries or filled lesions.
β estimates
Exponentiation of the estimates
Variables initially included in the multivariable regression model for new non-cavitated caries (Table 6) were: 1) 100% juice exposure frequency, 2) toothbrushing frequency, 3) proportion of new cavitated caries surfaces to surfaces at risk, 4) SES, 5) exam variable (1, 2 or 3), 6) the interaction term between toothbrushing frequency and exam variable and 7) the interaction term between proportion of new cavitated caries surfaces to surfaces at risk and SES. Four variables were significantly associated (p-value < 0.05) with new non-cavitated caries surfaces in the final model. The proportions of new non-cavitated caries were 37% and 50% lower for children with the middle and high frequency level of 100% juice exposure compared with children with the low frequency level of 100% juice exposure, respectively. For every increase of one in the frequency of toothbrushing per day, the proportion of new non-cavitated caries decreased by 33%. Being in the high SES category compared with the low/middle SES category decreased the proportion of new non-cavitated caries by 42%, while an increase of 10% in the proportion of new concurrent cavitated caries surfaces to surfaces at risk increased the proportion of new non-cavitated caries by 110%. The exam variable was not significantly associated with new non-cavitated caries.
Table 6.
Multivariable negative binomial GLMM regression results for assessing the associations between new non-cavitated caries and related factors 151 subjects)
| Variable | New Non-cavitated Caries* (d1s/D1S) |
||
|---|---|---|---|
| Est.§ | exp (Est.)£ | p-value | |
| 100% Juice Exposure Level (overall p-value) | (0.041) | ||
| • Low | 0 | 1 | Ref. |
| • Middle | −0.47 | 0.63 | 0.042 |
| • High | −0.69 | 0.50 | 0.02 |
| Tooth Brushing Frequency | −0.40 | 0.67 | 0.044 |
| Proportion of New Cavitated Caries Lesions to Surfaces at Risk (10% change) | 0.74 | 2.10 | 0.004 |
| SES | |||
| • Low/middle | 0 | 1 | Ref. |
| • High | −0.55 | 0.58 | 0.02 |
| Dentition (overall p-value) | (0.17) | ||
| • Primary Dentition (Exam 1) | 0 | 1 | Ref. |
| • Mixed Dentition (Exam 2) | 0.43 | 1.54 | 0.08 |
| • Permanent Dentition (Exam 3) | 0.37 | 1.45 | 0.13 |
Transitions are from sound to non-cavitated lesions.
β estimates
Exponentiation of the estimates
Note: p<0.05 to be retained, except dentition type, a control variable.
Table 7 presents results of the multivariable regression model for new cavitated caries. Variables initially included were: 1) 100% juice exposure frequency, 2) powdered beverage exposure frequency, 3) toothbrushing frequency, 4) proportion of new non-cavitated caries surfaces to surfaces at risk, 5) exam variable, and 6) the interaction term between powdered beverage and proportion of new non-cavitated caries to surfaces at risk. Three variables were significant in the final model (p-value < 0.05). The proportion of new cavitated caries was 48% lower for children with the high frequency level of 100% juice exposure compared with children with the low frequency level of 100% juice exposure. An increase of 10% in the proportion of new concurrent non-cavitated caries surfaces to surfaces at risk increased the proportion of new cavitated caries by 253%. The proportion of new cavitated caries was 120% higher for Exam 2 compared with Exam 1, while the proportion of new cavitated caries was 49% lower for Exam 3 compared with Exam 1.
Table 7.
Multivariable negative binomial GLMM regression results for assessing the associations between new cavitated caries and related factors (151 subjects)
| Variable | New Cavitated Caries* (d2+fs/D2+FS) |
||
|---|---|---|---|
| Est.§ | exp (Est.)£ | p-value | |
| 100% Juice Exposure Level (overall p-value) | (0.02) | ||
| • Low | 0 | 1 | Ref. |
| • Middle | 0.07 | 1.07 | 0.76 |
| • High | −0.65 | 0.52 | 0.03 |
| Proportion of New Non-cavitated Caries Lesions to Surfaces at Risk (10% change) | 1.26 | 3.53 | 0.007 |
| Dentition (overall p-value) | (<0.0001) | ||
| • Primary Dentition (Exam 1) | 0 | 1 | Ref. |
| • Mixed Dentition (Exam 2) | 0.79 | 2.20 | <0.0001 |
| • Permanent Dentition (Exam 3) | −0.67 | 0.51 | 0.003 |
Transitions are from sound/non-cavitated caries lesions to cavitated caries or filled lesions.
β estimates
Exponentiation of the estimates
Note: p<0.05 to be retained, except dentition type, a control variable.
Discussion
Most previously published studies of dental caries and caries-related factors were cross-sectional and examined the relationships between risk factors and caries outcomes at one time (concurrently) or at one subsequent time (prospective studies). The present study examined repeated caries outcomes longitudinally, with the risk factors at the ages of 3–5, 6–8 and 11–13 years associated with caries outcomes at Exam 1 (primary), Exam 2 (mixed) and Exam 3 (permanent dentition).
The strengths of this study include the prospective longitudinal design that collected detailed data on fluoride, dietary, other caries-related factors since recently after birth and dental caries outcomes of the primary, mixed and permanent dentitions. Detailed dietary information collected systematically by dietary diaries and detailed questionnaires allowed us to classify beverage exposures into meaningful categories for assessing caries risk factors.
Another strength of this study is that it used a mixed modeling approach that considers both fixed effects (explanatory variables) and random effects (individual differences). Thus, the individual differences among subjects were accounted for in our modeling framework. Moreover, the repeated outcomes for individual subjects allowed us to better control for individual differences. This improves the statistical power of inferential analyses. Also, this present analysis allowed us to assess the effect of risk factors jointly for the same children over three different age groups. Thus, the results indicated the overall, general effect of risk factors on dental caries across the different age periods and dentitions. The present study also has several limitations, including subjects being almost all white children, mostly middle to high SES, and with low to moderate caries levels. Moreover, there were only 156 children who met the criteria due to the extensive follow-up period, and these statistical analyses required all three dental exams plus risk factor data for all three periods prior to the exams. The primary dentition caries outcome for the present study did not have a baseline exam, therefore, all children were assumed to have no caries at birth. Additionally, non-beverage dietary variables, dental utilization, dental insurance, receipt of dental preventive services (sealants and professional topical fluorides), parental caries experience, parental behavioral factors and levels of cariogenic bacteria were not collected and/or assessed in the present analysis. Including these factors in the analysis might change the findings.
New non-cavitated caries and new cavitated caries were more common for Exam 2 than for Exam 1 and Exam 3. A longer duration of presence in the mouth and risk for caries for some teeth (about 7 years for primary molars) might be a reason for higher new cavitated caries for Exam 2 (mixed dentition). The difference was more pronounced for cavitated caries than for non-cavitated caries, probably because cavitated caries is an irreversible stage of the disease, in contrast with non-cavitated caries where there are chances to reverse to sound surfaces over the longer period. Among children with any cavitated caries, the lowest mean number of surfaces with new cavitated caries was in Exam 3 (permanent dentition). The shorter time since eruption and greater chances for preventive measures (sealants, professional and/or home fluoride use, etc.) might be reasons for lower caries for the Exam 3.
The method used in the present study did not consider reversals, since surfaces with prior caries were excluded from analyses as not being “at risk”. Thus, our report of new non-cavitated and cavitated caries counts is slightly higher than both net caries and adjusted caries increments would be.
Tooth brushing frequencies generally were higher for older children. Composite water fluoride levels (determined from home/school, bottled/filtered/tap water) were slightly lower on average for the older children. Increased usage of bottled water, which generally had lower fluoride levels, could have affected the composite water fluoride level.
The associations between dental caries and beverage exposure frequencies were not consistent dose-response relationships for most of the exposure categories. Therefore, the beverage variables were treated as categorical (not ordinal) variables in both univariable and multivariable regression analyses.
Frequency of 100% juice exposure was significantly related in the multivariable models to both new non-cavitated and cavitated caries. The negative association indicated lower caries in children with higher 100% juice exposure. There are two published studies that reported significant associations between greater 100% juice consumption and less caries. The first study (14) reported a significant association between greater 100% juice consumption (excluding orange juice) and fewer surfaces with caries experience (cross-sectionally at about age 4 years). The other (15) reported a significant negative correlation between fruit juice consumption and caries increment in adolescents. Also, in the previous IFS published study on age 5 caries experience and cavitated caries, there was a general tendency for greater daily 100% juice exposure at age 3, 4, 5 and for ages 1–5 combined to be associated with lower caries, but results were not statistically significant (8). However, greater 100% juice exposure has not otherwise been demonstrated in human incidence studies or laboratory experiments to be a protective factor by itself. Certainly, the sugar content in 100% juice is a source of fermentable carbohydrate. There are studies that report higher risk of dental caries for higher 100% juice exposures with bottle-feeding (16, 17).
There are several possible explanations for this preventive association with caries. First and most important, 100% juice exposure might not be a protective substance by itself; however, low 100% juice exposure might relate to an exposure pattern of other cariogenic beverages. For example, lower consumption frequency of 100% juice might be related to high combination exposures of other sugared beverages that were not associated with dental caries outcomes individually. Moreover, the 100% juice exposure might indicate more healthy beverage or food choices for the individual overall. Second, some 100% juices have been demonstrated to have anti-bacterial effects from the non-nutrients (phytochemicals) that might potentially protect against or inhibit the caries process in the oral cavity (18). Third, different compositions of sugars in 100% juice (fructose/sucrose/glucose) compared to other sugared beverages might explain the lower cariogenicity of 100% juice compared with other sugar-added beverages, especially those with high fructose corn syrup (19). There is a need for both laboratory and epidemiological studies to better explain the association between 100% juice exposure and dental caries.
Greater consumption of 100% juice was associated with less caries. However, juice has been associated with malnutrition in children. Substitution of 100% juice consumption for other sugared beverages might be recommended. However, the total amount of 100% juice should be less than 4–6 ounces daily according to American Academy of Pediatrics recommendations. Beyond that juice intake level, the beverages should be primarily milk, water and other non-caloric beverages.
The directions and strength of associations between dental caries outcomes and non-dietary caries-related factors were similar in both the univariable and multivariable regression models. This indicated that the dietary variables did not modify these associations. Thus, the results from both univariable and multivariable models can be interpreted and discussed together.
Greater toothbrushing frequency was consistently associated with fewer new non-cavitated caries surfaces and tended to be associated with fewer new cavitated caries surfaces. In this study, almost all children (>99%) used fluoridated toothpaste. Moreover, inconsistency of the associations between oral hygiene and/or plaque index and caries has been reported in other published studies (6, 20). For the present study, we suggested that the protective effect of frequent tooth brushing is mainly from exposure to fluoride in toothpaste.
Studies assessing associations between SES and cavitated caries outcomes found mixed results. Most of the earlier studies (21–23) found strong relationships between SES and caries, but several more recent ones (1, 24) did not. This probably is due in part to different definitions of caries outcomes, SES, etc., but also may be due to the fluoridated dentifrice and water ubiquity, great variety of dietary exposures and complexities of self-care behaviors. High SES was associated with smaller numbers of new non-cavitated caries in the present analysis. SES was categorized based on mother’s education and family income. Greater number of new non-cavitated caries in lower SES children could be explained by lower frequency of seeing the dentist for both prevention and treatment in this group of subjects and generally less favorable preventive behaviors. For cavitated caries, the present study found a trend of fewer new cavitated caries for those of high SES, however, the association was not statistically significant. Higher SES children usually have better access to care that might result in better prevention, fluoride exposures and counseling, which collectively can result in lower caries. However, they also had a greater chance to receive restorative treatment, which could have increased the likelihood of getting over-treatment of non-cavitated caries (thereby increasing the number of new cavitated caries surfaces). These might be reasons for the non-significant association between cavitated caries and SES in the present study.
Previous caries experience consistently has been found to be associated with increased risk of having caries. As discussed in other studies, strong associations between previous caries and new caries outcomes generally reduced the contribution of other weaker explanatory variables (25, 26). Excluding previous caries experience from multivariable regression models allowed us to better explore the relationships of other modifiable variables which generally have weaker associations with caries outcomes. Although previous caries experience was not used as an explanatory variable, this factor indirectly influenced the analyses. Children with more tooth surfaces with caries experience had fewer surfaces at risk for caries. However, having one carious surface would have changed only 1% to 2% of the surfaces at risk (e.g., if caries-free children have 88 surfaces at risk, children with 1 surface with caries would have 87 surfaces at risk).
This study is the first of its type to look at children’s caries risk factors in this way using repeated measures analysis with the primary, mixed and permanent dentitions. Such studies are needed because we might find common caries-related factors that could be used to develop general preventive measures in children. There are many studies that look at caries risk factors at specific ages. In theory, repeated measures analysis has advantages over the single outcome study. However, we cannot conclude that the repeated measures analysis provides a better mechanism for understanding strategies for caries prevention.
The present analyses concerning non-cavitated and cavitated caries and risk factors across the 3 exams (primary, mixed and permanent dentitions) can be summarized as follows.
Greater frequency of 100% juice exposures was related to fewer new non-cavitated and fewer new cavitated caries.
Frequency of other beverage exposures was not found to be significantly associated with increased risk for either type of caries outcome.
Lower SES was significantly associated with greater new non-cavitated caries counts.
Greater toothbrushing frequency (almost all with fluoride toothpaste) was associated with fewer new non-cavitated caries counts and with fewer new cavitated caries counts.
References
- 1.Burt BA, Eklund SA, Morgan KJ, Larkin FE, Guire KE, Brown LO, et al. The effects of sugars intake and frequency of ingestion on dental caries increment in a three-year longitudinal study. J Dent Res. 1988 Nov;67(11):1422–1429. doi: 10.1177/00220345880670111201. [DOI] [PubMed] [Google Scholar]
- 2.Holbrook WP, Arnadottir IB, Takazoe I, Birkhed D, Frostell G. Longitudinal study of caries, cariogenic bacteria and diet in children just before and after starting school. Eur J Oral Sci. 1995 Feb;103(1):42–45. doi: 10.1111/j.1600-0722.1995.tb00009.x. [DOI] [PubMed] [Google Scholar]
- 3.Ismail AI, Lim S, Sohn W, Willem JM. Determinants of early childhood caries in low-income African American young children. Pediatr Dent. 2008 Jul-Aug;30(4):289–296. [PubMed] [Google Scholar]
- 4.Levine RS, Nugent ZJ, Rudolf MC, Sahota P. Dietary patterns, toothbrushing habits and caries experience of schoolchildren in West Yorkshire, England. Community Dent Health. 2007 Jun;24(2):82–87. [PubMed] [Google Scholar]
- 5.Ollila P, Larmas M. A seven-year survival analysis of caries onset in primary second molars and permanent first molars in different caries risk groups determined at age two years. Acta Odontol Scand. 2007 Feb;65(1):29–35. doi: 10.1080/00016350600963590. [DOI] [PubMed] [Google Scholar]
- 6.Sayegh A, Dini EL, Holt RD, Bedi R. Oral health, sociodemographic factors, dietary and oral hygiene practices in Jordanian children. J Dent. 2005 May;33(5):379–388. doi: 10.1016/j.jdent.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Tsai AI, Chen CY, Li LA, Hsiang CL, Hsu KH. Risk indicators for early childhood caries in Taiwan. Community Dent Oral Epidemiol. 2006 Dec;34(6):437–445. doi: 10.1111/j.1600-0528.2006.00293.x. [DOI] [PubMed] [Google Scholar]
- 8.Marshall TA, Broffitt B, Eichenberger-Gilmore J, Warren JJ, Cunningham MA, Levy SM. The roles of meal, snack, and daily total food and beverage exposures on caries experience in young children. J Public Health Dent. 2005 Summer;65(3):166–173. doi: 10.1111/j.1752-7325.2005.tb02807.x. [DOI] [PubMed] [Google Scholar]
- 9.Franzman MR, Levy SM, Warren JJ, Broffitt B. Tooth-brushing and dentifrice use among children ages 6 to 60 months. Pediatr Dent. 2004 Jan-Feb;26(1):87–92. [PubMed] [Google Scholar]
- 10.Levy SM, Warren JJ, Davis CS, Kirchner HL, Kanellis MJ, Wefel JS. Patterns of fluoride intake from birth to 36 months. J Public Health Dent. 2001 Spring;61(2):70–77. doi: 10.1111/j.1752-7325.2001.tb03369.x. [DOI] [PubMed] [Google Scholar]
- 11.Hamasha AA, Warren JJ, Levy SM, Broffitt B, Kanellis MJ. Oral health behaviors of children in low and high socioeconomic status families. Pediatr Dent. 2006 Jul-Aug;28(4):310–315. [PubMed] [Google Scholar]
- 12.Warren JJ, Levy SM, Broffitt B, Kanellis MJ. Longitudinal study of non-cavitated carious lesion progression in the primary dentition. J Public Health Dent. 2006 Spring;66(2):83–87. doi: 10.1111/j.1752-7325.2006.tb02560.x. [DOI] [PubMed] [Google Scholar]
- 13.Pitts NB. Diagnostic tools and measurements--impact on appropriate care. Community Dent Oral Epidemiol. 1997 Feb;25(1):24–35. doi: 10.1111/j.1600-0528.1997.tb00896.x. [DOI] [PubMed] [Google Scholar]
- 14.Kolker JL, Yuan Y, Burt BA, Sandretto AM, Sohn W, Lang SW, et al. Dental caries and dietary patterns in low-income African American children. Pediatr Dent. 2007 Nov-Dec;29(6):457–464. [PubMed] [Google Scholar]
- 15.Clancy KL, Bibby BG, Goldberg HJ, Ripa LW, Barenie J. Snack food intake of adolescents and caries development. J Dent Res. 1977 Jun;56(6):568–573. doi: 10.1177/00220345770560060301. [DOI] [PubMed] [Google Scholar]
- 16.Du M, Luo Y, Zeng X, Alkhatib N, Bedi R. Caries in preschool children and its risk factors in 2 provinces in China. Quintessence Int. 2007 Feb;38(2):143–151. [PubMed] [Google Scholar]
- 17.Lewis CW, Riedy CA, Grossman DC, Domoto PK, Roberts MC. Oral health of young Alaska Native children and their caregivers in Southwestern Alaska. Alaska Med. 2002 Oct-Dec;44(4):83–87. [PubMed] [Google Scholar]
- 18.Cranberry juice for prophylaxis of urinary tract infections--conclusions from clinical experience and research. Phytomedicine. 2008 Sep;15(9):653–667. doi: 10.1016/j.phymed.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 19.Marshall TA, Levy SM, Broffitt B, Warren JJ, Eichenberger-Gilmore JM, Burns TL, et al. Dental caries and beverage consumption in young children. Pediatrics. 2003 Sep;112(3 Pt 1):e184–e191. doi: 10.1542/peds.112.3.e184. [DOI] [PubMed] [Google Scholar]
- 20.Chung CS, Hankin JH, Miyamoto W, Kau MC. Dental plaque and dietary intakes in schoolchildren in Hawaii. J Dent Res. 1977 Jan;56(1):11–16. doi: 10.1177/00220345770560010101. [DOI] [PubMed] [Google Scholar]
- 21.Beck JD, Weintraub JA, Disney JA, Graves RC, Stamm JW, Kaste LM, et al. University of North Carolina Caries Risk Assessment Study: comparisons of high risk prediction, any risk prediction, and any risk etiologic models. Community Dent Oral Epidemiol. 1992 Dec;20(6):313–321. doi: 10.1111/j.1600-0528.1992.tb00690.x. [DOI] [PubMed] [Google Scholar]
- 22.Brown LP, Mulqueen TF, Storey E. The effect of fluoride consumption and social class on dental caries in 8-year-old children. Aust Dent J. 1990 Feb;35(1):61–68. doi: 10.1111/j.1834-7819.1990.tb03029.x. [DOI] [PubMed] [Google Scholar]
- 23.Evans RW, Lo EC, Darvell BW. Determinants of variation in dental caries experience in primary teeth of Hong Kong children aged 6–8 years. Community Dent Oral Epidemiol. 1993 Feb;21(1):1–3. doi: 10.1111/j.1600-0528.1993.tb00707.x. [DOI] [PubMed] [Google Scholar]
- 24.Petti S, Cairella G, Tarsitani G. Rampant early childhood dental decay: an example from Italy. J Public Health Dent. 2000 Summer;60(3):159–166. doi: 10.1111/j.1752-7325.2000.tb03322.x. [DOI] [PubMed] [Google Scholar]
- 25.Leroy R, Bogaerts K, Lesaffre E, Declerck D. Multivariate survival analysis for the identification of factors associated with cavity formation in permanent first molars. Eur J Oral Sci. 2005 Apr;113(2):145–152. doi: 10.1111/j.1600-0722.2005.00199.x. [DOI] [PubMed] [Google Scholar]
- 26.Tagliaferro EP, Ambrosano GM, Meneghim Mde C, Pereira AC. Risk indicators and risk predictors of dental caries in schoolchildren. J Appl Oral Sci. 2008 Nov-Dec;16(6):408–413. doi: 10.1590/S1678-77572008000600010. [DOI] [PMC free article] [PubMed] [Google Scholar]