Abstract
Despite the consistent link between parenting stress and postpartum depressive symptoms, few studies have explored the relationships longitudinally. The purpose of this study was to test bidirectional and unidirectional models of depressive symptoms and parenting stress. Uniquely, three specific domains of parenting stress were examined: parental distress, difficult child stress, and parent–child dysfunctional interaction (PCDI). One hundred and five women completed the Beck Depression Inventory and the Parenting Stress Index–Short Form at 3, 7, and 14 months after giving birth. Structural equation modeling revealed that total parenting stress predicted later depressive symptoms, however, there were different patterns between postpartum depressive symptoms and different types of parenting stress. A unidirectional model of parental distress predicting depressive symptoms best fit the data, with significant stability paths but non-significant cross-lagged paths. A unidirectional model of depressive symptoms predicted significant later difficult child stress. No model fit well with PCDI. Future research should continue to explore the specific nature of the associations of postpartum depression and different types of parenting stress on infant development and the infant–mother relationship.
Keywords: Postpartum depression, Parenting stress, Maternal cognitions
1. Introduction
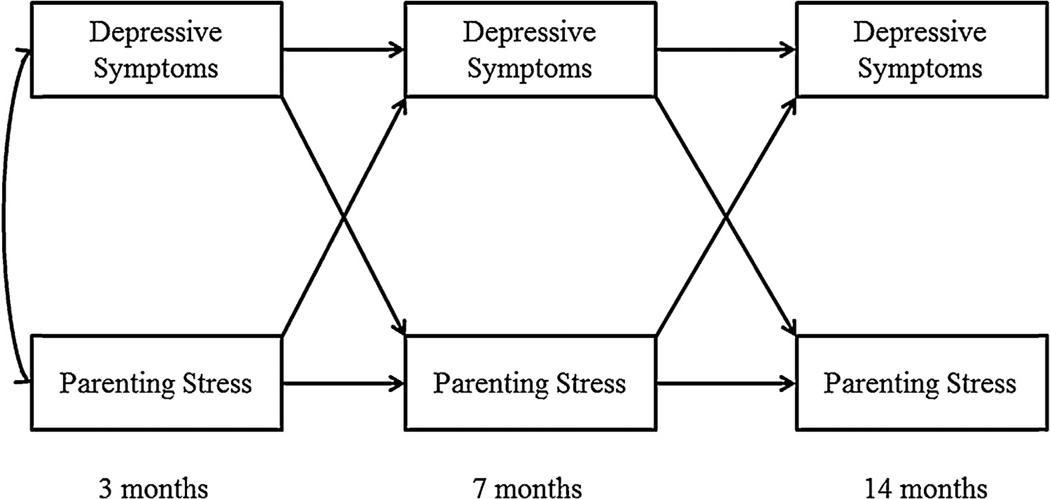
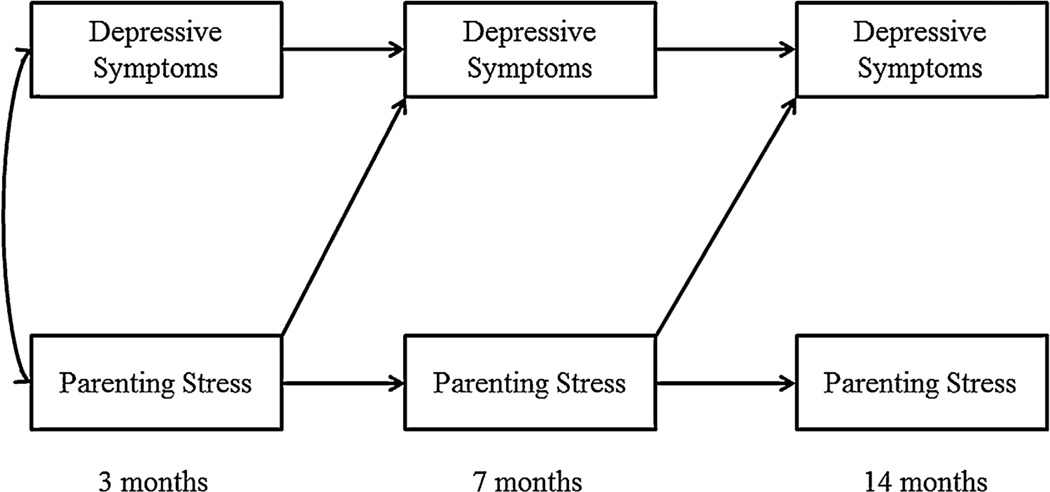
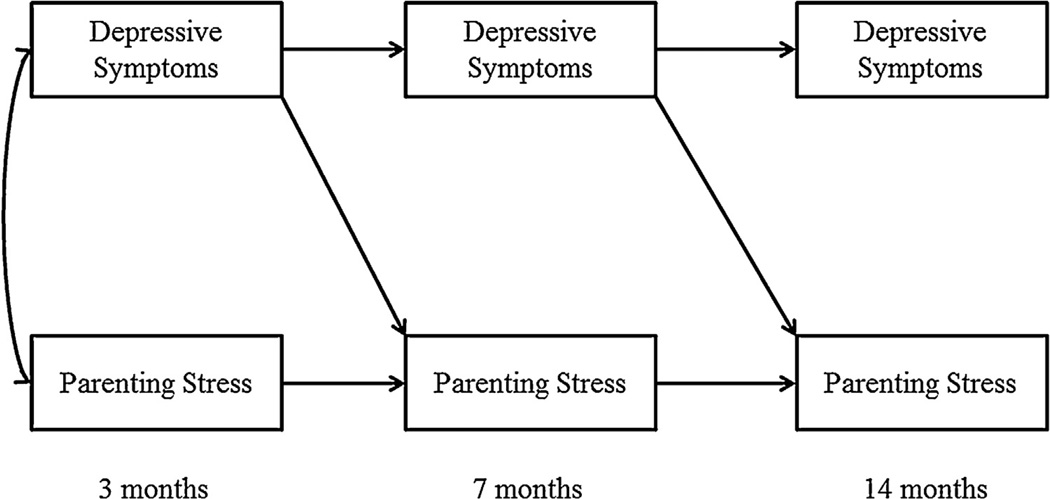
Postpartum depression is an important risk factor that negatively impacts children’s development, as well as parenting, maternal health, and well-being (C. T. Beck, 1998; Cummings, Davies, & Campbell, 2000; Downey & Coyne, 1990; Field, 2010). Even mild levels of depression that do not meet criteria for a major depressive episode may result in adverse effects for women and children (Ashman, Dawson, & Panagiotides, 2008). A consistent link between maternal depressive symptoms and parenting stress has been established (Cornish et al., 2006; Gelfand, Teti, & Fox, 1992; Gerdes et al., 2007; Sidor, Kunz, Schweyer, Eickhorst, & Cierpka, 2011). Yet, few studies have explored relations between parenting stress and maternal depressive symptoms longitudinally over the postpartum period, which is important for predicting maternal depressive symptoms across the perinatal period. Does a bidirectional model or a unidirectional model best explain the development of maternal depressive symptoms? A bidirectional model (see Fig. 1) would suggest that depressive symptoms and parenting stress mutually influence one another over time. On the other hand, a unidirectional model would demonstrate that either earlier parenting stress predicts later depressive symptoms (see Fig. 2) or that earlier depressive symptoms predict later parenting stress (see Fig. 3). This study will test whether a bidirectional or unidirectional model best explains the association between maternal depressive symptoms and parenting stress during the first postpartum year. Additionally, these models will be tested with three specific subtypes of parenting stress (parental distress, difficult child stress, and stress related to dysfunctional mother-child interactions) to examine if different types of parenting stress have different relations with maternal depressive symptoms. Understanding how different domains of parenting stress are related to depression over the first year can help inform future research and intervention efforts by identifying and targeting specific sources of stress.
Fig. 1.
Bidirectional model (Models 1 and 2) examining the stability and bidirectional effects of maternal depressive symptoms and maternal parenting stress from 3-months postpartum, 7-months postpartum, 14-months postpartum. Error terms are not shown.
Fig. 2.
Unidirectional model of parenting stress predicting maternal depressive symptoms (Model 3).
Fig. 3.
Unidirectional model of maternal depressive symptoms predicting parenting stress (Model 4).
1.1. Relations between postpartum depressive symptoms and parenting stress
Types of parenting stress include stress related to the parental domain, such as women’s perceived stress of the parental role, and stress related to the child domain, such as perceptions of how difficult the infant is, as well as stress related to mother-child interaction. Stress associated with the parental role has consistently been related to depressive symptoms (Cornish et al, 2006; Horowitz & Goodman, 2004; Misri, Reebye, Milis, & Shah, 2006; Sidor et al., 2011). The findings regarding perceptions of stress associated with a difficult child are mixed, with some researchers finding that depressed mothers report their children are more difficult (Britton, 2011; Cornish et al., 2006; McGrath, Records, & Rice, 2008; Milgrom & McCloud, 1996), whereas others find no connection between depressive symptoms and perceptions of a difficult child (Misri et al., 2006; Pritchard et al., 2012). Parenting stress specific to the parent-child interaction has been examined to a lesser extent. Some studies suggest mothers’ stress with regard to the parent-child interaction is related to depressive symptoms (Mason, Briggs, & Silver, 2011; Sidor et al., 2011), but others have not found the same association (Horowitz & Goodman, 2004; Pritchard et al., 2012). The inconsistent findings regarding specific types of parenting stress, and the importance of parenting stress for maternal behavior and child outcomes, make parenting stress an area worthy of further exploration. Many of these studies were cross-sectional or assessed stress at only one postpartum timepoint (Britton, 2011; Gelfand et al., 1992; Horowitz & Goodman, 2004; Mason et al., 2011; Sidor et al., 2011). Other studies focused on differences between depressed and non-depressed groups of women, with parenting stress as the outcome (Gelfand et al., 1992; Mason et al., 2011; McGrath et al., 2008; Milgrom & McCloud, 1996; Pritchard et al., 2012), but none of these studies allowed for an examination of longitudinal relations at multiple timepoints. A longitudinal approach may illuminate the specific nature of the relations between parenting stress and maternal depressive symptoms during the postpartum period.
One exception is a longitudinal study that examined parenting stress at multiple timepoints. Cornish et al. (2006) followed 112 first-time mothers at 4, 12, and 15 months postpartum and categorized them as never, briefly (4 months only), or chronically (12 months or longer) depressed, and included measures of parenting stress over time. They found that briefly and chronically depressed women had higher levels of parenting stress than the never depressed women, but did not explore if maternal depressive symptoms and parenting stress influenced one another over time.
1.2. Cognitive theory of depression
Beck’s model of depression (A. T. Beck, 1976) proposes that although an individual may have a predisposition toward negative cognitions associated with depression, these cognitions (and subsequent depressive episode) are not activated until the individual experiences some sort of stressor, suggesting a unidirectional approach toward the onset of depressive symptoms, one in which stress leads to depression. This model is particularly appropriate in conceptualizing the emergence of postpartum depression, because we hypothesize that the stress of caring for a young infant is the impetus for developing depressive symptoms when the woman also has negative cognitions associated with this stress.
It is possible that a bidirectional, or transactional, approach could also explain the development of depression and stress over time if an individual is prone to negative cognitions. Once activated, the negative cognitions maintain depressive symptoms and lead an individual to choose more negative interpretations of future events as true, regardless of the reality, which in turn leads to an individual feeling more stress and a bidirectional cycle is formed, which would explain the continuation of depressive symptoms. Some research has explored the bidirectional model and concluded that the bidirectional nature of the relationship may depend on the type of stress involved (Pianta & Egeland, 1994). Both models of depression may provide an explanation of why some women develop postpartum depression as a result of caring for an infant whereas others do not. We wanted to test both unidirectional and bidirectional models in this study to explore relations between depressive symptoms and parenting stress over time.
The primary goal of this study was to test a bidirectional model of the relations between parenting stress and maternal depressive symptoms (see Fig. 1) and compare this to a unidirectional model in which parenting stress predicts later maternal depressive symptoms (see Fig. 2). In order to rule out alternative explanations, the reverse unidirectional model was also tested (see Fig. 3), with earlier depressive symptoms predicting later parenting stress.
We hypothesized that, based on cognitive theory, a unidirectional model, with significant paths from earlier parenting stress predicting later depressive symptoms, would result in a better fit with the data than a bidirectional model of depressive symptoms and parenting stress. We hypothesized this model would fit best for overall parenting stress, as well as the domains of Parental Distress and Difficult Child. We hypothesized that a bidirectional model would be a better fit for Parent-Child Dysfunctional Interaction stress and maternal depressive symptoms based on cognitive theory and developmental perspectives (Beck, 1976; Cummings & Davies, 1994; Pianta & Egeland, 1994). If a woman is depressed she is more likely to be less sensitive and less responsive to her child, which would result in less optimal parent-child interactions. The child may respond in such ways that would be less reinforcing for the mother, which in turn would exacerbate her low mood. We expected that all cross-lagged paths would be significant in the bidirectional model.
2. Method
2.2. Eligibility and enrollment
Upon approval by the university’s institutional review board, pregnant women were recruited through obstetric offices affiliated with a large university health care system in the Midwestern United States, as part of an 18-month longitudinal study that examined women at-risk for postpartum depression. Women were eligible to participate if they were over the age of 20, were fluent in English, planned to stay in the area for two years, planned to keep their child, and had no substance abuse, eating disorders, bipolar illness, or current depression.
Subjects were 154 women recruited from obstetrics clinics, participating in a longitudinal study starting at 28 weeks of pregnancy and followed at 3,7, and 14 months postpartum. Twenty-four mothers attrited by the 14-month timepoint, leaving 81 mothers (77% of 3-month sample) with data at the 3, 7, and 14-month timepoints. There were significant differences between women who remained in the study until 14 months and women who dropped after the 3-month visit with regard to age, parity, and education. Women who remained in the study were more likely to be primiparous, χ2(1, n = 104) = 10.76, p = .001, and more educated, χ2(2, n = 104) = 8.26, p = .016 than those who dropped. Women who remained in the study were also older (M = 31.30, SD = 4.34), t(103) = 2.08, p = 04, than those who dropped (M = 29.08, SD = 5.33). There were no differences by partner status, child gender, level of depressive symptoms, or parental stress for women remaining in the study and those who attrited.
The mean maternal age for the 105 participants was 30.79 years (SD = 4.65). Forty-six percent (n = 48) of the sample was first-time mothers and 96% (n = 101) lived with their husband or partner. Seventy-seven percent (n = 79) of the households had an income of $50,000 or more, and 81 % (n = 84) of the mothers had a bachelor’s degree or above. Fifty-one percent (n = 54) of the babies were male. The sample was 75% white (n = 79), 6% African American (N = 6), 10% Asian (n = 10), 6% Hispanic (n = 6), and 4% other (n = 4).
2.2. Procedure
After providing informed consent, women were recruited and interviewed for the first time during the 28th week of pregnancy. Women were administered the Structured Clinical Interview for DSMIV by trained clinical personnel and eligible for the study if they were not currently depressed.
Physiological data, such as salivary cortisol, and psychological self-report scales such as those measuring depressive symptoms and marital satisfaction were also collected at 32 and 37 weeks prenatal, 2 weeks, 6 weeks, and 3, 7, and 14 months postpartum through home and lab visits. Because the current study focuses on parenting stress after the arrival of the infant, after controlling for initial depressive symptoms at 2 weeks postpartum, only the postpartum timepoints that had both parenting stress and maternal depressive symptoms were utilized in the structural equation models, which were the 3 (T1), 7 (T2), and 14-month (T3) postpartum timepoints.
2.3. Measures
2.3.1. Maternal depressive symptoms
The Beck Depression Inventory-II (BDI-II, Beck, Steer, & Brown, 1996) was used to assess depressive symptoms at 3, 7, and 14 months postpartum (3-month α = .90, 7-month α = .89, 14-month α = .89). The BDI-II is a 21-item self-report that has been established as a valid and reliable measure with postpartum women (Ji et al., 2011). Participants were asked to rate the intensity of their symptoms, on a scale from 0 to 3, by choosing the statement that best described their feelings over the past two weeks for items such as Sadness: 0 = I do not feel sad; 1 = I feel sad much of the time; 2 = I am sad all of the time; 3 = I am so sad or unhappy that I can’t stand it. Scores were summed for the 21 items.
2.3.2. Maternal stress
The Parenting Stress Index - Short Form (PSI-SF) (Abidin, 1995), a 36-item self-report questionnaire, was used to assess perceived stress from the mother’s point of view at 3, 7, and 14 months postpartum (3-month α = .91, 7-month α = .92, 14-month α = .92). The questionnaire is also separated into three domains of parenting-related stress, with each subscale consisting of twelve items: (a) Parental Distress (α = .83–.86) measured the mother’s feelings of competence about being a parent and the associated responsibilities (e.g., “I feel trapped by my responsibilities as a parent”); (b) Difficult Child (α = .84–.91) focused on perceptions of how challenging the child was (e.g., “My child generally wakes up in a bad mood”); (c) Parent-Child Dysfunctional Interaction (α = .85–.87) measured the mother’s feelings about her interactions with her child (e.g., “When I do things for my child, I get the feeling that my efforts are not appreciated very much”). Mothers used a 5-point Likert scale ranging from 1 = strongly agree to 5 = strongly disagree to rate items with higher scores indicating less parenting stress. Mean scores were derived for the total parenting stress score and all three subscales. For ease of interpretation, each score was multiplied by −1 so that a higher score represented more parenting stress.
2.3.3. Data analysis plan
Preliminary analyses examined relations between parenting stress and maternal depressive symptoms. Four structural equation models were conducted to test bidirectional and unidirectional models of maternal depressive symptoms and parenting stress. Initial level of depressive symptoms at the first postpartum timepoint (2 weeks) was controlled for in all models so that changes in depression at later timepoints could be identified as a result of cross-lagged effects and not from higher initial postpartum depressive symptom levels. As illustrated in Fig. 1, the bidirectional model (Model 1) consisted of stability across timepoints (A), the cross-lagged effect or prediction of change by maternal depressive symptoms to parenting stress (B), the cross-lagged effect or prediction of change by parenting stress to maternal depressive symptoms (C), and their within-time covariances (D) to account for similar times of measurement. The unconstrained model, which allowed all paths to be freely estimated, was tested and examined for fit with the data. Next, each construct was set to be equal across time for all timepoints in order to establish measurement invariance and to test a more parsimonious model (Model 2). Two unidirectional models were also conducted for comparison with the bidirectional model. The first unidirectional model (Model 3) tested the pathway from stress to depression (see Fig. 2). The second unidirectional model (Model 4) tested the pathway from depression to stress (see Fig. 3). After finding the best-fitting model for parenting stress and maternal depressive symptoms by examining the fit statistics and the chi-square difference test, additional analyses were conducted for each subtype of parenting stress (Parental Distress, Difficult Child, and Parent-Child Dysfunctional Interaction). All analyses were completed using SPSS 20 and AMOS 20.
3. Results
3.1. Descriptive analyses
Table 1 shows the means and standard deviations of maternal depressive symptoms and parenting stress. Bivariate correlations (see Table 1) revealed that parenting stress and all parenting stress subtypes were positively associated with maternal depressive symptoms at all timepoints, with the exception of 3-month Difficult Child stress, which was not significantly associated with maternal depressive symptoms at 14 months.
Table 1.
Correlation coefficients, means, and standard deviations of depressive symptoms and parenting stress at 3, 7, and 14 months postpartum.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. 3 month DS | - | ||||||||||||||
| 2. 7 month DS | .68*** | - | |||||||||||||
| 3. 14 month DS | .62*** | .63*** | - | ||||||||||||
| 4. 3 month PSI | .62*** | .53*** | .42*** | - | |||||||||||
| 5. 7 month PSI | .54*** | .59*** | .47*** | .82*** | - | ||||||||||
| 6. 14 month PSI | .52*** | .52*** | .50*** | .78*** | .78*** | - | |||||||||
| 7. 3 month PD | .70*** | .58*** | .44*** | .86*** | .76*** | .67*** | - | ||||||||
| 8. 7 month PD | .51*** | .67*** | .49*** | .66*** | .84*** | .63*** | .76*** | - | |||||||
| 9. 14 month PD | .53*** | .52*** | .59*** | .74*** | .72*** | .81*** | .72*** | .75*** | - | ||||||
| 10. 3 month PCDI | .43*** | .42*** | .36*** | .82*** | .64*** | .61*** | .57*** | .50*** | .57*** | - | |||||
| 11. 7 month PCDI | .42*** | .33** | .24* | .68*** | .80*** | .57*** | .54*** | .48*** | .45*** | .69*** | - | ||||
| 12. 14 month PCDI | .33** | .34** | .25* | .63*** | .59*** | .80*** | .45*** | .39*** | .44*** | .67*** | .61*** | - | |||
| 13. 3 month DC | .35*** | .30** | .21 | .80*** | .63*** | .67*** | .47*** | .34** | .54*** | .56*** | .51*** | .50*** | - | ||
| 14. 7 month DC | .35*** | .35*** | .34** | .65*** | .78*** | .69*** | .48*** | .40*** | .47*** | .42*** | .57*** | .48*** | .73*** | - | |
| 15. 14 month DC | .37*** | .39*** | .33** | .58*** | .60*** | .85*** | .45*** | .36** | .45*** | .37** | .38*** | .64*** | .62*** | .73*** | - |
| Mean | 6.65 | 6.18 | 5.35 | − 4.28 | − 4.33 | − 4.30 | − 3.85 | − 3.92 | − 3.97 | − 4.61 | − 4.66 | − 4.65 | − 4.35 | − 4.40 | − 4.25 |
| Standard deviation | 6.21 | 5.88 | 5.66 | .44 | .44 | .43 | .66 | .69 | .60 | .42 | .43 | .39 | .52 | .50 | .57 |
Notes. DS: depressive symptoms; PSI: Parenting Stress Index; PD: parental distress, PCDI: parent–child dysfunctional interaction; DC: difficult child.
p < .05.
p < .01.
p < .001.
3.2. Structural equation modeling
The bidirectional and unidirectional models of maternal depressive symptoms and parenting stress over the first 14 months postpartum for the sample were examined using structural equation modeling. The following fit indices were used to evaluate model fit: (1) the Comparative Fit Index (CFI), which should be above .90 for an acceptable fit and above .95 for a good fit; (2) Root Mean Square Error of Approximation (RMSEA), where less than .05 is a good fit, between .05 and .08 is an acceptable fit, and below .10 is a poor fit (Browne & Cudeck, 1993; Kline, 2005). The chi-square should be as small as possible; it would ideally not be significant, but it is highly dependent on sample size and a significant chi-square alone does not disqualify the model fit (Schumacker & Lomax, 2010).
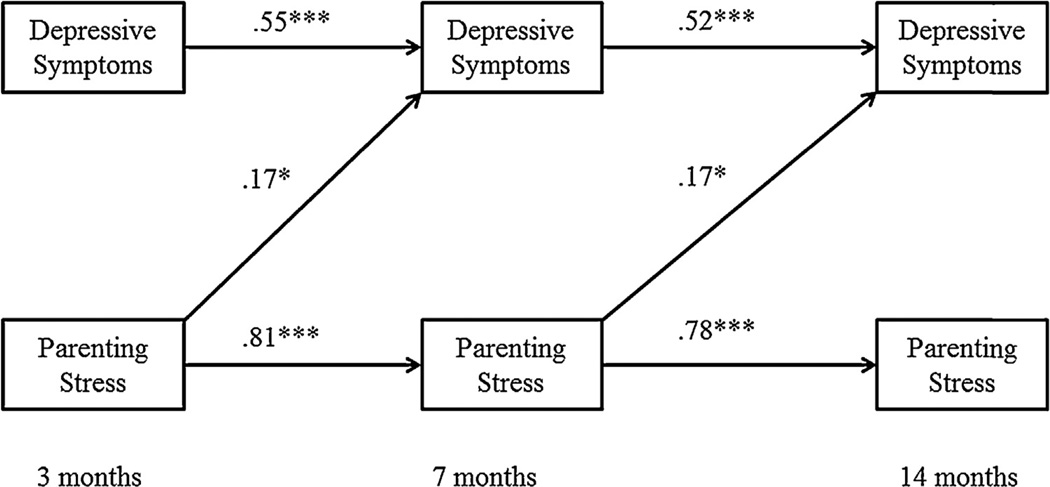
3.2.1. Parenting stress
Model 3, which deleted the cross-lagged paths from maternal depressive symptoms to parenting stress, was the best-fitting model and the most parsimonious, χ2(13) = 22.36, p = .050, RMSEA=.08 [.00, .14], CFI = .97 (see Fig. 4). All stability coefficients were significant, indicating that maternal depressive symptoms and parenting stress were dependent on the previous time point of measurement. T1 parenting stress significantly predicted an increase in T2 maternal depressive symptoms and T2 parenting stress predicted the increase in T3 maternal depressive symptoms. The hypothesis that the unidirectional model of earlier parenting stress would predict later maternal depressive symptoms and fit the data better than the bidirectional model was supported.
Fig. 4.
Unidirectional model of total parenting stress predicting maternal depressive symptoms across 3, 7, and 14 months with standardized estimates, resulting in acceptable model fit. χ2(13) = 22.36, p = .050, RMSEA = .08 [.00, .14], CFI = .97. Initial 2 week postpartum depressive symptoms control variable and covariance estimates are not shown. *p<.05, **p<.01, ***p<.001.
3.2.2. Parental distress
Evaluation of multiple fit indices indicated that the third model resulted in the best fit and was the most parsimonious, χ2(13) = 23.03, p = .041, RMSEA = .09 [.02, .14], CFI = .97. The hypothesis that the unidirectional model of parental distress predicting depressive symptoms was only partially supported, however, as there were no significant paths from parental distress to depressive symptoms.
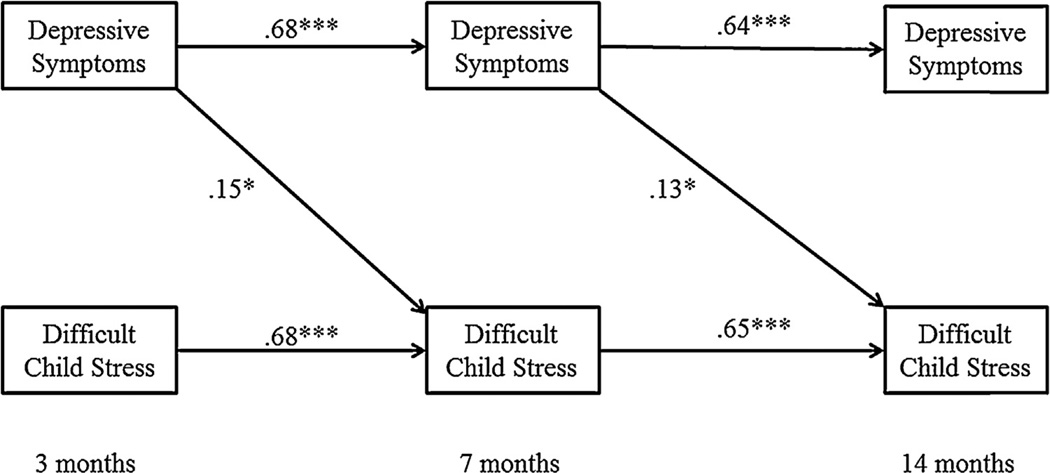
3.2.3. Difficult child
Evaluation of multiple fit indices indicated that the fourth model, with depressive symptoms predicting difficult child stress, resulted in the best fit and was the most parsimonious, χ2(13) = 21.11, p = .071, RMSEA = .08 [.00, .14], CFI = .97 (see Fig. 5). The hypothesis that the unidirectional model of difficult child stress predicting depressive symptoms was not supported.
Fig. 5.
Unidirectional model of difficult child stress and maternal depressive symptoms across 3,7, and 14 months with standardized estimates, resulting in acceptable model fit. χ2(13) = 21.11, p = . 071, RMSEA=. 08 [.00,. 14], CFI = .97. Initial 2 week postpartum depressive symptoms control variable and covariance estimates are not shown. *p<.05, ** p<.01, ***p ≤ .001.
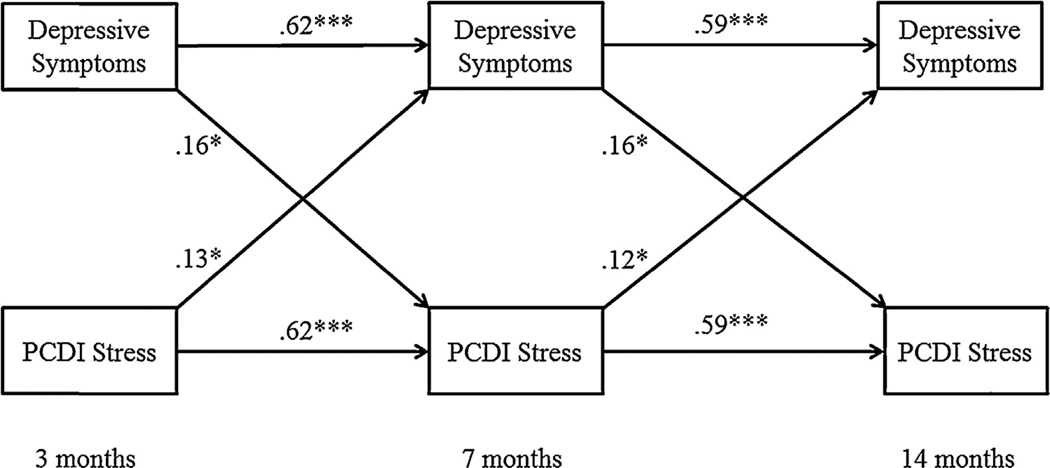
3.2.4. Parent-child dysfunctional interaction
Evaluation of multiple fit indices indicated that neither the unidirectional or bidirectional models were an acceptable fit for the data, although the constrained bidirectional model (Model 2) fell just outside acceptable fit and had significant cross-lagged paths, χ2(12) = 23.35, p = .025, RMSEA=.095 [.03, .15], CFI = .95. The hypothesis that the bidirectional model would be the best-fitting model was not supported (Fig. 6).
Fig. 6.
Bidirectional model of parent-child dysfunctional interaction (PCDI) stress and maternal depressive symptoms across 3, 7, and 14 months with standardized estimates, resulting in poor model fit. χ2(12) = 23.35, p = .025, RMSEA=.095 [.03, .15], CFI = .95. Initial 2 week postpartum depressive symptoms control variable and covariance estimates are not shown. *p<.05, **p<.01, ***p≤.001.
4. Discussion
The purpose of this study was to test bidirectional and unidirectional models of maternal depressive symptoms and parenting stress over the first 14 months postpartum, looking at both overall parenting stress and different domains of parenting stress. This was done by first examining the preliminary relations between maternal depressive symptoms and parenting stress. Next, structural equation modeling was used to compare bidirectional and unidirectional models of the relations between maternal depressive symptoms and parenting stress over time. We hypothesized that unidirectional models of stress predicting depressive symptoms would fit the data best for overall parenting stress, parental distress, and difficult child stress and that the paths from stress to depressive symptoms would be significant. We hypothesized that a bidirectional model would fit the data best for maternal depressive symptoms and parent-child dysfunctional interaction stress and that all cross-lagged paths would be significant.
Preliminary correlations revealed that maternal depressive symptoms and overall parenting stress were significantly and positively associated in the full sample within and across all time points. Further examination revealed that this held true for specific subtypes of parenting stress and maternal depressive symptoms, with the exception of 3-month difficult child stress with 14-month maternal depressive symptoms. These findings support previous research that has found associations between maternal depressive symptoms and parental distress (Cornish et al., 2006; Horowitz & Goodman, 2004; Misri et al., 2006; Sidor et al., 2011), and maternal depressive symptoms and dysfunctional parent-child interaction (Mason et al., 2011; Sidor et al., 2011). There have been conflicting findings with regard to difficult child stress and maternal depressive symptoms. Some studies have reported a connection (Britton, 2011; Cornish et al., 2006; McGrath et al., 2008; Milgrom & McCloud, 1996), whereas other studies have not found such an association (Misri et al., 2006; Pritchard et al., 2012). The two studies that did not find relations between maternal depressive symptoms and a more difficult child were unusual in that one had a sample of preterm infants (Pritchard et al., 2012) and the other used the full Parenting Stress Index, rather than the PSI-Short Form, which may account for some differences. The child domain of the full PSI measures things such as distractibility, and the ability to reinforce the parent, whereas those items are grouped in the Parent-Child Dysfunctional Interaction subscale of the PSI-SF. In any event, the preliminary findings indicated that perceptions of a difficult child and maternal depressive symptoms were related.
Structural equation models explored directionality of maternal depressive symptoms and parenting stress over the first 14 months postpartum. For overall parenting stress and maternal depressive symptoms, the unidirectional model, with parenting stress predicting depressive symptoms, fit the data best. There were significant cross-lagged effects of earlier parenting stress predicting later maternal depressive symptoms, supporting the hypothesis. These findings support cognitive theory, which suggests that stress activates depressive symptoms (Beck, 1976), and is consistent with the few studies finding that concurrent parenting stress predicted maternal depressive symptoms (Honey, Morgan, & Bennett, 2003; Horowitz & Goodman, 2004).
Although the unidirectional model was the best-fitting model for parental distress and depressive symptoms, the hypothesis that there would be significant cross-lagged effects of parental distress to maternal depressive symptoms in the SEM model was not supported. This was surprising given the strength of the correlations. Other research has also examined parental distress and postpartum depressive symptoms and found a strong association between the two, but because parental distress was only measured at one timepoint in those studies, no conclusions could be made regarding directionality (Horowitz & Goodman, 2004; Sidor et al., 2011). There are likely other important factors, such as social support, that may mediate the relations between parental distress and maternal depressive symptoms. If a woman is experiencing significant distress but has a good support system, perhaps this buffers the development of depressive symptoms. Additionally, the majority of women in this sample lived with their husband or partner, suggesting that they have a certain level of support others may not have. It would also be interesting to explore if cognitive vulnerabilities such as a ruminative response style may interact with parental distress. Rumination, or passively and repetitively focusing on the sources and consequences of one’s distress, has been suggested as a possible mechanism through which depression is intensified and it is associated with more depressive symptoms, lower levels of self-efficacy, and reduced problem-solving skills (Lyubomirsky & Nolen-Hoeksema, 1995; Lyubomirsky, Tucker, Caldwell, & Berg, 1999; Nolen-Hoeksema, 2000; Treynor, Gonzalez, & Nolen-Hoeksema, 2003), all of which could amplify feelings of parental distress and exacerbate depressive symptoms. Lastly, there were low levels of depressive symptoms in this sample. More heterogeneity in depressive symptoms may be required to understand how parental distress and depressive symptoms are related over time.
For maternal depressive symptoms and difficult child stress, a unidirectional model fit the data best, however, it was not the hypothesized stress predicting depressive symptoms model, but the alternative depressive symptoms predicting stress model. There was a cross-lagged effect for earlier depressive symptoms predicting later difficult child stress, indicating that depressed mothers are more likely to perceive their child as difficult. We hypothesized that a unidirectional model would fit best with significant cross-lagged effects of difficult child stress to maternal depressive symptoms, believing that having a difficult child would precede the increase in depressive symptoms. The results, however, suggest that earlier maternal depressive symptoms increase the likelihood that mothers will view their child as difficult, which is supported by some previous research. Gartstein et al. (2010), using latent growth curve modeling, found that 4-month maternal depressive symptoms were associated with significant increases in mother-reported infant fearfulness over the first year postpartum. Although they did not explore the bidirectional effects over time of depressive symptoms and infant temperament, the results correspond with the results of this study, indicating that women with higher levels of maternal depressive symptoms are more likely to perceive their child as difficult. A next step in the examination of this relationship would be to explore independent ratings of infant temperament along with maternal depressive symptoms over time and would also address a limitation of this study, which was that there was no independent rating of infant temperament through observation. Mothers who are higher in depressive symptoms may report their children as being more difficult, which compromises the validity of maternal report and indicates the need for an independent rating of infant temperament (Gartstein, Bridgett, Dishion, & Kaufman, 2009; Najman, Bor, Andersen, O’Callaghan, & Williams, 2000).
We hypothesized that a bidirectional relationship would exist between parent-child dysfunctional interaction and depressive symptoms, proposing that mothers who felt stress related to their interactions with their child would also feel more depressed and feeling more depressed in turn would make them feel more stress regarding their interactions with their child (Beck, 1976; Cummings & Davies, 1994). However, this hypothesis was not supported as the bidirectional model was just outside the acceptable fit criterion, indicating that the significant cross-lagged paths were not interpretable or conclusive. The limitations of this sample may explain why the model did not fit well, as the majority of the sample had the support of a partner, which may buffer the effects of depression and stress. Additionally, if the mother worked outside the home, there would be less opportunity for interaction with the child and, therefore, less stress.
Additional limitations of this study were that the women in the sample were primarily white, highly educated, and had relatively high levels of household income. Women who dropped from the study by 14 months were less educated, younger, and had more than one child than those who remained. These factors limit the generalizability of the results.
Clinical implications of this research include the need to focus on women’s specific needs and understand that different types of stress have distinctive associations with depressive symptoms. For example, knowing that women who are higher in depressive symptoms are more likely to experience stress because they view their infants as difficult and are less likely to have a positive outlook, clinicians could focus on the positive, reinforcing aspects of infants’ behavior, such as when the infant smiles at the mother. This may also alleviate stress related to the parent-child interaction, since this particular type of stress appears to have a reciprocal relationship with depressive symptoms. The findings also support the importance of normalization of mothers’ feelings and reassurance of mothers that their infants’ behavior is typical and appropriate. Problem-solving aimed at helping mothers to develop coping strategies when their infants are particularly difficult for them may also be useful. Emphasis on the time-limited nature of infancy may also be of benefit for women. As infants mature and develop into toddlers, they become much more autonomous and need less care, which may alleviate mothers’ stress. The aforementioned strategies could be used in home-based interventions, whether the clinician is a paraprofessional home visitor, infant mental health specialist, or visiting nurse. Pediatricians’ offices consistently see mothers and infants over the first year and it would be important to incorporate questions into pediatric visits to ask about day-to-day stressors and acknowledge that the mother’s wellbeing is important, not just the physical health of the infant. This would provide women with an opportunity to be heard and may open up a dialog that women may be embarrassed or ashamed to broach on their own.
This study provides a first step for examining parenting stress longitudinally, something that has been overlooked in prior research. Despite the call for transactional research that examines risk factors for children’s development (Cummings & Davies, 1994), very few studies have examined parenting stress in conjunction with maternal depressive symptoms in longitudinal studies. More research is needed with larger, more diverse samples. It may also be useful to examine the development of parenting stress and depressive symptoms with women’s depression risk as a moderator, as well as including other variables, such as social support and treatment status. We found that there were clearly different patterns with regard to maternal depressive symptoms and specific types of parenting stress. No one model fit best across the different domains of parenting stress and it is vital that researchers and clinicians continue to consider that parenting stress consists of several unique factors that may relate differently with maternal depressive symptoms. Having a better understanding of how these different aspects of parenting stress and depressive symptoms may interact will provide clinicians and researchers with opportunities to develop better and more targeted interventions for depressed mothers.
References
- Abidin RR. Parenting Stress Index, third edition: Professional manual. Odessa, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- Ashman SB, Dawson G, Panagiotides H. Trajectories of maternal depression over 7 years: Relations with child psychophysiology and behavior and role of contextual risks. Development and Psychopathology. 2008;20(1):55–77. doi: 10.1017/S0954579408000035. [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: Meridian; 1976. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory – II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck CT. The effects of postpartum depression on child development: A meta-analysis. Archives of Psychiatric Nursing. 1998;12(1):12–20. doi: 10.1016/s0883-9417(98)80004-6. [DOI] [PubMed] [Google Scholar]
- Britton JR. Infant temperament and maternal anxiety and depressed mood in the early postpartum period. Women & Health. 2011;51(1):55–71. doi: 10.1080/03630242.2011.540741. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Beverly Hills, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Cornish AM, McMahon CA, Ungerer JA, Barnett B, Kowalenko N, Tennant C. Maternal depression and the experience of parenting in the second postnatal year. Journal of Reproductive and Infant Psychology. 2006;24(2):121–132. [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Child Psychology & Psychiatry & Allied Disciplines. 1994;35(1):73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Developmental psychopathology and family process: Theory, research and clinical implications. New York: Guilford Press; 2000. [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108(1):50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Bridgett DJ, Dishion TJ, Kaufman NK. Depressed mood and maternal report of child behavior problems: Another look at the depression-distortion hypothesis. Journal of Applied Developmental Psychology. 2009;30:149–160. doi: 10.1016/j.appdev.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gartstein MA, Bridgett DJ, Rothbart MK, Robertson C, Iddins E, Ramsay K, et al. A latent growth examination of fear development in infancy: Contributions of maternal depression and the risk for toddler anxiety. Developmental Psychology. 2010;46(3):651–668. doi: 10.1037/a0018898. [DOI] [PubMed] [Google Scholar]
- Gelfand DM, Teti DM, Fox CR. Sources of parenting stress for depressed and nondepressed mothers of infants. Journal of Clinical Child Psychology. 1992;21(3):262–272. [Google Scholar]
- Gerdes AC, Hoza B, Arnold LE, Pelham WE, Swanson JM, Wigal T, et al. Maternal depressive symptomatology and parenting behavior: Exploration of possible mediators. Journal of Abnormal Child Psychology. 2007;35(5):705–714. doi: 10.1007/s10802-007-9134-3. [DOI] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behavior and Development. 2010;33:1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honey KL, Morgan M, Bennett P. A stress-coping transactional model of low mood following childbirth. Journal of Reproductive and Infant Psychology. 2003;21(2):129–143. [Google Scholar]
- Horowitz JA, Goodman J. A longitudinal study of maternal postpartum depression symptoms. Research and Theory for Nursing Practice: An International Journal. 2004;18(2):149–163. doi: 10.1891/rtnp.18.2.149.61285. [DOI] [PubMed] [Google Scholar]
- Ji S, Long Q, Newport D, Na H, Knight B, Zach EB, et al. Validity of depression rating scales during pregnancy and the postpartum period: Impact of trimester and parity. Journal of Psychiatric Research. 2011;45(2):213–219. doi: 10.1016/j.jpsychires.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York, NY, USA: Guilford Press; 2005. [Google Scholar]
- Lyubomirsky S, Nolen-Hoeksema S. Effects of self-focused rumination on negative thinking and interpersonal problem solving. Journal of Personality and Social Psychology. 1995;69(1):176–190. doi: 10.1037//0022-3514.69.1.176. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Tucker KL, Caldwell ND, Berg K. Why ruminators are poor problem solvers: Clues from the phenomenology of dysphoric rumination. Journal of Personality and Social Psychology. 1999;77(5):1041–1060. doi: 10.1037//0022-3514.77.5.1041. [DOI] [PubMed] [Google Scholar]
- Mason ZS, Briggs RD, Silver EJ. Maternal attachment feelings mediate between maternal reports of depression, infant social-emotional development, and parenting stress. Journal of Reproductive and Infant Psychology. 2011;29(4):382–394. [Google Scholar]
- McGrath JM, Records K, Rice M. Maternal depression and infant temperament characteristics. Infant Behavior & Development. 2008;31(1):71–80. doi: 10.1016/j.infbeh.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milgrom J, McCloud P. Parenting stress and postnatal depression. Stress Medicine. 1996;12(3):177–186. [Google Scholar]
- Misri S, Reebye P, Milis L, Shah S. The impact of treatment intervention on parenting stress in postpartum depressed mothers: A prospective study. American Journal of Orthopsychiatry. 2006;76(1):115–119. doi: 10.1037/0002-9432.76.1.115. [DOI] [PubMed] [Google Scholar]
- Najman JM, Bor W, Andersen MJ, O’Callaghan M, Williams GM. Preschool children and behaviour problems: A prospective study. Childhood. 2000;7:439–466. [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109(3):504–511. [PubMed] [Google Scholar]
- Pianta RC, Egeland B. Relation between depressive symptoms and stressful life events in a sample of disadvantaged mothers. Journal of Consulting and Clinical Psychology. 1994;62(6):1229–1234. doi: 10.1037//0022-006x.62.6.1229. [DOI] [PubMed] [Google Scholar]
- Pritchard MA, Colditz PB, Cartwright D, Gray PH, Tudehope D, Beller E. Six-week postnatal depression predicts parenting stress profiles in mothers of preterm children. Journal of Reproductive and Infant Psychology. 2012;30(3):303–311. [Google Scholar]
- Schumacker RE, Lomax RG. A beginner’s guide to structural equation modeling. Third edition. New York: Routledge; 2010. [Google Scholar]
- Sidor A, Kunz E, Schweyer D, Eickhorst A, Cierpka M. Links between maternal postpartum depressive symptoms, maternal distress, infant gender and sensitivity in a high-risk population. Child and Adolescent Psychiatry and Mental Health. 2011;5 doi: 10.1186/1753-2000-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27(3):247–259. [Google Scholar]