Abstract
Individual health outcomes differ greatly between neighborhoods, and recent research has begun to examine how neighborhood environment affects individual health. A common hypothesis is that the inequitable distribution of healthcare resources limits access to health care for individuals in disadvantaged neighborhoods, causing poorer long-term health. Yet, research has not examined if neighborhood environment actually affects an individual’s ability to access primary care. Data from the Los Angeles Family and Neighborhood Survey suggests there is significant variation between neighborhoods in an individual’s ability to access primary care. This neighborhood-level effect is not explained by the composition of individuals living in the neighborhood. Four mechanisms through which neighborhood environment could affect an individual’s ability to access primary care are examined: (1) neighborhood information networks, (2) neighborhood health behavior norms, (3) neighborhood social capital and (4) neighborhood healthcare resources. Social capital and healthcare resources significantly predict an individual’s primary care access. Since differences in primary care access may explain individual-level health disparities between neighborhoods, policies designed to improve primary care access must account for both individual and neighborhood effects.
Keywords: Neighborhood environment, Primary care, Healthcare access, USA, Individual effects
Introduction
Individuals who live in poorer and more disadvantaged neighborhoods have inferior health outcomes (Acevedo-Garcia, 2000; Pickett & Pearl, 2001; Robert, 1999). Several reviews of studies using multilevel analysis have concluded that neighborhood socioeconomic status (SES) has an independent effect on a wide variety of individual health outcomes even when controlling for individual SES and other individual characteristics (Ellen, Mijanovich, & Dillman, 2001; Pickett & Pearl, 2001; Robert, 1999). However, the mechanisms linking neighborhood environment to individual health are not well understood. Differences between neighborhoods in the availability of structural resources, including healthcare, have led researchers to hypothesize one mechanism is decreased access to and use of health care (Macintyre, Ellaway, & Cummins, 2002). This paper examines whether restricted primary care access is one plausible mechanism explaining the disparities in individual health between neighborhoods.
Primary care and health outcomes
Primary care is defined as care that gives patients entry into the healthcare system, coordinates healthcare services for patients, provides care to the same patient over time, is comprehensive (i.e. curative and preventive) and takes into account the patient’s societal context outside the healthcare system (Macinko, Starfield, & Shi, 2003). This integration of curative and preventive healthcare over time improves individual and population health (Macinko et al., 2003; Shi, 1994) by helping patients prevent and control illnesses (Blumenthal, Mort, & Edwards, 1995). Macinko et al. (2003) compared mortality rates between countries with similar SES and found countries with stronger primary care systems have lower all-cause and all-cause preventable mortality.
Furthermore, studies have found access to primary care can attenuate the negative effects of lower SES and income inequality on health (Casanova and Starfield, 1995; Shi, Starfield, Kennedy, & Kawachi, 1999; Shi, Starfield, Politzer, & Regan, 2002). Casanova and Starfield (1995) link SES, primary care and preventable hospitalizations. While children from different social classes in the United States have different rates of preventable hospitalizations, they argue these differences are not observed in Spain where all children have a regular source of care (RSOC). Similarly, Shi et al. (1999) found that although income inequality between states significantly predicted all-cause mortality, once models controlled for primary care physician supply, income inequality was not a significant predictor of all-cause mortality.
Predictors of primary care access
Past research has largely focused on individual characteristics that predict primary care access and utilization. The Anderson Behavioral Model of Health Service Use traditionally predicts healthcare use based on predisposing, enabling and need factors. Predisposing factors influence an individual’s inclination to utilize health care, such as health beliefs. Enabling factors help individuals access care, such as having insurance coverage to help pay for care. These factors must be present for use to take place. Need factors reflect individuals’ perception of how important it is to access care based on their health status. All three factors are essential in explaining healthcare utilization (Andersen, 1995; Gross, 1972).
Yet, recent research argues an individual’s ability to access healthcare is independently affected by where he or she lives. Characteristics of an individual’s Metropolitan Statistical Area (MSA) were found to affect his or her healthcare access, even when controlling for differences in the composition of individuals living in these MSAs (Brown et al., 2004; Cunningham & Kemper, 1998). Brown et al. (2004) used the 1995 and 1996 National Health Interview Survey and found significant variation across MSAs in the odds of whether low-income adults visited a physician in the last year. Cunningham and Kemper (1998) found over a two-fold difference in the proportion of the uninsured who reported having difficulty accessing healthcare among MSAs included in the Community Tracking Study. These studies selected MSAs with populations of at least 330,000 and 200,000, respectively. Clearly, MSAs are much larger than an individual’s actual neighborhood, and researchers have not examined if neighborhood environment independently affects healthcare access using a more precise geographic definition of neighborhood, such as census tracts. Census tracts have a moderate population size (approximately 5500) and lack man-made or natural cross-cutting boundaries (e.g. freeways) (Sastry, Ghosh-Dastidar, Adams, & Pebley, 2003).
This paper finds that neighborhood (defined as census tract) environment affects an individual’s primary care access. It then examines potential mechanisms between neighborhood environment and individual primary care access by examining the effects of neighborhood information networks, health behavior norms, social capital and healthcare resources on primary care access.
Neighborhood environment and primary care access
Strong neighborhood information networks may encourage individuals to use primary care because individuals often seek advice from peers before seeking out preventive healthcare (Earp et al., 2002; Levy-Storms & Wallace, 2003). Levy-Storms and Wallace (2003) examined the effect of informal health communication networks on mammogram use among Samoan women in Los Angeles. Women who were the most central in these networks were significantly more likely to plan to have a mammogram and to have had a recent mammogram compared to women who were outside of these networks. Individuals living in neighborhoods with strong information networks may get advice on how to access primary care from their neighbors (Ellen et al., 2001) encouraging primary care use.
The decision to use primary healthcare (especially preventive services) can be viewed as a health-seeking behavior, similar in some ways to other health-related behaviors, such as the decision not to smoke. Social norms or the shared attitude about the importance of health-seeking behaviors differ between neighborhoods, and individuals often behave in concordance with the social norms of their environment (Curry et al., 1993; Ellen et al., 2001). Thus, if an individual lives in a neighborhood with social norms that encourage practicing healthy behaviors, he or she may be more likely to obtain primary care.
Social capital results from aspects of the social structure that provide resources to individuals and facilitate collective action. It can be conceptualized into two components: (1) cognitive and (2) structural (Kawachi & Berkman, 2000; Subramanian, Kim, & Kawachi, 2002). The cognitive component assesses individuals’ perceptions of the level of interpersonal trust, sharing and reciprocity in the community (Subramanian et al., 2002). Sampson (2003) argues this cognitive component can be viewed as collective efficacy, or the expectation that community members will act collectively for the common good, securing needed social goods. Thus, collective efficacy may help keep the healthcare system accountable to the community (Hendryx, Ahern, Lovrich, & McCurdy, 2002; Steinberg & Baxter, 1998). Steinberg and Baxter (1998) conducted a qualitative case study of 12 MSAs in the Community Tracking Study. MSAs where residents shared common values toward healthcare were more effective at holding the local healthcare system accountable to the needs of residents, such as protecting access to care among vulnerable populations. Individuals in communities with greater community social trust, civic engagement and self-esteem have more trust in their physicians (Ahern & Hendryx, 2003), which may lead to increased healthcare utilization. Neighborhood social capital may also increase individual self-esteem (Kawachi & Berkman, 2000) and in turn affect the importance people place on protecting their health and their likelihood of seeking primary care.
The structural component of social capital includes the extent and intensity of associational links (e.g. density of civic associations) (Subramanian et al., 2002). Individuals living in neighborhoods with well-established structural aspects of social capital may also have more social interaction. This could lead to direct functional support that increases primary care access. For example, neighbors could provide child care while an individual goes to the doctor. Thus, neighborhood social capital may increase primary care access through collective efficacy, psychosocial effects and direct functional support.
Finally, neighborhoods differ in their supply of healthcare resources. Areas with greater wealth have more healthcare resources (Jiang & Begun, 2002). The types of industries in a community affect healthcare resources since certain types of employers are more likely to provide private health insurance coverage, which has higher reimbursement rates than public insurance (Brown, Ponce, & Rice, 2001; Cunningham & Ginsburg, 2001; Komaromy, Lurie, & Bindman, 1995). Thus, the spatial distribution of healthcare resources is far from equitable with severely disadvantaged neighborhoods, such as inner cities, having fewer healthcare resources (Fossett, Perloff, Kletke, & Peterson, 1992; Grumbach, Coffman, Young, Vranizan, & Blick, 1998). Also, populations with a greater percentage of the very young or elderly may demand more healthcare since these ages have greater healthcare needs, bringing more providers to an area (Cunningham & Kemper, 1998; Jiang & Begun, 2002). Individuals living in neighborhoods with greater healthcare resources may be more likely to use primary care due to shorter travel distances required to see a provider (Gross, 1972) and greater provider choice.
This study examines if the above neighborhood characteristics influence an individual’s primary care access. Individuals living in a neighborhood with stronger information networks, stronger social norms against negative health behaviors, greater social capital and more healthcare resources are hypothesized to have better primary care access.
Methods
Data source
Analyses are based on Wave 1 of the 2000–2001 Los Angeles Family and Neighborhood Survey (L.A. FANS), which was designed to examine the effects of family and neighborhood environment on children’s physical and social development. Thus, the detailed information at the individual, family and neighborhood level allows researchers to use multi-level models to test emerging hypotheses about the social determinants of health for adults and children. Further information on L.A. FANS can be found at www.lasurvey.rand.org.
L.A. FANS defined a neighborhood as a census tract. The 1652 Los Angeles County census tracts in 1990 were divided into very poor, poor and non-poor strata based on percent in poverty. A total of 65 tracts were sampled: 20 each from the very poor and poor strata and 25 from the non-poor stratum. Within each sampled tract, 40–50 dwelling units were sampled at random, with an oversample of households with children. Within each household, L.A.FANS randomly sampled one adult for interview. A total of 2623 adult respondents were interviewed. For more details, see Sastry et al. (2003). This analysis was limited to randomly selected adults (RSAs) between 18 and 64.
Outcome measures
Two measures of primary care access were used: (1) having a RSOC at the time of interview and (2) receiving a preventive check-up in the last 2 years. Having a RSOC has been consistently linked to high-quality primary care, such as receiving check-ups or preventive screenings, and reporting greater patient satisfaction (Bindman, Grumbach, Osmond, Vranizan, & Stewart, 1996; Ettner, 1999; Weiss & Ramsey, 1989). Respondents who reported having a doctor’s office, clinic, health center, health maintenance organization (HMO) or hospital outpatient department for receiving a physical were classified as having a RSOC. Respondents who reported no RSOC went to the hospital emergency room for a physical, or gave friends or family members as their RSOC were classified as having no RSOC. Eighty percent of the sample had a RSOC at the time of interview (Table 1).
Table 1.
Distribution of individual-level controls; L.A. FANS 2000–2001, adults aged 18–64 years old
| Total % or median of the sample (SD)a | |
|---|---|
| Outcome measures | |
| Has a RSOCb | |
| Yes | 80 |
| No | 20 |
| Received a check-up in last two years | |
| Yes | 71 |
| No | 29 |
| Individual covariates | |
| Predisposing factors | |
| Gender | |
| Male | 51 |
| Female | 49 |
| Race | |
| Latino | 40 |
| White | 34 |
| Black | 10 |
| Asian/Pacific Islander or Other | 16 |
| Age | |
| Less than 25 years old | 22 |
| 25–50 years old | 61 |
| 51–64 years old | 17 |
| Marital status | |
| Never married | 38 |
| Married | 49 |
| Divorced or widowed | 13 |
| RSA has child aged 0–5 in household | |
| Yes | 21 |
| No | 79 |
| Employment status | |
| Unemployed | 26 |
| Working full time in high-status occupation | 30 |
| Working full time in low-status occupation | 32 |
| Working part time | 12 |
| Current smoker | |
| Yes | 34 |
| No | 66 |
| Enabling factors | |
| Language of interview | |
| English | 76 |
| Spanish | 24 |
| Educational attainment | |
| Less than high school | 22 |
| High school graduate | 23 |
| Some college | 31 |
| College graduate or post graduate | 23 |
| Median yearly family income | $36,002 (83,634) |
| Reported $0 for family income | |
| Yes | 3 |
| No | 97 |
| Reported $0 for non-housing assets | |
| Yes | 13 |
| No | 87 |
| Insured | |
| Yes | 70 |
| No | 30 |
| Need factors | |
| Has chronic conditionc | |
| Yes | 33 |
| No | 67 |
| N = 2080b | |
SD = Standard deviation.
Unweighted N’s and weighted percentages and medians were reported. Percentages may not add up to 100 due to rounding.
Except for the percentage of respondents that have a RSOC all percents and medians are based on the sample of individuals used for the check-up analyses (n = 2080). There is little difference in the basic descriptive statistics between these two samples.
Respondents were classified as having a chronic condition if they reported ever being told by a doctor they had high blood pressure, diabetes, cancer, chronic lung disease, heart attack, coronary heart disease, arthritis, asthma or major depression.
Simply having a RSOC does not guarantee primary care use, so another set of models predicted receiving a preventive check-up anytime during the previous 2 years. This timeframe was chosen based on previous primary care research (Brown, Ojeda, Wyn, & Levan, 2000) and on current guidelines for frequency of preventive screenings (e.g. hypertension) (National Guideline Clearing House, 2002). Seventy-one percent of the sample received a check-up in the last 2 years (Table 1).
Individual-level control variables
This paper examines whether the neighborhood environment affects individual primary care access even when controlling for individual characteristics. Table 1 gives the distribution of the individual control variables that were selected based on the Andersen Behavioral Model of Health Services Use and past research predicting primary care access (Andersen, 1995; Bloom, Simpson, Cohen, & Parsons, 1997; DeVoe, Fryer, Phillips, & Green, 2003; Joung, Meer, & Mackenbach, 1995; Woloshin, Schwartz, Katz, & Welch, 1997). Having a RSOC was included as a predictor of receiving a check-up.
The odds of receiving a check-up anytime during the 2 years before the interview were estimated. Check-up analyses included individual characteristics at the beginning of the 2-year period based on information collected in a 2-year retrospective history. Some individual characteristics included in the model were collected only at the time of interview, including education, language of interview, family income, smoking status, chronic conditions and having a RSOC. Sensitivity analyses of limited retrospective information on smoking, education and family income showed these characteristics changed little over the 2-year period. RSOC analyses included individual characteristics at the time of interview. The final samples predicting receiving a check-up and having a RSOC were 2080 and 2041, respectively, due to differences in missing data.
Neighborhood-level independent variables
Table 2 gives the distribution and categorization of neighborhood characteristics from L.A. FANS and Census 2000. RSAs were asked questions about their neighborhood environment and their level of disapproval of different health behaviors. Individual responses within each census tract were averaged to generate a mean score for the entire census tract that was assigned to all individuals living in the same tract. Several neighborhood scores were dichotomized based on their distributions. For example, neighborhoods where people strongly agreed that neighbors were willing to help each other (neighborhood score <2) were compared to neighborhoods where people agreed, were neutral or disagreed that people were willing to help each other (neighborhood score≥2). L.A. FANS was collected during 2000–2001, so neighborhood socioeconomic measures from Census 2000 were also included in the models to supplement attitude measures with more objective measures of the neighborhood environment. Due to redefinition of census tracts between 1990 and 2000, characteristics of 90 tracts are included.
Table 2.
Hypothesized mechanism, distribution and categorization of neighborhood-level variables used to predict primary care access; Census 2000 and L.A. FANS 2000–2001 (adults 18–64, n = 90)
| Neighborhood characteristic | Mean or % (SD) | Categorization |
|---|---|---|
| Information networks | ||
| Percent with high school or greater educationa | 54.5 (23.1) | Quartiles |
| Frequency neighbors ask adviceb | 2.80 (0.29) | Often (1) or sometimes versus rarely or never (4) |
| Number of neighbors talked to in last 30 daysb | 2.37 (0.23) | Linear ranging from 1 (none) to 4 (6 or more) |
| Health behavior norms | ||
| Adult smokingb,c | 2.33 (0.18) | Linear ranging from 1 (do not disapprove) to 3 (strongly disapprove) |
| Social capital | ||
| Percent in same house 5 years agoa | 49.8 (10.4) | Quartiles |
| Predominant ethnic groupa | 63.3 | Predominantly white or Latino versus no predominant group |
| Neighborhood is close-knitb | 2.89 (0.39) | Strongly agree (1) or agree versus unsure, disagree or strongly disagree (5) |
| People are willing to help neighborsb | 2.38 (0.35) | Strongly agree versus agree, unsure, disagree or strongly disagree |
| Neighbors do not share same valuesb | 3.07 (0.35) | Strongly disagree, disagree or unsure versus agree or strongly agree |
| Neighbors can be trustedb | 2.66 (0.46) | Strongly agree or agree versus unsure, disagree or strongly disagree |
| Friends living in neighborhoodb | 1.93 (0.23) | None (1) versus a few, many, most or all (4) |
| Frequency neighbors do favors for one anotherb | 2.33 (0.30) | Often (1) versus sometimes, rarely or never (4) |
| Healthcare resources | ||
| Incomea | $40,861 ($25,728) | Quartiles |
| Percent age 65 or oldera | 7.8 (4.8) | Highest quartile versus lowest three quartiles |
| Percent age 5 or youngera | 10.9 (3.2) | Highest quartile versus lowest three quartiles |
| Highly disadvantaged neighborhooda | 15.6 | Tracts in highest quartile of both unemployment and poverty versus all other |
From Census 2000.
Variables from L.A. FANS measuring neighborhood attitudes are based on questions asked to RSAs in the adult module. A mean score for each neighborhood was calculated by averaging all of the individual responses in the same tract. This mean score was assigned to each individual in the census tract.
The question about smoking disapproval was also asked of another adult in the household, who may be a different person than the RSA. The mean score for neighborhood included responses from all respondents living in the same neighborhood.
The four mechanisms through which neighborhood characteristics are hypothesized to affect primary care access are: (1) information networks, (2) health behavior norms, (3) social capital and (4) healthcare resources. Measures of information networks include education level from Census 2000, the frequency that neighbors ask advice from one another and the number of neighbors individuals spoke to in the last 30 days from L.A. FANS. Individuals may learn more about health-care opportunities and practices by talking to highly educated neighbors who can effectively navigate the healthcare system.
Health behavior norms are measured by neighborhood approval of adults regularly smoking cigarettes. This item came from the Monitoring the Future Study (www.monitoringthefuture.org), a yearly study measuring youth health behaviors and attitudes, and was modified to ask about adult behaviors. The response options were do not disapprove, disapprove and strongly disapprove. L.A. FANS also measured disapproval of binge drinking and marijuana use for adults over 18. These measures were excluded because it is unclear if the questions are measuring attitudes toward health behaviors or illegal activity (18 years old was included in the question for drinking).
Measures used in L.A. FANS to measure social capital and information networks were derived from the Project for Human Development in Chicago neighborhoods (Sampson, 2003). L.A. FANS measures neighborhood collective efficacy, such as the level of mutual trust between neighbors (e.g. neighborhood is close knit) and perceived norms of reciprocity (e.g. willingness to help neighbors), and measures of direct social interaction and functional support (e.g. number of friends living in neighborhood). Residential stability and whether there is a dominant ethnic group (either white or Latino; no neighborhoods were predominantly Black or Asian-Pacific Islander) in the neighborhood from Census 2000 are measures of population stability and homogeneity.
A direct measure of healthcare resources, such as primary care physician supply, is not included in the models due to the low quality of the limited data available for healthcare resources at the census tract level. Instead, neighborhood measures that proxy availability of health-care resources are included. These include the median income of tracts, the age structure of the population and whether the neighborhood is severely disadvantaged from Census 2000. A measure of severely disadvantaged neighborhoods was constructed by comparing neighborhoods in the highest quartile of percent of population in both poverty status and unemployment from Census 2000 to all other neighborhoods.
Analyses
Statistical analyses were completed using STATA 8.0 updated with the GLLAMM program for random intercept multilevel models (Rabe-Hesketh, Skrondal, & Pickles, 2005; Statacorp, 2003). Analyses are weighted using weights created for the L.A. FANS RSAs that adjust for sample design and eligibility. Differential non-response was not a major issue in L.A. FANS, and the survey design provided detailed information on factors associated with non-response that were incorporated into the weighting. For more detail on response rates see Sastry and Pebley (2003).
The first question of interest is whether the neighborhood environment affects primary care access even when controlling for individual characteristics. Fixed effects multilevel logit models that included both individual characteristics and a fixed effect for neighborhood predicted both outcomes. The fixed effect was included as a dummy variable for each census tract. Wald-tests were used to test whether the dummy variables for neighborhood were significant as a group in models predicting both primary care measures. If significant, the neighborhood environment affects primary care access independent of individual characteristics.
To examine whether individual characteristics and neighborhood environment independently predict primary care access, a fixed effects model that only includes dummy variables for each tract was also run. Using both this model and the fixed effects model discussed above including tract dummy variables and individual characteristics, the predicted neighborhood means and variances of having a RSOC or check-up were generated. The change in variance of the predicted means between the two fixed effects models is the proportion of the between neighborhood variance that is due to differences in the types of individuals that live in different neighborhoods (i.e. composition).
Fixed effects models do not give insight into which neighborhood characteristics affect primary care access because specific neighborhood characteristics are not included in the model. A two-level (level 1 = individuals, level 2 = census tract) random intercept logit model included all the individual and neighborhood characteristics from Tables 1 and 2 in the actual model. The random intercept is shared by all individuals living in the same census tract and serves as an indirect control for neighborhood factors not included in the models that may affect primary care access. Adaptive Gaussian quadrature was used to estimate the marginal likelihood because it has been found to provide accurate estimates for dichotomous data with various cluster sizes (Rabe-Hesketh et al., 2005). The variance of the random intercept was calculated for three models: (1) no covariates included, (2) only individual characteristics included and (3) both individual and neighborhood characteristics included.
Results
Does the neighborhood environment affect primary care access?
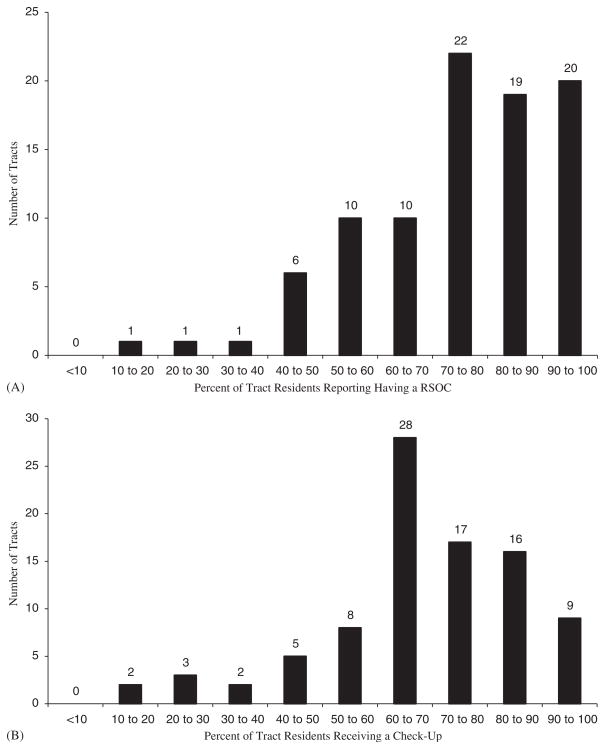
As shown in Fig. 1A and B, the percentage of residents in a census tract that report having a RSOC or receiving a check-up varies largely between census tracts. Across all neighborhoods, the proportion of a census tract with a RSOC ranged from 12% to 100%, while this proportion ranged from 14% to 100% for receiving a check-up. The average number of respondents per tract is 23 for both outcomes.
Fig. 1.
(A) Histogram showing the distribution of residents reporting having a RSOC in each census tract; L.A. FANS 2000–2001 (Adults 18–64 years old, n = 2041). The mean number of respondents per tract is 23. Tracts with 100% have a range of 2–33 people. (B) Histogram showing the distribution of residents receiving a check-up in each census tract; L.A. FANS 2000–2001 (Adults 18–64 years old, n = 2080). The mean number of respondents per tract is 23. Tracts with 100% have a range of 2–9 people.
The significant variation between neighborhoods remains in multilevel models. In models that include individual characteristics and a fixed effect for neighborhood, there was significant variation between neighborhoods for both outcomes (χ2 = 134.59, p = 0.0004– RSOC; χ2 = 159.43, p≤0.001–check-up).
Furthermore, the variance of the predicted means by neighborhood changes little between a model that includes only a fixed effect for neighborhood and a model that includes both a fixed effect for neighborhood and individual characteristics. In models predicting having a RSOC, the variance decreases from 1.3414 to 0.9979 when individual characteristics are included, a 26% reduction. For receiving a check-up in the last 2 years, this variance decreases from 0.9384 to 0.9004, a 4% reduction. These results imply little of the neighborhood effect on primary care access, especially for receiving a check-up, is explained by the composition of individuals in the neighborhood. Thus, neighborhood environment and individual characteristics have independent and significant effects on an individual’s ability to access primary care.
Random intercept multilevel logit model
Table 3 shows the adjusted odds ratio and 95% confidence intervals of the random intercept multilevel model predicting having a RSOC and receiving a checkup in the last 2 years when both individual and neighborhood characteristics are included. The bottom of Table 3 gives the variance of the random intercept when (1) no covariates are included, (2) only individual characteristics are included and (3) both individual and neighborhood characteristics are included. The inclusion of both individual and neighborhood characteristics decreases the variance of the random intercept for both outcomes. The significance levels for the individual-level parameter estimates between the model that only includes individual characteristics and the model that includes both individual and neighborhood characteristics do not change (data not shown), further emphasizing the independent roles of individual and neighborhood characteristics.
Table 3.
Adjusted odds ratios and 95% confidence intervals of multilevel random intercept logit models predicting having a RSOC and receiving a check-up in the last 2 years; L.A. FANS 2000–2001 (Adults aged 18–64 years old)a
| Has a RSOC (n = 2041)
|
Received a check-up in the last 2 years (n = 2080)
|
|||
|---|---|---|---|---|
| AORb | 95% CI | AOR | 95% CI | |
| Individual characteristics | ||||
| Predisposing factors | ||||
| Male (ref = female) | 0.28c | (0.17, 0.47) | 0.36c | (0.23, 0.57) |
| Race (ref = Latino) | ||||
| White | 0.82 | (0.43,1.58) | 0.86 | (0.49, 1.50) |
| Black | 1.00 | (0.44, 2.24) | 2.13 | (0.84, 5.39) |
| Asian/Pacific Islander or Other | 0.42d | (0.18, 1.00) | 0.59d | (0.34, 1.02) |
| Marital status (ref = never married) | ||||
| Married | 1.45d | (0.94, 2.24) | 0.96 | (0.65, 1.43) |
| Divorced or widowed | 1.42 | (0.70, 2.89) | 1.46d | (0.96, 2.21) |
| Employment status (ref = unemployed) | ||||
| Working full time in high-status occupation | 0.88 | (0.50, 1.55) | 0.45c | (0.25, 0.79) |
| Working full time in low-status occupation | 1.60d | (0.93, 2.74) | 0.74 | (0.46, 1.19) |
| Working part time | 0.91 | (0.39, 2.14) | 0.58d | (0.32, 1.05) |
| Enabling factors | ||||
| Education (ref = less than high school) | ||||
| High school graduate | 1.42 | (0.88, 2.29) | 1.15 | (0.68, 1.95) |
| Some college | 1.26 | (0.69, 2.27) | 1.49 | (0.80, 2.81) |
| College graduate or post graduate | 2.73c | (1.19, 6.24) | 2.58c | (1.31, 5.09) |
| Interviewed in English (ref = Spanish) | 1.72c | (1.00, 2.96) | 0.84 | (0.50, 1.40) |
| Log of family income | 1.35c | (1.06, 1.71) | 0.98 | (0.77, 1.23) |
| Has health insurance (ref = uninsured) | 5.64c | (3.42, 9.28) | 1.52c | (1.04, 2.23) |
| Reports having a RSOC (ref = no RSOC) | — | — | 6.61c | (4.40, 9.95) |
| Need factors | ||||
| Has chronic condition (ref = no chronic condition) | 2.20c | (1.39, 3.49) | 1.87c | (1.18, 2.95) |
| Neighborhood characteristics | ||||
| Information networks | ||||
| Percent of tract with high school or greater education (ref = tract in Q1-lowest)e | ||||
| Q2 | 0.98 | (0.59, 1.65) | 0.70 | (0.42, 1.15) |
| Q3 | 1.23 | (0.65, 2.33) | 0.52c | (0.29, 0.91) |
| Q4-highest | 1.07 | (0.36, 3.19) | 0.44d | (0.17, 1.16) |
| Neighbors ask advice more often (ref = neighbors ask advice less often) | 0.83 | (0.50, 1.38) | 0.95 | (0.63, 1.43) |
| Number of neighbors talked to in last 30 days; linear ranging from 1 (none) to 4 (6 or more) | 0.62 | (0.20, 1.86) | 0.31c | (0.12, 0.79) |
| Health behavior norms | ||||
| Adult smoking; linear ranging from 1 (do not disapprove) to 3 (strongly disapprove) | 3.62d | (0.96, 13.68) | 1.95 | (0.75, 5.07) |
| Social capital | ||||
| Percent of tract in same house 5 years ago (ref = tract in Q1-lowest)e | ||||
| Q2 | 1.92c | (1.15, 3.21) | 0.68d | (0.44, 1.07) |
| Q3 | 2.20c | (1.30, 3.73) | 0.74 | (0.50, 1.11) |
| Q4-highest | 1.84d | (0.98, 3.46) | 0.73 | (0.45, 1.17) |
| Dominant ethnic group (ref = no) | ||||
| Yes | 0.65d | (0.41, 1.05) | 0.92 | (0.63, 1.33) |
| Neighborhood is more close-knit (ref = neighborhood is less close knit) | 0.83 | (0.49, 1.38) | 0.68d | (0.46, 1.01) |
| People are more willing to help neighbors (ref = people are less willing to help neighbors) | 3.95c | (1.66, 9.39) | 2.45c | (1.31, 4.58) |
| Disagree that neighbors do not share same values (ref = agree that neighbors do not share same values) | 0.70 | (0.46, 1.09) | 0.74 | (0.50, 1.09) |
| Neighbors can be trusted (ref = neighbors are less trustworthy) | 0.99 | (0.59, 1.66) | 1.31 | (0.87, 1.97) |
| Friends living in neighborhood (ref = no friends in neighborhood) | 0.93 | (0.64, 1.35) | 1.12 | (0.85, 1.49) |
| Neighbors do more favors for one another (ref = neighbors do fewer favors) | 0.35c | (0.17, 0.71) | 0.58c | (0.35, 0.98) |
| Healthcare resources | ||||
| Median income (ref = tracts in Q1-lowest)e | ||||
| Q2 | 0.59 | (0.27, 1.31) | 1.10 | (0.58, 2.06) |
| Q3 | 0.84 | (0.40, 1.75) | 1.40 | (0.81, 2.41) |
| Q4-highest | 0.57 | (0.24, 1.35) | 1.77d | (0.93, 3.37) |
| Tract in highest quartile (Q4) of percent of population aged 65 or older (ref = Q1–Q3)e | 1.28 | (0.75, 2.19) | 1.75c | (1.11, 2.77) |
| Tract in highest quartile (Q4) of percent of population under age 5 (ref = Q1–Q3)e | 1.50 | (0.76, 2.97) | 1.68d | (0.92, 3.05) |
| Highly disadvantaged neighborhood (ref = not highly disadvantaged neighborhood) | 1.37 | (0.59, 3.20) | 0.43c | (0.21, 0.87) |
| Variance of random intercept
|
||||
| Has a RSOC | Check-up | |||
|
|
|
|||
| No individual or neighborhood characteristics | 0.82678 | 0.32240 | ||
| Individual characteristics only | 0.43770 | 0.24880 | ||
| Individual and neighborhood characteristics | 0.07152 | 0.03138 | ||
The model also controls for variables listed in Table 1 including, age, having children under 5, reporting no family income, reporting no assets and smoking habits.
AOR = adjusted odds ration; CI = confidence interval.
Significant at p<0.05.
Significant at p<0.10.
Q = quartiles.
For both outcomes, results agree with past research that emphasizes the importance of enabling factors, such as education or income, and need factors, such as having a chronic condition, when predicting healthcare access (Andersen, 1995; Bloom et al., 1997; Devoe et al., 2003; Joung et al., 1995). Individuals with health insurance coverage are significantly more likely to have a RSOC and receive a check-up compared to those without insurance, and individuals with a RSOC had over six times the odds of receiving a check-up compared to those without a RSOC.
Neighborhood characteristics
Neighborhood information networks do not significantly predict having a RSOC. Respondents living in the third quartile of neighborhoods with percent of the population with at least a high school education are significantly less likely to receive a check-up in the last 2 years compared to respondents living in a neighborhood in the lowest quartile of neighborhood education level. There is also a significant negative association between number of neighbors spoken to in the last month and receiving a check-up.
An increase in smoking disapproval from ‘do not disapprove’ to ‘disapprove’ or from ‘disapprove’ to ‘strongly disapprove’ increases the odds of having a RSOC almost four times, which borders on significance (p<0.10). No effect of health behavior norms is seen when predicting receiving a check-up.
For both outcomes, several measures of social capital are significant in contradictory directions. Living in neighborhoods where people are willing to help their neighbors causes individuals to have almost four and over two times the odds of having a RSOC and receiving a check-up, respectively, compared to individuals in neighborhoods where people are less willing to help their neighbors. However, respondents in neighborhoods where neighbors do favors for one another more often have significantly lower odds for both outcomes compared to people in neighborhoods where neighbors do favors for each other less often. Individuals in the second and third quartile of the most residentially stable neighborhoods, as measured by the percent of the tract that lived in the same house 5 years ago, had significantly higher odds of reporting a RSOC compared to individuals in neighborhoods with the least residential stability.
Healthcare resources have no effect on having a RSOC but do significantly predict receiving a check-up in the last 2 years. Individuals living in a tract with a high percentage of the population over 65 have almost two times the odds and individuals living in severely disadvantaged areas have a 57% lower chance of receiving a check-up compared to individuals living in neighborhoods with a lower population of residents over 65 and individuals living in less disadvantaged environments.
Conclusion
Neighborhood environment affects primary care access
Researchers have often hypothesized that one mechanism through which the neighborhood environment affects individual health is decreased access to healthcare (Acevedo-Garcia, 2000; Ellen et al., 2001; Macintyre et al., 2002). Despite this being a common hypothesis, little research has examined whether neighborhood environment independently affects an individual’s ability to access healthcare after controlling for individual characteristics, such as health insurance coverage.
These analyses show that the neighborhood environment significantly affects having a RSOC and receiving a check-up in the last 2 years (Fig. 1), independent of individual characteristics. In multilevel fixed effect logit models that control for individual characteristics, significant variation between neighborhoods remains, indicating that the neighborhood environment affects primary care access even when controlling for individual characteristics. Furthermore, the between neighborhood variance changes little once individual characteristics are included in a model that includes a fixed effect for neighborhood. Therefore, the significant neighborhood effect is not ‘explained away’ by differences in the composition of individuals living in different neighborhoods. Although the significant effect of neighborhood may be due to individual characteristics that are not explicitly controlled for in the models, this is unlikely since most individual characteristics commonly associated with primary care access are included. Results did not change when including more extensive individual controls, such as drinking behavior (data not shown).
How does the neighborhood environment affect primary care access?
Four mechanisms were considered to investigate how the neighborhood environment affects primary care access: (1) information networks, (2) health behavior norms, (3) social capital and (4) healthcare resources. Neighborhood social capital affects primary care access, but the specific mechanism is not clear from these results. Social capital could influence individuals’ primary care access by neighbors providing direct functional support, but this does not appear to be the case. Measures of neighborhood interaction, including neighborhood information networks and frequency neighbors do favors for one another, are not significant or have a negative association with primary care access (Table 3). Individuals living in neighborhoods with greater residential stability are significantly more likely to have a RSOC, which could be a proxy for increased social interaction between neighbors. However, this also may be because individuals who move may take some time to find a new RSOC, causing neighborhoods with a high percentage of recent moves to have a lower proportion of the population with a RSOC.
The ability of neighborhood social capital to influence primary care access without direct functional support and interaction supports Sampson’s theory of collective efficacy (Sampson, 2003). Individuals living in neighborhoods where people strongly agree neighbors are more willing to help each other are significantly more likely to have a RSOC and receive a check-up compared to individuals living in neighborhoods where people are less likely to agree that neighbors are willing to help each other. Thus, increased neighborhood collective efficacy may increase an individual’s primary care access. However, other measures of collective efficacy, such as ‘neighborhood is close-knit,’ border on having a negative association with both outcomes (p<0.10), which argues against this hypothesis.
Future research should determine if collective efficacy affects primary care, and if so, how. For example, it may increase an individual’s trust in healthcare institutions (Ahern & Hendryx, 2003), or it may increase individual self-esteem (Kawachi & Berkman, 2000), which may in turn affect the importance individuals place on their health. Individuals living in neighborhoods with strong social cohesion may have more positive attitudes toward their life chances, positively affecting their views on how important it is to take care of their health and adhere to positive health behaviors (Ellen et al., 2001; Siegrist, 2000), such as seeking out primary care. For example, Mitchell, Gleave, Bartley, Wiggins, and Joshi (2000) found that individuals who felt they were part of their community had significantly higher physical health outcomes when controlling for individual and neighborhood characteristics, such as deindustrialization. In this present study, a significant interaction between increased smoking disapproval and living in a neighborhood where neighbors are more willing to help each other was found to significantly increase the odds of having a RSOC. However, the estimate was unstable due to small cell sizes (data not shown). Future research should further investigate this hypothesis.
Going to a health provider for a check-up is a different process than just having a RSOC, and the neighborhood mechanisms differ between these two processes. For example, neighborhood healthcare resources were important predictors of actually using preventive care use but did not predict having a RSOC (Table 3). This finding supports past research that found low-income adults living in an MSA with more community health centers were significantly more likely to report visiting a physician in the past year even when controlling for individual factors, such as health insurance coverage (Brown et al., 2004). Research determining supply of healthcare resources on the neighborhood level in the United States or more detailed geographic analyses of healthcare resources would help to further elaborate this mechanism.
Since neighborhood independently affects primary care access, further research is essential to increase our understanding of how neighborhood environment influences primary care access. First, research should examine how other aspects of the neighborhood environment impact primary care access. For example, characteristics of neighborhoods that impede individuals from getting to the doctor may be important. Balfour and Kaplan (2002) found that elderly living in neighborhoods with poor access to public transportation were more likely to report a decline in physical functioning and hypothesize this may be due to the inability of the elderly in these neighborhoods to attain needed services. Phillips (1979) found the availability of bus routes affected where individuals with lower SES traveled to obtain general practitioner services. Finally, cross-level interactions between individual and neighborhood characteristics need to be investigated. For example, individuals who face the greatest barriers to the healthcare system (e.g. low-income) or who have the greatest need for health care (e.g. chronic condition) may benefit most from a neighborhood environment supportive of primary care. Small cell sizes in this study prevented an effective analysis of cross-level interactions.
Policy implications
The neighborhood environment affects an individual’s ability to access primary care. However, it does not displace the importance of policies that remove barriers impeding individuals from accessing the healthcare system. Having health insurance significantly predicts both outcomes, and having a RSOC is a strong individual predictor of actually receiving a check-up in the last 2 years even when controlling for neighborhood characteristics. Public policies that increase individuals’ access to the healthcare system, such as increasing insurance coverage or providing individuals with a RSOC, will significantly increase an individual’s access to quality and use of primary care (DeVoe et al., 2003).
However, since neighborhood independently affects primary care access, policies that focus on changing the neighborhood environment may also increase primary care access. For example, if neighborhood social capital influences individuals’ primary care access through collective efficacy and individual self-esteem, community empowerment programs that organize community members and build their collective efficacy may also increase individuals’ access to primary care. Policies that ensure the equitable distribution of healthcare resources across neighborhoods will also increase primary care access.
Acknowledgments
The Los Angeles Family and Neighborhood Survey was funded by NICHD, NIH/OBSSR, DHHS/OASPE, and NIA. Salary support for the author was provided by a Health Services Research Fellowship from the Department of Veteran Affairs. I am grateful to Anne Pebley, Rob Mare and two anonymous reviewers for their helpful comments on earlier drafts of this work.
References
- Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Social Science and Medicine. 2000;51:1143–1161. doi: 10.1016/s0277-9536(00)00016-2. [DOI] [PubMed] [Google Scholar]
- Ahern MM, Hendryx MS. Social capital and trust in providers. Social Science and Medicine. 2003;57:1195–1203. doi: 10.1016/s0277-9536(02)00494-x. [DOI] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda county study. American Journal of Epidemiology. 2002;155(6):507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- Bindman AB, Grumbach K, Osmond D, Vranizan K, Stewart AL. Primary care and receipt of preventive services. Journal of General Internal Medicine. 1996;11:269–276. doi: 10.1007/BF02598266. [DOI] [PubMed] [Google Scholar]
- Bloom B, Simpson G, Cohen RA, Parsons PE. Access to health care: Part 2: Working-age adults. Vital Health Stat. 1997;10(197):1–8. [PubMed] [Google Scholar]
- Blumenthal D, Mort E, Edwards J. The efficacy of primary care for vulnerable population groups. Health Services Research. 1995;30(1):253–273. [PMC free article] [PubMed] [Google Scholar]
- Brown ER, Davidson PL, Yu H, Wyn R, Andersen RM, Becerra L, et al. Effects of community factors on access to ambulatory care for lower-income adults in large urban communities. Inquiry. 2004 Spring;41:39–56. doi: 10.5034/inquiryjrnl_41.1.39. [DOI] [PubMed] [Google Scholar]
- Brown ER, Ojeda VD, Wyn R, Levan R. Racial and ethnic disparities in access to health insurance and health care. Los Angeles and Menlo Park, CA: UCLA Center for Health Policy Research and Henry J. Kaiser Family Foundation; 2000. [Google Scholar]
- Brown ER, Ponce N, Rice T. The state of health insurance in California: Recent trends, future prospects. Los Angeles: UCLA Center for Health Policy Research; 2001. [Google Scholar]
- Casanova C, Starfield B. Hospitalization of children and access to primary care: A cross-national comparison. International Journal of Health Services. 1995;25(2):283–294. doi: 10.2190/PCF7-ALX9-6CN3-7X9G. [DOI] [PubMed] [Google Scholar]
- Cunningham PJ, Ginsburg PB. What accounts for differences in uninsurance rates across communities? Inquiry. 2001;38(1):6–21. doi: 10.5034/inquiryjrnl_38.1.6. [DOI] [PubMed] [Google Scholar]
- Cunningham PJ, Kemper P. Ability to obtain medical care for the uninsured: How much does it vary across communities? Journal of the American Medical Association. 1998;280(10):921–927. doi: 10.1001/jama.280.10.921. [DOI] [PubMed] [Google Scholar]
- Curry SJ, Wagner EH, Cheadle A, Diehr P, Koepsell T, Psaty B, et al. Assessment of community-level influences on individuals’ attitudes about cigarette smoking, alcohol use, and consumption of dietary fat. American Journal of Preventive Medicine. 1993;9(2):78–84. [PubMed] [Google Scholar]
- DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: Insurance status and usual source of care. American Journal of Public Health. 2003;93(5):786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earp JA, Eng E, O’Malley MS, Alpeter M, Rauscher G, Mayne L, et al. Increasing use of mammography among older, rural African American women: Results from a community trial. American Journal of Public Health. 2002;92(4):646–654. doi: 10.2105/ajph.92.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellen IG, Mijanovich T, Dillman KN. Neighborhood effects on health: Exploring the links and assessing the evidence. Journal of Urban Affairs. 2001;23(3–4):391–408. [Google Scholar]
- Ettner S. The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Medical Care. 1999;37(6):547–555. doi: 10.1097/00005650-199906000-00004. [DOI] [PubMed] [Google Scholar]
- Fossett JW, Perloff JD, Kletke PR, Peterson JA. Medicaid and access to child health care in Chicago. Journal of Health Politics, Policy and Law. 1992;17(2):273–298. doi: 10.1215/03616878-17-2-273. [DOI] [PubMed] [Google Scholar]
- Gross PF. Urban health disorders, spatial analysis, and the economics of health facility location. International Journal of Health Services. 1972;2(1):63–83. doi: 10.2190/1238-4PKR-MU69-Q8DJ. [DOI] [PubMed] [Google Scholar]
- Grumbach K, Coffman JM, Young JQ, Vranizan K, Blick N. Physician supply and medical education in California: A comparison with national trends. Western Journal of Medicine. 1998;168:412–421. [PMC free article] [PubMed] [Google Scholar]
- Hendryx MS, Ahern MM, Lovrich NP, McCurdy AH. Access to health care and community social capital. Health Services Research. 2002;37(1):87–103. [PubMed] [Google Scholar]
- Jiang HJ, Begun JW. Dynamics of change in local physician supply: An ecological perspective. Social Science and Medicine. 2002;54:1525–1541. doi: 10.1016/s0277-9536(01)00132-0. [DOI] [PubMed] [Google Scholar]
- Joung IMA, Meer JBWVD, Mackenbach JP. Marital status and health care utilization. International Journal of Epidemiology. 1995;24(3):569–575. doi: 10.1093/ije/24.3.569. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Berkman L. Social cohesion, social capital and health. In: Berkman L, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. 174–190. [Google Scholar]
- Komaromy M, Lurie N, Bindman AB. California physicians’ willingness to help the poor. Western Journal Of Medicine. 1995;162:127–132. [PMC free article] [PubMed] [Google Scholar]
- Levy-Storms L, Wallace SP. Use of mammography screening among older Samoan women in Los Angeles County: A diffusion network approach. Social Science and Medicine. 2003;57:987–1000. doi: 10.1016/s0277-9536(02)00474-4. [DOI] [PubMed] [Google Scholar]
- Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970–1998. Health Services Research. 2003;38(3):831–865. doi: 10.1111/1475-6773.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place effects on health: How can we conceptualise, operationalise and measure them? Social Science and Medicine. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Mitchell R, Gleave S, Bartley M, Wiggins D, Joshi H. Do attitude and area influence health? A multilevel approach to health inequalities. Health and Place. 2000;6:67–79. doi: 10.1016/s1353-8292(00)00004-6. [DOI] [PubMed] [Google Scholar]
- National Guideline Clearing House. Agency for Healthcare Research and Quality, US Department of Health and Human Services; 2002. [accessed 8/1/2004]. www.guideline.gov. [Google Scholar]
- Phillips DR. Spatial variations in attendance at general practitioner services. Social Science and Medicine. 1979;13D:169–181. doi: 10.1016/0160-8002(79)90004-2. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology and Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A, Pickles A. Maximum likelihood estimation of limited and discrete dependent variable models with nested random effects. Journal of Econometrics. 2005 doi: 10.1016/j.jeconom.2004.08.017. in press. [DOI] [Google Scholar]
- Robert SA. Socioeconomic position and health: The independent contribution of community socioeconomic context. Annual Review of Sociology. 1999;25:489–516. [Google Scholar]
- Sampson RJ. The neighborhood context of well-being. Perspectives in Biology and Medicine. 2003;46(3):S53–S64. [PubMed] [Google Scholar]
- Sastry N, Ghosh-Dastidar B, Adams J, Pebley AR. The design of a multilevel longitudinal survey of children, families, and communities: The Los Angeles Family and neighborhood survey (Working Paper-DRU-2400/1-1-LAFANS) Santa Monica: RAND Corporation; 2003. [Google Scholar]
- Sastry N, Pebley AR. Non-response in the Los Angeles family and neighborhood survey. Santa Monica: RAND Corporation; 2003. (Working Paper-DRU-2400/7-LAFANS) [Google Scholar]
- Shi L. Primary care, specialty care, and life chances. International Journal of Health Services. 1994;24(3):431–458. doi: 10.2190/BDUU-J0JD-BVEX-N90B. [DOI] [PubMed] [Google Scholar]
- Shi L, Starfield B, Kennedy B, Kawachi I. Income inequality, primary care and health indicators. Journal of Family Practice. 1999;48(4):275–284. [PubMed] [Google Scholar]
- Shi L, Starfield B, Politzer R, Regan J. Primary care, self-rated health, and reductions in social disparities in health. Health Services Research. 2002;37(3):529–549. doi: 10.1111/1475-6773.t01-1-00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist J. Place, social exchange and health: Proposed sociological framework. Social Science and Medicine. 2000;51:1283–1293. doi: 10.1016/s0277-9536(00)00092-7. [DOI] [PubMed] [Google Scholar]
- Statacorp. Stata Statistical Software: Release 8.0. College Station, TX: Stata Corporation; 2003. [Google Scholar]
- Steinberg CR, Baxter RJ. Accountable communities: How norms and values affect health system change. Health Affairs. 1998;17(4):149–157. doi: 10.1377/hlthaff.17.4.149. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Kim DJ, Kawachi I. Social trust and self-rated health in US communities: A multilevel analysis. Journal of Urban Health. 2002;79(4):S21–S34. doi: 10.1093/jurban/79.suppl_1.S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss GL, Ramsey CA. Regular source of primary medical care and patient satisfaction. Quality Review Bulletin. 1989;15(6):180–184. doi: 10.1016/s0097-5990(16)30289-5. [DOI] [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM, Katz SJ, Welch HG. Is language a barrier to the use of preventive services? Journal of General Internal Medicine. 1997;12:472–477. doi: 10.1046/j.1525-1497.1997.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]