Abstract
Background
Although the number of elderly patients with fractures is increasing, there have been only a few studies to date of the efficacy of collaborative treatment by trauma surgeons and geriatricians.
Methods
Data on patients over age 75 with femoral neck, trochanteric, proximal humeral, and pelvic ring fractures were evaluated from the eras before and after the establishment of a certified center for geriatric traumatology (CGT) (retrospective analysis, n = 169; prospective analysis, n = 216). Moreover, data were also analyzed from younger patients (aged 65–74) with the same types of fracture who were not treated in the CGT. The main outcome parameter was in-hospital mortality. Other ones were the frequency and length of stays in the intensive care unit, the overall length of hospital stay, and the use of inpatient rehabilitation after acute hospitalization.
Results
Before the CGT was established, 20.7% of all patients over age 75 (95% confidence interval [CI], 14.8–27%) were treated in an intensive care unit; the corresponding figure after the establishment of the CGT was 13.4% (95% CI, 9.3–18.5%, p = 0.057). The mean length of stay in the intensive care unit before and after establishment of the CGT was 48 hours (95% CI, 32–64 hours) and 53 hours (95% CI, 29–77 hours), respectively (p = 0.973). The in-hospital mortality declined from 9.5% (95% CI, 5.3–13.8%) to 6.5% (95% CI, 3.7–9.5%, p = 0.278), while the overall length of hospital stay increased from 13.7 days (95% CI, 12.6–14.8 days) to 16.9 days (95% CI, 16.1–17.7 days, p<0.001). The percentage of patients transferred to an inpatient rehabilitation facility upon discharge decreased slightly, from 53.8% to 49.1%. Among the younger patients who were not treated in the CGT, no comparable trends were seen toward lower in-hospital mortality or toward less treatment in an intensive care unit. In fact, the developments over time in the younger age group tended to be in the opposite direction.
Conclusion
The collaborative treatment of elderly patients with fractures by trauma surgeons and geriatric physicians can markedly improve their acute care.
Numbers of inpatient treatments and surgeries in older patients are rising in Western industrialized countries, including for fractures (1– 5). The most common fractures for which patients receive inpatient treatment include proximal femoral, proximal humeral, and pelvic fractures (1). In 2012, 166 000 patients were treated for proximal femoral fractures in Germany alone (6), the majority caused by falls among the elderly (7). In recent years a number of care structures have been developed for these patients, taking account of increasing age, rising complication rates, and the associated increase in morbidity and mortality (8).
Pioli has divided collaboration between trauma surgery and geriatrics during fully inpatient acute care into four models (9):
Treatment by a trauma surgeon able to consult a geriatrician
As above, with the addition of weekday visits by a geriatrician
Treatment by a geriatrician able to consult a trauma surgeon
Joint treatment by a trauma surgeon and a geriatrician from admission to discharge, on an equal basis and by agreement
Various analyses indicate that there are advantages to a patient being treated simultaneously by both a trauma surgeon and a geriatrician (Pioli’s fourth model [9]) (8). A meta-analysis and a systematic review highlight a lack of data on the interdisciplinary treatment model in elderly patients with fractures: To date, absolutely no randomized controlled trials on this subject have been conducted in Germany (10).
This article therefore aims to present and compare outcomes before and after a center for geriatric traumatology (CGT) was established in an urban hospital providing routine care. The main target parameter was in-hospital mortality, which was established as a quality criterion in the certified CGT. The following were also investigated:
Length of hospital stay
Need for treatment in an intensive care unit (ICU)
Further care following treatment in the acute care hospital
Methods
Working method of the center for geriatric traumatology (CGT)
The research was conducted at the Diakonissenkrankenhaus Mannheim hospital, where the “geriatric concept of Baden–Württemberg” is realized with an acute-care geriatric ward and a geriatric rehabilitation facility. On April 1, 2012 an ISO 9000–certified center for geriatric traumatology was opened, following a year of preparation and the compilation of a handbook containing appropriate treatment guidelines. Patients with fractures were treated jointly by a trauma surgeon and a geriatrician/internist from admission onwards. The following remained unchanged compared to the time before April 1, 2012:
Diagnosis by a trauma surgeon
Aim to perform surgery within 24 hours of admission
Perioperative management by a trauma surgeon and an anesthesiologist
Daily visit by a trauma surgeon
Care on a trauma surgery ward, including previous care
Physiotherapy exercises.
With the CGT came admission of patients by an intern with geriatric training under the supervision of a geriatrician and the identification of individual risk factors for falls. In addition, joint identification and treatment of complications of both acute and chronic diseases by a trauma surgeon and a geriatrician/internist took place from admission. All comorbidities and indications for all drugs were documented in the CGT from a geriatric and internal medicine point of view. Medication was tailored to the acute situation. Daily visits by the intern geriatrician and weekly joint patient visits by a trauma surgeon and a geriatrician also aided in this. In addition there were weekly, patient-centered, interdisciplinary team discussions with the trauma surgeon; the geriatrician; nursing, physiotherapy, and occupational therapy staff; and the social worker/case manager. Occupational therapy (daily if necessary) can be offered as part of treatment in addition to physiotherapy if indicated, on the basis of basic geriatric assessment (activities of daily living, cognition, depression, mobility, social situation). All staff are offered regular training. A steering team meeting involving those in charge of treatment, nursing, and medicine is held in the CGT four times a year to deal with organizational issues. This means that direct collaboration between geriatrics and trauma surgery begins on the day on which an elderly patient with a fracture is admitted (Pioli’s fourth model) (9).
Retrospective comparison involved a group of patients treated immediately before the CGT was established, at the same facility (Pioli’s first model, see above) (9). More intensive collaboration was discussed during this period, and outcomes were documented. The trauma surgery team was the same as during the CGT phase. Because resources were limited, only patients aged 75 years and older with at least one new fracture to the following areas have so far been treated in the CGT:
Femoral neck fracture (ICD-10: S72.01 to 72.08)
Trochanteric fracture (ICD-10: S72.10 to 72.2)
Proximal humeral fracture (ICD-10: S42.20 to 42.29)
Pelvic ring fracture (ICD-10: S32.1 to 32.89).
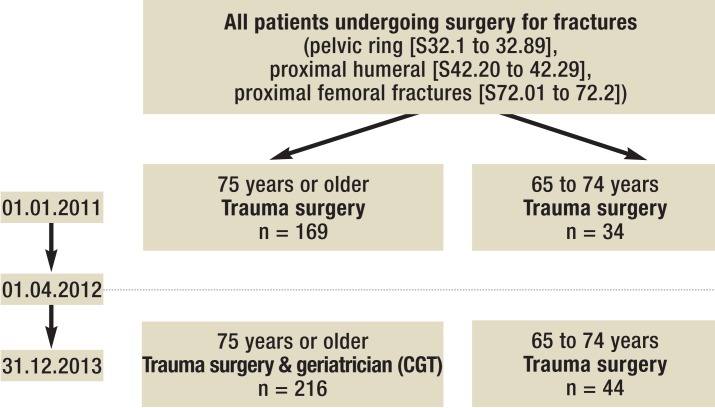
There were four groups for comparative evaluation (Figure). Patients over 75 were divided as follows:
Figure.
Groups by patient age and time. CGT: Center for geriatric traumatology
Before CGT established: January 1, 2011 to March 31, 2012 (before CGT)
After CGT established: April 1, 2012 to December 31, 2013 (CGT).
Patients aged between 65 and 74 years who received treatment according to Pioli’s first model (9) (see above) during the same period were also evaluated, in order to identify any changes in treatment other than the establishment of the CGT.
In-hospital mortality, length of hospital stay, and destination on release (home, nursing home, inpatient rehabilitation, or referral to another department/hospital) were established as quality criteria for certification as CGT. They were documented prospectively from April 1, 2012 onwards and retrospectively before this. The frequency and duration of ICU treatment were documented retrospectively in order to clarify any changes in the main target parameter, in-hospital mortality. The dataset according to Article 21 of the German Hospital Payments Act was used as the basis for retrospective data collection. After patients had been identified, data reliability was tested on the basis of physicians’ letters, patients’ records, and the internal hospital information system. Where necessary, data was then corrected and added to.
Statistics
The software program SPSS 21 was used for statistical analysis and presentation. The results were presented descriptively using means and frequencies. Confidence intervals (CIs) are shown in parentheses. A two-tailed chi-square test was used to compare all frequencies, and continuous variables were compared using the Wilcoxon–Mann–Whitney test where distribution was not normal.
Results
Comparison of the groups before (age over 75 years, n = 169; 65 to 74 years, n = 34) and after the CGT was established (age over 75 years, n = 216; 65 to 74 years, n = 44) shows no changes in patient age, sex distribution, or frequency of fractures (Table 1).
Table 1. Fractures. age (mean). sex distribution. length of hospital stay (days). and number of complex early geriatric rehabilitation treatments (GFK: 8–550.1 and 2. see text) before and after the establishment of a center for geriatric traumatology (CGT).
| Type of fracture | n | Age | Sex | Length of hospital stay (days) | GFK | |||
|---|---|---|---|---|---|---|---|---|
| Mean | 95% CI | F (n) | F (%) | Mean | 95% CI | n (%) | ||
| Before CGT (75 years and older) | ||||||||
| Total | 169 | 84.8*1 | 84.0 to 85.6 | 139*2 | 82.2 | 13.7*5 | 12.6 to 14.8 | 6 (3.6)*6 |
| Femoral neck | 49 | 85.0 | 83.4 to 86.7 | 40 | 81.6 | 12.9 | 10.9 to 14.9 | 1 (2.0) |
| Trochanter | 65 | 84.9 | 83.8 to 86.0 | 52 | 80.0 | 13.9 | 12.0 to 15.8 | 4 (6.1) |
| Humerus | 32 | 82.5 | 80.7 to 84.4 | 26 | 81.2 | 11.3 | 9.9 to 12.8 | 1 (3.1) |
| Pelvis | 23 | 87.0 | 84.5 to 89.6 | 21 | 91.3 | 18.0 | 14.1 to 21.9 | 0 |
| CGT (75 years and older) | ||||||||
| Total | 216 | 85.1*1 | 84.4 to 85.9 | 180*2 | 83.3 | 16.9*5 | 16.1 to 17.7 | 108 (50.0)*6 |
| Femoral neck | 69 | 85.4 | 83.9 to 87.0 | 56 | 81.2 | 16.8 | 15.4 to 18.2 | 34 (49.3) |
| Trochanter | 94 | 85.5 | 84.5 to 86.5 | 77 | 81.9 | 17.0 | 15.5 to 18.4 | 52 (55.3) |
| Humerus | 31 | 82.8 | 80.9 to 84.8 | 26 | 83.9 | 15.8 | 14.5 to 17.2 | 12 (38.7) |
| Pelvis | 22 | 85.8 | 83.7 to 88.0 | 21 | 95.5 | 18.2 | 16.6 to 19.9 | 10 (45.5) |
| Before CGT (65 to 74 years) | ||||||||
| Total | 34 | 70.2*3 | 69.1 to 71.3 | 26*4 | 76.5 | 12.4*7 | 10.8 to 14.1 | 0*8 |
| Femoral neck | 9 | 70.6 | 68.5 to 72.6 | 3 | 33.3 | 13.4 | 11.0 to 15.9 | 0 |
| Trochanter | 7 | 70.3 | 67.2 to 73.4 | 5 | 71.4 | 13.6 | 8.7 to 18.5 | 0 |
| Humerus | 13 | 69.0 | 67.0 to 71.1 | 13 | 100 | 10.3 | 7.0 to 13.6 | 0 |
| Pelvis | 5 | 72.4 | 70.7 to 74.1 | 5 | 100 | 14.6 | 10.9 to 18.3 | 0 |
| No CGT (65 to 74 years) | ||||||||
| Total | 44 | 70.8*3 | 70.0 to 71.7 | 31*4 | 70.5 | 14.5*7 | 12.7 to 16.3 | 4 (9.1)*8 |
| Femoral neck | 12 | 71.3 | 69.8 to 72.9 | 10 | 83.3 | 14.7 | 12.4 to 16.9 | 2 (16.7) |
| Trochanter | 13 | 71.4 | 70.1 to 72.8 | 6 | 46.2 | 14.5 | 9.8 to 19.3 | 1 (7.7) |
| Humerus | 15 | 69.4 | 67.7 to 71.1 | 11 | 73.3 | 13.1 | 10.2 to 16.0 | 1 (6.7) |
| Pelvis | 4 | 72.8 | 68.8 to 76.7 | 4 | 100 | 19.5 | 10.3 to 28.7 | 0 |
Before CGT: Trauma surgery between January 1. 2011 and March 31. 2012
No CGT: Trauma surgery between April 1. 2012 and December 31. 2013
CGT: Treatment by trauma surgeon and geriatrician between April 1. 2012 and December 31. 2013
p-value for age and sex: *1p = 0.531; *2p = 0.779; *3p = 0.319; *4p = 0.553
p-value for length of hospital stay and GFK: *5p <0.001; *6p <0.001; *7p = 0.09; *8p = 0.071
GFK. complex early geriatric rehabilitation treatment (geriatrische frührehabilitative Komplexbehandlung); CI. confidence interval
Length of hospital stay, complex treatment
Mean length of hospital stay increased by 3.2 days to 16.9 days (95% CI: 16.1 to 17.7 days) in the CGT group, significantly longer than in the control group (Table 1). There is also an increasing tendency in the 65 to 74 age group: a rise of 2.1 days to 14.5 days (95% CI: 12.7 to 16.3 days). There was a very substantial increase in the number of patients who met the criteria for complex early geriatric rehabilitation treatment according to the German hospital payment system (German diagnosis-related groups [G-DRGs)]: Classification of Operations and Procedures [OPS, Operationen- und Prozedurenschlüssel] codes 8–550.1 and 2). In those aged over 75 years the length of stay of patients with these codes (n = 108) was 19.3 days in the CGT group (95% CI: 18.3 to 20.3 days) versus 14.3 days (95% CI: 13.4 to 15.5 days) for those with no OPS code (n = 108). The six patients who received complex early geriatric rehabilitation treatment before the CGT was established received inpatient treatment for a mean of 26.8 days (95% CI: 16.2 to 37.4 days), versus 13.2 days (95% CI: 12.1 to 14.3 days).
ICU stays, in-hospital mortality
As shown in Table 2, after the CGT was established the percentage of patients requiring intensive care treatment fell from 20.7% (95% CI: 14.8 to 27%) to 13.4% (95% CI: 9.3 to 18.5%; p = 0.057). In contrast, this figure rose in patients aged 65 to 74 years: 11.8% (n = 4) versus 20.5% (n = 9); p = 0.307. Length of ICU stay remained unchanged in both older and younger patients after the CGT was established.
Table 2. No. of patients admitted to ICU. length of ICU stay. in-hospital mortality before and after the establishment of a center for geriatric traumatology (CGT).
| Before CGT (75 years and older) |
CGT (75 years and older) |
p | Before CGT (65 to 74 years) |
No GCT (65 to 74 years) |
p | |
|---|---|---|---|---|---|---|
| ICU admissions | ||||||
| n (%) | 35 (20.7) | 29 (13.4) | 0.057 | 4 (11.8) | 9 (20.5) | 0.307 |
| 95% confidence interval | 14.8 to 27 | 9.3 to 18.5 | * | * | ||
| Length of ICU stay (hours) | ||||||
| Mean | 48 | 53 | 0.973 | 65 | 75 | 0.94 |
| 95% confidence interval | 32 to 64 | 29 to 77 | –42 to 171 | –7 to 157 | ||
| In-hospital mortality | ||||||
| n (%) | 16 (9.5) | 14 (6.5) | 0.278 | 0 (0) | 3 (6.8) | 0.12 |
| 95% confidence interval | 5.3 to 13.8 | 3.7 to 9.5 | * | |||
Before CGT: Trauma surgery between January 1. 2011 and March 31. 2012
No CGT: Trauma surgery between April 1. 2012 and December 31. 2013
CGT: Treatment by trauma surgeon and geriatrician between April 1. 2012 and December 31. 2013
*Confidence interval not stated due to small number of cases
In-hospital mortality was lower among CGT patients than in patients of the same age before the CGT was established: 9.5% (95% CI: 5.3 to 13.8%) versus 6.5% (95% CI: 3.7 to 9.5%); p = 0.278. For the period from April 1 to December 31, 2012 (the beginning of the CGT implementation phase), in-hospital mortality was 8.0%, versus only 5.4% the following year. Post hoc analysis of proximal femoral fractures reveals a drop in in-hospital mortality in this subgroup from 12.2% to 6.7% (p = 0.057). In contrast, in-hospital mortality rose in patients aged 65 to 74 years (0% versus 6.8%).
Place of residence before and subsequent care after acute hospital treatment
Patients’ place of residence before admission is shown in Table 3. Use of inpatient rehabilitation following acute care fell slightly after the CGT was established (Table 3): 53.8% (95% CI: 46.3 to 61.6%) versus 49.1% (95% CI: 42.7 to 56%). Frequency of inpatient rehabilitation also decreased in patients aged 65 to 74 after April 1, 2012: 41.2% (95% CI: 24.2 to 57%) versus 34.1% (95% CI: 19.5 to 48.5%). Almost all patients with pelvic fractures required subsequent inpatient rehabilitation (increasing tendency compared to the time before the CGT was established); inpatient rehabilitation was required in the fewest cases in patients with humeral fractures (decreasing tendency compared to the time before the CGT was established). Somewhat more patients were discharged from the CGT to a nursing home than were resident in a nursing home before admission: 1.8% (n = 3) before the CGT versus 4.3% (n = 10) in the CGT group. This development was even more marked in patients aged 65 to 74: 2.8% (n = 1) versus 9.1% (n = 5). However, the proportion of patients already living in a nursing home before admission was significantly lower in this age group.
Table 3. Situation on admission and discharge before and after the establishment of a center for geriatric traumatology (CGT).
| Type of fracture | From home n (%) | From nursing home n (%) | From other department n (%) | To inpatient rehabilitation n (%) | To home n (%) | To nursing home n (%) | Referred to other department n (%) |
| Before CGT (75 years and older) | |||||||
| Total | 130 (76.9) | 35 (20.7) | 4 (2.3) | 91 (53.8) | 21 (12.4) | 38 (22.5) | 3 (1.8) |
| Femoral neck | 39 (79.6) | 10 (20.4) | 0 | 25 (51.0) | 6 (12.2) | 14 (28.6) | 0 |
| Trochanter | 49 (75.4) | 16 (24.6) | 0 | 34 (52.3) | 5 (7.7) | 15 (23.1) | 1 (1.6) |
| Humerus | 28 (87.5) | 4 (12.5) | 0 | 15 (46.9) | 9 (28.1) | 6 (18.8) | 2 (6.3) |
| Pelvis | 14 (60.9) | 5 (21.7) | 4 (17.4) | 17 (73.9) | 1 (4.3) | 3 (13.0) | 0 |
| GTC (75 years and older) | |||||||
| Total | 165 (76.4) | 51 (23.6) | 0 | 106 (49.1) | 32 (14.8) | 61 (28.2) | 3 (1.4) |
| Femoral neck | 48 (69.6) | 21 (30.4) | 0 | 34 (49.3) | 6 (8.7) | 22 (31.9) | 1 (1.4) |
| Trochanter | 72 (76.6) | 22 (23.4) | 0 | 43 (45.7) | 16 (17.0) | 28 (29.8) | 2 (2.1) |
| Humerus | 27 (87.1) | 4 (12.9) | 0 | 11 (35.5) | 8 (25.8) | 10 (32.3) | 0 |
| Pelvis | 18 (81.8) | 4 (18.2) | 0 | 18 (81.8) | 2 (9.1) | 1 (4.5) | 0 |
| Before CGT (65 to 74 years) | |||||||
| Total | 29 (85.3) | 2 (5.9) | 3 (8.8) | 14 (41.2) | 17 (50.0) | 3 (8.8) | 0 |
| No CGT (65 to 74 years) | |||||||
| Total | 42 (95.5) | 2 (4.5) | 0 | 15 (34.1) | 19 (43.2) | 7 (15.9) | 3 (6.8) |
Before CGT: Trauma surgery between January 1. 2011 and March 31. 2012
No CGT: Trauma surgery between April 1. 2012 and December 31. 2013
CGT: Treatment by trauma surgeon and geriatrician between April 1. 2012 and December 31. 2013
Discussion
After the CGT was established fewer patients were treated in the ICU. They were less likely to die in the hospital although their ages were broadly the same and their inpatient treatment lasted longer. In our view, the continuous reduction in in-hospital mortality and length of ICU stay was the consequence of complex intervention as a result of establishing the CGT as described, but no conclusions can be drawn concerning the efficacy of individual components. On the basis of day-to-day practice, we consider the following essential, in addition to unchanged management of rapid traumatology diagnosis and the aim of swift surgery following admission:
Joint management of complications (particularly delirium) and comorbidities
Adaptation of long-term pharmacological therapy to acute situation
The wider range of available treatment (particularly occupational therapy), which is based on geriatric assessment and agreed upon daily by the whole treatment team.
As shown here, the longer treatment duration is due in particular to the availability of more intensive complex occupational therapy and physiotherapy (as part of OPS procedure 8–550) in addition to the likelihood of more intensive diagnostics, including explanation of falls and treatment for comorbidities (11). The results shown here confirm the suspicion of Buecking et al. (10) that the differences in length of hospital stay (7.4 to 26.7 days) (8) are the result of differences between the health systems of different states and individual features of local structures rather than a quality criterion in the treatment of geriatric traumatology patients. In addition, in Germany there are considerable differences between healthcare systems even within individual states; this is particularly true of the implementation of geriatric care structures (12).
To date, frequency and duration of intensive care treatment has not been shown to reflect the efficacy of trauma surgery/geriatric treatment. Quite the reverse: intensive care “monitoring” of all geriatric traumatology patients is occasionally called for. Whether this is beneficial is controversial (13). ICU treatment was indicated on an individual basis in the CGT described here. This was also the case during the control periods. In most cases, patients’ destination on leaving the anesthetic recovery room was decided by the surgeon and the anesthesiologist. When the patient was returned to a normal ward, this was decided by the treating trauma surgeon and, after the CGT was established, jointly with the geriatrician, provided this was possible at that time (no geriatrician available or on-call service at night and during weekends). The decrease in intensive care stays is therefore probably due to prevention of complications and acute diseases that make ICU treatment unavoidable, rather than the influence of a geriatrician in the direct decision-making process (intensive care: yes or no). Because ICU stays are not a CGT quality criterion, the decision for or against ICU treatment was not affected by the CGT. According to our results, avoiding ICU stays is achieved substantially better using a CGT according to Pioli’s fourth model than according to his first model (9). These results support the hypothesis that inpatient treatment in an ICU in particular initially entails risks for the elderly which are independent of their illnesses. Avoiding ICU stays may also have made an additional contribution to reducing mortality. Especially important here are avoidable risk factors for delirium. If patients present delirium, this leads to an increase in in-hospital mortality (14). Specific risks for delirium in an ICU are as follows:
Excessive immobility
Sleep disorder and restlessness (resulting from light, noise, emergencies)
Disorientation caused by additional change of location within the hospital
Reduced contact with familiar individuals
Increased risk of infection by problematic microbes
More frequent catheter use and associated complications.
Most randomized controlled trials conducted to date on interdisciplinary geriatric traumatology treatment have concerned proximal femoral fractures and been conducted outside Germany. We therefore analyzed in-hospital mortality of patients with proximal femoral fractures separately. Here the trend towards falling in-hospital mortality was even clearer. Such a trend can also be seen in prospective nonrandomized (15– 17) and randomized trials (18– 21) in which some patients were younger and differing inclusion and exclusion criteria were used. A meta-analysis on joint geriatric treatment of a total of 970 patients also found a reduction in in-hospital mortality, but the decrease was not statistically significant (10). The Quality Report for Germany for 2012, however, indicates in-hospital mortality of 5.2% for proximal femoral fractures only, regardless of age, in patients with a severe and incapacitating systemic disease (class III of the American Society of Anesthesiologists) (7). For fractures treated with hip prosthesis from 2003, in-hospital mortality was 8.5% for those aged 80 to 89 years and 13.6% for those aged over 89. This is higher than shown here (22).
There is little change in destination on discharge. There was almost no change in patients’ rehabilitation needs after acute care. This research cannot clarify whether these patients began rehabilitation with better functional status than previously. However, apprehensions that joint geriatric treatment increases referrals to a rehabilitation facility cannot be confirmed. Neither did these results provide substantial evidence of the reverse (particularly as a result of beginning complex treatment and rehabilitation early).
A particular limitation of the research presented here, which is descriptive and nonrandomized, is the historical nature of its controls. We attempted to minimize this limitation by selecting a control period that immediately preceded establishment of the CGT and performing comparison only with patients who underwent surgery. Fracture distribution, sex distribution, and mean age were comparable. Other limitations are the heterogeneous nature of the fracture groups and the subgroups, some of which were small. In addition, comorbidities, complications, and their severity were not documented because the research design was mainly retrospective.
Patients aged 65 to 74 years are also shown here, in order to identify changes in hospital treatment in general, traumatology surgery in particular, and contamination effects. In this group, which was significantly smaller, some trends went against those in the total group (more frequent ICU stays and increasing in-hospital mortality). However, even in this younger group a geriatrician performed joint treatment or took on a patient more frequently (less than 10% of cases) after the CGT was established. This usually took place only in the course of inpatient treatment. Length of hospital stay also rose slightly among younger patients. On the strength of these results the minimum age of 75 years, which was established on the basis of staff and bed capacity, no longer seems sound. Instead, the general definition (23), according to which a geriatric patient is 70 years old or more with multimorbidity typical for geriatric patients or 80 years old or more on the basis of increased vulnerability, should be used. As it can be assumed that a patient who has fallen and suffered a fracture often presents multimorbidity typical for geriatric patients, a minimum age of 70 years for admission to a CGT appears sensible.
Key Messages.
In-hospital mortality fell after a center for geriatric traumatology was established. Length of hospital stay increased overall.
ICU stays seem to decrease after a center for geriatric traumatology is established.
There is no significant reduction in subsequent rehabilitation after a center for geriatric traumatology is established.
The minimum age of 75 years for admission to joint geriatric care for age-related fractures seems too high. It should be reduced to 70 years or below.
Further randomized controlled trials would seem to be beneficial in order to increase the level of evidence on the subject “configuration of a center for geriatric traumatology.”
Acknowledgments
Translated from the original German by Caroline Devitt, M.A.
We would like to thank the nursing staff, therapists, and doctors of the Departments for Geriatrics and Trauma Surgery for their considerable help in the practical development of the Center for Geriatric Traumatology. We would also like to thank Controlling and Karin Müller from case management for their support in data collation. Prof. Dr. Kieser from the Department for Biometrics of the Heidelberg University deserves special thanks for his advice during statistical evaluation.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Gesundheitsberichterstattung des Bundes. Diagnosedaten der Krankenhäuser ab 2000. www.gbe-bund.de/ (last accessed on 25 September 2014) [Google Scholar]
- 2.Marks R. Hip fracture epidemiological trends, outcomes, and risk factors, 1970-2009. Int J Gen Med. 2010;3:1–17. [PMC free article] [PubMed] [Google Scholar]
- 3.Gosch M, Kammerlander C, Roth T, et al. Tiroler Zentrum für Altersfrakturen. Traumatologisch-geriatrisches Komanagement: Erste Erfahrungen und Ergebnisse. Journal für Mineralstoffwechsel. 2011;18:7–12. [Google Scholar]
- 4.Eurostat - Europäische Kommision. In Krankenhäusern durchgeführte chirurgische Eingriffe und Verfahren nach ICD-9-CM (hlth_co_proc2) http://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do. (last accessed on 20 September 2014)
- 5.Eurostat - Europäische Kommision. Krankenhausentlassungen nach Diagnose, stationäre Patienten, Gesamtzahl (hlth_co_disch1) http://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do. 2014. (last accessed on 20 September 2014)
- 6.Statistisches Bundesamt Deutschland Gesundheit. www-genesis.destatis.de. Wiesbaden: Diagnose der Krankenhauspatienten 2012. (last accessed on 25 May 2014) [Google Scholar]
- 7.AQUA - Institut für angewandte Qualitätsförderung und Forschung im Gesundheitswesen. Qualitätsreport 2012, Hüftgelenknahe Femurfrakturen. www.sqg.de/sqg/upload/CONTENT/Qualitaetsberichte/2012/AQUA-Qualitaetsreport-2012.pdf. (last accessed on 18 May 2014)
- 8.Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service—a literature review comparing different models. Osteoporos Int. 2010;21:637–646. doi: 10.1007/s00198-010-1396-x. [DOI] [PubMed] [Google Scholar]
- 9.Pioli G, Giusti A, Barone A. Orthogeriatric care for the elderly with hip fractures: where are we? Aging Clin Exp Res. 2008;20:113–122. doi: 10.1007/BF03324757. [DOI] [PubMed] [Google Scholar]
- 10.Buecking B, Timmesfeld N, Riem S, et al. Early orthogeriatric treatment of trauma in the elderly—a systematic review and metaanalysis. Dtsch Arztebl Int. 2013;110:255–262. doi: 10.3238/arztebl.2013.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kolb G, Breuninger K, Gronemeyer S, et al. 10 Jahre geriatrische frührehabilitative Komplexbehandlung im DRG-System. Z Gerontol Geriat. 2014;47:6–12. doi: 10.1007/s00391-013-0592-7. [DOI] [PubMed] [Google Scholar]
- 12.Bundesverband Geriatrie e. V. (eds.) Stuttgart: Kohlhammer; 2010. Weißbuch Geriatrie: Die Versorgung geriatrischer Patienten: Struktur und Bedarf - Status Quo und Weiterentwicklung. Eine Analyse durch die GEBERA Gesellschaft für betriebswirtschaftliche Beratung mbH. [Google Scholar]
- 13.Draganescu M, Hopf HB. Senkt eine routinemäßige postoperative intensivmedizinische Überwachung die Krankenhaussterblichkeit geriatrischer Patienten mit Schenkelhalsfraktur? Intensivmedizin und Notfallmedizin. 2008;45:89–97. [Google Scholar]
- 14.Lorenzl S, Füsgen I, Noachtar S. Acute confusional states in the elderly-diagnosis and treatment. Dtsch Arztebl Int. 2012;109:391–400. doi: 10.3238/arztebl.2012.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antonelli Incalzi R, Gemma A, Caparella O, et al. Continuous geriatric care in orthopedic wards: a valuable alternative to orthogeriatric units. Aging (Milano) 1993;5:207–216. doi: 10.1007/BF03324157. [DOI] [PubMed] [Google Scholar]
- 16.Fisher AA, Davis MW, Rubenach SE, et al. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20:172–178. doi: 10.1097/01.bot.0000202220.88855.16. [DOI] [PubMed] [Google Scholar]
- 17.Friedmann S, Mendelson D, Kates S, et al. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56:1349–1356. doi: 10.1111/j.1532-5415.2008.01770.x. [DOI] [PubMed] [Google Scholar]
- 18.Gilchrist WJ, Newman RJ, Hamblen DL, et al. Prospective randomised study of an orthopaedic geriatric inpatient service. BMJ. 1988;279:1116–1118. doi: 10.1136/bmj.297.6656.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naglie G, Tansey C, Kirkland JL, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ. 2002;167:25–32. [PMC free article] [PubMed] [Google Scholar]
- 20.Vidán M, Serra JA, Moreno C, et al. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53:1476–1482. doi: 10.1111/j.1532-5415.2005.53466.x. [DOI] [PubMed] [Google Scholar]
- 21.Stenvall M, Olofsson B, Nyberg L, et al. Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med. 2007;39:232–238. doi: 10.2340/16501977-0045. [DOI] [PubMed] [Google Scholar]
- 22.Wissenschaftliches Institut der AOK (WIdO) Bonn: WIdO; 2007. Qualitätssicherung der stationären Versorgung mit Routinedaten (QSR) [Google Scholar]
- 23.DGG - Deutsche Gesellschaft für Geriatrie. Was ist Geriatrie? www.dggeriatrie.de/nachwuchs/91-was-ist-geriatrie.html. (last accessed on 25 May 2014)