Abstract
In Bangladesh, the health risks of unplanned urbanization are disproportionately shouldered by the urban poor. At the same time, affordable formal primary care services are scarce, and what exists is almost exclusively provided by non-government organizations (NGOs) working on a project basis. So where do the poor go for health care? A health facility mapping of six urban slum settlements in Dhaka was undertaken to explore the configuration of healthcare services proximate to where the poor reside. Three methods were employed: (1) Social mapping and listing of all Health Service Delivery Points (HSDPs); (2) Creation of a geospatial map including Global Positioning System (GPS) co-ordinates of all HSPDs in the six study areas and (3) Implementation of a facility survey of all HSDPs within six study areas. Descriptive statistics are used to examine the number, type and concentration of service provider types, as well as indicators of their accessibility in terms of location and hours of service. A total of 1041 HSDPs were mapped, of which 80% are privately operated and the rest by NGOs and the public sector. Phamacies and non-formal or traditional doctors make up 75% of the private sector while consultation chambers account for 20%. Most NGO and Urban Primary Health Care Project (UPHCP) static clinics are open 5–6 days/week, but close by 4–5 pm in the afternoon. Evening services are almost exclusively offered by private HSDPs; however, only 37% of private sector health staff possess some kind of formal medical qualification. This spatial analysis of health service supply in poor urban settlements emphasizes the importance of taking the informal private sector into account in efforts to increase effective coverage of quality services. Features of informal private sector service provision that have facilitated market penetration may be relevant in designing formal services that better meet the needs of the urban poor.
Keywords: Health service providers, private providers, urban slum, urban health
KEY MESSAGES.
Unlike rural areas, organized systems of primary care provision are lacking in urban Bangladesh, and apart from limited services through non-government organization, is altogether absent in urban slums.
Informal private-for-profit providers have strategically filled this gap and cannot be ignored in efforts to increase effective coverage of services particularly for the urban poor.
Formal service delivery efforts can learn from the successful strategies employed by this sector, and at the same time, harm can be minimized through intelligently crafted incentives that encourage the application of quality standards.
Introduction
Following Bangladesh’s independence in 1971, a national health infrastructure was put in place to serve the health needs of a predominantly rural population. This system includes secondary and tertiary hospitals in all divisional cities, district and sub-district health facilities, as well as primary care provided through community clinics at the union level [Ministry of Health and Family Welfare (MoHFW) 2012]. With the exception of secondary and tertiary public hospitals, this infrastructure does not extend to urban areas, where the provision of primary healthcare services falls under the remit of local government (Ahmad 2007; Local Government Division 2010). With the exception of a handful of urban dispensaries in several large cities, and outpatient services in the public hospitals, the majority of public primary care services are contracted out by local Government to non-government organizations (NGOs) on a project basis, or provided by NGOs directly.
Like countries worldwide, Bangladesh is rapidly urbanizing with projections that more than half of its citizens will live in cities by 2050 (Streatfield and Karar 2008; Department of Economic and Social Affairs Population Division 2012). Pull and push factors ranging from economic opportunity to climate change have resulted in an influx of rural migrants into metropolitan areas throughout the country contributing to a growth rate of almost 3% per year (Department of Economic and Social Affairs Population Division 2012). In Dhaka City Corporation, the country’s capital, at least 1500 new migrants arrive daily making it one of the fastest growing megacities in the world (European Commission Humanitarian Aid Office 2010). Most of these incoming migrants settle in slums, contributing to an alarming growth rate of almost 7% per year (Streatfield and Karar 2008). Nationwide, over 35% of the urban population reside in poor slum settlements that lack even the most basic amenities of safe water and sanitation (Streatfield and Karar 2008). This situation of poverty, overcrowding and lack of services is reflected in health indicators, with child mortality rate reaching 95 per 1000 live births among slum residents, compared to 53 and 66 per 1000 live births in urban non-poor and rural populations, respectively (National Institute of Population Research and Training (NIPORT) 2008; Ahmed et al. 2009; Bangladesh Bureau of Statistics Planning Division and Ministry of Planning Government of the People's Republic of Bangladesh 2010). Similar patterns of urban inequities in health are found in cities across Africa, Asia and Latin America (UN-Habitat 2008; Agarwal 2011; Szwarcwald et al. 2002), and unless addressed threaten sustained urban development, prosperity, and well-being (World Health Organization and UN-Habitat 2010).
In Bangladesh, these disparities are further exacerbated by lack of equitable access to quality healthcare services despite the density and array of service options in urban centres. Growing evidence on health service utilization documents the reliance of the urban poor on private sector services of dubious quality. In a scoping study of health care seeking in urban slums, the authors documented slum dwellers’ preference for certain kinds of providers: drug sellers for general health problems as they provide low cost treatments for a range of illnesses; homeopaths and traditional healers for conditions like hepatitis, Reproductive Track Infections (RTIs) and Sexually Transmitted Diseases (STDs) that are believed to have no allopathic cure; and low-cost home deliveries by traditional birth attendants despite awareness of quality maternity services provided by Marie Stopes, Manoshi or Smiling Sun (Rasheed and Adams 2012). Another situational analysis on slums in Dhaka city estimated that two in every five cases of people experiencing illness sought treatment from pharmacies (Save the Children 2014).
Less is known about the supply side, and the extent to which quality services are distributed across the urban landscape, and in close proximity to the urban poor. This article reports on findings from a census of formal and informal healthcare provisioning in the slums of Dhaka, with the purpose of understanding the configuration of health services from a supply-side perspective, and recommending appropriate actions to increase effective coverage of quality primary care.
Methods
The unpublished data for this article are furnished by a health facility census conducted by International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) in six slum areas of Dhaka City Corporation in 2012. The census served to pilot test the feasibility of creating a Master Facility List (MFL) (World Health Organization 2012) for urban Bangladesh. As per Ministry of Local Government and Rural Development and Co-operatives (MoLGRDC) estimate, a total of 3.5 million people are living in 4000 slums in the Dhaka metropolitan area (up to February 2013). These poor urban settlements typically exhibit one or more defining characteristics including poor structural quality and durability of housing, insufficient living area, a lack of secure tenure, poor access to water, and lack of sanitation facilities (UN Habitat 2006).
With a few exceptions such as Karail and Kamrangir Char, slums in Dhaka generally exist as segmented patches or clusters rather than contiguous areas. These clusters frequently exceed 200 000 inhabitants per square kilometre (Streatfield and Karar 2008).
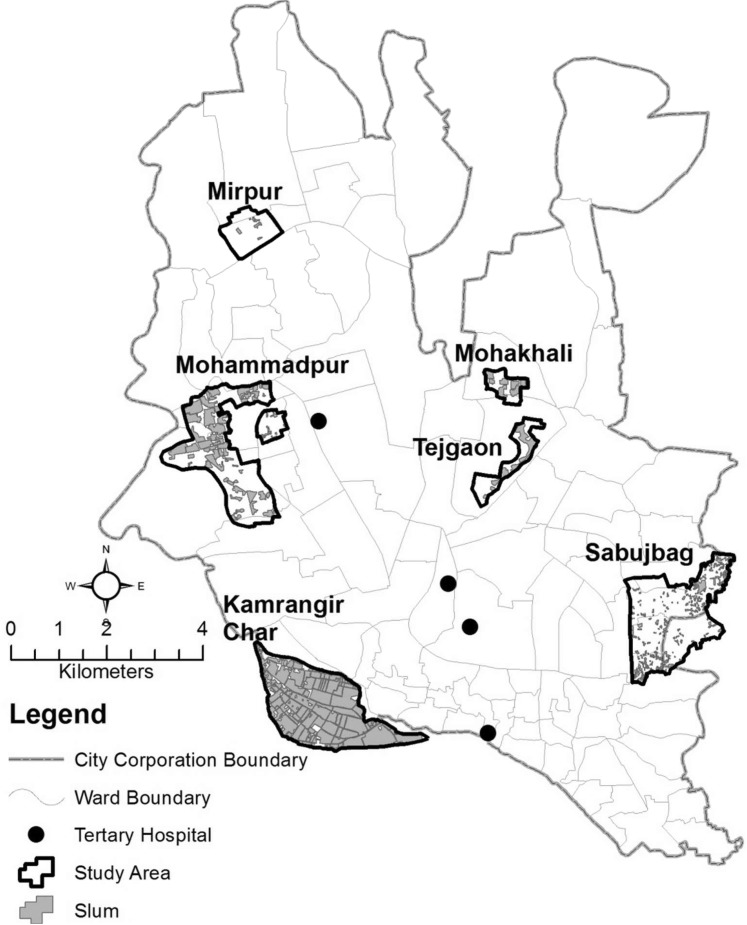
For the purposes of this study, the sampling frame was limited to areas of the city where the largest clusters of slums are located (at least 100 households in each). These clusters are identified with the help of a large NGO involved in the delivery of slum-based Maternal, Neonatal, and Child Health (MNCH) services in city corporations across the country.1 From this sampling frame, a convenience sample of seven slum clusters (study areas) was drawn based on qualitative assessments of relative stability and size: Karail, Sattola, Begunbari, Mirpur, Mohammadpur, Sabujbag and Kamrangir Char. Later Karail was removed from the survey due to a sudden eviction drive by Government in one area of the slum. Each study area included both slum and non-slum areas within a defined boundary (Figure 1).
Figure 1.
Location of the six study areas in Dhaka
Certain features were common across slums in the sample. Most notable was tenure insecurity and overcrowding, manifested in a lack of adequate housing, drainage and water and sanitation systems, and related vulnerability to waterlogging and disease outbreak. Most housing in the six study areas was one-storied and constructed of tin sheets, with the exception of Sattola and Sabujbag slums where some two-storied structures were found. Families generally consisted of two to three generations living together in a one or two roomed dwelling with kitchen and toilet facilities shared between 6 and 10 households. Within slums, small alleyways prevent vehicular movement other than rickshaws or bicycles. In Mohammadpur, Begunbari and Kamrangir Char slum areas were defined by water bodies and major road networks which further constrained entry and exit, and impeded access to emergency care. A description of the particular characteristics of slum areas included in the sample is provided in Table 1.
Table 1.
Characteristics of slums in each study area
| Slum name | Type | Access roads to and within slum | Subject to waterlogging |
|---|---|---|---|
| Sattola | Residential | Moderate. Alleys open on to one major road | Yes |
| Begunbari | Industrial | Insufficient. Several narrow roads | Yes |
| Mirpur | Residential | Good road network | Yes |
| Mohammadpur | Residential, low lying | Moderate. Few narrow roads, a major road in the North | Yes |
| Sabujbag | Residential, peri urban | Moderately connected roads | Yes |
| Kamrangir Char | Char, low lying | Moderate. 2–3 major wide roads | Yes |
In each study area, a census of all health service delivery points (HSDPs) was conducted—those within slums, and those in neighbouring non-slum areas that were close enough to permit access by slum dwellers.
Three methods were used to assemble the data set used in analysis:
Social mapping and listing of all HSDPs: a small team of trained researchers consulted with local residents to establish a plausible study boundary around the slum clusters in each area. Within this boundary or study area, they walked every alley and lane in the area and drew them on paper (social map). In parallel, they indicated HSDPs in relation to landmarks like mosques, schools or shops. Later the team returned and compiled a complete census listing of HSDPs indicating the name (as per signboards), address and contact number for each.
Creation of a geospatial map including Global Positioning System (GPS) co-ordinates of all HSPDs in and around the six slum areas: The consolidated list of HSDPs prepared during social mapping was handed to a team of Geographic Information Systems (GIS) specialists2 who visited each facility and collected their GPS co-ordinates using standard GPS machines to an accuracy of 5 m. Additionally, for purposes of comparison, geographical co-ordinates of all tertiary hospitals in Dhaka and Urban Primary Health Care Project (UPHCP) and NGOs facilities within one km from the outer boundary of the six study areas were collected. This team also created digitized maps that indicated the position of HSDPs relative to landmarks and Google Earth images.
Implementation of a survey of all health providers and services in six slum areas: A semi-structured tool was developed to collect information on each HSDP in terms of its management entity, type of facility, staffing details, hours of operation and range of services offered and their prices. Designed after the World Health Organization (WHO) MFL (World Health Organization 2012), the tool included staple facility identifiers as signature domains while service domains comprised basic service capacity information. This barebones approach differs from detailed service delivery surveys such as Service Availability and Readiness Assessment (SARA), Service Availability Mapping (SAM) and Service Provision Assessment (SPA), but provides a useful sampling frame for these methods.
The same team of researchers, who inventoried HSDPs, administered the survey. Two days of training on elements of the questionnaire was received as well as instructions about survey administration. This was followed by a two day pretest to refine survey strategies. The survey was administered to HSDP owners or managers in the context of facilities or pharmacies, and with doctors in the case of private chambers given their comprehensive knowledge of service details. Information collected was based on self-report by respondents, but due to resource constraints, verification by observation did not occur. Whenever service and price lists were available in the form of brochures or on signage, this information was used to cross-check information reported by respondents. If a knowledgeable person was not available, the team returned at another time to conduct the survey. This problem was encountered frequently among private providers due to the erratic timing of service provision. Multiple and night time visits were often necessary to contact an appropriate informant. In the case of smaller HSDPs, the field team was able to complete the survey in one visit; however, in larger tertiary care settings, multiple follow-up visits were necessary to gather all required information given the size of staff and the range of available services.
For the purposes of analysis, health services are categorized by management entity: public, private and not-for-profit (NGOs). Operational definitions are provided in Box 1 and supplemented by contextual information provided below:
Operational definitions of health service delivery points (HSDPs).
| HSDP type | Definitions |
|---|---|
| Hospital | Any formal institution providing both outdoor and indoor services with more than 30 beds |
| Clinic | Any formal institution with or without indoor services having <30 beds. Can be static (services continually provided in one location) or satellite (services provided on certain days and hours of the week). Clinic services are usually administered by some sort of management entity (like an NGO or a private group) and served by multiple staff |
| Diagnostic Centre | Facilities that provide medical testing and imaging facilities. Some also provide outpatient services |
| Delivery Centre (DC) | Informal MNCH facilities run by BRAC where poor women can receive Antenatal Care (ANC) and Postnatal Care (PNC) services and have normal deliveries assisted by trained birth attendants or midwives |
| Doctor’s/ consultation chamber | Independent doctor-run HSDPs that operate out of a small establishment or ‘chamber’, sometimes with the help of an assistant. Minimum qualifications of doctors include: MBBS or above; Diploma or Bachelors in Unani medicine; Diploma or Bachelors in Homeopathic medicine |
| Dental chamber/clinic | HSDPs that provide dental care and treatments solely |
| Traditional doctor’s Chamber | Kabiraj, Hakim or faith healers who are often referred to as ‘Doctors’ but lack recognized medical qualification by the Bangladesh Medical and Dental Council |
| Pharmacy/ drug shop | Establishments that sell drugs with or without a doctor’s prescription to the general public. Some may have a doctors’ chamber attached |
| Others | Rehabilitation centres (for substance abusers), physiotherapy centres and optic shops |
Public services
The public sector category of providers refers to services that are the responsibility of the Ministry of Local Government, Rural Development and Co-operatives (MoLGRC) and MoHFW. Under the Municipal Administration Ordinance of 1960, the Pourashova Ordinance of 1977, the City Corporation Ordinance of 1983 and the Local Government Act of 2009 the provision of preventive health and curative care is the responsibility of city corporations and municipalities. With the exception of outdoor patient services including Expanded Programme on Immunization (EPI), and 35 urban dispensaries, the role of MoHFW in urban areas is limited to the provision of secondary and tertiary care, and the stewardship functions of setting technical standards, regulation and strategy and policy development. Given lack of capacity within local government, urban primary care service provision has been contracted out to NGOs under the donor funded UPHCP3 since 1998.
Private sector services
The private sector category consists of providers operating on a for-profit basis, providing either formal (qualified) or informal services. These services tend to focus on remedial care, including drug supply, tertiary care and diagnostic testing.
NGO services
The NGO category is comprised of not-for-profit actors involved in primary care and maternity services, with a focus on service provision for the urban poor and other disadvantaged groups. These include Marie Stopes, Smiling Sun Clinics (now US Agency for International Development's (USAID) NGO Health Services Delivery Project) and BRAC’s (formerly known as Bangladesh Rural Advancement Committee) MNCH Manoshi Project. Health services are further categorized by delivery modality, i.e. whether provided in static facilities designated for healthcare provision, or in satellite, or non-purpose built locations where basic services are provided on certain days or hours of the week.
Data analysis relies on simple univariate statistics and crosstabs to examine the number, type and concentration of HSDPs, as well as indicators of their accessibility in terms of location and hours of service. All analysis considers HSDPs with in the study areas as demarcated by social mapping (see Figures 1, 3 and 5) unless otherwise specified. Classification of HSDPs in terms of formal and informal categories proved somewhat challenging due to lack of guidance in the published literature. A systematic review on informal providers (Sudhinaraset et al. 2013) provided three criteria in this regard; however, they were found to be unsuitable to healthcare providers in urban settings. One criterion specified that informal providers be entrepreneurs and not collect payment from formal institutions, while another stated that informal providers operate beyond any institutional oversight. These do not hold true in the context of Bangladesh where the Government and NGOs employ many Community Heath Workers (CHW), and maintain their paycheck and supervision. As Omaswa et al. (2006) notes in his discussion of the role of informal healthcare workers, even formal providers are known to work outside the regulations of health system and to provide services beyond their skill set. Given the lack of time or data to make such judgments, a simpler typology was employed for the purposes of this study. Healthcare providers (including drug sellers, shop owners and clinic support staff involved in service provision) who reported possessing academic/professional training and certifications for medical (allopathic, homeopathic and unani/herbal), nursing, midwifery, dentistry and allied health practice, were considered formal, while the rest were classified as informal. Categorizing HSDP facilities in a similar fashion, however, was not possible. While any HSDP with permission and registration from Directorate General of Health Services (DGHS) can be categorized as formal, including hospitals and clinics, the same criteria are not readily available for pharmacies/drug shops and doctors’ chambers. For this reason, analysis was confined to assessing the distribution and concentration of formal and informal health staff only.
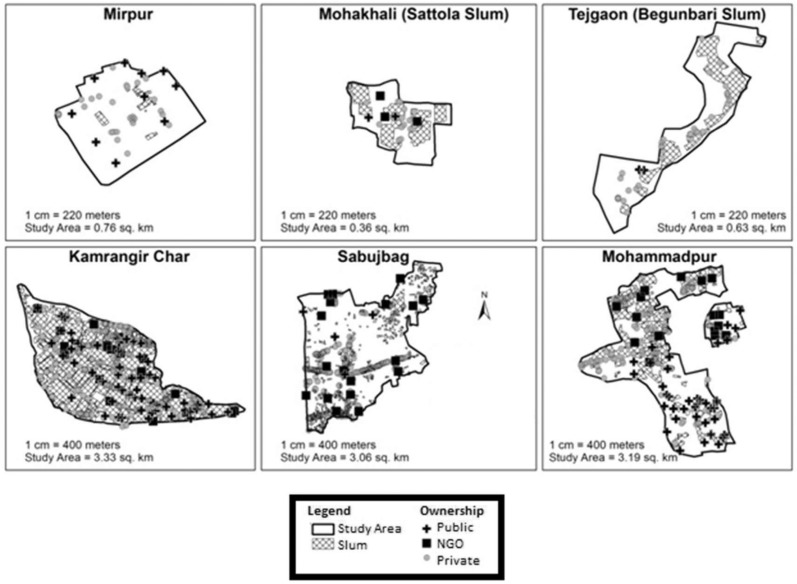
Figure 3.
Map of the study areas showing all HSDPs
Figure 5.
(a) Health service delivery points (private) per 10 000 population. (b) Health service delivery points (Public and NGO) per 10 000 population
To conduct population-based analysis, we applied projected population growth rates (UN-Habitat 2013) on previously reported population density figures for slum and non slum areas in Dhaka given the absence of current census data delineated by slum. One limitation of this approach was a failure to take variation in population concentration into account, leading to an underestimation of population size in some areas. This divergence is minimized by aggregate analyses. Cartographic visualization is employed to illustrate and examine the distribution of health services in and around urban slums. Statistical Package for Social Sciences (SPSS) v. 20 and ArcGIS v.10.1 had been used for data analysis.
Results
Geospatial analyses are presented by slum in the form of density maps to illustrate the diversity that exists between slums. Because a comparative assessment of availability between areas is not supported by study design, most analyses combine data from all six study areas to provide a general understanding of the supply-side configuration of health services located in and around poor urban settlements.
Distribution
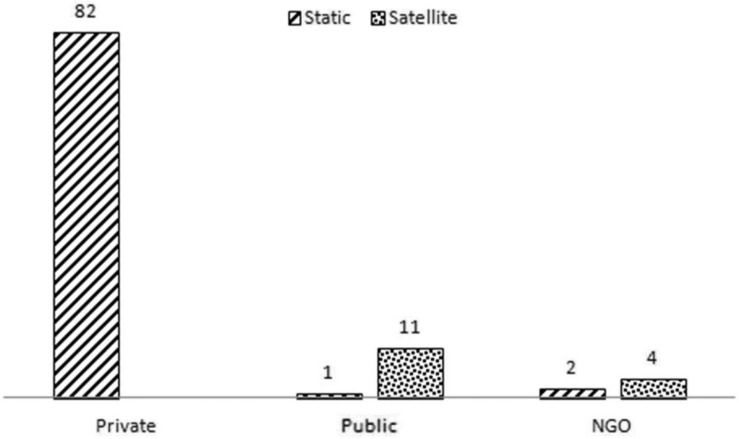
A total of 1041 HSDPs were mapped within the six study areas. Figure 2 illustrates the overall distribution of facilities by management entity and delivery modality. Over 80% of the facilities surveyed were privately operated, with the rest being provided by NGOs either independently or public. Other than an EPI and a National Tuberculosis (TB) programme clinic, the rest were under the local government’s UPHCP project. This distribution is illustrated in Figure 3 where maps of each study area indicate the comparative density of health service provision. The smaller study areas (in the top row) had very few or no NGOs and UPHCP HSDPs. A total of 26 static and 154 satellite clinics were mapped within the perimeter of the six study areas. A noteworthy finding, however, is that 1 km outside study area boundaries, a further 37 static clinics and 249 satellite clinics were identified (see Table 2).
Figure 2.
HSDPs by management entity (%) in the study areas. Note: Twelve delivery centres (DC) from BRAC’s Manoshi project have been mapped in these study areas and are categorized as static clinics in analysis
Table 2.
Proximity of NGO and public health service delivery points to six study areas
| Within study area (n = 179) |
1 km outside study area (n = 286) |
|||
|---|---|---|---|---|
| Static | Satellite | Static | Satellite | |
| Public | 5 | 116 | 21 | 190 |
| NGO | 21 | 38 | 16 | 59 |
| Total | 25 | 154 | 37 | 249 |
Figure 4 provides a more detailed examination of private sector HSDPs, showing that pharmacies and non-formal or traditional doctors made up three quarters of this sector, with private consultation chambers, either attached or unattached to drug shops, accounting for the remaining 20%. Private clinics or diagnostic centers were rarely located within or adjacent to slum settlments. UPHCP and NGO clinics were seen in greater numbers in Kamrangir Char, Mohammadpur and Sabujbag study areas.
Figure 4.
Types of HSDPs within the private sector. *Private clinics and diagnostics centre. **Kabiraj, Hakim, faith healers, doctors without medical qualification. ***Other facilities are Rehabilitation centres, Physiotherapy centres and Optic shops
To investigate the distribution of clinics in greater depth, the density of HSDPs per 10 000 population was calculated (see Figures 5a and b). In total, Kamrangir Char had the highest HSDP density with 2.9 private HSPDs per 10 000 population, while the combined density of NGO and UPHCP service provision was 0.7 per 10 000 population. The lowest population to UPHCP and NGO HSDP ratio was found in Sabujbag (0.2 HSDPs per 10 000 population) and Sattola (0.1 HSDPs per 10 000 population) study areas. The lowest density of private HSDPs was recorded in Mirpur 2 (0.97 HSDPs per 10 000 population), although even then it was 2.6 times higher than the density of UPHCP and NGO HSDPs. The collective ratio for all the study areas was 1.5 HSDPs per 10 000 population inclusive of all formal and informal service delivery points run by NGOs, local government, as well as drug shops, doctors’ chambers, and traditional providers.
Collection of geographical co-ordinates of tertiary hospitals in Dhaka city enabled visualization of the relative aerial distances from each study area. Four particular public hospitals4 that provide low cost general services and are especially frequented by the urban poor are considered here. As shown in Figure 1, the large majority of these facilities are located at least 3 km from the six study areas. In terms of actual travel time (considering road distance, road condition, transport availability and traffic factors), accessibility to these affordable tertiary facilities is much diminished.
Time of service
Given that the large majority of slum residents are involved in income generation activities during daytime hours, important attributes of health service delivery in poor urban settlements are days and hours of service. As shown in Table 3, among formal and informal private sector facilities, 98% were accessible to care seekers every day either continuously between 8 am to 12 am (34%) or during morning and evening hours (44%). The large majority of NGO and public static clinics were open 5–6 days a week, but during limited hours from 10 am to 4 pm in the afternoon. Only UPHCP maternity centres and NGO delivery centres provided 24/7 services. While comparatively large in number, satellite clinics offered services only 1 or 2 days a week in any locality. Evening services were almost exclusively the remit of private HSDPs.
Table 3.
Service days and hours at different HSDPs in six study areas (n = 1041)
| Private % | Public |
NGO |
|||
|---|---|---|---|---|---|
| (n = 861) | Static % (n = 5) | Satellite % (n = 116) | Statica % (n = 21) | Satellite % (n = 38) | |
| Service time | |||||
| 2–3 hours 1–2 times a week | 100 (116) | 100 (38) | |||
| Morning (8 am–12 pm) | 1.6 (14) | ||||
| Morning–afternoon (8 am–4 pm) | 2.0 (17) | 80 (4) | 38.1 (8) | ||
| Morning–evening (8 am–12 am) | 34.1 (294) | 4.8 (1) | |||
| 24-Hours | 1.7 (15) | 20 (1) | 57.1 (12) | ||
| Afternoon–evening (12 pm–12 am) | 2.4 (21) | ||||
| Evening (5 pm–12 am) | 14.3 (123) | ||||
| Morning and evening | 43.8 (377) | ||||
| Service days | |||||
| 1–2 days | 0.6 (5) | 93.1 (108) | 97.4 (37) | ||
| 3–4 days | 0.1 (1) | 2.5 (3) | 2.6 (1) | ||
| 5–6 days | 1.4 (12) | 100 (5) | 0.9 (1) | 42.9 (9) | |
| All week | 97.8 (842) | 57.1 (12) | |||
| Random | 0.1 (1) | 3.5 (4) | |||
aIncludes 12 delivery centres (DC) from BRAC’s MNCH project that support normal delivery and referral in case of complications.
Available heath staff
Table 4 shows the number and composition of available health providers in the six study areas by their designation. A total of 2422 staff was enumerated in the survey, 23% of whom had management roles and 77% who had health service provision roles. This table excludes 52 staff, showing a total of 2370 staff, whose academic/professional qualifications could not be obtained. Those with any medical qualifications such as MBBS (Bachelor of Medicine, Bachelor of Surgery)/BDS (Bachelor of Dental Surgery) doctors (4–5 years), bachelors or diploma in nursing (3–4 years), and diplomas in midwifery (3 years), pharmacy (1–3 years), paramedics (2–3 years), medical/dental assistant (2–3 years) and medical technology (3 years) were categorized as formal. Overall, drug sellers, who go by designations such as drug shop owners, managers, assistants or pharmacists; village doctors; and medical assistants, form the majority (56%) of those who reported being actively involved in providing health care. Only 13% were allopathic doctors or nurses. Seventy percent (1655 out of 2370) of all staff were attached to the private sector, and among the health staff 60% were informal. Support staff was far more numerous in public (66%) and NGO (45.4%) managed HSPDs compared to the private sector (8%). NGOs also employed many informal providers but they generally arranged in-house trainings for their staff.
Table 4.
Available health human resource in six study areas (n = 2370)a
| Designation | Private (n = 1655) |
Public (n = 444) |
NGO (n = 271) |
Total (n = 2370) | |||
|---|---|---|---|---|---|---|---|
| Formal | Informal | Formal | Informal | Formal | Informal | ||
| Health staff | 34.0 (563) | 57.5 (951) | 33.1 (147) | 0.9 (4) | 24.7 (67) | 29.9 (81) | 76.5 (1813) |
| Drug seller (shop owner/manager/assistant/pharmacist) | 4.6 (75) | 32.9 (550) | 26.3 (625) | ||||
| Village doctor | 1.0 (17) | 21.2 (351) | 15.5 (368) | ||||
| Lab Tec/Assistant, Medical/Dental Assistant | 6.3 (104) | 1.0 (17) | 31.1 (138) | 0.5 (2) | 16.6 (45) | 2.2 (6) | 13.2 (312) |
| Doctor (MBSS/BDS/Specialist) | 16.3 (270) | 2.03 (9) | 2.9 (8) | 12.1 (287) | |||
| Doctor (Ayurvedic/Homeopathic) | 5.6 (94) | 0.1 (1) | 4.0 (95) | ||||
| Community health worker or urban birth attendant | 0.2 (1) | 26.5 (72) | 3.1 (73) | ||||
| Nurse/midwife | 0.2 (3) | 1.0 (17) | 0.2 (1) | 5.2 (14) | 1.1 (3) | 1.6 (38) | |
| Spiritual/traditional healer | 0.9 (15) | 0.6 (15) | |||||
| Management and support staff | 8.5 (141) | 66.0 (293) | 45.4 (123) | 23.5 (557) | |||
aTotal staff = Health (formal + informal) + Management and support staff
The academic/professional qualifications of the 1813 health staff are presented in Table 5. As shown, only 37% of private sector health providers possessed some kind of formal academic medical qualification. A breakdown of this figure shows: 18% held a Bachelor of Medicine Bachelor of Surgery (MBBS) degree, while 14% reported having nursing or health associate degrees. In public and NGO facilities, there were far fewer MBBS doctors on staff, but many more nurses and qualified health associates. Over 60% of health staff in the private-for-profit sector had no medical related academic training, compared to 2.6% in public clinics, and 50% in NGOs who were mostly community health workers. A very small proportion of informal providers possessed education beyond high school.
Table 5.
Educational qualifications of health staff (n = 1813)
| Provider qualification | Private % (n) = 1514 | Public % (n) = 151 | NGO % (n) = 148 |
|---|---|---|---|
| Formala | 37.2 | 97.4 | 45.3 |
| Bachelor of Medicine, Bachelor of Surgery (MBBS) and above | 17.6 | 6.0 | 6.1 |
| Bachelor in Dental Surgery (BDs) and above | 0.9 | ||
| DUMSc, DHMSd and above | 5.0 | ||
| Nurse, midwife, medical assistant, paramedic and pharmacist | 13.7 | 91.4 | 39.2 |
| Informalb | 62.8 | 2.6 | 54.7 |
| Bachelor and above | 16.9 | 0.7 | 4.0 |
| High School and below | 45.9 | 1.9 | 50.7 |
| Total | 100 | 100 | 100 |
aTotal number of formal staff: 777. bTotal number of informal staff: 1036. cDiploma in Unani Medicine and Surgery. dDiploma in the Homeopathic Medical System.
In addition to formal academic qualifications, the study collected information on health-related training among health staff. As shown in Table 6, training from NGOs on issues such as Oral Rehydration Therapy, family planning counselling, and infection prevention in clinical settings, was common across all the three sectors. An almost equal proportion (50%) of formal and informal private providers reported having received such training from NGOs, compared to 70% of informal staff in the NGO sector. Many more doctors in the private sector reported being engaged in postgraduation training in some specialized clinical subjects than in the public or NGO sectors. Among informal groups lacking formal medical degrees, 34% had received the Local Medical Assistant and Family Planning Training (LMAF) or Rural Medicine Practitioner (RMP) training neither of which confers any accredited qualification to practise medicine formally. The latter training was a 12-month government sponsored programme that was offered in the 1980s but subsequently discontinued. Other informal private providers reported personal experience gained while working under the supervision of doctors, other pharmacists (not necessarily formally trained) or in work settings like clinics or nursing homes. Very few had received medical assistant or pharmacist trainings which differ from diploma courses given their short duration and specialized curriculum.
Table 6.
Type of health related training received by health staff (n = 1813; multiple response)
| Provider qualification | Private % | Public % | NGO % |
|---|---|---|---|
| Formal Provider (n = 777) | n = 563 | n = 147 | n = 67 |
| Training from NGO | 56.5 | 35.3 | 17.5 |
| LMAF/RMP training | 21.8 | ||
| Post Graduation traininga | 16.4 | 1.5 | 6.0 |
| Medical/dental assistant | 3.0 | ||
| Chemist/pharmacist | 7.0 | ||
| Personal experience/apprenticeship | 6.2 | ||
| Informal provider (n = 1036) | n = 951 | n = 4 | n = 81 |
| Training from NGO | 51.9 | 25.0 | 70.3 |
| LMAF/RMP training | 34.1 | ||
| Medical/dental assistant | 0.5 | ||
| Chemist/pharmacist | 5.9 | ||
| Personal experience/apprenticeship | 9.4 |
aFor MBBS doctors.
Healthcare services
In general, private HSDPs operating in and around the slums provide limited general clinical services including prescriptions. Rather, drug dispensing appears to be the specialty of pharmacies/drug shops. Public and NGO clinics do not report selling drugs as a rule but provide medicines at discounted rates to subscribers of their voucher schemes only. For family planning, especially long-term methods, or maternal, and child health services, slum residents have to rely on the public or NGO HSDPs which are few and far between in the slum areas under study. Nutrition and diagnostic services were lacking in all HSDPs. The most versatile were traditional doctors and the formally recognized Unani or Homeopath doctors who reported treating a range of diseases spanning from simple cough to tumor and cancer. Table 7 shows the availability of selected primary healthcare services across 1007 HSDPs, excluding dental chambers or clinics which provided some specialized services only.
Table 7.
Service availability in HSDPs by management entity (n = 1007a; multiple response)
| Private% (n = 827) | Public (n = 121) |
NGO (n = 59) |
||||
|---|---|---|---|---|---|---|
| Service name | Static% (n = 5) | Satellite% (n = 116) | Static% (n = 21) | Satellite% (n = 38) | Total% (1007) | |
| General clinical serviceb | 99.5 (823) | 100 (5) | 99.3 (115) | 42.9 (9) | 100 (38) | 98.0 (990) |
| Drug sale | 94.3 (780) | 4.8 (1) | 77.6 (781) | |||
| Maternal health | ||||||
| Antenatal checkup | 3.9 (32) | 60.0 (3) | 60.4 (70) | 66.7 (14) | 81.6 (31) | 14.9 (150) |
| Post-natal checkup | 2.5 (21) | 60.0 (3) | 60.4 (70) | 71.4 (15) | 84.2 (32) | 14.0 (141) |
| Normal delivery | 0.5 (4) | 20.0 (1) | 66.7 (14) | 1.9 (19) | ||
| Caesarean delivery | 20.0 (1) | 0.1 (1) | ||||
| Menstrual regulation | 0.5 (4) | 60.0 (3) | 14.3 (3) | 1.0 (10) | ||
| Dilatation and curettage | 0.5 (4) | 20.0 (1) | 14.3 (3) | 0.8 (8) | ||
| RTI/Sexually Transmitted Infection (STI) treatment | 14.8 (122) | 60.0 (3) | 33.6 (39) | 14.3 (3) | 55.3 (21) | 18.7 (188) |
| Family planning | ||||||
| Condom, pill | 52.2 (432) | 60.0 (3) | 98.3 (114) | 28.6 (6) | 92.1 (35) | 58.5 (590) |
| Injectable | 5.6 (46) | 60.0 (3) | 100 (116) | 28.6 (6) | 65.8 (25) | 19.5 (196) |
| Intrauterine device | 60.0 (3) | 19.1 (4) | 0.7 (7) | |||
| Implant | 40.0 (2) | 0.2 (2) | ||||
| Sterilization | ||||||
| Child health | ||||||
| Acute respiratory infection | 16.3 (135) | 40.0 (2) | 7.8 (9) | 14.3 (3) | 55.6 (21) | 16.9 (170) |
| Diarrhoeal diseases | 0.6 (5) | 3.5 (4) | 9.5 (2) | 73.7 (28) | 3.9 (39) | |
| Expanded programme of immunization (EPI) | 0.1 (1) | 80.0 (4) | 39.7 (46) | 33.3 (7) | 86.8 (33) | 9.0 (91) |
| Nutrition | 0.4 (3) | 20.0 (1) | 0.4 (4) | |||
| Immunization | ||||||
| Influenza | 1.7 (14) | 40.0 (2) | 66.67 (6) | 2.2 (22) | ||
| Tetanus typhoid | 60.0 (3) | 5.17 (6) | 55.56 (5) | 15.8 (6) | 2.0 (20) | |
| Hepatitis B | 9.9 (82) | 60.0 (3) | 66.67 (6) | 15.8 (6) | 9.6 (97) | |
| Diagnostic tests | ||||||
| Pregnancy test | 28.4 (235) | 60.0 (3) | 33.3 (7) | 24.3 (245) | ||
| Diabetic test | 39.2 (324) | 20.0 (1) | 28.6 (6) | 32.9 (331) | ||
| Blood routine test | 1.5 (12) | 28.6 (6) | 1.8 (18) | |||
| Urine routine test | 0.1 (1) | 40.0 (2) | 4.8 (1) | 0.4 (4) | ||
| Stool routine test | 0.1 (1) | 9.5 (2) | 0.3 (3) | |||
| Ultrasound | 0.1 (1) | 40.0 (2) | 4.8 (1) | 0.4 (4) | ||
aExcluding dental chamber (n = 34).
bGeneral Clinical Service: cough fever, first aid (minor cut, injury repair, burn); wound dressing, Blood Pressure (BP) and weight measurement.
In general, service charges were much higher in private clinics followed by consultation chambers. A simple procedure such as Menstrual Regulation (MR) could be as expensive as 2300 taka (tk) in private clinics, compared to 1000 tk through UPHCP, and a normal delivery could cost up to 3500 tk in a private facility compared to 500 tk with a traditional doctor (Table 8). Interestingly, doctors at consultation chambers charged fairly competitive fees for consultations and checkups: around 120–130 tk for a general, antenatal or postnatal checkup, and 50 tk for consulting on child health problems. Diagnostic tests could be expensive with the exception of do-it-yourself testing procedures like blood glucose testing using glucometers or home pregnancy tests which were typically administered in drug shops and doctors’ chambers.
Table 8.
Mean costs of selected services (in Bangladesh tk) in HSDPs
| Service name | Private |
Public | NGO | ||||
|---|---|---|---|---|---|---|---|
| Pharmacy | Consultation chamber | Pvt. clinica | Trad doctorb | Otherc | |||
| General clinical | 100 | 117 | 150 | 43 | 100 | 23 | 30 |
| Maternal health | |||||||
| Antenatal checkup | 170 | 128 | 450 | 57 | 21 | 31 | |
| Post-natal checkup | 178 | 138 | 20 | 21 | 34 | ||
| Normal delivery | 1750 | 3500 | 500 | 950 | 1100 | ||
| Caesarean delivery | 9500 | ||||||
| Menstrual regulation | 2333 | 1000 | 1000 | 1967 | |||
| Dilatation and curettage | 1000 | 2000 | 1500 | 4000 | |||
| Child health | |||||||
| Acute respiratory infection | 50 | 20 | 34 | ||||
| Diarrhoeal diseases | 50 | 30 | 35 | ||||
| Nutrition | 20 | 20 | 20 | 40 | |||
| Immunization | 300 | 510 | |||||
| Tetanus typhoid | 43 | 51 | 42 | 20 | |||
| Hepatitis B | 257 | 313 | 275 | ||||
| Diagnostic tests | |||||||
| Pregnancy test | 27 | 26 | 55 | 27 | 30 | 70 | |
| Diabetic test | 41 | 40 | 35 | 42 | 40 | 90 | 117 |
| Blood routine test | 140 | 60 | 200 | 60 | 80 | ||
| Urine routine test | 150 | 120 | |||||
| Ultrasound | 540 | 23 | 30 | ||||
aPrivate clinics and diagnostics centre.
bTraditional doctors—kabiraj, Hakim, faith healers, doctors without medical qualification.
cOther facilities: rehabilitation centre, physiotherapy centre and optic shop.
Discussion
The most prevalent form of health service provision in slum areas under study was the informal private sector, with formal provision limited to a few NGOs operating maternal, neonate and child care services, and satellite clinics providing basic primary care on specific days and hours of the week. Satellite services were typically confined to general counselling for adults and children on cough, fever and diarrhoea, antenatal and post-natal checkups, the provision of non-prescription drugs including vitamins, paracetemol and iron folate tablets, and referral to static clinics. While outreach services are intended to increase utilization in slum populations following the successful application of this approach in rural Bangladesh (Arifeen et al. 2013), its effectiveness in the urban context has not been systematically assessed. One obvious shortcoming is the failure of formal services to take into account the needs of the working poor who are unable to avail services during daytime hours. The proliferation of informal drug sellers and itinerant doctors within slum areas can be interpreted as a supply-side response to demand for accessible services. Outside of the regulatory framework, and with minimal financial investment, these providers are able to offer extended hours of services, and can set up and relocate easily as per the needs of the poor urban populations they serve.
By contrast, static primary care clinics within slum areas are very few in number, reflecting the challenges of justifying infrastructural investments in the context of tenure insecurity. Given that the large majority of slums in Bangladesh are located on private land that is frequently contested (Brueckner and Selod 2009), negotiating for space and security of tenure are complex and difficult to assure. As a result, the large majority of both UPHCP and NGO static facilities are found on or beyond slum area boundaries where physical infrastructure is easier to secure.
Findings also draw attention to the unequal distribution of HSDPs across urban areas, and in particular, coverage gaps in the availability of low cost primary care services offered by UPHCP and other NGO providers. Clustering of HSDPs in certain study areas and sparse concentrations of services per 10 000 population in others, indicate the need to relocate or more rationally allocate services, and further emphasize the value of facility mapping for decision-making. The substantial travel time between slum study areas and low-cost public tertiary facilities is also cause for concern particularly in the context of health events requiring emergency care. For this reason, WHO is currently advocating for the creation and maintenance of national-level master facility lists to enable informed health systems planning and management (World Health Organization 2012). The implementation of listing and mapping exercises at scale, similar to this study, would support the creation of a master list of this nature.
Although it is well known that the informal private sector constitutes a first point of care for the poor in Bangladesh (Ahmed et al. 2009), this assessment is the first to provide geospatial evidence of their actual density in urban slums, as well as comprehensive data on their characteristics such as health staff qualifications, days and hours of operation, services on offer and associated costs. Unlike the large majority of private sector studies undertaken globally (Mills et al. 2002), this study mapped a full spectrum of formal and non-formal providers. Every drug vendor, frontline worker, itinerant doctor and traditional healer was inventoried within the perimeter of the six slum areas identified for study, thus permitting a more textured analysis of this diverse sector and its responsiveness to the primary health needs of the urban poor.
Demand side factors like familiarity, convenience, accessibility and flexible payment options (Mills et al. 2002; Mahmood et al. 2010; Iqbal et al. 2009) have been cited by many studies as explanations for the proclivity of the poor towards the informal private sector (Mills et al. 2002). Study findings provide supply-side support to this demand-side finding. Working outside of the regulatory framework, the informal private sector has infiltrated slum settlements that are already overlooked by the formal health system, providing longer service hours and convenient access to the working poor (Bloom et al. 2011). Of course, the downside of dependence on the unregulated informal system are issues of quality and rational care, both of which demand attention (Zulu et al. 2011). As in many countries in Africa and South Asia, unauthorized medical treatments and unnecessary or harmful drug dispensing can be detrimental to health and wealth, disease transmission and drug resistance (Mills et al. 2002; Shah et al. 2011; Wachter et al. 1999). Lack of choice and lack of consumer knowledge or awareness of what constitutes quality services or necessary treatment can be exploited by private providers in the interest of maximizing income or maintaining a client base (Parr et al. 2012; Sudhinaraset et al. 2013). The threat of medical impoverishment is substantial particularly given the absence of social protection systems that cover catastrophic payments (Krishna 2010).
Notwithstanding these dangers, it remains that the informal private sector is present and important in urban slums, and cannot be ignored in efforts to increase effective coverage of services. It is ironic, therefore, that so little is known about the underlying business strategies that make the private sector viable in slum settlements. The fact that few public primary care service options exist that are proximate to slums and open at hours convenient to the working poor, suggests that the informal private sector is responding to a lucrative market opportunity. Indeed, an examination of selected service fees/charges reveals that informal private-for-profit providers are strategically positioning themselves as preferred providers, offering comparable or even less costly services than NGO or government providers. Consultation chambers where qualified doctors practise may also be higher priced; however, their proximity to the slum population also confers a competitive advantage.
Formal service delivery efforts can learn from the successful strategies employed by the informal private sector, and at the same time, harm can be minimized through intelligently crafted incentives that encourage the application of quality standards and appropriate referral. Social Marketing Company (SMC) and Smiling Sun have been working with such models to train and engage private sector practitioners and community health workers to provide contraceptive services and timely referral (Schlein and Montagu 2012). Planning efforts should prioritize the provision of affordable and comprehensive quality care close to where the poor reside, and at hours convenient to the working population. Finally, community-based outreach focused on increasing the health literacy of the urban poor, and familiarity with the advantages of formal services in terms of quality and referral, will be critical in encouraging utilization.
Acknowledgements
International Centre for Diarrhoeal Disease Research, Bangladesh, acknowledges with gratitude the commitment of DFID to the Centre's research efforts. We further acknowledge the tireless and dedicated work of the urban mapping team with special mention of Md. Atique Iqbal, Shahnewaz Morshed, Syed Jafar Raza and Shakil Ahmed for their assistance with data management and analysis.
Funding
This research activity was funded by Department for International Development, Uk (DFID), grant number GR-00932. icddr,b acknowledges with gratitude the commitment of DFID to its research efforts. icddr,b is thankful to the Governments of Australia, Bangladesh, Canada, Sweden, and UK for providing core/unrestricted support.
Conflict of interest statement. None declared.
Endnotes
1 BRAC’s Manoshi project provides maternal, neonatal and child health services to poor urban women through community health workers and trained birth attendants. http://health.brac.net/manoshi
2 A GIS firm ‘Concept and Ideas’ was contracted for this purpose.
3 Now known as Urban Primary Health Care Services Delivery Project (UPHCSDP).
4 Dhaka Medical College Hospital (MCH), Sir Salimullah (MCH), Shaheed Sohrawardy (MCH), Bangabandhu Sheikh Mujib Medical University Hospital.
References
- Ahmad A. 2007. Provision of Primary Healthcare Services in Urban Areas of Bangladesh—The Case of Urban Primary Health Care Project. Working paper No 07_9. [Google Scholar]
- Ahmed SM, Hossain MA, Chowdhury MR. Informal sector providers in Bangladesh: how equipped are they to provide rational health care? Health Policy Plan. 2009;24:467–78. doi: 10.1093/heapol/czp037. [DOI] [PubMed] [Google Scholar]
- Agarwal S. The state of urban health in India; comparing the poorest quartile to the rest of the urban population in selected states and cities. Environment & Urbanization. 2011;23(1):13–28. DOI: 10.1177/0956247811398589. [Google Scholar]
- Arifeen SE, Christou A, Reichenbach L, et al. Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. The Lancet. 2013;382:2012–26. doi: 10.1016/S0140-6736(13)62149-2. [DOI] [PubMed] [Google Scholar]
- Badiane A (Ed.) A framework for addressing urban challenges in Africa. Nairobi: UN-HABITAT; 2008. The State of Africa s Cities 2008. [Google Scholar]
- Bangladesh Bureau of Staistics Planning Division and Ministry of Planning Government of the People's Republic of Bangladesh. 2010. Multiple Indicator Cluster Survey 2009. UNICEF. [Google Scholar]
- Bloom G, Standing H, Lucas H, et al. Making health markets work better for poor people: the case of informal providers. Health Policy Plan. 2011;26:45–52. doi: 10.1093/heapol/czr025. [DOI] [PubMed] [Google Scholar]
- Brueckner JK, Selod H. A theory of urban squatting and land-tenure formalization in developing countries. American Economic Journal: Economic Policy. 2009;1:28–51. [Google Scholar]
- Department of Economic and Social Affairs Population Division, World Urbanization Prospects. The 2011 Revision. 2012. United Nations: New York. [Google Scholar]
- European Commission Humanitarian Aid Office, A.D.P.C., Plan Bangladesh, and Islamic Relief Worldwide Bangladesh. 2010. Urban Risk Assessment: A Facilitator's Guidebook. [Google Scholar]
- Krishna A. One Illness Away: Why People Become Poor and How They Escape Poverty. U.S.A: Oxford University Press; 2010. [Google Scholar]
- Iqbal A. Perceptions of quality of care for serious illness at different levels of facilities in a rural area of Bangladesh. Journal of Health Population and Nutrition. 2009;27:396–405. doi: 10.3329/jhpn.v27i3.3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Local Government Division, Local Government (Pourashova) Act 2009. Bangladesh. 2010. Bangladesh Gazette. [Google Scholar]
- Mahmood SS, Iqbal M, Hanifi SM, Wahed T, Bhuiya A. Are ‘Village Doctors’ in Bangladesh a Curse or a Blessing? BMC International Health and Human Rights. 2010;10:18. doi: 10.1186/1472-698X-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills A, Brugha R, Hanson K, McPake B. What can be done about the private health sector in low-income countries? Bulletin of World Health Organization. 2002;80:325–30. [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare (MoHFW), Bangladesh Health Bulletin 2012. 2012. Ministry of Health and Family Welfare, Government of People's Republic of Bangladesh. [Google Scholar]
- Moreno EL, Arimah BC, Mboup G, Halfani M, Oyeyinka OO. USA and Canada: UN-HABITAT; 2013. State of the World’s Cities 2012/2013: Prosperity of Cities. [Google Scholar]
- National Institute of Population Research and Training (NIPORT) 2008. Bangladesh Urban Health Survey 2006. National Institute of Population Research and Training (NIPORT), MEASURE Evaluation, International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), Associates for Community and Population Research (ACPR) [Google Scholar]
- Omaswa F. Informal health workers—to be encouraged or condemned? [Editorial] Bulletin of the World Health Organization. 2006;84(2):83. doi: 10.2471/blt.05.027979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parr J, Lindeboom W, Khanam M, Sanders J, Koehlmoos TP. Informal allopathic provider knowledge and practice regarding hypertension in urban and rural Bangladesh. PLoS One. 2012;7(10) doi: 10.1371/journal.pone.0048056. e48056. doi:10.1371/journal.pone.0048056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasheed S, Adams AM. 2012. Health Care Seeking Among the Urban Poor: What Do We Know, In Lesson Learning Around Urban MNCH FP and Nutrition Service Delivery in Bangladesh: Mapping Challenges And Oppurtunities for Effective Coverage of the Poorest. Unpublished document. Report prepared by the Centre for Equity and Health Systems, icddr,b for DFID Bangladesh. [Google Scholar]
- Save the Children. 2014. Study Brief: Situational Analysis of Selected Slums of Dhaka City. [Google Scholar]
- Schlein K, Montagu D. San Francisco: The Global Health Group, Global Health Sciences, University of California, San Francisco; 2012. Clinical Social Franchising Compendium: An Annual Survey of Programs, 2012. [Google Scholar]
- Shah N, Brieger W, Peters D. Can Interventions Improve health services from informal private providers in low and middle-income countries? A comprehensive review of the literature. Health Policy Plan. 2011;26:275–87. doi: 10.1093/heapol/czq074. [DOI] [PubMed] [Google Scholar]
- Sudhinaraset M, Ingram M, Lofthouse HK, Montagu D. What is the role of informal healthcare providers in developing countries? A systematic review. PLoS ONE. 2013;8:e54978. doi: 10.1371/journal.pone.0054978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streatfield PK, Karar ZA. Population challenges for Bangladesh in the coming decades. Journal of Health Population and Nutrition. 2008;26:261–72. [PMC free article] [PubMed] [Google Scholar]
- Szwarcwald CL, Andrade CLTd, Bastos FI. Income inequality, residential poverty clustering and infant mortality: a study in Rio De Janeiro, Brazil. Social Science and Medicine. 2002;55:2083–92. doi: 10.1016/s0277-9536(01)00353-7. [DOI] [PubMed] [Google Scholar]
- UN-HABITAT. (2006). State of the World's Cities 2006/7: 30 Years Of Shaping the Habitat Agenda. UK and USA: UN-HABITAT. [Google Scholar]
- Wachter D, Joshi M, Rimal B. Antibiotic Dispensing by Drug Retailers in Kathmandu, Nepal. Tropical Medecine and International Health. 1999;4:782–88. doi: 10.1046/j.1365-3156.1999.00476.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization & UN-HABITAT. Switzerland: World Health Organization, UN-HABITAT; 2010. Hidden Cities: Unmasking and Overcoming Health Inequities in Urban Settings. [Google Scholar]
- World Health Organization. 2012. Creating a master health facility list. Geneva: World Health Organization. Available from: http://www.who.int/healthinfo/systems/WHO_CreatingMFL_draft.pdf?ua=1 [accessed 01 September2013] [Google Scholar]
- Zulu EM, Beguy D, Ezeh AC, et al. Overview of migration, povertyand health dynamics in Nairobi City's slum settlements. Journal of UrbanHealth, Bulletin of the New York Academy of Medicine. 2011;88:185–99. doi: 10.1007/s11524-011-9595-0. [DOI] [PMC free article] [PubMed] [Google Scholar]