Abstract
Burkina Faso implemented a national subsidy for emergency obstetric and neonatal care (EmONC) covering 80% of the cost of normal childbirth in public health facilities. The objective was to increase coverage of facility-based deliveries. After implementation of the EmONC policy, coverage increased across the country, but disparities were observed between districts and between primary healthcare centres (PHC). To understand the variation in coverage, we assessed the contextual factors and the implementation of EmONC in six PHCs in a district. We conducted a contrasted multiple case study. We interviewed women (n = 71), traditional birth attendants (n = 7), clinic management committees (n = 11), and health workers and district health managers (n = 26). Focus groups (n = 62) were conducted within communities. Observations were carried out in the six PHCs. Implementation was nearly homogeneous in the six PHCs but the contexts and human factors appeared to explain the variations observed on the coverage of facility-based deliveries. In the PHCs of Nogo and Tara, the immediate increase in coverage was attributed to health workers’ leadership in creatively promoting facility-based deliveries and strengthening relationships of trust with communities, users’ positive perceptions of quality of care and the arrival of female professional staff. The change of healthcare team at Iata’s PHC and a penalty fee imposed for home births in Belem may have caused the delayed effects there. Finally, the unchanged coverage in the PHCs of Fati and Mata was likely due to lack of promotion of facility-based deliveries, users’ negative perceptions of quality of care, and conflicts between health workers and users. Before implementation, decision-makers should perform pilot studies to adapt policies according to contexts and human factors.
Keywords: Maternal health policy, contextual factors, heterogeneity of effects, qualitative study, health worker's leadership, Burkina Faso
KEY MESSAGES.
Perceived quality of care and collaboration beween health workers and communities should be improved to increase success of health policies.
A thick description of the context and actors involved in the implementation of health policy remains fundamental to understanding how effects are produced.
More studies are needed to understand the heterogeneity of effects of health policies.
Health worker's leadership should be encouraged.
Introduction
One strategy widely recognized to reduce maternal mortality is improved access to skilled birth attendance (AbouZahr and Wardlaw 2001; Ronsmans and Graham 2006). Access to a skilled birth attendant (SBA) during labour and early postpartum care could prevent 75% of maternal deaths (Shiferaw et al. 2013). In Africa, this strategy has been expressed in policies to eliminate totally or partially the fees associated with childbirth in public health facilities (Walker and Gilson 2004; Witter et al. 2007; Diarra 2012). Since the implementation of these policies, there has been a growing emergence of literature (Dzakpasu et al. 2013).
However, this literature suffers from three important gaps: (1) a lack of discussion on variations observed in outcomes, (2) the absence of contextual data to interpret the effects and (3) a lack of discussion on the presumed causal links between implementation and outcomes (Ridde and Morestin 2011; Lagarde et al. 2012; Dzakpasu et al. 2013).
Variations in outcomes have been observed between districts and between primary healthcare centres (PHC) in many countries after the implementation of user fees exemption policies but have not been sufficiently explored (Lagarde et al. 2012; Dzakpasu et al. 2013). For example, in Senegal, Ghana and Burkina Faso, variation in facility-based deliveries coverage was observed between districts (Witter et al. 2007, 2010; Ridde et al. 2011). In Burkina Faso, facility-based deliveries coverage increased nationally from 38% in 2003 to 66% in 2010 (INSD 2012). However, disparities were observed between districts and between PHCs (Ridde et al. 2011). For example, in 2010, within the district of Djibo, the facility-based deliveries coverage was estimated (in internal documents supplied by the district health department) at 12% in one PHC compared with 73% in another. Although analysis of effects has shown the increased use of maternal health services, it does not explain the disparities observed in facility-based deliveries coverage. To understand how the effects of health policies occurred requires going beyond this analysis. In this study, we hypothesized that the variations could be explained by problems related to implementation and/or contextual and/or human factors that interact with policies. As well, to interpret effects, it is important to know whether the policy was properly implemented (Carroll et al. 2007). Researchers evaluating user fees exemption policies in Senegal and Ghana did not assess the extent to which implementation followed directives (Witter et al. 2007, 2010), so it is not known whether all components were implemented as intended. Moreover, only some components of the policies were assessed, and those were not examined in relation to the effects observed. In Ghana, for example, health workers’ poor attitudes and informal payments were raised as problematic but they were not considered in connection with the issue of access to maternal healthcare (Witter et al. 2007). Finally, the absence of contextual data in studies on the effects of these policies has been identified as a major weakness in their evaluation (Lagarde and Palmera 2008; Ridde and Morestin 2011; Lagarde et al. 2012; Dzakpasu et al. 2013). Yet, an understanding of contextual and human factors is essential for comprehensive evaluation of the effects of policies (Victora et al. 2005; Gilson et al. 2011). To our knowledge, contextual factors have to date received little attention in relation to user fees exemption policies. Considering these three gaps, we believe that the observed effects of these policies in Africa have not yet been appropriately interpreted. The aim of this research was to narrow these gaps by evaluating the disparities observed in the coverage of facility-based deliveries after implementation of the emergency obstetric and neonatal care (EmONC) policy. To understand how this policy led to variation in the coverage of facility-based deliveries, we looked at if it was implemented in six PHCs and explored contextual and human factors such as the communities’ perceptions of childbirth in health facilities and the interactions between communities and health workers.
Context and intervention (EmONC)
Burkina Faso is a West African country with 17 million inhabitants, most of whom live in rural areas (77%). The population is predominantly young, with 47% under the age of 15 (Ministry of Health 2012). It is one of the world’s poorest countries, with 47% of the population living below the poverty line (Ministry of Health 2012). Life expectancy was 57 years in 2011. Rates of mortality and morbidity are high especially among the most vulnerable populations (pregnant women and children). The maternal mortality ratio has been estimated at 300 maternal deaths per 100 000 live births (OMS 2013): Statistiques sanitaires mondiales 2013, Geneva (p172). The health system spans three levels: district, regional hospital and university hospital. The first level (district) is subdivided into two levels. The district hospital serves as reference for complicated cases coming from the PHCs. At the PHC level, usually two nurses (one of whom is the head nurse, or ICP: ‘infirmier chef de poste’) and a SBA manage the care. They provide basic outpatient and inpatient care, both curative and preventive, including vaccinations and antenatal care. They also provide basic non-surgical emergency obstetric care.
Cases requiring surgical intervention, including caesarean section, are sent to the district hospital.
The second level is the regional hospital, which serves as reference for district hospitals. The third level is the university hospital, which provides specialized care. SBAs at PHCs are trained health professionals who perform deliveries in health facilities. Since 2007, the role of traditional birth attendants (TBA) has been to raise awareness about reproductive healthcare and help women to reach a PHC to give birth. Although TBA no longer have the right to perform deliveries, some continue to do so in remote villages (Ministry of Health 2007). Community management committees (COGES) are responsible for the financial management of PHCs.
In October 2006, the government of Burkina Faso adopted a policy to subsidize EmONC. The main objective of this policy was to increase the coverage of facility-based deliveries and caesarean sections by reducing their costs for patients. The policy subsidizes 80% of those costs, with women paying the remaining 20% depending on the level at which care was provided. For example, for an uncomplicated delivery at a PHC, women have to pay 900 F Franc de la communauté financière Africaine (CFA) (1.4 Euros), which is supposed to cover the medical acts, drugs, supplies and observations. The EmONC policy guidelines list the items that are supposed to be included in the delivery kit (Ministry of Health 2006). They also describe the clinical protocol for each type of childbirth, for example, uncomplicated, complicated (dystocic labour) and caesarean. In cases of obstetric complications, the policy covers the cost of transportation between the PHC and the district hospital. Officially, the worst-off are fully exempted from childbirth costs. However, the policy’s implementation guide provides only a cursory list of the criteria for identifying this population (social isolation, disability) and little guidance on how beneficiaries should be selected (Ministry of Health 2006).
This policy does not address either prenatal or postpartum care. The government had already implemented free preventive prenatal care beginning in 2002, but women were left to pay for postpartum care. Financial resources are directly allocated to districts. District health managers allocate resources to the PHCs. These allocations, based on the volume of services provided to the target population, reimburse the cost of drugs and supplies used for childbirth. The main source of funding is the State, and the budget to finance this policy is 30 billion F CFA (45 million Euros) for the period 2006–15.
It should be noted that, although the policy was announced in October 2006, the actual ‘boot time’ of the implementation in most PHCs was around March or April 2007.
Methods
Conceptual framework
We began with a process evaluation of the EmONC policy implementation that consisted of documenting its operationalization and describe the processes that may explain the observed effects (Chen 2005). We paid particular attention to contextual factors that could influence the outcome (facility-based deliveries coverage). We defined contextual factors as all elements at the microlevel that might have an influence on the use of skilled birth attendance. These factors can be found at the individual level, such as perceived quality of care (satisfaction, staff behaviour) and experience of childbirth in health facilities, and at the organizational level (health centres, human resources) and in the interactions between these two levels (relations between patients and health workers). We organized these factors based on the literature on the determinants of access to skilled birth attendance, which is substantial (Thaddeus and Maine 1994; Ensor and Cooper 2004; Hounton et al. 2008; Gabrysch and Campbell 2009). Gabrysch and Campbell (2009), building upon the work of Thaddeus and Maine (1994), identify four main factors that have a potential influence on access to skilled birth attendance: sociocultural factors (marital status, ethnicity), perceived needs and benefits (health knowledge, quality of care, information, prenatal care), economic accessibility (capacity to cope with costs associated with maternal healthcare) and physical accessibility (transport, distance). We adopted this framework because it summarizes the factors that have potential impact on access to and use of skilled birth attendance in low- and middle-income countries (LMIC). These four determinants guided our data collection, case descriptions and analysis. We used both an inductive and a deductive approach and an iterative process (between conceptual framework and empirical data) throughout the research process to capture factors that might influence outcomes and that could explain the observed variation in facility-based deliveries coverage (Miles and Huberman 1994).
Study design
The district of Djibo was chosen because, during the time of our data collection, it was free of any Non-governmental organization (NGO) intervention to lower the financial barrier to access to skilled birth attendance, thus providing a natural, ‘untouched’ field for exploration of the issues under study. We generated graphs showing facility-based deliveries coverage using interrupted time series analysis with an observation window from January 2004 to September 2009 (for details, see Ridde et al. 2011). Visual analysis of these graphs revealed three trends in facility-based deliveries coverage in the PHCs of Djibo district after implementation of the EmONC policy: (1) ‘immediate effect’: immediate increase in coverage, (2) ‘delayed effect’: increase in coverage beginning more than 1-year post-implementation (2008) and (3) ‘no effect’: coverage unchanged (Figure 1). Quantitative analysis was only used to observe these trends. Within each category of effects, we selected two contrasted PHCs. The list of selected PHCs was discussed and validated with the health district team.
Figure 1.
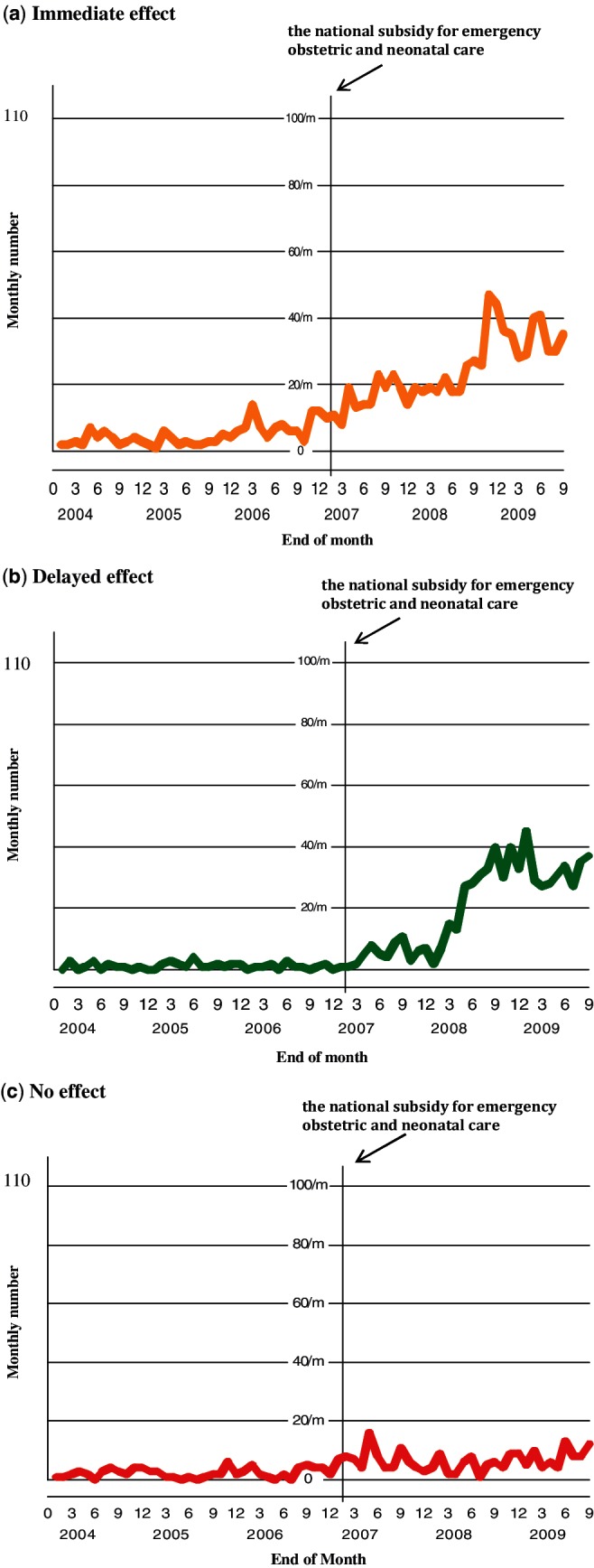
Categories of post-implementation effects of EmONC subsidy: (a) immediate effect, (b) delayed effect, (c) no effect.
We used a multiple case study approach, which involves analysing a contemporary phenomenon within its real-life context, based on various and multiple sources of evidence (Yin 2013b). Within this approach, we employed a multiple contrasted case study design, in which each PHC represented a case. This design is particularly useful for understanding presumed causal relations between a policy and its context (Yin 2013b).
The cases were six PHCs (Tara, Nogo, Belem, Iata, Fati and Mata) of the Djibo district. The cases were contrasted in terms of sociocultural profile (Mossi, Fulani, Fulce, agricultural workers, herders), maternal health (prenatal care coverage, skilled birth attendance) and category of effects observed after implementation of the EmONC policy (immediate, delayed or no effect) (Tables 1 and 2). Contrasted cases were employed to understand why PHCs with different profiles were found to produce similar effects.
Table 1.
Characteristics of the PHCs studied
| PHCs | Population in 2010 | Number of villages | PHC situated close to thoroughfare | Economic activities main | Social and cultural background |
|---|---|---|---|---|---|
| Immediate effect | |||||
| Nogo | 16 199 | 15 | Yes | Animal husbandry | Fulani |
| Tara | 10 962 | 6 | No | Agriculture | Mossi |
| Delayed effect | |||||
| Belem | 13 920 | 8 | Yes | Agriculture | Fulce, Mossi |
| Iata | 6312 | 8 | No | Animal husbandry | Mossi, Fulani |
| No effect | |||||
| Mata | 13 443 | 4 | Yes | Agriculture | Fulce, Mossi |
| Fati | 16 455 | 7 | No | Animal husbandry | Fulani, Songhai |
Table 2.
Epidemiological profiles of the six PHCs studied
| PHCs | Female skilled birth attendants in 2010 | Infrastructure (maternity building) in 2010 | Population (%) living more than 10 km from CSPSa (%) | Contacts per inhabitant per yearb | Rate of antenatal care 2006b (%) | Rate of antenatal care 2010b (%) | Rate of facility-based deliveries 2006b (%) | Rate of facility-based deliveries 2010b (%) |
|---|---|---|---|---|---|---|---|---|
| Immediate effect | ||||||||
| Nogo | Yes | Yes | 19.4 | 0.13 | 14 | 45 | 1.6 | 15 |
| Tara | Yes | No | 40 | 0.25 | 103 | 93 | 21 | 73 |
| Delayed Effect | ||||||||
| Belem | No | Yes | 49 | 0.12 | 33 | 56 | 19.2 | 51 |
| Iata | Yesc | No | 0 | 0.66 | 14 | 95 | 11 | 60 |
| No effect | ||||||||
| Mata | Yes | Yes | 49.4 | 0.23 | 38 | 50 | 36 | 40 |
| Fati | Yesc | No | 85 | 0.10 | 6 | 31 | 3 | 12 |
aDjibo district 2010 action plan.
bData from Djibo district health information system.
cFemale nurse.
Data collection
Data were collected between November 2010 and February 2011 using in-depth interviews, focus group discussions (FGD) and observations. The triangulation of these three methods was used to increase the validity of this study (Yin 2013b). Data were collected from six stakeholder groups: district health managers, health workers, TBA, COGES, women and communities.
In-depth interviews were conducted with health workers and district health managers (n = 26), TBA (n = 7), COGES (n = 11) and women (n = 71), all of whom are key actors involved in this policy (Table 3). All interviews were audio-recorded, translated and transcribed.
Table 3.
Number of interviews per category of actors
| Women | COGES | TBA | Health workers, district health managers | Villages (CHW, women and men) | Total | |
|---|---|---|---|---|---|---|
| Interviews | 71 | 11 | 7 | 26 | 115 | |
| Focus groups | 62 | 62 |
The criterion for selecting women was that they had given birth in a PHC within the previous 8 months. To recruit women for the interviews, we used the birth registry of each PHC to compile a list of names and contact information of 10–15 women from different villages. In those villages, the community health workers (CHW) helped to locate the selected women.
Focus groups (n = 62) of 8–10 individuals were organized in the villages, 46 with men and 16 with women. As no men were interviewed individually, we conducted more FGD with men to collect the necessary information regarding organizing transportation, costs of childbirth and perceptions of their relationships with PHCs. Our aim in conducting such a large number of FGD was to gather the perceptions of residents in all villages covered by the PHCs to better understand the trends observed in facility-based deliveries coverage after implementation of the EmONC policy. The sampling method used to select the members of the FGD consisted in identifying a relatively homogeneous group (people living in rural areas, sharing the same socioeconomic characteristics) with diverse respondents (young, elders, married, unmarried, polygamous, monogamous) in the same group to obtain a wide range of views (Poupart et al. 1997).
At each FGD, the graph illustrating the facility-based deliveries coverage of their local PHC (Figure 1) was shown and explained. Communities were asked to identify factors that could explain the observed trends and to rank these factors according to their importance in influencing the coverage of facility-based deliveries. FGD were conducted in the local language (Fulfulde) by a local assistant, audio-recorded, transcribed and translated into French. The first author was present at all the FGD.
Non-participant observations were conducted in the six PHCs to understand the relationships between health workers and the communities and to assess how these interactions influenced the coverage of facility-based deliveries. The goal of these observations was to ascertain whether the facts presented in the interviews and focus groups were still relevant and current at the time of the study. The first author spent 7–10 days in each PHC and prepared ethnographic notes at the end of each observation day (Emerson et al. 2011).
Data analysis
QDA Miner® qualitative software was used to code the data from the interviews and FGD. We used a thematic approach to organize the data (Miles and Huberman 1994). The coding scheme was mixed (Van der Maren 1996) and was based both on factors identified in the literature as having an influence on access to skilled birth attendance and on empirical data from fieldwork (Van der Maren 1996). Each PHC was analysed individually to understand how and why the EmONC policy produced the trend of effects observed. Then, the two PHCs in each category of effects were examined together for similarities and contrasts. Finally, the six PHCs were analysed together to identify any cross-cutting factors that could explain the variations in facility-based deliveries coverage. Our aim in this study was to document the causes of variations in facility-based deliveries coverage after the implementation of the EmONC policy. As recommended by Yin (2013b), we adopted an explanation building strategy, which is useful when trying to understand how or why something happened, and used a narrative approach because: ‘In most existing case studies explanation building has occurred in narrative form’ (Yin 2013b). We aimed to capture all factors related to community life, health centres, human resources, etc. that might have an influence on facility-based deliveries coverage in each PHC.
Study area
The district of Djibo is located in the province of Soum in Burkina Faso. The population estimate in 2011 was 402 646 inhabitants, predominantly Muslim; 37% live below the poverty line. The main economic activities are farming and agriculture. Forty-two per cent of the population lives more than 10 km away from the nearest PHC (Ministry of Health 2012). Djibo has 30 PHCs and one district hospital. Of the 30 PHCs, 27 do not meet structural standard lacking in the basic infrastructure required for normal functioning, for example, a separate maternity unit, a pharmacy, living quarters for health workers. Three PHCs (10%) do not have sufficient professional staff. On average, Djibo’s PHCs serve 12 500 inhabitants, whereas the national average is 10 000. Estimates from 2010 suggest that there is one midwife per 25 165 inhabitants in Djibo, in stark contrast to the national average of one per 5000. The average distance between villages and PHCs is estimated at 11.4 km (Ministry of Health 2012).
The number of curative consultations was 0.3 per year per capita in 2011 against a national average of 0.7. In 2010, the facility-based deliveries coverage was estimated at 55% against a national average of 66%. Eighty-two per cent of women had attended two antenatal care visits. The rate of postpartum consultation was estimated at 50.6%. The rate of prevalence of contraception was 22% in 2010. The district recorded 179 maternal deaths for 100 000 parturients in 2011. The main causes of death identified were infections and haemorrhage (Ministry of Health 2012).
Results
In the following sections we present the results pertaining to the implementation of the EmONC policy in the six PHCs, followed by the contextual factors that could explain the variations in facility-based deliveries coverage observed following the policy’s implementation in early 2007.
Implementation of the EmONC policy in the six PHCs
Overall, the six PHCs implemented the EmONC policy faithfully and almost homogeneously. The majority of components was implemented (Table 4). The reimbursement system for the EmONC subsidy and the free transport by ambulance were properly implemented in the six PHCs. No significant shortages of drugs or supplies were observed, except in Fati, where low drug stocks reflected low attendance at the health centre.
Table 4.
Results of the implementation of the EmONC policy in the six PHCs
| EmONC Components | PHCs | |||||
|---|---|---|---|---|---|---|
| Tara | Nogo | Belem | Iata | Fati | Mata | |
| Subsidies | ||||||
| Reimbursement system | I | I | I | I | I | I |
| Real cost of childbirth | V | V | V | V | V | V |
| Worst-off exemptions | N | N | N | N | N | N |
| Emergency transport | I | I | I | I | I | I |
| Quality of care | ||||||
| Drug and supplies | Good | Good | Good | Good | Not good | Good |
I, implemented; V, variation from policy; N, not implemented.
We noted a disparity between what women actually paid for childbirth and what they were supposed to pay (900 F CFA, 1.4 Euros). This disparity was observed in all six PHCs. However, we did not explore the reasons behind this disparity. Others studies have been assessing this implementation gap (Ben Ameur et al. 2012; Ridde et al. 2013).
Although the costs were reduced compared with the costs before the policy’s implementation (4000 F CFA, 6 Euros), women still had to pay between 750 F CFA (1.14 Euros) and 2400 F CFA (3.66 Euros). Few of them knew the real costs and what items (drugs, supplies, acts and hospitalization) were included in this amount. The majority of them had paid for cleaning products. Some had to pay for antibiotics and episiotomy sutures.
The subsidy for the worst-off was not implemented in any of the six PHCs. The apparent reason for this failure was that health workers and district managers did not know of the existence of this component of the policy. ‘I’m not aware of this system. Maybe it’s at the level of the financial management’ (District manager).
Contextual factors
Although the EmONC policy was generally well implemented, our data suggested that the variations could be explained mainly by contextual and human factors.
Immediate effect (Nogo, Tara)
Our data showed that the immediate increase observed in facility-based deliveries coverage in the PHCs of Nogo and Tara could be explained by health workers’ leadership and transmission of information about the subsidy, the communities’ positive perceptions of quality of care and the arrival of female professional staff.
Health workers’ leadership
Health workers’ leadership, expressed through both creative strategies to promote facility deliveries and close co-operation with communities (COGES, CHW), had a positive influence on the coverage of facility-based deliveries. Generally, promoting the use of maternal health services is a standard part of health workers’ daily responsibilities. They are expected to raise awareness during prenatal care and children’s vaccinations, and to provide information on EmONC during these activities. However, in the PHCs of Nogo and Tara, the promotion of facility-based deliveries was particularly original, intensive and specific compared with the other PHCs. In fact, respondents in those communities identified two strategies they considered to be key sources of encouragement to women to give birth in health centres. In Nogo’s PHC, the COGES funded fuel to enable health workers, particularly the ICP, to travel around the area between early 2007 (policy boot time) and 2008 to promote facility-based deliveries. ‘My role was to mobilize the COGES to enable women to come here for maternity services’ (ICP, Nogo). The ICP informed villagers about the risks of home births and the benefits of facility-based deliveries, as well as about the subsidy. In Tara, between November 2007 and December 2009, the ICP, in collaboration with local authorities, recruited 10 women per village as volunteers whose task was to encourage pregnant women to use the PHC for childbirth. These volunteers went door-to-door, speaking informally with pregnant women about the importance of giving birth in a health centre. These creative initiatives to promote facility-based deliveries led to a positive perception of childbirth in public health centres. Women identified these activities as the trigger that led them to go to the health centre to give birth. ‘It’s only now we’re being told to give birth in the PHC’ (Female, Nogo). ‘It was the health workers who told me to give birth there. For my first children, I wasn’t told to go to the PHC’ (Woman, Tara).
Both strategies were based on relationships of trust with community agents. Men reported: ‘They (health workers) do a great job. Our CHW is working with them (health workers)’ (FGD, Nogo). Nogo’s health workers were particularly effective in transmitting information to villagers on the existence of the EmONC subsidy. This was identified as a key factor in the immediate increase in facility-based deliveries. ‘Before, if you went there and had no money, you suffered a lot because you had to spend so much you often went into debt. But now you can’t go into debt for just 900 francs’ (FGD, Nogo).
Positive perceptions of quality of care
The communities’ positive perceptions of quality of care not only contributed to a positive experience of facility-based childbirth for women but also helped to strengthen relationships between communities and their health centre. The availability of health workers was particularly appreciated by communities. ‘The health workers who are there now, we haven’t yet had any problem with them. No matter when you go there, even if it is night, you can go wake the person and he’ll come to see you’ (FGD, Nogo). According to the women, the positive experience of giving birth at the health centre was associated with a healthier, cleaner, easier, less painful childbirth (compared with home birth). The staff was available and helpful. ‘Giving birth at the health centre is not difficult’ (Woman, Tara).
“Before when a woman gave birth at home, we couldn’t go into the home because of the smell of blood. And the woman was exhausted, and there were no drugs. Today [at the health centre] you don’t smell bad [from blood], and you return home clean and nice-smelling, with your clothes in good condition. And you’re healthier, too” (TBA, Nogo).
‘She [skilled birth attendant] is doing a great job. When we arrived, I was in a lot of pain. She was working; we called her and she ran right over to us. The child was born fast’ (Woman, Nogo). ‘She [skilled birth attendant] was never harsh with me, not even once’ (Woman, Nogo). ‘I have seen the benefits, because I usually gave birth at home and none of my children survived. I gave birth to this one, and now he is still alive. All this, thanks to their treatment’(Woman, Nogo).
The arrival of female professional staff
The arrival of female staff in both PHCs not only helped increase the provision of maternity services but also made the communities more comfortable because childbirth was managed by female professionals. It is important to note that the positive influence of this human resources factor on facility-based deliveries coverage was not due to gender alone, but rather to the combined effect of gender and professional role.
In Tara, when a female SBA joined the team in early 2008, it strengthened the already positive trend in facility-based deliveries.
“Before, it was only men working there. We didn’t very much like having a man working with a woman, and so the women didn’t go there. But when that midwife arrived, people were happy and that’s why women go there” (FGD, Tara).
In Nogo, four female professionals (two SBAs, a nurse and a midwife) successively joined the medical team from April 2007 to April 2009. The nurse and one of the SBAs provided care during the night when they were working; they slept on-site, whereas the other health workers routinely went home nights. According to district health managers, these two female staff were known for their good work. Before their arrival, the PHC did not provide maternal health services during the night. However, it should be mentioned that this increase in human resources was unplanned and not directly related to the EmONC policy, but rather to particular circumstances having to do with some of these workers’ family situations. It is noted that all the factors that contribute to the immediate increase on the coverage of facility-based deliveries are related to human resources and more specifically to quality of work of health professionals.
Delayed effect (Iata, Belem)
At Iata and Belem, where the policy’s effect was delayed, our data suggested that these delays might be explained by the change of healthcare team in Iata and the implementation of a penalty fine for home births in Belem.
The arrival of a new healthcare team at Iata’s health centre
Between April 2007 (implementation boot time) and February 2008, the staff of Iata’s PHC was completely replaced. A new ICP was assigned in April 2007, temporarily assisted by a nurse from the previous team who remained until two new nurses, including one woman, arrived in February 2008. The change had a positive influence on the coverage of facility-based deliveries, which increased markedly with the arrival of the two nurses. The change provided female staff to manage the maternity ward, and led to improved relationships with the communities. This team also developed creative initiatives to promote facility-based deliveries. The new team appeared to be closer to the people they served. ‘Those who are here today, we haven’t yet had any problem with them. They also work well’ (FGD, Iata). They collaborated more positively with communities and built relationships of trust with them.
“To be effective in raising awareness, you first need to create a relationship of trust between you and the villagers. To integrate into the community, you need to be at their level. Once you feel integrated, that’s when you try to change things” (ICP, Iata).
Our observations confirmed this finding. The PHC was always open; people came and went freely. A TBA was often in the PHC assisting health workers in the maternity ward. The team’s positive relationship with the TBA helped strengthen the relationship between health workers and the community.
This team developed activities to promote facility deliveries. The two male health workers focused on raising awareness among men as a strategy to reach women. These strategies were informal and social, such as playing cards or drinking tea with them. ‘We ask our friends to bring their wives to give birth in the PHC’ (ICP, Iata). These activities have a positive influence on facility-based deliveries coverage. ‘It was the health workers who came to tell us about this. That’s when our husbands started telling us to go, and even all our relatives’ (Woman, Iata). Another woman said, ‘It’s the health workers who tell us to give birth there’ (Iata).
The application of a penalty fee for home births at Belem’s health centre
In Belem, a penalty fee for home births was implemented between September 2008 and
December 2009. Under this system, husbands paid a fee ranging from 10 000 F CFA (15 Euros) to 15 000 F CFA (22 Euros) if their wives gave birth at home. This fee was introduced by local authorities with the knowledge of the health district. It was eventually halted by the highest authorities of the region, who pronounced it illegal. Several focus groups identified the penalty fee as a major incentive to use maternal health services. ‘When the penalty fee was introduced, no one gave birth at home anymore’ (FGD, Belem). ‘It was the penalty fee that had the most impact [on the coverage of facility-based deliveries]’ (FGD, Belem).
The delayed effect could be explained by human factors. Indeed, the change of the new healthcare team (being considered more positive for communities) of Iata and the implementation of the penalty fee in Belem are related to actors’ initiatives to make changes on the coverage of facility-based deliveries.
No effect (Mata, Fati)
In Mata and Fati, our results identified five factors that had a negative influence on facility-based deliveries coverage and might explain the lack of effect: the absence of activities to promote facility-based deliveries, a poor perception of quality of care by communities due to negative attitudes of health workers, conflicts between communities and health workers, informal or illegal payments, and distance between villages and the PHCs.
The absence of activities to promote facility-based deliveries
Because facility-based deliveries were not promoted, there was a perception in the community that health services must be used only in cases of complications. Indeed, women delayed seeking care based on their ability to endure pain. ‘If there are no complications, we don’t go to the PHC’ (FGD, Fati). Few women were aware of the risks associated with home births; most believed that antenatal consultation at PHCs was sufficient preparation to be able to give birth at home. This lack of knowledge was due to low attendance at the health centre. ‘They go [to the PHC] to be weighed. If there are really no complications, they give birth at home’ (FGD, Fati).
Poor perceptions of quality of care
The communities’ poor perceptions of the quality of care were a key element in explaining the unchanged coverage of facility-based deliveries. In fact, women reported that health workers’ unavailability and negative attitudes (rudeness, hostility, verbal abuse) were the main obstacles to their use of health services in both centres. For example, five SBAs worked successively in Mata from 2004 to 2009. Several conflicts were reported between some of them and the women. ‘Many women said they were not well received. She [the SBA] was not at all easy to get along with’ (ICP, Mata). ‘There was a skilled birth attendant there who had no head on her shoulders’ (TBA, Mata). However, the arrival of the most recent (fifth) SBA in 2010 had a positive influence on the quality of care perceived by communities. We observed that she was close to the communities. She was often invited to marriages and baptisms. She distributed porridge for pregnant women and children. She worked very closely with a TBA, who was with her every day in the PHC and even nights during childbirth. ‘She really helped me a lot, the one who is here now’ (Woman, Mata). ‘She washes our loincloths, cleans the baby; you really have to have a heart to do that’ (Woman, Mata).
Conflicts between communities and health workers
In both PHCs, we observed serious conflicts between the healthcare team and the COGES, CHW and TBA. Health workers perceived these agents as non-collaborative in helping with health centre activities. ‘In the 30 PHCs, maybe 2% of the COGES work well. If you take a COGES chairman, he doesn’t even know what is his tasks are’ (current ICP, Mata). ‘They rarely come to the PHC. Or they come, they attend the meeting, and then they disappear’ (previous ICP, Mata).
For their part, the COGES members, CHW and TBA complained that the health workers did not involve them in their activities. They felt excluded. ‘Most of the time, it [the relationship] doesn’t work. There’s no collaboration between the health workers and us’ (COGES, Fati).
“As CHWs assigned to the villages, we’re supposed to work with them. So, if I’m supposed to work with you, we need to understand each other. When I talk go there for any problem, they don’t even want to hear us, they don’t even consider us” (FGD, Fati).
Informal or illegal payments and distance
At Fati, the relationship between the healthcare team and several villages had deteriorated over the years, resulting in a negative perception of the PHC. This was due in large part to the health workers’ practice of demanding informal and illegal payments, which we observed and which was reported by communities only with regard to this health centre. Prices of drugs and supplies were not respected. ‘A drug you can get for 1000 francs [1.5 Euros] in Iata, they [in Fati] might sell it to you for 5000 francs [7 Euros]’ (FGD, Fati). Some drugs that were supposed to be free or subsidized were charged to users. In particular, drugs and supplies used for prenatal care were charged at full price. ‘They won’t even give you your health record. I know it used to cost 100 francs [0.15 Euros], but now they charge 450 francs [0.7 Euros]’ (FGD, Fati).
The important factors that explain the lack of effect on the coverage of facility-based deliveries are related to the quality of work of health workers.
Finally, in Fati, the average distance between villages and the health centre is greater than for the other PHCs. Of the eight villages located in that PHC’s catchment area, only three are located within 10 km. ‘It’s mainly because of the distance [that we don’t go there]’ (FGD, Fati).
Discussion
The results of the study show that the directives for implementation of the EmONC policy were generally respected and that implementation was almost homogeneous in the six PHCs. However, the subsidy for the worst-off was not implemented in any of them due to health workers’ and district health managers’ lack of knowledge about the policy (Belaid and Ridde 2012). Disparities were observed in the six PHCs between what women really paid for their childbirth and what they were supposed to pay according to the policy. However, we did not assess the reasons behind these disparities observed in this study. Two quantitative studies carried out in Burkina Faso have evaluated this heterogeneity of costs related to the EmONC policy (Ben Ameur et al. 2012; Ridde et al. 2013).
Our data suggest that variations in facility-based deliveries coverage could be explained by contextual and human factors. The leadership of health workers, expressed in creative initiatives to promote facility-based deliveries, strong relationships of trust with communities, users’ positive perceptions of quality of care and the arrival of female professional staff, could explain the immediate effect observed in the PHCs of Nogo and Tara. The change of healthcare team at Iata’s health centre during the first year of implementation and the application of a penalty fee for home births in Belem may explain the delayed effect of the EmONC policy on facility-based deliveries coverage in those two areas. Finally, the absence of activities to promote facility-based deliveries, a poor perception of quality of care, and negative relationships between health workers and communities could explain the unchanged coverage of facility-based deliveries in the PHCs of Fati and Mata (Table 5).
Table 5.
Synthesis of results
| Categories of effects | Contextual factors |
|---|---|
| Immediate effect (Nogo and Tara) |
|
| Delayed effect (Iata and Belem) |
|
| No effect (Mata and Fati) |
|
Health workers’ leadership: a key determinant of use of skilled birth attendance and essential to the success of health policies
Leadership, or lack thereof, seems to be a key explanatory factor for the three types of effects observed. Based on our findings, we defined leadership as the development of a particular set of skills, which include taking personal initiatives to improve health indicators by providing better information and increasing knowledge in communities, delivering positive quality of care, and building relationships of trust with communities (Bedwell et al. 2012). Although the study was not intended to study leadership in depth, the characteristics we identified through this study are the same as those found in the literature on health system performance (Wong and Cummings 2007; Haddad et al. 2009; Meda et al. 2011).
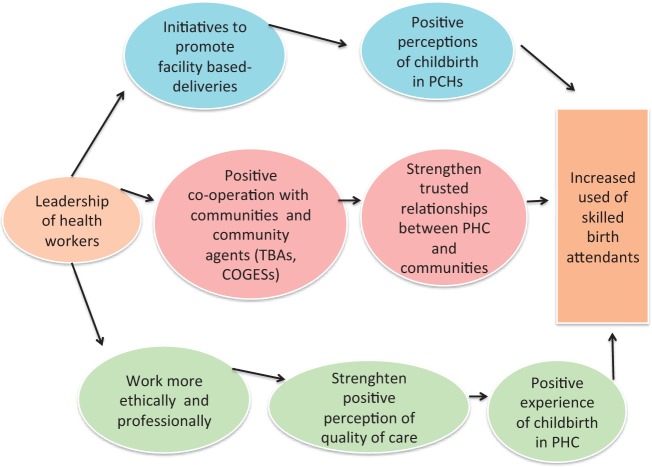
Health workers’ leadership appeared to act on three main factors—perceptions regarding childbirth in PHCs, perceived quality of care and relationships with communities—and on both the individual and the community levels (Figure 2) (Haddad et al. 1998, 2009). The promotion of facility-based deliveries has changed women’s perception of childbirth assisted by qualified health staff. Our findings support the literature showing that women who have more knowledge about obstetric risks and complications are more likely to give birth in a health facility (Stekelenburg et al. 2004; Gage 2007).
Figure 2.
Effects of leadership of health workers on use of skilled birth attendance.
The perceived quality of care is a subjective matter that ‘largely depends on [people’s] own experiences with the health system and those of people they know’ (Thaddeus and Maine 1994, as cited in Gabrysch and Campbell 2009, p. 9). In this study, we included within this component women’s satisfaction with the intervention (labour during childbirth) and with health workers’ behaviour. According to the literature, perceived quality of care is identified as a major determinant of access to skilled birth attendance (Kyomuhendo 2003; D’Ambruoso et al. 2005; Mrisho et al. 2007; Wild et al. 2010; Some et al. 2011). Negative behaviours of health workers (verbal and physical abuse, rudeness) are often mentioned as an important deterrent to use of skilled birth attendance (Jewkes et al. 1998; Gilson et al. 2005). By working more professionally and ethically (being more available in health centres, respecting the fees for consultations and drugs), health workers can improve communities’ perceptions of the quality of care. Although the literature on healthcare leadership in high-income countries does not necessarily include the dimensions of ethics and professionalism, it appears very important to include them as characteristics of leadership in LMIC because these two dimensions affect perceived quality of care, which has been identified as a key determinant of health services access and use (Haddad and Fournier 1995; Haddad et al. 1998). Thus, in LMIC, positive perceptions of quality of care contribute both to a better childbirth experience for women in health centres (individual level) and to more effective co-operation with communities (CHW, TBA, COGES) (community level) (Amooti-Kaguna and Nuwaha 2000; D’Ambruoso et al. 2005). Positive collaboration with communities results in better dissemination of information and health knowledge and stronger relationships of trust with the health centre. This was exemplified by the positive relationships with communities created by the new health team in Iata. The literature supports this finding. In Mali, for example, when health workers built relationships of trust with communities, the use of skilled birth attendance increased (Dogba et al. 2012). The collaboration between the new SBA and the TBA in Mata had a positive influence on facility-based deliveries coverage. The importance of CHW should not be underestimated; most recent guidelines of international organizations recommend working with them to develop interventions. Indeed, international interventions rely increasingly on trained CHW, especially in reproductive health and child health (malaria) (Ejembi et al. 2013). Moreover, community-based agents are still considered important actors within communities. A study in Ethiopia has shown that women prefer home birth assisted by a TBA, who is still a culturally important figure (Shiferaw et al. 2013). Another study has shown how integrating midwives at the community level has a positive influence on the health system, specifically in countries with limited resources (Sherratt 2013). However, the literature on leadership in LMIC is sparse, and policy changes in LMIC are still ‘considered to be situated at the top level of the health system and more focused on financial and administrative considerations’ (Gilson 2003; Haddad et al. 2009). Our research findings suggest strongly that it is time to focus on making changes at the bottom of the health system pyramid to foster health workers’ empowerment and leadership, because they make a difference in health outcomes and are key actors in the success of health policies. In fact, several studies have shown how the leadership of health district managers has contributed to better performance in health indicators (Gilson et al. 2005; Haddad et al. 2009; Meda et al. 2011).
Assessing context: essential for interpretation of health policies
A major weakness in analyses of user fees exemption policies is the lack of contextual data (Lagarde et al. 2012; Dzakpasu et al. 2013). The causal relationships between these policies and increased use of health services need to be assessed more carefully, as these policies are implemented in real-life contexts that necessarily interact with the policies (Wilkinson et al. 2001; Nabyonga et al. 2005; Penfold et al. 2007; Witter et al. 2007). Indeed, our study shows that contextual factors, especially human factors, appear to influence facility-based deliveries coverage, both positively and negatively. Taking contextual factors into consideration would enable better interpretation of effects observed and would increase the internal and external validity of interventions (Victora et al. 2005). This study has shown how the human factor was central in explaining variations in facility-based deliveries coverage. By human factors, we include the quality of work of health workers, their performance, their leadership, their initiatives and strategies to improve the use of maternal health services. Yet this factor is still largely neglected in the literature on access to skilled birth attendance, which remains primarily focused on geographic and economic accessibility (Thaddeus and Maine 1994; Gabrysch and Campbell 2009). In our study, geographic and economic barriers to skilled birth attendance emerged as secondary in importance, except in Fati (for the geographic barrier). In our findings, economic accessibility was not identified as an explanatory factor for the variation in facility-based deliveries coverage, except in Nogo, where information on the EmONC subsidy was particularly well disseminated. One explanation for this finding could be the observation that the costs of childbirth varied in the six PHCs. Few women knew the exact cost of their childbirth and what items were included in the package. Other explanations along the same lines might be that people did not fully understand the costs because they were not used to attending health centres (Tara, Iata, Mata), or that health workers had already undertaken strategies to reduce costs prior to the implementation of the EmONC policy (Belem), or even, in centres where informal/illegal payments were demanded by health workers (Fati), that users were not told the real costs of EmONC.
This study’s strengths reside in the intensive fieldwork (four months) and the diversity of data collection methods and study population. Some limitations should be kept in mind. First, the three categories of effects were defined at a given point in time (autumn 2010) from the available data. The trends we observed may have changed since that time. Second, the interview guide and transcripts required translation, which introduces the potential of translation bias. To limit such bias, the interview guide was translated by two local assistants and the results compared; only very minor differences were noted and adjustments made. The interviews were translated orally during the investigation and translated again after transcription. No differences were observed between the two translations.
Third, the study was limited to one district due to budget and time constraints. Consequently, the results cannot be generalized to the whole country. However, using a multiple contrasted case study as a research design allowed us to carry out analytic generalization, which Yin suggests contributes ‘to a better understanding of an intervention and its outcomes’ (Yin 2013a). Analytic generalization was facilitated in two ways. First, we used a strong conceptual framework to guide our study design, data collection, and analyses within and across cases. Second, we applied the same case selection criteria systematically to all six cases. These methodological strategies have been used successfully for analytic generalization in other settings (Mookherji and LaFond 2013).
Conclusion
The aim of this study is to understand how a policy implemented at the national level resulted in variable effects (coverage of facility-based deliveries). This is one of only a handful of studies using a qualitative in-depth fieldwork methodology at the micro level to analyse a national health policy. Our results show that contextual and human factors explained much more of the variation observed than did implementation factors.
This research uncovered relevant data on the importance of health workers’ leadership. This finding emerged from the fieldwork and explains much of the variation observed in facility-based deliveries coverage after the implementation of the EmONC policy. This factor seems to act on several levels—for example, in the relationships between providers and patients, populations, CHW, TBA and COGES—and contributes to the achievement of policy objectives insofar as it acts as a positive confounding factor.
For health researchers, it is essential to study leadership in health professionals at the district and health centre levels. This area of research is still largely neglected in LMIC (Haddad et al. 2009). For the health system, it is important to develop interventions to strengthen health workers’ leadership. An essential step in this direction would be for the Ministry of Health and those charged with operationalizing such policies to establish a platform for discussion and reflection with the research communities, in order to develop effective interventions.
It would also be important to conduct pilot studies before implementing policies and then, based on the results, to adapt the policies to the contexts and actors, which was not done in Burkina Faso. Paying attention to contextual factors that could act negatively on the effects targeted by policies and strengthening the factors that could potentially reinforce desired political effects are vital to the success of any such policy, as are collaboration, reflection and discussion on strategies to improve health workers’ leadership at the primary healthcare level.
Supplementary Material
Acknowledgements
The authors wish to thank all district managers, health workers and communities of the District of Djibo. They would also like to thank the NGOs HELP and Médecins du Monde for their support during field data collection. They wish to thank Dr Heinmuller Rolf for his contribution in doing time series and graphical representation of the rates of facility based deliveries that were used for this study, Dr Sabine Gabrysch and Professor Pierre Fournier for their reading of the manuscript and their helpful comments, and Donna Riley for her linguistic and editing revision of the article.
L.B. is a Ph.D. candidate in Public Health at the University of Montreal. V.R., Ph.D., has been doing research on equity and access to healthcare systems in Africa for more than 10 years. He is Associate Professor in Global Health at the University of Montreal/CRCHUM and an Associate Researcher at the Institut de Recherche en Science de la Santé of the CNRST in Burkina Faso.
Funding
This article is drawn from a research programme co-ordinated by the LASDEL of Niamey (Niger) and the University of Montreal-CRCHUM (Canada). It was funded by the Agence Française de Développement (AFD) and the International Development Research Centre (IDRC) of Canada. L.B. received a bursary from the faculty of graduate studies of the University of Montreal. V.R. is a ‘New Investigator’ of the Canadian Institutes of Health Research (CIHR).
Competing interest
The authors declare no competing interests.
Authors’ contributions
Both authors participated to the study design. L.B. collected and analysed the data and wrote the first draft under the supervision of V.R. Both authors read the final draft and approved it.
Ethical approval
The health research ethical committees of the Ministry of Health of Burkina Faso (no. 2010-072) and of the CRCHUM (Centre de recherche du centre hospitalier de l’Université de Montréal) (10.178) approved the study. Authorization from the Directorate of Health Sahel was obtained (2010 06 04 MS-RSHL-DRS) to carry out this research. Fictitious names were given to the six PHC to preserve the confidentiality of participants.
Conflict of interest statement: None declared.
References
- AbouZahr C, Wardlaw T. Maternal mortality at the end of a decade: signs of progress? Bulletin of the World Health Organization. 2001;79:561–8. Erratum: 1177. [PMC free article] [PubMed] [Google Scholar]
- Amooti-Kaguna B, Nuwaha F. Factors influencing choice of delivery sites in Rakai district of Uganda. Social Science and Medicine. 2000;50:203–13. doi: 10.1016/s0277-9536(99)00275-0. [DOI] [PubMed] [Google Scholar]
- Bedwell WL, Wildman JL, DiazGranadoz D, et al. Collaboration at work: an integrative multilevel conceptualization. Human Resource Management Review. 2012;22:128–45. [Google Scholar]
- Belaid L, Ridde V. An implementation evaluation of a policy aiming to improve financial access to maternal health care in Djibo district, Burkina Faso. BMC Pregnancy and Childbirth. 2012;12:143. doi: 10.1186/1471-2393-12-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Ameur A, Ridde V, Bado AR, Ingabire MG, Queuille L. User fee exemptions and excessive household spending for normal delivery in Burkina Faso: the need for careful implementation. BMC Health Services Research. 2012;12:412. doi: 10.1186/1472-6963-12-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll C, Patterson M, Wood S, et al. A conceptual framework for implementation fidelity. Implementation Science. 2007;2:40. doi: 10.1186/1748-5908-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen HT. Thousand Oaks: CA Sage; 2005. Practical program evaluation: assess and improve program planning implementation and effectiveness. [Google Scholar]
- D’Ambruoso L, Abbey M, Hussein J. Please understand when I cry out in pain: women’s accounts of maternity services during labour and delivery in Ghana. BMC Public Health. 2005;5:140. doi: 10.1186/1471-2458-5-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diarra A. Mise en oeuvre locale de l’exemption des paiements des soins au Niger: évaluation dans les districts sanitaires. Afrique Contemporaine. 2012;3:77–93. [Google Scholar]
- Dogba M, Fournier P, Berthe-Cisse S. Qualification of staff, organization of services, and management of pregnant women in rural settings: the case of Diema and Kayes districts (Mali) ISRN Obstetrics and Gynecology. 2012;8:649412. doi: 10.5402/2012/649412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzakpasu S, Powell-Jackson T, Campbell OMR. Impact of user fees on maternal health service utilization and related health outcomes: a systematic review. Health Policy and Planning. 2013;10 doi: 10.1093/heapol/czs142. 1093/heapol/czs142. [DOI] [PubMed] [Google Scholar]
- Ejembi CL, Norick P, Starrs A, Thapa K. New global guidance supports community and lay health workers in postpartum hemorrhage prevention. International Journal of Gynecology and Obstetrics. 2013;122:187–9. doi: 10.1016/j.ijgo.2013.05.001. [DOI] [PubMed] [Google Scholar]
- Emerson RM, Fretz RI, Shaw LL. Writing Ethnographic Fieldnotes. 2nd. Chicago: University of Chicago Press; 2011. [Google Scholar]
- Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy and Planning. 2004;19:69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- Gabrysch S, Campbell OMR. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth. 2009;9:34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage AJ. Barriers to the utilization of maternal health care in rural Mali. Social Science and Medicine. 2007;65:1666–82. doi: 10.1016/j.socscimed.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Gilson L. Trust and the development of health care as a social institution. Social Science and Medicine. 2003;56:1453–68. doi: 10.1016/s0277-9536(02)00142-9. [DOI] [PubMed] [Google Scholar]
- Gilson L, Hanson K, Sheikh K, et al. Building the field of health policy and systems research: social science matters. PLoS Medicine. 2011;8:e1001079. doi: 10.1371/journal.pmed.1001079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson L, Palmer N, Schneider H. Trust and health worker performance: exploring a conceptual framework using South African evidence. Social Science and Medicine. 2005;61:1418–29. doi: 10.1016/j.socscimed.2004.11.062. [DOI] [PubMed] [Google Scholar]
- Haddad S, Bicaba A, Feletto M, et al. System-level determinants of immunization coverage disparities among health districts in Burkina Faso: a multiple case study. BMC International Health and Human Rights. 2009;9(Suppl. 1):S15. doi: 10.1186/1472-698X-9-S1-S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad S, Fournier P. Quality, cost and utilization of health services in developing countries: a longitudinal study in Zaïre. Social Science and Medicine. 1995;40:743–53. doi: 10.1016/0277-9536(94)00134-f. [DOI] [PubMed] [Google Scholar]
- Haddad S, Fournier P, Machouf N, Yatara F. What does quality mean to lay people? Community perceptions of primary health care services in Guinea. Social Science and Medicine. 1998;47:381–94. doi: 10.1016/s0277-9536(98)00075-6. [DOI] [PubMed] [Google Scholar]
- Hercot D, Meessen B, Ridde V, Gilson L. Removing user fees for health services in low-income countries: a multi-country review framework for assessing the process of policy change. Health Policy and Planning. 2011;26(Suppl. 2):ii5–15. doi: 10.1093/heapol/czr063. [DOI] [PubMed] [Google Scholar]
- Hounton S, Chapman G, Menten J, et al. Accessibility and utilisation of delivery care within a Skilled Care Initiative in rural Burkina Faso. Tropical Medicine & International Health. 2008;13(Suppl. 1):44–52. doi: 10.1111/j.1365-3156.2008.02086.x. [DOI] [PubMed] [Google Scholar]
- INSD. Enquête démographique et de santé et à indicateurs multiples (EDSBF-MICS IV) 2010 [Demographic and Health Survey with Multiple Indicators] 2012. Ouagadougou: Government of Burkina Faso, Institut national de la statistique et de la démographie (INSD)/Ministère de l’économie et des finances. [Google Scholar]
- Jewkes R, Abrahams N, Mvo Z. Why do nurses abuse patients? Reflections from South African obstetric services. Social Science and Medicine. 1998;47:1781–95. doi: 10.1016/s0277-9536(98)00240-8. [DOI] [PubMed] [Google Scholar]
- Kyomuhendo GB. Low use of rural maternity dervices in Uganda: impact of women's status, traditional beliefs and limited resources. Reproductive Health Matters. 2003;11:16–26. doi: 10.1016/s0968-8080(03)02176-1. [DOI] [PubMed] [Google Scholar]
- Lagarde M, Barroy H, Palmer N. Assessing the effects of removing user fees in Zambia and Niger. Journal of Health Services Research & Policy. 2012;17:30–6. doi: 10.1258/jhsrp.2011.010166. [DOI] [PubMed] [Google Scholar]
- Lagarde M, Palmera N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bulletin of the World Health Organization. 2008;86:839–48. doi: 10.2471/BLT.07.049197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meda ZC, Konate L, Ouedraogo H, et al. Leadership et vision exercée pour la couverture universelle des soins dans les pays à faible revenu. Santé. 2011;21:178–84. doi: 10.1684/san.2011.0268. [DOI] [PubMed] [Google Scholar]
- Meessen B, Gilson L, Tibouti A. User fee removal in low-income countries: sharing knowledge to support managed implementation. Health Policy and Planning. 2011;26(Suppl. 2):ii1–4. doi: 10.1093/heapol/czr071. [DOI] [PubMed] [Google Scholar]
- Miles M, Huberman M. Qualitative Data Analysis. 2nd. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Ministry of Health. Stratégie nationale de la subvention des accouchements et des soins obstétricaux et néonataux d'urgence au Burkina Faso [National Subsidy for Childbirth and Emergency Obstetric and Neonatal Services in Burkina Faso] 2006. Ouagadougou: Government of Burkina Faso. [Google Scholar]
- Ministry of Health. Guide d’orientation pour la mise en oeuvre du nouveau rôle des accoucheuses villageoises [Guidelines for the Implementation of the New Role of Traditional Midwives] 2007. Ouagadougou: Government of Burkina Faso. [Google Scholar]
- Ministry of Health. Annuaire statistique 2011 [Annual Statistical Report] 2012. Ouagadougou: Government of Burkina Faso. [Google Scholar]
- Mookherji S, LaFond A. Strategies to maximize generalization from multiple case studies: lessons from the Africa Routine Immunization System Essentials (ARISE) project. Evaluation. 2013;19:284–303. [Google Scholar]
- Mrisho M, Schellenberg JA, Mushi A, et al. Factors affecting home delivery in rural Tanzania. Tropical Medicine & International Health. 2007;12:862–72. doi: 10.1111/j.1365-3156.2007.01855.x. [DOI] [PubMed] [Google Scholar]
- Nabyonga J, Desmet M, Karamagi H, et al. Abolition of cost sharing is pro-poor: evidence from Uganda. Health Policy and Planning. 2005;20:101–8. doi: 10.1093/heapol/czi012. [DOI] [PubMed] [Google Scholar]
- OMS. Geneva: 2013. Statistiques annuaires mondiales. [Google Scholar]
- Penfold S, Harrison E, Bell J, Fitzmaurice A. Evaluation of the delivery fee exemption policy in Ghana: population estimates of changes in delivery service utilization in two regions. Ghana Medical Journal. 2007;41:100–9. [PMC free article] [PubMed] [Google Scholar]
- Poupart J, Deslauriers J-P, Groulx L-H, et al. La recherche qualitative. Enjeux épistémologiques et méthodologiques. Montreal: Gaëtan Morin; 1997. [Google Scholar]
- Ridde V, Kouanda S, Yameogo M, Kadio K, Bado A. Why do women pay more than they should? A mixed methods study of the implementation gap in a policy to subsidize the costs of deliveries in Burkina Faso. Evaluation and Program Planning. 2013;36:145–52. doi: 10.1016/j.evalprogplan.2012.09.005. [DOI] [PubMed] [Google Scholar]
- Ridde V, Morestin F. A scoping review of the literature on the abolition of user fees in health care services in Africa. Health Policy and Planning. 2011;26:1–11. doi: 10.1093/heapol/czq021. [DOI] [PubMed] [Google Scholar]
- Ridde V, Richard F, Bicaba A, Queuille L, Conombo G. The national subsidy for deliveries and emergency obstetric care in Burkina Faso. Health Policy and Planning. 2011;26(Suppl. 2):ii30–40. doi: 10.1093/heapol/czr060. [DOI] [PubMed] [Google Scholar]
- Ronsmans C, Graham WJ. Maternal mortality: who, when, where, and why. Lancet. 2006;368:1189–200. doi: 10.1016/S0140-6736(06)69380-X. [DOI] [PubMed] [Google Scholar]
- Sherratt DR. Strengthening health systems by focusing on community midwifery. Revue Humanitaire. 2013;35:68–79. [Google Scholar]
- Shiferaw S, Spigt M, Godefrooij M, Melkamu Y, Tekie M. Why do women prefer home births in Ethiopia? BMC Pregnancy and Childbirth. 2013;13:5. doi: 10.1186/1471-2393-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Some TD, Sombie I, Meda N. Women’s perceptions of homebirths in two rural medical districts in Burkina Faso: a qualitative study. Reproductive Health. 2011;8:3. doi: 10.1186/1742-4755-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stekelenburg J, Kyanamina S, Mukelabai M, Wolffers I, van Roosmalen J. Waiting too long: low use of maternal health services in Kalabo, Zambia. Tropical Medicine & International Health. 2004;9:390–8. doi: 10.1111/j.1365-3156.2004.01202.x. [DOI] [PubMed] [Google Scholar]
- Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Social Science and Medicine. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- Van der Maren J-M. Méthodes de recherche pour l'éducation. 2nd. Montreal: Presses de l’Université de Montreal; 1996. [Google Scholar]
- Victora CG, Schellenburg JA, Huicho L, et al. Context matters: interpreting impact findings in child survival evaluations. Health Policy and Planning. 2005;20(Suppl. 1):i18–31. doi: 10.1093/heapol/czi050. [DOI] [PubMed] [Google Scholar]
- Walker L, Gilson L. “We are bitter but we are satisfied”: Nurses as street-level bureaucrats in South Africa. Social Science and Medicine. 2004;59:1251–61. doi: 10.1016/j.socscimed.2003.12.020. [DOI] [PubMed] [Google Scholar]
- Wild K, Barclay L, Kelly P, Martins N. Birth choices in Timor-Leste: a framework for understanding the use of maternal health services in low resource settings. Social Science and Medicine. 2010;71:2038–45. doi: 10.1016/j.socscimed.2010.09.012. [DOI] [PubMed] [Google Scholar]
- Wilkinson D, Gows E, Sach M, Karim SS. Effect of removing user fees on attendance for curative and preventive primary health care services in rural South Africa. Bulletin of the World Health Organization. 2001;79:665–71. [PMC free article] [PubMed] [Google Scholar]
- Witter S, Arhinful DK, Kusi A, Zakariah-Akoto S. The experience of Ghana in implementing a user fee exemption policy to provide free delivery care. Reproductive Health Matters. 2007;15:61–71. doi: 10.1016/S0968-8080(07)30325-X. [DOI] [PubMed] [Google Scholar]
- Witter S, Dieng T, Mbengue D, Moreira I, De Brouwere V. The national free delivery and caesarean policy in Senegal: evaluating process and outcomes. Health Policy and Planning. 2010;25:384–92. doi: 10.1093/heapol/czq013. [DOI] [PubMed] [Google Scholar]
- Wong CA, Cummings GG. The relationship between nursing leadership and patient outcomes: a systematic review. Journal of Nursing Management. 2007;15:508–21. doi: 10.1111/j.1365-2834.2007.00723.x. [DOI] [PubMed] [Google Scholar]
- Yin RK. Validity and generalization in future case study evaluations. Evaluation. 2013a;19:321–32. [Google Scholar]
- Yin RK. Case Study Research: Design and Methods. 5th. Thousand Oaks, CA: Sage Publications; 2013b. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.