Abstract
Introduction
Spinal hydatid cyst is a rare, but serious condition.
Presentation of the case
Herein, we present a 17-year-old male patient with back pain radiating to the legs and progressive weakness in the lower limbs. CT and MRI showed a spinal-paraspinal hydatid cyst with a dumbbell appearance that caused neural foraminal widening and spinal cord compression. The case was explored via right T3-T4 hemilaminectomy, and the hydatid cyst was completely removed.
Discussion
The clinical presentation, diagnosis, and surgical treatment of this rare case of spinal hydatid disease are discussed, and all published cases of primary dumbbell hydatid cyst are reviewed.
Conclusion
Even if serological test results are negative, hydatid cysts should be considered in the differential diagnosis of cystic lesions of the spine.
Keywords: Echinococcosis, Hydatid cyst, Surgical treatment, Thoracic spine
1. Introduction
Hydatid cyst disease is caused by Echinococcus granulosus infection [1,2]. Transmission of the pathogen to humans occurs via ingestion of food infected with the parasite’s eggs. The liver and lungs are the most frequent locations of E. granulosus infection [1,2,6,22], whereas 0.5–2.0% of all cases occur in the musculoskeletal system, of which 50% of cases are spinal hydatid cyst [2,4,14,17,26].
The appearance of a dumbbell-shaped mass in the thoracic spine is highly suggestive of neurofibroma. Hydatid cysts, although very rare, can have a similar appearance [2,11,13,26]. Hydatid cysts of the bone and muscle are always primary, and neurologic recovery is possible because they are slow-growing lesions. Herein we present a 17-year-old male patient with a spinal-paraspinal hydatid cyst with a dumbbell apperence that caused neural foraminal widening and spinal cord compression. The patient was treated successfully via total surgical excision; no further medical treatment was required. The case’s clinical symptoms and differential diagnosis are discussed, and the relevant literature is reviewed.
2. Case report
A 17-year-old male presented with a 2-month history of back pain radiating to the legs, progressive weakness in the lower limbs, and difficulty walking. Physical examination findings were normal. Neurological examination showed paraparesis, which was prominent on the left side. The patient also had urinary and fecal incontinence.
There are no specific laboratory signs of hydatid disease. The patient had a negative history of surgery for hydatid cysts. Abdominal ultrasonography, and MRI of the cranium and cervical region were normal. CT showed cystic lesions originating from the vertebral body and erosive widening of left T3-T4 neural foramen, which produced a dumbbell appearance because there were intraspinal and paraspinal components. The lesion was hypointense on T1-weighted MRI and hyperintense on T2-weighted MRI (Fig. 1a and b). Sagittal MRI showed epidural region extension of the lesion, which was compressing the dura and spinal cord. Initially, the lesion was considered a hydatid cyst, but serological testing (specific ELISA/Western blot) proved negative. The cyst was surgically exposed via left T3 hemilaminectomy and T3-T4 partial facetectomy, dissected from the spinal dura, nerve root, surrounding bone, and paraspinal space, and completely removed (Fig. 2). The exposure showed an encapsulated destructive lesion arising from the T3-T4 neural foramen. The area was irrigated with hydrogen peroxide. Histopathological examination confirmed the diagnosis of hydatid cyst.
Fig. 1.
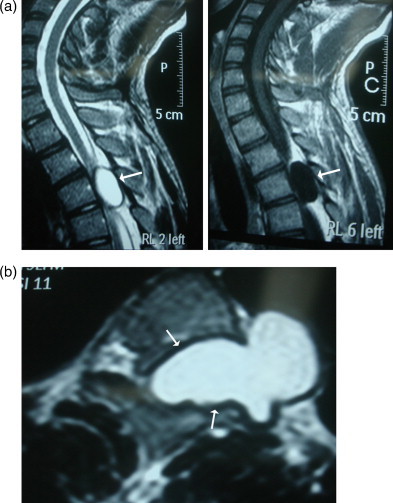
(a) The cystic lesion (white arrows) is seen as hypointense in T1-weighted and hyperintense in T2-weighted sagittal MRI at the T3 and T4 levels. (b) The cystic lesion (white arrows) is seen as hyperintense in T2-weighted axial MRI at the T3 and T4 levels.
Fig. 2.

The hydatid cyst was dissected from the spinal dura, nerve root, surrounding bone, and paraspinal space, and completely removed.
Follow-up examination 5 months post surgery showed that the patient’s paraparesis resolved almost completely and postoperative MRI showed that the hydatid cyst had been completely removed (Fig. 3). The patient was completely recovered 6 months post surgery.
Fig. 3.

T2-weighted sagittal MRI shows that the hydatid cyst was completely removed (white arrows).
3. Discussion
Hydatid disease is a zoonosis produced by the larval stage of E. granulosus and Echinococcus multilocularis, and occurs worldwide [1,2,4,6,10,12,18,20]. E. granulosus manifests as the common hydatid form and E. multilocularis manifests as the rare alveolar form. The former is the more benign form and is characterised by cyst formation, whereas the latter is not encapsulated and presents as a ramifying, porous, and necrotic mass. The prognosis for the alveolar form is extremely poor, with an almost 100% mortality rate [5,7,10]. Their gradual invasion of adjacent tissue is tumor-like and sections of parasite may metastasize to distal parts of body. Initial imaging studies are usually highly suspicious for carcinoma or sarcoma [6,7,10].
In humans hydatid disease involves the liver in approximately 75% of cases, the lungs in 15%, and other anatomic locations in 10%. The frequency of osseous involvement in hydatid disease is 0.5–4% [18,20,24,26]. It most commonly occurs in the spine (50%) and pelvis [4,5,7,18]. In the presented case the lesion extended to the paraspinal and intraspinal space. Spinal hydatid cysts are usually situated in the dorsal region and generate medullary or radicular symptoms, according to their location [2,6,12,15,16,20]. In the present case the hydatid cyst was extradural and located in the dorsal region, with paraspinal extension. To the best of our knowledge widening of the spinal neural foramen caused by hydatid cyst has been reported only one case [17]. Parvaresh et al. [17]. reported a dumbbell hydatid cyst of the spine, but in their case spinal involvement of hydatid disease was considered secondary, because the primary lesion was located in the liver, whereas in the presented case spinal involvement was primary.
Primary hydatid infestation of the spine without any other systemic involvement can be explained by the direct porto-vertebral venous shunt theory, as follows: in rare instances the disease begins in the extradural area, suggesting that the parasite’s embryo is possibly being transported through the porto-vertebral venous shunts [6,9,10]. Braithwaite and Lees classified spinal hydatid cysts into 5 radiological types: intramedullary, intradural-extramedullary, extradural, hydatid cyst of vertebrae, and paravertebral lesions extending to spinal structures [6]. The last 2 types affect the spinal neural structures via extension and these are more common, but the first 3 types are primary and extremely rare. Based on the presented case, we think that hydatid cysts can pass through the neural foramen to produce a dumbbell-shaped lesion. CT and MRI findings in the presented case were typical for hydatid cyst, which facilitated exclusion of the aforementioned lesions from the differential diagnosis.
All known published cases of primary spinal extradural hydatid cysts are presented in Table 1; in total, there are only 13 cases, including the presented case [2,10,13,26]. In case reports prior to the advent of CT and MRI the possibility of the existence of a single extradural hydatid cyst or of soft tissue involvement without bony origin was viewed with skepticism [12,15,19,23,25,26]. Preoperative diagnosis of the lesion informs the choice of surgical method; as such, the natural history of the disease, and serological and radiological studies are used for diagnosis. The Casoni-Weinberg test alone is not completely reliable for diagnosis. Specific ELISA/Western blot serological tests have a sensitivity of 80–100% and specificity of 88–96% for liver hydatid disease, versus 50–56% sensitivity for lung disease and 25–56% for other organs, which explains why serological findings in the presented case were negative. Direct roentgenogram, CT, and MRI are useful tools for diagnosing vertebral hydatid cases. CT and MRI show the anatomical position of the lesion, the osseous portion of the lesion, extension, and neuronal involvement. MRI is the best tool for determining if the disease is multicystic, as in the presented case. In the differential diagnosis, especially if the hydatid cyst is unilocular and complicated, lytic metastatic tumors and metastatic bone neoplasms must be considered. Furthermore, the natural history of the disease, serological test results, and CT and MRI findings must be thoroughly evaluated.
Table 1.
Details of all published cases of primary spinal extradural hydatid cyst (CT, MRI, and ultrasonography).
| No of patients |
Age (years) |
Gender | Location | Serology | Neurological status | Imaging | Treatment | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| Pluchino and Lodrini (1981) [17] | 1 | 56 | Male | T10-L2 | Casoni (–) | Paraparesis | Myelography | Posterior | Complete recovery |
| Wani et al. recovery (1989) [22] |
1 | 14 | Male | T9-10 | Paraparesis | Myelography | Surgery | Complete recovery | |
| Kars et al. (1990) [10] | 1 | 40 | Male | C5-6 | Casoni (–) | Tetraparesis | CT, USG | Posterior | |
| Bavbek et al. (1992) [3] | 1 | 40 | Male | T5-9 | Normal | MRI | Posterior | Normal | |
| Tekkök and Benli (1993) [20] | 1 | 54 | Male | L2-5 | Cauda equina syndrome | CT,MRI | Posterior | No change | |
| Baysefer recovery (1996) [2] |
1 | 21 | Male | T5-6 | Paraparesis | Myelography | Posterior | Complete | |
| Pandey and Chaudhari (1997) [14] | 1 | 15 | Male | S1-2 | Cauda equina syndrome | MRI | Posterior | Improved | |
| Bayar et al. (1997) [1] | 1 | 30 | Female | L5-S1 | S1 radicular findings | MRI | Posterior | Improved | |
| Berk et al. (1998) [4] | 1 | 17 | Male | T7-9 | Paraparesis | CT,MRI | Posterior | ||
| Bouklata et al. (2000) [5] | 1 | 8 | Male | T8-11 | Paraparesis | MRI | Posterior | ||
| Karadereler (2002) [9] | 1 | 8 | Male | L2-5 | ELISA (–) | Cauda equina syndrome | MRI | Posterior |
Radiological diagnosis and determination of hydatid cyst extension are usually provided via MRI [14,18,19,23,24]. Hydatid cysts do not have a solid component and have a tendency to invade anatomical cavities. Additionally, they do not show contrast enhancement, but exhibit a cerebral spinal fluid-like signal intensity on MRI. The final diagnosis is made, as in the presented case, via surgical exploration.
4. Conclusion
Treatment of hydatid cysts is primarily surgical, demanding complete removal without rupture. Based on the clinical and neuroradiological findings reported herein, even if serological test results are negative, hydatid cysts should be considered in the differential diagnosis of cystic lesions of the spine.
Conflicts of interest
None.
Sources of funding
None.
Consent
None.
Author’s contribution
Ahmet Karakasli, M.D. : collecting data.
Murat Yilmaz, M.D. : writing the paper.
Ali Osman Mucuoglu : collecting data.
Alaattin Yurt, M.D. : editing and design.
Acknowledgments
None.
References
- 1.Assefa G., Abebe M., Belete A., Schnider J. Epidural and para spinal thoracic hydatidosis presenting with progressive paraparesis and paraplegia: a case report. Ethiop. Med. J. 2014;52(January (1)):49–51. [PubMed] [Google Scholar]
- 2.Bayar M.A., Erdem Y., Habip N. Primary intraspinal extradural hydatid disease causing radicular compression. Turk. Neurosurg. 1997;7:33–35. [Google Scholar]
- 3.Baysefer A., Gonul E., Canakci Z., Erdogan E., Aydogan N., Kayali H. Hydatid disease of the spine. Spinal Cord. 1996;34:297–300. doi: 10.1038/sc.1996.54. [DOI] [PubMed] [Google Scholar]
- 4.Berk C., Ciftci E., Erdogan A. MRI in primary intraspinal extradural hydatid disease: case report. Neuroradiology. 1998;40:390–392. doi: 10.1007/s002340050608. [DOI] [PubMed] [Google Scholar]
- 5.Bouklata S., El Mahi M., Karmouni W., El Hassani M.R., Chakir N., Jiddane M., Boukhrissi N. Isolated dorsal extradural hydatid cyst. a case report. J. Neuroradiol. 2000;27:285–286. [PubMed] [Google Scholar]
- 6.Braithwaite P.A., Lees R.F. Vertebral hydatid disease: radiological assessment. Radiology. 1981;140:763–766. doi: 10.1148/radiology.140.3.7280247. [DOI] [PubMed] [Google Scholar]
- 7.Charles R.W., Govender S., Naidoo K.S. Echinococcal infection of the spine with neural involvement. Spine. 1988;13:47–49. doi: 10.1097/00007632-198801000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Joshi K.C., Jagannath A.T., Varma R.G. Dumbbell shaped spinal hydatidosis. Neurol. India. 2014;62(January–February (1)):113–114. doi: 10.4103/0028-3886.128363. [DOI] [PubMed] [Google Scholar]
- 10.Karadereler S., Orakdögen M., Kılıç K., Özdoğan C. Primary spinal extradural hydatid cyst in a child: case report and review of the literature. Eur. Spine. 2002;11:500–503. doi: 10.1007/s00586-002-0411-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kars H.Z., Hekimoglu B., Cepoglu C. Spinal epidural hydatid cyst: radiological and ultrasonographical workup of a case. Eur. J. Radiol. 1990;11:212–214. doi: 10.1016/0720-048x(90)90059-k. [DOI] [PubMed] [Google Scholar]
- 12.Lakhdar F., Arkha Y., Rifi L., Derraz S., El Ouahabi A., El Khamlichi A. Spinal intradural extramedullary hydatidosis: report of three cases. Neurosurgery. 2009;65(August (2)):372–376. doi: 10.1227/01.NEU.0000349751.39742.E3. discussion 376–7. [DOI] [PubMed] [Google Scholar]
- 13.McCormick P.C. Surgical management of dumbbell and para-spinal tumours of the thoracic and lumbar spine. Neurosurgery. 1996;38:67. doi: 10.1097/00006123-199601000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Maiuri F., Laconnetta G., Benvenuti D., Rendano F., Sera L.L. Hydatid cyst of the lumbosacral spine with large pelvic mass. Acta Neurol. (Napoli) 1993;15:215–221. [PubMed] [Google Scholar]
- 15.Pamir N., Akalan N., Ozygen T. Spinal hydatid cysts. Surg. Neurol. 1984;21:53–57. [PubMed] [Google Scholar]
- 16.Pandey M., Chaudhari M.P. Primary hydatid cyst of sacral spinal canal: case report. Neurosurgery. 1997;40:407–409. doi: 10.1097/00006123-199702000-00040. [DOI] [PubMed] [Google Scholar]
- 17.Parvaresh M., Moin H., Miles J.B. Dumbbell hydatid cyst of the spine. Br. J. Neurosurg. 1996;10:211–213. doi: 10.1080/02688699650040403. [DOI] [PubMed] [Google Scholar]
- 18.Pedrosa I., Saiz A., Arrazola J., Ferreiros J., Pedrosa C.S. Hydatid disease: radiologic and pathologic features and complication. RadioGraphics. 2000;20:795–817. doi: 10.1148/radiographics.20.3.g00ma06795. [DOI] [PubMed] [Google Scholar]
- 19.Pluchino F., Lodrini S. Multiple primitive epidural spinal hydatid cysts. Acta Neurochir. 1981;59:257–262. doi: 10.1007/BF01406356. [DOI] [PubMed] [Google Scholar]
- 20.Ranganadham P., Dinkar I., Sundaram C., Ratnakar K.S., Vive Kanada T. Posterior mediastinal paravertebral hydatid cyst presented as spinal compresion: a case report. Clin. Neurosurg. 1990;92:149–151. doi: 10.1016/0303-8467(90)90091-i. [DOI] [PubMed] [Google Scholar]
- 22.Scarlata F., Giordano S., Saporito L., Marasa L., Li Pani G., Odierna A., Scaglione V., Di Carlo P., Romano A. Cystic hydatidosis: a rare case of spine localization. Infez. Med. 2011 Mar;19(1):39–41. [PubMed] [Google Scholar]
- 23.Teekkök I.H., Benli K. Primary spinal extradural hydatid disease: report of a case with magnetic resonance characteristics and pathological correlation. Neurosurgery. 1993;33:320–3233. [PubMed] [Google Scholar]
- 24.Tsitouridis I., Dimitraidis A.S. CT and MRI in vertebral hydatid disease. Eur. Radiol. 1997;7:1207–1210. doi: 10.1007/s003300050275. [DOI] [PubMed] [Google Scholar]
- 25.Wani M.A., Taheri S.A., Babu M.L., Ahangar G.A., Wani H. Primary spinal extradural hydatid cyst. Neurosurgery. 1989;24:631–632. doi: 10.1227/00006123-198904000-00026. [DOI] [PubMed] [Google Scholar]
- 26.Zibis A.H., Markonis A., Karantanas A.H. Unusual cause of spinal foramninal widening. Eur. Radiol. 2000;10:144–148. doi: 10.1007/s003300050022. [DOI] [PubMed] [Google Scholar]


