Highlights
-
•
Brachial artery injuries after closed shoulder dislocations are uncommon.
-
•
A high index of suspicion should be maintained in order to make the diagnosis early.
-
•
Exploration with excision of the injured segment and reverse vein interposition grafting is the treatment of choice in these cases.
Keywords: Vascular, Trauma, Fracture, Dislocation
Abstract
Introduction
Brachial artery injuries from elbow dislocations are uncommon, but they may lead to disastrous consequences if the diagnosis is delayed.
Presentation of case
We report a case of a patient who sustained a fall onto the elbow, with dislocation and brachial artery injury, despite an ipsilateral radial pulse being palpable.
Discussion
Clinicians should maintain a high index of suspicion for brachial injury when patients present with a fall onto the elbow coupled with signs suggestive of fracture-dislocation, nerve injury and/or signs of limb ischemia. Frank ischamia, however, is uncommon as there is a rich collateral anastomosis in the upper limb.
Conclusion
A high index of suspicion should be maintained in order to make the diagnosis early. Exploration with excision of the injured segment and reverse vein interposition grafting is the treatment of choice in these cases.
1. Introduction
Compared to penetrating trauma, brachial artery injuries after closed elbow dislocations are uncommon. Only few case reports [1–7] and small case series [8–12] exist in the medical literature, with the largest series reporting on 12 brachial artery injuries [12]. Although there has been a rise in the incidence of traumatic vascular injuries in the Caribbean over the past three decades [13–18], there has been no report of brachial artery injuries from elbow dislocations in the regional literature. We report the clinical features in a patient who sustained this injury.
2. Presentation of case
An intoxicated 23-year old man fell off the tray of a truck approximately 6 ft to the pavement. He landed onto the left elbow and immediately began to experience severe pain and swelling at the site. Upon clinical evaluation, the left elbow was tender and swollen. There was subtle deformity at the joint and the skin over the antecubital fossa was tense and contused. The brachial pulse could not be appreciated but there was a palpable ipsilateral radial pulse that was lower in volume compared to the contralateral limb. No motor or sensory deficits were present. A diagnosis of dislocation with spontaneous reduction of the left elbow was made and a suspicion of vascular injury was entertained. Duplex doppler revealed the presence of triphasic flow in the brachial artery up to the level of the elbow joint with no flow distal to the elbow. Therefore, the patient was prepared for general anaesthesia and taken emergently to the operating theatre.
The elbow was explored using a curvilinear incision across the joint. The common flexor origin was disrupted and there was a large haematoma at this point with significant soft tissue contusion and oedema (Fig 1). A 5 cm segment of the brachial artery was contused and there was a significant reduction in arterial pulsations in the artery beyond this point (Fig 1). There was also a 5 cm segment of contusion in the ulnar recurrent artery.
Fig. 1.
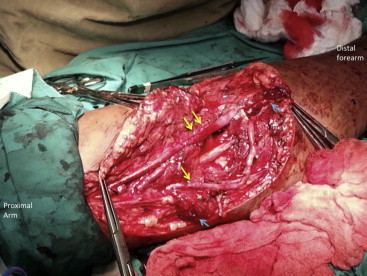
Open exploration of the injured elbow joint. Double yellow arrows demonstrate a segment of contused brachial artery. Single yellow arrows demonstrate the contused segment of the ulnar collateral artery; Blue arrows demonstrate the disrupted ends of the common flexor origin with markedly oedematous and contused remnant tissues.
The ipsilateral great saphenous vein was harvested for use as an interposition graft. Both arteries were repaired using the vein interposition graft with end-to-end anastomoses using 6/0 polypropylene sutures. The decision was made to address the ulnar recurrent artery since it was accessible in the operative wound, obviously injured and technically easy to repair. Post repair, good volume pulses were appreciated at the radial and ulnar arteries in the distal limb. The disrupted muscle at the common flexor origin was approximated without tension using 1/0 vicryl sutures. After revascularization, closed fasciotomies were performed at the ipsilateral forearm and the joint was immobilized with an external fixator (Fig 2).
Fig. 2.

Application of an external fixator to the reduced elbow joint.
Post-fixation radiographs were acceptable (Fig 3). The post-operative recovery was uneventful and the patient was discharged on clopidogrel for one year. At his follow up clinic visits at one year, the limb was viable, there were normal pulses appreciated in the limb and there were no restrictions in movement.
Fig. 3.

Lateral and antero–posterior radiographs of the elbow joint post reduction and stabilization.
3. Discussion
Over the past three decades, there has been a surge in the incidence of penetrating vascular injuries in Trinidad and Tobago [17,18] and across the wider Caribbean [13–16]. These injuries may lead to limb loss [9], especially when the diagnosis is missed and there is a delay to restore perfusion.
As in our case, brachial artery injuries commonly result from a fall on the outstretched hand [19–20] that results in anterior elbow dislocation [21]. They tend to occur in children [4,6,9,12], although the diagnosis should not be discounted in adults [21–22]. Clinicians should maintain a high index of suspicion for brachial injury when patients present with blunt trauma from a fall onto the elbow coupled with signs suggestive of fracture-dislocation (painful swelling, bruising, loss of contour, and decreased range of motion) and signs of limb ischemia [21].
Unfortunately, the diagnosis is often missed because the injuries are uncommon. The annual incidence of brachial artery injuries after closed elbow injuries has been reported to range from 0.47% [23] to 0.5% [24]. Additionally, the signs of ischaemia are usually attenuated since there is rich collateral flow in the upper limb through the profunda brachii, ulnar and radial collateral arteries [21]. This explains why Brahmamdam et al. [12] described these upper limbs as “pink pulseless hands”. Instead of frank ischaemia, these patients have subtle signs such as palpable but reduced pulses, decreased capillary refill and reduced pulse oximetry readings [10–12,21,22]. This was similar to a previously reported case by Guler et al. [21] where there was normal capillary refill and radial artery pulsation in a patient with total disruption of the brachial artery from a closed elbow dislocation. These cases emphasize the need to maintain a high index of suspicion because only subtle signs of ischaemia may be present due to continued perfusion from upper limb collaterals.
When Frank ischaemia is present, emergent operative intervention is indicated. Even in cases where limb viability is not immediately threatened, a delay in restoring full perfusion may lead to long-term complications of limb ischaemia such as cold intolerance, reduced range of motion, and Volkmann’s contracture [10,12]. Therefore, most authorities recommend mandatory operative exploration for these injuries [4–6,8,10,12].
Arteriography is recommended to confirm and localize the injury in order to plan the operative intervention [8]. However, this may not be readily available under emergent conditions, especially in developing Caribbean countries. Despite being user dependent, duplex doppler ultrasound offers a reasonable alternative [25] since, it is readily available and rapidly completed. Otherwise, on the table angiography offers another reasonable alternative [25].
The commonest pathologic lesions encountered at operation are arterial obstruction from thrombosis or intimal flaps at the injury site [9,12] or complete arterial transection [9]. In these cases, the ideal treatment is to excise the injured segment and use the great saphenous vein [4,6] or an arm vein [5] as an interposition graft to restore flow. This was done in the index patient with good outcomes.
Surgeons must be vigilant for nerve injuries that are frequently associated with posterior elbow dislocations [26]. Compartment syndrome after closed elbow trauma with brachial artery injury is uncommon [27,28], but can occur. Therefore, small-incision fasciotomies were performed prophylactically in this case. This provides a good balance between compartment decompression and wound complications [29] since, up to 12.5% of incisions will require vacuum therapy and/or skin grafting after open fasciotomy [30].
4. Conclusion
Brachial artery injuries after closed shoulder dislocations are uncommon. A high index of suspicion should be maintained in order to make the diagnosis early. Exploration with excision of the injured segment and reverse vein interposition grafting is the treatment of choice in these cases.
Conflict of interest
There are no conflicts of interests declared for any of the authors.
Funding
No funding was received for this work.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
SC conceptualized and wrote the manuscript. PH collected data, performed data collection and approved intellectual content. SB wrote the manuscript and approved intellectual content. DH performed data collection and approved intellectual content.
Acknowledgements
None declared. No funding was received for this work.
References
- 1.Martin D.J., Fazzi U.G., Leach W.J. Brachial artery transection associated with closed and open dislocation of the elbow. Eur. J. Emerg. Med. 2005;12(1):30–32. doi: 10.1097/00063110-200502000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Micic I., Kim S.Y., Park I.H., Kim P.T., Jeon I.H. Surgical management of unstable elbow dislocation without intra-articular fracture. Int. Orthop. 2009;33(4):1141–1147. doi: 10.1007/s00264-008-0624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reynders P., Broos P., Stoffelen D. Brachial artery injury in closed posterior elbow dislocation case report. J. Bone Joint Surg. Br. 2004;86(7):1050–1058. [PubMed] [Google Scholar]
- 4.Manouel M., Minkowitz B., Shimotsu G., Haq I., Feliccia J. Brachial artery laceration with closed posterior elbow dislocation in an eight year old. Clin. Orthop. Relat. Res. 1993;296:109–112. [PubMed] [Google Scholar]
- 5.Slowik G.M., Fitzimmons M., Rayhack J.M. Closed elbow dislocation and brachial artery damage. J. Orthop. Trauma. 1993;7(6):558–561. doi: 10.1097/00005131-199312000-00012. [DOI] [PubMed] [Google Scholar]
- 6.D'Ambrosia R., Zink W. Fractures of the elbow in children. Pediatr. Ann. 1982;11(6):541–548. doi: 10.3928/0090-4481-19820601-12. [DOI] [PubMed] [Google Scholar]
- 7.Friedmann E. Simple rupture of the brachial artery, sustained in elbow dislocation. J. Am. Med Assoc. 1961;22(177):208–209.. doi: 10.1001/jama.1961.73040290015013. [DOI] [PubMed] [Google Scholar]
- 8.Hennig K., Franke D. Arterial involvement in elbow-proximal injuries. Chirurg. 1978;49(9):580–584. [PubMed] [Google Scholar]
- 9.Snyder A., Crick J.C. Brachial artery injuries in children. J. Surg. Orthop. Adv. 2013;22(2):105–112. doi: 10.3113/jsoa.2013.0105. [DOI] [PubMed] [Google Scholar]
- 10.Kelsch G., Savvidis E., Jenal G., Parsch K. Concomitant vascular complications in supracondylar humerus fractures in children. Unfallchirurg. 1999;102(9):708–715. doi: 10.1007/s001130050469. [DOI] [PubMed] [Google Scholar]
- 11.Moneim M.S., Garst J.R. Vascular injuries associated with elbow fractures and dislocations. Int. Angiol. 1995;14(3):307–312. [PubMed] [Google Scholar]
- 12.Brahmamdam P., Plummer M., Modrall J.G., Megison S.M., Clagett G.P., Valentine R.J. Hand ischemia associated with elbow trauma in children. J.Vasc. Surg. 2011;54(3):773–778. doi: 10.1016/j.jvs.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Plummer J.M., McFarlane M.E., Jones K.G., Mitchell D. Popliteal artery transection associated with blunt knee injury: controversies in management – a case report. West Ind Med J. 2005;54(1):82–84. doi: 10.1590/s0043-31442005000100016. [DOI] [PubMed] [Google Scholar]
- 14.Ramphal P.S., Irvine R.Q., Spencer H.W. Penetrating injury to the great vessels. Case reviews and management approaches for West Indian surgeons. West Ind. Med. J. 2000;49(2):134–137. [PubMed] [Google Scholar]
- 15.Williams E.W., Cawich S.O., James M., Felix R.A., Ashman H., Douglas V., Williams-Johnson J., French S., McDonald A.H. Penetrating neck trauma and the aberrant subclavian artery. West Ind. Med. J. 2007;56(3):288–293. doi: 10.1590/s0043-31442007000300021. [DOI] [PubMed] [Google Scholar]
- 16.Crandon I.W., Harding H.E., Cawich S.O., McDonald A.H., Fearron-Boothe D. Motorcycle accident injury profiles in Jamaica: an audit from the University Hospital of the West Indies. Int. J. Inj. Contr. Saf. Promot. 2009;16(3):175–178. doi: 10.1080/17457300903024236. [DOI] [PubMed] [Google Scholar]
- 17.Naraynsingh V., Ramdass M.J. Missile injury by a weed wacker resulting in a false aneurysm of the brachial artery. Open Cardiovasc. Med. J. 2011;5:218–219. doi: 10.2174/1874192401105010218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramroop S., Turner M.C., Bynoe R., Garner M.J., Clarke R., Krewski D., Francis M. Injury surveillance in Trinidad: an accident and emergency based injury surveillance system at the San Fernando General Hospital. West Ind. Med. J. 2009;58(2):118–123. [PubMed] [Google Scholar]
- 19.Ayel J.E., Bonnevialle N., Lafosse J.M., Pidhorz L., Al Homsy M., Mansat P., Chaufour X., Rongieres M., Bonnevialle P. Acute elbow dislocation with arterial rupture: analysis of nine cases. Orthop. Traumatol. Surg. Res. 2009;95(5):343–351. doi: 10.1016/j.otsr.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 20.Siebenlist S., Reeps C., Kraus T., Martetschläger F., Schmitt A., Stöckle U., Freude T. Brachial artery transection caused by closed elbow dislocation in a mature in-line skater: a case report with review of the literature. Knee Surg. Sports Traumatol. Arthrosc. 2010;18(12):1667–1670. doi: 10.1007/s00167-010-1202-5. [DOI] [PubMed] [Google Scholar]
- 21.Guler F., Baz A.B., Kose O., Cicek E.I., Akalin S. Delayed diagnosis of rupture of brachial artery due to closed posterior elbow dislocation. Hong Kong J. Emerg. Med. 2011;18:112–115. [Google Scholar]
- 22.Soh R.C., Tawng D.K., Mahadev A. Pulse oximetry for the diagnosis and prediction for surgical exploration in the pulseless perfused hand as a result of supracondylar fractures of the distal humerus. Clin. Orthop. Surg. 2013;5(1):74–81. doi: 10.4055/cios.2013.5.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sparks S.R., DeLaRosa J., Bergan J.J., Hoyt D.B., Owens E.L. Arterial injury in uncomplicated upper extremity dislocations. Ann. Vasc. Surg. 2000;14(2):110–113. doi: 10.1007/s100169910020. [DOI] [PubMed] [Google Scholar]
- 24.Garrigues G.E., Patel M.B., Colletti T.P., Weaver J.P., Mallon W.J. Thrombosis of the brachial artery after closed dislocation of the elbow. J. Bone Joint. Surg. 2009;91:1097–1099. doi: 10.1302/0301-620X.91B8.21882. [DOI] [PubMed] [Google Scholar]
- 25.Benedetti Valentini M., Farsetti P., Martinelli O., Laurito A., Ippolito T. The value of ultrasonic diagnosis in the management of vascular complications of supracondylar fractures of the humerus in children. Bone Joint J. 2013;95(5):694–698. doi: 10.1302/0301-620X.95B5.31042. [DOI] [PubMed] [Google Scholar]
- 26.Carter S.J., Germann C.A., Dacus A.A., Sweeney T.W., Perron A.D. Orthopedic pitfalls in the ED: neurovascular injury associated with posterior elbow dislocations. Am. J. Emerg. Med. 2010;28(8):960–965. doi: 10.1016/j.ajem.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 27.Seigerman D.A., Choi D., Donegan D.J., Yoon R.S., Liporace F.A. Upper extremity compartment syndrome after minor trauma: an imperative for increased vigilance for a rare, but limb-threatening complication. Patient Saf. Surg. 2013;7(1):5. doi: 10.1186/1754-9493-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim J.Y., Buck D.W., Forte A.J., Subramanian V.S., Birman M.V., Schierle C.F., Kloeters O., Mattox K.L., Wall M.J., Epstein M.J. Risk factors for compartment syndrome in traumatic brachial artery injuries: an institutional experience in 139 patients. J. Trauma. 2009;67(6):1339–1344. doi: 10.1097/TA.0b013e318197b999. [DOI] [PubMed] [Google Scholar]
- 29.Hori D., Noguchi K., Nomura Y., Lefor A., Tanaka H. Small incision fasciotomy in a patient with compartment syndrome and peripheral arterial occlusive disease. Ann. Thoracic Cardiovasc. Surg. 2013;19(3):234–238. doi: 10.5761/atcs.cr.12.01904. [DOI] [PubMed] [Google Scholar]
- 30.Fowler J.R., Kleiner M.T., Das R., Gaughan J.P., Rehman S. Assisted closure of fasciotomy wounds: a descriptive series and caution in patients with vascular injury. Bone Joint Res. 2012;1(3):31–35. doi: 10.1302/2046-3758.13.2000022. [DOI] [PMC free article] [PubMed] [Google Scholar]


