Highlights
-
•
We presented a dengue hemorrhagic fever case that evolved with sudden deafness.
-
•
Dengue hemorrhagic is a vascular leak syndrome.
-
•
The etiology of sudden deafness is not well established in literature.
-
•
Viral and vascular are possible causes of sudden deafness.
-
•
The association of sudden deafness with dengue is been questioned.
Keywords: Dengue, Sensorineural deafness, Hearing loss
Abstract
Introduction
Dengue is an acute febrile infectious disease, with high fever followed by symptoms flu-like. Dengue hemorrhagic fever (DHF) is a vascular leak syndrome and could present spontaneous bleeding and worsening of symptoms after some days. Dengue could have some ENT manifestations, however hearing loss is not one of them. Sudden hearing loss is considered as sensorineural or perceptual hearing loss with a sudden onset in a person without other prior otological history. The relation between infectious diseases and sudden hearing are been investigated, some viruses were already linked, but the relation between dengue virus and sudden hearing still remains unknown. This article has the goal of presenting a case of DHF that evolved with SSHL in his hospitalization process.
Presentation of case
We report a 60 years-male patient of with DHF who developed bilateral secretory otitis media and sensorineural hearing loss after the fifth day of onset of symptoms. His hearing loss remained even after 7 months and the patient was referred for hearing aid fitting.
Discussion and conclusion
This is the first case report that brings together DHF and sudden hearing loss. In the development of this case no other cause to sudden hearing loss was found and the correlation between dengue and hearing loss was questioned. In the literature review was found that some viruses, as mumps virus, varicella-zoster virus and HSV-1 and HSV-2 are related to sudden hearing loss, all of them fit in the viral theory. Besides the viral theory of sudden hearing loss, there is the vascular theory that is the occlusion of the end artery that supplies the cochlea. DHF has a vascular commitment, and the hypothesis of a vascular cause could be elicited in this case. Many studies in this area are needed and this article has the objective of elicit the discussion about the subject. Could dengue be associated with sensorineural hearing loss?
1. Introduction
Dengue is considered the most important arboviral disease affecting humans in terms of morbidity and mortality.1,2 Dengue is the most rapidly spreading mosquito-borne viral disease in the world. In the last 50 years, incidence has increased 30-fold with increasing geographic expansion to new countries and, in the present decade, from urban to rural settings.2 It constitutes a serious public health problem in the world,1–3 an estimated 50 million infections per year occur across approximately 100 countries,1,2 and approximately 2.5 billion people live in dengue endemic countries.2
Dengue is an acute febrile infectious disease caused by one of the four RNA viruses (dengue virus type 1–4),1–4 which belongs to the family Flaviviridae and is transmitted by the Aedes aegypti mosquito.1–6 This antigenic diversity is important, since the lack of long-term cross-immunity among the four virus types allows for multiple sequential infections.1
The majority of patients is asymptomatic or display mild symptoms of dengue fever (DF) which include rapid onset of fever, viremia, headache, pain, and rash.1–3 Patients with Dengue Hemorrhagic fever (DHF) and Dengue shock Syndrome (DSS) display symptoms of DF in addition to increased edema, hemorrhage, thrombocytopenia, and shock.1–5
After an incubation period of 3–7 days, symptoms start suddenly and follow three phases: an initial febrile phase, a critical phase around the time of defervescence, and a spontaneous recovery phase. The initial phase is typically characterized by high temperature (≥38.5 °C) accompanied by headache, vomiting, myalgia, and joint pain, sometimes with a transient macular rash. Mild hemorrhagic manifestations such as petechiae and bruising, particularly at venipuncture sites, and a palpable liver are commonly noted. This phase lasts for 3–7 days, after which patients recover without complications.1–3
In Dengue Hemorrhagic the initial symptoms are the same, but on the third or fourth day, the condition worsens with agitation, lethargy, increased pulse rate, hypotension, hemorrhagic manifestations spontaneous, cyanosis and decreasing temperature.1–3
In a small proportion of patients, typically in children and young adults, a systemic vascular leak syndrome becomes apparent around the time of defervescence, evidenced by increasing hemoconcentration, hypoproteinemia, pleural effusions, and ascites. The altered vascular permeability is short-lived, reverting spontaneously to a normal level after approximately 48–72 h, and is concurrent with rapid improvement in the patient's symptoms.1
There is no evidence that the virus infects endothelial cells.4 Although no specific pathway has been identified linking known immunopathogenic events with definitive effects on microvascular permeability, thromboregulatory mechanisms, or both, preliminary data suggest that occurs a transient disruption in the function of the endothelial glycocalyx layer occurs.1
ENT manifestations observed in Dengue reported in the literature are sore throat, runny nose, nasal congestion, ear pain, dizziness, epistaxis, salivary glands alterations, tinnitus, and gingival bleeding.3
Sudden hearing loss (sudden deafness – SD) is considered as sensorineural or perceptual hearing loss with a sudden onset, within 72 h, with a loss of over 30 dB, in at least 3 consecutive frequencies of tonal audiometry, without other prior otological history.7,8
The precise cause of sudden sensorineural hearing loss has not been identified, although several pathophysiological mechanisms have been proposed.8,9 Possible causes are autoimmune forms (sarcoidosis, multiple sclerosis, Crohn's disease), immune-mediated inner ear disease,10 infectious (infectious mononucleosis, syphilis, meningitis, HIV infections, etc.), neoplastic or vascular.7,8
Evidence suggests that varicella-zoster virus can cause sudden hearing loss8,9,11 in patients with Ramsay Hunt syndrome, also evidence from case series suggests that mumps virus can be a cause, accounting for about 7% of adult cases.8 The data for other viruses are conflicting and incomplete.8
In a study in Boston, was detected seroconversion with mumps, rubella, varicella-zoster virus, cytomegalovirus, or influenza in 63% of 122 patients; whereas in a Greek study with 262 patients with unilateral sudden hearing loss only in 27% the serological tests showed recent infection by Epstein–Barr virus, herpes simplex type I and II virus, or cytomegalovirus.8
There is no other description in medical literature that correlates dengue with hearing loss in any time of the natural evaluation of this pathology. This paper aims to describe a case of a patient with hemorrhagic dengue who had sudden hearing loss during his hospitalization process.
2. Methods
A clinical retrospective study of medical records of a patient who had bilateral hemorrhagic dengue and that developed deafness after this clinical situation.
This article was performed after a review of the medical literature in PubMed and SciELO/Lilacs, covering articles published since 1980 in Portuguese, Spanish or English, using the following terms (MeSH terms): “dengue”; “deafness”; “hearing loss”; “sudden hearing loss”.
2.1. Inclusion and exclusion criteria
Only patients with confirmed diagnosis (clinical and radiological) of heamorragic dengue who developed sensorioneural deafness after this clinical situation.
The medical records of the subjects were used in this review and detailed all the parameters this medical evaluation.
2.2. Ethics
The institutional review board approved this study and all subjects gave written informed consent. This case report complies with the rules of the ethics committee of the institution.
3. Case report
Male patient, 60 years old, white, farm worker. Patient sought emergency after onset of acute severe febrile illness without control with anti-thermal and petechial rush in the limbs and trunk, associated with generalized arthralgia, headache and nausea. The blood count showed hemoconcentration and thrombocytopenia (3000). Hospitalized for diagnostic evaluation and treatment of a possible framework for dengue. Denied comorbidities, use of drugs, surgery or other hospitalizations. Still denied any change in hearing acuity before.
He was treated with intravenous hydration and transfusion of platelet concentrates showing improved platelet count after the fourth day. Serology for dengue confirmed the suspected diagnosis. On the third day of hospitalization he developed ascites and small pleural effusion which reversed spontaneously after 3 days. On the fourth day presented confusional clinical picture with normal cranial computed tomography improvement on the next day. It was detected bilateral secretory otitis media associated with hearing loss after the fifth day, being conducted treatment with amoxicillin and clavulanate. On the eighth day of hospitalization he was discharged lying stable, afebrile, only presenting bilateral hearing impairment, antibiotic was maintained for 7 days.
Fifteen days after discharge, he sought the otolaryngologist and performed audiometry presenting right sensorineural hearing loss with a descending trend and average of up to 2 kHz of 60 dB showing loss until getting no response at high frequencies and on the left side showed no response at all frequencies (Fig. 1). He was appointed to bilateral hearing aids, showing partial improvement reported by patient.
Fig. 1.
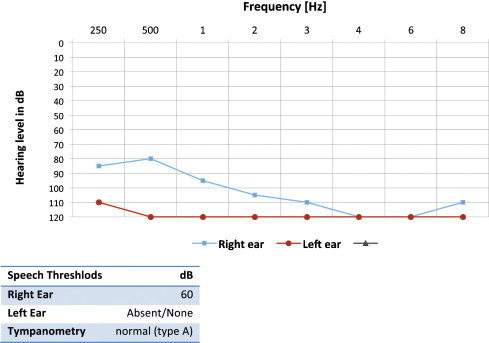
Pure tone audiometric thresholds 15 days after hospitalization.
After 7 months he repeated audiometry for control, showing worsening of hearing loss on the right with worsening to around 30 dB for frequencies up to 3000 Hz (Fig. 2). Kept guiding the use of hearing aids and periodic reevaluations.
Fig. 2.
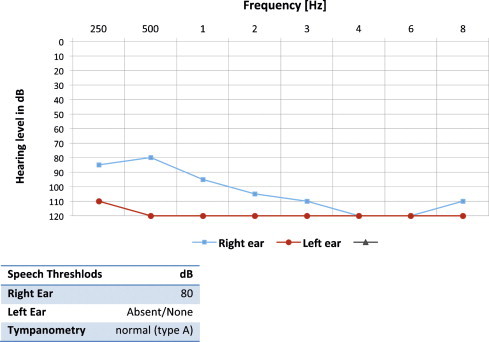
Pure tone audiometric thresholds 7 months after hospitalization.
The study with magnetic resonance imaging and computerized tomography of skull and ears showed no changes of any kind. Patient still was also subjected to a full laboratory investigation being researched autoimmune, genetics, inflammatory and infectious with no apparent changes identified. It was not identify any cause related to deafness besides the hemorrhagic dengue.
4. Discussion
In the case presented the patient was diagnosed with dengue and with sudden sensorineural hearing loss (SSHL). Dengue is an acute febrile infectious disease1–3 and SSHL is considered as sensorineural or perceptual hearing loss with a sudden onset without other prior otological history.7,8 As it was not found in the patient's history or in exams other cause for hearing loss, the association of SSHL with dengue virus is been questioned once viruses can cause sudden hearing loss, as described in the literature.8–12
Mechanisms involved in the induction of hearing loss by different viruses vary, ranging from direct damage to inner ear structures to induction of host immune-mediated damage. Viruses as mumps virus and varicella-zoster virus had already been linked to SSHL.8–10 On the other hand, in the literature no relation with arbovirus infection, which causes dengue and hearing loss was described.
There are mechanisms that have been proposed to explain how a viral infection can lead to SD. As first mechanism the viral invasion of the fluid spaces and/or soft tissues of the cochlea (cochleitis) or invasion of cochlear nerve (neuritis). The second mechanism is reactivation of a virus that is latent within tissues of the inner ear. There is a third scenario that does not deal strictly with a direct viral attack on the inner ear. This third mechanism involves a systemic or distant viral infection that triggers an antibody response that cross-reacts with an inner ear antigen (the immune-mediated hypothesis).8–10
Westmore et al. were able to isolate live mumps virus from the perilymph of a young woman who presented with SSHL after mumps parotitis. This is the only report that has demonstrated a direct role of a virus as a causative agent in SSHL.10,13
The symptoms that frequently are unspecific: patients with fever, without any changes in physical examination or with only a mild hyperemia of oropharynx and nasal mucosa; lead to suspicious of a viral process. Dengue, as differential diagnosis is quite important in the presence of the epidemic situation.1–3
Headache usually of frontal location is a frequent general manifestation, reaching 93% of cases.3,5 Also, retro-orbital pain often associated with nasal obstruction and rhinorrhea can present in cases of dengue, simulating a case of acute sinusitis. Symptoms related to the ear, ear pain, vertigo and tinnitus appear in 36.6%, 20.0% and 6% of cases of dengue, respectively.3,5 The ear pain is, usually unilateral and intense and hardly improves with simple analgesics and may persist for days. Vertigo is rotational and presents itself persistent and recurrent, staying in some cases within 30 days after the viral infection.3,5 However, SSHL has not been described in the literature as a dengue manifestation.
In the course of this case, the patient presented a systemic vascular leak syndrome, evidenced by pleural effusions, and ascites. It was suspected that the patient had dengue hemorrhagic, with the recent revision of the WHO this patient would be classified as having severe dengue (one of those: plasma leaking resulting in shock, accumulation of serosal fluid sufficient to cause respiratory distress, or both; severe bleeding; and severe organ impairment).1,2,4
The cardinal manifestations of DHF, plasma leakage and hemorrhagic tendency, are suggestive of changes in the vascular functions.1,4 A common observation from autopsy or biopsy studies has been diapedesis of circulating mononuclear and red blood cells across the vascular endothelium, perivascular cellular accumulation and edema. But, the extent of endothelial cell death and inflammatory cell infiltration are usually minimal and are not likely the underlying mechanism of increased vascular permeability.4
Some studies showed that during shock phase in severe dengue cases there was an increased urinary excretion of small protein molecules such as albumin and transferrin in comparison to the excretion rate measured after recovery.4
Although glomerular vascular bed is not the major site where leakage occurs in DHF, these findings may reflect the perturbation of vascular permeability regulation that occurs at other anatomical sites such as the pleural and abdominal cavities.4
Even though, the disruption in the endothelial cells in the dengue has not been proved,1–4 there is a vascular leak syndrome in hemorrhagic dengue that can affect any vascular segment in the body.1,3–5 As other causes of sudden hearing loss were discarded in this case, the probability of the sudden hearing loss being a consequence of a vascular alteration caused in the course of hemorrhagic dengue is been questioned.
The cochlea is supplied by an end artery, and vascular occlusion was postulated as a cause of sudden hearing loss since 1949.8 However, many clinical and experimental studies do not support this theory.8,10 The labyrinthine artery is a terminal artery that supplies both the cochlea and the vestibular sensory organ.8
Therefore, it is difficult to explain cases of SSHL without vertigo using the vascular theory. The experimental compromise of the cochlear blood supply results in an irreversible hearing loss after 1 h of occlusion even if the flow is restored subsequently.8
In the described case were searched all other causes of deafness and nothing was found, after an intense investigation. The only positive and correlated factor was the dengue hemorrhagic fever. So this article elicits the hypothesis that these two conditions are correlated.
However, it is not possible to assert a relationship cause and effect type between these two conditions in a study of this kind, but we always must perform carefully differential diagnosis and further studies can help clarify this doubt.
Most patients with sudden sensorineural hearing loss cannot be given a cause for their diagnosis. The evidences indicates that viral and vascular can, in some cases, lead to sudden deafness. However, the published evidence cannot support these two causes as a commom cause. Hence, future study to elucidate the precise etiopathogenesis of sudden deafness is vital for the appropriate approach and treatment of this condition.
5. Final comments
In our literature review no case report or study was found relating sudden hearing loss with dengue fever. As a case report this article has no strength to establish a correlation cause and effect between dengue and sudden hearing loss. Still, this case report can be a spark in the study of the relation of these conditions and help other studies to understand the viral and vascular etiology of sudden deafness.
Conflict of interest
The authors declare that they have no competing interests.
Funding
None.
Ethical approval
According to the standards of the Ethics Committee of the institution.
Authors’ contributions
Bruna Natália Freire Ribeiro wrote the manuscript and reviewed the literature. Carlos Eduardo Monteiro Zappelini, Alexandre Guimarães Caixeta, Felipe Yazawa, Guilherme Machado de Carvalho and Edi Lucia Sartorato were also involved in the process of reviewing the literature. Felipe Yazawa translated and reviewed the study. Tammy Fumiko Takara Messiah was responsible for the writing, reviewing and bibliographic section of the study. Guilherme Machado de Carvalho and Edi Lucia Sartorato were involved in the advising and reviewing of the study.
Acknowledgements
We would like to thanks the ORL staff for all help needed and the subjects.
Contributor Information
Bruna Natália Freire Ribeiro, Email: bruninhatalia@gmail.com.
Alexandre Caixeta Guimarães, Email: alecgxl2@hotmail.com.
Felipe Yazawa, Email: felipeyazawa@gmail.com.
Tammy Fumiko Messias Takara, Email: tammymessias@gmail.com.
Guilherme Machado de Carvalho, Email: guimachadocarvalho@gmail.com.
Carlos Eduardo Monteiro Zappelini, Email: czappelini2@hotmail.com.
References
- 1.Simmons C.P., Farrar J.J., Vinh Chau N., Wills B. Dengue. N Engl J Med. 2012;366:1423–1432. doi: 10.1056/NEJMra1110265. [DOI] [PubMed] [Google Scholar]
- 2.WHO . 2009. Dengue guidelines for diagnosis, treatment, prevention and control – new edition.http://www.who.int/topics/dengue/en/ [PubMed] [Google Scholar]
- 3.Guzman M.G., Kourí G. Dengue: an update. Lancet Dis. 2002;2(1):33. doi: 10.1016/s1473-3099(01)00171-2. [DOI] [PubMed] [Google Scholar]
- 4.Srikiatkhachorn A., Kelley J.F. Endothelial cells in dengue hemorrhagic fever. Antiviral Res. 2014;109:160–170. doi: 10.1016/j.antiviral.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fonseca B.A., Fonseca S.N. Dengue virus infections. Curr Opin Pediatr. 2002;14(1):67–71. doi: 10.1097/00008480-200202000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Figueiredo R.M.P., Mourão M.P.G., Abi-Abib Y.E.C., Oliveira C.M., Roque R., Azara T. Identification of dengue viruses in naturally infected Aedes aegypti females captured with BioGents (BG) – sentinel traps in Manaus, Amazonas, Brazil. Rev Soc Bras Med Trop. 2013;46(2):221–222. doi: 10.1590/0037-8682-1096-2013. [DOI] [PubMed] [Google Scholar]
- 7.Plaza G., Durio E., Herráiz C., Rivera T., García-Berrocal J.R. Asociación Madrileña de ORL. Consensus on diagnosis and treatment of sudden hearing loss. Asociación Madrileña de ORL. Acta Otorrinolaringol Esp. 2011;62(2):144–157. doi: 10.1016/j.otorri.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 8.Schreiber B.E., Agrup C., Haskard D.O., Luxon L.M. Sudden sensorineural hearing loss. Lancet. 2010;375:1203–1211. doi: 10.1016/S0140-6736(09)62071-7. [DOI] [PubMed] [Google Scholar]
- 9.Merchant S.N., Durand M., Adams J.C. Sudden deafness: is it viral? ORL J Otorhinolaryngol Relat Spec. 2008;70(1):52–62. doi: 10.1159/000111048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greco A., Fusconi M., Gallo A., Marinelli C., Macri G.F., Vincentiis M. Sudden sensorineural hearing loss: an autoimmune disease? Autoimmun Rev. 2011;10:756–761. doi: 10.1016/j.autrev.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Cohen B.E., Durstenfeld A., Roehm P.C. Viral causes of hearing loss: a review for hearing health professionals. Trends Hear. 2014;18:1–17. doi: 10.1177/2331216514541361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scalia G., Palermo C.I., Maiolino L., Costanzo C.M., Zappalà D., Grillo C. Detection of serum IgA to HSV1 and its diagnostic role in sudden hearing loss. New Microbiol. 2013;36:41–47. [PubMed] [Google Scholar]
- 13.Westmore G.A., Pickard B.H., Stern H. Isolation of mumps virus from the inner ear after sudden deafness. BMJ. 1979;1:14–15. doi: 10.1136/bmj.1.6155.14. [DOI] [PMC free article] [PubMed] [Google Scholar]


