Abstract
Background
The use of computer assisted joint replacement has facilitated precise intraoperative measurement of knee kinematics. The changes in “screw home mechanism” (SHM) resulting from Total Knee Arthroplasty (TKA) with different prostheses and constraints has not yet been accurately described.
Methods
A pilot study was first completed. Intraoperative kinematic data was collected two groups of 15 patients receiving different prostheses.
Results
On average, patients lost 5.3° of ER (SD = 6.1°). There was no significant difference between the prostheses or different prosthetic constraints.
Conclusions
There significant loss of SHM after TKA. Further research is required to understand its impact on patient function.
Keywords: Arthroplasty, Knee rotation, Screw home mechanism, Computer assisted surgery, Osteoarthritis
1. Introduction
Osteoarthritis (OA) of the knee affects 12.5% of the population aged 45 years or over.1 Total Knee Arthroplasty (TKA) is the definitive treatment once less invasive modalities have been explored. TKA successfully relieves pain and corrects functional abnormalities associated with severe OA of the knee.2,3 While good results are usually reported, it has been found that only 70–84% of TKA patients are satisfied with the function of their prostheses for activities of daily living.4 At one year or more post-TKA, 72% of patients have limited ability to kneel, 75% are limited in squatting and 54% experience limited ability to garden.5 These issues may be attributable to prosthesis kinematics not matching those of a natural knee.6
The two major variations in TKA constraint are Cruciate Retaining (CR) and Posterior Stabilized (PS). The Australian Joint Replacement Registry 2010 Annual Report demonstrates that PS knees are used in 23% of Total Knee Replacements performed in Australia.7 Variations in constraint and design of implants result in changes to knee kinematics. While neither design reproduces normal knee kinematics,8–10 it has been shown that PS designs more closely resemble the natural kinematics of the knee with regard to femoral “roll back”.11 It has also been well documented that patients who receive PS designs gain a greater degree of flexion, which is statistically significant but of uncertain clinical significance.12 The intra-operative effect of TKAs on the SHM has not yet been examined in detail. Research suggests that the SHM relies on the 4-bar linkage system in the knee, which requires functioning anterior and posterior cruciate ligaments.13 Arthritis of the knee causes changes in the path of motion and joint laxity.6 One would anticipate that these changes persist post TKA, even with appropriate component alignment and balance. These changes should particularly affect tibial internal-external rotations and anterior-posterior translations, across the range of knee flexion-extension. Variations in this axial rotation may contribute to patient dissatisfaction post TKA. The recent introduction of computer navigation has allowed for detailed intraoperative analysis of knee kinematics, enabling prosthetic implants to be examined precisely.6
It has been suggested that reproducing natural knee kinematics post TKA will increase patient satisfaction, rehabilitation and extensor function whilst improving the longevity of the implant itself.14 The aim of this study is to examine the kinematics of OA and post-TKA knees with respect to SHM, and to compare the impact of different prostheses and levels of prosthetic constraint. We hypothesised that SHM would decrease post TKA and that PS knees would more closely resemble their pre-operative counterparts than CR knees.
2. Materials and methods
The inclusion and exclusion criteria for this study are shown in table one (Table 1). Initially a retrospective review was performed on 50 patients (54 knees) undergoing navigated TKA with Cruciate Retaining Genesis II prostheses. This sample group included 26 females (mean age 67 years) and 24 males (mean age 65 years). All patients underwent the procedure using Orthosoft V.2.1 software (Zimmer, Wasaw, Indiana). The total ER of the tibia relative to the femur was determined during intraoperative extension (from 90° flexion to maximum extension) using the computer navigation system (see Fig. 1). Total average ER of the pre-operative knees was compared to the ER post-operatively using a paired two tailed sample t-test and SPSS V.16 software. For the purposes of this review a p value of <0.05 was considered to be statistically significant.
Table 1.
Inclusion and exclusion criteria for study participation.
| Inclusion criteria | Exclusion criteria |
|---|---|
| 1. Patient presents with osteoarthritis, requiring total knee replacement. 2. Patient is receiving the surgeon's standard PS or CR prosthesis. 3. Patient has given appropriate consent. |
1. Patient has an active, local infection or systemic infection. 2. Patient has grade 3 collateral ligament insufficiency. 3. Patient has knee flexion <90°. 4. Patient has fixed flexion deformity >15°. 5. Patient has an inflammatory arthropathy. |
Fig. 1.
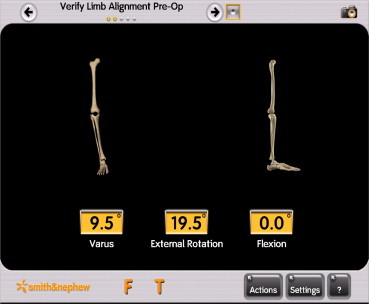
A snapshot from the computer navigation system showing how the data was collected.
Subsequent to the retrospective review, detailed rotational data was collected to allow comparison between two different prostheses and different levels of prosthetic constraint. This analysis was performed on two groups of 15 patients, each group consisted of patients who met the inclusion criteria and received consecutive operations. One group received Genesis II prostheses (Smith and Nephew, Memphis, Tennessee) and the other received the Scorpio NRG (Stryker, Mahwah, New Jersey). The Genesis II group underwent the procedure with the aid of Orthosoft V.2.1 navigation system (Zimmer, Warsaw, Indiana), and the Scorpio NRG procedures were performed with the aid of Precision Navigation V.4.0 (Stryker, Mahwah, New Jersey). In both series, the navigation equipment (and rotational axis) was calibrated using the same landmarks (centre of hip, centre of ankle, posterior femoral condyles, tibial plateau and anterior tibial eminence). Once the navigation landmarks were identified, tibial rotation was then recorded at 0°, 15°, 30°, 60° and 90° flexion. Care was taken to avoid axial rotation or any additional torque forces by the surgeon when recording values. If full extension was not possible pre operatively, the rotation in maximal extension was recorded. Tibial rotation at 90° flexion was the baseline for internal-external rotation measurements and hence was considered to be 0°ER in all cases. The initial measurements were made prior to replacement (representative of the preoperative knee). Once the final tibial and femoral components were cemented in situ, the measurements were then repeated with a Cruciate Retaining (CR) trial polyethylene insert in place and then again with the final Posterior Stabilized (PS) polyethylene insert.
Once the data was collected and collated for each individual group it was analysed using SPSS V.16 software to perform paired two tailed sample t-tests. The total loss of rotation for the Genesis II and Scorpio groups was then compared using an independent t-test. A p value of < 0.05 was considered significant. The study was approved by the South Eastern Area Health Service institutional review committee.
3. Results
The retrospective review showed that, on average, total ER was 14.9° (SD = 6.0°) prior to undergoing the TKA. With the components in situ, using the CR Genesis II system the average total ER when the knee was extended was 8.2° (SD = 6.1°), demonstrating an average loss of 6.7° ER (SD = 5.5°, p < 0.001).
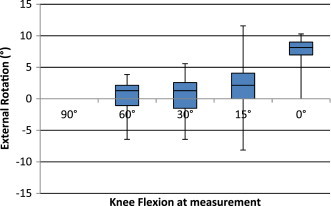
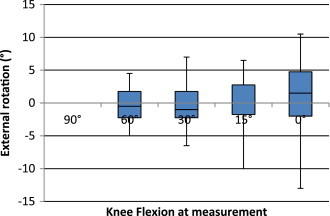
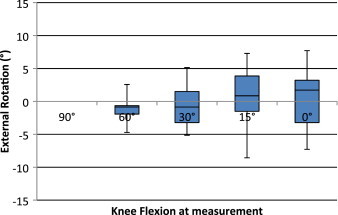
In the prospective groups, the Genesis II pre-operative group demonstrated an average total ER during extension of 16.1° (SD = 4.4°) (Fig. 2). The CR group retained 8.6° (SD = 5.2°) (Fig. 3) and the PS group retained 8.3° (SD = 5.6°) (Fig. 4). The difference between pre-operative and post-operative groups was statistically significant (CR group p < 0.001 and PS group p < 0.001). However there was no significant difference between the CR and PS groups (p = 0.477).
Fig. 2.
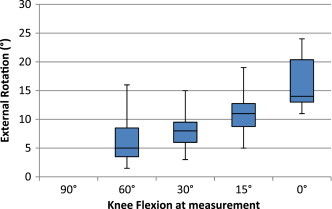
Box-plot of ER profile for pre-operative Genesis II group.
Fig. 3.
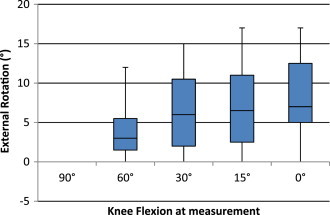
Box-plot of ER profile for CR Genesis II group.
Fig. 4.
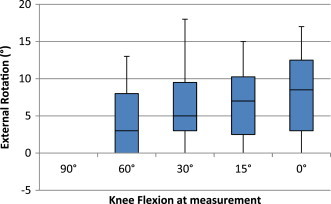
Box-plot of ER profile for PS Genesis II group.
The Scorpio NRG prosthesis showed similar results with average ER of the pre-operative knees was 8.3° (SD = 4.6°) (Fig. 5) and the ER in CR and PS groups was 1.1° (SD = 5.8°) (Fig. 6) and 0.7° (SD = 5.0°) (Fig. 7) respectively. There was a significant difference between the pre-operative and post-operative results using CR (p = 0.02) and PS (p = 0.01) TKA, but no significant difference when the CR and PS groups were compared to each other (p = 0.75). Of note, the average loss of ER in terminal extension was not significantly different when comparing the Genesis II prosthesis with the Scorpio NRG (p = 0.08).
Fig. 5.
Box-plot of ER profile for Pre-operative Scorpio group.
Fig. 6.
Box-plot of ER profile for CR Scorpio NRG group.
Fig. 7.
Box-plot of ER profile for PS Scorpio NRG group.
4. Discussion
This study confirms our hypothesis that patients who have undergone TKA experience significant loss of the SHM. This is consistent with other studies and, as suggested in the literature, this is likely to be a consequence of both the resection of the ACL and the design of the implant.2,15 We also found no significant difference between different prostheses or levels of prosthetic constraint in this regard.
The limitations of this study include the fact that the SHM is a dynamic movement which results from both the physical structure of the knee and muscular involvement. Consequently, measuring SHM in a passive model is challenging. The rotational measurements obtained by computer navigation are also impacted by the forces applied by the surgeon's hands. Additionally, the SHM varies significantly between patients so comparison between relatively small groups is difficult. As such, it was felt that the use of a crossover study was appropriate, despite the need to assess the CR prostheses after PCL resection with trial components only. The authors felt that this CR measurement should be included in analysis because it may provide an approximation of CR prostheses kinematics. This was because research has demonstrated that the function of the PCL in controlling knee rotation is often compromised post-TKA.16 The SHM is known to be reduced in arthritic knees.2,6 Ideally, a study of knee kinematics would directly compare post-operative knees to healthy knees. However, such a study would be very difficult to perform.
Detailed research on the changes to knee kinematics post TKA is vital for future improvements in prosthetic design. Many studies have focused on movement in the sagittal plane; however few have documented the changes in rotational kinematics. It has been shown that post-TKA patients experience changes in swing patterns and sagittal movement patterns.17 It is not known to what degree the loss of rotation in terminal extension contributes to this and how these changes impact on functionality post-TKA.
5. Conclusion
Our study shows that knees lose SHM after TKA using the Genesis II and Scorpio NRG systems when compared to pre-operative arthritic knees. This was independent of PS or CR design. Further research to validate these findings and determine clinical significance may lead to improvements in prosthetic design, and consequently improve patient satisfaction.
Conflicts of interest
All authors have none to declare.
References
- 1.Bedson J., Jordan K., Croft P. The prevalence and history of knee osteoarthritis in general practice: a case–control study. J Fam Pract. 2005;22:103–108. doi: 10.1093/fampra/cmh700. [DOI] [PubMed] [Google Scholar]
- 2.Siston R., Giori N., Goodman S., Delp S. Intraoperative passive kinematics of osteoarthritic knees before and after total knee arthroplasty. J Orthop Res. 2006;24:1607–1614. doi: 10.1002/jor.20163. [DOI] [PubMed] [Google Scholar]
- 3.Carr A., Robertson O., Graves S. Knee replacement. Lancet. 2012;379:1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 4.Bourne R., Chesworth B., Davis A., Mahomed N., Charron K. Patient satisfaction after total knee arthroplasty. Clin Orthop Relat Res. 2009;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss J.M., Noble P.C., Conditt M.A. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res. 2002;404:172–188. doi: 10.1097/00003086-200211000-00030. [DOI] [PubMed] [Google Scholar]
- 6.Bull A., Kessler O., Alam M., Amis A. Changes in knee kinematics reflect the articular geometry after arthroplasty. Clin Orthop Relat Res. 2008;466:2491–2499. doi: 10.1007/s11999-008-0440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. AOA; Adelaide: 2010. [Google Scholar]
- 8.Uvehammer J., Kärrholm J., Brandsson S. In vivo kinematics of total knee arthroplasty. J Bone Jt Surg. 2000;82:499–505. doi: 10.1302/0301-620x.82b4.10651. [DOI] [PubMed] [Google Scholar]
- 9.Uvehammer J. Knee joint kinematics, fixation and function related to joint area design in total knee arthroplasty. Acta Orthop Scand Suppl. 2001;72:1–52. [PubMed] [Google Scholar]
- 10.Uvehammer J., Kärrholm J., Brandsson S. In vivo kinematics of total knee arthroplasty: flat compared with concave tibial joint surface. J Orthop Res. 2000;18:856–864. doi: 10.1002/jor.1100180603. [DOI] [PubMed] [Google Scholar]
- 11.Banks S., Hodge A. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res. 2004;426:187–193. doi: 10.1097/01.blo.0000138956.04316.ac. [DOI] [PubMed] [Google Scholar]
- 12.Bercik M., Joshi A., Parvizi J. Posterior cruciate-retaining verses posterior-stabilised total knee arthroplasty: a meta-analysis. J Arthroplasty. 2013;28:439–444. doi: 10.1016/j.arth.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 13.Amiri S., Cooke D., Kim I., Wyss U. Mechanics of the passive knee joint. Part 2: interaction between the ligaments and the articular surfaces in guiding the joint motion. J Eng Med. 2007;221:821–832. doi: 10.1243/09544119JEIM181. [DOI] [PubMed] [Google Scholar]
- 14.Patil S., Colwell C., Ezzet K., D'Lima D. Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Jt Surg. 2005;87:332–338. doi: 10.2106/JBJS.C.01467. [DOI] [PubMed] [Google Scholar]
- 15.Moglo K.E., Shirazi-Adl A. Cruciate coupling and screw-home mechanism in passive knee joint during extension-flexion. J Biomech. 2005;38:1075–1083. doi: 10.1016/j.jbiomech.2004.05.033. [DOI] [PubMed] [Google Scholar]
- 16.Yue B., Varadarajan K., Rubash G., Li G. In vivo function of posterior cruciate ligament before and after posterior cruciate ligament-retaining total knee arthroplasty. Int Orthop. 2012;36:1387–1392. doi: 10.1007/s00264-011-1481-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McClelland J.A., Webster K.E., Feller J.A. Gait analysis of patients following total knee replacement: a systematic review. The Knee. 2007;14:253–263. doi: 10.1016/j.knee.2007.04.003. [DOI] [PubMed] [Google Scholar]


